Abstract
Background
Little is known about the impact of dialysis facility treatment philosophy on access to transplant. The aim of our study was to determine the relationship between dialysis facility transplant philosophy and facility-level access to kidney transplant waitlisting.
Methods
A 25-item questionnaire administered to Southeastern dialysis facilities (n=509) in 2012 captured facility transplant philosophy (categorized as “transplant is our first choice,” “transplant is a great option for some,” and “transplant is a good option, if the patient is interested”) .. Facility-level waitlisting and facility characteristics were obtained from the 2008-2011 Dialysis Facility Report. Multivariable logistic regression was used to examinethe association between dialysis facility transplant philosophy and facility waitlisting performance (dichotomized using the national median), where low performance was defined as less than 21.7% of dialysis patients waitlisted within a facility.
Results
Fewer than 25% (n=124) of dialysis facilities reported “transplant is our first option.” A total of 131 (31.4%) dialysis facilities in the Southeast were high-performing with respect to waitlisting. Adjusted analysis showed that facilities who reported “transplant is our first option” were twice (OR=2.0, 95% CI 1.0, 3.9) as likely to have high waitlisting performance compared to facilities who reported “transplant is a good option, if the patient is interested.”
Conclusions
Facilities with staff who had a more positive transplant philosophy were more likely to have better facility waitlisting performance. Future prospective studies are needed to further transplantation.
Keywords: dialysis, chronic kidney failure, kidney transplantation, patient education
INTRODUCTION
The Southeastern United States has a high prevalence of end-stage renal disease (ESRD), with the Southeastern Kidney Council (ESRD Network 6) serving >40,000 ESRD patients in the states of North Carolina (NC), South Carolina (SC), and Georgia (GA) in 2014 [1]. Kidney transplantation is associated with improved ESRD patient quality of life, decrease mortality, , reduce hospitalization [2], and costs [3], compared to dialysis. Despite the benefits of kidney transplantation and the Southeast’s high burden of kidney disease, this region has the lowest kidney transplantation rate in the country [4].
Little is known about how dialysis facility transplant philosophy impacts facility performance in kidney transplantation access. Previous literature suggests that treatment philosophies of health care staff are associated with patient outcomes [5-9]. For example, studies report that health professionals’ attitudes about kidney transplant impact patient and family decisions regarding transplantation [10]. However, it is unknown how dialysis facility transplant philosophy affects access to kidney transplantation among patients treated at the facility. In addition, while educational materials have been successful in improving dialysis facility staff attitudes and perceptions and knowledge about transplantation [5], no studies to our knowledge have explored the roles of educational materials and staff perceptions on transplantation, including how these factors may influence access to transplant among ESRD patients treated in dialysis facilities.
The Southeastern Kidney Transplant Coalition of ESRD Network 6 is an academic and community partnership that formed in 2011 with a mission of increasing kidney transplantation rates for the Southeastern region of the US and reducing disparities in kidney transplantation access [11, 12]. In 2012, the Southeastern Kidney Transplant Coalition conducted a survey of dialysis facilities in ESRD Network 6 to examine dialysis facility practices, protocols, available educational resources, and transplant philosophy. The primary aim of this study was to determine the relationship between dialysis facility transplant philosophy and facility-level waitlisting. Secondly, we explored whether the association between transplant philosophy and waitlisting varied by facility staff perceptions about transplantation and available transplant educational resources.
MATERIALS AND METHODS
Study Design and Data Sources
This study was a cross-sectional survey of dialysis facility staff employed in dialysis facilities in GA, NC, and SC in July to September 2012. The Southeastern Kidney Transplant Coalition [11, 12] developed a 25-item dialysis facility survey as part of a needs assessment within the Reducing Disparities in Access to kidNey Transplantation (RaDIANT) Community Study (R24MD008077; www.clinicaltrials.gov: NCT02092727) [12]. The link to the online survey was e-mailed to all facility medical directors in NC, SC, and GA (n=586) by ESRD Network 6 staff. A cover letter instructed the medical directors to have the staff member who was primarily responsible for kidney transplant education complete the survey. Almost all of the 586 dialysis facilities in NC, SC, and GA responded to the questionnaire (n=547, 93.3%) with the majority of respondents being nurse managers (51.0%) and social workers (21.8%) [13]. Approximately 93% (n=510) of the completed surveys were successfully matched to dialysis facility demographics in the 2008-2011 Dialysis Facility Report (DFR) data via facility provider number. The DFR is published annually by the University of Michigan Kidney Epidemiology and Cost Center (Ann Arbor, MI) and includes aggregate facility-level data such as patient demographics, clinical characteristics, and outcomes including waitlisting, transplantation, and mortality. There were no statistically significant differences in survey answers and type of responder between the study population and the 38 dialysis facilities excluded because they did not match facilities in the DFR. The study was approved by the Institutional Review Boards of Emory University and the University of South Carolina.
Study Variables
Dialysis facility transplant philosophy
The primary exposure variable for the study was dialysis facility transplant philosophy. Transplant philosophy was assessed by a single multiple-choice item: “If you could characterize the transplant philosophy of your facility, considering patient care staff and nephrologists’ opinions, which of the following best describes your facility.” The available responses were: a) “Transplant is our first choice for treatment. Nearly every patient should be considered for a transplant”; b) “Transplant is a great option for some people and they should be referred to a transplant center for evaluation”; c) “If a patient is interested in transplant, we should help them get evaluated, but we don’t push that for patients who are not interested”; and d) “Transplant has a lot of financial and other barriers/burdens; We think patients are better off on dialysis.” Answer choice (a) was classified as “Transplant is our first choice,” answer (b) was classified as “Transplant is a great option for some,” and (c) was classified as “Transplant is a good option, if the patient is interested.” One dialysis facility that selected (d) as their transplant philosophy was excluded.
Dialysis facility waitlisting performance
The outcome variable for this analysis was an indicator variable representing whether facilities met the 2008-2011 national median proportion of prevalent ESRD patients age 18-69 waitlisted within a dialysis facility (“high performing”). The Kolmogorov-Smirnov [14] normality test showed that waitlisting performance was not normally distributed (p<0.01) across U.S. facilities and the national median (21.7%) was used as a cut-point. The percentage of patients waitlisted at each facility was obtained through the DFR and dichotomized based on the national median.
Staff perceptions and available educational resources
We explored whether staff perceptions and the availability of transplant educational resources within a facility would affect the association between facility transplant philosophy (our main exposure of interest) and kidney transplant waitlisting (our outcome). Staff perceptions about patient access to kidney transplantation were collected by asking the staff to report the percentages of their patients who: “were interested in transplantation,” “were eligible for transplantation,” “were referred for kidney transplant,” and “had completed the transplant evaluation process and were successfully waitlisted.” The responses to each question were dichotomized based on the staff perception that ≥50% (vs. <50%) of their patients were interested/eligible/referred/waitlisted for transplant. Dialysis facility educational resources available for patients was collected through 10 items assessing modes of education reported to be available (such as posters and bulletin boards on kidney transplantation, videos, discussions between staff and patients on the topic of kidney transplantation, and discussions between staff and patients’ family members on kidney transplantation). The facility received 1 point for each educational resource available to its patients and a composite score (range, 0-10) was created to determine the availability of kidney transplantation education resources at each dialysis facility. We used the composite score for educational resources in subsequent descriptive and regression analyses.
Other variables
Other facility demographic, clinical, and transplant access characteristics were obtained from the DFR, including: average number of patients per facility, number of staff, profit status, average age of dialysis patients, and the percentages of patients that are white, African American, uninsured, unemployed, diagnosed with diabetes, diagnosed with hypertension, reported to be smokers, alcohol dependent, and not informed of transplant options (http://www.dialysisreports.org/Methodology.aspx).
Statistical Analysis
Demographic characteristics of the facilities that completed the survey were reported for the total sample and stratified by facility transplant philosophy and facility waitlisting performance. Kruskal-Wallis and chi-square tests compared the differences across strata for continuous and categorical variables, respectively. Descriptive statistics were generated to determine how the percentage of their patients completing various steps in the transplantation process varied by staff transplant philosophy. We used logistic regression analyses to answer our main study question of whether dialysis facility transplant philosophy was associated with facility waitlisting performance.
Correlation analysis and crude logistic regression assessed potential confounders that might influence transplant philosophy and waitlisting/transplant access, including demographic and clinical characteristics. We also tested for interactions of staff attitudes and available educational resources with transplant philosophy. All analyses were conducted using SAS® version 9.3 (SAS Institute, Cary, NC).
RESULTS
Characteristics of Dialysis Facilities by Reported Transplant Philosophy
About a quarter (24.4%) of responding dialysis facilities from ESRD Network 6’s service area reported that “transplant is the first choice for treatment,” whereas 57.2% reported that “transplant is great for some,” and 18.3% reported that “transplant is a good option if the patient is interested.” Dialysis facilities that reported “transplant is our first choice for treatment” (n=124) (Table 1) were more likely to have a higher proportion of African American dialysis patients, fewer patients with hypertension, and a higher transplant rate, compared to dialysis facilities whose staff reported “transplant is great for some.” A higher percentage of for-profit dialysis facilities were more likely to report that “transplant is a good option if the patient is interested” (88.2%) compared to 80.6% of for-profit facilities reporting “transplant is our first option” (p=0.05).
Table 1.
Characteristics of ESRD Network 6 (GA, NC, SC) dialysis facilities that completed the 25 item questionnaire (n=509), stratified by transplant philosophy
| Facility Characteristics | TOTAL (n=509) |
Transplant is our first option (n=124) 24.4% |
Transplant is great for some (n=291) 57.2% |
Transplant is a good option if the patient is interested (n=93) 18.3% |
Compari son p- value† |
|---|---|---|---|---|---|
| Demographic and Clinical Characteristics | |||||
| No. patients per facility, median (IQR) |
43.0 (30.0, 67.0) |
43.0 (31.0, 69.0) |
44.0 (29.0, 68.0) |
43.0 (31.0, 69.0) |
0.53 |
| Number of staff, median (IQR) | 11.0 (7.0, 15.0) |
7.0 (7.0, 16.0) |
15.0 (7.0, 15.0) |
11 (7.0, 16.0) |
0.42 |
| % for-profit | 87.0 | 80.6 | 89.3 | 88.2 | 0.05 |
| Patient age, median (IQR) | 61.7 (58.5, 65.0) |
60.9 (56.8, 64.6) |
61.7 (58.8, 65.1) |
60.9 (56.8, 64.6) |
0.09 |
| % of patients classified as white | 37.9 | 38.0 | 40.0 | 38.0 | <0.001 |
| % of patients classified as African American |
60.0 | 60.0 | 57.1 | 60.0 | <0.001 |
| % patients uninsured | 8.7 | 8.3 | 9.5 | 8.3 | 0.20 |
| % patients unemployed | 75.0 | 75.0 | 68.4 | 75.0 | 0.22 |
| Patient time on dialysis (years), median (IQR) |
4.9 (4.2, 5.4) |
4.9 (4.1, 5.4) |
4.8 (4.3, 5.4) |
4.9 (4.1, 5.4) |
0.91 |
| % patients with diabetes | 61.1 | 61.5 | 61.5 | 61.5 | 0.88 |
| % patients with hypertension | 92.3 | 90.9 | 91.9 | 90.9 | 0.02 |
| % patients currently smoking | 6.4 | 6.3 | 6.7 | 6.3 | 0.94 |
| % patients alcohol-dependent | 0.0 | 0.0 | 0.0 | 0.0 | 0.31 |
| Patient count of comorbid conditions, median (IQR) |
3.1 (2.5, 3.6) |
3.0 (2.5, 3.5) |
3.1 (2.6, 3.6) |
3.0 (2.5, 3.5) |
0.36 |
| Standardized Transplant Ratio, median (IQR) |
0.6 (0.3, 0.9) |
0.8 (0.4, 1.1) |
0.6 0.4, 0.9) |
0.8 (0.4, 1.1) |
0.02 |
| Dialysis Facility-Reported Characteristics | |||||
| % reporting availability of a patient and caregiver support group |
87.6 | 86.3 | 88.3 | 87.1 | 0.84 |
| % reporting established protocol to educate patients on KTx |
83.9 | 85.5 | 83.2 | 83.9 | 0.84 |
| Number of transplant education resources available, median (IQR) |
6 (4, 7) | 6 (5, 8) | 6 (4, 7) | 5 (4,7) | 0.0004 |
| % perceiving ≥ 50% of their patients: |
|||||
| Are interested in KTx | 18.4 | 28.2 | 16.3 | 11.5 | 0.003 |
| Are eligible for KTx | 23.1 | 36.6 | 17.7 | 21.4 | <0.001 |
| Have been referred for KTx | 37.4 | 55.7 | 31.1 | 32.1 | <0.0001 |
| Have completed evaluation and been waitlisted for KTx |
9.1 | 11.7 | 9.5 | 4.6 | 0.21 |
Abbreviations: IQR, interquartile range; KTx: Kidney Transplantation
Chi-square or Kruskal Wallis comparison tests were used to determine statistical differences between categorical or continuous variables, respectively
Characteristics of Dialysis Facilities by Dialysis Facility Waitlisting Performance
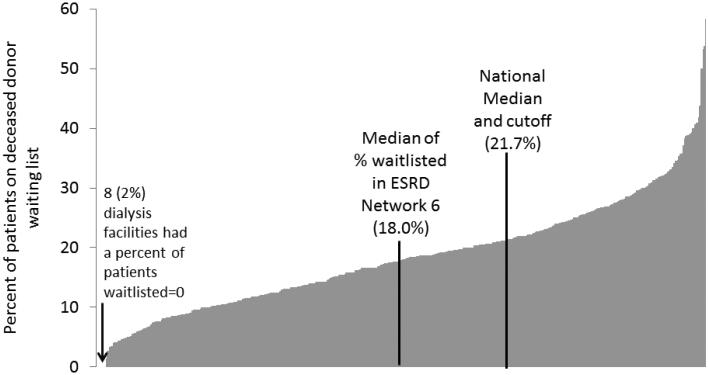
More than two-thirds (68%) of the responding dialysis facilities were low-performing in terms of waitlisting (61.7%, 76.2%, and 70.2% of facilities in NC, SC, and GA, respectively) and the median percentage of patients waitlisted at facilities in ESRD Network 6 was 18.0% (IQR 11.5%, 23.8%). Facility characteristics that were associated with lower waitlist performance (Table 2) included a higher proportion of patients in a facility who were African American (OR: 0.99; 95% CI: 0.98-0.99), and a higher number of comorbidities (OR: 0.7; 95% CI: 0.6-0.9). Figure 1 shows the distribution of dialysis facility performance measured by waitlisting performance.
Table 2.
Characteristics of ESRD Network 6 (GA, NC, SC) Dialysis Facilities (n=509) stratified by Waitlisting Performance
| TOTAL (n=509) |
%Waitlisting Above National Median† (n=160) 31.4% |
%Waitlisting Below National Median (n=349) 68.6% |
Crude Logistic Regression Odds Ratio (at or above vs. below) (95% CI) |
|
|---|---|---|---|---|
| Dialysis Facility Demographics | ||||
| No. patients per facility, median (IQR) | 43.0 (30.0, 67.0) |
44.0 (30.5, 75.0) |
43.0 (29.0, 64.0) |
1.01 (1.00, 1.02) |
| Number of staff, median (IQR) | 11.0 (7.0, 15.0) |
11.0 (7.0, 16.0) |
11.0 (7.0, 15.0) |
1.02 (0.99, 1.04) |
| % for-profit | 87.0 | 87.4 | 86.3 | 0.92 (0.53, 1.59) |
| Patient age, median (IQR) | 61.6 (58.5, 65.1) |
61.8 (58.1, 64.5) |
61.5 (58.6, 65.2) |
0.98 (0.95, 1.01) |
| % of patients classified as white | 37.5 | 46.2 | 33.3 | 1.02 (1.01, 1.02) |
| % of patients classified as African American |
60.0 | 50.0 | 62.5 | 0.985 (0.98, 0.99) |
| % patients uninsured | 8.7 | 8.0 | 9.1 | 0.99 (0.97, 1.01) |
| % patients unemployed | 71.4 | 66.7 | 75.0 | 0.99 (0.98, 1.00) |
| Patient time on dialysis (years), median (IQR) |
4.8 (4.2, 5.4) |
4.8 (4.4, 5.4) |
4.7 (4.2, 5.5) |
0.97 (0.81, 1.16) |
| % patients with diabetes | 61.5 | 58.3 | 62.5 | 0.99 (0.97, 1.00) |
| % patients with hypertension | 92.3 | 90.4 | 93.3 | 0.99 (0.98, 1.00) |
| % patients currently smoking | 6.5 | 6.3 | 6.7 | 1.00 (0.98, 1.02) |
| Patient count of comorbid conditions, median (IQR) |
3.1 (2.6, 3.6) | 3.0 (2.5, 3.4) | 3.1 (2.6, 3.7) | 0.74 (0.58, 0.93) |
| Dialysis Facility-Reported Characteristics | ||||
| Transplant Philosophy | ||||
| Transplant is a good option if the patient is interested |
18.3 | 12.6 | 20.9 | 1.00 |
| Transplant is a great option for some |
57.3 | 57.9 | 57.0 | 1.47 (0.80, 2.68) |
| Transplant is our first option | 24.4 | 29.6 | 22.1 | 2.56 (1.33, 4.91) |
| Percentage of Dialysis Facilities that perceive ≥ 50% of their patients are… |
||||
| Interested in KTx |
18.4 | 26.8 | 14.5 | 2.15 (1.35, 3.41) |
| Eligible for KTx |
23.1 | 27.9 | 20.8 | 1.47 (0.95, 2.29) |
| Referred for KTx |
37.4 | 45.2 | 33.7 | 1.62 (1.10, 2.39) |
| Completed Evaluation and were Waitlisted for KTx |
9.1 | 16.5 | 5.9 | 3.16 (1.70, 5.89) |
| Number of transplant education resources available, median (IQR) |
6 (4, 7) |
6 (4, 7) |
6 (4, 7) |
0.99 (0.91, 1.07) |
Abbreviations: IQR, interquartile range; KTx, kidney transplantation
National median for waitlisting was 21.7% of patients (age<70 years), 2008-2011
Figure 1.
Distribution of the percentage of prevalent patients on the kidney transplant waiting list (2008-2011) among responding Southeastern (ESRD Network 6 of GA, NC, and SC) dialysis facilities (n=509)
Staff Perceptions and Available Educational Resources
Overall, facilities varied in their reporting that more than half of their patients were interested in kidney transplant (18.3%), eligible for a kidney transplant (23.1%), referred for kidney transplant (37.4%), and had completed evaluation and were waitlisted for a kidney transplant (9.1%). Facility perceptions of patient interest, eligibility, and referral varied by transplant philosophy; facilities with the most positive transplant philosophy (“transplant is our first option”) reported a significantly higher proportion of patients who were interested in kidney transplant (28.2% vs. 11.5%), eligible for kidney transplant (36.6% vs. 21.4%), or referred for kidney transplant (55.7% vs. 32.1%) compared to “transplant is a good option if the patient is interested” (Table 1). Facilities with staff perceiving more than 50% of their patients were interested in (OR=2.2; 95% CI 1.5, 3.4), eligible (OR=1.5; 95% CI 0.95, 2.3), or referred (OR=1.6; 95% CI 1.1, 2.4) for a kidney transplant were more likely be high-performing (meeting or exceeding the national median of waitlisting) in crude analyses, compared to facilities that perceived less than half of their patients were interested/eligible/referred/waitlisted for transplant (Table 2).
The median number of transplant educational resources available within participating dialysis facilities was 6 (IQR: 4-7). Dialysis facilities that reported “transplant is our first option” were more likely to have more transplant educational resources available to their patients compared to facilities that reported “transplant is a good option if the patient is interested” (p-value=0.04).
Association of Dialysis Facility Transplant Philosophy with Facility Waitlisting Performance
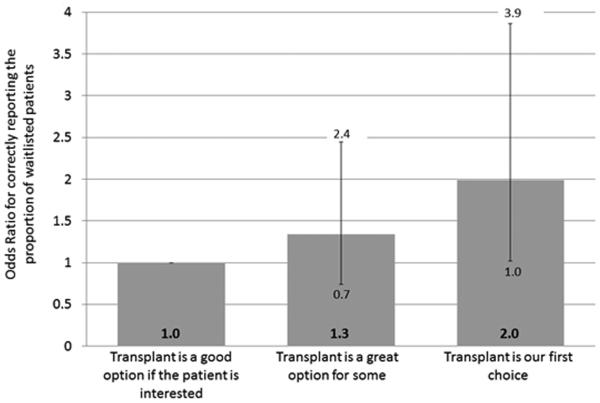
In crude analysis, a more positive transplant philosophy was associated with higher waitlisting performance, with “transplant is a great option for some” and “transplant is our first option” being associated with 1.5- and 2.6-fold higher odds of waitlisting (Table 2). After adjustement for facility characteristics, dialysis facility transplant philosophy remained positively associated with facility waitlist performance. Dialysis facilities that reported “transplant is a great option for some” were 30% (OR=1.3, 95% CI 0.7, 2.4) more likely to be high-performing with respect to kidney transplantion, compared to facilities that reported “transplant is a good option if the patient is interested.” Dialysis facilities that reported “transplant is our first choice” were more than twice (OR=2.0, 95% CI 1.0, 3.9) as likely as those that reported “transplant is a good option if the patient is interested” to be high-performing (Figure 2). Statistical tests for interaction reported no significant interaction between staff perceptions of patient interest (p=0.77), eligibility (p=0.72), or referral status (p=0.44) and facility transplant philosophy. Tests for interaction also showed no statistically significant interaction between number of available education resources (p=0.22) and facility transplant philosophy.
Figure 2.
Multivariable-adjusted odds ratios for high waitlisting performance (percentage of patients waitlisted > national median value) by dialysis facility transplant philosophy in 509 Southeastern (ESRD Network 6 of GA, NC, and SC) dialysis facilities
*Adjusted for dialysis facility demographics including number of patients, average age, percent of African American patients, percent of patient on hemodialysis, percent of patients unemployed, and average count of patient comorbidities
DISCUSSION
To our knowledge, this is the first-large scale, dialysis facility questionnaire in the Southeast with a completion rate >90% to assess dialysis facility philosophy with respect to kidney transplantation and the first study to examine the association of this philosophy with waitlisting performance at the facility. We reported that dialysis facilities with the most positive transplant philosophy had two-fold higher odds of meeting or exceeding the national median waitlisting percentage, compared to those facilities that had the least positive transplant philosophy.
Our results have important implications for how policy makers, such as ESRD Networks, who may be able to intervene at the dialysis facility level to improve access to kidney transplantation for patients. Only one-quarter of the dialysis facilities we surveyed agreed that transplant was the best option for patients, which is in contrast to the 75% of nephrologists who agreed that transplant was the best option for patients in an international survey of nearly 1,500 nephrologists [15]. A previous study demonstrated that health care professionals’ attitudes toward transplantation affected access to transplant [10, 16]. Conesa et al found that, in a survey of 160 primary care physicians, positive and negative attitudes toward transplantation have an overwhelming influence on the patients and families’ decision about transplant [16]. Our study supports this association and showed that facilities who reported “transplant is our first choice” and “transplant is great for some” were more likely to be high performing facilities based on waitlisting, compared to facilities that reported the philosophy “transplant was a good option if the patient is interested.” By identifying facilities with less positive transplant philosophies, it may be possible to focus interventions on improving the attitudes about the benefits of kidney transplant among dialysis facility providers. This may be particularly important in the Southeastern US, where transplant rates are the lowest in the United States [11]. We also found that dialysis facilities with lower waitlisting performance had a higher proportion of African American patients, and more patients with diabetes and hypertension. These results are similar to previous literature [4] that reported diminished access to kidney transplantation was significantly associated with higher proportion of African Americans and higher percentage of patients with diabetes. Identifying dialysis facilities with less positive transplant philosophy and low waitlisting performance may be helpful to improve and concentrate efforts to increase access to transplant. Public health interventions could also focus on staff-level interventions that educate staff on the benefits of kidney transplantation [5] and the transplant process.
Our study found that there were no statistically significant interactions of the association between transplant philosophy and waitlisting performance by either staff perceptions or available education resources, suggesting that these factors do not substantially modify the observed association between facility transplant philosophy and waitlisting performance. . While literature shows staff perceptions can be associated with patient outcomes, prior studies suggests that there may be a discordance between staff perceptions and patient-reported metrics [17]. Among dialysis patients residing in the Baltimore area (n=348), Salter et al [18] found that physicians reported 78% of their dialysis patients were “informed of transplant” while only 20% of those patients verified this education through self-report [18]. This research complements previous findings that patients reporting that they were informed of transplant options were 3 times as likely to be waitlisted as dialysis patients reporting that they were not informed [19]. This suggests that facility staff should not rely on their perceptions of patient interest in transplant and should be discussing all ESRD treatment options, developing a plan to pursue transplant, and tracking the progress through the transplantation process for each dialysis patient [20]. Research has also shown dialysis facilities may have insufficient educational resources [5, 21, 22], a theme echoed by dialysis patients [23, 24], despite randomized control trials that support enhancing patient education is likely to increase patient transplant knowledge and decision-making [25, 26]. Public health researchers should continue to develop culturally sensitive educational materials that inform patients of the benefits of transplant [27] while teaching them skills to explore living donation transplant [28].
This study has a few limitations. Although the survey was primarily completed by the facility social worker or nurse manager, who are familiar with facility practices and philosophy, the survey was still self-reported and items may have been subject to misclassification. It is unknown whether the health care staff examined in this study accurately reported facility-level philosophy and perceptions about kidney transplant. The Southeastern Kidney Transplant Coalition developed the survey to provide an accurate account of facility protocols and perceptions, but the responders could have provided the more social desirable answer that may be more in accordance with regulations and government mandates; however, there is no mandate requiring the facilities to have a specific transplant philosophy. A small percentage (7%) of participating facilities did not match to the 2008-2011 Dialysis Facility Report, creating the potential for selection bias. However, our analyses did not find any differences in facility characteristics between those not matched and those included in our study. Another potential limitation is that this survey was conducted in NC, SC, and GA dialysis facilities and the results of this survey should be carefully generalized to other populations. It should also be recognized that the statistical tests for interaction may have been limited by small sample sizes within each strata and the analyses should be replicated on a larger sample of dialysis facilities. Additionally, survey items for transplant philosophy, attitudes, and educational resources have not been validated; however, survey items do have good face and content validity since a team of stakeholders from the kidney disease community, including nephrologists, social workers, and researchers, developed the items. Finally, the analyses were limited to dialysis facility-level characteristics available in the DFR, which did not include data on neighborhood poverty or rural and urban classification. Future studies could obtain these characteristics and determine whether poverty and rural and urban classification, which are associated with access to kidney transplantation [29], are similarly associated with transplant philosophy .
To the best of our knowledge, this is the first study to investigate the association between dialysis facility’s transplant philosophy and access to kidney transplantation. Our study suggests that facilities with a more positive transplant philosophy are twice as likely to have higher waitlisting performance compared to facilities that had a less positive transplant philosophy, regardless of staff perceptions and available educational resources. Dialysis facility staff members have the opportunity to make a significant impact on their patients’ health and quality of life by educating their dialysis patients on the benefits of all treatment options. Future research should investigate the relationships between dialysis facility protocols, practices, and transplant philosophy to provide an improved understanding of their effect on access to transplantation. Research or evidence-based quality improvement interventions are needed to determine whether targeting dialysis facility- and staff-level interventions to facilities with less positive transplant philosophy could improve waitlisting performance.
Acknowledgements
The authors acknowledge the Southeastern Kidney Council and all of the members of the Southeastern Kidney Transplant Coalition for their significant assistance with this work. The authors disclosed receipt of the following financial support for the research, authorship, and or publication of this article: This work was supported in part by NIH NIDDK Award R15DK088707 (Browne) and NIH NIMHD Award R24MD008077 (Amamoo, Gander, Patzer, Pastan). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDDK, NIMHD or the NIH. The analyses upon which this publication is based were performed under Contract Number HHSM-500-2013-NW006C entitled End Stage Renal Disease Networks Organization for the State (Commonwealth) of GA, NC & SC, sponsored by the Centers for Medicare & Medicaid Services, Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
Footnotes
Conflicts of Interest and Disclosures
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Dr. Pastan is a minority shareholder in Fresenius College Park Dialysis, College Park, GA.
References
- 1.System, U.S.R.D. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health. National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2013. U S Renal Data System. [Google Scholar]
- 2.Tonelli M, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- 3.Laupacis A, et al. A study of the quality of life and cost-utility of renal transplantation. Kidney international. 1996;50(1):235–242. doi: 10.1038/ki.1996.307. [DOI] [PubMed] [Google Scholar]
- 4.Patzer RE PL, Krisher J, Pastan SO. Dialysis Facility and Network Factors Associated with Low Kidney Transplantation Rates Among United States Dialysis Facilities. American Journal of Transplantation. 2014;14(7) doi: 10.1111/ajt.12749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waterman AD, Hyland S, Goalby C, Robbins M, Dinkel K. Improving Transplant Education in the Dialysis Setting: The "Explore Transplant" Initiative. Dialysis and Transplantation. 2010:236–241. [Google Scholar]
- 6.Sneeuw K, et al. Value of caregiver ratings in evaluating the quality of life of patients with cancer. Journal of Clinical Oncology. 1997;15(3):1206–1217. doi: 10.1200/JCO.1997.15.3.1206. [DOI] [PubMed] [Google Scholar]
- 7.McDonald MV, et al. Nurses' recognition of depression in their patients with cancer. Oncology nursing forum. 1999 [PubMed] [Google Scholar]
- 8.Kane RL, et al. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Medical care. 2007;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 9.Blegen MA, Goode CJ, Reed L. Nurse staffing and patient outcomes. Nursing research. 1998;47(1):43–50. doi: 10.1097/00006199-199801000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Siminoff LA, Arnold RM, Caplan AL. Health care professional attitudes toward donation: effect on practice and procurement. Journal of Trauma and Acute Care Surgery. 1995;39(3):553–559. doi: 10.1097/00005373-199509000-00025. [DOI] [PubMed] [Google Scholar]
- 11.Patzer R, Pastan S. Kidney transplant access in the southeast: View from the bottom. American Journal of Transplantation. 2014 doi: 10.1111/ajt.12748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patzer RE, et al. The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC nephrology. 2014;15(1):171. doi: 10.1186/1471-2369-15-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Browne T, Amamoo A, Gander G, Sauls L, Krisher J, Patzer RE, Pastan S. National Kidney Foundation. Las Vegas, NV: 2014. Environmental Scan of Kidney Transplant Referral Practices in Southeastern United States. [Google Scholar]
- 14.Razali NM, Wah YB. Power comparisons of shapiro-wilk, kolmogorov-smirnov, lilliefors and anderson-darling tests. Journal of Statistical Modeling and Analytics. 2011;2(1):21–33. [Google Scholar]
- 15.Ghahramani N, et al. Nephrologists’ perceptions of renal transplant as treatment of choice for end-stage renal disease, preemptive transplant, and transplanting older patients: an international survey. Experimental and clinical transplantation: official journal of the Middle East Society for Organ Transplantation. 2011;9(4):223. [PMC free article] [PubMed] [Google Scholar]
- 16.Conesa C, et al. Transplantation proceedings. Elsevier; 2005. Rural primary care centers as a source of information about organ donation. [DOI] [PubMed] [Google Scholar]
- 17.Sneeuw KC, Sprangers MA, Aaronson NK. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. Journal of clinical epidemiology. 2002;55(11):1130–1143. doi: 10.1016/s0895-4356(02)00479-1. [DOI] [PubMed] [Google Scholar]
- 18.Salter ML, et al. Health-Related and Psychosocial Concerns about Transplantation among Patients Initiating Dialysis. Clinical Journal of the American Society of Nephrology. 2014 doi: 10.2215/CJN.03310414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salter ML, et al. Patient-and Provider-Reported Information about Transplantation and Subsequent Waitlisting. Journal of the American Society of Nephrology. 2014 doi: 10.1681/ASN.2013121298. ASN. 2013121298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Register F. Conditions for coverage for ESRD facilities. U.S. Government Printing Office; Washington, DC: 2008. [Google Scholar]
- 21.Maiorano A, Schena F. The dynamics of kidney donation: Viewpoints from the donor, the recipients, and the transplant team. Kidney international. 2008;73(10):1108–1110. doi: 10.1038/ki.2008.118. [DOI] [PubMed] [Google Scholar]
- 22.Conesa C, et al. Transplantation proceedings. Elsevier; 2005. Attitude of primary care nurses toward living kidney donation. [DOI] [PubMed] [Google Scholar]
- 23.Browne T, et al. National Kidney Foundation Clinical Meeting. Las Vegas, NV: 2014. Patient identified barriers and facilitators to kidney transplantation. [Google Scholar]
- 24.Vianello A, et al. Attitudes and knowledge about transplantation in dialyzed patients requesting a cadaveric kidney graft. Clinical nephrology. 2000;53(4):64–6. suppl. [PubMed] [Google Scholar]
- 25.Moody E, et al. Improving on-line information for potential living kidney donors. Kidney international. 2007;71(10):1062–1070. doi: 10.1038/sj.ki.5002168. [DOI] [PubMed] [Google Scholar]
- 26.Waterman AD, et al. Renal patients' use of the internet to learn about transplantation. Transplantation. 2006;82(1):594. [Google Scholar]
- 27.Patzer RE, Larsen CP, McClellan WM, Howard D, Huang E, Arriola KJ. American Society of Nephrology Kidney Week 2013. Atlanta, GA: 2014. Dialysis or transplant: Use of a novel shared decision making tool for treatment options. B.M. [Google Scholar]
- 28.Arriola K. Project living ACTS: Living donor transplant education for African American end-stage renal disease patients; 141st APHA Annual Meeting (November 2-November 6, 2013); 2013. APHA. [Google Scholar]
- 29.Tonelli M, et al. Access to kidney transplantation among remote-and rural-dwelling patients with kidney failure in the United States. JAmA. 2009;301(16):1681–1690. doi: 10.1001/jama.2009.545. [DOI] [PubMed] [Google Scholar]