Abstract
Among gay and bisexual men (GBM), a syndemic describes a situation in which negative conditions (e.g., childhood sexual abuse, intimate partner violence, depression, polysubstance use) co-occur such to amplify HIV risk. Research has suggested that sexual compulsivity (SC) may also be a syndemic condition. Between 2011 and 2013, 368 highly sexually active (9+ male partners in 90 days) GBM completed a survey of syndemic factors as well as measures of sexual compulsivity (Sexual Compulsivity Scale [SCS]) and hypersexuality (hypersexual disorder screening inventory [HDSI]). Based on scores on the SCS and HDSI, participants were organized into three groups—negative on both (“Neither SC nor HD”); positive on the SCS only (“SC Only”), and positive on both the SCS and the HDSI (“Both SC and HD”). We found support for the utility of a three-group classification of sexual compulsivity/hypersexuality as one of the syndemic factors that contribute to HIV risk. The average number of syndemic factors experienced was lowest among those who experienced Neither SC nor HD and highest among the group that experienced Both SC and HD, with those experiencing SC Only falling between the two other groups. This study provided further evidence that sexual compulsivity/hypersexuality is a contributing factor to the syndemics model of HIV risk for GBM and that considering three levels of severity (i.e., SC along with HD) led to stronger model predictions than considering SC alone. SC/HD severity provides another modifiable target for HIV prevention intervention development.
Keywords: Sexual compulsivity, Syndemics, Gay and bisexual men, HIV, Condom use, Sexual orientation
Introduction
Gay, bisexual, and other men who have sex with men (GBMSM) continue to be disproportionately affected by HIV, accounting for 83 % of new infections among men in the United States in 2011 (Johnson et al., 2014). Further, although the annual rate of HIV diagnoses in the United States from 2002 to 2011 decreased overall by 33 %, rates among GBMSM remained stable with significant increases noted among some age groups.
Syndemic theory provides a useful framework for understanding health disparities among marginalized communities (Singer, 1994; Singer et al., 2006), including vulnerability to HIV infection among GBMSM (Stall et al., 2003). A syndemic is the interaction of multiple co-occurring conditions and psychosocial risk factors working synergistically to increase the risk of negative health outcomes.
Several studies have examined the influence of syndemics—psychosocial health problems, such as childhood sexual abuse, depression, substance use, and intimate partner violence—on HIV risk among GBMSM living in the United States and found support for the hypothesis that as the number of syndemic factors increase, so do sexual risk behaviors and risk of HIV infection (Dyer et al., 2012; Mustanski, Garofalo, Herrick, & Donenberg, 2007; O’Leary, Jemmott, Stevens, Rutledge, & Icard, 2014; Parsons, Grov, & Golub, 2012; Stall et al., 2003). Empirical support for the connection between syndemics and HIV risk has also been identified among GBMSM in Canada (Ferlatte, Hottes, Trussler,& Marchand, 2014), Thailand (Guadamuz et al., 2014), Belgium (Wim, Christiana, & Marie, 2014), and also in a global sample of GBMSM across 151 countries (Santos et al., 2014). Collectively, these studies support syndemic factors as having an additive effect on sex risk among GBMSM (Starks, Millar, Eggleston, & Parsons, 2014).
Another factor that has been studied as a correlate of sexual risk behavior among GBMSM is sexual compulsivity (SC; Coleman et al., 2010; Grov, Golub, Mustanski, & Parsons, 2010a; Grov, Parsons, & Bimbi, 2010b; Kalichman & Rompa, 1995). SC is characterized by sexual thoughts and behaviors that reach levels of intensity and frequency such that they interfere with personal, interpersonal, or vocational pursuits (Kafka, 2010; Kalichman & Rompa, 1995; Muench & Parsons, 2004; Parsons, Kelly, Bimbi, Muench, & Morgenstern, 2007). Although the role of SC as a syndemic factor is understudied, some data have demonstrated individual associations between SC and known syndemic factors—substance use, depression, childhood sexual abuse, and intimate partner violence (Carrico et al., 2012; Dyer et al., 2012; Herrick et al., 2013; Parsons et al., 2012). For example, in a study of syndemic production among GBMSM living in four major cities across the United States, SC was found to be significantly associated with depressive symptoms and intimate partner violence (Herrick et al., 2013). Similarly, in a study of GBMSM living in New York City, SC was associated with intimate partner violence, depression, and childhood sexual abuse and operated along with these syndemic conditions to increase sexual risk (Parsons et al., 2012). Thus, evidence suggests that SC and other syndemic conditions work synergistically to increase both sexual risk behavior and risk of HIV infection.
These findings, however, are based on studies that did not account for the influence of potentially confounding factors. For example, most studies did not control for levels of sexual activity and studies have typically utilized samples in which most of the participants reported limited sexual activity or few sex partners in a given period (Parsons et al., 2012). Previous research indicates that sexually compulsive GBMSM report a greater number of sex partners than GBMSM do in general (Grov et al., 2010b). Additionally, studies focusing on SC have typically classified men as compulsive or not, but emerging research on hypersexuality (Kafka, 2010) points to the importance of differentiating across the SC continuum to classify gay and bisexual men (GBM) into distinctive groups (Parsons, Rendina, Ventuneac, Moody, & Grov, 2015). Using the Sexual Compulsivity Scale (SCS; Kalichman & Rompa, 1995) and the Hypersexual Disorder Screening Inventory (HDSI; Kafka, 2010), previous work has suggested that a three-group classification of highly sexually active GBM—negative on both, “neither sexually compulsive nor hypersexual;” (2) positive on the SCS only, “sexually compulsive only;” and (3) positive on both the SCS and the HDSI, “both sexually compulsive and hypersexual”—may provide a more nuanced examination of HIV risk among highly sexually active GBM (Parsons et al., 2015).
Current Study
The current study sought to examine the role of SC as a syndemic factor in increasing HIV risk in an urban sample of GBM who engage in a similar level of high sexual activity. Our goals were to examine the association between SC and the other factors in the syndemics framework and to test several models that would provide evidence about whether or not SC has an additive impact in predicting HIV risk. Given that a three-group classification has been shown to be a useful approach in examining risk among highly sexually active GBM, we investigated whether using both the SCS and HDSI might be a better way of examining SC as a syndemic factor than using the SCS alone, as has been done in prior research. We hypothesized that utilizing a three-group SC classification is an additional contributor to the syndemics framework in explaining HIV risk. An alternative consideration, however, is that SC is not, in and of itself, a syndemic factor, but rather mediates the association between other syndemic conditions and HIV risk. For example, SC could mediate the relationship between depression and HIV sexual risk, in that depression results in more sexual acting out, which in turn leads to sexual risk. To rule out this competing hypothesis, we also tested whether SC mediates the association between syndemics and HIV risk.
Most previous studies of syndemics among GBM have utilized broad samples in terms of rates of sexual activity and number of partners. Further, many studies of SC have also relied on broad samples in which those with many sexual partners are compared to those with few. In these samples, the SC people are—by the nature of the distribution of sexual behavior—highly sexually active, and those without SC are not. However, to understand the specific connections between syndemics and SC, relying on a sample of highly sexually active GBM enables one to examine a behaviorally similar sample in terms of psychosocial differences. For this reason, we sought to examine these relationships in a sample of highly sexually active GBM.
Method
Participants and Procedure
Data for this study were taken from Pillow Talk, a longitudinal study that focused on issues related to syndemics and SC among highly sexually active GBM in New York City. The primary goal of the study was to enroll GBM who were similar with regard to the amount of sexual behavior but different in the extent to which these behaviors were causing problems in their lives—consistent with SC. Data were obtained from 376 GBM enrolled in the project; four individuals had incomplete data for the survey and four individuals had inconsistent data on the SCS and HSDI (i.e., they met the threshold for the SCS but not the HDSI), and thus the present analyses focus on an analytic sample of 368 men.
Between 2011 and 2013, we enrolled participants utilizing a combination of recruitment strategies: (1) respondent-driven sampling; (2) Internet-based advertisements on social and sexual networking websites; (3) email blasts through New York City gay sex party listservs; and (4) active recruitment in New York City venues such as gay bars/clubs, concentrated gay neighborhoods, and ongoing gay community events. All participants completed a brief, phone-based screening to determine eligibility, which was defined as: (1) at least 18 years of age; (2) biologically male and self-identified as male; (3) a minimum of 9 different male sexual partners in the prior 90 days; (4) self-identification as gay, bisexual, or some other non-heterosexual identity (e.g., queer);(5) able to complete assessment in English, and (6) daily access to the internet in order to complete Internet-based portions of the study.
For the purposes of this project, we operationalized highly sexually active as having at least 9 sexual partners in the 90 days prior to enrollment based on prior research (Grov et al., 2010b; Parsons, Bimbi, & Halkitis, 2001; Parsons et al., 2008), including a probability-based sample of urban GBMSM (Stall et al., 2002, 2003) that found that 9 partners was 2–3 times the average number of sexual partners among sexually active GBM. All eligibility criteria were confirmed at the baseline appointment, with sex criteria being confirmed using the timeline follow-back (TLFB) interview in which a calendar was used to recall sexual behavior (Sobell & Sobell, 1992). Participants were excluded from the project if they demonstrated evidence of serious cognitive or psychiatric impairment that would interfere with their participation or limit their ability to provide informed consent, as indicated by a score of 23 or lower on the Mini-Mental Status Examination (MMSE; Folstein, Folstein, & McHugh, 1975) or evidence of active and unmanaged symptoms on the psychotic symptoms or suicidality sections of the Structured Clinical Interview for the DSM-IV-IR (SCID; First, Spitzer, Gibbon, & Williams, 2002); a total of 10 otherwise eligible participants were excluded.
Participation in the study involved both at-home (Internet-based) and in-office assessments. After a member of the research staff confirmed participants’ eligibility over the phone, participants were sent a link to complete an Internet-based survey at home prior to their first in-office appointment that took approximately 1 h to complete. Informed consent was obtained for both online and in-person portions of the study. All procedures were reviewed and approved by the Institutional Review Board of the City University of New York.
Measures
Quantitative measures used for these analyses were completed as part of one of three components of the study: (1) the at-home survey prior to the baseline appointment, (2) the in-office survey completed during the baseline appointment, and (3) the structured TLFB interview. After providing online consent to continue with the survey, participants completed measures of demographics and SC. All later measures (including syndemics) were grouped into the matic blocks (e.g., stigma, sexuality, mental health) and the order of blocks within the survey and the order of measures within blocks were both randomized in order to evenly distribute the order effects that can result from serial positioning and priming.
Childhood Sexual Abuse
We assessed childhood sexual abuse (CSA) utilizing a measure and criteria from the first study of syndemics among GBMSM (Paul, Catania, Pollack, & Stall, 2001; Stall et al., 2003). Participants were first asked to respond to the question, “Thinking back from your childhood to the present, have you ever been forced or frightened by someone into doing something sexually that you did not want to do?” Participants were also asked to respond to the question, “Sometimes peoples’ views about their experiences change overtime. Did you ever have an experience when you felt at the time that you were forced or frightened into doing something sexually that you did not want to do?” Participants were also asked to report the age at which the event first occurred and the approximate age of the person who did this to them. We recoded responses of “yes” to either of the first two questions into a dichotomous indicator of whether participants reported such an experience at age 16 or younger with a partner at least 10 years older based on prior research (Parsons et al., 2012; Paul et al., 2001; Stall et al., 2003).
Intimate Partner Violence
Participants were asked whether, in the past 5 years, they had experienced a variety of 12 violent acts within an intimate relationship, ranging from verbal attacks (e.g., “verbally threatened you in any way,” “made fun of your appearance”) to physical assault (e.g., “kicked you,” “forced you to get high or drunk,” “hit you with an object”). Consistent with previous syndemic studies (Greenwood et al., 2002; Stall et al., 2003), any response of yes was coded as having experienced intimate partner violence (IPV). As such, this variable includes a heterogeneous group of individuals whose experiences in the prior 5 years ranged from verbal abuse to physical and sexual assault.
Depressive Symptoms
Participants completed the 6 depression items of the Brief Symptom Inventory (BSI; Derogatis, 1975) with response options ranging from 0 (Not at all) to 4 (Extremely). The scale had high internal consistency in this sample (α=0.93) and previous work has shown that a cutoff of 0.5 has high reliability and validly distinguishes clinical from non-clinical populations (Schulte-van Maaren et al., 2012).
Polysubstance Use
Participants completed a 6-week (i.e., 42 day) TLFB interview (Sobell & Sobell, 1992), which included an assessment of daily substance use. Consistent with syndemics research, we created a dichotomous indicator of whether the participant had used at least three different recreational drugs during the 42-day recall period. These included, cocaine, crack, inhalants (“poppers”), GHB, heroin, ketamine, marijuana, methamphetamine, MDMA (“ecstasy”), and psychedelics (e.g., LSD, acid) as well as any use of prescription sedatives, stimulants, and pain killers without a prescription or other than as originally prescribed (Stall et al., 2003).
Operational Definition of Syndemic Conditions
Using the four aforementioned measures, and consistent with previous work on syndemic conditions and HIV risk among GBM (Stall et al., 2003), we created dichotomous indicators of each of the four commonly cited syndemic conditions—CSA, IPV, depressive symptoms, and polysubstance use—to create an overall score ranging from 0 to 4 (Starks et al., 2014).
Sexual Compulsivity
We utilized the most common measure of SC in studies of GBM (Hook, Hook, Davis, Worthington, & Penberthy, 2010)—the Sexual Compulsivity Scale (SCS; Kalichman & Rompa, 1995). The SCS consists of 10 items, which were rated on a Likert-type scale from 1 (not at all like me) to 4 (very much like me). Responses to each item were summed to get an overall score (range, 10–40). The SCS has been shown to have high reliability and validity (Hook et al., 2010; Parsons et al., 2015) and had strong internal consistency in this sample (α = 0.91). Individuals with a score of 24 or greater were categorized as SC (Grov et al., 2010b; Parsons et al., 2001; Rendina, Golub, Grov, & Parsons, 2012; Ventuneac, Rendina, Grov, Mustanski, & Parsons, 2015).
Problematic Hypersexuality
Participants completed the HDSI, proposed by the American Psychiatric Association’s DSM-5 Workgroup on Sexual and Gender Identity Disorders (APA, 2010; Kafka, 2010, 2014). The scale consists of seven items split into two sections (A and B) measuring criteria met within the prior 6 months. Section A consisted of five items measuring recurrent and intense sexual fantasies, urges, and behaviors and Section B contains two items measuring distress and impairment as a result of these fantasies, urges, and behaviors. Responses ranged from 0 (Never true) to 4 (Almost always true), with responses of 3 or 4 keyed as a present symptom. Polytomous scoring criteria suggest that a participant who experiences four of the five symptoms from Section A and at least one of the symptoms for Section B should be considered to have screened positive for hypersexual disorder (HD). Prior research has found the scale to have strong reliability (Parsons et al., 2013) and internal consistency was strong (α= 0.90).
Sexual Compulsivity/Hypersexuality Severity
We also utilized the respective cutoffs for the SCS and the HDSI to classify participants’ level of severity as 0 (Neither SC nor HD), 1 (SC Only), or 2 (Both SC and HD). This approach has been shown to be more useful than either of the cutoffs by itself for studying the impact of sexual compulsivity and hypersexuality (Parsons et al., 2015).
HIV Risk Outcomes
As has been typically done to show support for syndemic models, we utilized two dichotomous outcomes: (1) whether a participant had any condomless anal sex (CAS) with a serodiscordant or unknown HIV-status partner in the 42-days preceding the baseline appointment (on the TLFB); and (2) HIV status verified via on-site rapid HIV test or via proof of HIV-positive status at baseline.
Statistical Analyses
We examined the association between SC/HD groups and the four syndemic conditions utilizing Chi square statistics and post hoc comparisons with Bonferroni adjustment for multiple comparisons. Then, we examined whether SC/HD was a result of syndemic exposure and mediated the syndemic-HIV risk association or, alternatively, if SC/HD was a syndemic condition itself. We did so by testing a series of models. In the first model, the syndemic conditions variable had an exogenous path to the SC/HD group variable and both variables had exogenous paths to the two HIV risk outcomes. We tested for both direct and indirect effects of syndemics on HIV risk outcomes, examining whether the hypothesis of SC/HD mediating the association between syndemics and HIV risk was supported. To examine whether SC/HD group might be meaningful additions to the syndemics framework, as has received support in previous research (Carrico et al., 2012; Herrick et al., 2013; Parsons et al., 2012, 2015), we tested two additional models:
A path model whereby the dichotomous indicator from the SCS (1 =24 or greater) was added to the existing syndemic conditions variable and was entered as the only predictor of the two HIV risk outcomes;
A path model where by the SC/HD group variable was added to the existing syndemic conditions variable and was entered as the only predictor of the two outcomes.
Path models were calculated in Mplus version 7.2. The SC/HD group was specified as an ordinal outcome and the HIV risk variables were specified as dichotomous outcomes using weighted least squares estimation with bootstrapped standard errors using 10,000 bootstrap draws was specified.
Results
As shown in Table 1, the sample was diverse with regards to racial and ethnic background, HIV status, employment, and education. The majority of the sample identified as gay, queer, or homosexual and the majority were single. The sample ranged in age from 18 to 73 years, with an average age of 37. Nearly half (48.9 %) of this highly sexually active sample was classified as Neither SC nor HD, 30.0 % were classified as SC Only, and 21.1 % were classified as Both SC and HD.
Table 1.
Demographic Characteristics of the Sample (N = 368)
| n | % | |
|---|---|---|
| Race/ethnicity | ||
| Black | 74 | 20.1 |
| Latino | 50 | 13.6 |
| White | 186 | 50.5 |
| Asian/Native Haw./Pac. Islander | 43 | 11.7 |
| Other/Multiracial | 15 | 4.1 |
| HIV status | ||
| Negative | 206 | 56.0 |
| Positive | 162 | 44.0 |
| Sexual orientation | ||
| Gay, queer, or homosexual | 324 | 88.0 |
| Bisexual | 44 | 12.0 |
| Employment status | ||
| Full-time | 118 | 32.1 |
| Part-time | 93 | 25.3 |
| On disability | 48 | 13.0 |
| Student (unemployed) | 32 | 8.7 |
| Unemployed | 77 | 20.9 |
| Highest educational attainment | ||
| High school diploma or GED | 41 | 11.1 |
| Some college or Associate’s degree | 115 | 31.3 |
| Bachelor’s or other 4-year degree | 123 | 33.4 |
| Graduate degree | 89 | 24.2 |
| Relationship status | ||
| Single | 294 | 79.9 |
| Partnered | 74 | 20.1 |
|
| ||
| M | SD | |
|
| ||
| Age (in years) | 36.8 | 11.4 |
The three SC/HD groups were compared on the extent to which they experienced each of the syndemic conditions, and the results are shown within Table 2 as well as graphically in Fig. 1. As depicted, the three groups differed significantly on the experience of IPV and depressive symptoms. Post hoc analyses revealed that a significantly smaller proportion of the Neither SC nor HD group had experienced IPV when compared with the Both SC and HD group. Conversely, the Neither SC nor HD group differed significantly from both the SC Only and Both SC and HD groups on depressive symptoms, with nearly 30 % more men experiencing depressive symptoms in the latter two groups. The differences across the three groups with regard to the least frequently endorsed syndemic factors, CSA and poly-substance use, showed a similar pattern, but failed to reach statistical significance. Finally, as shown in Table 2, results suggested that all three groups significantly differed on their mean number of syndemic conditions and the pattern indicated that the number of syndemic conditions increased across the three levels of SC/HD severity. Specifically, the Both SC and HD group was significantly higher than the SC Only (p = .03) and Neither SC nor HD (p<.001) groups, and the SC Only group was higher than the Neither SC nor HD Group (p =.001).
Table 2.
Group differences in individual and total number of syndemic conditions
| Syndemic condition | Neither SC nor HD (n = 181)
|
SC Only (n = 110)
|
Both SC and HD (n = 77)
|
χ2(2) | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Intimate partner violence | 98a | 54.1 % | 71a,b | 64.5 % | 58b | 75.3 % | 10.80** |
| Childhood sexual abuse | 26 | 14.4 % | 14 | 12.7 % | 19 | 24.7 % | 6.38† |
| Depression | 102a | 56.4 % | 91b | 82.7 % | 65b | 84.4 % | 32.22*** |
| Polysubstance use | 46 | 25.4 % | 32 | 29.1 % | 28 | 36.4 % | 3.16 |
|
| |||||||
| M | SD | M | SD | M | SD | F(2, 365) | |
|
| |||||||
| Number of Syndemic Conditions | 1.50a | 1.00 | 1.89b | 0.90 | 2.21c | 1.02 | 15.42*** |
Cells within the same row with superscripts of different letters differed significantly (p<.05) in post hoc analyses
p = .06;
p<.05;
p<.01;
p<.001
Fig. 1.
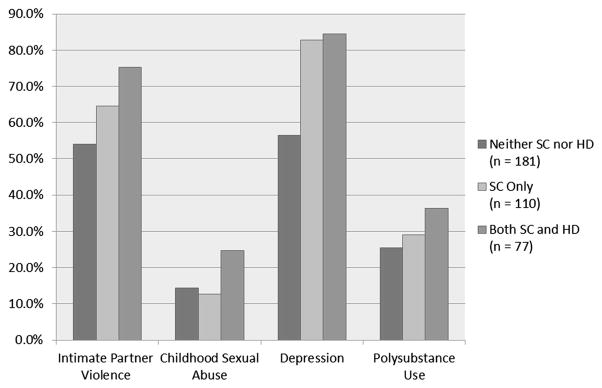
Comparisons of the proportion of men in the three SC/HD groups that experienced each of the syndemic conditions. Test statistics are reported in Table 1
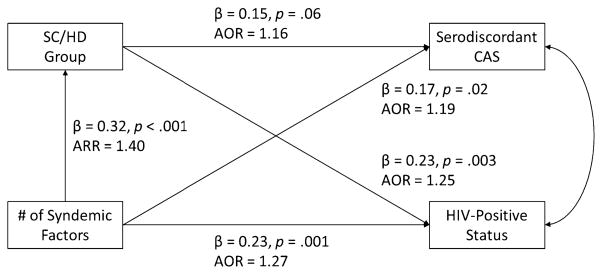
In the first path model, we tested for the role of syndemic conditions and SC/HD group on having CAS with a serodiscordant or unknown status partner and being HIV-positive. As can be seen in Fig. 2, the number of syndemic factors experienced by men was significantly associated with increased odds of both serodiscordant CAS as well as HIV-positive status, with each additional syndemic factor increasing the odds of serodiscordant CAS by approximately 20 % and the odds of being HIV-positive by 27 %. Moreover, syndemic factors were positively associated with the SC/HD group variable, with each additional syndemic factor increasing the odds of being 1-unit higher on SC/HD (i.e., going from Neither SC nor HD to SC Only or going from SC Only to Both SC and HD) by 40 %. Moving up by one unit on the ordinal SC/HD group variable had a marginally significant impact on whether or not men had engaged in serodiscordant CAS and was significantly associated with a 25 % increase in the odds of being HIV-positive.
Fig. 2.
Path model depicting the direct associations between syndemic factors, SC/HD group, and HIV risk outcomes. All beta coefficients displayed are standardized model effects and p values are based on bootstrapped standard errors
To examine whether there was any evidence that SC/HD group mediated the impact of syndemics on HIV risk outcomes, we calculated indirect effects with bootstrapped standard errors. Results suggested that SC/HD grouping did not act as a significant indirect pathway from syndemic factors to serodiscordant CAS (B = .05, p = .08). However, there was a significant indirect effect from syndemic factors to HIV-positive status through SC/HD group (B =.08, p =.01) and this accounted for 24 % of the total effect of syndemics on HIV-positive status.
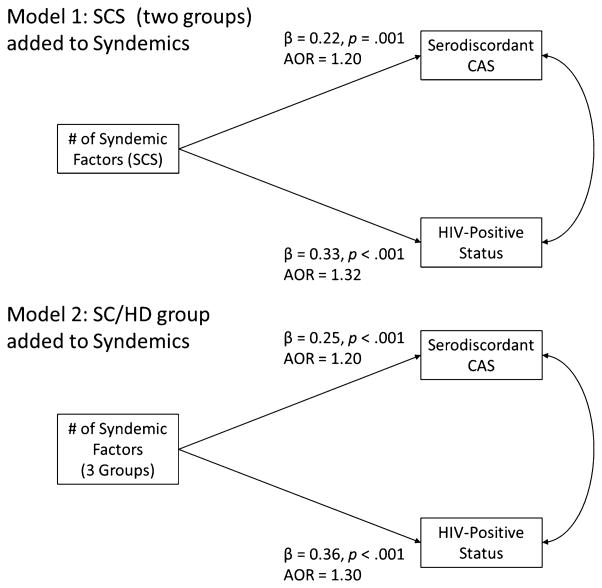
Given that we found significant associations between syndemic factors and SC/HD grouping as well as between SC/HD grouping and HIV risk outcomes but did not find strong evidence for SC/HD group serving an intermediary role between syndemics and HIV risk, we next conducted two models to examine whether SC/HD might contribute to HIV risk as a syndemic factor itself. In the first, we added a 1 to the existing syndemic variable for anybody who scored 24 or higher on the SCS; in the second, we added a 1 for those who reached the cutoff for the SCS but not the criteria for the HDSI (i.e., SC Only), and a 2 for those who met both (i.e., Both SC and HD). As can be seen in Fig. 3, the new syndemics variable was a significant predictor of both out-comes in each of the models and the impact of syndemics on both outcomes became meaningfully stronger, with standardized beta coefficients increasing by more than .05 in all cases when compared with the previous model in which SC/HD grouping was entered as a separate variable.
Fig. 3.
Comparing two models whereby SC or SC/HD group are added as syndemic factors in predicting HIV risk outcomes. All beta coefficients displayed are standardized model effects and p values are based on bootstrapped standard errors
In comparing the two models—one in which the SCS was considered alone and the second in which the SC/HD grouping was considered simultaneously—we utilized the total odds ratio as well as the standardized beta coefficients from Mplus. The value of the odds ratio is tied directly to the scale of the predictor variable to which it is associated—one can interpret this as being the change in odds associated with a one-unit increase in the predictor variable. As such, the re-scaling of the variable (going from a range of five to six) changes the overall meaning of the odds ratio and makes the AOR lack direct comparability across models. Examining the total odds ratio associated with going from the lowest group (i.e., 0 syndemic conditions) to the highest (i.e., 5 in the first model and 6 in the second) indicates that the former is associated with a 4.0 times increase in the odds while the latter is associated with a 4.8 times increase in the odds. As can be seen in Fig. 3, these standardized beta coefficients for the association between syndemics and HIV risk outcomes were strongest in the model in which the three-group conceptualization of SC/HD (β=0.36) was considered rather than that with SC alone (β=0.33). These results suggest that the SC/HD group added previously unexplained variance in HIV risk outcomes to the syndemics variable over and above even that which has been explained in previous models utilizing the SCS only.
Discussion
In these analyses, we found support for the utility of a three-group classification of sexual compulsivity/hypersexuality as one of the syndemic factors that contribute to HIV risk in a sample of highly sexually active GBM. Examining three groups that differed in their levels of SC/HD severity, we found that the average number of syndemic factors experienced was lowest among those who experienced neither SC nor HD and highest among the group that experienced both SC and HD, with those experiencing SC only falling between the two other groups. We found similar patterns when examining the proportion in each group who experienced each of the original four syndemic factors (Stall et al., 2003). We next examined two competing hypotheses—that SC/HD severity acted as a mediator of the syndemics-HIV risk association versus that SC/HD were syndemic factors themselves, as has been previously suggested (Parsons et al., 2012). These results provided additional support for the notion that sexual compulsivity/hypersexuality acts as a syndemic factor (i.e., contributes over and above the effects of the original factors included in the syndemics framework) and suggested that considering its severity as three distinct groups rather than two might be a more meaningful conceptualization.
In line with previous research (Parsons et al., 2015), this study supported the notion that sexual compulsivity/hypersexuality severity may be best conceptualized with three rather than two levels. Specifically, meaningful differences emerged between the three groups in the average number of syndemic conditions they experienced in general, as well as in the proportion of men in each group who experienced intimate partner violence and depressive symptoms. Though not statistically significant, similar patterns of results were found for CSA and polysubstance use. In all cases, the Neither SC nor HD group experienced the lowest levels of syndemic factors and the Both SC and HD group experienced the highest levels. However, the SC Only group at times appeared to have similar severity as the Neither SC nor HD group (e.g., with regard to CSA), at others appeared to be more similar to the Both SC and HD group (e.g., with regard to depressive symptoms), and still others appeared to be somewhere between the other two groups (e.g., with regard to IPV and polysubstance use). This echoes findings from previous analyses that suggested that research which has examined only the difference between men who did and did not experience SC may have been collapsing across two heterogenous groups with distinct psychosocial and behavioral profiles (Parsons et al., 2015). In essence, the Both SC and HD group would be considered as meeting criteria for diagnosis with problematic and compulsive sexual behavior, whereas the SC Only group could be considered “at risk” for the eventual development of a clinical problem in this area. Alternatively, the SC Only group could be simply manifesting low levels of or only one type of symptom rather than the elevated and multifaceted syndrome required to meet the threshold for classification with HD.
In addition to providing further evidence for the utility of a three-group conceptualizing of SC/HD severity, we sought to test whether the experience of SC/HD may be thought of as a result of syndemic conditions and, thus, potentially mediate the impact of syndemics on HIV risk or, conversely, whether it might be better considered to be a syndemic condition in-and-of itself. In doing so, we found support for a significant indirect pathway from syndemics to HIV-positive status through SC/HD severity, but not to serodiscordant CAS. In both cases, the indirect effects were substantially smaller than the direct effects. When examining the impact of adding sexual compulsivity/hypersexuality to the existing syndemics framework, we found that it not only strengthened the association between syndemics and both HIV risk outcomes, but also that these effects were strongest when considering three levels of SC/HD severity rather than only two (SC versus non-SC), as has been done in previous research.
Clinicians are already providing treatment for SC/HD, despite the lack of diagnostic criteria in the DSM-5. Many of these treatments utilize an addictions-based model (Rosenberg, Carnes, & O’Connor, 2014), and there has been some evidence for the utility of pharmacologic treatment (Wainberg et al., 2006). However, since previous studies have shown significant levels of co-morbidity between SC and depression and substance use disorders (both syndemic factors) among GBM (Morgenstern et al., 2011; Raymond, Coleman, & Miner, 2003; Scanavino et al., 2013), it may be that intervention approaches for these men should adopt a broader syndemics-focused approach, one in which the focus of treatment is not simply issues with SC/HD, but the full spectrum of syndemic factors. It has been suggested (Pachankis et al., 2014) that the minority stress model (Meyer, 2003) may provide a useful framework for this.
Minority stress refers to the stress that GBM are exposed to because of societal stigma, and it has been shown to play a role in other mental health problems among GBM (Hatzenbuehler, Nolen-Hoeksema, & Erickson, 2008; Pachankis & Bernstein, 2012). Since being exposed to minority stress can create problems with emotion regulation (Hatzenbuehler, Nolen-Hoeksema, & Dovidio, 2009; Pachankis & Bernstein, 2012), and sexual compulsivity/hypersexuality has been viewed as related to emotion regulation (Bancroft & Vukadinovic, 2004), it is possible that treatments which address stressors specific to GBM (such as internalized homonegativity) and emotion regulation, could effectively alleviate issues with SC/HD, depression, and substance use, there by addressing multiple syndemic conditions (Pachankis et al., 2014). In fact, not only may interventions designed for GBM that focus exclusively on one condition, such as depression, be inefficient, it is possible that behavioral interventions designed to reduce sexual risk among GBM have shown only modest results because they have failed to consider syndemic factors (Safren et al., 2015). A unified approach that addresses the connection between minority stressors faced by GBM and the likelihood of multiple syndemic conditions has been proposed (Pachankis, 2014), but this is clearly an area in which significant research is necessary to develop evidence-based approaches.
Limitations
The strengths of this study should be understood in light of its limitations. By study design, we set out to enroll a sample of GBM who were highly sexually active in New York City; consequently, our findings may not be generalizable to all GBM. Nevertheless, highly sexually active GBM represent an important subset of GBM with regards to risk for HIV and this group warrants further study. Our data were based on GBM’s self-reports on very sensitive topics (childhood sexual abuse, intimate partner violence, drug use, and HIV risk) and, therefore, some response bias may have been introduced. Although many scales demonstrated high internal consistency, we do not know if participants provided socially desirable responses and/or if they had problems with recall. In addition, although we utilized definitions of IPV and CSA that were consistent with prior syndemics research with GBM, there are several ways to operationalize these constructs (Paul et al., 2001) and we did not examine the extent to which differing definitions might alter the present findings. Lastly, although hypotheses were specified with language suggesting cause-and-effect, causal associations cannot be conclusively drawn from these findings given the observational and cross-sectional design of the study.
Conclusions
This study was conducted with a diverse sample of behaviorally similar, highly sexually active GBM. Building on previous research suggesting that both the SCS and HDSI are reliable and valid measures, but that their cutoffs provide unique rather than overlapping information (Parsons et al., 2013, 2015; Reid et al., 2012), this study represented the first of its kind to examine more than two levels of SC/HD severity within the syndemics model of HIV risk. As previous research has suggested (Parsons et al., 2012), this study provided further evidence that sexual compulsivity/hypersexuality is a contributing factor to the syndemics model of HIV risk and also that considering three levels of severity (i.e., SC along with HD) led to stronger model predictions than considering SC alone. A better understanding of the ways in which SC/HD severity adds to the negative impact of other syndemic factors (i.e., CSA, IPV, depression, polysubstance use) provides another modifiable target for intervention development. Moreover, the interrelation between the previous syndemic factors and SC/HD severity suggests that interventions that target one of these factors such as SC/HD may also meaningfully reduce the impact of other syndemic factors, thus potentially leading to decreases in HIV risk behavior.
Acknowledgments
This project was supported by a research Grant from the National Institute of Mental Health(R01-MH087714; Jeffrey T. Parsons, Principal Investigator). H. Jonathon Rendina was supported in part by a National Institute of Mental Health Ruth L. Kirchstein Individual Predoctoral Fellowship (F31-MH095622). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to acknowledge the contributions of the Pillow Talk Research Team: Brian Mustanski, John Pachankis, Ruben Jimenez, Demetria Cain, and Sitaji Gurung. We would also like to thank the CHEST staff who played important roles in the implementation of the project: Chris Hietikko, Chloe Mirzayi, Anita Viswanath, and Thomas Whitfield, as well as our team of recruiters and interns. Finally, we thank Chris Ryan, Daniel Nardicio, and Stephan Adelson and the participants who volunteered their time for this study.
References
- American Psychiatric Association’s DSM-5 Workgroup on Sexual and Gender Identity Disorders (APA) Hypersexual disorder screening inventory. 2010 Retrieved July 26, 2011 from http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=415#.
- Bancroft J, Vukadinovic Z. Sexual addiction, sexual compulsivity, sexual impulsivity, or what? Toward a theoretical model. Journal of Sex Research. 2004;41:225–234. doi: 10.1080/00224490409552230. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Pollack LM, Stall RD, Shade SB, Neilands TB, Rice TM, Moskowitz JT. Psychological processes and stimulant use among men who have sex with men. Drug and Alcohol Dependence. 2012;123:79–83. doi: 10.1016/j.drugalcdep.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E, Horvath KJ, Miner M, Ross MW, Oakes M, Rosser BS Men’s INTernet Sex (MINTS-II) Team. Compulsive sexual behavior and risk for unsafe sex among internet using men who have sex with men. Archives of Sexual Behavior. 2010;39:1045–1053. doi: 10.1007/s10508-009-9507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. Brief symptom inventory. Baltimore: Clinical Psychometric Research; 1975. [Google Scholar]
- Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, Stall R. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. Journal of Urban Health. 2012;89:697–708. doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlatte O, Hottes TS, Trussler T, Marchand R. Evidence of a syndemic among young Canadian gay and bisexual men: Uncovering the associations between anti-gay experiences, psychosocial issues, and HIV risk. AIDS and Behavior. 2014;18:1256–1263. doi: 10.1007/s10461-013-0639-1. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition with psychotic screen (SCID-I/P W/PSY Screen) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Greenwood GL, Relf MV, Huang B, Pollack LM, Canchola JA, Catania JA. Battering victimization among a probability-based sample of men who have sex with men. American Journal of Public Health. 2002;92:1964–1969. doi: 10.2105/ajph.92.12.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Golub SA, Mustanski B, Parsons JT. Sexual compulsivity, state affect, and sexual risk behavior in a daily diary study of gay and bisexual men. Psychology of Addictive Behaviors. 2010a;24:487–497. doi: 10.1037/a0020527. [DOI] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Archives of Sexual Behavior. 2010b;39:940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guadamuz TE, McCarthy K, Wimonsate W, Thienkrua W, Varangrat A, Chaikummao S, van Griensven F. Psychosocial health conditions and HIV prevalence and incidence in a cohort of men who have sex with men in Bangkok, Thailand: Evidence of a syndemic effect. AIDS and Behavior. 2014;18:2089–2096. doi: 10.1007/s10461-014-0826-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio J. How does stigma “get under the skin”? The mediating role of emotion regulation. Psychological Science. 2009;20:1282–1289. doi: 10.1111/j.1467-9280.2009.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: Results from a prospective study of bereaved gay men. Health Psychology. 2008;27:455–462. doi: 10.1037/0278-6133.27.4.455. [DOI] [PubMed] [Google Scholar]
- Herrick AL, Lim SH, Plankey MW, Chmiel JS, Guadamuz TT, Kao U, Stall R. Adversity and syndemic production among men participating in the Multicenter AIDS Cohort Study: A life-course approach. American Journal of Public Health. 2013;103:79–85. doi: 10.2105/AJPH.2012.300810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hook JN, Hook JP, Davis DE, Worthington EL, Jr, Penberthy JK. Measuring sexual addiction and compulsivity: A critical review of instruments. Journal of Sex and Marital Therapy. 2010;36:227–260. doi: 10.1080/00926231003719673. [DOI] [PubMed] [Google Scholar]
- Johnson AS, Hall HI, Hu X, Lansky A, Holtgrave DR, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. Journal of the American Medical Association. 2014;312:432–434. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kafka MP. Hypersexual disorder: A proposed diagnosis for DSM-V. Archives of Sexual Behavior. 2010;39:377–400. doi: 10.1007/s10508-009-9574-7. [DOI] [PubMed] [Google Scholar]
- Kafka MP. What happened to hypersexual disorder? Archives of Sexual Behavior. 2014;43:1259–1261. doi: 10.1007/s10508-014-0326-y. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: Validity, and predicting HIV risk behavior. Journal of Personality Assessment. 1995;65:586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Muench F, O’Leary A, Wainberg ML, Parsons JT, Hollander E, Irwin T. Non-paraphilic compulsive sexual behavior and psychiatric co-morbidities in gay and bisexual men. Sexual Addiction and Compulsivity. 2011;18:114–134. doi: 10.1080/10720162.2011.593420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muench F, Parsons JT. Sexual compulsivity and HIV: Identification and treatment. Focus. 2004;19:1–5. [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Leary A, Jemmott JB, Stevens R, Rutledge SE, Icard LD. Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS and Behavior. 2014;18:1991–1997. doi: 10.1007/s10461-014-0708-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE. Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology: Science and Practice. 2014;21:313–330. doi: 10.1111/cpsp.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Bernstein L. An etiological model of anxiety in young gay men: From early stress to public self-consciousness. Psychology of Men and Masculinity. 2012;13:107–122. [Google Scholar]
- Pachankis JE, Rendina HJ, Restar A, Ventuneac A, Grov C, Parsons JT. A minority stress–emotion regulation model of sexual compulsivity among highly sexually active gay and bisexual men. Health Psychology. 2014 doi: 10.1037/hea0000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Bimbi DS, Halkitis PN. Sexual compulsivity among gay/bisexual male escorts who advertise on the Internet. Sexual Addiction & Compulsivity. 2001;8:101–112. [Google Scholar]
- Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health. 2012;102:156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Archives of Sexual Behavior. 2008;37:817–826. doi: 10.1007/s10508-007-9218-8. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Kelly BC, Bimbi DS, Muench F, Morgenstern J. Accounting for the social triggers of sexual compulsivity. Journal of Addictive Diseases. 2007;26:5–16. doi: 10.1300/J069v26n03_02. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Rendina HJ, Ventuneac A, Cook KF, Grov C, Mustanski B. A psychometric investigation of the Hypersexual Disorder Screening Inventory among highly sexually active gay and bisexual men: An item response theory analysis. Journal of Sexual Medicine. 2013;10:3088–3101. doi: 10.1111/jsm.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Rendina HJ, Ventuneac A, Moody RL, Grov C. Hypersexual, sexually compulsive, or just highly sexually active? Investigating three distinct groups of gay and bisexual men and their profiles of HIV-related risk. AIDS and Behavior. 2015 doi: 10.1007/s10461-015-1029-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: The Urban Men’s Health Study. Child Abuse and Neglect. 2001;25:557–584. doi: 10.1016/s0145-2134(01)00226-5. [DOI] [PubMed] [Google Scholar]
- Raymond NC, Coleman E, Miner MH. Psychiatric comorbidity and compulsive/impulsive traits in compulsive sexual behavior. Comprehensive Psychiatry. 2003;44:370–380. doi: 10.1016/S0010-440X(03)00110-X. [DOI] [PubMed] [Google Scholar]
- Reid RC, Carpenter BN, Hook JN, Garos S, Manning JC, Gilliland R, Fong T. Report of findings in a DSM-5 field trial for hypersexual disorder. Journal of Sexual Medicine. 2012;9:2868–2877. doi: 10.1111/j.1743-6109.2012.02936.x. [DOI] [PubMed] [Google Scholar]
- Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and sexual compulsivity in a community-based sample of HIV-positive gay and bisexual men. AIDS and Behavior. 2012;16:741–750. doi: 10.1007/s10461-011-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg KP, Carnes P, O’Connor S. Evaluation and treatment of sex addiction. Journal of Sex and Marital Therapy. 2014;40:77–91. doi: 10.1080/0092623X.2012.701268. [DOI] [PubMed] [Google Scholar]
- Safren SA, Perry N, Blashill A, O’Cleirigh C, Ribaudo H, Mayer K. The cost and intensity of behavioral interventions to promote HIV self-care for high-risk HIV-positive MSM compared to the cost and intensity of standard HIV treatment. Archives of Sexual Behavior. 2015 doi: 10.1007/s10508-014-0455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos G-M, Do T, Beck J, Makofane K, Arreola S, Pyun T, Ayala G. Syndemic conditions associated with increased HIV risk in a global sample of men who have sex with men. Sexually Transmitted Infections. 2014;90:250–253. doi: 10.1136/sextrans-2013-051318. [DOI] [PubMed] [Google Scholar]
- Scanavino MDT, Ventuneac A, Abdo CHN, Tavares H, do Amaral ML, Messina B, Parsons JT. Compulsive sexual behavior and psychopathology among treatment-seeking men in São Paulo, Brazil. Psychiatry Research. 2013;209:518–524. doi: 10.1016/j.psychres.2013.01.021. [DOI] [PubMed] [Google Scholar]
- Schulte-van Maaren YW, Carlier IV, Zitman FG, van Hemert AM, de Waal MW, van Noorden MS, Giltay EJ. Reference values for generic instruments used in routine outcome monitoring: The Leiden Routine Outcome Monitoring Study. BMC Psychiatry. 2012;12:203. doi: 10.1186/1471-244X-12-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer MC. AIDS and the health crisis of the US urban poor: The perspective of critical medical anthropology. Social Science and Medicine. 1994;39:931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, Nicolaysen AM. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science and Medicine. 2006;63:2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: The Urban Men’s Health Study. Addiction. 2002;96:1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- Starks TJ, Millar BM, Eggleston JJ, Parsons JT. Syndemic factors associated with HIV risk for gay and bisexual men: Comparing latent class and latent factor modeling. AIDS and Behavior. 2014;18:2075–2079. doi: 10.1007/s10461-014-0841-9. [DOI] [PubMed] [Google Scholar]
- Ventuneac A, Rendina HJ, Grov C, Mustanski B, Parsons JT. An item response theory analysis of the Sexual Compulsivity Scale and its correspondence with the Hypersexual Disorder Screening Inventory among a sample of highly sexually active gay and bisexual men. Journal of Sexual Medicine. 2015;12:481–493. doi: 10.1111/jsm.12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainberg ML, Muench F, Morgenstern J, Hollander E, Irwin TW, Parsons JT, O’Leary A. A double-blind study of citalopram versus placebo in the treatment of compulsive sexual behaviors in gay and bisexual men. Journal of Clinical Psychiatry. 2006;67:1968–1973. doi: 10.4088/jcp.v67n1218. [DOI] [PubMed] [Google Scholar]
- Wim VB, Christiana N, Marie L. Syndemic and other risk factors for unprotected anal intercourse among an online sample of Belgian HIV negative men who have sex with men. AIDS and Behavior. 2014;18:50–58. doi: 10.1007/s10461-013-0516-y. [DOI] [PubMed] [Google Scholar]