Abstract
Background
Risk estimates for the same patient can vary substantially among cardiovascular risk calculators and the reasons are not fully explained. We compared the relative risk increases for consistent risk factors changes across different cardiovascular risk calculators.
Methods
Five clinicians independently selected 16 calculators providing absolute risk estimations. Hypothetical patients were generated using a combination of seven risk factors [age, gender, smoking, blood pressure, high-density lipoprotein (HDL), total cholesterol and diabetes] dichotomized to high and low risk, generating 27 patients (128 total). Relative risk increases due to specific risk factors were determined and compared.
Results
The 16 selected calculators were from six countries, used 5- and 10-year predictions, and estimated CVD or coronary heart disease risk. Across the different calculators for non-diabetic patients, changing age from 50 to 70 produced average relative risk increases from 82 to 395 %, gender (female to male) 35–225 %, smoking status 31–118 %, systolic blood pressure (120–160 mmHg) 16–124 %, total cholesterol (4–7 mmol/L) 51–302 % and HDL (1.3–0.8 mmol/L) 27–133 %. Similar results were found among diabetic patients. Some calculators appeared to have consistently higher relative risk increases over multiple risk factors.
Conclusions
Cardiovascular risk calculators weigh the same risk factors differently. For each risk factor, the relative risk increase from the calculator with the highest increase was generally three to eight times greater than the relative risk increase from the calculator with lowest increase. This likely contributes to some of the inconsistency in risk calculator estimation. It also limits the use of risk calculators in estimating the benefits of therapy.
Electronic supplementary material
The online version of this article (doi:10.1186/s13104-015-1401-8) contains supplementary material, which is available to authorized users.
Keywords: Cardiovascular risk calculator, Cardiovascular risk prediction, Relative risk, Relative risk increase, Risk factor
Background
Guidelines frequently encourage clinicians to use cardiovascular disease (CVD) risk calculators to estimate a patient’s cardiovascular risk. The information is often used to classify patients into different risk categories to guide treatment decisions. Alternatively, calculators can provide absolute values to explain a patient’s estimated risk and discuss the benefits of differing therapies.
Although up to 74 % of primary care physicians who are specifically interested in cardiac disease may regularly use CVD risk calculators [1], most studies show only 22–48 % physicians regularly use risk calculators [2–4]. Some of the diverse reasons why calculators have not been universally adopted include lack of time, a feeling that the information is not helpful, a sense of oversimplification with risk tools, and an ability to predict risk subjectively [2–4].
The inconsistency among CVD risk calculators [5–8] presents another possible limitation to their adoption and application. A review of 25 risk calculators found 33 % of the time different calculators assigned the same patient to a different risk category [8]. For individual patients, the highest calculated absolute risk was, on average, five times higher than the lowest calculated absolute risk [8]. Focusing on diabetic or non-diabetic patients, cardiovascular or coronary heart disease outcomes, and/or 5- or 10-year time horizons made little difference in risk calculation agreement [8]. Only by focusing on CVD outcomes with a 10-year time horizon from Framingham-derived calculators did agreement approach 90 % [8].
Although inconsistency is common among risk calculator estimations, the causes of the broad variation in absolute risk and frequent disagreement in risk category assignment has not yet been described. As identified above, eliminating most of the variables appeared to improve agreement but did not fully explain the reasons for disagreement. Our objective in this study was to determine how different risk calculators weigh individual cardiovascular risk factors (e.g. smoking).
Methods
This is a sub-study of risk factor increases from our initial study of CVD risk calculator agreement [8]. Selection of calculators and generation of hypothetical patients has been explained previously [8] but are reviewed below.
Calculator selection
We searched for and then independently selected a broad range of CVD and coronary heart disease (CHD) risk calculators. Our goal was to identify representative sample of calculators from different countries, were or were not associated with guidelines, used different data sources (Framingham and others), used different formats (internet, paper and pencil, other) and calculated different outcomes durations (5 or 10 years). Originally, 20 calculators were selected and 4 more were added to enhance diversity. In this sub-study, absolute risk estimates are needed to compare the relative risk increases that result from risk factor changes. Therefore, we excluded seven calculators that did not provide absolute numbers. We also excluded the SCORE calculator as it only provided CVD mortality risk. Calculator inclusion and exclusion flow are presented in Fig. 1.
Fig. 1.
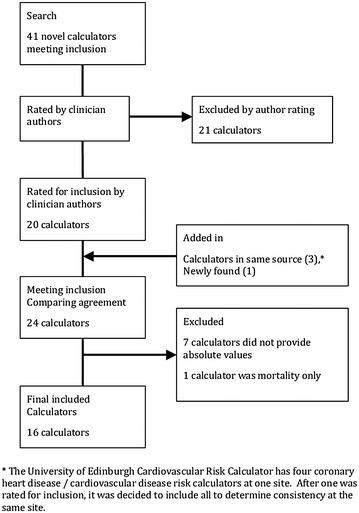
Flow of identification and selection of cardiovascular risk calculators for inclusion
Patient variables
Seven risk factors common to all included calculators were age, gender, smoking status, diabetes, systolic BP, total cholesterol and HDL (or the total cholesterol/HDL ratio). Using a specific increase for each risk factor facilitated comparison across different calculators. We assigned two values for each risk factor: age 70 or 50; gender male or female; current smoking status yes or no; systolic BP 160 or 120 mmHg; total cholesterol 7 or 4 mmol/L; HDL 0.8 or 1.3 mmol/L. The two values for each seven risk factors created 27 or 128 distinct patients.
Two authors independently completed the risk assessment for all 128 hypothetical patients on each calculator. Ethics approval was not required for this study (as patients were hypothetical).
Analysis
Calculation of relative risk increase
To analyze the relative risk increase associated with each risk factor from each calculator, we performed individual risk factor analysis. For individual risk factor analysis (i.e., BP), we started with the lower risk option for that risk factor (120 mmHg) and then varied other risk factors (age, gender, smoking status, total cholesterol, HDL, and diabetes) between high and low risk values to create 64 unique patients. For each patient, we increased the individual risk factor to the high-risk option (i.e. 160 mmHg) and recalculated the risks. This created pairs of identical patients with the same risk factors except for the individual risk factor analyzed, which was low-risk and high-risk for each patient in the pair. We then subtracted the lower-risk estimate from the higher-risk estimate, and divided the risk difference by the low-risk estimate. This created the patient’s relative risk increase for the specific individual risk factor.
As an example, one patient pair in the BP risk factor analysis started with a 50 year old, male, smoker, non-diabetic, with a 7 mmol/L total cholesterol, and a 0.8 mmol/L HDL. The low-risk patient had a 120 mmHg systolic BP while the high-risk was 160 mmHg. Edinburgh ASSIGN risk calculator estimated the low-risk patient’s risk (with the 120 mmHg BP) as 16.6 % and the high-risk patient’s risk (with the 160 mmHg BP) as 25.3 %. The calculated relative risk increase would be (25.3–16.6 %)/16.6 % = 52.4 %.
Mean relative risk increase
The 128 patients provided 64 patient pairs in each individual risk factor analysis. As some calculators do not estimate risk in diabetic patients, diabetic and non-diabetic patients were analyzed and presented separately. This halved the numbers again, leaving 32 diabetic and 32 non-diabetic patient pairs. Therefore, each risk factor analysis had 32 relative risk increases for each calculator (among diabetics or non-diabetics). For each risk factor, we calculated the mean and standard deviation of the relative risk increase of each calculator. An example of the full formula is below.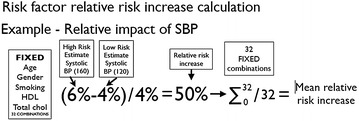
For each risk factor, we ranked calculators from lowest to highest average relative risk increase. We also performed a sub-group analysis when permitted by the number of calculators per sub-group.
Results
Characteristics of the 16 calculators, 10 of which included diabetics, are summarized in Table 1 [9–21].
Table 1.
Characteristics of included risk calculators
| Risk calculator | Composite outcome | Time frame | Include diabetes | Design | Country | Cohort data used |
|---|---|---|---|---|---|---|
| Edinburgh (Framingham CVD) [9] | CVD | 10 (can choose) | Yes | Web | UK | Framingham |
| Edinburgh (ASSIGN) [9] | CVD | 10 | Yes | Web | UK | ASSIGN |
| Primary CVD risk calculator [10] | CVD | 10 | Yes | Web | UK | Framingham |
| Framingham Heart Study [11] | CVD | 10 | Yes | Web | USA | Framingham |
| QRISK2-2011 [12] | CVD | 10 | Yes | Web | UK | GP data in UK |
| Progetto Cuore [13] | CVD | 10 | Yes | Web | Italy | Longitudinal Italian Studies |
| JBS Assessor [14] | CVD | 10 | No | Download | UK | Framingham |
| Edinburgh (BNF) [9] | CVD | 10 | No | Web | UK | BNF |
| Reynolds Risk Score [15] | CVD | 10 | No | Web | USA | Reynolds |
| Australian absolute CVD risk [16] | CVD | 5 | No (ranges for diabetes) | Web | Australia | National Vascular Disease Prevention Alliance |
| New Zealand know your numbers [17] | CVD | 5 | Yes | Web | New Zealand | Framingham |
| UKPDS risk engine [18] | CHD | 10 | Yes | Download | UK | UKPDS |
| i-phone STAT ATPIII lipid management [19] | CHD | 10 | No | i-phone | USA | Framingham |
| Edinburgh (Framingham CHD) [9] | CHD | 10 | Yes | Web | UK | Framingham |
| PROCAM health check [20] | CHD | 10 | Yes | Web | Germany | German Data |
| National cholesterol Education Program [21] | CHD (MI) | 10 | No | Web | USA | Framingham |
Comparison of risk increase due to specific risk factors
For non-diabetic patients, the mean relative risk increases for each risk factor and calculator are summarized on Table 2. The mean relative risk increase varied considerably across calculators. For example, changing age from 50 to 70 years, the average relative risk increase ranged from 82 % for Edinburgh (Framingham, CHD) to 395 % for PROCAM (Health Check), a 4.8 times difference. The ratios of highest average relative increase divided by lowest for the other risk factors was 6.4 for gender, 3.8 for smoking status, 7.8 systolic BP, 5.9 total cholesterol and 4.9 for HDL.
Table 2.
Average relative risk increase due to specific risk factor for each included risk calculator among non-diabetic patients (relative risk increase ± standard deviation)
| Risk calculator | Age (50–70) (%) | Gender (female to male) (%) | Smoking (non-smoker to smoker) (%) | Systolic BP (120–160 mmHg) (%) | Total chol (4–7 mmol/L) (%) | HDL (1.3–0.8 mmol/L) (%) |
|---|---|---|---|---|---|---|
| Edinburgh (Framingham CVD) | 112 ± 35 | 44 ± 12 | 70 ± 24 | 73 ± 25 | 51 ± 17 | 42 ± 14 |
| Edinburgh (ASSIGN) | 222 ± 53 | 35 ± 28 | 37 ± 8 | 49 ± 6 | 60 ± 21 | 27 ± 3 |
| Primary CVD risk calculator | 103 ± 31 | 56 ± 18 | 59 ± 15 | 69 ± 17 | 66 ± 20 | 56 ± 19 |
| Framingham Heart Study | 121 ± 23 | 91 ± 33 | 67 ± 11 | 83 ± 26 | 78 ± 13 | 41 ± 7 |
| QRISK2-2011 | 335 ± 91 | 53 ± 20 | 57 ± 20 | 30 ± 17 | 51 ± 15 | 43 ± 14 |
| Progetto CUORE | 313 ± 30 | 141 ± 57 | 87 ± 27 | 75 ± 13 | 66 ± 26 | 29 ± 4 |
| JBS Assessor | 110 ± 35 | 48 ± 16 | 59 ± 15 | 43 ± 13 | 63 ± 19 | 54 ± 18 |
| Edinburgh (BNF) | 105 ± 31 | 56 ± 18 | 59 ± 13 | 71 ± 19 | 68 ± 22 | 56 ± 18 |
| Reynolds Risk Score | 344 ± 96 | 119 ± 82 | 83 ± 50 | 124 ± 44 | 89 ± 42 | 60 ± 35 |
| Australian absolute CVD risk | 153 ± 50 | 61 ± 20 | 95 ± 38 | 98 ± 37 | 65 ± 20 | 55 ± 19 |
| New Zealand Know Your Numbers | 154 ± 49 | 60 ± 19 | 95 ± 37 | 99 ± 37 | 60 ± 22 | 50 ± 21 |
| UKPDS Risk Engine | 182 ± 16 | 79 ± 8 | 31 ± 3 | 16 ± 2 | 77 ± 8 | 64 ± 6 |
| i-phone STAT ATPIII lipid management | 210 ± 228 | 225 ± 140 | 116 ± 110 | 72 ± 32 | 154 ± 124 | 61 ± 14 |
| Edinburgh (Framingham CHD) | 82 ± 32 | 64 ± 26 | 55 ± 16 | 51 ± 5 | 88 ± 26 | 73 ± 22 |
| PROCAM Health Check | 395 ± 204 | 114 ± 82 | 118 ± 27 | 35 ± 8 | 302 ± 67 | 133 ± 30 |
| National Cholesterol Education Program | 198 ± 203 | 201 ± 124 | 110 ± 125 | 69 ± 49 | 141 ± 129 | 61 ± 33 |
| Overall average | 196 ± 140 | 91 ± 80 | 75 ± 54 | 66 ± 37 | 92 ± 80 | 57 ± 30 |
For diabetic patients, the mean relative risk increases for each risk factor and calculator are summarized on Table 3. The ratios of highest average relative increase divided by lowest was 4.9 for age, 18.2 for gender, 3.5 for smoking status, 4.9 systolic BP, 8.1 total cholesterol, 4.9 for HDL and 3.4 diabetic status.
Table 3.
Average relative risk increase due to specific risk factor for each included risk calculator among diabetic patients (relative risk increase ± standard deviation)
| Risk calculator | Age (50–70) (%) | Gender (female to male) (%) | Smoking (non-smoker to smoker) (%) | Systolic BP (120–160 mmHg) (%) | Total chol (4–7 mmol/L) (%) | HDL (1.3–0.8 mmol/L) (%) | Diabetes (yes or no) (%) |
|---|---|---|---|---|---|---|---|
| Edinburgh (Framingham CVD) | 79 ± 28 | 11 ± 6 | 50 ± 18 | 52 ± 19 | 37 ± 13 | 31 ± 11 | 62 ± 33 |
| Edinburgh (ASSIGN) | 172 ± 47 | 15 ± 21 | 31 ± 10 | 40 ± 10 | 49 ± 20 | 23 ± 6 | 111 ± 28 |
| Primary CVD risk calculator | 96 ± 30 | 9 ± 10 | 52 ± 11 | 66 ± 16 | 51 ± 18 | 44 ± 16 | 60 ± 31 |
| Framingham Heart Study | 104 ± 24 | 62 ± 27 | 59 ± 14 | 73 ± 27 | 68 ± 17 | 35 ± 9 | 70 ± 18 |
| QRISK2-2011 | 197 ± 65 | 37 ± 19 | 54 ± 20 | 28 ± 17 | 47 ± 14 | 40 ± 13 | 84 ± 37 |
| Progetto CUORE | 297 ± 35 | 164 ± 63 | 84 ± 28 | 72 ± 14 | 63 ± 25 | 28 ± 4 | 46 ± 8 |
| New Zealand know your numbers | 74 ± 13 | 11 ± 6 | 48 ± 7 | 49 ± 7 | 31 ± 6 | 25 ± 6 | 158 ± 123 |
| UKPDS risk engine | 167 ± 22 | 73 ± 11 | 29 ± 4 | 15 ± 2 | 72 ± 11 | 60 ± 9 | 50 ± 7 |
| Edinburgh (Framingham CHD) | 67 ± 30 | 17 ± 16 | 44 ± 13 | 41 ± 12 | 70 ± 20 | 58 ± 17 | 53 ± 31 |
| PROCAM health check | 327 ± 196 | 76 ± 65 | 101 ± 38 | 31 ± 11 | 251 ± 93 | 113 ± 42 | 88 ± 32 |
| Overall average | 158 ± 113 | 48 ± 56 | 55 ± 28 | 47 ± 24 | 74 ± 69 | 46 ± 30 | 78 ± 57 |
Ranking of calculators by mean relative risk increase
For each risk factor, ranking of calculators based on mean relative risk increases from lowest to highest among non-diabetic and diabetic patients is provided in Table 4. Among the 16 non-diabetic calculators, Edinburgh (Framingham CVD), Edinburgh (ASSIGN), QRISK2-2011 and JBS Assessor had the lowest relative risk increase (ranked four or less) for three or four of the six risk factors. Reynolds Risk Score, iPhone ATPIII lipid management, PROCAM (Health Check), and National Cholesterol Education Program had the highest relative risk increases (ranked 13 or more) for three or four of the six risk factors.
Table 4.
Ranking of each calculator by the average relative risk increase for each risk factor
| Risk calculators | Age (50–70) | Gender (female to male) | Smoking (non-smoker to smoker) | Systolic BP (120–160 mmHg) | Total chol (4–7 mmol/L) | HDL (1.3 to 0.8 mmol/L) | Diabetes (non-diabetic to diabetic) |
|---|---|---|---|---|---|---|---|
| Non-diabetic patients | |||||||
| Edinburgh (Framingham CVD) | 5 | 2 | 9 | 11 | 1 | 4 | |
| Edinburgh (ASSIGN) | 12 | 1 | 2 | 5 | 4 | 1 | |
| Primary CVD risk calculator | 2 | 5 | 6 | 8 | 7 | 10 | |
| Framingham Heart Study (CVD) | 6 | 11 | 8 | 13 | 11 | 3 | |
| QRISK2-2011 | 14 | 4 | 4 | 2 | 2 | 5 | |
| Progetto CUORE | 13 | 14 | 11 | 12 | 8 | 2 | |
| JBS Assessor | 4 | 3 | 7 | 4 | 5 | 7 | |
| Edinburgh (BNF) | 3 | 6 | 5 | 9 | 9 | 9 | |
| Reynolds Risk Score | 15 | 13 | 10 | 16 | 13 | 11 | |
| NZ know your numbers | 8 | 7 | 13 | 15 | 3 | 6 | |
| Australian absolute CVD risk | 7 | 8 | 12 | 14 | 6 | 8 | |
| UKPDS | 9 | 10 | 1 | 1 | 10 | 14 | |
| iPhone ATP III lipid management | 11 | 16 | 15 | 10 | 15 | 13 | |
| Edinburgh (Framingham CHD) | 1 | 9 | 3 | 6 | 12 | 15 | |
| PROCAM (Health Check) | 16 | 12 | 16 | 3 | 16 | 16 | |
| National Cholesterol Education Program | 10 | 15 | 14 | 7 | 14 | 12 | |
| Diabetic patients | |||||||
| Edinburgh (Framingham CVD) | 3 | 2 | 5 | 7 | 2 | 4 | 5 |
| Edinburgh (ASSIGN) | 7 | 4 | 2 | 4 | 4 | 1 | 9 |
| Primary CVD risk calculator | 4 | 1 | 6 | 8 | 5 | 7 | 4 |
| Framingham Heart Study (CVD) | 5 | 7 | 8 | 10 | 7 | 5 | 6 |
| QRISK2-2011 | 8 | 6 | 7 | 2 | 3 | 6 | 7 |
| Progetto CUORE | 9 | 10 | 9 | 9 | 6 | 3 | 1 |
| NZ know your numbers | 2 | 3 | 4 | 6 | 1 | 2 | 10 |
| UKPDS | 6 | 8 | 1 | 1 | 9 | 9 | 2 |
| Edinburgh (Framingham CHD) | 1 | 5 | 3 | 5 | 8 | 8 | 3 |
| PROCAM (Health Check) | 10 | 9 | 10 | 3 | 10 | 10 | 8 |
Among the 10 diabetic calculators, Edinburgh (Framingham CVD), NZ Know Your Numbers, UKPDS, and Edinburgh (Framingham CHD) had the lowest relative risk increase (ranked three or less out of 10 calculators) for three or four of the seven risk factors. Progetto CUORE, UKPDS and PROCAM (Health Check) had the highest relative risk increases (ranked eight or more out of ten calculators) for three or four of the seven risk factors.
Sub-group comparison
Additional file 1: Table S1 provides the subgroup comparisons of the relative risk increase among non-diabetic calculators. Only two five-year calculators were identified and, therefore, were excluded. We did not complete subgroup analysis on diabetic calculators, as the number of calculators was too small.
Among 16 calculators for non-diabetic patients, there were 14 10-year calculators, 5 for CHD and 9 for CVD. The average relative risk increases were higher for CHD compared to CVD for all risk factors except BP. Additionally, the range of relative risk increases across the sample of calculators was higher for CHD compared to CVD for all risk factors except BP.
Among the 16 non-diabetic calculators, half were derived from the Framingham database and the other half from eight different databases. We excluded the 5-year risk calculators and the CHD calculators to focus the comparison on the four Framingham-derived 10-year CVD calculators versus the five non-Framingham-derived 10-year CVD calculators. The average relative risk increases for Framingham- and non-Framingham-derived calculators were remarkably similar, except for age. The range of relative risk increases was higher for non-Framingham-derived calculators compared to Framingham-derived calculators. Therefore, although the pooled relative risk increases are similar, there is more variability between non-Framingham-derived calculators.
Sample patient
Figure 2 illustrates the relative risk increases for each calculator when individual risk factors are changed for a sample patient. The sample patient is a 50-year-old, female, non-diabetic, smoker, with 160 mmHg systolic BP, 7 mmol/L total cholesterol, and 0.8 mmol/L HDL. For example, changing total cholesterol from 4 to 7 mmol/L, the relative risk increase for Progetto CUORE was 42 and 340 % for PROCAM.
Fig. 2.

Sample of relative risk increases for each risk factor for a 50-year-old, female, smoker, 160 mmHg systolic blood pressure, 7 mmol/L total cholesterol, 0.8 mmol/L HDL, non-diabetic
Discussion
The mean relative risk increase for specific risk factors varied considerably among the CVD risk calculators. The highest average relative risk increase from a calculator was generally three to eight times greater than the calculator with the lowest average. For example, among non-diabetic risk calculators, an increase in total cholesterol from 4 to 7 mmol/L resulted in an average relative risk of 302 % using the PROCAM Health Check Calculator compared to 51 % using the Edinburgh (Framingham CVD) calculator.
While there was a lot of variation among the overall group of calculators assessed, some calculators had remarkably similar results. For example, among non-diabetic calculators, the average relative risk increases for JBS Assessor and Edinburgh (BNF) were frequently within 8 % for 5 of 6 risk factors (the other 28 %). Alternatively, considering the relative risk increases associated with smoking among non-diabetics, the lowest average relative risk increase was 31 % while the highest was 118 %, a spread of 87 %. However, 11 of the 16 calculators had an average relative risk increase from 55 to 95 %, a difference of only 40 %. Similar results were found for gender that had a spread of 190 % (35–225 %), although 9 of 16 calculators were within a 29 % spread and 13 of 16 were within an 84 % spread.
Past research has shown frequent disagreement among risk calculators [5–8]. In our previous work, the disagreement in risk categorization occurred 33 % of the time for paired risk calculator comparisons [8]. As well, the absolute risk estimation varied considerably among different calculators, with the highest estimate five times greater than the lowest estimate for the same patient. In the previous study, subgroup testing found that limiting analysis to 5- or 10-year outcomes or CVD or CHD outcomes, did not meaningfully improve agreement. Agreement only improved by limiting analysis to 10-year CVD outcomes all derived from Framingham [8].
This is the first study to explore the reasons for differences in risk estimation. It is possible that poor agreement could have arisen, in part, from different baseline risk. However, as our original study showed, the lowest risk patient had remarkably similar risk estimation (≤4 %) across 14 different calculators. Alternatively, the weighting of risk factors among calculators could have been variable from patient to patient without any distinct pattern. However, we found large variation in how calculators weight risk factors, with some calculators consistently providing more or less weight for a certain risk factors.
Why is there a difference in relative risk increase among the calculators? Compared to calculators using a CVD endpoint, the relative risk increase for all risk factors for CHD calculators was higher, except systolic BP. As CVD includes stroke (and systolic BP is an important risk factor for stroke), the higher relative risk increases for systolic BP in CVD as compared to CHD calculators makes sense. Compare this to total cholesterol which had an average relative risk increase of 152 % in CHD calculators versus 56 % in CVD calculators. Thus, some of the variability in relative risk increases result from the type of outcomes assessed.
The database used to derive the calculator appears to play some role in the variability of the relative risk increase. Calculators derived from non-Framingham databases varied more broadly than those derived from Framingham. This corresponds to the results of our first study showing that agreement was better among Framingham-derived calculators than among non-Framingham-derived calculators [8]. As different populations have different risks and susceptibility to CVD, the variability with calculators derived from other databases could be anticipated. The Framingham-derived calculators must modify their model to better predict outcomes in different populations [22].
The variability in relative risk increases raises important concerns around the use of calculators to assess the benefits of therapeutic interventions that target specific risk factors. Although it may seem reasonable to estimate potential therapy benefits simply by changing the risk factor in the calculator, there are a number of problems with this approach. Clinicians cannot assume that medications taking a systolic BP from 160 to 140 mmHg will yield the clinical benefits similar to the risk difference between 160 and 140 mmHg. Additionally, we know that some interventions that modify risk factors (atenolol [23], torcetrapib [24], rosiglitazone [25] to name a few) do not reduce CVD. Another potential failing in this approach, identified in this study, is the different weighting that calculators appear to place on some risk factors. A change in systolic BP from 120 to 160 mmHg increases the average patient’s risk by 16 % (using the UKPDS engine) to 124 % (Reynolds Risk Score), a greater than seven-fold difference. Some studies try to estimate the absolute cardiovascular benefits from interventions designed to modify risk factors (e.g. naturopathic medicine for CVD risk [26]). By using changes in CVD estimations in this way, careful selection of risk calculator will result in dramatic difference in the calculated risks, and therefore perceived benefit of the intervention. For example, if the Reynolds Risk Score was used to estimate risk associated with BP changes, the estimated absolute cardiovascular risk benefit would be much greater than if the UKPDS calculator was used. Researchers, journal editors and reviews should recognize that calculator choice in these studies could easily change the results in both a statistical and clinically significant way.
Limitations
Many of the limitations of this sub-study mirror those of our original study [8]. Although we used hypothetical patients, this did allow us to focus on specific changes in risks across a variety of patients, permitting easy calculation of the relative risk increases due to risk factor change.
Conclusion
There is considerable variation among CVD risk calculators in the relative risk increase for each specific risk factor. The highest average relative risk increase for a calculator was 3.4–18.2 higher than the lowest average relative risk increase, depending on risk factor. Some calculators more often produce higher relative risk changes (e.g. PROCAM) while others more often produce lower relative risk changes [e.g. Edinburgh (ASSIGN)]. However, there was also similarity among some of the calculators. Although consistency could occur among calculators derived from different databases, 10-year CVD Framingham calculators appeared to have the most consistent relative risk increases. Researchers and clinicians should not assume risk differences from reductions in risk factors are reliable or consistent from one calculator to the next.
Authors’ contributions
GMA conceived of the study, attained funding, analyzed the data, and completed the first draft of the manuscript. GMA, FN, CK, MRK and JM did original risk estimations on hypothetical patients. BV provided statistical advice and assistance with analysis. All authors helped refine the study concept, provided input in analysis, critically contributed to the manuscript, approve the manuscript and are accountable for all aspects of the report. All authors read and approved the final manuscript.
Acknowledgements
The final draft of the article was reviewed and edited for grammar by Lynda Cranston, medical writer. The project is funded by a Grant from the Edmonton North Primary Care Network. The funder had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Compliance with ethical guidelines
Competing interests One of the authors (JM) is presently developing a free cardiovascular risk calculator to enhance shared informed decisions making. It uses the Framingham database.
Abbreviations
- CVD
cardiovascular disease
- CHD
coronary heart disease
- BP
blood pressure
- HDL
high density lipoprotein
Additional file
Additional file 1: Table S1. Comparison of Averages and Ranges of Relative Risk Increases across Risk Factors for Selected Subgroups of Non-diabetic Calculators.
Contributor Information
G. Michael Allan, Email: michael.allan@ualberta.ca.
Faeze Nouri, Email: faeze.nouri@gmail.com.
Christina Korownyk, Email: tina.korownyk@ualberta.ca.
Michael R. Kolber, Email: mkolber@ualberta.ca
Ben Vandermeer, Email: bv1@ualberta.ca.
James McCormack, Email: james.mccormack@ubc.ca.
References
- 1.Gupta M, Singh N, Tsigoulis M, Kajil M, Hirjikaka S, et al. Perceptions of Canadian primary care physicians towards cardiovascular risk assessment and lipid management. Can J Cardiol. 2012;28:14–19. doi: 10.1016/j.cjca.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Eichler K, Zoller M, Tschudi P, Steurer J. Barriers to apply cardiovascular prediction rules in primary care: a postal survey. BMC Fam Pract. 2007;8(3):1. doi: 10.1186/1471-2296-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sposito AC, Ramires JAF, Jukema JW, Molina JC, da Silva PM, et al. Physicians’ attitudes and adherence to use of risk scores for primary prevention of cardiovascular disease: cross-sectional survey in three world regions. Curr Med Res Opin. 2009;25:1171–8117. doi: 10.1185/03007990902846423. [DOI] [PubMed] [Google Scholar]
- 4.Graham IM, Stewart M, Hertog MG. Cardiovascular round table task force. Factors impeding the implementation of cardiovascular prevention guidelines: findings from a survey conducted by the European Society of Cardiology. Eur J Cardiovasc Prev Rehabil. 2006;13:839–845. doi: 10.1097/01.hjr.0000219112.02544.24. [DOI] [PubMed] [Google Scholar]
- 5.Quaglini S, Stefanelli M, Boiocchi L, Campari F, Cavallini A, Micieli G. Cardiovascular risk calculators: understanding differences and realising economic implications. Int J Med Inform. 2005;74:191–199. doi: 10.1016/j.ijmedinf.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 6.Fornasini M, Brotons C, Sellarès J, Martinez M, Galán ML, Sáenz I, et al. Consequences of using different methods to assess cardiovascular risk in primary care. Fam Pract. 2006;23:28–33. doi: 10.1093/fampra/cmi092. [DOI] [PubMed] [Google Scholar]
- 7.Chia YC. Review of tools of cardiovascular disease risk stratification: interpretation, customisation and application in clinical practice. Singapore Med J. 2011;52:116–123. [PubMed] [Google Scholar]
- 8.Allan GM, Nouri F, Korownyk C, Kolber MR, Vandermeer B, McCromack J. Agreement among cardiovascular disease risk calculators. Circulation. 2013;127:1948–1956. doi: 10.1161/CIRCULATIONAHA.112.000412. [DOI] [PubMed] [Google Scholar]
- 9.Edinburgh: Framingham CVD, ASSIGN, BNF, and Framingham CHD. Payne R. cardiovascular risk calculators (Internet). Edinburgh: University of Edinburgh (updated 2010 May 10; cited 2012 May 9). http://cvrisk.mvm.ed.ac.uk/calculator/calc.asp.
- 10.Thomas H. Primary cardiovascular risk calculator (Internet). UK: Patient.co.uk (updated 2011 January 13; cited 2012 May 9). http://www.patient.co.uk/doctor/Primary-Cardiovascular-Risk-Calculator.htm.
- 11.D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, et al. A general cardiovascular risk profile for use in primary care: The Framingham Heart Study (Internet). US: The Framingham Heart Study (updated 2012 April 23; cited 2012 May 11). http://www.framinghamheartstudy.org/risk/gencardio.html#.
- 12.Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, et al. Qrisk 2-2011 cardiovascular disease risk calculator (Internet). UK: UK National Health Service (updated 2012 April; cited 2012 May 11). http://www.qrisk.org/index.php.
- 13.Giampaoli S, Panico S, Vanuzzo D, Palmieri L, Donfrancesco C, et al. PROGETTO CUORE individual risk score (Internet). Italy: National Institute of Health (updated 2008 September 29; cited 2012 May 11). http://www.cuore.iss.it/sopra/calc-rischio_en.asp.
- 14.Durrington PN. JBS CV risk assessor (Software). UK: University of Manchester. http://www.heartuk.org.uk/HealthProfessionals/index.php/jbs_cv_risk_assessor/.
- 15.Ridker PM, Buring JE, Rifai N, Cook NR. Reynolds Risk Score (Internet). US: Reynoldsriskscore.org (cited 2012 May 9). http://www.reynoldsriskscore.org/Default.aspx.
- 16.NVDPA Guidelines: Australian absolute cardiovascular risk calculator (Internet). Australia: National Vascular Disease Prevention Alliance (NVDP) (cited 2012 May 9). http://www.cvdcheck.org.au/.
- 17.Wells S, Kerr A. Your heart forecast (Internet). New Zealand: Heart Foundation (updated 2011; cited 2012 May 10). http://www.knowyournumbers.co.nz/heart-age-forecast.aspx.
- 18.Stevens RJ, Kothari V, Adler AI, Stratton IM. UKPDS risk engine (Software). UK: University of Oxford (cited 2012 May 10). http://www.dtu.ox.ac.uk/riskengine/download.php.
- 19.Statcoder. STAT ATPIII lipid management (iphone app). US: Austin Physician Productivity (updated 2011 July 15; cited 2012 May 11). http://statcoder.com/.
- 20.PROCAM health check (Internet). Switzerland: International Task Force for Prevention of Coronary Heart Disease (cited 2012 May 10). http://www.chd-taskforce.de/procam_interactive.html.
- 21.National Cholesterol Education Program, Grundy SM, Becker D, Clark LT, Cooper RS, Denke MA, et al. Risk assessment tool for estimating your 10-year of having a heart attack (Internet). US: Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (updated 2004; cited 2012 May 9). http://hp2010.nhlbihin.net/atpiii/calculator.asp.
- 22.D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P, CHD Risk Prediction Group Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 23.Carlberg B, Samuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004;364:1684–1689. doi: 10.1016/S0140-6736(04)17355-8. [DOI] [PubMed] [Google Scholar]
- 24.Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357:2109–2122. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 25.Singh S, Loke YK, Furberg CD. Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA. 2007;298:1189–1195. doi: 10.1001/jama.298.10.1189. [DOI] [PubMed] [Google Scholar]
- 26.Seely D, Szczurko O, Cooley K, Fritz H, Aberdour S, Herrington C. Naturopathic medicine for the prevention of cardiovascular disease: a randomized clinical trial. CMAJ. 2013;185:E409–E416. doi: 10.1503/cmaj.120567. [DOI] [PMC free article] [PubMed] [Google Scholar]


