Abstract
The tumor adaptive resistance to therapeutic radiation remains to be a barrier for further improvement of local cancer control. SIRT3, a member of the sirtuin family of NAD+-dependent protein deacetylases in mitochondria, promotes metabolic homeostasis through regulation of mitochondrial protein deacetylation and plays a key role in prevention of cell aging. Here, we demonstrate that SIRT3 expression is induced in an array of radiation-treated human tumor cells and their corresponding xenograft tumors including colon cancer HCT-116, glioblastoma U87 and breast cancer MDA-MB231 cells. The SIRT3 transcriptional activation is due to SIRT3 promoter activation controlled by the stress transcription factor NF-κB. Post-transcriptionally, the SIRT3 enzymatic activity is further enhanced via Thr150/Ser159 phosphorylation by Cyclin B1/CDK1, which is also induced by radiation and relocated to mitochondria together with SIRT3. Cells expressing the Thr150Ala/Ser159Ala mutant SIRT3 show a reduction in the mitochondrial protein lysine deacetylation, ΔΨm, MnSOD activity and mitochondrial ATP generation. The clonogenicity of Thr150Ala/Ser159Ala mutant transfectants is lower and significantly decreased under radiation. Tumors harboring the Thr150Ala/Ser159Ala mutant SIRT3 show inhibited growth and sensitivity to in vivo local irradiation. These results demonstrate that enhanced SIRT3 transcription and post-translational modifications in mitochondria contribute to the adaptive radioresistance in tumor cells. The CDK1-mediated SIRT3 phosphorylation is a potential effective target to sensitize tumor cells to radiotherapy.
Keywords: SIRT3, CDK1, mitochondria, tumor radioresistance, deacetylation
Introduction
Tumor radiotherapy alone or combined with surgery and chemotherapy, continues to be the most powerful tool in cancer growth control (1–3). However, increased tumor resistance to therapeutic radiation especially the recurrent and metastatic lesions with enhanced aggressiveness remains to be the major factor causing poor prognosis and shortening patients’ survival (4–6). Accumulating evidence suggests that tumors can develop so-called adaptive radioresistance to current cancer therapies (7–9). A pro-survival network regulated by the transcription factor NF-κB has been linked with the aggressive growth and radioresistance of a fraction of breast cancer cells surviving long-term irradiation (10–12). Sirtuins are a group of NAD+-dependent histonedeacetylases (HDACs) in mammalian cells and are involved in an array of critical cellular functions including cell proliferation, apoptosis, metabolism, stress responses, aging and longevity (13, 14). Among seven sirtuin members (SIRT1–7), SIRT3 is the best characterized mitochondrial sirtuin, functioning to regulate mitochondrial proteins involved in oxidative phosphorylation, fatty acid oxidation, the urea cycle, and the antioxidant response (14–21). Several studies have highlighted the role of SIRT3 in metabolism and homeostasis in normal cells and revealed new targets and substrates for SIRT3-dependent deacetylation (22). SIRT3 is the primary mitochondrial deacetylase regulating mitochondrial protein lysine acetylation involved in many cellular functions (23). Utilizing the mitochondrial NAD pool, SIRT3 functions as a stress-responsive deacetylase leading to homeostasis and pro-survival effects (24). SIRT3 knockout mice exhibit decreased oxygen consumption and develop oxidative stress in skeletal muscle with a significant reduction in ATP levels in the heart, kidney, and liver (25). Enforced exogenous SIRT3 expression enhances mitochondrial respiration and reduces mitochondrial ROS levels (26). Several key metabolic enzymes in mitochondria are identified to be regulated by SIRT3, including MnSOD that protects the cells by detoxifying reactive oxygen species (27). Recently, SIRT3 is shown to deacetylate ATP synthase F1 to enhance mitochondrial bioenergetics in nutrient and exercise-induced stress (28). These observations suggest that SIRT3 functions as a metabolic sensor that monitors energy availability and directs mitochondrial processes so as energy production matches energy needs as well as consumption. However, how SIRT3 is regulated in tumor cells especially under genotoxic conditions such as therapeutic ionizing radiation (IR) remains to be elucidated.
It is not clear whether SIRT3 gene and/or its post-translational modifications could be regulated under genotoxic stress conditions such as clinical radiotherapy. It has been observed that irradiation of SIRT3-lacking cells result in deterioration of mtDNA, mitochondrial dysfunction, and apoptosis (29) probably due to lack of MnSOD deacetylation and activation by SIRT3 (27). Down-regulation of SIRT3 inhibits growth and sensitizes oral squamous carcinoma cells to IR (30). Recently, Cyclin B1/CDK1 is found to regulate mitochondrial function via phosphorylation of an array mitochondrial proteins including complex I subunits (31) and MnSOD (32), resulting in improved mitochondrial homeostasis and cell cycle progression. In this study, we aim to determine whether SIRT3 transcription can be induced by IR and whether its post-translational modification is involved in CDK1-medaited mitochondrial homeostasis. The data demonstrate that SIRT3 gene transcription is upregulated in tumor cells by IR under the control of NF-κB regulation and SIRT3 enzymatic activity is further enhanced by Cyclin B1/CDK1-mediated Thr150/Ser159 phosphorylation in mitochondria. These results reveal a cooperative mechanism by which SIRT3 enhances mitochondrial homeostasis and tumor adaptive radioresistance; which may serve as an effective target to inhibit tumor growth by radiotherapy.
Materials and Methods
Cell culture and treatment
Human colon carcinoma cell lines HCT116 were kindly provided by Dr. Bert Vogelstein in 2007 (Johns Hopkins University, MD) and maintained in McCoy’s 5A medium supplemented with 10% fetal bovine serum (HyClone, Logan, UT), penicillin (100 units per ml) and streptomycin (100 μg/ml) in a humidified incubator at 37°C (5% CO2). HCT116 cell lines were not authenticated by our lab. MDA 231 and U87 cells were obtained from ATCC in 2004 and 2011, respectively, and were not authenticated by our lab. MDA 231 and U87 cells were maintained in MEM medium supplemented with 10% fetal bovine serum (HyClone, Logan, UT), 1% non-essential amino acids, penicillin (100 units per ml) and streptomycin (100 μg/ml) in a humidified incubator at 37°C (5% CO2). Exponentially growing cells in T75 flask with 70–80% confluence were exposed to radiation at room temperature using a Cabinet X-rays System Faxitron Series (dose rate: 0.997 Gy/min; 130 kVp; Hewlett Packard, McMinnville, OR). Cells that did not receive radiation were used as the sham-IR control. WR1065 was kindly provided by Dr. David Grdina (Northwestern University, IL). 1 M of stock solution was made in PBS immediately before use. Before radiation, cells were treated with WR-1065 at final concentration of 4 mM for 30min or 40 μM for 24h.
Antibodies
Antibodies used in this study were as follows: The antibodies against β-actin (sc-8432), cdc2 p34 (sc-137035), CyclinB1 (sc-245), p53 (sc-126), SOD-2 (sc-133134), NDUFA9 (sc-58392), phospho-serine (sc-81514), phospho-threonine (sc-5267), and caspase-3 (sc-7148) were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). The antibodies against SIRT3 (2627s), acetylated-lysine (9441), Cox IV (4844) were purchased from Cell Signaling (Beverly, MA). Anti-cytochrome c (05-479) was purchased from Upstate Biotechnology (Lake Placid, NY). Anti-FLAG M2 (F-3165) was purchased from Sigma (St Louis, MO).
Mitochondria Isolation
Exponentially growing HCT116 cells at 50–80% confluence were harvested and re-suspended in Buffer A (134mM NaCl, 5mM KCl, 0.7mM Na2HPO4, 2.5mM Tris HCl pH 7.5). After centrifugation, the pellet was resuspended in Buffer B (10mM NaCl, 1.5mM MgCl2, 10mM Tris HCl pH 7.5) and the cells were lysed using a glass homogenizer followed by the addition of Buffer C (2M Sucrose, 35mM EDTA, 50mM Tris HCl pH 7.5). Centrifugation twice got rid of the cell debris and the supernatant was centrifuged at 10000 rpm for 20 minutes to pellet the mitochondria. After washing the pellet with Buffer D (0.33M Sucrose, 1mM EDTA, 8.3mM Tris HCl pH 7.5), the mitochondrial pellet was lysed and stored.
Expression and purification of GST-tagged proteins
Escherichia coli BL-21 containing a GST-tagged SIRT3 expressing vector was cultured in Luria-Bertani (LB) broth with 50 μg/ml of ampicillin until an optical density of 0.6 was reached. To induce fusion protein production, 0.1 mM isopropyl-b-D-thio-galactopyranoside (IPTG) was added, and the culture was incubated for an additional 3 h. The induced culture was collected and suspended in PBS buffer containing 5 mM dithiothreitol, proteinase inhibitor cocktail and 0.1% lysozyme. Cells were lysed by sonication, cellular debris was removed by centrifugation, and the whole cell protein extract was collected in the supernatant. This protein extract was incubated with glutathione-sepharose 4B beads (Pierce Protein Research, IL) at a volume ratio of 4:1 (supernatant: bead) for 1 h. The GST-fusion proteins were eluted from the beads using glutathione elution buffer (10 mM reduced glutathione in 50 mM Tris-HCl, pH 8.0), and the eluted proteins were subjected to dialysis in molecular porous membrane tubing (Spectrum labs) with 1×PBS/1 mM EDTA. The purified protein was analyzed by SDS-PAGE and immunoblotting.
Immunoblotting and co-immunoprecipitation
Unless noted otherwise, cytosolic fraction or total cell or mitochondrial lysates (20 μg) were separated by SDS-PAGE and transferred to a nitrocellulose membrane. The membrane was incubated with specific primary antibody overnight at 4°C, followed by the horseradish peroxidase-conjugated secondary antibody for 1h, and visualized by the ECL Western blotting detection system (Amersham, Arlington Heights, IL). After various treatments, mitochondrial proteins (250–500 μg) were pre-cleared using normal mouse or rabbit IgG and Protein A/G PLUS-Agarose (Pierce). The pre-cleared supernatants were incubated with primary antibodies overnight at 4°C with shaking. The reaction was further incubated with Protein A/G PLUS-Agarose for 3 h at 4°C. The immunoprecipitated samples were rinsed three times with washing buffer (1 M NaCl, 1% NP-40, 50 mM Tris–HCl, pH 8.0) and further analyzed by immunoblotting analysis using different antibodies. Normal IgG was applied as a negative control for immuno-precipitation.
Quantitative RT-PCR analysis
The qRT-PCR primers were as follows: SIRT3 (forward: 5′-tgctcctgcaaattcacacaa-3′, reverse: 5′-atcttggcttttcacatctgcaa-3′); β-actin (forward: 5′-cgtgacatcaa ggagaagct-3′, reverse: 5′-tcgtggataccgcaagattc-3′). Total RNA was extracted from control and irradiated HCT116, U87 and MDA-MB-231 cells and then treated with DNase I. Following reverse transcription reaction, quantitative RT-PCR was performed with Applied Biosystems 7300 Real-Time PCR system using the Taqman mRNA Assay kit. The expression of mRNA was normalized and presented as fold change of each mRNA in radiated cells relative to the sham-radiation controls.
SIRT3 mutant construction and transfection
The mutations of SIRT3 in Thr150 to Alanine and Ser159 to Alanine were generated from the SIRT3-expression vector pCDNA3-SIRT3-Flag (Addgene, NYU) by the QuikChange Site-Directed Mutagenesis Kit using the primers 5′GCC GGC ATC AGC GCA CCC AGT GGC ATT CCA3′ and 5′TGG AAT GCC ACT GGG TGC GCT GAT GCC GGC3′ or 5′ATT CCA GAC TTC AGA GCG CCG GGG AGT GGC CTG and 5′CAG GCC ACT CCC CGG CGC TCT GAA GTC TGG AAT, respectively. The SIRT3 cDNAs were cloned into the pGEX-5X-1 vector using the BamH1and Xho1 sites. Cell transfectants were obtained by using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) and selected with G418 (1 mg/ml) for >14 days.
Ex vivo and in vitro kinase assay
Cyclin B1/CDK1 kinase used for assay was either commercially purchased or isolated from mitochondria from previously irradiated HCT-116 cells by immunoprecipitation purification. SIRT3 protein was endogenous or transfected and purified using immunoprecipitation by anti-SIRT3 or anti-flag antibody, respectively. One microgram recombinant GST-SIRT3 was also used for kinase assays. Specified SIRT3 protein was incubated with designated Cyclin B1/CDK1 kinase in kinase buffer (50 mM Tris-HCl, 10 mM MgCl2, 1 mM EGTA, 2 mM DTT, 0.01% Brij 35, pH 7.5) supplemented with 100 μM of cold ATP and 100 μCi/μmol of [γ-32P] ATP at 30°C for 2 h. The same amount of histone H1 was included as a positive control phosphorylation substrate for Cdk1 and GST-protein served as a negative control. Samples were separated via SDS-PAGE and visualized by autoradiography.
Clonogenic survival assay
Cells were grown until they reached 70% confluence and were subjected to sham or radiation of 5 Gy. At the end of the treatment, both of the sham control and irradiated cells were trypsinized and reseeded on 60-mm tissue culture dishes in triplicates. The cell numbers applied were 9000, 6000, and 3000 cells per plate for the irradiated plates and 3000, 1000, 500 cells per plate for the untreated control plates. Following incubation for 10–12 days after seeding, the media were removed and 2 ml of Coomassie blue staining solution was added to the plates and the clones were stained for 5 minutes. The colonies with more than 50 cells were counted and normalized to the plating efficiency of each cell line.
SIRT3-mediated tumor radioresistance tested by in vivo mouse irradiation
All mouse handling and experiments were conducted according to Animal Care & Use guidelines and IACUC approved protocol. Stable transfected HCT-116 cells with mock, SIRT3 wild-type and SIRT3 mutant were harvested from growing cultures and 3.3×106 cells were injected subcutaneously into the right and left flanks of mouse (n = 6). When individual tumor volume reached ~ 0.1–0.3 cm3 on 7th days after inoculation, a single dose of 5 Gy IR was locally delivered to tumor using an Elekta Beam Modulator Agility linear accelerator (Elekta AB, Crawley, UK). The dose was delivered with 6 MeV electrons directed through a 1 cm cut out for tumor coverage and maximal sparing of the surrounding tissues. A bolus of 0.5 cm “superflab” material was used over the tumor site, which ensured full dose coverage up to the skin surface and further spared the underlying tissues. The thermoluminescent detectors (TLD) were used to calibrate the small field dose with an accuracy of ± 2%. The accuracy of dose delivery was confirmed with a 3D printed phantom representation of the mouse with tumors on each flank. The dose to the irradiated target was measured within 1% of the prescription with a MOSFET detector, with the sham irradiated side was measured at only 4% of the prescription dose. The tumors were measured every 3 days with Vernier calipers, and the tumor volumes were calculated according to the formula 0.52 × a × b2 (a = small diameter, b = large diameter). The tumor volume was normalized to the volume before irradiation. The animal studies were conducted under the IACUC 15315 protocol approved by the University of California Davis Institutional Animal Care and Use Committee for research in vertebrate animals.
Statistical analysis
The data are presented as means ± S.E.M. Statistical significance among groups was determined by using t-tests or one-way ANOVA with SPSS software (version 11.0). The findings were considered significant at P<0.05 and highly significant at P<0.01.
Results
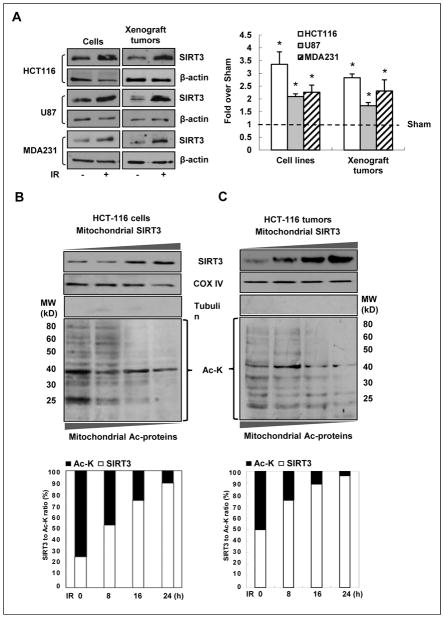
Radiation enhances SIRT3 expression and reduces mitochondrial acetylated proteins
In vitro experiments using human colon cancer HCT-116 cells, breast MDA-MB231, and glioblastoma U87 cells showed that SIRT3 expression was induced after exposure to 5 Gy IR (Fig. 1A). Similarly, in vivo irradiated tumors also showed enhanced SIRT3 expression following 5 Gy irradiation (Fig. 1A). Accordingly, IR-induced SIRT3 expression was timely conjugated with decreased overall mitochondrial protein deacetylation both in HCT116 tumor cells and their xenograft tumor models (Fig. 1B–C). Similar results obtained with MDA231 (Fig. S1A) and U87 cells (Fig. S1B), suggesting a universal mechanism by which radiation induces SIRT3 expression and deacetylation of mitochondrial proteins. The induction of SIRT3 may represent a predominant feature of tumor cells after irradiation.
Figure 1.
Radiation-induced SIRT3 expression results in reduced levels of acetylated proteins both in vitro and in vivo. A, enhanced SIRT3 protein expression in human cancer cell lines and their corresponding mouse xenograft tumors receiving in vitro and local in vivo irradiation. Left panel, western blot of SIRT3 in human colon cancer (HCT-116), glioblastoma (U87) and breast cancer (MDA-MB231) cells and their corresponding mouse xenograft tumors 24 h after sham (−) or 5 Gy IR (+). Right panel, the levels of SIRT3 expression in irradiated cells and tumors were estimated by measuring the band intensity using ImageJ software, normalized with β-actin and compared with the sham radiation controls (n=3, *P < 0.05). B, western blot of SIRT3 as well as the acetylated proteins of mitochondrial fractions isolated from HCT-116 cells and the corresponding xenograft tumors (C) at different times after 5 Gy IR. The total acetylated mitochondrial protein levels were estimated by densitometry and normalized with COX IV as SIRT3/Ac-K ratio (lower panels).
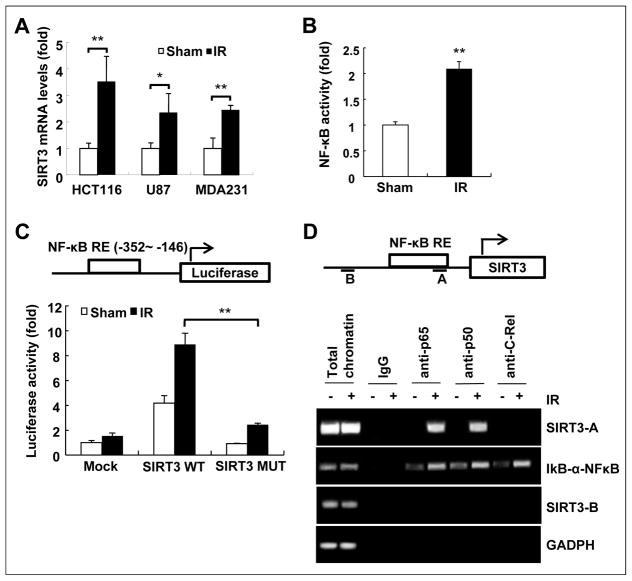
NF-κB controls SIRT3 transcription in irradiated tumor cells
Our data indicate that SIRT3 expression, although decreased in human cancers, can be induced via NF-κB-mediated SIRT3 promoter activation (Fig. 2). Similar to SIRT3 protein levels, SIRT3 mRNA levels were also increased after 5 Gy IR in three different cancer cell lines, HCT116, U87, and MDA231 (Fig. 2A). A database search identified a potential NF-κB binding motif in the human SIRT3 promoter region (−352 to −146), which was identified as a critical cis-acting element that plays a role in IR-induced SIRT3 transactivation (Fig. 2C). Importantly, NF-κB activity (Fig. 2B) and binding to SIRT3 promoter (Fig. 2C) were also induced by radiation. When the NF-κB response element on SIRT3 promoter was mutated, NF-κB binding was significantly reduced (Fig. 2C). Chromatin immunoprecipitation assay also showed an increase in p65 and p50 subunit binding to the SIRT3 promoter following IR (Fig. 2D). These results indicate that SIRT3 transcription is directly regulated by NF-κB upon radiation exposure.
Figure 2.
NF-κB is responsible for radiation induced SIRT3 expression. A, enhanced SIRT3 mRNA levels in irradiated HCT-116, U87 and MDA-MB231 cells measured by quantitative RT-PCR. B, NF-κB reporter activity measured 24 h after sham or 5 Gy IR. C, NF-κB responsive fragment (−352 to −146) containing NF-κB-RE consensus sequence (−184 to −171) was identified in the promoter region of human SIRT3 gene. Luciferase reporter plasmids with wild type (SIRT3 WT) or mutant (SIRT3 MUT; lacking the NF-κB fragment) SIRT3 promoter region or Mock (empty vector control) were transfected to HCT-116 cells and luciferase activity was measured 24 h after sham or 5 Gy IR. Data were normalized to β-gal activity (n = 3; *P < 0.05, **P < 0.01). D, ChIP assay of NF-κB in SIRT3 promoter region. Fragment A (−352 to −146): encompassing the NF-κB consensus sequence; Fragment B (−1311 to −1509): a non-relevant upstream sequence as the control. Protein-DNA complexes were extracted from IR (5 Gy)-treated HCT-116 cells and immunoprecipitated using anti-NF-κB (anti-p65, anti-p50) with precipitation of normal IgG as the negative control, and anti-C-Rel as the positive control; DNA fragments were amplified with primers specific for the SIRT3 promoter sequence of fragment A (SIRT3-A) or fragment B (SIRT3-B). Total chromatin was included as the input control for PCR. The IκB promoter region (IκB-α-NFκB) and GAPDH were included as positive and negative controls.
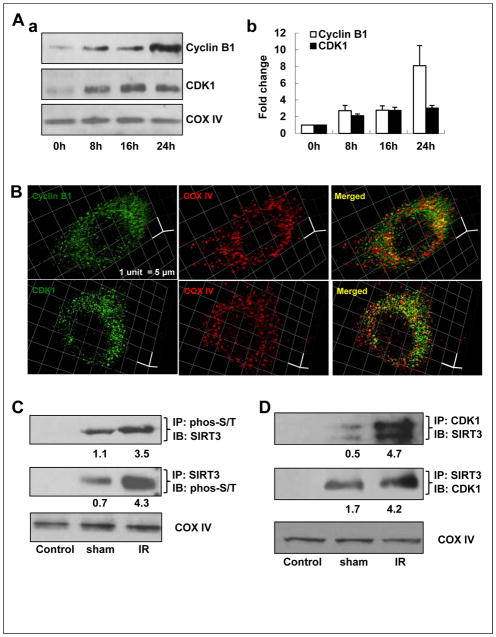
Mitochondrial Cyclin B1/CDK1 is linked with SIRT3 phosphorylation
Both Cyclin B1 and CDK1 protein levels were enhanced in the mitochondria after 5Gy IR, shown by western blotting of the mitochondrial fractions (Fig. 3A, a–b). Purity of the mitochondrial fractions are shown in Fig. S1C. The 3-D deconvolution fluorescence microscopy also revealed that a fraction of Cyclin B1 or CDK1 was co-localized with COX IV, a mitochondrial resident protein (Fig. 3B). Unlike COXIV, Cyclin B1 and CDK1 are not mitochondrial resident proteins, therefore their mitochondrial localization is a dynamic process following radiation. At any given point, there will be both mitochondrial and cytoplasmic/nuclear Cyclin B1/CDK1. Therefore, in Fig. 3B, there are some green only spots indicating non-mitochondrial localization of the complex. Similarly, the presence of red only spots suggests that not all mitochondria has Cyclin B1 and CDK1; assuming that the immunostaining was %100 efficient. Nevertheless, the mitochondrial localization of a portion of Cyclin B1 and CDK1 is evident. Next, we investigated whether SIRT3 can also be phosphorylated by the mitochondrial Cyclin B1/CDK1 upon radiation. Co-immunoprecipitation (Co-IP) assays showed that SIRT3 is Ser/Thr phosphorylated in the mitochondria, which is enhanced after irradiation (Fig. 3C). These findings indicate that the Ser/Thr phosphorylation of SIRT3 is responsive to radiation, which may be linked to IR-induced mitochondrial Cyclin B1/CDK1 complex. In addition, a mitochondrial Co-IP also showed a direct interaction between CDK1 and SIRT3 in irradiated HCT-116 cells (Fig. 3D).
Figure 3.
SIRT3 co-localizes with CyclinB1/CDK1 in the mitochondria. A, mitochondrial accumulation of Cyclin B1 and CDK1. a, Time-course analysis of mitochondrial Cyclin B1 and CDK1 in IR-treated HCT-116 cells detected by western blot. b, Cyclin B1 and CDK1 protein levels were quantified by measuring band intensity from three western blots using Image J software and normalized with COX IV. B, representative images of mitochondrial localization of cyclin B1 (green, upper panel) and CDK1 (green, lower panel), co-stained with mitochondria marker, COX IV (red), in HCT-116 cells by 3-D structured illumination super-resolution microscopy. Scale bar, 1 unit = 5 μm. C, mitochondrial proteins were immunoprecipated (IP) with anti-phosphoserine (phos-S/T) or anti-SIRT3 followed by immunoblotting (IB) with anti-SIRT3 or anti-phos-S/T, respectively. IP with normal IgG serves as negative control and COXIV serves as equal loading control. D, co-IP of mitochondrial CDK1 and SIRT3 using mitochondrial fractions isolated from 5 Gy-irradiated or sham-irradiated HCT-116 cells (n=3).
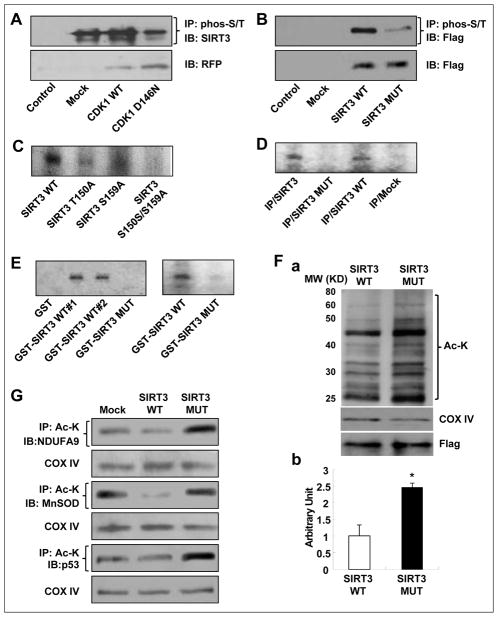
CDK1-mediated SIRT3 Thr150/Ser159 phosphorylation enhances SIRT3 activity
To determine whether CDK1 is responsible for SIRT3 phosphorylation, we utilized plasmid constructs containing an 87 base MTS (mitochondria targeting sequence) linked to GFP tagged wild type or dominant negative CDK1 (9). The phosphorylation of SIRT3 was significantly reduced in the mutant CDK1 expressing cells (Fig. 4A), indicating that mitochondrial CDK1 is required for IR-induced SIRT3 phosphorylation in mitochondria. To determine the specific CDK1-controlled phosphorylation of SIRT3, Netphos 2.0, Automotif server 2.0 was used (33) and two potential CDK1 consensus phosphorylation motifs (Thr150 and Ser159) were identified (S/T*-P; Fig. S2). To test whether these two residues are phosphorylated in vitro, we generated wild type flag-tagged SIRT3 and double mutant flag-tagged SIRT3 (pCDNA3.1/SIRT3/T150A/S159A mut) plasmids. Co-IP showed that the double mutation of SIRT3 protein clearly reduced Ser/Thr phosphorylation of this mitochondrial deacetylase compared to wild type SIRT3 (Fig. 4B), pointing at these two residues as potential phosphorylation target sites.
Figure 4.
SIRT3 is phosphorylated by mitochondrial CDK1 after radiation. A, CDK1-mediated SIRT3 phosphorylation was analyzed by IP with mitochondrial fractions isolated from HCT-116 cells harboring mitochondria-targeted wild type (pERFP-MTS-CDK1) or mutant (pERFP-MTS-CDK1-D146N, deficient phosphorylation activity) CDK1 with anti-phos-S/T followed by IB with anti-SIRT3 (Control, normal IgG; Mock, empty vector transfectants of HCT-116). IB of mitochondria fractions with anti-RFP antibody was used as equal IP loading control of exogenous wild type and mutant CDK1. B, phosphorylation of SIRT3 in mitochondria of irradiated HCT-116 cells harboring Flag tagged wild type or mutant SIRT3 were analyzed by IP using anti-phos-S/T followed by IB with anti-flag. IB of mitochondria fractions with anti-Flag antibody was used as equal IP loading control of exogenous wild type and mutant SIRT3. C, kinase assay using commercial Cyclin B1/CDK1 and total proteins isolated from HCT-116 cells harboring wild type, single mutant SIRT3/T150A or SIRT3/S159A and double mutant SIRT3/T150A/S159A. D, kinase assay using commercial Cyclin B1/CDK1 and total proteins isolated from HCT-116 cells harboring wild type or double mutant SIRT3 (IP/SIRT3 as input SIRT3; IP/Mock was the empty vector control). E, kinase assay using commercial (left) and immunoprecipitated mitochondrial (right) CDK1 with wild type (duplicate 1 and 2) or Thr150/Ser159 mutant SIRT3 proteins synthesized in E. coli (GST, negative control) (n=3). F, western blot of mitochondrial acetylated proteins of irradiated HCT-116 cells harboring wild-type or Thr150/Ser159 mutant SIRT3 (a). COX IV, mitochondrial protein equal loading control; Flag, equal loading control of mitochondria targeted expression of wild type and mutant SIRT3. The acetylated protein levels were estimated by densitometry and normalized with COX IV from three separated blots (b, *P < 0.05). G, SIRT3 targeted deacetylation of NDUFA9, MnSOD and p53 in irradiated HCT-116 cells harboring mock, wild type or Thr150/Ser159 mutant SIRT3 detected by IP with anti-Ac-K followed by IB with respective antibodies.
To further identify these residues of SIRT3 as CDK1 target sites, we performed an in vivo kinase assay using commercial Cyclin B1/CDK1 protein as the kinase source and wild type and mutant flag-tagged SIRT3 proteins immunoprecipitated from the transfected cells as the substrate. The results showed that a single mutation of either T150A or S159A greatly reduced the phosphorylation of SIRT3; while the T150A and S159A double mutation completely inhibited phosphorylation of SIRT3 (Fig. 4C). To show that endogenous SIRT3 can also be phosphorylated by CDK1, we performed another kinase assay including the endogenous SIRT3 as a substrate along with the exogenous wild type and mutant SIRT3 proteins. The endogenous SIRT3 (IP/SIRT3) immunoprecipitated from non-transfected cells gave a positive phosphorylation signal (Fig. 4D), as did the exogenous flag-tagged wild type SIRT3 (IP/SIRT3 WT). Similarly, we performed an in vitro kinase assay using GST-tagged wild type and mutant SIRT3 proteins synthesized in bacteria as the substrate commercial CDK1 (Fig. 4E, left panel), and the mitochondrial CDK1 immunoprecipitated from the HCT-116 cells (Fig. 4E, right panel) as the kinase. The two clones of recombinant wild type GST-SIRT3 were phosphorylated by commercial CDK1 while in contrast; the mutant GST-SIRT3 was not phosphorylated (Fig. 4E, left panel). Immunoprecipitated endogenous mitochondrial CDK1 can also phosphorylate the wild type SIRT3, but not the mutant GST-SIRT3 (Fig. 4E, right panel). Both SIRT3 T150 and S159 phosphorylated by CDK1 indicates that CDK1-SIRT3 pathway may play a role in the overall mitochondrial protein acetylation involved in mitochondrial homeostasis and apoptosis (34). CDK1-mediated SIRT3 Thr150/Ser159 phosphorylation appears to orchestrate mitochondrial metabolic homeostasis that may contribute to an adaptive radioresistance phenotype in tumor cells. On the other hand, since Cyclin B1/CDK1 is also induced by IR under NF-κB regulation (35), Cyclin B1/CDK1 and SIRT3 may serve as fundamental factors under the control of NF-κB to guide the mitochondrial homeostasis and Cyclin B1/CDK1 serves as the kinase responsible for SIRT3 phosphorylation and activation in the mitochondria.
To determine whether the deacetylase activity of SIRT3 can be regulated via phosphorylation at Thr150 and/or Ser159, we compared the acetylation of mitochondrial proteins in cells transfected with wild type or Thr150A/Ser159A mutated SIRT3. As expected, total acetylation was reduced in the wild type SIRT3 expressing cells, while an increased acetylation of overall mitochondrial proteins were observed in mutant SIRT3 expressing cells following radiation exposure (Fig. 4F, a–b). Similar results were also observed in U87 and MDA-MB231 cells (Fig. S3). The acetylation of three key SIRT3 mitochondrial substrates; NDUFA9 (a complex I subunit), MnSOD (mitochondrial antioxidant), and p53, were all increased in mutant SIRT3 transfected cells, as compared to wild-type SIRT3 expressing cells (Fig. 4G), indicating a critical role of SIRT3 deacetylase activity in regulating mitochondrial function and homeostasis.
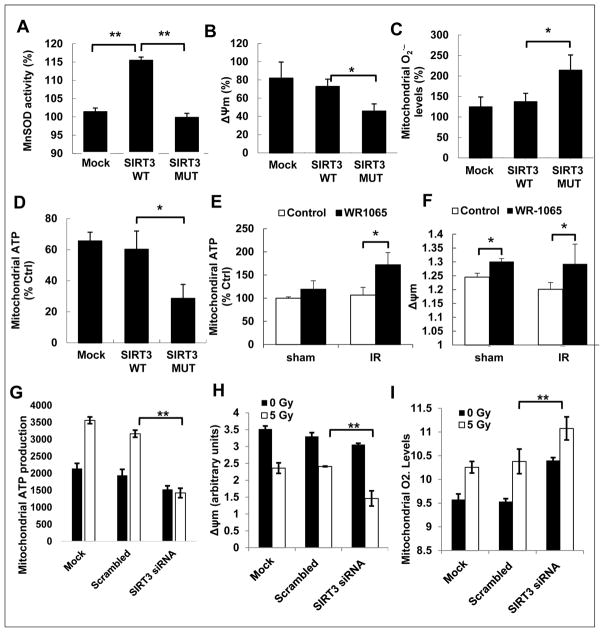
CDK1-mediated SIRT3 Thr150A/Ser159A phosphorylation enhances SIRT3 targets and mitochondrial bioenergetics
SIRT3 has been recently shown to protect cells from oxidative stress by activating key mitochondrial metabolic/detoxification proteins including MnSOD. To test the significance of CDK1-mediated SIRT3 T150/S159 phosphorylation for protecting mitochondrial function under radiation, we investigated the mitochondrial functions in cells transfected with wt or T150A/S159A mutant SIRT3. An increased MnSOD activity was detected after IR exposure in wild type SIRT3, but not mutant SIRT3 transfected cells (Fig. 5A). To address the clinical relevance of SIRT3 phosphorylation-mediated MnSOD activity, we tested the MnSOD activity in wt or mutant SIRT3-transfected mammary epithelial MCF10A cells. Like in MCF7 cells, MCF10A cells showed a similar MnSOD activation regulated by SIRT3 phosphorylation (Fig. S4). These results raise a concern in protecting normal tissues when tumor cells are radio-sensitized by inhibition of the SIRT3-MnSOD pathway. Therefore, specific targets of SIRT3 phosphorylation mediated MnSOD in tumor cells need to be further investigated. Additional evidence of CDK1-SIRT3 mediated mitochondrial homeostasis include the decreased ΔΨm, (Fig. 5B), enhanced mitochondrial superoxide level (Fig. 5C) with lowered ATP production (Fig. 5D) in cells expressing mutant SIRT3 with the deficient CDK1-mediated phosphorylation. The lowered ΔΨm and ATP production were rescued by SOD mimics, WR1165, pre-treatment 24 h before IR in mutant SIRT3 bearing cells (Fig. 5E–F), suggesting that the reduced mitochondrial functions are due to the inability of mutant SIRT3 to induce MnSOD activity. In addition, we also utilized SIRT3 siRNA to knocn down the expression of SIRT3 and followed the mitochondrial functions. Similar to MUT SIRT3 expressing cells, SIRT3 knock out cells showed lowered ΔΨm and ATP production, as well as enhanced superoxide levels (Fig. 5G–I).
Figure 5.
Expression of Thr150/Ser159 mutant SIRT3 decreases MnSOD activity and mitochondrial functions. HCT116 cells harboring mock, wild type SIRT3 or Thr150/Ser159 mutant SIRT3 were treated with sham or 5 Gy IR. MnSOD activity (A), ΔΨm (B), mitochondrial superoxide levels (C) and mitochondrial ATP production (D) were measured 24 h after radiation. HCT116 cells harboring Thr150/Ser159 mutant SIRT3 were treated with MnSOD mimic drug, WR1065 (40 μM, 24 h), followed by sham or 5 Gy IR. Mitochondrial ATP production (E) and mitochondrial membrane potential (F) were measured 24 h after radiation. ATP production (G), mitochondrial membrane potential (H), and mitochondrial superoxide levels (I) were measured 24 h post IR in HCT116 cells transfected with scrambled control or SIRT3 siRNA for 48 h. (n = 5, *, P < 0.05, **, P < 0.01).
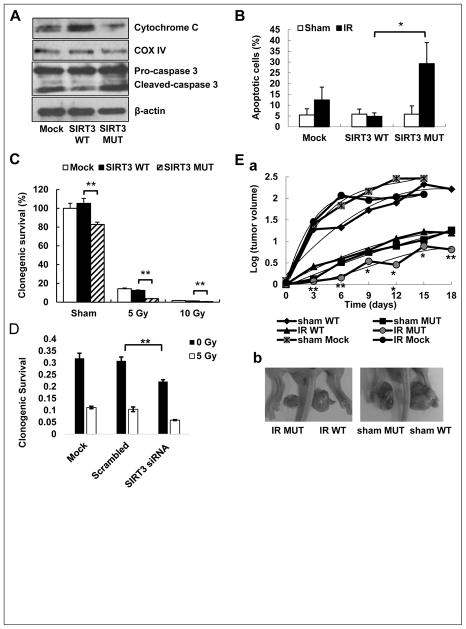
CDK1-mediated SIRT3 phosphorylation in tumor radioresistance
To gain further insight into the effects of SIRT3 phosphorylation on HCT-116 cell survival and proliferation, we performed apoptosis and colony-formation assays with cells transfected with wild type and the Thr150A and/or Ser159A mutant SIRT3 genes after IR exposure. Cells expressing the SIRT3 T150A/S159A mutant promoted apoptosis, as measured by a significant release of cytochrome c from the mitochondria after radiation (Fig. 6A). In addition, cleavage of caspase-3, a key enzyme initiating the execution stage of apoptotic pathway, was increased in the mutant SIRT3 transfectants (Fig. 6A). Comparison of apoptotic cells within the wt or mutant SIRT3 transfectants revealed a greater percentage of apoptosis in mutant SIRT3 bearing cells (Fig. 6B). Likewise, mutant SIRT3 T150A/S159A transfectants exhibited lower clonogenic survival (decreased 19.8%) in basal clonogenicity and an additional 73.5% reduction after 5 Gy IR, as compared to wild type SIRT3 transfected cells (Fig. 6C, a–b, Fig. S5A–B). Similarly, knocking down SIRT3 via siRNA transfection, resulted in reduced clonogenic survival of cells, which is further decreased by 5 Gy irradiation (Fig. 6D). In mutant SIRT3-bearing cells, CDK1-mediated SIRT3 activation will not be achieved, therefore, downstream targets of SIRT3 including MnSOD will not be activated by deacetylation. Lack of MnSOD activation will then lead to the accumulation of ROS and oxidative damage resulting in cell death and enhanced radiosensitivity. MnSOD overexpression in SIRT3 mutant cells did not rescue the clonogenic cell death, because SIRT3 mutant-expressing cells were unable to induce MnSOD activity even though MnSOD is overexpressed (Fig. S5C–D). However, pre-treatment with MnSOD mimics prior to irradiation did rescue the clonogenic survival, suggesting that SIRT3-dependent cell survival is mediated via MnSOD activation. These results indicate that CDK1-mediated SIRT3 phosphorylation results in a tumor cell resistant phenotype or promotes survival after exposure to therapeutic IR.
Figure 6.
Expression of Thr150/Ser159 mutant SIRT3 inhibits clonogenic survival and increases tumor radiosensitivity. A, western blot of cytochrome c and caspase 3 cleavage in HCT-116 cells harboring wild type or Thr150/Ser159 mutant SIRT3 24 h after 5 Gy IR. B, apoptosis assay in HCT-116 cells harboring wild type or Thr150/Ser159 mutant SIRT3 upon sham or 5 Gy IR (n = 3, *, P < 0.05). C, Clonogenic survival rates were measured in above HCT-116 stable transfectants after irradiation with 5 and 10 Gy. Survival fractions normalized to mock sham controls were shown (n = 5, *, P < 0.05, **, P < 0.01). D, Clonogenic survival of HCT116 cells that are transfected with scrambled control or SIRT3 siRNA for 48 h, with or without radiation (n=3, *p<0.01). E, HCT-116 cells stably transfected with mock, wild type or mutant SIRT3 were inoculated in mice and when tumor reached ~ 0.3 cm3, 5 Gy IR was delivered locally to tumors with surrounding tissue shielded. a, tumor volumes were measured post-irradiation every 3 days (mean ± SD; n = 6). b, Representative photographs of surgically removed tumors at the end of experiments were shown (see also Fig. S6).
Finally, we analyzed the role of radiation-induced mitochondrial CDK1-mediated SIRT3 phosphorylation in vivo. To generate a mouse xenograft tumor model, mock/HCT-116, SIRT3 WT/HCT-116 and SIRT3 MUT/HCT-116 cells (5 million cells each) were subcutaneously implanted into each side of nude mice flanks. On the seventh day after tumor cell implantation, the mice were divided into two groups, sham or 5 Gy irradiation. Compared to wild type SIRT3, mutant SIRT3 xenograft tumors showed a significant delayed tumor growth rate of 4.5 days for sham and 6 days for irradiated tumors (Fig. 6E, a–b, Fig. S6). Radiation-induced TGD was calculated as 3 days for WT SIRT3 and 4.5 days for MUT SIRT3 tumors. These results, as well as those in vitro, strongly suggest that SIRT3 T150/S159 phosphorylation through mitochondrial CDK1 can be induced by radiation which cooperatively promotes the cellular adaptive response under genotoxic stress and tumor radioresistance.
Discussion
SIRT3 is a major factor controlling the mitochondrial homeostasis and bioenergetics against cell aging (22, 36, 37). Our current data indicate that under genotoxic stress including the therapeutic ionizing radiation, SIRT3 can be induced in tumor cells via NF-κB-mediated SIRT3 promoter activation. SIRT3 transcripts and protein levels were induced in irradiated human cancer cells, and in vivo irradiated tumors. Importantly, SIRT3 expression was timely conjugated with decreased overall mitochondrial protein deacetylation, indicating that induction of SIRT3 is a predominant feature of tumor cells after irradiation. The highly selective binding of p65/p50 heterodimer to the SIRT3 promoter suggests that IR-induced SIRT3 transcription is regulated by a classical IKK-dependent NF-κB activation and SIRT3 is a NF-κB target gene in tumor cells. HCT-116 cells expressing a deacetylation-null mutant SIRT3 gene (SIRT3dn) show sensitivity to ROS stress (38), and inhibition of SIRT3 reduces oral cancer cell proliferation and increases sensitivity to IR (30). Our current data reveal that SIRT3 gene expression together with CDK1-mediated T150/S159 phosphorylation contributes to the enhanced mitochondrial homeostasis and tumor resistance to therapeutic radiation.
NF-kB and SIRT3 regulation
Recently, luciferase-based reporter to monitor the transcriptional activity of the SIRT3 promoter is established and indicates that SIRT3 promoter is sensitive to oxidative stress (39). We show here that SIRT3 gene transcription can be activated in tumor cells under genotoxic stress conditions such as therapeutic ionizing radiation via NF-κB controlled SIRT3 promoter activation. A unique NF-κB-RE consensus sequence (−184 to −171) is linked to the NF-κB-controlled SIRT transcription. NF-κB is a well-defined stress-sensitive transcription factor promoting survival (40–43). Not surprisingly, NF-κB activity is emphasized in many different cancers (44) and more importantly, it is involved in therapy-resistance, recurrence and poor survival of cancer patients (45, 46). Our recent work showed the importance of radiation-induced NF-κB in the regulation of therapy-resistance in breast cancer via controlling the expression of a survival factor, MKP1, which is also localized to mitochondria upon radiation (47). Therefore, a cluster of pro-survival mitochondrial proteins including SIRT3 and MKP1 controlled by NF-κB may enhance mitochondrial homeostasis for cancer cell survival and resistance to anti-cancer therapy. Therefore, further elucidation of the NF-κB controlled mitochondrial activity especially the factors controlling the mitochondrial bioenergetics in irradiated tumor cells will help to define novel drug targets to block tumor adaptive response and significantly enhance the local control of the aggressive metastatic lesions by radiotherapy.
SIRT3-MnSOD
There is a cluster of mitochondrial proteins that are regulated via SIRT3 deacetylation (27, 28). As much as 20% of mitochondrial proteins are lysine acetylated, among which a substantial amount is deacetylated by SIRT3. In this regard, it was found that radiation-induced SIRT3 activation and deacetylation of mitochondrial proteins was alleviated at least in the known SIRT3 targets NDUFA9, MnSOD and p53 by introducing the phosphorylation mutant SIRT3, causing decreased ATP generation and membrane potential and increased apoptotic and clonogenic death in radiation. This suggests that SIRT3-deacetylated targets contribute to mitochondrial metabolic homeostasis and cellular adaptive resistance to radiation. Recently, MnSOD was found to be deacetylated by SIRT3 responding to changes in mitochondrial nutrient and/or redox status, and its lysine acetylation significantly altered MnSOD enzymatic activity (48). The deacetylated MnSOD prevented IR-induced foci formation and immortalization of MEFs by a single oncogene, as well as IR-induced genomic instability and loss of contact inhibition, suggesting that mitochondrial acetylation plays a role, at least in part, in regulation of MnSOD function (27). Apart from normal cells, most cancer cells have diminished MnSOD activity (49). Deficiencies in MnSOD may contribute to oxidative stress that promotes neoplastic transformation and/or maintenance of the malignant phenotype. Overexpression of MnSOD reduces tumor multiplicity, incidence, and metastatic ability in various in vitro and in vivo models (50). Accumulating evidence show that MnSOD is implicated in the resistance of tumor cells to some therapies, such as chemo- and radio-therapy through scavenging cellular ROS produced by mitochondria oxidative phosphorylation (51, 52). In mice lacking SIRT3, the ability of MnSOD to reduce cellular ROS and promote oxidative stress resistance is greatly enhanced by SIRT3 (53), indicating that SIRT3-MnSOD pathway is a pro-survival network in cancer cells. Given that NF-kB induces the expression of SIRT3 and MnSOD upon radiation, and that SIRT3 can activate MnSOD via deacetylation, there seems to be a positive additive circle of events that would have alarming consequences, especially in pathological conditions such as cancer. Cells overexpressing SIRT3 and MnSOD could have an overactive pro-survival network, which would eventually lead to resistance to radiation therapy.
CDK1-SIRT3
SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation (20). Expressing CDK1-phosphorylation deficient SIRT3 exhibited less MnSOD deacetylation with reduced MnSOD activity and enhanced mitochondrial superoxide accumulation. Cyclin B1/CDK1 and MnSOD are also regulated by NF-κB in irradiated cells and MnSOD enzymatic activity can be increased by CDK1-mediated phosphorylation (32), indicating that MnSOD enzymatic activity as well as other metabolic enzymes in mitochondria can be regulated via both deacetylation and phosphorylation, by SIRT3 and CDK1, respectively. With this regard, a simultaneous regulation of protein deacetylation and phosphorylation seems to be necessary for increasing and/or maintaining the mitochondrial homeostasis. The orchestrated NF-κB/CDK1/SIRT3-pro-survival network is potentially responsible for cellular adaptive response to therapeutic radiation.
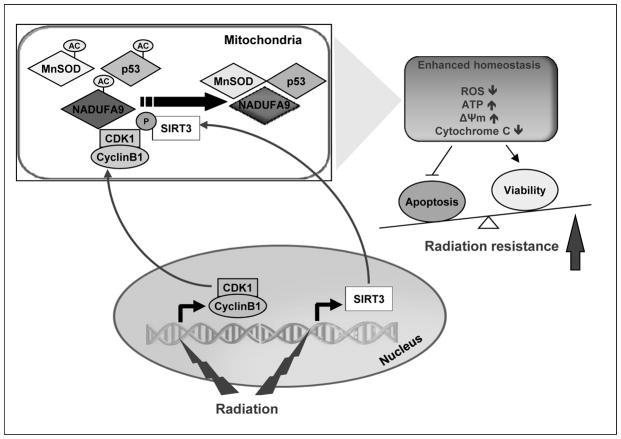
In summary, we demonstrate that SIRT3 deacetylation activity is induced in tumor cells at both the transcriptional and post-translational levels after therapeutic irradiation. IR induces SIRT3 transcription via NF-κB binding to and activation of the SIRT3 promoter. IR-induced Cyclin B1/CDK1 enhances the SIRT3 deacetylation activity via Thr150/Ser159 phosphorylation as measured by decrease mitochondrial protein acetylation and ATP generation, and enhance radiosensitivity (Fig. 7). These results support a mechanism by which tumor cells generate adaptive resistance by enhancing SIRT3-mediated mitochondrial homeostasis via both gene transcription and post-translational modifications in mitochondria.
Figure 7.
A mitochondrial homeostasis model in tumor radioresistance. Findings from this study demonstrate a unique mechanism by which SIRT3 is upregulated in tumor cells by radiation via NF-κB-mediated SIRT3 promoter activation. SIRT3 enzymatic activity is further enhanced in mitochondria via Cyclin B1/CDK1-mediated SIRT3 Thr150/Ser159 phosphorylation. Expression of the mutant Thr150/Ser159 SIRT3 decreases the level of mitochondrial protein deacetylation, MnSOD activity and ATP generation whereas increases cell radiosensitivity.
Supplementary Material
Acknowledgments
Financial Support: This work was supported by NIH NCI Grants CA133402 and RO1 CA152313, and the US Department of Energy Office of Science Grant DE-SC0001271 (J.J. Li); NCI-1R01CA168292-01A1 and NCI-1R01CA16383801A1 (D.R. Gius).
Footnotes
The authors declare no financial conflicts.
References
- 1.Recht A, Come SE, Henderson IC, Gelman RS, Silver B, Hayes DF, et al. The sequencing of chemotherapy and radiation therapy after conservative surgery for early-stage breast cancer. N Engl J Med. 1996;334:1356–61. doi: 10.1056/NEJM199605233342102. [DOI] [PubMed] [Google Scholar]
- 2.Auperin A, Le Pechoux C, Rolland E, Curran WJ, Furuse K, Fournel P, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:2181–90. doi: 10.1200/JCO.2009.26.2543. [DOI] [PubMed] [Google Scholar]
- 3.Peters LJ, O’Sullivan B, Giralt J, Fitzgerald TJ, Trotti A, Bernier J, et al. Critical impact of radiotherapy protocol compliance and quality in the treatment of advanced head and neck cancer: results from TROG 02.02. J Clin Oncol. 2010;28:2996–3001. doi: 10.1200/JCO.2009.27.4498. [DOI] [PubMed] [Google Scholar]
- 4.Liang K, Lu Y, Jin W, Ang KK, Milas L, Fan Z. Sensitization of breast cancer cells to radiation by trastuzumab. Mol Cancer Ther. 2003;2:1113–20. [PubMed] [Google Scholar]
- 5.Debeb BG, Xu W, Woodward WA. Radiation resistance of breast cancer stem cells: understanding the clinical framework. J Mammary Gland Biol Neoplasia. 2009;14:11–7. doi: 10.1007/s10911-009-9114-z. [DOI] [PubMed] [Google Scholar]
- 6.Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21–8. doi: 10.1016/S1470-2045(09)70311-0. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed KM, Dong S, Fan M, Li JJ. Nuclear factor-kappaB p65 inhibits mitogen-activated protein kinase signaling pathway in radioresistant breast cancer cells. Mol Cancer Res. 2006;4:945–55. doi: 10.1158/1541-7786.MCR-06-0291. [DOI] [PubMed] [Google Scholar]
- 8.Guo G, Yan-Sanders Y, Lyn-Cook BD, Wang T, Tamae D, Ogi J, et al. Manganese superoxide dismutase-mediated gene expression in radiation-induced adaptive responses. Mol Cell Biol. 2003;23:2362–78. doi: 10.1128/MCB.23.7.2362-2378.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta S, Koru-Sengul T, Arnold SM, Devi GR, Mohiuddin M, Ahmed MM. Low-dose fractionated radiation potentiates the effects of cisplatin independent of the hyper-radiation sensitivity in human lung cancer cells. Mol Cancer Ther. 2011;10:292–302. doi: 10.1158/1535-7163.MCT-10-0630. [DOI] [PubMed] [Google Scholar]
- 10.Hadian K, Krappmann D. Signals from the nucleus: activation of NF-kappaB by cytosolic ATM in the DNA damage response. Sci Signal. 2011;4:pe2. doi: 10.1126/scisignal.2001712. [DOI] [PubMed] [Google Scholar]
- 11.Cao N, Li S, Wang Z, Ahmed KM, Degnan ME, Fan M, et al. NF-kappaB-mediated HER2 overexpression in radiation-adaptive resistance. Radiat Res. 2009;171:9–21. doi: 10.1667/RR1472.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z, Cao N, Nantajit D, Fan M, Liu Y, Li JJ. Mitogen-activated protein kinase phosphatase-1 represses c-Jun NH2-terminal kinase-mediated apoptosis via NF-kappaB regulation. J Biol Chem. 2008;283:21011–23. doi: 10.1074/jbc.M802229200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang JY, Hirschey MD, Shimazu T, Ho L, Verdin E. Mitochondrial sirtuins. Biochim Biophys Acta. 2010;1804:1645–51. doi: 10.1016/j.bbapap.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 14.He W, Newman JC, Wang MZ, Ho L, Verdin E. Mitochondrial sirtuins: regulators of protein acylation and metabolism. Trends Endocrinol Metab. 2012;23:467–76. doi: 10.1016/j.tem.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Houtkooper RH, Pirinen E, Auwerx J. Sirtuins as regulators of metabolism and healthspan. Nat Rev Mol Cell Biol. 2012;13:225–38. doi: 10.1038/nrm3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hallows WC, Albaugh BN, Denu JM. Where in the cell is SIRT3?--functional localization of an NAD+-dependent protein deacetylase. Biochem J. 2008;411:e11–3. doi: 10.1042/BJ20080336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schlicker C, Gertz M, Papatheodorou P, Kachholz B, Becker CF, Steegborn C. Substrates and regulation mechanisms for the human mitochondrial sirtuins Sirt3 and Sirt5. J Mol Biol. 2008;382:790–801. doi: 10.1016/j.jmb.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 18.Shimazu T, Hirschey MD, Huang JY, Ho LT, Verdin E. Acetate metabolism and aging: An emerging connection. Mech Ageing Dev. 2010;131:511–6. doi: 10.1016/j.mad.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Hallows WC, Yu W, Smith BC, Devries MK, Ellinger JJ, Someya S, et al. Sirt3 promotes the urea cycle and fatty acid oxidation during dietary restriction. Mol Cell. 2011;41:139–49. doi: 10.1016/j.molcel.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hirschey MD, Shimazu T, Goetzman E, Jing E, Schwer B, Lombard DB, et al. SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation. Nature. 2010;464:121–5. doi: 10.1038/nature08778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu W, Dittenhafer-Reed KE, Denu JM. SIRT3 protein deacetylates isocitrate dehydrogenase 2 (IDH2) and regulates mitochondrial redox status. J Biol Chem. 2012;287:14078–86. doi: 10.1074/jbc.M112.355206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verdin E, Hirschey MD, Finley LW, Haigis MC. Sirtuin regulation of mitochondria: energy production, apoptosis, and signaling. Trends Biochem Sci. 2010;35:669–75. doi: 10.1016/j.tibs.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finkel T, Deng CX, Mostoslavsky R. Recent progress in the biology and physiology of sirtuins. Nature. 2009;460:587–91. doi: 10.1038/nature08197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scher MB, Vaquero A, Reinberg D. SirT3 is a nuclear NAD+-dependent histone deacetylase that translocates to the mitochondria upon cellular stress. Genes Dev. 2007;21:920–8. doi: 10.1101/gad.1527307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahn BH, Kim HS, Song S, Lee IH, Liu J, Vassilopoulos A, et al. A role for the mitochondrial deacetylase Sirt3 in regulating energy homeostasis. Proc Natl Acad Sci U S A. 2008;105:14447–52. doi: 10.1073/pnas.0803790105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fernandez-Marcos PJ, Jeninga EH, Canto C, Harach T, de Boer VC, Andreux P, et al. Muscle or liver-specific Sirt3 deficiency induces hyperacetylation of mitochondrial proteins without affecting global metabolic homeostasis. Sci Rep. 2012;2:425. doi: 10.1038/srep00425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tao R, Coleman MC, Pennington JD, Ozden O, Park SH, Jiang H, et al. Sirt3-mediated deacetylation of evolutionarily conserved lysine 122 regulates MnSOD activity in response to stress. Mol Cell. 2010;40:893–904. doi: 10.1016/j.molcel.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vassilopoulos A, Pennington DJ, Andresson T, Rees D, Fearnley I, Ham A, et al. SIRT3 Deacetylates ATP Synthase F1 Complex Proteins in Response to Nutrient and Exercise-Induced Stress. Antioxid Redox Signal. 2013 doi: 10.1089/ars.2013.5420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheng Y, Ren X, Gowda AS, Shan Y, Zhang L, Yuan YS, et al. Interaction of Sirt3 with OGG1 contributes to repair of mitochondrial DNA and protects from apoptotic cell death under oxidative stress. Cell Death Dis. 2013;4:e731. doi: 10.1038/cddis.2013.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alhazzazi TY, Kamarajan P, Joo N, Huang JY, Verdin E, D’Silva NJ, et al. Sirtuin-3 (SIRT3), a novel potential therapeutic target for oral cancer. Cancer. 2011;117:1670–8. doi: 10.1002/cncr.25676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Z, Fan M, Candas D, Zhang TQ, Qin L, Eldridge A, et al. Cyclin B1/Cdk1 coordinates mitochondrial respiration for cell-cycle G2/M progression. Dev Cell. 2014;29:217–32. doi: 10.1016/j.devcel.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Candas D, Fan M, Nantajit D, Vaughan AT, Murley JS, Woloschak GE, et al. CyclinB1/Cdk1 phosphorylates mitochondrial antioxidant MnSOD in cell adaptive response to radiation stress. J Mol Cell Biol. 2013;5:166–75. doi: 10.1093/jmcb/mjs062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takeda DY, Wohlschlegel JA, Dutta A. A bipartite substrate recognition motif for cyclin-dependent kinases. J Biol Chem. 2001;276:1993–7. doi: 10.1074/jbc.M005719200. [DOI] [PubMed] [Google Scholar]
- 34.Averbeck NB, Durante M. Protein acetylation within the cellular response to radiation. J Cell Physiol. 2011;226:962–7. doi: 10.1002/jcp.22466. [DOI] [PubMed] [Google Scholar]
- 35.Ahmed KM, Li JJ. NF-kappa B-mediated adaptive resistance to ionizing radiation. Free Radic Biol Med. 2008;44:1–13. doi: 10.1016/j.freeradbiomed.2007.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bell EL, Guarente L. The SirT3 divining rod points to oxidative stress. Mol Cell. 2011;42:561–8. doi: 10.1016/j.molcel.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown K, Xie S, Qiu X, Mohrin M, Shin J, Liu Y, et al. SIRT3 reverses aging-associated degeneration. Cell Rep. 2013;3:319–27. doi: 10.1016/j.celrep.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacobs KM, Pennington JD, Bisht KS, Aykin-Burns N, Kim HS, Mishra M, et al. SIRT3 interacts with the daf-16 homolog FOXO3a in the mitochondria, as well as increases FOXO3a dependent gene expression. Int J Biol Sci. 2008;4:291–9. doi: 10.7150/ijbs.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Satterstrom FK, Haigis MC. Luciferase-based reporter to monitor the transcriptional activity of the SIRT3 promoter. Methods Enzymol. 2014;543:141–63. doi: 10.1016/B978-0-12-801329-8.00007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bradbury CM, Markovina S, Wei SJ, Rene LM, Zoberi I, Horikoshi N, et al. Indomethacin-induced radiosensitization and inhibition of ionizing radiation-induced NF-kappaB activation in HeLa cells occur via a mechanism involving p38 MAP kinase. Cancer Res. 2001;61:7689–96. [PubMed] [Google Scholar]
- 41.Delhalle S, Blasius R, Dicato M, Diederich M. A beginner’s guide to NF-kappaB signaling pathways. Ann N Y Acad Sci. 2004;1030:1–13. doi: 10.1196/annals.1329.002. [DOI] [PubMed] [Google Scholar]
- 42.Jung M, Dritschilo A. NF-kappa B signaling pathway as a target for human tumor radiosensitization. Semin Radiat Oncol. 2001;11:346–51. doi: 10.1053/srao.2001.26034. [DOI] [PubMed] [Google Scholar]
- 43.Weichselbaum RR, Hallahan D, Fuks Z, Kufe D. Radiation induction of immediate early genes: effectors of the radiation-stress response. Int J Radiat Oncol Biol Phys. 1994;30:229–34. doi: 10.1016/0360-3016(94)90539-8. [DOI] [PubMed] [Google Scholar]
- 44.Bours V, Bentires-Alj M, Hellin AC, Viatour P, Robe P, Delhalle S, et al. Nuclear factor-kappa B, cancer, and apoptosis. Biochem Pharmacol. 2000;60:1085–9. doi: 10.1016/s0006-2952(00)00391-9. [DOI] [PubMed] [Google Scholar]
- 45.Biswas DK, Shi Q, Baily S, Strickland I, Ghosh S, Pardee AB, et al. NF-kappa B activation in human breast cancer specimens and its role in cell proliferation and apoptosis. Proc Natl Acad Sci U S A. 2004;101:10137–42. doi: 10.1073/pnas.0403621101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Helbig G, Christopherson KW, 2nd, Bhat-Nakshatri P, Kumar S, Kishimoto H, Miller KD, et al. NF-kappaB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J Biol Chem. 2003;278:21631–8. doi: 10.1074/jbc.M300609200. [DOI] [PubMed] [Google Scholar]
- 47.Candas D, Lu CL, Fan M, Chuang FY, Sweeney C, Borowsky AD, et al. Mitochondrial MKP1 is a target for therapy-resistant HER2-positive breast cancer cells. Cancer Res. 2014;74:7498–509. doi: 10.1158/0008-5472.CAN-14-0844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen Y, Zhang J, Lin Y, Lei Q, Guan KL, Zhao S, et al. Tumour suppressor SIRT3 deacetylates and activates manganese superoxide dismutase to scavenge ROS. EMBO Rep. 2011;12:534–41. doi: 10.1038/embor.2011.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oberley LW, Buettner GR. Role of superoxide dismutase in cancer: a review. Cancer Res. 1979;39:1141–9. [PubMed] [Google Scholar]
- 50.Liu J, Gu X, Robbins D, Li G, Shi R, McCord JM, et al. Protandim, a fundamentally new antioxidant approach in chemoprevention using mouse two-stage skin carcinogenesis as a model. PLoS One. 2009;4:e5284. doi: 10.1371/journal.pone.0005284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Indo HP, Inanami O, Koumura T, Suenaga S, Yen HC, Kakinuma S, et al. Roles of mitochondria-generated reactive oxygen species on X-ray-induced apoptosis in a human hepatocellular carcinoma cell line, HLE. Free Radic Res. 2012;46:1029–43. doi: 10.3109/10715762.2012.698012. [DOI] [PubMed] [Google Scholar]
- 52.Zhou J, Du Y. Acquisition of resistance of pancreatic cancer cells to 2-methoxyestradiol is associated with the upregulation of manganese superoxide dismutase. Mol Cancer Res. 2012;10:768–77. doi: 10.1158/1541-7786.MCR-11-0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qiu X, Brown K, Hirschey MD, Verdin E, Chen D. Calorie restriction reduces oxidative stress by SIRT3-mediated SOD2 activation. Cell Metab. 2010;12:662–7. doi: 10.1016/j.cmet.2010.11.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.