Abstract
Young men who have sex with men are at increased risk for HIV. Research with older men and high risk populations suggests that network dynamics may contribute to the spread of infectious disease and HIV, but little is known about the sexual networks of young men who have sex with men. Utilizing a unique dataset, this study presents novel descriptive data about the sexual networks of racially diverse 17- to 23-year-old young men who have sex with men. Additionally, individual, partner, and network characteristics of these young men who have sex with men were examined as potential drivers of HIV, STI, and unprotected intercourse. Results indicated several partner- and network-level factors associated with HIV and associated outcomes.
Keywords: Sexual Networks, HIV, Young Men, Gay
Introduction
Young men who have sex with men (YMSM) have an alarming HIV/AIDS prevalence. Out of the 39,495 HIV infections estimated in the United States in 2011 within males, 78.2% of the HIV infections were among men who had sex with men and of those, 25% of infections occurred within youth 13-24 years old (CDC, 2013). Additionally, YMSM are one of the only risk groups showing an increasing rate of infections from 2008-2011 (CDC, 2013). Despite the urgent need for a developmentally-specific knowledge-base regarding HIV/AIDS in YMSM, there has been insufficient research focused specifically on understanding the sexual behaviors and risk factors of this population (Harper & Riplinger, 2013; B. S. Mustanski, Newcomb, Du Bois, Garcia, & Grov, 2011). Additionally, although social network research is a high priority area in HIV research due to the disease’s high transmission dependence on drug and sexual network dynamics (Friedman et al., 1997; Johnson et al., 2010; C. A. Latkin, Forman, Knowlton, & Sherman, 2003; Weeks, Clair, Borgatti, Radda, & Schensul, 2002), the majority of HIV research that has been conducted with YMSM has focused on understanding individual-level sexual behaviors (Johnson et al., 2010). Studies of individual-level HIV-related risk behavior, while critically important, have limitations for understanding and intervening on spread of HIV/AIDS (Johnson et al., 2010).
Dyadic Research and HIV
Although few network studies have been conducted with YMSM, there have been several studies which demonstrate that characteristics of sexual relationships and sexual partners influence risk-taking behaviors (e.g., Newcomb, Ryan, Garofalo, & Mustanski, 2014). One consistent finding is the association of relationship-type and sexual risk behavior, with YMSM being more likely to engage in unprotected anal intercourse when they deem relationships as serious and committed (Bingham et al., 2003; MacKellar et al., 2005; B. Mustanski, 2007; Newcomb, Ryan, Garofalo, et al., 2014; Tieu et al., 2014; Webster et al., 2003). Similarly, when YMSM indicated knowledge of a sexual partner having concurrent sexual relationships, condom usage increased (B. Mustanski, Newcomb, & Clerkin, 2011; Newcomb, Ryan, Garofalo, et al., 2014). Relationships indicated to be committed and exclusive may be perceived as less risky to YMSM, which may decrease condom use (Greene, Andrews, Kuper, & Mustanski, 2014).
Characteristics of sexual partners may also influence perceptions of sexual risk and condom use. Partner age, race and gender have all been linked to condom use during anal intercourse, with individuals reporting decreased condom use when having anal intercourse with older partners, non-African American partners, and female partners (Clerkin, Newcomb, & Mustanski, 2011; Newcomb, Ryan, Garofalo, et al., 2014). Furthermore, sexual partner characteristics have been shown to be associated with HIV status. In a study of racially diverse MSM aged 23-29, when controlling for participants’ demographics and risk behaviors, HIV+ men were more likely to have had older and African American sexual partners (Bingham et al., 2003).
And finally, characteristics of the sexual encounter itself may also be related to risk behavior. Research supports that using drugs prior to sex significantly increases the likelihood of unprotected anal intercourse among YMSM (B. Mustanski et al., 2011; Newcomb, Ryan, Garofalo, et al., 2014; Pantalone, Huh, Nelson, Pearson, & Simoni, 2014). Overall, this research suggests that HIV risk cannot be understood only by examining individual-level characteristics; attributes of relationships, partners, and sexual events influence individual decision-making around condom use, as well as influence the likelihood of contact with HIV+ sexual partner (Cooper, 2010).
Network Research and HIV
While the previously discussed literature examined dyadic associations between individuals and their immediate sexual partners, network studies allow greater understanding of an individual’s overall system of relationships. Outcomes may be examined by attributes of network members or by the structure of relationships between network members. Further, network studies may examine a variety of social linkages or interactions between network members, such as sexual relationships, friendships, or drug use. The network dynamics of these systems may provide understandings into HIV transmission unable to be seen at merely the individual or dyadic level.
Few observational studies of the sexual networks of YMSM currently exist due to both the difficulty of accessing hidden-populations (Meyer & Wilson, 2009) and the resource intensiveness of network data capture (Scott & Carrington, 2011). Therefore, much of the work which has demonstrated the importance of network dynamics in infectious disease has been computational (Kretzschmar & Morris, 1996; Morris & Kretzschmar, 1997; Morris, Podhisita, Wawer, & Handcock, 1996; Shirley & Rushton, 2005). Using simulations of sexual network data, these studies have found that even small increases in sexual partner concurrency are able to lead to significant decreases in overall network path length (e.g. the speed at which HIV is able to move through a network) (Kretzschmar & Morris, 1996; Morris & Kretzschmar, 1997). However, thus far empirical data supporting these computational findings have been mixed (Kretzschmar & Carael, 2012). Therefore, it has been advised that network models be both informed and validated by empirical observations of the susceptible population (Kretzschmar & Carael, 2012; Shirley & Rushton, 2005).
Although there is a limited observational data on the sexual networks of YMSM, several key findings have emerged based on empirical studies of MSM. In particular, several studies have demonstrated that HIV status, as well as HIV-related risk behaviors, cluster significantly by network. For example, HIV+ individuals are significantly more likely to have social network members who are also HIV+ (Amirkhanian, 2014; Drumright & Frost, 2010; El-Bassel, Gilbert, Wu, & Chang, 2006; Kelly et al., 2010). Another study of Russian YMSM networks interviewed 187 participants within 38 social circles. Their analysis demonstrated that social network membership accounted for 27-29% of the observed variance across three sexual-risk outcomes, while individual attributes only accounted for 3-8% of the observed variance (Amirkhanian et al., 2006) and that social network membership was the only significant predictor of an individual’s STI status (Amirkhanian et al., 2006). These results suggest that similar to other individual characteristics (McPherson, Smith-Lovin, & Cook, 2001), HIV-related characteristics also display strong homophily within social networks (i.e., “birds of a feather flock together”). However, the mechanisms driving this network clustering (i.e. selection or socialization) are undetermined and should be interpreted with caution (Kandel, 1978).
In addition to network clustering, a few other sexual and social network attributes have been associated with HIV, STI, and sexual risk behavior in MSM. One is sexual network degree (e.g., the number of sexual partners), with many studies indicating that greater sexual degree is associated with greater likelihood of being positive for HIV or another STI (e.g., Drumright & Frost, 2010; El-Bassel et al., 2006; Ellen et al., 2006). Additionally, there is preliminary evidence that the selection of a sexual partner who is not also a social network member (i.e., low multiplexity) is protective against STI infection (Ellen et al., 2006). Further research is needed to understand this dynamic, but two possible mechanisms are that: 1) multiplex sexual/social relationships may lead to changes in the sexual network structure and thereby increase the speed at which STI infection may spread; or 2) like findings around reduced condom use with serious partners; multiplex social/sexual partners may be viewed as lower risk (i.e., “known partners are safe partners) (C. Latkin et al., 2012). Another finding is that in addition to sexual network structure, the structure of the social network may also be important. A number of studies have reported decreased sexual risk behaviors are associated with high social network density (El-Bassel et al., 2006; Smith, Grierson, Wain, Pitts, & Pattison, 2004), which suggests protective influence by social networks. And finally, in one of the first MSM network studies to move beyond egocentric data to examine sexual network structure, bridging position was found to be associated with HIV status in young black MSM (Shah et al., 2014).
The Current Study
The current study reports rich descriptive data taken from 175 network interviews with YMSM, with a focus on sexual networks. Detailed information about attributes of participants and their sexual partners is provided, followed by details about sexual behavior, as well as characteristics important to networks (i.e., concurrency, sexual network density, multiplexity, and homophily). Sexual network characteristics are then examined as correlates of HIV, STI, and unprotected anal intercourse. Finally, associations with unprotected anal intercourse are examined in a multilevel model, including both individual and partner-level attributes
Method
Participants
A sub-sample of 175 participants, taken from a larger, ongoing longitudinal research study analyzing the prevalence, course, and predictors of health issues facing YMSM (Kuhns et al., In Press; B. Mustanski, Ryan, & Garofalo, 2014; Newcomb, Ryan, Garofalo, et al., 2014; Newcomb, Ryan, Greene, Garofalo, & Mustanski, 2014), were recruited to participate in a separate cross-sectional study aimed at better understanding YMSM’s social, sexual and substance using network structure. Participants for this network study were recruited via the parent study at either the 12-month or 24-month follow-up visits between June of 2011 and October of 2012. In order to be eligible for the parent study, an individual had to be assigned male sex at birth, 16 to 20 years at baseline, an English speaker, report a sexual encounter with a male or have a gay/bisexual identity, and be available for 2 years of follow-up. A total of 204 parent study participants were contacted about partaking in this network study, of which 179 (88%) agreed to participate. However, two participants never showed up for their scheduled appointment and two enrolled, but subsequently withdrew. Eight participants reported never having a sex partner and thus were excluded from many of the subsequent analyses. At the time of their network interview participants ranged from 17 to 23 years old. The final demographic characteristics of egos (n=167) and sex partners (n=837) can be found in Table 1. The study protocol was approved by the Institutional Review Boards at each site and participants were provided $25 for their participation.
Table 1. Demographic Characteristics of Egos and Alters Who are Sex Partners.
| Egos (n=167) |
Alters (n=837) |
|||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age1 | 20.1 | 1.4 | 22.4 | 4.5 |
| N | % | N | % | |
| Gender | ||||
| Male | 167 | 100.0 | 767 | 91.6 |
| Female | 0 | 0.0 | 63 | 7.5 |
| Transgender | - | - | 7 | 0.8 |
| Race | ||||
| Black | 91 | 54.5 | 410 | 49.0 |
| Latino | 37 | 22.2 | 176 | 21.0 |
| White | 22 | 13.2 | 189 | 22.6 |
| Other | 17 | 10.2 | 61 | 7.3 |
| Missing | 0 | 0.0 | 1 | 0.1 |
| Sexual Orientation | ||||
| Gay/Lesbian | 140 | 83.9 | 629 | 75.1 |
| Bisexual | 21 | 12.6 | 128 | 15.3 |
| Heterosexual | 3 | 1.8 | 65 | 7.8 |
| Other | 3 | 1.8 | 7 | 0.8 |
| Missing | 0 | 0.0 | 8 | 1.0 |
| Relationship Type | - | - | ||
| Main Partner | - | - | 306 | 36.6 |
| Friend | - | - | 279 | 33.3 |
| Non-Main/Non-Friend | - | - | 252 | 30.1 |
| Neighborhood | ||||
| Chicago | 143 | 85.6 | 461 | 55.1 |
| Outside City of Chicago | 24 | 14.4 | 276 | 33.0 |
| Unknown | - | - | 100 | 11.9 |
| HIV Prevalence | 19 | 11.4 | - | - |
| STI Prevalence | 12 | 7.2 | - | - |
Alter age was missing for 5 sex partners
Procedure
An egocentric data collection approach was adopted to gather information from respondents’ self-reported perceptions of their network alters instead of firsthand interviews with network members themselves (Scott & Carrington, 2011). Procedures used to obtain network data have been explained in detail elsewhere (Kuhns et al., In Press), and included the following processes: 1) asking respondents to enumerate all persons for which they have a social, sexual, or substance using connection with; 2) to describe characteristics of all network members, and to portray connections between all network members. In order to capture this network-based information, interviewers utilized a two method approach that consisted of completion of a pre-numbered list form to enumerate alters and to capture alter characteristics, as well as a participant-aided sociogram – or a chart of people and their relationships to each other – to elicit respondent’s reported connections between alters.
Measures
Name Generator
Sexual network information was determined in the network interviews by first eliciting a list of individuals the participant had supportive relationships with via five initial name generating items (See Kuhns et al. (In Press) for a detailed description of these items and the network interview). After the initial list of supportive individuals were generated, participants were then asked which individuals on that list they had “used drugs or alcohol with” or “had sex with.” Then they were asked to name anyone else that they had not yet listed that they had “used drugs or alcohol with” or “had sex with”. And finally they were asked if there was anyone that they had not listed yet that has ‘used drugs or alcohol’ or ‘had sex with’ two or more of the people on their list. Data from up to 40 alters were collected. After the list of names of alters was generated, demographic characteristics (age, race, gender, perceived sexual identity, cross-streets of where the individual lives), characteristics of the relationship (frequency of contact, strength of relationship, and relationship type), and behaviors with that person (first and last dates of sexual contact, frequency of sexual contact, condom use) were assessed. In addition to the above measures, HIV and STI infection status of the respondent (ego) was drawn from the matching wave of the parent longitudinal study. Finally, only alters who were indicated to have had sex with the egos were deemed to be part of the sexual network (n = 837).
Relationship Type
Relationship type was coded from an item which allowed egos to categorize the type of relationship held with an alter from a choice of 28 different categories (e.g., Mother, Cousin, Friend, Boyfriend, Teacher). Participants were also able to answer this question twice to assign two relationship types. Additionally, participants were able to choose “Other” and write in their own description of the relationship. Sex partners that were labeled as a boyfriend, girlfriend, partner, ex-boyfriend, ex-girlfriend, or another term similar term such as ‘Boo’, were coded as Main Partners. Sex Partners which were not coded as Main Partners and were labeled as a friend were coded as Friend. Sex Partners that met neither of these criteria were labeled as Non-Main/Non-Friend.
Drug Use with Sex Partner
Drug use was coded 1 if the participant indicated that they ever used substances or drugs at any time with the sexual partner.
Concurrent Partner
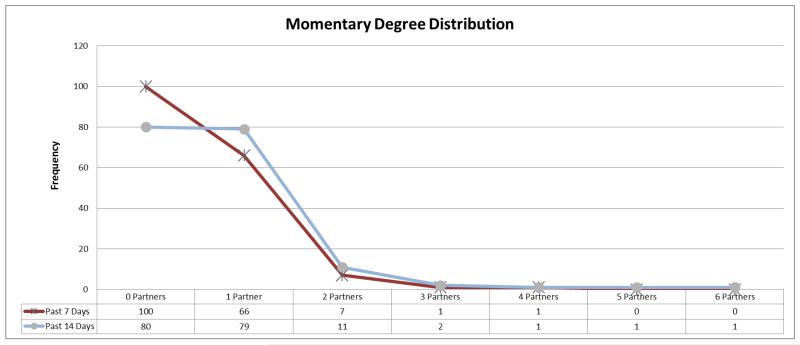
For each partner, the ego indicated the start and end date of sexual contact. Using those dates, concurrency was defined as occurring when a partner’s sexual relationship overlapped with another sexual partner. Concurrency was coded 1 if the sexual partner was indicated to be concurrent with at least 1 other sexual partner. Additionally, momentary degree over the prior 7 and 14 days was also calculated (Morris, Kurth, Hamilton, Moody, & Wakefield, 2009). In this case, momentary degree refers to the number of sexual partners an ego indicated over the prior 7 or 14 days. For example, a sample with an average 7 day momentary degree of 0 would have indicated no sexual partners in the prior week, while an average degree of 1 would have indicated the sample had an average of one sexual partner over the prior week, and finally, an average degree >1 would have indicated a tendency for the sample to have more than 1 sexual partner, on average, over the 7 day period.
Density
Density of each sexual network was calculated by summing the number of sexual connections observed between the egos/alter and alter/alter pairs, and then dividing by the total number of possible pairs given the number of support, sex, and drug connections that were reported by each ego (Marsden, 2002).
Multiplexity
Multiplexity was calculated by determining the extent of overlap between multiple networks (e.g., sex, support, and drug). In this analysis we were interested in the overlap of sex and drug networks and sex and support networks, as individuals with sex partners who are also drug partners, or sex partners who are also embedded within their support network, may display differing levels of risk (Neaigus et al., 1994). Correlations between ego sexual networks, drug networks, and support networks were calculated by utilizing QAP Correlation function within UCINET (Borgatti, Everett, & Freeman, 2002), which calculates a measure of the association between the observed matrices. After calculating a Pearson’s correlation coefficient between the matrices, the function uses quadratic assignment procedures to develop standard errors by randomly permuting the cells of one matrix and re-computing the correlation 500 times. If the proportion of random correlations greater than the observed correlation is low (p < 0.05), there is a relationship between the matrices unlikely to be observed by chance (Borgatti et al., 2002).
Racial Homophily
Newman’s Assortativity Coefficient was used to describe the racial mixing pattern in our sample (Newman, 2002). The Assortativity Coefficient is calculated from the racial mixing matrix, a matrix comprised of the proportion of sexual relationships between Black, White, Hispanic, and Other Egos and Alters. The formula for the Assortativity Coefficient (AC), with M equaling the mixing matrix, is:
AC ranges from 1.0 to −1.0, with 1.0 indicating that Egos only have sexual partnerships with individuals of their same race, −1.0 that Egos only have sexual partners of a different race, and 0 indicating that sexual partnerships are not influenced by race.
Age Homophily
For scalar variables, AC is equivalent to calculating a Pearson Correlation Coefficient (Newman, 2002), with a positive correlation indicating that Egos tend to have sexual partners who are older and a negative correlation indicting that Egos tend to have sexual partners who are younger.
HIV/STI
Participants were tested for HIV, gonorrhea, and chlamydia prior to their network interview. HIV status was assessed using a rapid oral screening test (OraQuick ADVANCE 1/2; OraSure Technologies, Bethlehem, PA) and confirmed by OraSure testing. Urethral gonorrhea and chlamydia infections were determined via urine polymerase chain reaction (PCR).
Analyses
After data collection, key alter attributes were summarized by ego. Descriptive statistics for ego demographics, sexual partner demographics, and sexual behaviors were calculated. Next, bivariate correlations were calculated between several key network characteristics and three outcomes: ego HIV status; STI status; and the number of unprotected anal intercourse (UAI) acts the ego reported across their last three partners in the prior six months. Analyses for both HIV and STI were restricted to participants who indicated ever being sexually active. Analyses for UAI were restricted to those who reported being sexually active in the prior six months. Hierarchical Linear Modeling (HLM) version 7 (Scientific Software International, Lincolnwood, IL) was then utilized to examine ego and alter characteristics related to unprotected anal and vaginal intercourse. HLM accounts for the clustering of data by ego. Three multivariate models were constructed. Model 1 examined basic ego and partner demographics: ego age (centered at 17); sexual partner age difference in years; ego race (coded into White, Hispanic, Other Race and the reference group Black), sexual partner race (coded with the reference group being Black), and partner gender (dichotomized with reference group male). Model 2 added level-2 ego variables such as: ego drug and alcohol use (dichotomous with any drug or alcohol use in the last 6 months coded as 1); ego’s total number of sexual partners in the past 6 months; and social/sexual multiplexity (the correlation of the ego’s social network and sexual network). Model 3 added level-1 partner variables such as: sexual partner relationship type (dummy-coded into three categories: main partner, friend, with the reference group being non-main partner/non-friend); using drugs with the sex partner (dichotomized), and sexual concurrency with that sexual partner (dichotomized with any sexual concurrency with at least 1 other sexual partner coded as 1).
Of all YMSM who participated, 144 (82.3%) indicated having at least 1 sexual partner in the 6 months prior to the date surveyed. Of these, 367 sex partners in the prior six months were indicated, or on average 2.5 partners per young man who was sexually active in the prior six months. Figure 1 visualizes these sexual relationships over the past six months. As details of sexual behaviors (intercourse type and use of condoms) were only assessed with the sexual partners an ego reported within the past 6 months, and due to missing data, the sample size for HLM analyses was reduced to 130 egos (study participants who reported sexual partners in the past six months) and 338 sexual partners (reported sexual partners of egos over the past six months).
Figure 1.
Visualizing sexual relationships over the prior six months
Node Size = Large (Ego), Small (Sex Partner within the Prior 6 Months). Node Color = Dark Red (HIV+ Egos), Light Grey (HIV-Egos), Blue (Male Sex Partners), Pink (Female Sex Partners), Green (Transgender Sex Partners).
Results
Number of Partners
Of the 175 YMSM who participated, 167 (95.4%) indicated having at least 1 prior sexual partner while 8 (4.6%) indicated not ever having prior sexual partners. Of the men who were sexually active ever, 837 sexual partners were indicated, or on average 4.8 partners per sexual active young man.
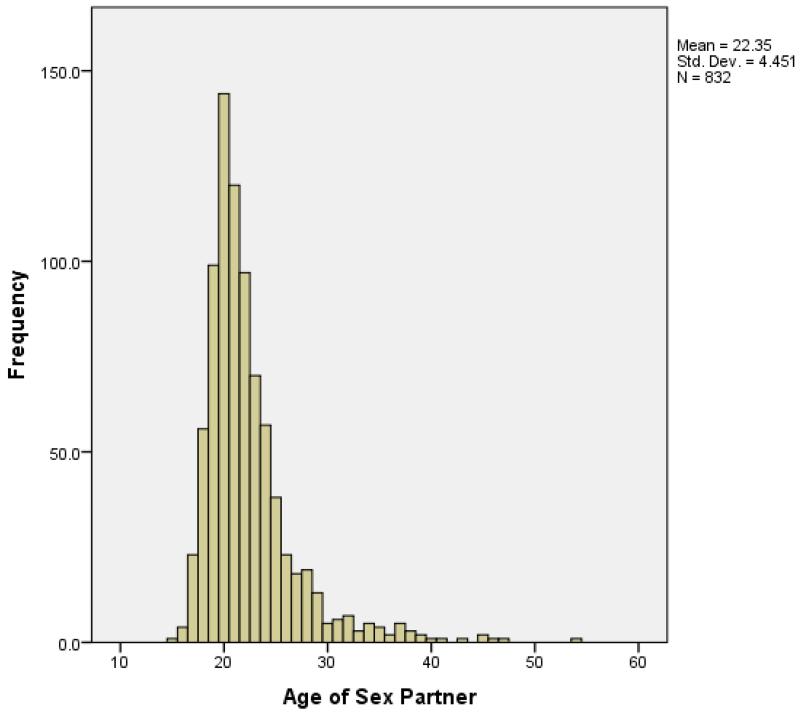
Characteristics of Egos and Partners
Descriptive characteristics of study egos and sexual partner alters are listed in Table 1. On average sexual partners were 22.4 years old, which was 2.3 years older than study egos. Sex partner age difference ranged from 4.3 years younger than egos to 26.8 years older. Most sexual partners were male, with 7.5% of partners indicated to be female and 0.8% indicated to be transgender. Racial demographics of sexual partners were similar to that of the egos, though a significantly higher proportion of sexual partners were white (22.6%) versus egos (13.2%) (χ2 = 7.42, p < 0.01). Most sexual partners were indicated to be gay males (74.3%). However, 12.7% of sexual partners were bisexual males, followed by 4.4% heterosexual females, 3.3% heterosexual men, 2.6% were bisexual women and 0.4% lesbian women. The remaining sexual partners (2.3%) were comprised of transgender individuals and those whose sexual orientation was queer or missing. Sexual partners were evenly split between main partners, friends, and non-main partner/non-friends (χ2 = 5.226, p = 0.07).
Sex Behaviors
Of those who reported a sexual partner within the past 6 months (n = 144), 95.8% reported having oral sex, 9.0% reported having vaginal sex, and 93.1% reported having anal sex. Additionally, the average number of partners they reported was 2.3 oral sex partners, 0.2 vaginal sex partners, and 1.97 anal sex partners in the prior 6 months. Of those who reported having oral sex (n = 137), on average 6.1 oral sex acts occurred in the prior 6 months and 10.9% of egos reported always using a condom during these acts. Of those who reported having vaginal sex (n = 13), on average 5.3 vaginal sex acts occurred in the prior 6 months and 76.9% of egos reported always using a condom during these acts. Of those who reported having anal sex (n = 134), on average 4.90 anal sex acts occurred in the prior 6 months and 44.8% of egos reported always using a condom during these acts.
Concurrency
Of the 175 YMSM, 100 (57.1%) reported ever having concurrent partners and 56 (32%) reported having concurrent partners in the last 6 months. Of the 837 sexual partner alters, 495 (59.1%) were concurrent. The average total number of concurrent partners per ego was 2.82 for the entire sample. Momentary degree was calculated as the number of active sexual partnerships reported by the ego both 7 days and 14 days prior to the interview. When considering the prior 7 days the mean momentary degree was 0.52 for the entire sample, and 1.16 when ignoring isolates (those without a sexual partner). Twelve percent of the non-isolates reported a momentary degree greater than 1. When considering the prior 14 days the mean momentary degree was 0.73 for the entire sample, and 1.28 when ignoring isolates. Of the non-isolates, 16.8% reported a momentary degree greater than 1. See Figure 2 for the momentary degree distribution.
Figure 2.
The 7-day and 14-day Momentary Sexual Partner Degree Distribution for Young Men Who Have Sex with Men
Density
Sexual network density was then examined by summing the number of sexual connections observed between egos and alters, and alters and alters, and diving by the total number of possible pairs given the number of support, sex, and drug connections reported by each ego. Density of sexual networks across egos ranged from 0 to 0.286, with an average Density of 0.048 (SD=0.036).
Multiplexity
In this analysis we were interested in the overlap of an ego’s sex, drugs, and social networks. Our results indicated that for most YMSM (68%), their sexual and social networks were uncorrelated to each other (i.e., QAP correlation non-significant), however 32% of YMSM did show significant overlap, with social ties being significantly more likely to also be sexual ties. Across all egos however, this association was low with a mean correlation of 0.14. However, both sex/drug and drug/social networks displayed greater overlap, with only 39% and 35% of YMSM respectively not showing significant correlation between those networks. Most YMSM (61%) showed significant multiplexity between their sexual and drug networks, with the average sex ties being significantly more likely to also be drug ties (mean QAP correlation = .40). And finally, most YMSM (65%) also showed significant multiplexity between their social and drug networks, with the average social ties being significantly more likely to also be drug ties (mean QAP correlation = 0.66).
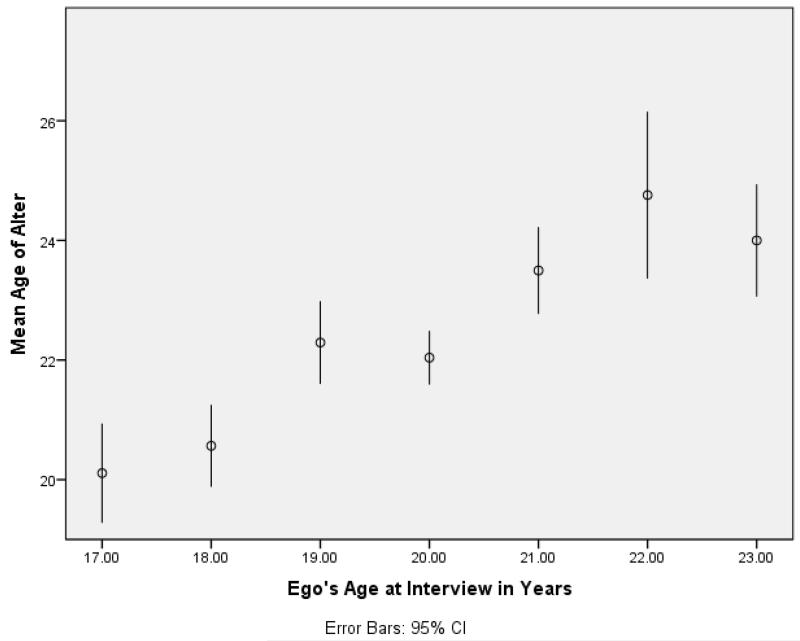
Homophily by Race, Age
Sexual networks tended to show strong racial homophily. A high positive Assortativity Coefficient (AC = 0.58) was estimated for the sample, indicating that most egos report sexual relationships with individuals of the same race. Additionally, the overall sample showed a significant preference for older sexual partners, r(830) = 0.24, p < .001. Figures 3 and 4 display distributions of sexual partner age.
Figure 3.
Sex Partner Age by Age of Ego among Young Men Who Have Sex with Men
Figure 4.
The Distribution of Sex Partner Age among Young Men Who Have Sex with Men
Correlates of HIV, STI, and Unprotected Anal Intercourse
Bivariate correlations were calculated between network characteristics and ego HIV status, STI status, and the number of unprotected anal intercourse acts the ego reported with their last three partners. Results appear in Table 2. The strongest significant correlate of HIV status was partner race, with ever having sex with an African American partner significantly associated with HIV positive status, r(165) = 0.22, p < .01. Partner gender was also a significant correlate, with egos who reported only having sex with a male being more likely to be HIV positive, r(165) = 0.18, p < .05. There were also non-significant trends for HIV positive egos to have multiplex social/sexual partners (p = .07), older partners (p = .08), and multiplex sex/drug partners (p = .12). None of the tested variables significantly correlated with STI status. Additionally, there was a non-significant trend for the number of sexual partners reported by the ego ever (p = .08) and in the past six months (p = .07) to correlate with STI status. And finally, there was a trend for having multiplex sexual and social relationships to correlate with increased STI status (p = .07).
Table 2. Sexual Network Correlates of HIV, STI, and Unprotected Anal Intercourse.
| HIV |
STI |
UAI1 |
||||
|---|---|---|---|---|---|---|
| r |
p |
r |
p |
r |
p |
|
| Sexual Behavior | ||||||
|
| ||||||
| Number of Sex Part. Ever | −0.04 | 0.64 | 0.14 | 0.08 | 0.00 | 0.97 |
| Number of Sex Part. 6 Mos | −0.04 | 0.66 | 0.14 | 0.07 | −0.12 | 0.17 |
| Ever Concurrent Part | −0.02 | 0.79 | 0.05 | 0.52 | −0.02 | 0.86 |
| Sex Partner Characteristics | ||||||
|
| ||||||
| Average Age of Sex Part. | 0.14 | 0.08 | −0.02 | 0.82 | −0.11 | 0.20 |
| Only Sex with Males | 0.18 | 0.02 | −0.07 | 0.41 | 0.10 | 0.28 |
| Ever Sex African American | 0.22 | 0.00 | 0.03 | 0.75 | −0.07 | 0.43 |
| Proportion Main Partners | 0.07 | 0.35 | −0.03 | 0.70 | 0.15 | 0.09 |
| Network Characteristics | ||||||
|
| ||||||
| Race Homophily | 0.16 | 0.35 | −0.02 | 0.83 | −0.10 | 0.28 |
| Sexual Network Density | −0.08 | 0.34 | 0.03 | 0.70 | −0.10 | 0.29 |
| Multiplexity (sex/drug) | 0.13 | 0.13 | 0.09 | 0.31 | 0.02 | 0.85 |
| Multiplexity (sex/social) | 0.15 | 0.07 | 0.15 | 0.08 | 0.28 | 0.00 |
= Analyses restricted to include only sex partners over past 6 months
The only significant correlate of number of UAI acts was sexual/social multiplexity, with high overlap between sexual partners and social partners to be correlated with an increased number of UAI acts, r(140) = 0.275, p < .01. There was also a non-significant trend with having a high proportion of main partners correlating with increased UAI (p = .08).
Predicting Unprotected Intercourse
HLM was utilized to form three multivariate models of unprotected anal and vaginal intercourse (UAVI). As shown in Table 3, the first model examined both ego and sexual partner demographics (ego/partner race, ego/partner age, partner sex). The only significant predictor of UAVI was ego race in which egos whose race/ethnicity was Other (i.e., not White, Hispanic, or Black) were significantly more likely (odds ratio = 3.82) than Black egos to have had UAVI.
Table 3. A Multilevel Model of Unprotected Anal Vaginal Intercourse.
| Model 1 |
Model 2 |
Model 3 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SIG | LOW | UPP | OR | SIG | LO W |
UPP | OR | SIG | LOW | UPP | |
|
|
|
|
|
|
|
|
|
|
||||
| Intercept (Level 2) | 0.39 | * | 0.17 | 0.92 | 0.15 | *** | 0.05 | 0.44 | 0.06 | *** | 0.02 | 0.23 |
| Ego Age | 1.06 | 0.86 | 1.30 | 1.01 | 0.82 | 0.24 | 0.99 | 0.78 | 1.26 | |||
| Ego Race (ref=Black) | ||||||||||||
| Latino | 1.86 | 0.67 | 5.19 | 1.88 | 0.67 | 5.32 | 2.18 | 0.76 | 6.20 | |||
| White | 1.81 | 0.54 | 6.10 | 1.84 | 0.54 | 6.32 | 1.45 | 0.36 | 5.94 | |||
| Other | 3.82 | ** | 1.65 | 8.90 | 4.63 | *** | 1.82 | 11.78 | 4.15 | ** | 1.55 | 11.08 |
| Ego Alcohol/Drug Use | 3.55 | ** | 1.42 | 8.91 | 3.30 | ** | 1.27 | 8.60 | ||||
| Num Part Past 6m | 0.91 | 0.77 | 1.08 | 0.95 | 0.80 | 1.14 | ||||||
| Multiplex SexSocial | 7.75 | * | 1.10 | 54.61 | 6.12 | 0.64 | 58.13 | |||||
| Slope (Level 1) | ||||||||||||
| Partner Age Difference Partner Race (ref=Black) |
1.01 | 0.96 | 1.07 | 1.02 | 0.97 | 1.07 | 1.05 | 0.99 | 1.10 | |||
| Latino | 0.57 | 0.25 | 1.32 | 0.48 | 0.20 | 1.13 | 0.53 | 0.21 | 1.36 | |||
| White | 0.69 | 0.29 | 1.61 | 0.62 | 0.25 | 1.56 | 0.71 | 0.25 | 1.97 | |||
| Other | 1.32 | 0.58 | 3.03 | 1.23 | 0.54 | 2.82 | 1.13 | 0.51 | 2.48 | |||
| Partner is a Female | 0.31 | 0.09 | 1.13 | 0.27 | 0.06 | 1.35 | 0.29 | 0.06 | 1.34 | |||
| Partner Type (ref= Not Main/Friend) |
||||||||||||
| Main Partner | 2.65 | ** | 1.40 | 5.01 | ||||||||
| Friend | 0.53 | * | 0.28 | 1.00 | ||||||||
| Used Drugs with Partner | 1.87 | * | 1.02 | 3.43 | ||||||||
| Concurrent with Partner | 1.22 | 0.72 | 2.05 | |||||||||
= p < 0.001
= p < 0.01
= p < 0.05
The second model added possible ego-level risk factors (ego drug and alcohol use, number of sex partners in the past 6 months, and social/sexual multiplexity). An ego who used alcohol and drugs was significantly more likely (odds ratio = 3.55) to have had UAVI. Additionally, the more an ego’s sexual and social networks overlapped (sexual/social multiplexity) the greater the odds (odds ratio = 7.75) of having UAVI. Ego race also retained significance with egos of Other race were significantly more likely (odds ratio = 4.63) than Black egos to have had UAVI.
The third model added possible partner-level risk factors (sexual partner relationship type, partner drug use, and sexual concurrency). An ego with a sexual partner who is their main partner was significantly more likely (odds ratio = 2.65) to have had UAVI while an ego with a sexual partner who is their friend was significantly less likely (odds ratio 0.53) to have had UAVI versus partners who were neither main partners nor friends. Additionally, an ego who indicated using drugs with their sexual partner was significantly more likely (odds ratio = 1.87) to have UAVI. Both Other ego race and ego alcohol and drug use retained significance with both being more likely (odds ratios =4.15; 3.30) to have UAVI. However, sexual/social multiplexity was no longer was a significant predictor of UAVI.
Discussion
This study presents novel descriptive data about the sexual networks of young men who have sex with men. Additionally, individual, partner, and network characteristics of these YMSM were examined as potential drivers of HIV, STI, and unprotected intercourse. Results indicated several partner- and network-level factors associated with HIV and associated outcomes.
The descriptive data of sexual networks of YMSM results in several key findings. First, this study supports that approximately 1 in 3 YMSM have concurrent sexual behavior in the prior six months. These rates of sexual concurrency appear higher than among heterosexuals, as a study of heterosexual men found only 11% indicated sexual concurrency in the prior year (Adimora, Schoenbach, & Doherty, 2007). However, YMSM rates of concurrency are comparable to the few measurements of concurrency in MSM (Bohl, Raymond, Arnold, & McFarland, 2009; Rosenberg, Khosropour, & Sullivan, 2012). Furthermore, a significant preference for racial homophily in sexual partners was shown, but this was no greater than has been observed in non-YMSM populations (McPherson et al., 2001). A preference for older partners was also shown, which supports prior work which suggests age differentials in sexual partnerships in MSM are common (Bocour, Renaud, Wong, Udeagu, & Shepard, 2011).
This work highlights the need for more knowledge about the sexual networks of high-risk populations; but it also highlights the importance of studying networks other than only sexual networks in order to understand HIV and associated risk factors. This study found that although most egos did not indicate significant overlap in their sexual partners and social relationships (multiplex sexual/social), those who did were more likely to have unprotected intercourse and had a trend towards being more likely to have an STI. This may support preliminary evidence that the selection of a sexual partner who is not also a social network member may be protective against STI infection (Ellen et al., 2006). By examining social and drug networks, as well as sexual networks, researchers can better understand the possible protective and risk factor dynamics associated with HIV and associated outcomes (Amirkhanian, 2014). For some individuals, social and drug networks may influence sex networks and sex behavior. For example, analyses indicated that high overlap between social and sexual networks was significantly correlated with unprotected anal intercourse. Additionally, statistical trends were found between multiplexity and testing positive for HIV (p = 0.07) or an STI (p = 0.08). Further work is necessary to examine these linkages, but retaining former sex partners in drug or social circles may possibly increase the likelihood for sexual re-engagement, or create new pathways for disease transmission (e.g., IDU), or social and drug relationships may create additional barriers for condom use.
In addition to multiplexity, several important sexual partner characteristics were identified. For HIV, the only significant correlates were having sexual partners who were African American and having sexual partners who were all male. This demonstrates the importance of partner-characteristics and population-related factors in driving HIV transmission and the need to expand research designs beyond the focus on individual sexual behavior (e.g., number of sex partners). As authors have shown in another article (B. Mustanski, Birkett, Kuhns, Latkin, & Muth, 2014), and as demonstrated in review of the literature on racial disparities (Millett, Flores, Peterson, & Bakeman, 2007), these partner- and population-related factors are also likely a driver of the strong HIV disparities in black YMSM.
Another important partner-level variable was relationship-type, which was significantly associated with UAI, even when controlling for all other factors. YMSM were significantly more likely to have UAI with main partners, and significantly less likely to have UAI with friends. Similar to social/sexual multiplexity, dual relationships with sexual partners likely changes relationship dynamics. Several papers have also shown partnership type to be an important predictor of unprotected sex (B. Mustanski et al., 2011; Newcomb, Ryan, Garofalo, et al., 2014), with YMSM being less likely to use condoms during anal intercourse when they believe the relationship to be serious and committed. These risk behaviors may be driven in part by the perceived sense of safety with main partners that makes condoms seem unnecessary.
There was less evidence of individual sexual behaviors being associated with HIV or STIs, although there was a trend of more sexual partners increasing STI. There were also no significant relationships between our measure of density and any of the examined outcomes. However, measures of true sexual network density are unable to be obtained without full (i.e., sociometric) network data. As this study only utilizes egocentric data, our estimates are limited to density estimates based on the observations of only one ego versus actual density estimates from the perspective of the full populations.
Several important strengths exist for this study. Most importantly, the study reported rich descriptive information for a high risk population and their networks. A diverse community-based sample of YMSM was analyzed. However, this study also has several weaknesses. First, all data were self-report. Therefore, our results are impacted by inaccurate reporting by the ego and potentially missing alter data. Another major limitation was the collection of egocentric network data. While egocentric network data are easier to collect (e.g. less resource intensive), they lack the ability to give the true perspective of the entire network. For example, it is unknown how many sex partners an ego’s sex partner had. In an additional study of these data, a macronetwork dataset will be created by utilizing and consolidating matched alter data. This macronetwork data may allow us to develop more accurate estimates of variables such as density.
Finally, this study provides an important reminder for HIV interventions: disease transmission is a complex process. By examining individual, partner, and network variables, as well as social, drug, and sex networks, our results suggest that HIV, STI, and UAI may be driven by complex and overlapping mechanisms. While UAI is largely a function of relationship characteristics, our preliminary analyses suggest HIV is driven by partner demographics. More data are necessary to further tease apart the relationships between HIV and sexual behavior in this population, and inform intervention. Our preliminary data suggest though that interventions which target only UAI behavior, without a broader understanding of HIV in population dynamics, will not effectively target the mechanisms driving and sustaining infection in YMSM.
REFERENCES
- Adimora AA, Schoenbach VJ, Doherty IA. Concurrent sexual partnerships among men in the United States. American Journal of Public Health. 2007;97(12):2230–2237. doi: 10.2105/AJPH.2006.099069. doi: Doi 10.2105/Ajph.2006.099069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirkhanian YA. Social networks, sexual networks and HIV risk in men who have sex with men. Current HIV/AIDS Reports. 2014;11(1):81–92. doi: 10.1007/s11904-013-0194-4. doi: 10.1007/s11904-013-0194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirkhanian YA, Kelly JA, Kirsanova AV, DiFranceisco W, Khoursine RA, Semenov AV, Rozmanova VN. HIV risk behaviour patterns, predictors, and sexually transmitted disease prevalence in the social networks of young men who have sex with men in St Petersburg, Russia. International Journal of STD & AIDS. 2006;17(1):50–56. doi: 10.1258/095646206775220504. doi: 10.1258/095646206775220504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men’s Survey, Los Angeles, 1999-2000. AIDS Education and Prevention. 2003;15(1 Suppl A):39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- Bocour A, Renaud TC, Wong MR, Udeagu CC, Shepard CW. Differences in risk behaviors and partnership patterns between younger and older men who have sex with men in New York City. Journal of Acquired Immune Deficiency Syndromes. 2011;58(4):417–423. doi: 10.1097/QAI.0b013e318230e6d9. doi: 10.1097/QAI.0b013e318230e6d9. [DOI] [PubMed] [Google Scholar]
- Bohl DD, Raymond HF, Arnold M, McFarland W. Concurrent sexual partnerships and racial disparities in HIV infection among men who have sex with men. Sexually Transmitted Infections. 2009;85(5):367–369. doi: 10.1136/sti.2009.036723. doi: 10.1136/sti.2009.036723. [DOI] [PubMed] [Google Scholar]
- Borgatti Stephen P., Everett Martin G., Freeman LC. Ucinet for Windows: Software for Social Network Analysis. Analytic Technologies; Harvard, MA: 2002. [Google Scholar]
- CDC . HIV Surveillance Report, 2011. Vol. 23. Center for Disease Control and Prevention; Atlanta, GA: 2013. [Google Scholar]
- Clerkin EM, Newcomb ME, Mustanski B. Unpacking the racial disparity in HIV rates: the effect of race on risky sexual behavior among Black young men who have sex with men (YMSM) Journal of Behavioral Medicine. 2011;34(4):237–243. doi: 10.1007/s10865-010-9306-4. doi: 10.1007/s10865-010-9306-4. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Toward a person x situation model of sexual risk-taking behaviors: illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology. 2010;98(2):319–341. doi: 10.1037/a0017785. doi: 10.1037/a0017785. [DOI] [PubMed] [Google Scholar]
- Drumright LN, Frost SD. Rapid social network assessment for predicting HIV and STI risk among men attending bars and clubs in San Diego, California. Sexually Transmitted Infections. 2010;86(Suppl 3):iii17–23. doi: 10.1136/sti.2010.045914. doi: 10.1136/sti.2010.045914. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Chang M. A social network profile and HIV risk among men on methadone: do social networks matter? Journal of Urban Health. 2006;83(4):602–613. doi: 10.1007/s11524-006-9075-0. doi: 10.1007/s11524-006-9075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellen JM, Gaydos C, Chung SE, Willard N, Lloyd LV, Rietmeijer CA. Sex partner selection, social networks, and repeat sexually transmitted infections in young men: a preliminary report. Sexually Transmitted Diseases. 2006;33(1):18–21. doi: 10.1097/01.olq.0000187213.07551.a6. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Neaigus A, Jose B, Curtis R, Goldstein M, Ildefonso G, Des Jarlais DC. Sociometric risk networks and risk for HIV infection. American Journal of Public Health. 1997;87(8):1289–1296. doi: 10.2105/ajph.87.8.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene GJ, Andrews R, Kuper L, Mustanski B. Intimacy, monogamy, and condom problems drive unprotected sex among young men in serious relationships with other men: a mixed methods dyadic study. Archives of Sexual Behavior. 2014;43(1):73–87. doi: 10.1007/s10508-013-0210-1. doi: 10.1007/s10508-013-0210-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper GW, Riplinger AJ. HIV prevention interventions for adolescents and young adults: what about the needs of gay and bisexual males? AIDS and Behavior. 2013;17(3):1082–1095. doi: 10.1007/s10461-012-0178-1. doi: 10.1007/s10461-012-0178-1. [DOI] [PubMed] [Google Scholar]
- Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge B, Sheeran P, Fishbein M. A network-individual-resource model for HIV prevention. AIDS and Behavior. 2010;14(Suppl 2):204–221. doi: 10.1007/s10461-010-9803-z. doi: 10.1007/s10461-010-9803-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB. Homophily, Selection, and Socialization in Adolescent Friendships. American Journal of Sociology. 1978;84(2):427–436. doi: Doi 10.1086/226792. [Google Scholar]
- Kelly JA, Amirkhanian YA, Seal DW, Galletly CM, Difranceisco W, Glasman LR, Rosado N. Levels and Predictors of Sexual HIV Risk in Social Networks of Men who Have Sex with Men in the Midwest. AIDS Education and Prevention. 2010;22(6):483–495. doi: 10.1521/aeap.2010.22.6.483. doi: 10.1521/aeap.2010.22.6.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretzschmar M, Carael M. Is concurrency driving HIV transmission in sub-Saharan African sexual networks? The significance of sexual partnership typology. AIDS and Behavior. 2012;16(7):1746–1752. doi: 10.1007/s10461-012-0254-6. doi: 10.1007/s10461-012-0254-6. [DOI] [PubMed] [Google Scholar]
- Kretzschmar M, Morris M. Measures of concurrency in networks and the spread of infectious disease. Mathematical Biosciences. 1996;133(2):165–195. doi: 10.1016/0025-5564(95)00093-3. [DOI] [PubMed] [Google Scholar]
- Kuhns LM, Birkett M, Muth SQ, Latkin CA, Ortiz-Estes I, Garofalo R, Mustanski B. Methods for Collection of Participant-aided Sociograms for the Study of Social, Sexual and Substance-using Networks among Young Men Who Have Sex with Men. Connections. doi: 10.17266/35.1.1. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Social Science and Medicine. 2003;56(3):465–476. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- Latkin C, Yang C, Tobin K, Roebuck G, Spikes P, Patterson J. Social network predictors of disclosure of MSM behavior and HIV-positive serostatus among African American MSM in Baltimore, Maryland. AIDS and Behavior. 2012;16(3):535–542. doi: 10.1007/s10461-011-0014-z. doi: 10.1007/s10461-011-0014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, Young Men’s Survey Study, Group Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. Journal of Acquired Immune Deficiency Syndromes. 2005;38(5):603–614. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- Marsden PV. Egocentric and sociocentric measures of network centrality. Social Networks. 2002;24(4):407–422. doi: Pii S0378-8733(02)00016-3 Doi 10.1016/S0378-8733(02)00016-3. [Google Scholar]
- McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: Homophily in social networks. Annual Review of Sociology. 2001;27:415–444. doi: DOI 10.1146/annurev.soc.27.1.415. [Google Scholar]
- Meyer IH, Wilson PA. Sampling Lesbian, Gay, and Bisexual Populations. Journal of Counseling Psychology. 2009;56(1):23–31. doi: 10.1037/a0012844. doi: Doi 10.1037/A0014587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. 1997;11(5):641–648. doi: 10.1097/00002030-199705000-00012. [DOI] [PubMed] [Google Scholar]
- Morris M, Kurth AE, Hamilton DT, Moody J, Wakefield S. Concurrent partnerships and HIV prevalence disparities by race: linking science and public health practice. American Journal of Public Health. 2009;99(6):1023–1031. doi: 10.2105/AJPH.2008.147835. doi: 10.2105/AJPH.2008.147835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris M, Podhisita C, Wawer MJ, Handcock MS. Bridge populations in the spread of HIV/AIDS in Thailand. AIDS. 1996;10(11):1265–1271. doi: 10.1097/00002030-199609000-00013. [DOI] [PubMed] [Google Scholar]
- Mustanski B. The influence of state and trait affect on HIV risk behaviors: a daily diary study of MSM. Health Psychology. 2007;26(5):618–626. doi: 10.1037/0278-6133.26.5.618. doi: 10.1037/0278-6133.26.5.618. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The Role of Geographic and Network Factors in Racial Disparities in HIV Among Young Men Who have Sex with Men: An Egocentric Network Study. AIDS and Behavior. 2014 doi: 10.1007/s10461-014-0955-0. doi: 10.1007/s10461-014-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychology. 2011;30(5):597–605. doi: 10.1037/a0023858. doi: 10.1037/a0023858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Ryan DT, Garofalo R. Associations of sexually transmitted infections with condom problems among young men who have sex with men. Sexually Transmitted Diseases. 2014;41(7):427–432. doi: 10.1097/OLQ.0000000000000150. doi: 10.1097/OLQ.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. Journal of Sex Research. 2011;48(2-3):218–253. doi: 10.1080/00224499.2011.558645. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neaigus A, Friedman SR, Curtis R, Jarlais DCD, Furst RT, Jose B, Wright JW. The Relevance of Drug Injectors Social and Risk Networks for Understanding and Preventing Hiv-Infection. Social Science and Medicine. 1994;38(1):67–78. doi: 10.1016/0277-9536(94)90301-8. doi: Doi 10.1016/0277-9536(94)90301-8. [DOI] [PubMed] [Google Scholar]
- Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Archives of Sexual Behavior. 2014;43(1):61–72. doi: 10.1007/s10508-013-0207-9. doi: 10.1007/s10508-013-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Ryan DT, Greene GJ, Garofalo R, Mustanski B. Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug and Alcohol Dependence. 2014;141:65–71. doi: 10.1016/j.drugalcdep.2014.05.005. doi: DOI 10.1016/j.drugalcdep.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman ME. Assortative mixing in networks. Physical Review Letters. 2002;89(20):208701. doi: 10.1103/PhysRevLett.89.208701. doi: Artn 208701 Doi 10.1103/Physrevlett.89.208701. [DOI] [PubMed] [Google Scholar]
- Pantalone DW, Huh D, Nelson KM, Pearson CR, Simoni JM. Prospective predictors of unprotected anal intercourse among HIV-seropositive men who have sex with men initiating antiretroviral therapy. AIDS and Behavior. 2014;18(1):78–87. doi: 10.1007/s10461-013-0477-1. doi: 10.1007/s10461-013-0477-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg ES, Khosropour CM, Sullivan PS. High prevalence of sexual concurrency and concurrent unprotected anal intercourse across racial/ethnic groups among a national, Web-based study of men who have sex with men in the United States. Sexually Transmitted Diseases. 2012;39(10):741–746. doi: 10.1097/OLQ.0b013e31825ec09b. doi: 10.1097/OLQ.0b013e31825ec09b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott John, Carrington Peter J. The SAGE handbook of social network analysis. SAGE; London; Thousand Oaks, Calif.: 2011. [Google Scholar]
- Shah NS, Iveniuk J, Muth SQ, Michaels S, Jose JA, Laumann EO, Schneider JA. Structural bridging network position is associated with HIV status in a younger Black men who have sex with men epidemic. AIDS and Behavior. 2014;18(2):335–345. doi: 10.1007/s10461-013-0677-8. doi: 10.1007/s10461-013-0677-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirley MDF, Rushton SP. The impacts of network topology on disease spread. Ecological Complexity. 2005;2(3):287–299. doi: DOI 10.1016/j.ecocom.2005.04.005. [Google Scholar]
- Smith AM, Grierson J, Wain D, Pitts M, Pattison P. Associations between the sexual behaviour of men who have sex with men and the structure and composition of their social networks. Sexually Transmitted Infections. 2004;80(6):455–458. doi: 10.1136/sti.2004.010355. doi: 10.1136/sti.2004.010355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tieu HV, Nandi V, Frye V, Stewart K, Oquendo H, Bush B, Team, Nyc M. M. Study Concurrent partnerships and HIV risk among men who have sex with men in New York City. Sexually Transmitted Diseases. 2014;41(3):200–208. doi: 10.1097/OLQ.0000000000000090. doi: 10.1097/OLQ.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster RD, Darrow WW, Paul JP, Roark RA, Woods WJ, Stempel RR. HIV infection and associated risks among young men who have sex with men in a Florida resort community. Journal of Acquired Immune Deficiency Syndromes. 2003;33(2):223–231. doi: 10.1097/00126334-200306010-00018. [DOI] [PubMed] [Google Scholar]
- Weeks Margaret R., Clair Scott, Borgatti Stephen P., Radda Kim, Schensul Jean J. Social Networks of Drug Users in High-Risk Sites: Finding the Connections. AIDS and Behavior. 2002;6(2):193–206. doi: 10.1023/a:1015457400897. [Google Scholar]