Abstract
Background
This pilot study conducted a preliminary examination of whether Cognitive Bias Modification (CBM), a computerized task to retrain cognitive-approach biases towards smoking stimuli, (1) changed approach bias for cigarettes, and (2) improved smoking cessation outcomes in adolescent smokers.
Methods
Sixty adolescent smokers received four weeks of Cognitive Behavioral Therapy (CBT) for smoking cessation, with CBM (90% avoidance/10% approach for smoking stimuli and 10% avoidance/90% approach for neutral stimuli) or sham (50% avoidance/50% approach for smoking and neutral stimuli) training in the Netherlands (n = 42) and the United States (n = 18).
Results
While we did not observe changes in action tendencies related to CBM, adolescents with higher smoking approach biases at baseline had greater decreases in approach biases at follow up, compared to adolescents with smoking avoidance biases, regardless of treatment condition (p = 0.01). Intent-to-treat (ITT) analyses showed that CBM, when compared with sham trended toward higher end-of-treatment, biochemically-confirmed, seven-day point prevalence abstinence, (17.2% vs. 3.2%, p = 0.071). ITT analysis also showed that regardless of treatment condition, cotinine level (p = 0.045) and average number of cigarette smoked (p ≤ 0.001) significantly decreased over the course of treatment.
Conclusions
The findings from this pilot study suggests that re-training approach biases toward cigarettes shows promise for smoking cessation among adolescent smokers. Future research should utilize larger samples and increased distinction between CBM and sham conditions, and examine mechanisms underlying the CBM approach.
Keywords: attentional bias, Approach-Avoidance Task, Cognitive Bias Modification, smoking, intervention, adolescents
INTRODUCTION
Most tobacco use is initiated during adolescence (1). Existing evidence suggests that 11% of high school students in the Netherlands (2) and 9% of 12th grade students in the United States of America (USA) are daily smokers (3). High school students who smoke daily often want to quit: 61% have made a quit attempt, but a majority of them are unsuccessful (4), and there are few empirically validated smoking interventions for adolescents (5, 6).
Dual process theories (7, 8) suggest that addiction may be related to an imbalance between two qualitatively different sets of processes that influence behavior: fast associative impulsive processes, which are responsible for the automatic appraisal of stimuli and immediate behavioral action tendencies and slower reflective processes, which consciously regulate emotions and cognitive processes related to the outcome of the behaviors (9). In addicted individuals, the combination of strong impulsive and weak reflective processes results in susceptibility to cues triggering the addictive behavior, leading to difficulties in inhibiting the tendency to engage in the addictive behavior. Several studies have demonstrated stronger effects of implicit addiction-related processes in adolescents with relatively weak ability to moderate impulses for a variety of addictive behaviors, including smoking (10) and alcohol use (10-13). Thus, an adolescent smoker may want to quit smoking but may not be able to because direct or indirect exposure to cigarette-associated stimuli may automatically activate implicit action tendencies to approach smoking.
Implicit processes may be stronger among adolescents than they are in adults, because impulse control processes are not fully developed, while more emotional and reward-seeking processes are most active in adolescence (8, 14). Indeed, the association between implicit drinking associations and binge drinking was stronger in adolescents than in adults (15). Furthermore, in adolescents, positive implicit attitudes toward smoking predict initiation (16) and frequency of smoking behaviors (10), whereas negative implicit attitudes predict future smoking cessation. Adult smokers also have stronger implicit processes toward smoking-related stimuli than do non-smokers (17-21). These implicit processes toward smoking are associated with nicotine craving and urge to smoke (17, 22, 23), nicotine dependence (23), and withdrawal symptoms (24). (25). Given the above evidence, re-training implicit approach tendencies may have important prevention and cessation implications for adolescent smoking behaviors.
Cognitive Bias Modification (CBM), a modification of the alcohol Approach-Avoidance Task (AAT; 26), presents smoking-specific and neutral images on a computer screen and requires participants to either push or pull the joystick in response to the format of the images (rotated right/left) rather than the content of the image. For example, pushing the joystick results in the image to zoom out, mimicking avoidance tendencies, whereas pulling the joystick results in the image to zoom in, mimicking approach tendencies (27). CBM has been used to modify automatic action tendencies toward alcohol-related stimuli (28-30). Among hazardous young adult drinkers, CBM produced stronger action tendencies related to avoidance of alcohol (30). Furthermore, among a clinical sample of alcohol dependent adults (N = 214), CBM in conjunction with Cognitive Behavioral Therapy (CBT) led to 13% less relapse at one-year follow up compared to the CBT only group (29). The latter finding was replicated in a larger clinical sample of adult alcohol-dependent inpatients (N = 509) (28). At one-year follow-up, the relapse rates in the training group compared to the control group showed a 10% reduction in relapse rates. This effect was moderated by a change in the approach-tendencies, with individuals with stronger alcohol bias showing greater treatment effect. While CBM shows promise in alcohol treatment, its effect on other substances remains to be established (for a review, see 31). A recent pilot study provided CBM via online methods to 257 adult smokers and found that the CBM relative to the control condition yielded reductions in cigarette use, cigarette dependence, and compulsive drive to smoke cigarettes (32).
The main aims of this pilot study were to assess whether CBM can re-train approach bias toward smoking and to determine if CBM, when provided in addition to Cognitive Behavioral Therapy (CBT), increases smoking cessation rates among adolescent smokers. Improving interventions for adolescent smokers is crucial given that currently existing psychosocial interventions, such as CBT alone have not been shown to be particularly effective (33). Importantly, CBT and CBM target different processes which may be particularly useful; CBM targets automatic processes and CBT targets purposeful processes that involve paying attention to a specific cue and processing the cue to either discard irrelevant information or store and retrieve information related to the cues (34). We hypothesized that adolescents who received CBT plus CBM would (1) have decreases in their approach bias to smoking-related stimuli and (2) achieve greater smoking cessation rates at end of treatment (EOT) than adolescents who received CBT in addition to a sham training (control condition). Our secondary goals were to explore mechanism of change and changes in smoking behaviors at EOT. CBM has shown to be more effective among those who have an approach bias to substance-related stimuli prior to treatment (28), so we assessed whether CBM would have a differential effect on adolescents with a smoking approach bias than a smoking avoidance at baseline. We hypothesized that adolescents with an approach bias toward smoking stimuli would show greater decreases in approach bias toward smoking-related stimuli and would more likely to be abstinent than those with an avoidance bias. We also explored other smoking outcomes: (1) seven-day point prevalence (PP) abstinence at three-month follow-up, (2) number of days abstinent during treatment, (3) changes in self-reported number of cigarettes smoked seven days prior to baseline and seven days prior to EOT, and (4) changes in cotinine levels between baseline and EOT.
METHODS
Procedures
Participants were recruited from preparatory middle-level applied education (VMBO), middle-level applied education (MBO), and vocational training high schools in the NL (Amsterdam and Haarlem) and public high schools in the USA (Connecticut) to participate in this pilot study. The inclusion criteria were (1) ages 14-18, (2) self-reported daily smoking in the past 6 months, and (3) willing to participate in a smoking cessation program. The study procedures were approved by the Department of Developmental Psychology, University of Amsterdam, the Institutional Review Board at Yale University School of Medicine and the participating schools. Information sheets detailing the study were mailed to parents two weeks before recruitment, and parents of adolescents 17 years old and younger were informed to contact the school or research staff if they did not want their child to participate. Interested adolescents signed up at recruitment tables during lunch periods. Assent was obtained from adolescents 14-17 years old and consent was obtained from 18 years old or older.
Baseline Assessment
Study participants provided demographic information and completed a variety of measures. Tobacco use was assessed using 7-day Time Line Follow Back (TLFB; 35) and nicotine dependence was assessed with the modified Fagerström Tolerance Questionnaire (mFTQ; 36).
Participants completed the computerized Smoking-Approach/Avoidance Task (S-AAT), which measured automatic approach tendencies toward cigarette smoking. The images used in the S-AAT was developed and tested in the USA and are described in detail in Larsen, et al. (37). Participants viewed 20 smoking-related images (e.g., cigarettes, cigarette packs, adolescents smoking) and 20 neutral images (e.g., pencil, lipstick) that were rotated 3° left or right. Participants were instructed to push or pull the joystick in response to the rotation of the picture and not the image content. Pushing or pulling the joystick caused the image to zoom out (decrease in size) or zoom in (increase in size), thereby mimicking avoidance and approach actions, respectively (26). Each image was shown equal number of times rotated to the left and rotated to the right, resulting in 50% push and 50% pull for a total of 300 trials. The picture content and push-pull assignment was counterbalanced: half of the participants were instructed to pull if the picture was tilted right and half to pull if it was tilted left. S-AAT was preceded by 15 practice trials. A red cross would appear if an error was made and the image appeared again to allow for a correct response.
Treatment Conditions
Cognitive Behavioral Therapy (CBT)
All participants received weekly CBT for smoking cessation. We used a manual-guided protocol to deliver CBT for smoking cessation (38-40). The manual was translated to Dutch for use in the Netherlands. All therapists had at least a master's level education and all had extensive training and experience in working with adolescents and were supervised by licensed clinical psychologists. The therapists and supervisors in the Netherlands were trained on the CBT protocol by a licensed clinical psychologist in the USA with experience in providing CBT for smoking cessation to adolescents. The supervisors on both sites discussed all ongoing cases at least on a monthly basis to ensure consistency across sites.
Participants received a “preparation to quit” session about one week prior to quitting and a “pre-quit” session one day prior to quitting in which therapists used motivational and cognitive behavioral strategies to motivate abstinence, emphasize benefits of quitting and risks of continued use of tobacco, and teach adolescents to gain social support and practical quit tips. The four weekly CBT sessions following the quit day focused on these key skills: (1) self-monitoring to understand patterns of tobacco use and to identify high risk situations, (2) coping with cravings and urges to smoke, (3) becoming assertive and developing effective tobacco-refusal skills, (4) improving problem-solving skills to deal with high risk situations for smoking, and (5) coping with lapses.
CBM and Sham-training
The CBM was an adaptation of the S-AAT (37) and was designed to re-train approach bias toward smoking stimuli by inducing an avoidance bias. Participants in the CBM condition received 90% of the smoking-related images in the push format and 10% in the pull format and neutral images in 10% push and 90% pull format (30). The CBM had 40 images (20 smoking and 20 neutral images) and each image was shown about 6.5 times, with 90% of the smoking in the push and 10% in the pull format, results in a total of 260 trials. Each CBM session was preceded with 15 practice trials, followed by 20 images (10 smoking and 10 neutral stimuli), with 50% of smoking-related and neutral images in the push format and 50% of the neutral images in the pull format, for a total of 40 trials (same as the S-AAT). Participants in the CBM were exposed to a total of 300 trials in each session.
Participants in the sham-training also received 15 practice trials followed by a total 300 trials of 50% of smoking-related and neutral images in the push format and 50% of the neutral images in the pull format (same as the S-AAT).
Following the “pre-quit” CBT session, participants received either the CBM or the sham-training following each weekly session of CBT. All therapists were blinded to the CBM and sham condition. Due to a computer error discovered at the end of the trial, the CBM condition in the USA received the sham-training instead of CBM at the final session, so the Dutch CBM condition received five sessions in total and the American CBM received four sessions.
Outcome Measures
Changes in approach bias were assessed with the S-AAT obtained at baseline and at three-month follow-up. The primary smoking cessation outcome was determined by seven-day point prevalence (PP) abstinence (defined as self-reports of not smoking during the seven days prior to assessment, and biochemically verified using (i.e., cotinine levels of ≤ 50 ng/ml; 41; Graham Massey Analytical Labs, Shelton, CT and ATAL Medisch Diagnostisch Centrum, Amsterdam, NL) at end-of-treatment. Secondary outcome were (1) seven-day PP abstinence outcomes at three-month follow-up, (2) number of days abstinent during treatment, (3) changes in self-reported number of cigarettes smoked seven days prior to baseline and seven days prior to EOT, and (4) changes in cotinine levels between baseline and EOT.
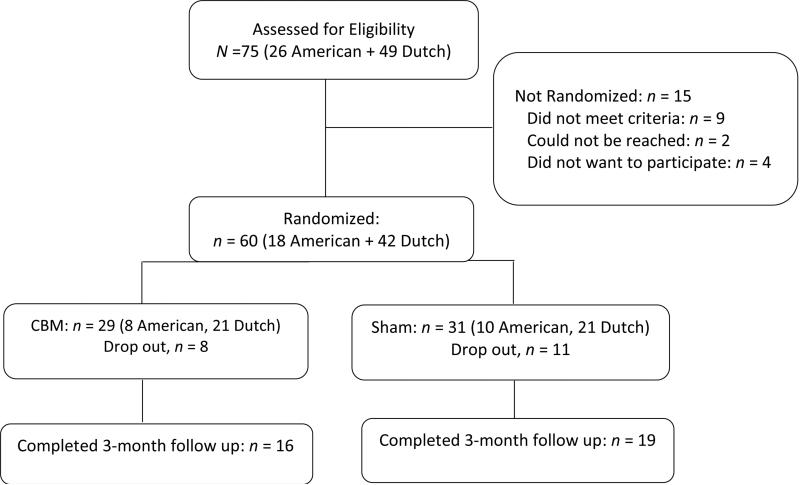
Participants
Of the 75 adolescents presented to participate in the study, 60 (80%) were randomized to receive weekly CBT with either weekly CBM (n = 29) or with sham training (n = 31). (See Figure 1 for CONSORT diagram). Of the randomized sample, 19 dropped out during treatment and this rate did not differ by treatment condition (CBM vs. sham: Χ2 [1, N = 60] = 0.43, p = 0.51) and site (United States vs. Netherlands: Χ2 [1, N = 60] = 1.06, p = 0.30). The three-month follow-up completion rate was 60%.
Figure 1.
CONSORT diagram
Data Analysis
See Supplemental Materials for preparation of the AAT data. The bias scores were computed by subtracting mean approach RT from mean avoidance RT for smoking and neutral stimuli separately, resulting in one bias score for each of the two image categories. Positive scores indicate an approach tendency (n = 21) and negatives scores indicate an avoidance tendency (n = 37).
The two primary outcome measures were: (1) changes in action tendencies (S-AAT) from baseline and three-month follow-up, using the randomized sample and (2) seven-day self-reported PP abstinence at end-of-treatment, using the Intention-To-Treat (ITT) sample. Participants who dropped out or missed end-of-treatment and/or three-month follow up appointments were considered to be smoking.
We used chi-square and t-tests to evaluate the baseline differences in treatment condition and site. We used repeated-measures analysis of variance (ANOVA) with smoking bias and neutral bias scores at baseline and three-month follow-up as within-subject factors, condition (training, sham), site (USA, NL) and baseline smoking approach bias status (approach vs. avoidant) as between-subject factors, and age as a covariate (Table 2). The treatment effect on changes in approach tendencies were assessed by the interactions between bias scores (smoking and neutral bias at baseline and three-month follow up) and treatment condition.
Table 2.
Repeated-measures ANOVA of smoking and neutral approach tendencies/biases at baseline and three-month follow up as a function of treatment condition (treatment vs. sham), site (USA vs. NL), and baseline smoking bias (approach vs. avoidance)
| F | p | η 2 | |
|---|---|---|---|
| Between Subject Factors | |||
| Treatment Condition (treatment vs. sham) | 0.03 | 0.86 | 0.01 |
| Site (USA vs. NL) | 12.13 | 0.002 | 0.32 |
| Baseline Smoking Bias (approach vs. avoidance) | 10.42 | 0.003 | 0.29 |
| Within Subject Factors | |||
| Smoke Bias Score | 1.42 | 0.24 | 0.05 |
| Smoke Bias × Site | 2.86 | 0.10 | 0.10 |
| Smoke Bias × Treatment Condition | 0.45 | 0.51 | 0.02 |
| Smoke Bias × Baseline Smoking Bias | 7.22 | 0.01 | 0.22 |
| Smoking Bias × Treatment Condition × Baseline Smoking Bias | 0.00 | 0.99 | 0.00 |
| Neutral Bias Score | 3.10 | 0.09 | 0.11 |
| Neutral Bias × Site | 0.13 | 0.73 | 0.01 |
| Neutral Bias × Treatment Condition | 0.002 | 0.96 | 0.00 |
| Neutral Bias × Baseline Smoking Bias | 1.15 | 0.29 | 0.04 |
| Neutral Bias × Treatment Condition × Baseline Smoking Bias | 0.34 | 0.56 | 0.01 |
Note: The model controlled for age.
Smoking cessation outcomes were examined using chi-square tests to evaluate the effect of treatment condition on seven-day PP abstinence at EOT and three-month follow up using the ITT sample. Number of days abstinent during treatment was examined as a continuous outcome using a linear regression model with site, treatment condition, smoking approach bias at baseline, and the interaction between (1) site and treatment condition and (2) smoking approach bias at baseline and treatment condition as independent variables. We also conducted repeated-measures ANOVA with cotinine level at baseline and at follow up as a within-subject factor and site, treatment condition, and smoking approach bias status as between-subject factors. Similar analysis was conducted with self-report of number of cigarettes smoked per day seven days prior to baseline and seven days prior to EOT as a within-subject factor.
RESULTS
The randomized sample (N = 60; 65% males) was 16.57 (SD = 1.24) years old and smoked 11.72 (SD = 6.55) cigarettes per day, with mFTQ score of 2.86 (SD = 1.35), and cotinine values of 957.59 (SD = 649.66) at baseline. The adolescents in the sham condition were slightly older than those in the treatment condition (t (60) = -2.02, p = 0.048). The two treatment conditions did not differ on other baseline characteristics. American adolescents had a stronger approach bias than Dutch adolescents to smoking (t (60) = 3.75, p = 0.002) stimuli and neutral stimuli (t (60) = 2.85, p = 0.008). See Table 1 for the baseline study variables.
Table 1.
Baseline sample characteristics
| CBM (n = 29) | Sham (n =31) | |||
|---|---|---|---|---|
| American (n = 8) | Dutch (n = 21) | American (n = 10) | Dutch (n = 21) | |
| Gender (% female) | 50.0 | 42.9 | 20.0 | 28.6 |
| Age (M, SD) | 16.63, 0.74 | 16.10, 1.51 | 16.90, 1.10 | 16.86, 1.06 |
| # of cigarettes smoked per day in the past month (M, SD) | 10.99, 6.72 | 13.69, 6.38 | 9.25, 6.42 | 11.20, 6.63 |
| mFTQ (M, SD) | 3.04, 1.55 | 2.64, 1.28 | 3.33, 1.83 | 2.78, 1.08 |
| Cotinine (M, SD) | 1115.00, 638.10 | 827.27, 670.35 | 1059.20, 758.78 | 973.36, 602.62 |
| Smoking Push RT (M, SD) | 1066.16, 154.37 | 977.16, 166.32 | 1117.89, 181.56 | 982.91, 149.86 |
| Smoking Pull RT (M, SD) | 1033.19, 158.22 | 1053.04, 155.10 | 1061.12, 166.21 | 1039.49, 154.81 |
| Smoking Approach/Avoidance Bias (M, SD) | 32.97, 74.49 | −81.35, 173.81 | 59.77, 111.21 | −56.58, 76.66 |
| Neutral Push RT (M, SD) | 1045.10, 155.25 | 1008.55, 143.39 | 1072.30, 148.32 | 997.37, 144.96 |
| Neutral Pull RT (M, SD) | 1015.31, 193.53 | 1038.19, 130.85 | 1064,64, 197.71 | 1045.43, 139.02 |
| Neutral Approach/Avoidance Bias (M, SD) | 29.79, 89.64 | −27.93, 103.68 | 7.66, 72.96 | −68.07, 56.83 |
Note: mFTQ = modified Fagerström Tolerance Questionnaire. RT= reaction times
For the analyses examining changes in approach bias, the sample consisted of 35 participants (CBM: n = 16, sham: n = 19) who had complete data on S-AAT at both baseline and three-month follow-up. This sample was more likely to be male (Χ2 [1, N = 60] = 5.44, p = 0.02) than those with missing S-AAT data (n = 25), but they did not differ on other variables.
The overall attendance rate was 90%. The attendance rate differed by site (Dutch: 98% vs. American: 81%, t (35) −2.97, p = 0.008), but it did not differ by treatment condition (CBM: 89% vs. sham: 90%).
A repeated measures ANOVA showed significant main effects of site and baseline smoking approach bias (Table 2): American adolescents showed an approach bias toward smoking and neutral stimuli and Dutch adolescents showed an avoidance bias to these stimuli at baseline (see Table 1 for M and SD for each bias) and at follow up (American: smoking bias M = 30.73, SD = 83.58, neutral bias: M = 54.63, SD = 70.85; Dutch: smoking bias M = −32.45, SD = 98.76, neutral bias: M = −44.90, SD = 83.71). Adolescents with a smoking avoidance bias at baseline also had an avoidance bias toward smoking and neutral stimuli at baseline (smoking bias M = −73.75, SD = 60.38, neutral bias: M = −49.78, SD = 73.01) and at follow up (smoking bias M = −20.57, SD = 100.35, neutral bias: M = −31.96, SD = 100.35); conversely, those with a smoking approach bias had an approach bias to both stimuli at baseline (smoking bias M = 80.39, SD = 59.35, neutral bias: M = 6.68, SD = 83.58) and at follow up (smoking bias M = 18.16, SD = 89.50, neutral bias: M = 40.93, SD = 74.94).
Regarding the CBM effects on bias scores, the interaction between smoking bias scores and treatment condition and neutral bias scores and treatment condition were not significant (Table 2). However, we detected a significant interaction between smoking bias scores and baseline smoking approach bias status (Table 2, Figure 2). Post hoc analyses (See Supplemental Table 1), showed that at EOT, adolescents with a smoking approach bias at baseline showed significantly less approach bias at follow up (F (1, 17) = 4.71, p = 0.049), but did not show changes in neutral bias (F (1, 17) = 0.12, p = 0.74). Adolescents with a smoking avoidance bias at baseline did not show changes in either smoking (F (1, 18) = 2.18, p = 0.16) or neutral (F (1, 18) = 3.19, p = 0.10) biases (Figure 2). Furthermore, adolescents with a smoking avoidance at baseline showed a significant main effect of site (F (1, 18) = 9.98, p = 0.007) and an interaction effect of site and smoking bias scores (F (1, 18) = 4.55, p = 0.05); specifically, American adolescents with a smoking avoidance bias at baseline showed greater increase in smoking approach bias (baseline: M = -59.11, SD = 59.87, follow up: M = 99.02, SD = 58.63) compared to Dutch adolescents with a smoking avoidance bias at baseline (baseline: M = −.79.39, SD = 62.02, follow up: M = 23.86, SD = 97.48).
Figure 2.
Changes in smoking/neutral approach/avoidance bias scores from baseline to three-month follow-up separated smoking approach bias and smoking avoidance bias at baseline. Positive value indicates approach bias and negative values indicate avoidance bias. Error bars indicate ±1 Standard Error of the Mean (SEM).
Regarding effects on smoking cessation, the CBM condition had a trend toward higher end-of-treatment seven-day PP abstinence rates when compared with the sham condition (17.2% vs. 3.2%; Χ2(1, N = 60) = 3.27, p = 0.071) (Table 3)1. The abstinence rates at three-month follow-up did not differ by treatment condition and site (Table 3). The results of the linear regression analysis showed that site (p = 0.77), treatment condition (p = 0.61), smoking approach bias at baseline (p = 0.60), and the interaction terms (ps > 0.05) were not significantly associated with days abstinent during treatment. On average, participants were abstinent 46% of the days during treatment (results not shown).
Table 3.
Smoking cessation outcomes
| Total Sample (N = 60) | CBM (n = 29) | Sham (n = 31) | p | America n (n = 18) | Dutch (n = 42) | p | |
|---|---|---|---|---|---|---|---|
| % | % | ||||||
| End of Treatment | 10.0 | 17.2 | 3.2 | 0.07 | 0.0 | 14.3 | 0.09 |
| 3-Month Follow-up | 3.3 | 3.4 | 3.2 | 0.98 | 5.6 | 2.4 | 0.50 |
Note: Abstinence was defined as self-reported not smoking in the past 7 days, biochemically confirmed by urine cotinine levels ≤ 50 ng/ml. chi-square tests were conducted for categorical variables.
CBM=Cognitive Bias Modification
Repeated measures ANOVA showed that cotinine level (F (1, 39) = 4.38, p = 0.045) and average number of cigarette smoked (F (1, 41) = 52.67, p ≤ 0.001) significantly decreased over the course of treatment among all participants regardless of treatment condition (baseline: cotinine M = 911.36, SD = 674.60, number of cigarettes M = 11.42, SD = 6.74; follow-up: cotinine M = 710.30, SD = 573.42, number of cigarettes M = 1.99, SD = 3.36). No other main effects and interaction effects were significant (results not shown).
DISCUSSION
This exploratory pilot study is the first to examine whether a computerized CBM for smoking cessation re-trains the approach-bias for smoking-related cues and whether this retraining enhances smoking cessation among adolescent smokers who receive CBT for smoking-cessation. The findings indicate that relative to sham, CBM did not modify approach bias but it did show a statistical trend toward improving smoking cessation outcomes.
Prior studies among clinical samples of alcohol-dependent adults have observed that CBM improved abstinence outcomes (28, 29), and a more recent pilot study with adult smokers has also observed that CBM yielded promising treatment outcomes (32). These studies utilized larger sample sizes (over 200), compared with the sample size used in the current pilot trial. In fact, the effect size (d) of 0.2 detected in the current trial suggests that a sample size of approximately 200 participants is needed to observe significance.
Moreover, in the current trial the sham condition of 50% approach and 50% avoidance towards smoking stimuli may not have been sufficiently different from the CBM condition of 90% approach and 10% avoidance toward smoking stimuli. Indeed, we observed that regardless of treatment condition there was an overall decrease in cotinine levels and self-reported number of cigarettes smoked from baseline to end of treatment (EOT) among all participants. Furthermore, although we did not detect a differential change in smoking approach bias by treatment group, we observed that regardless of treatment condition, adolescents who had smoking approach bias at baseline significantly reduced their approach bias at EOT, suggesting that both treatment conditions may have re-trained approach tendencies among those who already had a smoking approach bias. This is consistent with previous studies that showed that the change in approach bias is moderated by the strength of approach bias at baseline (28). These findings suggest that future studies should consider utilizing schedules which have greater differences between the treatment and the sham condition.
We detected a difference in approach biases between Dutch and American adolescents. Specifically, Dutch adolescents had greater avoidance bias, while American adolescents had greater approach bias. This pattern of bias was also detected in a previous study that examined approach biases toward smoking stimuli among smoking and non-smoking adolescents (37). While we do not know why such differences in biases exist, they could possibly be related to the fact that the images used in the S-AAT were evaluated by American adolescents but not by Dutch adolescents (37). Future studies should validate the images in the sample in which they are administered, especially when it involves cross-cultural comparisons. This may be important to consider given that implicit tendencies are context dependent (42-44). For instance, context influenced implicit associations have been observed with food-related words among overweight individuals (44). Context may be particularly important for adolescents because their smoking often occurs in social settings in the presence of their peers (45) or under certain emotional states (e.g., stress, negative affect) (46), and it is possible that these contextual factors were different in the USA and in the NL. Thus, future studies should evaluate the images to ensure their context relevance.
In addition to the limitations mentioned earlier, it is also important to point out that the reliability and validity of the smoking AAT in adolescents has not yet been thoroughly investigated. Research using the alcohol-AAT has demonstrated that the validity of the task is improved when relevant feature tasks (i.e., participants respond to the content of the image) as opposed to irrelevant feature tasks (i.e., participants respond to the format of the image like its rotation rather than the image content) are used (47). Nevertheless, others have found that irrelevant feature tasks may still be suitable for the modification of substance-related cognitive biases (28, 29). Although reaction-time based interventions have shown promising clinical effects (e.g., 28, 29, 30), there is limited evidence for sufficient reliability of reaction-time assessments (48-50). However, despite these limitations, we observed an overall smoking cessation rate (10%; Table 3), which was comparable to the observed quit rates found among other adolescent smoking cessation interventions (51-53). In addition, the trend-level differences observed between the CBM and the sham-training control conditions, suggest that interventions that target the implicit processes show promise for adolescent smoking cessation. Future studies should be conducted to further explore the efficacy of such innovative interventions, as well as to examine the association between responses to CBM and cognitive constructs like working memory and impulsivity, which have been shown to be related to adolescent smoking behaviors (e.g. Larsen, et al. (37)) as well as adolescent smoking cessation (e.g. Krishnan-Sarin, et al. (54)). Importantly, earlier work has shown that the effectiveness of CBM may be related to individual differences in regulatory control among adolescents with anxiety (55) and low response inhibition and low working memory have also been shown to be correlated with approach bias toward alcohol-related stimuli and actual alcohol use (10-12). Future research could also focus on how to tailor and enhance the appeal of CBM for adolescents (56, 57). Perhaps game-elements can be added to CBM to make more interesting (31). Other intervention components such as optimal number of sessions needed for re-training to occur should also be identified. Studies examining CBM have used varied number of sessions, from two (58) to 12 (28), with recent data suggesting great variability in optimal length of training, among adult alcohol-dependent patients (59).
In summary, this exploratory pilot study was the first pilot study to examine the utility of a novel, computerized intervention designed to retrain action tendencies toward smoking-related stimuli among adolescent smokers. While the clinical utility of CBM for smoking cessation among adolescent smokers could not be established based on this pilot, the results show trends toward its utility, suggesting that carefully designed studies with larger samples are needed.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank Anne-Sophie Schürmann, Mirtemaaij van Schooten, Rianne Zomer, Xia Stevens, Marion Velten, Roos Knijnenburg, and Wenda Frederiks for their assistance in the study.
Sources of Support: This work was funded by a bi-national grant, jointly awarded to the two senior authors (SKS: National Institute on Drug Abuse supplement to R01DA01596 and P50 DA009241. RW: ZONMW grant: 60-60600-97-305). ES is supported by a grant from the Dutch National Science Foundation (VENI 451-10-029).
Footnotes
We also conducted survival analysis (time to first lapse) and found no significant differences between the treatment condition in time to first lapse during treatment (Wald χ2 = 0.12, p = 0.73).
DECLARATION OF INTERESTS
The authors do not have conflicts of interest and financial interests to declare.
References
- 1.U.S. Department of Health and Human Services . Preventing Tobacco Use among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and PRevention, Office on Smoking and Health; Atlanta: 2012. 2012. [Google Scholar]
- 2. http://www.who.int/tobacco/surveillance/policy/country_profile/nld.pdf?ua=1.
- 3.Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national results on drug use: 1975-2013: Overview, Key Findings on Adolescent Drug Use. Institute for Social Research, The University of Michigan; Ann Arbor: 2014. [Google Scholar]
- 4.Centers for Disease Control and Prevention High school students who tried to quit smoking cigarettes - United States, 2007. MMWR. 2009;58(16):428–431. [PubMed] [Google Scholar]
- 5.Backinger CL, Leischow SJ. Advancing the science of adolescent tobacco use cessation. Am J Health Behav. 2001;25:183–190. doi: 10.5993/ajhb.25.3.4. [DOI] [PubMed] [Google Scholar]
- 6.Grimshaw G, Stanton A. Tobacco cessation interventions for young people. Cochrane Database Syst Rev. 2006:CD003289. doi: 10.1002/14651858.CD003289.pub4. [DOI] [PubMed] [Google Scholar]
- 7.Stacy AW, Wiers RW. Implicit cognition and addiction: A tool for explaining paradoxical behavior. Annu Rev Clin Psycho. 2010;6:551–575. doi: 10.1146/annurev.clinpsy.121208.131444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiers RW, Bartholow BD, van den Wildenberg E, Thush C, Engels RCME, Sher KJ, Grenard J, Ames SL, Stacy AW. Automatic and controlled processes and the development of addictive behavior in adolescents: a review and a model. Pharmacol Biochem Be. 2007;86:263–283. doi: 10.1016/j.pbb.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Pers Soc Psychol Rev. 2004;8:220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- 10.Grenard JL, Ames SL, Wiers RW, Thush C, Sussman S, Stacy AW. Working memory moderates the predictive effects of drug-related associations. Psychol Addict Behav. 2008;22:426–432. doi: 10.1037/0893-164X.22.3.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peeters M, Wiers RW, Monshouwer K, van de Schoot R, Janssen T, Vollebergh WAM. Automatic processes in at-risk adolescents: the role of alcohol-approach tendencies and response inhibition in drinking behavior. Addiction. 2012;107:1939–1946. doi: 10.1111/j.1360-0443.2012.03948.x. [DOI] [PubMed] [Google Scholar]
- 12.Peeters M, Monshouwer K, van de Schoot RAGJ, Janssen T, Vollebergh WAM, Wiers RW. Automatic processes and the drinking behavior in early adolescence: A prospective study. Alcohol Clin Exp Res. 2013;37:1737–1744. doi: 10.1111/acer.12156. [DOI] [PubMed] [Google Scholar]
- 13.Thush C, Wiers RW, Ames SL, Grenard JL, Sussman S, Stacy AW. Interactions between implicit and explicit cognition and working memory capacity in the prediction of alcohol use in at-risk adolescents. Drug Alcohol Depen. 2008;94:116–124. doi: 10.1016/j.drugalcdep.2007.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krank MD, Goldstein AL. Adolescent changes in implicit cognitions and prevention of substance abuse. Handbook of implicit cognition and addiction. 2006:439–453. [Google Scholar]
- 15.Rooke SE, Hine DW. A dual process account of adolescent and adult binge drinking. Addict Behav. 2011;36(4):341–346. doi: 10.1016/j.addbeh.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Sherman SJ, Chassin L, Presson C, Seo D, Macy JT. The intergenerational transmission of implicit and explicit attitudes toward smoking: Predicting adolescent smoking initiation. J Exp Soc Psychol. 2009;45(2):313–319. doi: 10.1016/j.jesp.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mogg K, Bradley BP, Field M, De Houwer J. Eye movements to smoking-related pictures in smokers: relationship between attentional biases and implicit and explicit measures of stimulus valence. Addiction. 2003;98(6):825–836. doi: 10.1046/j.1360-0443.2003.00392.x. [DOI] [PubMed] [Google Scholar]
- 18.Bradley BP, Mogg K, Wright T, Field M. Attentional bias in drug dependence: Vigilance for cigarette-related cues in smokers. Psychol Addict Behav. 2003;17:66–72. doi: 10.1037/0893-164x.17.1.66. [DOI] [PubMed] [Google Scholar]
- 19.Ehrman RN, Robbins SJ, Bromwell MA, Lankford ME, Monterosso JR, O'Brien CP. Comparing attentional bias to smoking cues in current smokers, former smokers, and non-smokers using a dot-probe task. Drug Alcohol Depen. 2002;67:185–191. doi: 10.1016/s0376-8716(02)00065-0. [DOI] [PubMed] [Google Scholar]
- 20.Wiers CE, Kühn S, Javadi AH, Korucuoglu O, Wiers RW, Walter H, Gallinat J, Bermpohl F. Automatic approach bias towards smoking cues is present in smokers but not in ex-smokers. Pyschoph. 2013;229:187–197. doi: 10.1007/s00213-013-3098-5. [DOI] [PubMed] [Google Scholar]
- 21.Watson P, de Wit S, Cousijn J, Hommel B, Wiers RW. Motivational mechanisms underlying the approach bias to cigarettes. J Exp Soc Psychopathology. 2013;4:250–262. [Google Scholar]
- 22.Huijding J, de Jong PJ. Automatic associations with the sensory aspects of smoking: Positive in habitual smokers but negative in non-smokers. Addict Behav. 2006;31(1):182–186. doi: 10.1016/j.addbeh.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Waters A, Carter B, Robinson J, Wetter D, Lam C, Cinciripini P. Implicit attitudes to smoking are associated with craving and dependence. Drug Alcohol Depen. 2007;91:178–186. doi: 10.1016/j.drugalcdep.2007.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Payne BK, McClernon FJ, Dobbins IG. Automatic affective responses to smoking cues. Exp Clin Psychopharm. 2007;15:400–409. doi: 10.1037/1064-1297.15.4.400. [DOI] [PubMed] [Google Scholar]
- 25.Chassin L, Presson CC, Sherman SJ, Seo DC, Macy JT. Implicit and explicit attitudes predict smoking cessation: moderating effects of experienced failure to control smoking and plans to quit. Psychol Addict Behav. 2010;24:670–679. doi: 10.1037/a0021722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiers RW, Rinck M, Dictus M, van den Wildenberg E. Relatively strong automatic appetitive action-tendencies in male carriers of the OPRM1 G-allele. Genes Brain Behav. 2009;8:101–106. doi: 10.1111/j.1601-183X.2008.00454.x. [DOI] [PubMed] [Google Scholar]
- 27.Cousijn J, Goudriaan AE, Wiers RW. Reaching out toward cannabis: Apporach-bias in heavy cannabis users predicts changes in cannais use. Addiction. 2011;106:1667–1674. doi: 10.1111/j.1360-0443.2011.03475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eberl C, Wiers RW, Pawelczack S, Rinck M, Becker ES, Lindenmeyer J. Approach bias modification in alcohol dependence: Do clinical effects replicate and for whom does it work best? Dev Cogn Neurosci. 2013;4:38–51. doi: 10.1016/j.dcn.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wiers RW, Eberl C, Rinck M, Becker ES, Lindenmeyer J. Retraining automatic action tendencies changes alcoholic patients' approach bias for alcohol and improves treatment outcome. Psychol Sci. 2011;22(4):490–497. doi: 10.1177/0956797611400615. [DOI] [PubMed] [Google Scholar]
- 30.Wiers RW, Rinck M, Kordts R, Houben K, Strack F. Re-training automatic action-tendencies to approach alcohol in hazardous drinkers addiction. Addiction. 2010;105:279–287. doi: 10.1111/j.1360-0443.2009.02775.x. [DOI] [PubMed] [Google Scholar]
- 31.Wiers RW, Gladwin TE, Hofmann W, Salemink E, Ridderinkhof KR. Cognitive bias modifcations and cognitive control training in addition and related psychopathology: Mechansims, clinical perspecties, and ways forward. Clin Pyschol Sci. 2013;1:192–212. [Google Scholar]
- 32.Wittekind CE, Feist A, Viertel B, Moritz S, Fritzsche A. The Approach-Avoidance Task as an online intervention in cigarette smoking: A pilot study. J Be Ther Exp Psychiat. 2014 doi: 10.1016/j.jbtep.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 33.US Department of Health and Human Services . Tobacco Use and Dependence Guideline Panel, Treating Tobacco Use and Dependence: 2008 Update. Rockville (MD): 2008. [Google Scholar]
- 34.Baert S, Koster EHW, De Raedt R. Modification of information-processing biases in emotional disorders: Clinical relevant developments in experimental psychopathology. Int J Cogn Ther. 2011;4:208–222. [Google Scholar]
- 35.Sobell LC, Toneatto T, Sobell MB, Leo GI, Johnson L. Alcohol abusers' perceptions of the accuracy of their self-reports of drinking: Implications for treatment. Addict Behav. 1992;17(5):507–511. doi: 10.1016/0306-4603(92)90011-j. [DOI] [PubMed] [Google Scholar]
- 36.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom K-O. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Brit J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 37.Larsen H, Kong G, Becker D, Cousijn J, Boendermaker W, Cavallo D, Krishnan-Sarin S. Implicit motivational processes underlying smoking in American and Dutch adolescents. Front Psychiatry. 2014;5:1–9. doi: 10.3389/fpsyt.2014.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cavallo DA, Cooney JL, Duhig AM, Smith AE, Liss TB, McFetridge AK, Babuscio T, Nich C, Carroll KM, Rounsaville BJ, Krishnan-Sarin S. Combining cognitive behavioral therapy with contingency management for smoking cessation in adolescent smokers: a preliminary comparison of two different CBT formats. Am J Addiction. 2007;16(6):468–474. doi: 10.1080/10550490701641173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krishnan-Sarin S, Duhig AM, McKee SA, McMahon TJ, Liss T, McFetridge A, Cavallo DA. Contingency management for smoking cessation in adolescent smokers. Exp Clin Psychopharm. 2006;14(3):306–310. doi: 10.1037/1064-1297.14.3.306. [DOI] [PubMed] [Google Scholar]
- 40.Krishnan-Sarin S, Cavallo DA, Cooney JL, Schepis TS, Kong G, Liss TB, Liss AK, McMahon TJ, Nich C, Babuscio T, Rounsaville BJ, Carroll KM. An exploratory randomized controlled trial of a novel high-school-based smoking cessation intervention for adolescent smokers using abstinence–contingent incentives and cognitive behavioral therapy. Drug Alcohol Depen. 2013;132(1–2):346–351. doi: 10.1016/j.drugalcdep.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.SRNT Subcommittee on Biochemical Verification Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- 42.Sherman SJ, Rose JS, Koch K, Presson CC, Chassin L. Implicit and explicit attitudes toward cigarette smoking: The effects of context and motivation. J Soc Clin Psycho. 2003;22:13–39. [Google Scholar]
- 43.Mitchell JP, Nosek BA, Banaji MR. Contextual variations in implicit evaluation. J Exp Psychol Gen. 2003;132:455–469. doi: 10.1037/0096-3445.132.3.455. [DOI] [PubMed] [Google Scholar]
- 44.Roefs A, Quaedackers L, Werrij MQ, Wolters G, Havermans R, Nederkoorn C, van Breukelen G, Jansen A. The environment influences whether high-fat foods are associated with palatable or with unhealthy. Behav Res Ther. 2006;44(5):715–736. doi: 10.1016/j.brat.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 45.Kobus K. Peers and adolescent smoking. Addiction. 2003;98:37–55. doi: 10.1046/j.1360-0443.98.s1.4.x. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein SM, Mermelstein RJ. Dynamic associations of negative mood and smoking across the development of smoking in adolescence. J Clin Child Adol Psychol. 2013;42:629–642. doi: 10.1080/15374416.2013.794698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kersbergen I, Woud ML, Field M. The validity of different measures of automatic alcohol action tendencies. Psychol Addict Behav. 2014 doi: 10.1037/adb0000009. [DOI] [PubMed] [Google Scholar]
- 48.Brown HM, Eley TC, Broeren S, MacLeod C, Rinck M, Hadwin JA, Lester KJ. Psychometric properties of reaction time based experimental paradigms measuring anxiety-related information-processing biases in children. J Anxiety Dis. 2014;28(1):97–107. doi: 10.1016/j.janxdis.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 49.Ataya AF, Adams S, E. M, Cooper RM, Attwood AS, Munafo MR. Internal reliability of measures of substance-related cognitive bias. Drug Alcohol Depen. 2012;121:148–151. doi: 10.1016/j.drugalcdep.2011.08.023. [DOI] [PubMed] [Google Scholar]
- 50.Cousijn J, Luijten M, Wiers RW. Mechanisms underlying alcohol-approach action tendencies: the role of emotional primes and drinking motives. Front Psychiatry. 2014;5:44. doi: 10.3389/fpsyt.2014.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sussman S. Effects of sixty six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tob Induc Dis. 2002;1(1):35–81. doi: 10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sussman S, Sun P, Dent CW. A meta-analysis of teen cigarette smoking cessation. Health Psychology. 2006;25(5):549–557. doi: 10.1037/0278-6133.25.5.549. [DOI] [PubMed] [Google Scholar]
- 53.Sussman S, Sun P. Youth tobacco use cessation: 2008 update. Tob Induc Dis. 2009;5(1):1–11. doi: 10.1186/1617-9625-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krishnan-Sarin S, Reynolds B, Duhig AM, Smith AE, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depen. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Salemink E, Wiers RW. Adolescent threat-related interpretive bias and its modification: The moderating role of regulatory control. Behav Res Ther. 2012;50(1):40–46. doi: 10.1016/j.brat.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 56.McDonald P, Colwell B, Backinger CL, Husten C, Maule CO. Better practices for youth tobacco cessation: evidence of review panel. Am J Health Behav. 2003;27(Suppl. 2):S144–S158. doi: 10.5993/ajhb.27.1.s2.5. [DOI] [PubMed] [Google Scholar]
- 57.Milton M, Maule CO, Backinger CL, Gregory DM. Recommendations and guidance for practice in youth tobacco cessation. Am J Health Behav. 2003;27(Suppl. 2):S159–S169. [PubMed] [Google Scholar]
- 58.Fadardi JS, Cox WM. Reversing the sequence: reducing alcohol consumption by overcoming alcohol attentional bias. Drug Alcohol Depen. 2009;101:137–145. doi: 10.1016/j.drugalcdep.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 59.Eberl C, Wiers RW, Pawelczack S, Rinck M, Becker ES, Lindenmeyer J. Implementation of approach bias re-training in alcoholism-How many sessions are needed? Alcohol Clin Exp Res. 2013 doi: 10.1111/acer.12281. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.