Abstract
Widespread adoption of empirically-supported treatment innovations has the potential to improve effectiveness of treatment received by individuals with substance use disorders. However, the process of disseminating such innovations has been complex, slow, and difficult. We empirically describe the dissemination and adoption of a treatment innovation – an alcohol-treatment preparatory therapeutic procedure based on motivational interviewing (MI) – in the context of Rogers’ (2003) five stages of innovation-decision process (knowledge, persuasion, decision, implementation and confirmation). To this end, 145 randomly-chosen outpatient addiction treatment clinics in New York State received an onsite visit from a project trainer delivering one of three randomly-assigned dissemination intensities: a 15-minute, a half-day or a full-day presentation. Across these clinics, 141 primary administrators and 837 clinicians completed questionnaires assessing aspects of five innovation-decision stages. At each clinic, questionnaire administration occurred immediately pre- and post-dissemination, as well as one and six months after dissemination. Consistent with Rogers’ theory, earlier stages of the innovation-decision process predicted later stages. As hypothesized, dissemination intensity predicted clinicians’ post-dissemination knowledge. Clinician baseline characteristics (including gender, pre-dissemination knowledge regarding the MI preparatory technique, education, case load, beliefs regarding the nature of alcohol problems, and beliefs and behavior with regard to therapeutic style) predicted knowledge and persuasion stage variables. One baseline clinic characteristic (i.e., clinic mean beliefs and behavior regarding an MI-consistent therapeutic style) predicted implementation stage variables. Findings suggest that dissemination strategies should accommodate clinician and clinic characteristics.
Keywords: dissemination, adoption, addictions, treatment, innovation-decision process, motivational interviewing
1. Introduction
Improving the overall effectiveness of our nation’s alcohol and substance abuse treatment delivery system requires successful dissemination of empirically-supported treatment innovations. However, such empirically-supported approaches have been slow to gain acceptance and wide application in U.S. treatment programs (see Wilbourne & Weingardt, 2007). Recent research has improved our understanding of factors that affect the success of dissemination efforts (see, e.g., Gotham, 2004; Sorensen, Hettema & Chen, 2007). However, additional work is needed to describe the process of adoption that occurs following dissemination and to identify factors that can support or inhibit adoption.
1.1 The Innovation-Decision Process
Rogers (2003) articulates five stages through which individuals (or larger decision-making units) pass during the adoption of a novel idea -- the “innovation-decision” process. The first stage involves gaining knowledge about and exposure to the innovation. The second stage, persuasion, refers to the forming of favorable attitudes and beliefs regarding the innovation, in reaction to knowledge gained in the previous stage. The third, decision, reflects the development of behavioral intentions to implement the innovation. The fourth, implementation, references overt behavior. Finally, the confirmation stage includes the seeking of reinforcement of the decision that has been made and, if adopted, recognition of the benefits of the innovation. A key implication of Rogers’ formulation is that individuals are unlikely to exhibit behaviors consistent with adoption (e.g., use of a new therapeutic procedure) if they do not first come to believe that doing so would yield substantial advantages over their current practices. Thus, understanding factors that affect the early stages of adoption has the potential to substantially improve our ability to effectively disseminate therapeutic innovations.
Rogers (2003) observed that the speed with which an innovation is adopted is partly a function of potential adopters’ individual characteristics, such as personality traits, socioeconomic variables, and communication and leadership styles and skills (see also Gotham, 2004). Both Gotham and Rogers also have emphasized the impact that organizational characteristics such as leadership, overall climate and atmosphere, eagerness for change, degree of pessimism, and resistance can have on the innovation-decision process at both individual and organizational levels.
Building on these ideas, we propose that characteristics of individual clinicians (e.g., education, professional beliefs, and professional experience) will directly affect the knowledge, persuasion and confirmation stages of adoption, which largely reflect personal reactions to and beliefs about an innovation. In contrast, we propose that external influences and characteristics of organizations (e.g., size, population served, administrators’ professional beliefs, and organization milieu) will directly affect the decision and implementation stages, which encompass clinicians’ behavioral intentions and overt steps taken to make use of an innovation. For instance, a clinician may believe that a novel intervention approach will be useful because he finds it consistent with his own clinical style, but may choose not to implement the innovation because other clinicians at his workplace do not share his interest in learning about it and practicing its use.
Although several reports have applied innovation-decision and dissemination theory to work in the addictions (see Hartzler & Rabun, 2013; Laflin, Edmundson & Moore-Hirsch, 1995; Sharma, 2008), the model as a whole has not been directly and longitudinally tested in the context of substance abuse clinics. Such a test would improve our understanding of the process that ensues following efforts to disseminate an empirically-supported treatment innovation in the field of addictions treatment and has the potential to shed light on clinician and clinic characteristics that affect the adoption process in this context. Ultimately, insights gained from this research may point toward avenues for increasing the effectiveness of dissemination initiatives.
1.2 The Current Study
The first goal of the current study was to model the stages of the innovation-decision process with constructs assessed immediately following dissemination (knowledge, persuasion, and decision), one month post-dissemination (implementation), and six months post-dissemination (confirmation). The disseminated innovation was a specific preparatory therapeutic procedure that is based on motivational interviewing and has been shown to enhance outcomes of outpatient treatment for alcohol use disorders (Connors, Walitzer, & Dermen, 2002). Motivational interviewing (MI; Miller & Rollnick, 1991, 2002, 2013) is a form of brief intervention that was developed with the explicit goal of increasing client motivation to engage in healthy, adaptive behavior. Often adapted to incorporate the provision of personalized feedback regarding the client’s behavior (e.g., Miller, Sovereign, & Krege, 1988), MI has been used both as a stand-alone form of treatment for a variety of behavior change programs (e.g., Zweben & Zuckoff, 2002) and as a preparatory intervention for therapy (see Walitzer, Dermen, & Connors, 1999). Evidence for the efficacy of MI-based preparatory procedures has come from a large and still-growing set of clinical trials (Hettema, Steele, & Miller, 2005, Lundahl et al., 2010). Findings (e.g., Bien, Miller, & Boroughs, 1993; Brown & Miller, 1993) indicate that using MI-based procedures to prepare alcohol abusers for outpatient treatment can increase session attendance and reduce posttreatment heavy drinking. The procedure disseminated in the current study was tested in a clinical trial in which 126 clients (87 men, 39 women) scheduled for admission to a structured 12-week outpatient alcoholism treatment program were assigned randomly to one of three preparatory conditions: a role induction session, a session of MI (including presentation of personalized feedback), or a no-preparatory session control group (Connors, Walitzer, & Dermen, 2002). Clients assigned to the MI-based preparatory intervention attended more treatment sessions and had fewer heavy drinking days during treatment and in the year following treatment, and had more abstinent days during treatment and during the first three months posttreatment, relative to clients assigned not to receive a preparatory session. Outcomes of clients assigned to the role induction condition did not differ significantly from those assigned to the control group.
The second goal of the current study was to examine the differential impact of three levels of dissemination intensity on the innovation-decision process. We hypothesized that intensity of dissemination would directly affect the knowledge and persuasion stages of the innovation-decision process. Although successful dissemination of an MI-based preparatory procedure requires both that clinicians learn a new set of skills and procedures and that they competently implement those new skills and procedures with their clients, such skill development and implementation is unlikely to occur if clinicians are not first persuaded that the procedure can feasibly be implemented and is likely to have a positive impact on clients. Questions regarding how best to teach MI (e.g., Noonan & Moyers, 1997) have received empirical attention only recently (e.g., Baer et al., 2004; Bennett et al., 2007; Hartzler et al., 2007; Miller & Mount, 2001; Miller et al., 2004, 2008; Moyers et al., 2008; Shafer, Rhode, & Chong, 2004; Smith et al., 2007). Reviews of early studies in this area (Barwick, Bennett, Johnson, McGowan, & Moore, 2012; Madson, Loignon, & Lane, 2009) have found that general or introductory MI training presented in a seminar or workshop format usually succeeds in increasing clinicians’ MI-related knowledge and skills, although long-term maintenance of skills is likely to require some form of post-workshop support (Madson et al., 2009; Schwalbe et al., 2014; Walters et al., 2005). Only in recent years has work examined the extent to which clinicians incorporate the use of MI into regular clinical practice and investigated systematically the impact of training intensity or format on clinicians’ learning and adoption of MI (for example, see de Roten, Zimmermann, Ortega, & Despland, 2013).
The third goal of the current study was to examine clinician and clinic characteristics that influence the innovation-decision process. As reflected in the larger literature regarding potential facilitators of and barriers to adoption, several characteristics have been suggested as having a potential impact on adoption of MI and related methods. These include clinicians’ level of formal education, clinical orientation, pre-training beliefs regarding the potential value of MI, history of training in MI, post-training self-efficacy for use of MI and perceptions of program support for using MI, as well as the treatment agency’s tendency to reward autonomy and creativity among its staff and its administrators’ attitudes toward MI (Amodeo et al., 2011; Baer et al., 2009; Madson et al., 2009; Miller et al., 2008). Other clinic-level characteristics that may influence adoption include the proportion of the agency’s clients who belong to racial or ethnic minorities or have more severe addiction problems and the extent to which clients at a given agency tend to drop out early or have poor treatment outcomes (Carroll et al., 2006; Hettema, Steele, & Miller, 2005; Lundahl & Burke, 2009).
Clinician and clinic characteristics that have been identified as potentially influencing adoption of therapeutic innovations generally (beyond those identified specifically in relation to MI) include clinician age, gender, specialized certification, years of practice, caseload, and post-training ratings of the innovation’s relevance to clients’ needs and the desire for more training, as well as the extent to which there is a perceived need for the innovation at a given agency, the overall size of the agency’s caseload, and the extent to which staff and administrators at the agency are familiar with and endorse the innovation (Bartholomew et al., 2007; Beidas & Kendall, 2010; Haug et al., 2008; Henggeler et al., 2008; Miller, Sorensen, Selzer, & Brigham, 2006; Sholomskas et al., 2005; Story et al., 2002; Wiltsey Stirman, Crits-Christoph, & DeRubeis, 2004). For the current study, we also explored clinic characteristics such as the size of the treatment staff, the proportion of patients who are mandated to treatment or who have comorbid disorders, and administrators’ and clinicians’ beliefs regarding alcohol problems.
1.3 Hypotheses
Four sets of hypotheses were developed. First, we hypothesized that our data would be consistent with Rogers’ (2003) innovation-decision process model. Specifically, we expected that, immediately after training, clinicians’ knowledge levels would predict the extent to which they had been persuaded in favor of the innovation, which in turn would predict their having made a decision to implement the innovation. Decisions at post-training were then expected to predict self-reported implementation one month later, which in turn would predict confirmation of the decision six months after dissemination.
Second, we hypothesized that more intensive dissemination efforts would lead to greater increases in knowledge and resultant persuasion, relative to the effects of a low-intensity dissemination. The effects of training intensity on the remaining three stages (decision, implementation and confirmation) was expected to be indirect, mediated via knowledge and persuasion.
Third, we hypothesized that individual clinician characteristics measured at baseline would have direct influences on the knowledge, persuasion, and confirmation stages, as these stages represent personal reactions to and beliefs about the innovation.
Fourth, and in contrast, we hypothesized that clinic characteristics, including aspects of the clinic milieu as reflected in the aggregation of clinician characteristics at each clinic, would have direct influences on the decision and implementation stages, as these stages represent intentions to act and overt steps taken toward adoption, which seem more likely to be affected by external factors.
2 Materials and methods
2.1 Clinic eligibility and recruitment
Clinics eligible for the study met the following criteria: (1) licensed by the New York State Office of Alcoholism and Substance Abuse Services (OASAS) to provide outpatient services; (2) had, as reported by OASAS, a minimum of 3 FTE counseling staff; and (3) had, as reported by OASAS, a minimum of 50% of their clinical intakes with clients who reported alcohol as a primary or secondary problem substance.
At the onset of recruitment, 321 licensed clinics met these eligibility criteria. A randomly ordered list of these clinics was created, and recruitment attempts occurred in that order. During the period of March, 2006 through June, 2008, 231 clinics were invited to participate. Recruitment occurred via an introductory letter to the clinic’s administrator describing the experimental condition to which the clinic had been assigned, followed by a telephone call to the administrator. At the time of contact, nine clinics were determined to be ineligible and four had ceased operation. Of the remaining 218 eligible clinics that were contacted, 145 (66%) participated in the research project, 45 (21%) declined, and 28 (13%) did not respond.
2.2 Clinician eligibility and recruitment
All employed clinical staff at each participating clinic were invited to participate in study presentations and research. The presentation component was approved by OASAS to provide required continuing education credits, resulting in high levels of clinical staff participating in the presentation and research. It was not possible, however, to determine the overall proportions of staff participating at each clinic, because of ambiguities and complexities associated with determining the number of clinical staff employed at a given clinic.
Eight hundred seventy-two individuals provided informed consent and completed the baseline questionnaire. For purposes of the present paper, participants were included in analyses if they met either of two criteria: (1) they reported employment at the clinic as a “clinician/therapist/counselor” (as opposed to, e.g., nursing staff, intern, administrative staff), or (2) they reported experience “working as an addictions counselor.” Eight hundred thirty-seven substance abuse counselors met at least one of these two inclusion criteria. Clinics had a range of 1 to 21 consenting and eligible clinicians (M = 6.0, SD = 3.3).
2.3 Procedures
Eligible clinics were randomly assigned to one of three conditions (differing in intensity of dissemination) via urn randomization, taking region of New York State (five regions designated via population and location) and clinic size (each clinic’s new client census) into account to ensure that these two factors were evenly distributed across the three conditions. The experimental conditions were as follows: (1) Clinician Guides plus a 15-minute presentation (Guide-only; n = 50 clinics), (2) Guides plus a 3.5-hour presentation (Half-day; n = 47 clinics), and (3) Guides plus a 6.5-hour presentation and the offer of an individual 30-minute telephone consultation for each clinician three weeks later (Full-day; n = 48 clinics). In designing the study, the Full-day condition was considered to represent the maximum length training that was likely to be accepted by a majority of clinics. The Half-day condition was chosen as a more practical alternative that would be similar in length to training sessions typically offered at the clinics, but would serve as a reasonable introduction to the MI-based preparatory procedure. The Guide-only condition served as the control, comparison condition.
All clinics received an on-site visit by one of four project trainers; each trainer conducted presentations for all three dissemination conditions. Just prior to each presentation, administrators and clinicians who consented to participate in the research study completed a set of baseline questionnaires. Participants were asked to complete additional measures again immediately after the presentation. Follow-up assessments were conducted via mail at one and six months after the presentation. Clinicians received $5.00 remuneration for each post-presentation assessment completed.
All presentation attendees (clinicians and administrators) received a 154-page Clinician’s Guide, developed for this study, that contained general information on MI principles and methods, specific information on how to conduct a preparatory session using MI, and a list of educational resources regarding these methods. Clinic administrators also received a 15-page Administrator’s Guide that contained additional information on ways in which program directors and supervisors can facilitate implementation of preparatory sessions.
All presentations offered a description of and rationale for conducting a preparatory session using MI and provided an overview of MI principles and methods. (Materials used in the trainings are available from the first author upon request.) In terms of skills needed to conduct MI (as described by Miller & Moyers, 2006), the presentations primarily highlighted the importance of taking a collaborative stance with clients, using client-centered counseling methods, recognizing, eliciting, and reinforcing change talk, and rolling with resistance. In the Half-day and Full-day presentations, trainers sought to elicit from attendees their own reasons for considering the use of MI-based preparatory procedures, made use of a mixture of didactic, demonstration, and participatory (e.g., roleplay) methods to introduce attendees to the material, and engaged trainees in a discussion of how they might continue the learning process and apply what they had learned. Relative to Half-day presentations, the Full-day presentations included extended discussions of how MI was developed and the key principles and methods associated with MI and made greater use of group exercises and roleplay opportunities. The primary goal in all three dissemination conditions was to increase participants’ motivation to learn more about the use of MI-based preparatory procedures and to implement these methods with their clients.
2.4 Trainers
Development of the training protocols and training of project trainers was led by the second author, an experienced MI trainer and supervisor, with assistance from the first and third authors. All four trainers were female, master’s-level professionals with experience in substance abuse counseling and motivational interviewing. Three of the trainers participated in initial development and refinement of the dissemination training protocols and materials, and all participated in extensive didactic preparation, role play, and observed practice trainings conducted at local substance abuse treatment facilities. Over the course of the project, trainers met periodically with the third author to discuss issues that arose during the trainings and to reinforce adherence to the training protocol.
2.5 Measures
2.5.1 Baseline clinician characteristics
Variables assessed in the baseline questionnaire administered to clinicians included: (1) gender (coded 0 = female, 1 = male); (2) professional history (education; years as an addictions counselor; whether the clinician held a substance abuse counseling certification; years working at the facility); (3) professional role (whether the clinician conducted intakes; caseload); (4) the Understanding of Alcoholism Scale (UAS; Humphreys, Greenbaum, Noke, & Finney, 1996; Moyers & Miller, 1993, using an 8-item disease model subscale, alpha = .76, an 8-item psychosocial model subscale, alpha = .68, and a 3-item moral/spiritual model subscale, alpha = .71, with response options (coded from 1 to 5) ranging from “strongly disagree” to “strongly agree”; (5) whether the clinician had received previous instruction in MI; (6) knowledge regarding MI and its use in the preparatory procedure (see below) and (7) innovation-related beliefs and self-reported behaviors (see below).
Because standardized, psychometrically evaluated measures for assessing most constructs of interest were unavailable at the time that the study protocol was being prepared (see Madson et al., 2009), several of the assessment instruments administered were created specifically for use in this study. The knowledge test (Walitzer, Dermen, Barrick, & Shyhalla, 2009) consisted of 12 true-false items (e.g., “A confrontive therapeutic style is consistent with the principles of motivational interviewing” [false]; “A main goal of a preparatory session using motivational interviewing is to strengthen the client’s commitment to change” [true]). The beliefs/behavior measure consisted of two subscales developed for this study -- one assessing beliefs and behaviors consistent with using MI as a therapeutic style with new clients (14 items total, alpha = .79), the second assessing beliefs and behaviors consistent with using a confrontive therapeutic style with new clients (6 items, alpha = .74). Belief items assessed the perceived importance and helpfulness of the relevant clinical behaviors (e.g., “I believe it is helpful to use a confrontive style when talking with my clients about their alcohol or other drug addiction.”) and employed an ordinal response set (coded from 1 to 5) ranging from “strongly disagree” to “strongly agree.” Behavior items assessed frequency of use of the behaviors with new clients during the first few treatment sessions (e.g., “I emphasize my clients’ right to make their own choices with regard to drinking, drug use, and participation in treatment”) and employed an ordinal response set (coded from 1 to 5) linked to the following descriptors: “never,” “1/4 of the time,” “1/2 of the time,” “3/4 of the time,” and “always.”
2.5.2 Baseline clinic characteristics
Baseline characteristics of participating clinics were assessed in the following domains: (1) patient population (OASAS data regarding the percentage of clients who were mandated to treatment, carried a comorbid diagnosis, received a premature discharge, and were discharged with poor outcomes; primary administrator reports of the number of active outpatient clients and the number of intakes completed in the past month); (2) size of the clinic’s treatment staff (primary administrator report of full-time-equivalent therapist staffing; number of clinicians who attended the dissemination session); (3) therapeutic milieu with respect to beliefs about alcoholism (primary administrator scores on the three UAS-derived subscales; clinic means of clinician scores on these subscales); (4) therapeutic milieu with respect to familiarity with the intervention (whether the primary administrator had ever received MI instruction; proportion of clinicians who ever received MI instruction; clinic mean clinician knowledge score); and (5) therapeutic milieu with respect to innovation-related beliefs and behaviors (primary administrator beliefs; clinic mean clinician beliefs and behaviors).
2.5.3 Stage variables
Consistent with Rogers’ model of innovation-decision making (see Table 5–1 in Rogers [2003]), clinician adoption of the innovation was hypothesized to progress through the following stages: knowledge, persuasion, decision, implementation, and confirmation. Measures pertaining to the first three stages were administered to clinicians immediately following the dissemination session. The knowledge stage was represented by (1) the knowledge test score and (2) perceived self-efficacy for conducting a preparatory session using MI (e.g., “I have the skills to conduct a preparatory session using motivational interviewing;” 3 items, alpha = .83). The persuasion stage was represented by (1) beliefs with respect to the perceived importance and helpfulness of engaging in MI-consistent behavior with new clients (measured by repeating the seven relevant belief items originally administered prior to dissemination, alpha = .85) and (2) beliefs regarding the clinic’s support for using MI-related preparatory procedures with new clients (e.g., “I believe that this clinic would support setting aside time during the first few sessions to conduct a preparatory session using motivational interviewing;” 3 items, alpha = .81). The decision stage was represented by (1) intention to learn more about using MI-related preparatory procedures (by reading the Clinician’s Guide and seeking out other MI-related information or training; 2 items; alpha = .80) and (2) intention to incorporate some or all of the elements of the preparatory session using motivational interviewing into clinical practice (2 items; alpha = .83). Response options for the above scales (except knowledge) were coded from 1 to 5 and ranged from “strongly disagree” to “strongly agree.”
Measures pertaining to the implementation stage were administered one month after the date of the dissemination session. This construct was represented by (1) an index of time spent learning about MI and related preparatory procedures during the prior month (e.g., “reading the Clinician’s Guide,” 6 items with response options coded 1 to 5, ranging from “0 hours” to “11 or more hours”; alpha = .77) and (2) past-month frequency of engaging in MI-consistent clinical behaviors (e.g., “I emphasize my clients’ right to make their own choices with regard to drinking, drug use, and participation in treatment.”) with new clients during the first few treatment sessions (measured by repeating the seven relevant behavior items originally administered prior to dissemination; alpha = .79). Finally, the confirmation stage was represented by a scale, administered six months after dissemination, measuring the extent to which the clinician sees a benefit to conducting a preparatory session using MI (e.g., “setting aside part of the first few sessions to conduct a preparatory session using motivational interviewing would be a good use of time;” 3 items, alpha = .87).
2.6 Data analytic strategy
Structural equation modeling (MPlus 6.11) was used to evaluate: (1) the extent to which the data were consistent with the Rogers’ innovation-decision process model, (2) the effects of intensity of dissemination on the knowledge and persuasion stages, (3) the impact of individual clinician characteristics on the knowledge, persuasion, and confirmation Stages, and (4) the impact of aggregate clinic characteristics on the decision and implementation stages. Nine stage variables (two variables representing each of knowledge, persuasion, decision, and implementation; one variable representing confirmation) were proposed a priori, and 14 paths between those stage variables were hypothesized. Two dummy-coded variables describing dissemination condition assignment (i.e., HALF being Guide-only vs. Half-day; FULL being Guide-only vs. Full-day) were each hypothesized to have effects on the first two stages of the model. Finally, at the outset, 14 clinician characteristics and 21 clinic characteristics were considered for inclusion in the model.
Because clinicians are nested within clinics, we considered conducting analyses within a multilevel framework. However, because the average number of participating clinicians per clinic in our analyzed data was small (mean = 5.16), we expected nesting to have a negligible impact. Combining information on average cluster size with stage-variable intraclass correlations (which ranged from 0.000 [for six of the nine variables] to a maximum of 0.104) yielded a maximum design effect (indicating the effect of independence violations on standard error estimates) of 1.43. Design effect estimates greater than two are considered by some researchers to indicate a need for multilevel modeling (Peugh, 2010); design effects of two or less are considered small (Maas & Hox, 2005).
Construction and evaluation of the model took place in four phases. Phase 1 involved testing of the basic structure of Rogers’ innovation-decision process by assessing relationships among the nine stage variables. As such, a model that initially included all 14 hypothesized paths between adjacent stages was evaluated. Nonsignificant paths were deleted through an iterative process in which, at a given iteration, the path with the smallest standardized loading was eliminated and the coefficients between the remaining stage variables were recalculated. However, non-significant paths were retained if their elimination would leave all variables at a given stage disconnected from all prior or concurrent stage variables. Candidate paths between nonadjacent stages (e.g., from knowledge directly to decision) were added when consistent with theory and supported by modification indices.
Phase 2 involved examination of the addition of the two dummy-coded dissemination condition assignment contrasts (HALF, FULL) to the model. Specifically, eight paths were added from these contrast variables to the Knowledge and Persuasion variables. An iterative process was again used to eliminate non-significant paths from the model.
Phase 3 involved testing the ability of the 14 clinician variables to predict the knowledge, persuasion, and confirmation stages of adoption. Of these 14, only those that had demonstrated bivariate Pearson correlations of at least |r| = .10 with at least one of the five variables corresponding to the relevant stages were tested in the model. The iterative process described above was again used to eliminate non-significant paths.
Phase 4 involved testing the ability of the 21 clinic-level variables to predict the decision and implementation stages of adoption. Of these 21, only those that had demonstrated bivariate Pearson correlations of at least |r| = .10 with at least one of the four variables corresponding to the relevant stages were tested in the model. The iterative process described above was again used to eliminate non-significant paths.
Missing data in each model were treated in a manner consistent with MPlus maximum likelihood procedures, with the assumption that such data were missing at random. Specifically, any case missing data on an exogenous variable at a given phase of model testing was deleted list-wise from that phase; cases that were missing data on endogenous variables were retained unless a participant was missing data for all endogenous variables. Thus, sample size differed across model iterations as a function of which variables were exogenous to each model.
In addition to the model-testing analyses described above, supplementary analyses were conducted to identify predictors of whether or not clinicians in the Full-day condition took advantage of the offer of a telephone coaching session scheduled to occur three weeks after the dissemination session. For these exploratory analyses, all 14 clinician baseline, 21 clinic-level baseline, and 6 knowledge, persuasion, and decision stage variables were individually tested as predictors using logistic regression, with post-dissemination contact with the trainer (yes or no) as the dependent variable. All significant predictors were then tested simultaneously to determine whether any contributed unique variance above and beyond that of all other predictors. Finally, three ordinary least-squares regression analyses were conducted to determine whether the presence or absence of post-dissemination contact with a trainer was predictive of the Implementation and Confirmation stage adoption variables.
3. Results
3.1 Differences between participating and nonparticipating clinics
As described in section 2.1, 145 eligible clinics participated in the research, whereas 73 either refused or did not respond. To identify potential sample bias associated with non-participation, chi-square tests and one-way analyses of variance (ANOVAs) were used to examine the association of participation status with 16 clinic-level variables: region of New York State, clinic size (staffing size, client load, etc.), client characteristics (e.g., primary and secondary disorders), and clinic setting. Three of the 16 analyses identified significant differences. The proportion of clients with a primary or secondary alcohol diagnosis was higher in participating clinics (75.6%; sd = 10.0%) than in non-participating clinics (71.9%; sd = 10.7%), F(1, 216) = 6.30, p = .013, whereas the number of vacant full-time equivalent (FTE) positions was lower at participating clinics (0.52 FTE; sd = 0.70) than at non-participating clinics (0.86 FTE; sd = 1.04), F(1, 216) = 8.06, p = .005. Participation rates also varied by region, χ2(4) = 12.02, p = .017. Across regions, rates ranged from 46.4% to 79.6%. However, additional analyses (results not shown) suggested that the effect of region was due, at least in part, to average differences across regions on the other two variables.
3.2 Description of primary administrators and clinics
Of the 145 clinics that enrolled, 141 had one or more administrator complete a pre-training questionnaire at the time of the on-site visit; a total of 242 administrators participated. For clinics with one participating administrator (n = 68), this individual was designated as the primary administrator. For clinics with multiple participating administrators (n = 73), a primary administrator was identified based on job title. The resulting sample of 141 primary administrators (Guide Only n = 48; Half-day n = 46; Full-day n = 47) included clinic directors (74%), assistant directors (5%), supervisors (8%), and individuals with other administrative titles (13%). Primary administrators reported having worked at their facility for an average of 9.8 years (sd = 7.4). Table 1 provides additional descriptive information about this group. Administrator characteristics did not differ as a function of dissemination condition. Primary administrators’ reports also revealed that the average size of the substance abuse treatment counseling staff at participating clinics was 7.2 FTE (sd = 4.5), the average number of active outpatient clients was 157.9 (sd = 117.9), and the average number of new client intakes per month was 45.3 (sd = 36.0).
Table 1.
Characteristics of Primary Administrators and Clinicians
| Primary Administrators | Clinicians | |
|---|---|---|
| n = 141 | n = 837 | |
| Gender | ||
| Male | 44.6% | 33.2% |
| Female | 55.4% | 66.8% |
| Age | 49.6 (9.3) | 45.7 (12.0) |
| Education (Highest Degree) | ||
| Doctoral (e.g., PhD, MD) | 9.4% | 1.8% |
| Master’s | 63.8% | 43.8% |
| Bachelor’s (e.g., BA, RN) | 18.8% | 28.2% |
| Associate’s | 4.3% | 15.5% |
| High School | 3.6% | 10.7% |
| Race | ||
| White | 89.8% | 78.4% |
| Black | 7.3% | 16.3% |
| Asian | 2.9% | 2.9% |
| Native American | 0.0% | 2.2% |
| Hawaiian | 0.0% | 0.3% |
| Hispanic | 5.1% | 11.4% |
| Alcoholism Treatment Certificate | 71.0% | 51.4% |
| Previous MI Instruction | 65.9% | 49.8% |
3.3 Description of counselors
A total of 837 substance abuse counselors completed a pre-training questionnaire (Guide Only n = 325; Half-day n = 242; Full-day n = 270). Eighty-four percent identified themselves as full-time clinical staff, 9% as part-time clinical staff, and 6% as other staff. On average, clinicians reported having worked at their facility for 4.9 years (sd = 5.4) and having worked as an addictions counselor for 8.5 years (sd = 7.4). Table 1 provides additional descriptive information. Clinician characteristics did not differ as a function of dissemination condition.
3.4 Model testing results
Data were available at post-dissemination, 1-month follow-up, and 6-month follow-up from 798 (95.3% of baseline), 593 (70.8%), and 478 (57.1%) clinicians, respectively. In phase 1, eliminating non-significant paths and adding theory-consistent paths supported by modification indices yielded a model comprised of the nine stage variables connected by 15 paths. Overall, data were consistent with the Rogers (2003) innovation-decision process, in that variables representing the first four stages (knowledge, persuasion, decision, implementation) significantly predicted the immediately subsequent stage, often with multiple paths. Four additional paths suggested by modification indices were found to be consistent with theory and thus were added to the model: “self-efficacy for adoption” (a knowledge stage variable) positively predicted “intend to incorporate” (a decision stage variable), “information recall” (a knowledge stage variable) negatively predicted “time spent learning” (an implementation stage variable), “acceptance of innovation” (a persuasion stage variable) positively predicted “perceived benefits of innovation” (the confirmation stage variable), and “time spent learning” (an implementation stage variable) positively predicted “use of innovation” (an implementation stage variable). The covariance between “intend to learn more” and “intend to incorporate” (decision stage variables) also was added, as suggested by the relevant modification index. Although a modification index suggested adding the direct effect of “perceived clinic support” (a persuasion stage variable) on the confirmation stage variable, no compelling theoretical rationale could be identified for its inclusion, so the path was not added. At the completion of phase 1, model fit was acceptable, χ2(19) = 101.2, p < .001; RMSEA = .074; CFI = .938; n = 789.
In phase 2, the effects of two dissemination condition assignment contrasts (HALF, FULL) on the knowledge and persuasion stage variables were tested. Both contrasts were found to be significant predictors of “information recall;” longer presentations (Half-day, Full-day) were associated with greater knowledge recall, relative to the brief presentation (Guide-only). The HALF contrast also predicted ‘perceived clinic support;” the Half-day presentation was associated with less perceived clinic support, relative to the brief presentation. (The path from the FULL contrast to perceived support was retained in the model to maintain interpretability of the HALF contrast, but was not significant.) Contrast effects on self-efficacy for adoption and acceptance of the innovation were not significant, so these paths were excluded from the model. Model fit at the completion of phase 2 was acceptable, χ2(32) = 135.9, p < .001; RMSEA = .064; CFI = .925; n = 795.
In phase 3, eight baseline clinician variables (the pre-presentation knowledge test, gender, education, caseload, UAS – disease model beliefs, UAS – moral/spiritual model beliefs, MI style behavior-beliefs, confrontive style behavior-beliefs) were tested as predictors of the knowledge, persuasion, and confirmation stage variables. All eight predicted at least one stage variable and were retained in the model. A modification index also suggested inclusion of a path from gender to “time spent learning” (implementation stage variable); this path was added to the model. Regression coefficients for retained paths from clinician to stage variables are provided in Table 2; paths are also depicted in Figure 1. Model fit at the completion of phase was good, χ2(91) = 201.9, p < .001; RMSEA = .040; CFI = .939; n = 762.
Table 2.
Standardized Regression Coefficients of Clinician and Clinic Characteristics’ Direct Effects on the Knowledge, Persuasion, and Implementation Stages of the Innovation-Decision Process in Final Model
| Knowledge Stage
|
Persuasion Stage
|
Implementation Stage
|
||||
|---|---|---|---|---|---|---|
| Self-Efficacy for Adoption | Information Recall | Perceived Clinic Support | Acceptance of Innovation | Time Spent Learning | Use of Innovation | |
| Clinician Characteristics | ||||||
| Gender | −.08* | - | - | - | .19*** | - |
| Knowledge test | - | .27*** | - | - | - | - |
| Education | - | .13*** | - | .06* | - | - |
| Caseload | - | −.10** | - | - | - | - |
| UAS – Disease Model Scale | .11** | - | - | .12*** | - | - |
| UAS – Moral/Spiritual Scale | - | −.24*** | - | −.09* | - | - |
| Motivational behavior-beliefs | .22*** | - | - | .51*** | - | - |
| Confrontive behavior-beliefs | −.31*** | −.18*** | - | −.49*** | - | - |
| Clinic Characteristics | ||||||
| Clinic mean motivational behavior-beliefs | - | - | - | - | .11** | .21*** |
Notes.
p < .05,
p < .01,
p < .001.
“-“ = path not included in final model. UAS = Understanding of Alcoholism Scale. Coefficients for other paths in the final model can be found in Figure 1.
Figure 1. Intensity of Dissemination and Clinician and Clinic Characteristics Affect Stages of the Innovation-decision Process.
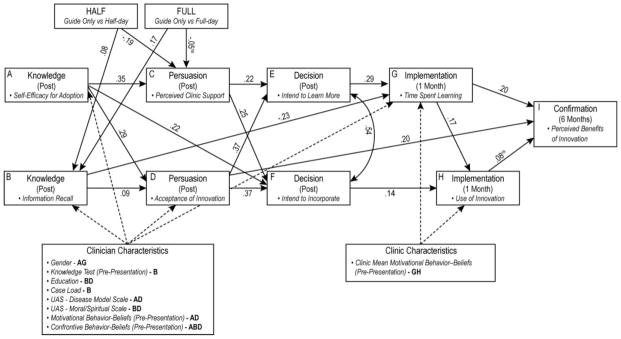
Standardized regression coefficients are significant (p < .001) unless marked not significant (ns). Solid lines represent direct paths between stage variables. Dotted lines represent direct paths from clinician and clinic characteristics to stage variables. Clinician and clinic characteristics noted with a capital letter have a significant (p < .05) direct effect on the stage variable with the same capital letter; these coefficients are presented in Table 2.
In phase 4, five clinic-level baseline variables representing therapeutic milieu (primary administrator’s prior MI training; clinic-level aggregated clinician scores on knowledge, psychosocial model beliefs, moral/spiritual model beliefs, and MI style behavior-beliefs) were tested as predictors of the decision and implementation stage variables. One of the five clinic-level variables predicted at least one of the stage variables and was retained in the model. Specifically, clinic mean MI style behavior-beliefs predicted the implementation variables “time spent learning” and “use of innovation.” Regression coefficients for these retained paths are presented in Table 2. Indices for the final model (depicted in Figure 1) indicated good fit; χ2(98) = 208.1, p < .001; RMSEA = .038; CFI = .940; n = 761.
3.5 Supplementary analysis results
3.5.1 Differences between trainers on stage variables
In order to evaluate whether the four trainers conducting the dissemination presentations differentially affected clinician scores on the knowledge, persuasion and decision stage variables (those assessed immediately following the trainings), ANOVAs were performed on these six stage variables with trainer (coded 1 through 4) as the independent variable, within each of the three dissemination conditions. In evaluating these tests, a Bonferroni-corrected alpha was applied to minimize Type I error. These tests yielded one significant finding; within the Full-day intensity condition, clinicians’ post-dissemination scores on the “information recall” knowledge variable differed as a function of trainer, F(3, 258) = 5.36, p = .001. Across the four trainers, mean scores ranged from 8.14 (sd = 2.34) to 10.63 (sd = 1.44). No other tests were significant.
3.5.2 Pre-presentation to post-presentation changes in information recall
One measure used to represent a stage variable – information recall – had also been administered at baseline. A paired t-test on pre- and post-dissemination scores demonstrated that knowledge regarding MI and its use in a preparatory procedure increased from pre- (mean = 7.77, sd = 2.41) to post-dissemination (mean = 10.13, sd = 1.77), t(774) = −28.53, p < .001.
3.5.3 Effects of HALF vs. FULL contrast on knowledge and persuasion stage variables
To supplement our Phase 2 model testing, which contrasted the effects of both the half-day and full-day training conditions on knowledge and persuasion stage variables against those of the Guide-only condition, we conducted t-tests that directly compared the effects of the half-day condition with those of the full-day condition. These tests revealed a significant difference between conditions in their effects on perceived clinic support, t (480) = −3.382, p = .001, but not on the other three stage variables. Clinicians who received the full-day training perceived significantly higher levels of support for adoption (M = 3.78, SD = 0.72) than did those who received the half-day training (M = 3.54, SD = 0.86).
3.5.4 Predicting telephone consultation contact with clinicians (Full-day condition)
Among clinicians who received the Full-day presentation, 40% took advantage of the offered telephone consultation. Logistic regression analyses (testing each potential predictor separately) showed that none of the 14 baseline clinician variables were predictive of post-dissemination contact with the trainer. Of the 21 baseline clinic-level variables, 11 were found to be significantly predictive. As shown in Table 3, predictors of an increased likelihood of clinician contact with the trainer included the primary administrator’s positive beliefs regarding the value of a confrontive style of working with clients, the clinic mean of clinicians’ knowledge regarding MI and the preparatory procedure, and the percentage of clients at the clinic who were mandated to treatment. Predictors of a decreased likelihood of clinician contact with the trainer included the primary administrator’s endorsement of a psychosocial model of alcoholism and positive beliefs regarding the value of a motivational interviewing style of working with clients, the clinic means of clinicians’ endorsement of a moral/spiritual model of alcoholism, positive beliefs regarding the value of a motivational interviewing style of working with clients, and positive beliefs regarding the value of a confrontational style of working with clients, as well as the percentage of clients at the clinic who received a premature discharge from the program and the percentage of clients at the clinic who were discharged with poor outcomes, and the size of the clinic’s active outpatient population.
Table 3.
Predictors of Telephone Consultation Contact within Full-Day Dissemination Intensity
| Predictor
|
B (SE)
|
Wald χ2(df)
|
Significance
|
|---|---|---|---|
| Percentage of clients mandated to treatment | 2.085 (0.671) | 9.67 (1) | p < .01 |
| Clinic mean of the clinician Knowledge Test scores | 0.382 (0.101) | 14.40 (1) | p < .001 |
| Primary Administrator beliefs/behaviors consistent confrontive therapeutic style | 0.456 (0.147) | 9.58 (1) | p < .01 |
| Percentage of clients who receive a premature discharge from program | −1.387 (0.550) | 6.35 (1) | p < .05 |
| Percentage of clients who are discharged with poor outcomes | −3.323 (1.001) | 11.01 (1) | p = .001 |
| Number of currently active outpatients | −0.003 (0.001) | 4.21 (1) | p < .05 |
| Clinic mean of the clinician UAS-derived Moral/Spirituality scores | −1.115 (0.343) | 10.57 (1) | p = .001 |
| Clinic mean of the clinician beliefs/behaviors of the MI-based procedures | −0.593 (0.291) | 4.15 (1) | p < .05 |
| Clinic mean of the clinician beliefs/behaviors of a confrontive therapeutic style | −0.416 (0.159) | 6.84 (1) | p < .01 |
| Primary Administrator score on UAS Psychosocial Model subscale | −0.765 (0.232) | 10.85 (1) | p = .001 |
| Primary Administrator beliefs of the MI-based procedures | −1.272 (0.373) | 11.61 (1) | p = .001 |
| Persuasion Stage Variable: Perceived Clinic Support | 0.476 (0.189) | 6.31 (1) | p < .05 |
Note. Results are from testing each predictor in a separate equation.
Of the six stage variables measured immediately after the dissemination session, only one was predictive. Clinicians who had stronger beliefs that their clinic’s support for using MI-related preparatory procedures with new clients were more likely to have post-dissemination contact with the trainer.
Combining the above significant predictors into a single, simultaneous logistic regression equation revealed that perceived clinic support was the only unique positive predictor, B = .590, Wald statistic (1 df) = 6.475, p = .011, and clinic-mean endorsement of a moral-spiritual model of alcoholism the only unique negative predictor, B = −.834, Wald statistic (1 df) = 4.137, p = .042, of contact with the trainer. Least-squares regression analyses revealed that the presence or absence of clinician contact with the trainer was not predictive of the clinicians’ time spent learning MI and preparatory procedures or extent of engagement in MI-consistent clinical behaviors during the month after the dissemination session, nor was it predictive of clinicians’ perceptions of benefits to conducting a preparatory session using MI, as measured at the six-month post-dissemination assessment.
4. Discussion
4.1 Evaluating the Innovation-Decision Process Model
Consistent with Rogers’ model, variables representing the knowledge, persuasion, decision, and implementation stages of the innovation-decision process directly predicted immediately subsequent stage variables. This set of findings further supports the utility of Rogers’ model for understanding adoption of innovations in addictions treatment. However, additional relationships present in our data suggest possibilities for expansion of Rogers’ model.
The direct path from self-efficacy to intentions suggests that the effect of clinicians’ confidence in their ability to implement an innovation on plans to do so does not depend entirely on the extent to which they are persuaded of its usefulness. More generally, the great extent to which self-efficacy both directly and indirectly affects downstream aspects of adoption highlights its importance as a key target of dissemination efforts. On the other hand, the direct negative effect of post-training information recall on time spent learning about the innovation during the following month suggests that clinicians who learned more during the workshop felt that the materials available to them did not provide additional useful information beyond that which they already possessed, although post-dissemination recall was also positively related to learning through its influence on acceptance and intentions to learn more about the innovation. This finding seems to echo an early training experience recently described by Bill Miller, who stated that “after the training, participants were somewhat less interested in learning more about MI. Why? ‘Because we have already learned it!’” (Miller, 2014; see also Miller & Mount, 2001).
The finding that clinicians’ immediate post-training level of acceptance of the innovation positively predicted such attitudes assessed six months later, independent of intermediate stage variables, suggests that dissemination efforts have the potential to yield a stable increase in clinicians’ receptivity toward an innovation, even among those who do not immediately implement the innovation.
4.2 Influences of workshop intensity on the innovation-decision process
The effects of longer workshops, relative to those of simply providing a brief introduction to the clinician guide, were less extensive than hypothesized and in one respect seem counterintuitive. The only effect of intensity that conformed to prediction was represented by the finding that both the half-day and full-day presentations had stronger effects on information recall than the guide-only presentation. Moreover, looking at the model as a whole, it appears that the sole mechanism by which half-day and one-day training workshops had an impact on adoption was by improving clinicians’ factual recall of information about the innovation.
The absence of a workshop effect on self-efficacy is unsettling, given the earlier noted pervasive influence of self-efficacy on adoption. Perhaps any potential increase in self-efficacy that may have resulted from participating in the longer workshops was counterbalanced by clinicians in those workshops developing a more accurate sense of the additional training and practice that would be required to develop competence in MI and its use in a preparatory session. In a similar vein, findings that the half-day presentation led to less perceived clinic support relative to receiving either just the guide or the full-day presentation suggest that the half-day presentation offered clinicians just enough information to alert them to the complexity and challenges of the innovation without fully illustrating its advantages and applicability, and that this imbalance left clinicians doubtful that their clinics would support implementation. In the full-day condition, the awareness of potential obstacles may have been counterbalanced by extended discussion of the methods used in a preparatory session and more extensive use of group exercises and roleplay, as well as the prospect of receiving a post-training phone consultation.
4.3 Influences of clinician and clinic characteristics on the innovation-decision process
Given the limited positive impact of dissemination intensity on adoption, the breadth and strength of relationships between baseline clinician characteristics and post-training adoption is especially striking. Overall, present findings are consistent with past research in suggesting that clinicians who hold pre-training beliefs and behaviors supportive of the innovation are more likely to evidence subsequent adoption, whereas those committed to a clinical approach inconsistent with the innovation are less likely to put it to use (e.g., Carpenter et al., 2012; see also Schumacher, Madson, & Nilsen, 2014).
Findings that clinicians who knew more about MI prior to the training had better recall of MI information after training, and that clinicians who endorsed and reported use of MI at baseline evidenced greater post-training self-efficacy and greater acceptance of the innovation, are consistent with past research showing that pre-training skill level positively predicts clinician proficiency following training in MI (Baer et al., 2004; Rash, et al., 2013). Such research has shown that clinicians who became proficient after training in MI had stronger skills prior to training (Baer et al., 2004) and that clinicians who had positive attitudes toward an innovation were more likely to adopt the innovation (Henggeler et al., 2008). Staff ratings of motivational enhancement therapy (MET) have been found to correlate positively with its perceived effectiveness (Herbeck et al., 2008), and allegiance to MI at baseline has been found to predict continued interest, confidence, and commitment with respect to MI after training in MI (Decker & Martino, 2013). Taken together, these findings are consistent with past research identifying a strong positive relationship between knowledge and perceptions of innovations and their adoption (Wiltsey Stirman et al., 2004).
In contrast, the findings that clinicians with a confrontive baseline style learned less and reported lower self-efficacy and less favorable attitudes toward the innovation, suggests that such clinicians had less interest in learning and using MI and recognized that to do so would have required a significant shift from their preferred style of interacting with clients. In prior research, staff resistance to, struggles with, and philosophical conflicts with MI have been found to be among the most frequently identified barriers to its adoption (Amodeo et al., 2011).
Although not surprising, findings showing strong effects of baseline clinician characteristics represent a continuing, unmet challenge to dissemination efforts. One approach to addressing this challenge involves tailoring training to take into account clinicians’ baseline familiarity and comfort with MI (e.g., see Decker & Martino, 2013; Martino et al., 2011). For example, previous research indicating that the correction of persistent misperceptions regarding an innovation may be related to knowledge gain (Rash et al., 2013) suggests that the addition of training components designed to identify and address such misunderstandings may improve dissemination outcomes.
The finding that clinicians who more strongly endorsed a disease model of alcoholism reported greater post-training self-efficacy and greater acceptance of the innovation is surprising in light of past research showing that endorsement of disease model beliefs predicts lower MI skill levels and smaller improvements in MI skills (Baer et al., 2009), and that endorsement of a 12-step model correlates with less motivation to use of behavioral treatment approaches such as MI (McGovern et al., 2004). It should be noted, however, that this analysis examined the effect of such beliefs after controlling for self-reported use of a confrontive style with clients. Thus, the current findings highlight the importance of distinguishing between clinicians’ beliefs regarding the nature of addiction and their beliefs and practices with respect to therapeutic style and serve as a reminder that holding disease model beliefs does not necessarily presage less interest in adopting MI and other evidence-based practices after receiving training (McGovern et al., 2004; Morgenstern et al., 2001). In contrast, the findings that clinician endorsement of a moral/spiritual model of alcoholism predicted worse post-training MI information recall as well as lower ratings of MI importance and helpfulness suggest that seeing alcoholism as “willful misconduct” (see Connors & Rychtarik, 1988) may support a perception that MI, which emphasizes the importance of clients’ making their own decisions with regard to substance use, is a waste of time.
The finding that higher educational levels among clinicians predict better post-training recall of MI information as well as stronger perceptions that employing MI with new clients is important and helpful suggests that education may serve as an indicator of both greater openness to and aptitude for learning empirically-supported methods (see Horvatich, 2006). In past research, higher educational attainment has predicted greater likelihood of adoption of contingency management (Henggeler et al., 2008), higher baseline levels of MI skill and, for some outcomes, greater improvements in MI skills over time (Baer et al., 2009). In contrast, clinicians with less education have been found to need additional training in order to reach criterion in MI training (Martino, Canning-Ball, Carroll, & Rounsaville, 2011). However, although clinicians with higher levels of education might be expected to experience the most benefit from training (Horvatich, 2006; Kerwin, Walker-Smith & Kirby, 2006), it may be that tailoring training to clinicians’ educational background can increase its efficacy (Martino et al., 2011).
The finding that clinicians with heavier caseloads showed worse recall of information about MI after training suggests that such clinicians paid less attention to the material during training. This finding is consistent with survey results showing that clinicians with larger caseloads report less exposure to and use of novel techniques (Saldana et al., 2007). Findings that female clinicians reported greater post-training self-efficacy for adoption but spent less time learning about the innovation than male clinicians have no obvious explanation, and research on dissemination has rarely reported gender differences in adoption. In one study of attitudes toward the possibility of receiving training to manage childhood adolescent obesity, female pediatricians were found to have greater interest in several aspects of training and were less likely to see treatment futility as a barrier than were male pediatricians, but were more likely to express concern about precipitating an eating disorder (Story et al., 2002).
In terms of the characteristics of clinics, clinicians who worked at a clinic with relatively high mean levels of baseline clinician-reported MI-consistent beliefs and behaviors were found to report spending more time learning about and implementing the MI-related preparatory procedures during the month after training. It may be that such clinics were more likely to provide opportunities for supervision in MI-based procedures from an on-site peer or supervisor. These findings seem to serve as additional evidence for the importance of clinicians’ receiving direct encouragement and support for learning new material (see Miller et al., 2006) and adopting new approaches (Heinrich & Cummings, 2014).
4.4 Limitations
Several methodological limitations of the present study are worth noting. First, because of clinician attrition from follow-up at the 1- and 6-month assessment points, results pertaining to prediction of the Implementation stage and especially the Confirmation stage should be viewed with some caution until replicated. Also, although the trainers employed for this study received thorough training, were given feedback on their performance during pilot training sessions, and received ongoing supervision, dissemination sessions were not recorded or directly observed by the trainers’ supervisor. Such observation in a study of this magnitude would have been logistically difficult and had the potential to trigger trainer or trainee reactivity. Thus, we have no objective confirmation regarding the extent to which trainers adhered to the training protocol. Likewise, we were unable to measure the training process or clinicians’ reactions during the dissemination workshop. It is conceivable that, as has been the case in evaluating the process of MI therapy sessions (e.g., Moyers et al., 2008), measuring the during-session behavior of trainers (e.g., use of a training style consistent with MI) and trainees (e.g., change talk and sustain talk with respect to innovation adoption) would be informative.
Similarly, due to practical constraints, we were unable to obtain work samples or other measures (e.g., Rosengren et al., 2008) from clinicians to directly assess clinician competence and skills at using MI or other aspects of the preparatory procedures that formed the basis of the innovation. Thus, measures of utilization of the innovation were derived solely from clinician self-reports of behavior. Also, despite our emphasis on encouraging clinicians to seek out post-training opportunities to develop their skills, our training efforts were probably too brief to have a significant, sustained impact on most clinicians’ practice (especially with respect to use of the MI style), although it is possible that clinicians who already possessed key MI skills and who already used a guiding (as opposed to directing) approach with clients were able to make use of the information provided to begin effective implementation of MI-based preparatory sessions. However, although it cannot be assumed that clinicians who reported making use of the innovation were doing so effectively (see Hartzler et al., 2007; Miller & Mount, 2001), understanding predictors of trainees’ efforts to learn more about and to implement the innovation is important because such activities can be seen as representing necessary, if not sufficient, conditions for successful adoption.
This study did not evaluate the utility of alternative formats of training, such as providing multiple training sessions over the course of one or more weeks, or of post-training supports such as providing supervision or feedback based on recorded practice samples. As noted earlier, a training experience of one full day was believed to be the maximum that would be supported by the majority of targeted clinics. It is possible also that providing structured, concrete assistance in designing and implementing innovation-related assessment and feedback procedures would have increased adoption. Although some evidence suggests that such enhancements may improve training outcomes, results in this regard have been mixed (see Schwalbe et al., 2014), and the field has yet to reach consensus on what array and sequence of training services are most likely to permit successful dissemination of MI-based innovations in addictions treatment.
Some evidence from prior studies suggests that training-driven increases in skill can be maintained for at least a three-month period, although the evidence is mixed with regard to the value of training enhancements. In a study involving behavioral health providers working with substance abuse clients in the Air Force, workshop training was found to yield an immediate increase in MI skills, but skills levels had decayed at the 4-month follow-up (Moyers et al., 2008). Providing personalized feedback and offering consultation phone calls to clinicians did not yield better training outcomes than workshop training alone. A study of training for community substance abuse treatment staff (Baer et al., 2009) found that post-workshop gains in skill generally were maintained over a 3-month follow-up period but found no difference in training outcomes between a standard two-day workshop approach and an enhanced, “context-tailored” training approach involving five two-to-three hour training sessions spaced over 10 weeks, with multiple, tailored opportunities for structured practice and feedback. Another study of training for addiction treatment providers (Martino et al., 2010) also found that training effects on skills were generally maintained over a 12-week follow-up period, but found minimal differences in training outcomes between an expert-led training approach (similar to that used most often in community settings) and a train-the-trainer approach to training. One pilot study (Bennett et al., 2007) did find an impact of training enhancement, such that substance abuse and mental health workers who participated in a workshop and later received both a booster workshop (“Update day”) and additional worksheets, feedback, and coaching had better skill outcomes (at a 15-week follow-up point) than those who received only the original and booster workshop.
With respect to the disseminated innovation itself, it should be noted that MI practice and theory has continued to evolve since this specific empirically-supported approach to the use of MI-based preparatory procedures was developed (see Miller & Rollnick, 2013). Thus, broader use of the dissemination materials and procedures developed for the present study, unless significantly modified and updated, probably would not be warranted. More generally, it may be that processes relevant to the adoption of MI-related preparatory procedures are different in some ways from those that might occur when disseminating other empirically supported clinical innovations. Future attempts at dissemination may yield different results to the extent that baseline levels of acceptance of and experience with the innovation have changed over time.
4.5 Implications for Dissemination Efforts
Research to date has suggested that, for most clinicians, long-term adoption and skillful use of MI is likely to require extended support for skill development, but additional research is needed to determine how best to provide such support (Carpenter et al., 2012; Dunn & Darnell, 2014). The current study, however, has focused on earlier stages that Rogers’ innovation-decision process model highlights as being logical prerequisites to effective, long-term incorporation of an innovation: knowledge and self-efficacy regarding the innovation, belief that the innovation will be helpful and acceptable in the clinical setting, development of intentions to learn and make use of the innovation, and early efforts to learn and begin implementing the innovation. For clinicians who do not pass through these initial stages of adoption, the offer of subsequent coaching or additional training seems unlikely to have a substantial impact, just as clients who lack motivation to change drinking (for example) may be unlikely to develop and consistently implement drink refusal skills (for example, see Mitcheson, Bhavsar, & McCambridge, 2009). Consistent with this assertion, Barwick et al. (2012) have identified “suboptimal practitioner engagement, as reflected in low motivation and tape return rate” (pg. 1792), as probably contributing to the failure of some studies to demonstrate significant change in practitioner MI skills after training. Also, Schwalbe et al. (2014) found that attrition from follow-up training protocols was associated with erosion in MI skill. Taken together, these findings highlight the importance of understanding early stages of the adoption process and of identifying clinician and clinic characteristics that predict levels of adoption at these stages.
It is possible that augmented or otherwise altered approaches to dissemination could succeed in improving outcomes for subgroups of trainees whose baseline characteristics suggest a diminished likelihood of adoption. In the current study, adoption was less likely to occur among clinicians who reported lower levels of prior knowledge, acceptance, and use of key elements of the innovation as well as higher levels of beliefs and practices that are inconsistent with use of the innovation. Adoption was also less likely among clinicians who reported lower levels of educational attainment and heavier caseloads and among those who had lower baseline levels of peer support for and experience with the innovation. Among clinicians who had the option of receiving a post-training telephone consultation (i.e., those in the Full day condition), choosing to participate in the consultation was less likely among those who perceived relatively little clinic support for adoption and whose fellow clinicians endorsed a moral-spiritual model of alcoholism. Thus, as suggested by Decker & Martino (2013), it would seem that future efforts to improve our ability to disseminate empirically supported innovations should focus on how dissemination efforts can best be tailored to these challenging populations of clinicians. These efforts might effectively include addressing possible misconceptions of the innovation during dissemination and, as appropriate, emphasizing the use of the innovation by other clinicians and clinics. Another option to consider is to focus initial dissemination efforts on those clinicians (and clinics) whose existing attitudes and practices are consistent with the innovation. For instance, with respect to MI, Miller (2014) has suggested that “it is best used by people who feel naturally drawn to it, who recognize it, in a way” (p. 4). In either case, attending to factors that influence early stages of the innovation-decision process would seem to be essential if we are to make best use of resources devoted to disseminating innovations in substance abuse treatment.
Acknowledgments
This research was supported by National Institute on Alcohol Abuse and Alcoholism grant R01 013992 to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health. We gratefully acknowledge the efforts of the staff: Patricia Aughtry, Isaac Dompreh, Charmaine Donnelly, Mary Beth Dreyer, Mark Duerr, Marsha Johnson, Carol Nottingham, and Laura Weichmann. We also appreciate Joseph Lucke, RIA Senior Statistician, who guided analyses; Robert Marczynski, who assisted with graphics and Kimberly Larkin who assisted with tables. Finally, we are indebted to the staff of the clinics who participated in this research.
Footnotes
Portions of these data were presented at the annual meeting of the Society for Behavioral Medicine, Montreal, Quebec, Canada in April, 2009.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amodeo M, Lundgren L, Cohen A, Rose D, Chassler D, Beltrame C, D’Ippolito M. Barriers to implementing evidence-based practices in addiction treatment programs: Comparing staff reports on Motivational Interviewing, Adolescent Community Reinforcement Approach, Assertive Community Treatment, and Cognitive-behavioral therapy. Evaluation and Program Planning. 2011;34:382–389. doi: 10.1016/j.evalprogplan.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Baer JS, Rosengren DB, Dunn CW, Wells EA, Ogle RL, Hartzler B. An evaluation of workshop training in motivational interviewing for addiction and mental health clinicians. Drug and Alcohol Dependence. 2004;73:99–106. doi: 10.1016/j.drugalcdep.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Baer JS, Wells EA, Rosengren DB, Hartzler B, Beadnell B, Dunn D. Agency context and tailored training in technology transfer: A pilot evaluation of motivational interviewing training for community counselors. Journal of Substance Abuse Treatment. 2009;37:191–202. doi: 10.1016/j.jsat.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholomew NG, Joe GW, Rowan-Szal GA, Simpson D. Counselor assessments of training and adoption barriers. Journal of Substance Abuse Treatment. 2007;33:193–199. doi: 10.1016/j.jsat.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barwick MA, Bennett LM, Johnson SN, McGowan J, Moore JE. Training health and mental health professionals in motivational interviewing: A systematic review. Children and Youth Services Review. 2012;34:1786–1795. [Google Scholar]
- Beidas RS, Kendall PC. Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clinical Psychology: Science and Practice. 2010;17:1–30. doi: 10.1111/j.1468-2850.2009.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GA, Moore J, Vaughan T, Rouse L, Gibbins JA, Thomas P, James K, Gower P. Strengthening motivational interviewing skills following initial training: A randomised trial of workplace-based reflective practice. Addictive Behaviors. 2007;32:2963–2975. doi: 10.1016/j.addbeh.2007.06.013. [DOI] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Boroughs JM. Motivational interviewing with alcohol outpatients. Behavioural Psychotherapy. 1993;21:347–356. [Google Scholar]
- Brown BS. From research to practice – The bridge is out and the water’s rising. In: Levy JA, Stephens RC, McBride DC, editors. Advances in medical sociology. Vol. 7. Greenwich, CT: JAI Press; 2000. pp. 345–365. [Google Scholar]
- Brown JM, Miller WR. Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors. 1993;7:221–218. [Google Scholar]
- Carpenter KM, Cheng WY, Smith JL, Brooks AC, Amrhein PC, Wain RM, Nunes EV. “Old dogs” and new skills: How clinician characteristics relate to motivational interviewing skills before, during, and after training. Journal of Consulting and Clinical Psychology. 2012;80:560–573. doi: 10.1037/a0028362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, Kunkel LE, Mikulich-Gilbertson SK, Morgenstern J, Obert JL, Polcin D, Snead N, Woody GE. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug and Alcohol Dependence. 2006;81:301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connors GJ, Rychtarik RG. The Supreme Court VA/disease model case: Background and implications. Psychology of Addictive Behaviors. 1988;2:101–107. [Google Scholar]
- Connors GJ, Walitzer KS, Dermen KH. Preparing clients for alcoholism treatment: Effects on treatment participation and outcomes. Journal of Consulting and Clinical Psychology. 2002;70:1161–1169. doi: 10.1037//0022-006x.70.5.1161. [DOI] [PubMed] [Google Scholar]
- Decker SE, Martino S. Unintended effects of training on clinicians’ interest, confidence, and commitment in using motivational interviewing. Drug and Alcohol Dependence. 2013;132:681–687. doi: 10.1016/j.drugalcdep.2013.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Roten Y, Zimmermann G, Ortega D, Despland JN. Meta-analysis of the effects of MI training on clinician’s behavior. Journal of Substance Abuse Treatment. 2013;45:155–162. doi: 10.1016/j.jsat.2013.02.006. [DOI] [PubMed] [Google Scholar]
- Dunn C, Darnell D. Commentary on Schwalbe et al. (2014): Two wishes for the future of motivational interviewing—workshops with fewer learning targets and sustainable coaching. Addiction. 2014;109:1295–1296. doi: 10.1111/add.12616. [DOI] [PubMed] [Google Scholar]
- Gotham HJ. Diffusion of mental health and substance abuse treatments: Development, dissemination, and implementation. Clinical Psychology: Science and Practice. 2004;11:160–176. [Google Scholar]
- Hartzler B, Bear JS, Dunn C, Rosengren DB, Wells E. What is seen through the looking glass: The impact of training on practitioner self-rating of motivational interviewing skills. Behavioural and Cognitive Psychotherapy. 2007;35:431–445. [Google Scholar]
- Hartzler B, Rabun C. Community treatment adoption of contingency management: A conceptual profile of U.S. clinics based on innovativeness of executive staff. International Journal of Drug Policy. 2013;24:333–341. doi: 10.1016/j.drugpo.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug NA, Shopshire M, Tajima B, Gruber V, Guydish J. Adoption of evidence-based practices among substance abuse treatment providers. Journal of Drug Education. 2008;38:181–192. doi: 10.2190/DE.38.2.f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich CJ, Cummings GR. Adoption and diffusion of evidence-based addiction medications in substance abuse treatment. Health Services Research. 2014;49:127–152. doi: 10.1111/1475-6773.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Chapman JE, Rowland MD, Halliday-Boykins CA, Randall J, Shackelford J, Schoenwald SK. Statewide adoption and initial implementation of contingency management for substance-abusing adolescents. Journal of Consulting and Clinical Psychology. 2008;76:556–567. doi: 10.1037/0022-006X.76.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbeck DM, Hser YI, Teruya C. Empirically supported substance abuse treatment approaches: A survey of treatment providers’ perspectives and practices. Addictive Behaviors. 2008;33:699–712. doi: 10.1016/j.addbeh.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Horvatich PK. Enhancing the EBP repertoire of substance abuse counselors: A commentary on Kerwin, Walker-Smith, and Kirby. Journal of Substance Abuse Treatment. 2006;30:171–172. doi: 10.1016/j.jsat.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Greenbaum MA, Noke JM, Finney JW. Reliability, validity, and normative data for a short version of the Understanding of Alcoholism Scale. (1996) Psychology of Addictive Behaviors. 1996;10:38–44. [Google Scholar]
- Kerwin ME, Walker-Smith K, Kirby KC. Comparative analysis of state requirements for the training of substance abuse and mental health counselors. Journal of Substance Abuse Treatment. 2006;30:173–181. doi: 10.1016/j.jsat.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Kirby KC, Benishek LA, Dugosh KL, Kerwin ME. Substance abuse treatment providers’ beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Laflin M, Edmundson EW, Moore-Hirsch S. Enhancing adoption of an alcohol abuse prevention program: An application of diffusion theory. The Journal of Primary Prevention. 1995;16:75–101. doi: 10.1007/BF02407234. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. Journal of Clinical Psychology: In Session. 2009;65:1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20:137–160. [Google Scholar]
- Maas CJ, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences. 2005;1:86. [Google Scholar]
- Madson MB, Loignon AC, Lane C. Training in motivational interviewing: A systematic review. Journal of Substance Abuse Treatment. 2009;36:101–109. doi: 10.1016/j.jsat.2008.05.005. [DOI] [PubMed] [Google Scholar]
- Martino S, Ball SA, Nich C, Canning-Ball M, Rounsaville BJ, Carroll KM. Teaching community program clinicians motivational interviewing using expert and train-the-trainer strategies. Addiction. 2010;106:428–441. doi: 10.1111/j.1360-0443.2010.03135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Canning-Ball M, Carroll KM, Rounsaville BJ. A criterion-based stepwise approach for training counselors in motivational interviewing. Journal of Substance Abuse Treatment. 2011;40:357–365. doi: 10.1016/j.jsat.2010.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Fox TS, Xie H, Drake RE. A survey of clinical practices and readiness to adopt evidence-based practices: Dissemination research in an addiction treatment system. Journal of Substance Abuse Treatment. 2004;26:305–312. doi: 10.1016/j.jsat.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Miller WR. [03-10-15];Helping others learn Motivational Interviewing (MI) 2014 retrieved from http://www.motivationalinterviewing.org/sites/default/files/tnt_manual_2014_d10_20150205.pdf.
- Miller WR, Hendrickson SML, Venner K, Bisono A, Daugherty M, Yahne C. Cross-cultural training in motivational interviewing. Journal of Teaching in the Addictions. 2008;7:4–15. [Google Scholar]
- Miller WR, Kurtz E. Models of alcoholism used in treatment: Contrasting A.A. and other perspectives with which it is often confused. Journal of Studies on Alcohol. 1994;55:159–166. doi: 10.15288/jsa.1994.55.159. [DOI] [PubMed] [Google Scholar]
- Miller WR, Mount KA. A small study of training in motivational interviewing: Does one workshop change clinician and client behavior? Behavioural and Cognitive Psychotherapy. 2001;29:457–71. [Google Scholar]
- Miller WR, Moyers TB. Eight stages in learning motivational interviewing. Journal of Teaching in the Addictions. 2006;5:3–17. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing. New York: Guilford Press; 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York, NY: Guilford Press; 2002. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3. New York, NY: Guilford; 2013. [Google Scholar]
- Miller WR, Sorensen JL, Selzer JA, Brigham GS. Disseminating evidence-based practices in substance abuse treatment: A review with suggestions. Journal of Substance Abuse Treatment. 2006;31:25–39. doi: 10.1016/j.jsat.2006.03.005. [DOI] [PubMed] [Google Scholar]
- Miller WR, Sovereign RG, Krege B. Motivational interviewing with problem drinkers: II. The drinker’s check-up as a preventive intervention. Behavioural Psychotherapy. 1988;16:251–268. [Google Scholar]
- Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. Journal of Consulting and Clinical Psychology. 2004;72:1050–1062. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- Mitcheson L, Bhavsar K, McCambridge J. Randomized trial of training and supervision in motivational interviewing with adolescent drug treatment practitioners. Journal of Substance Abuse Treatment. 2009;37:73–78. doi: 10.1016/j.jsat.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Morgan TJ, McCrady BS, Keller DS, Carroll KM. Manual-guided cognitive-behavioral therapy training: A promising method for disseminating empirically supported substance abuse treatments to the practice community. Psychology of Addictive Behaviors. 2001;15:83–88. [PubMed] [Google Scholar]
- Moyers TB, Manuel JK, Wilson PG, Hendrickson SML, Talcott W, Durand P. A randomized trial investigating training in motivational interviewing for behavioral health providers. Behavioural and Cognitive Psychotherapy. 2008;36:149–162. [Google Scholar]
- Moyers TB, Miller WR. Therapists’ conceptualizations of alcoholism: Measurement and implications for treatment decisions. Psychology of Addictive Behaviors. 1993;7:238–245. [Google Scholar]
- Peugh JL. A practical guide to multilevel modeling. Journal of School Psychology. 2010;48:85–112. doi: 10.1016/j.jsp.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Rash CJ, DePhilippis D, McKay JR, Drapkin M, Petry NM. Training workshops positively impact beliefs about contingency management in a nationwide dissemination effort. Journal of Substance Abuse Treatment. 2013;45:306–312. doi: 10.1016/j.jsat.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan WC, Moyers TB. Motivational interviewing. Journal of Substance Misuse. 1997;2:8–16. [Google Scholar]
- Rogers EM. Diffusion of Innovations. 5. New York: Free Press; 2002. [Google Scholar]
- Rosengren DB, Baer JS, Hartzler B, Dunn CW, Wells EA. The video assessment of simulated encounters (VASE): Development and validation of a group-administered method for evaluating clinician skills in motivational interviewing. Drug and Alcohol Dependence. 2005;79:321–330. doi: 10.1016/j.drugalcdep.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Saldana L, Chapman JE, Henggeler SW, Rowland MD. The Organizational Readiness for Change scale in adolescent programs: Criterion validity. Journal of Substance Abuse Treatment. 2007;33:159–169. doi: 10.1016/j.jsat.2006.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher JA, Madson MB, Nilsen P. Barriers to learning motivational interviewing: A survey of motivational interviewing trainers’ perceptions. Journal of Addictions & Offender Counseling. 2014;35:81–96. [Google Scholar]
- Schwalbe CS, Oh HY, Zweben A. Sustaining motivational interviewing: a meta-analysis of training studies. Addiction. 2014;109:1287–1294. doi: 10.1111/add.12558. [DOI] [PubMed] [Google Scholar]
- Shafer MS, Rhode R, Chong R. Using distance education to promote the transfer of motivational interviewing skills among behavioral health professionals. Journal of Substance Abuse Treatment. 2004;26:141–148. doi: 10.1016/S0740-5472(03)00167-3. [DOI] [PubMed] [Google Scholar]
- Sharma M. Diffusion of innovations theory for alcohol, tobacco, and drugs. Journal of Alcohol and Drug Education. 2008;52:3–7. [Google Scholar]
- Sholomskas DE, Syracuse-Siewert G, Rounsaville BJ, Ball SA, Nuro KF, Carroll KM. We don’t train in vain: A dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology. 2005;73:106–115. doi: 10.1037/0022-006X.73.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JL, Amrhein PC, Brooks AC, Carpenter KM, Levin D, Schreiber EA, et al. Providing live supervision via teleconferencing improves acquisition of motivational interviewing skills after workshop attendance. The American Journal of Drug and Alcohol Abuse. 2007;33:163–168. doi: 10.1080/00952990601091150. [DOI] [PubMed] [Google Scholar]
- Sorensen JL, Hettema JE, Chen T. Dissemination of evidence-based treatment into substance abuse clinical practice. In: Miller PM, Kavanagh D, editors. Translation of addictions science into practice. New York: Elsevier Academic Press; 2007. pp. 363–378. [Google Scholar]
- Story MT, Newmark-Stzainer DR, Sherwood NE, Holt K, Sofka D, Trowbridge FL, et al. Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–214. [PubMed] [Google Scholar]
- Walitzer KS, Dermen KH, Barrick C, Shyhalla K. Dissemination of a MI-based addictions preparatory session in New York: Assessing knowledge. Presented at the annual meeting of the Society for Behavioral Medicine; Montreal, Quebec, Canada. 2009. Apr, [Google Scholar]
- Walitzer KS, Dermen KH, Connors GJ. Strategies for preparing clients for treatment: A review. Behavior Modification. 1999;23:129–151. doi: 10.1177/0145445599231006. [DOI] [PubMed] [Google Scholar]
- Walters ST, Matson SA, Baer JS, Ziedonis DM. Effectiveness of workshop training for psychosocial addiction treatments: A systematic review. Journal of Substance Abuse Treatment. 2005;29:283–293. doi: 10.1016/j.jsat.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Wilbourne PI, Weingardt KR. Therapeutic outcome research and dissemination of empirically based treatment for alcohol use disorders. In: Miller PM, Kavanagh D, editors. Translation of addiction science into practice. New York: Elsevier Academic Press; 2007. [Google Scholar]
- Wiltsey Stirman SW, Crits-Christoph P, DeRubeis RJ. Achieving successful dissemination of empirically supported psychotherapies: A synthesis of dissemination theory. Clinical Psychology: Science and Practice. 2004;11:343–359. [Google Scholar]
- Zweben A, Zuckoff A. Motivational interviewing and treatment adherence. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people to change addictive behavior. 2. New York: Guilford Press; 2002. [Google Scholar]


