Abstract
Background
Many countries have integrated antenatal care as an essential part of routine maternal health services. The importance of this service cannot be overemphasized as many women’s lives are usually saved particularly through early detection of pregnancy related complications. However, while many women would attend at least one visit for ante natal care (ANC), completion of recommended number of visits (4+) has been a challenge of many health systems particularly in developing countries like Tanzania.
Methods
We conducted a cohort study to include ultrasound scanning using a portable hand-held Vscan to test whether by integrating it in routine ANC clinics at dispensary and health centre levels would promote number of ANC visits by women.
Health providers rendering ANC services in selected facilities were trained on how to use the simple technology of ultrasound scanning. Women living in catchment areas of the respective selected facilities were eligible to inclusion to the study when consented. A baseline status of the ANC attendance in the study area was established through baseline household and facility surveys. A total of 257 women consented and received the study treatment.
Results
Our results showed that, there was no a slight change between baseline (97.2 %) and endline (97.4 %) results among women attending ANC clinics at least once. However, there was a significant change in percentage of women attending ANC clinic four times or more (27.2 % during baseline and 60.3 %; p = 0001).
Conclusions
We conclude that, introduction of the simplified ultrasound scanning technology at lowest levels of care has an effect to improving ANC attendance in terms of number of visits and motivate facility delivery.
Keywords: ANC, Attendance, Vscan, Ultrasound, Facility delivery
Background
It is well acknowledged and known globally that early antenatal care (ANC) is important for early detection of pregnancy related complications and ultimately effective birth plan leading to better pregnancy outcomes [1]. WHO recommends a minimum of four visits in the period of pregnancy of a woman and in many cases when this is done, chances of women experiencing obstetric complications are reduced significantly [2].
Many developing countries (including Tanzania) have made in their health policy ANC services to be universal and provided without a cost in order to enable accessibility by the majority poor [3, 4]. However, despite such initiatives and efforts, utilization of ANC services has not been very satisfactory [5]. For example, while Tanzania has attained an average of about 96 % of women attending ANC clinics (at least once) between 2004 and 2010 (Fig. 1), the percentage of women attending four or more visits has been declining [2].
Fig. 1.
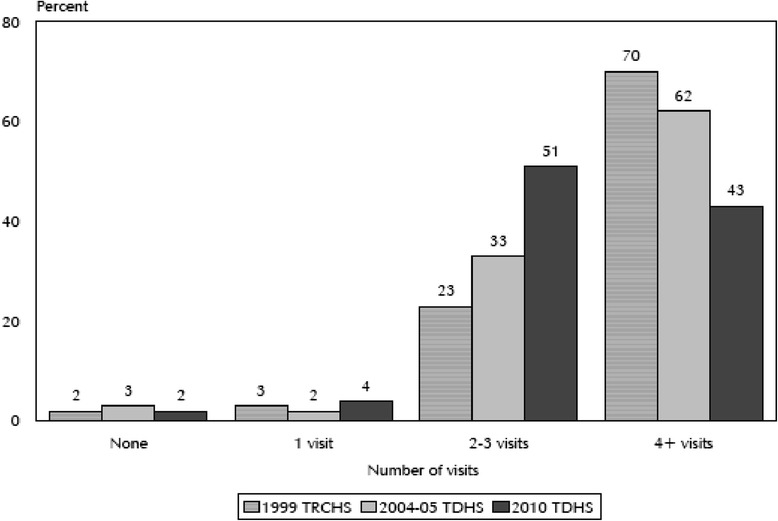
Trend of ANC attendance by Tanzanian women between 1999 and 2010 Source: NBS, 2010
A similar trend is also observed among women who make use of health facilities during delivery. While 47 % of women delivered in health facilities in year 2004, the increase in five years later was only 3 % amounting to only 50 % of all women who gave birth in 2010 [1, 2].
Many studies have been conducted to determine barriers towards these two important indicators followed by a number of interventions but improvement has been minimal and in some cases a negative change has been realized [6, 7].
We conducted a study to test whether by introducing a simple technology of Vscan – a portable handheld ultrasound device in routine ANC services can motivate women to attend ANC clinics and complete the four or more visits. The idea is born by the fact that some studies assessing health seeking behaviour especially among rural communities found that people value and prefer technological physical examinations to just being verbally told the progress of their health [8].
The goal of this study was to contribute to the Government efforts in reducing maternal mortality and newborn deaths in order to accelerate attainment of MDG 4 and 5 using simple and appropriate technologies in rural settings of Tanzania. It aimed at assessing and evaluating acceptability, feasibility, impact and cost-effectiveness of the introduced simple technologies on maternal and newborn health.
The primary objective was to measure whether the use of ultrasound would increase the number of ANC visits by pregnant women at the dispensary level.
Methods
Study type and intervention
This was a cohort study applying a before and after design. The study was a Health Facility Based intervention that included clinical service improvement through clinical guidelines and pathways that were used by health care providers, a supportive and structured education and clinical leadership training and workforce development of Non-Physician Clinicians, and implementing appropriate technologies at different levels of care which included those shown in Table 1.
Table 1.
Set of medical technologies implemented in the study
| Hospital Level | Health Centre Level | Dispensary Level |
|---|---|---|
| Venue 40 Portable ultrasound- 1 unit. Used by physicians at highest referral level in a district health system. | Venue 40 Portable ultrasound – 1 unit. Used by Assistant Medical Officers trained by the project in ultrasound scanning at the first referral level in district health system. | Vscan Handheld Portable ultrasound – 5 units. Used by Mid-level providers (clinical officers, nurse midwives and Medical Attendants) trained by the project in ultrasound. |
Mechanisms for data collection
A baseline survey at the beginning of the project and a follow up survey at the end of the project were conducted and used to establish the project effect on quality of care on maternal and neonatal health among users (in intervention and control arms) and health providers (in interventional arm). Structured questionnaires which were adapted from Averting Maternal Death and Disability (AMDD) were used to conduct both the baseline and follow up surveys. While the structured questionnaire enabled collection of primary quantitative data, a semi-structured tool was also developed for key informant interviews to collect qualitative data which would interpret some of the quantitative data collected. Special registers were developed to capture data from pregnant women receiving the intervention.
Study area and population
This study was conducted in Kisarawe district, one of six rural districts in the Coast Region of Tanzania. The district is third in least populated among the districts in the region (Table 2). At the time of implementing this study, the population in the district had increased to 230,456 from that indicated in Table 2. About 41 % of this population were women of reproductive age. According to district own projections, 10 % of all women who are at reproductive age were likely to become pregnant during the one year project life hence being the project targeted sub-population. Facility delivery in the district was at 73.1 % with 74 % of all deliveries attended by skilled personnel. The district has 1 hospital, 3 health centers and 20 dispensaries. Ten health facilities (and hence ten communities within catchment areas of these facilities) were selected of which five were used as intervention facilities while the remaining five were used as control facilities. In each arm, four dispensaries and one health centre were selected. The primary targeted audience was women of reproductive age who would benefit with the introduction of ultra sound scanning in routine antenatal clinic at primary facility level.
Table 2.
Population of Pwani Region by Sex, Average Household Size and Sex Ratio
| Serial No. | District/Council | Population (Number) | Average Household Size | Sex Ratio | ||
|---|---|---|---|---|---|---|
| Total | Male | Female | ||||
| Total | 1,098,668 | 537,826 | 560,842 | 4.3 | 96 | |
| 1 | Bagamoyo District Council | 311,740 | 154,198 | 157,542 | 4.4 | 98 |
| 2 | Kibaha District Council | 70,209 | 34,515 | 35,694 | 4.1 | 97 |
| 3 | Kisarawe District Council | 101,598 | 50,631 | 50,967 | 3.9 | 99 |
| 4 | Mkuranga District Council | 222,921 | 108,024 | 114,897 | 4.3 | 94 |
| 5 | Rufiji District Council | 217,274 | 104,851 | 112,423 | 4.4 | 93 |
| 6 | Mafia District Council | 46,438 | 22,954 | 23,484 | 3.9 | 98 |
| 7 | Kibaha Town Council | 123,488 | 62,653 | 65,835 | 4.1 | 95 |
Source: National Bureau of Statistics
Inclusion and exclusion criteria
Only women who were attending routine ANC were included. In order to standardise follow up results as an outcome of the interventions, recruitment of women to the study considered only women who started ANC in the first trimester of their pregnancy. Also, only women whose residences were within the selected health facility catchment area were involved. The age of targeted women was limited to 15–49 years. Pregnant women who use the facility through other inlets such as out patient department, emergency section, labour room or normal admission benefited from the interventions for ethical reasons but were not included in the study. A sample size of 257 women was pre-determined using STATA computer software.
Duration of the treatment
The study population received the interventions three times (during the first, second and third trimesters of the pregnancy). Only when clinically required, the client received an extra treatment of the interventions. The treatment was specifically provided from the 6th week (recruitment and first measurement) to 34th week of gestation. The project lasted for one year.
Statistical analysis
Analysis of data generated from training was generally descriptive, with frequency distribution of the respondents (pregnant women) across variables calculated. For each arm of the study (intervention and control), data from household surveys involving women who accessed ANC services within the catchment areas of the respective health facilities were developed into two separate data sets and analysed separately. Then the percentage change in the level of knowledge and confidence in assessing pregnancy related complications among health providers was derived by comparing the before and after intervention figures assessed during facility assessments. Normal frequency distribution across most of the variables was calculated and two-sided paired t-test used to generate statistical significance. The before and after figures were used to arrive into conclusion if changes have occurred in both arms while comparisons of results from the two arms was used to associate changes with interventions.
Research ethics
This work received ethical approval from the Ifakara Health Institute – Institutional Review Board (IHI – IRB) - certificate number IHI/IRB/No.35. The IRB is registered with FEDERAL WIDE ASSURANCE NUMBER: SWA 00002632.
Results
The primary indicator of the study was to determine whether by introducing ultrasound scanning in routine ANC services would increase the number of visits by women attending ANC clinics. While there was no a significant change between baseline and endline results among women attending ANC clinics at least once (97.2 % during baseline and 97.4 % during endline), there was a significant change in percentage of women attending ANC clinic four times or more. Similarly, facility delivery increased significantly (Table 3).
Table 3.
Change in key indicators as a result of introducing routine ultrasound scanning in ANC clinics (%)
| Indicator | Intervention area | Control area | ||||
|---|---|---|---|---|---|---|
| Baseline (n-381) | Endline (423) | p-value | Baseline (n-394) | Endline (383) | p-value | |
| ANC visits (at least once) | 97.2 | 97.4 | 0.0412 | 96.9 | 96.1 | 0.3002 |
| ANC Visits (four times and above) | 27.2 | 60.3 | 0.0001 | 32.4 | 34.1 | 0.0891 |
| Facility delivery | 79.2 | 87.9 | 0.002 | 67.7 | 69.4 | 0.0623 |
On the other hand, percentage of women who had access to ultrasound services increased significantly (Fig. 2). Before the study was introduced, the only facility where such services were available was the district hospital. More than 66 % (n =381) of the women from the study area used to traveling between 5 and 78 km to the district hospital to access ultrasound services when referred to by health providers from lower health facilities.
Fig. 2.
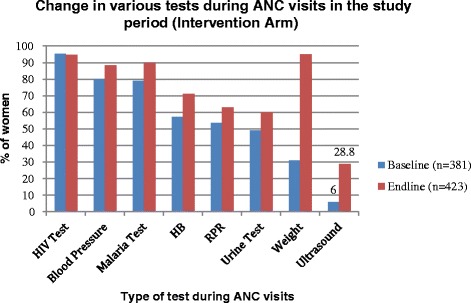
Improvement on availability of ultrasound scanning during ANC clinic in the study interventional arm
The results from the study also demonstrated increase (Tables 4 and 5) in confidence of mid-level providers in the study facilities in determining pregnancy related complications (p = 0.0001).
Table 4.
Confidence of health providers in detecting pregnancy related complications (%) [Baseline; n = 30]
| Anteparturm hemorrhage | Transverse lie | Placenta previa | Breech presentation | Ectopic pregnancy | Twins | Poly /oligo hydromnious | |
|---|---|---|---|---|---|---|---|
| Very confident | 23.3 | 13.3 | 10 | 13.3 | 3.3 | 13.3 | 0 |
| Confident | 50 | 60 | 23.3 | 56.7 | 16.7 | 60 | 33.3 |
| Not confident | 10 | 13.3 | 46.7 | 23.3 | 40 | 27.3 | 43.3 |
| Cannot measure/diagnose | 16.7 | 13.3 | 20 | 6.7 | 40 | 0 | 23.3 |
Table 5.
Confidence of health providers in detecting pregnancy related complications [End-line; n = 32]
| Anteparturm hemorrhage | Transverse lie | Placenta previa | Breech presentation | Ectopic pregnancy | Twins | Poly/oligo hydromnious | |
|---|---|---|---|---|---|---|---|
| Very confident | 29.03 | 45.16 | 25.81 | 41.94 | 19.35 | 25.81 | 25.81 |
| Confident | 67.74 | 41.94 | 41.94 | 51.61 | 29.03 | 54.84 | 29.03 |
| Not confident | 3.23 | 9.68 | 19.35 | 6.45 | 32.16 | 12.9 | 29.03 |
| Cannot measure/diagnose | - | 3.23 | 12.9 | - | 19.35 | 6.45 | 16.13 |
The results include also increase in referrals made to higher facilities from the study dispensaries. During baseline, only 148 obstetric referrals were made to the higher facilities (based on clinical guidelines of the ministry of health rather than actual detection of pregnancy related complications). At endline, a total of 765 referrals were made (comprising both those according to clinical guidelines and detected using the Vscan) after introducing the Vscan in the district. Although there was no baseline data for compliance of referral before the study started, the study realized 78 % compliance among women who were referred to higher facilities.
Discussion
Results from this study add to the body of knowledge currently available on strategies and interventions that can boost improvement in ANC utilization. While many interventions had been tied to the socio-cultural and health system factors [6, 9] the technological angle has not received a significant attention in this area [10]. Some studies have tried to improve ANC attendance through incentives such as cash and other physical goods and materials. In other places in Tanzania, locally inverted enforcement mechanisms such as fining a partner whose wife/partner has not attended one or all of ANC clinics have been tried but with less success or if successful then not sustainable [Mbuyita et al. 2007, unpublished observations].
Improvements in technology such as the Vscan are recent scientific positive resolutions that offer alternative solutions in public health [11]. In fact, the reproductive health sector has delayed to take advantage of this technology compared to the cardiology sector where quite a number of studies have been conducted using the device in detecting and managing cardiovascular related problems in rural settings where sophisticated machines are unavailable [12].
The simplicity of the Vscan in its use makes the training to health providers and its application being simple. It also offers a motivational tool to health providers working in rural clinics by building up their confidence [13]. In addition, the technology helps the health providers (majority of whom are less skilled) to make rational and correct decision [14] on the proper management of the pregnant women and or provide referral [15].
This study intends to also provide cost analysis of this intervention which we optimistically perceive to be cheap based on the available data (to be analysed) and when compared to the benefits of the pregnancy outcomes. In studies conducted in Asia, the use of the device was able to help 89 % of women at high risk of complicated delivery change their birth plan after being scanned and complications detected [16]. The improved ability of the rural ANC clinics in which majority of the women access ANC services will translate into reduced traveling distances hence less indirect cost in accessing maternal health services in addition to improved pregnancy outcomes [17] whose value cannot be compared in monetary terms.
Finally, compliance to referrals has been reported by several studies to be a problem in maternal health. Because of the traveling cost, lack of accommodation and food of the people accompanying the referred woman, long distances to the referral facilities and perceived loss of household income when bread winners have to accompany the woman to a referral facility, many women have not complied to referrals given. The high percentage of women who complied to the referral provided to them in the study area suggest that women and their families need a convincing evidence to make them believe that there is a need for a referral. Such convincing power can be offered by visual images from ultrasound scanning shown to the family.
Conclusions
This study concludes that, the introduction of the Vscan for routine ultrasound scanning as part of integrated ANC services has an effect to motivating women to attend ANC clinics four times or more. It also has an effect to making women comply to referrals provided in cases where complications were detected and in turn motivate women to deliver in health facilities.
Acknowledgements
The list of those who deserve to be acknowledged following completion of the work that lead to this publication is long. The authors would like to acknowledge all of them in a general statement and that their contribution during the project design and set up, approval, implementation, data collection, data processing and drafting the manuscript is very invaluable. Out of the long list, we would like to name a few due to their specific and vital contributions. These include the District Executive Director of Kisarawe District Council, District Medical Officer of Kisarawe district, The Medical Doctor in-charge of Kisarawe District hospital and The District Reproductive and Child Health Coordinator. We also acknowledge all health providers from the health facilities that were involved in the project. We are also grateful to GE Healthcare East Africa Services Limited who funded and supported the project [Grant number MWO/9292998].
This work was supported by GE Healthcare East Africa Services Limited [Grant number MWO/9292998].
Abbreviations
- ANC
Antenatal Care
- IHI
Ifakara Health Institute
- IRB
Institutional Review Board
- MDG
Millennium Development Goals
- TDHS
Tanzania Demographic Health Surveillance
Footnotes
Competing interests
All authors declared that they have no competing interest.
Authors’ contribution
SM prepared the draft manuscript for this publication. RT collected the data used for publication and reviewed the manuscript. RG collected the data used for publication and reviewed the manuscript. IK collected the data used for publication and reviewed the manuscript. JS conducted data analysis for this publication. GM reviewed the manuscript. All authors read and approved the final manuscript.
Authors’ information
SM is a research scientist and a public health specialist with over fifteen years’ experience in research. He has worked for Ifakara Health Institute for the last 14 years and in the last 8 years has conducted and lead implementation research on maternal, newborn and child health across the United Republic of Tanzania.
RT is a Medical Doctor working for Ifakara Health Institute as a Research Officer. He has been with the institute for 7 years and has participated in several clinical trials and implementation research projects. He is a national tutor for malaria especially malaria diagnostics.
RG is a young research officer currently employed by Ifakara Health Institute. She is a fast learning researcher with eagerness and vigour for growth. Her basic training is on social welfare and social protection and she serves as a social research officer at the institute.
IK is a research scientist at Ifakara Health Institute with over 8 years experience. She has been one of the potential members of the institute in socio-behavioural studies and managing qualitative data. She holds Masters in Management and Business Administration.
JS holds MSs in statistics and has developed strong capabilities in research designs, data analysis and interpretation. She is a Research scientist with over 8 years working experience currently employed by Ifakara Health Institute.
GM holds a PhD in Obs and Gyn. He is a senior scientist with over 25 years experience in research and over 35 years of practice as a Medical doctor specialist in obstetrics and gynaecology. He has published widely and is one of the world recognized champions of maternal health. He has received several global awards and recognition due to his contributions in innovating for locally feasible intervention to reduce maternal mortality in developing countries.
References
- 1.National Bureau of Statistics and ICF Macro. Tanzania Demographic Health Survey. United Republic of Tanzania. 2004.
- 2.National Bureau of Statistics and ICF Macro. Tanzania Demographic Health Survey. United Republic of Tanzania. 2010
- 3.United republic of Tanzania (URT). National Strategy for Growth and Reduction of Poverty. Vice President’s Office. 2005
- 4.Ministry of Health and Social Welfare. Human Resource for Health Strategic Plan-2008 – 2013. United Republic of Tanzania. 2008
- 5.Mwifadhi M, Schellenberg JA, Mushi AK. Factors affecting home delivery in rural Tanzania. Tropical Med Int Health. 2007;12(7):862–872. doi: 10.1111/j.1365-3156.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- 6.Mwifadhi M, Brigit O, Joanna Armstrong S. The use of antenatal and postnatal care: perspectives and experiences of women and health care providers in rural southern Tanzania. BMC Pregnancy Childbirth. 2009;9:10. doi: 10.1186/1471-2393-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahluwaliaa IB, Schmidb T, Kouletioc M, Kanendac O. An evaluation of a community-based approach to safer motherhood in north-western Tanzania. International Journal of Gynecology and Obstetrics: Special article; 2003. [DOI] [PubMed] [Google Scholar]
- 8.de Savigny D, Charles M, Eleuther M, Honorati M, Abdulatif M, Yahya M, Harun K, Graham R, Conrad M. Care-seeking patterns for fatal malaria in Tanzania. Malar J. 2004;3:27. doi: 10.1186/1475-2875-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pieter N, Dennis P. Shared antenatal care for Indigenous patients in a rural and remote community. Aust Fam Physician. 2003;32:3. [PubMed] [Google Scholar]
- 10.Brunette W, Gerard W, Hicks MA. Portable Antenatal Ultrasound Platform for Village Midwives. ACM DEV’10. 2010. London, United Kingdom
- 11.Choi BG, Mukherjee M, Dala P. Interpretation of Remotely Downloaded Pocket-Size Cardiac Ultrasound Images on a Web-Enabled Smartphone: Validation Against Workstation Evaluation. J Am Soc Echocardiogr. 2011. [DOI] [PubMed]
- 12.Nuno C, Covadonga Fernandez G, Daniel F. Usefulness of a New Miniaturized Echocardiographic System in Outpatient Cardiology Consultations as an Extension of Physical Examination. J Am Soc Echocardiogr. 2011;24:117–124. doi: 10.1016/j.echo.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Marjolein D, Pham Viet C, Le Vu A, Tim M. Identifying factors for job motivation of rural health workers in North Viet Nam. Hum Resour Health. 2003;1:10. doi: 10.1186/1478-4491-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powers J, Kremkau F. Medical ultrasound systems. R Soc. 2011. [DOI] [PMC free article] [PubMed]
- 15.Robert H, William M. Compact ultrasound for improving maternal and perinatal care in low resource settings. Review of potential benefits, implementation challenges and health issues. J Ultrasound Med. 2009;28:1067–1076. doi: 10.7863/jum.2009.28.8.1067. [DOI] [PubMed] [Google Scholar]
- 16.Ballard K, Gari L, Mosisa H, Wright J. Provision of individualised obstetric risk advice to increase health facility usage by women at risk of a complicated delivery: a cohort study of women in the rural highlands of West Ethiopia. BJOG. 2013 doi: 10.1111/1471-0528.12190. [DOI] [PubMed] [Google Scholar]
- 17.Nelson BP, Melnick ER, Li J. Portable ultrasound for remote environments, part i: feasibility of field deployment. J Emerg Med. 2011;40(2):190–197. doi: 10.1016/j.jemermed.2009.09.006. [DOI] [PubMed] [Google Scholar]


