Abstract
The use of virtual reality games (known as “exergaming”) as a neurorehabilitation tool is gaining interest. Therefore, we aim to collate evidence for the effects of exergaming on the balance and postural control of older adults and people with idiopathic Parkinson’s disease (IPD). Six electronic databases were searched, from inception to April 2015, to identify relevant studies. Standardized mean differences (SMDs) and 95% confidence intervals (CI) were used to calculate effect sizes between experimental and control groups. I2 statistics were used to determine levels of heterogeneity. 325 older adults and 56 people with IPD who were assessed across 11 studies. The results showed that exergaming improved static balance (SMD 1.069, 95% CI 0.563–1.576), postural control (SMD 0.826, 95% CI 0.481–1.170), and dynamic balance (SMD −0.808, 95% CI −1.192 to −0.424) in healthy older adults. Two IPD studies showed an improvement in static balance (SMD 0.124, 95% CI −0.581 to 0.828) and postural control (SMD 2.576, 95% CI 1.534–3.599). Our findings suggest that exergaming might be an appropriate therapeutic tool for improving balance and postural control in older adults, but more large-scale trials are needed to determine if the same is true for people with IPD.
Keywords: Parkinson’s, balance, exergaming, older, adults
Introduction
Idiopathic Parkinson’s disease (IPD) is the second most common neurological disease worldwide, affecting approximately 1% of all older adults aged 65 years or older (Moore et al., 2005; Lees et al., 2009). People with IPD experience tremors, rigidity, slowness of movement, and gait and balance dysfunction (Dibble et al., 2004; Lees et al., 2009; Zettergren et al., 2011). The balance impairments, which progressively worsen over time, increase the risk of falls, fall-related injuries, and mortality (Bloem et al., 2001; Wood et al., 2002) found 68.3% of people with IPD fell at least once per year, while 50.5% were recurrent fallers (two or more falls per year), while Lindholm et al. (2015) found 31% people with IPD reported nearly falling in the previous 12 months. Medications, such as levodopa, are often the first line of treatment for IPD and have shown promise in improving motor function in the early stages of the disease (Singh et al., 2007; Lees et al., 2009). However, the long-term efficacy of these treatments are poor, and levodopa therapy does little to preserve balance during the more advanced stages of the disease when balance is typically most affected (Bloem et al., 1996; Hely et al., 2005).
Exergaming, in this instance, is a term used to describe computer games that require players to physically move in response to game demands and/or an on-screen avatar (usually constructed from a sensor that records the player’s physical characteristics). Examples of exergaming models include interactive 3-Dimensional gaming modules, such as the Nintendo Wii Fit and the X-Box Kinect. Exergaming has the potential to facilitate balance improvements, including reducing standing center of pressure (CoP) variability (Rendon et al., 2012; Toulotte et al., 2012; Bieryla and Dold, 2013; Wuest et al., 2014), in a home-based setting for older adults (Miller et al., 2014) and for people recovering from spinal cord injury, brain injury (Betker et al., 2007 or stroke (Hung et al., 2014) who have severe balance impairments.
The wide variety of commercially available exergames and the scope of exergaming intensity levels allow for interventions to be tailored to target-specific aspects of balance (Kahlbaugh et al., 2011; Chao et al., 2014). Additionally, the range of exergames available to the consumer can stimulate diversity within training programs, which can aid in creating a fun and engaging “virtual” atmosphere (Barry et al., 2014; Ravenek et al., 2015). Such an environment is conducive to high levels of exercise adherence and participant motivation (Ravenek et al., 2015), which is likely to enhance the efficacy of the training. Duque et al. (2013) and Wuest et al. (2014) presented high interventional compliance rates (97 and 100%, respectively) in their exergaming interventions, though like many of the current exergaming studies, long-term exercise adherence was not reported. Moreover, some games include demanding cognitive and/or motor tasks that may be beyond the capability of people with IPD (Dos Santos Mendes et al., 2012). This may cause frustration and in turn cause people with IPD to avoid the games altogether (Dos Santos Mendes et al., 2012). This highlights the importance of individualized rehabilitation programing to effectively improve balance (Dos Santos Mendes et al., 2012).
Previous exergaming studies have attempted to quantify static and dynamic balance using the Berg balance scale (BBS) (Berg, 1989) and the Timed Up-and-Go test (TUG), for older adults (Agmon et al., 2011; Bateni, 2012; Franco et al., 2012), and for people with IPD (Zettergren et al., 2011; Mhatre et al., 2013). These tests are low-cost, simplistic assessments that are relatively quick to administer and convenient in the clinical setting. However, the subjective nature of these tests and their questionable sensitivity to detect slight changes in CoP deviation compared to posturographic technologies (Black, 2001) highlight the problematic use of these tests. Furthermore, of the current available exergaming randomized control trials (RCTs), there appears to be limited posturographic reporting of static or dynamic balance for older adults, and we know of only one RCT that has used posturography to report balance changes following exergaming for people with IPD (Yen et al., 2011).
Exergaming has the potential to increase exercise adherence, balance confidence, and exercise enjoyment (Barry et al., 2014; Miller et al., 2014; Ravenek et al., 2015), but it is unclear if it can improve the balance of people with IPD (Agmon et al., 2011; Meldrum et al., 2012; Holmes et al., 2013; Barry et al., 2014). There is limited evidence to suggest exergaming is an efficacious rehabilitation method for balance and postural issues experienced by older people and people with IPD. Therefore, we intend to systematically review exergaming RCTs and use a meta-analytical approach to compare the effects of exergaming on the balance of older adults and people with IPD.
Methods
Search strategy
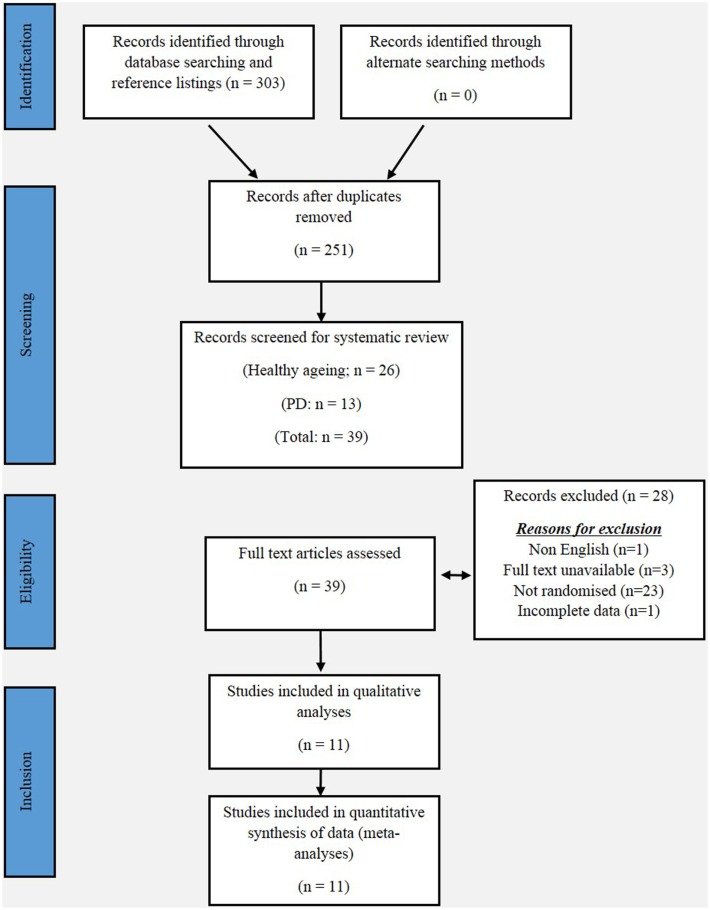
This review has been informed by the PRISMA statement. The following electronic databases were searched from their inception to April 2015: PubMed, MEDLINE, PsycINFO, Embase, Google Scholar, and Scopus. The following keywords were used in combinations: Parkinson, Parkinson’s disease, Parkinsonism, exergaming, gaming, virtual reality gaming, series gaming, gait, balance, aged, and elderly. Additionally, the reference lists of the included studies were also searched. Figure 1 shows a flow diagram of the processing of search results from initial searches to the final included studies.
Figure 1.
PRISMA flow chart for the selection of studies included in this meta-analyses.
Inclusion criteria
To determine the eligibility of each study, the title and abstract were screened independently by a single reviewer (Dale M. Harris). Studies were included if (1) it was printed in full English text, (2) the aim of the study was to examine the effects of exergaming on the static and dynamic balance of older adults and/or people with IPD, (3) the target population was aged 65 years or older, (4) the main intervention was exergaming, serious gaming, or virtual reality gaming, and (5) the effects of the gaming intervention were compared to either a control group, or an alternative training/rehabilitation intervention, including other forms of exercise, balance training, or scheduled general physical activity. All studies included were randomized, and only published articles (including articles in press) were included. All duplicate articles were removed.
Quality assessment of studies
Data were extracted by an independent reviewer (Dale M. Harris), and revised by a second reviewer (Wei-Peng Teo). The methodological quality of each study was independently assessed by two reviewers (Liam Johnson and Timo Rantalainen) using the physiotherapy evidence database (PEDro) scale (ranging from 0 to 10 points). The PEDro scale is an assessment tool for evaluating methodological quality of RCTs conducted in the field of physiotherapy with fair-to-good reliability (Maher et al., 2003). Any disagreements in scores were resolved by discussion between reviewers, with the judgment of the primary author (Dale M. Harris) being sought if consensus could not be reached. All scores assigned to each study were agreed upon by unanimity and are presented in Table 4.
Table 4.
Description of the study assessing postural control in people with IPD.
| Study | Assessment of postural control | VR intervention (n) | Control (n) | Total (n) | SMD | SE | 95% CI |
|---|---|---|---|---|---|---|---|
| Yen et al. (2011) | Mean equilibrium scores from six sensory organizational tests | 14 | 14 | 28 | 2.567 | 0.502 | 1.534–3.599 |
Selection of outcome measures
For the purpose of our meta-analysis, we categorized the balance outcome measures into static and dynamic assessments. We chose the BBS (Berg et al., 1991) as our measure of static balance. The BBS (Berg et al., 1991) consists of 14 balance-challenging tasks, whereby the participants base of support remained fixed, or moved marginally, and each task is scored on a 0–4 scale (maximum score = 56). A higher score is indicative of better balance (Thorbahn and Newton, 1996).
We have also used postural control (PC) measures as assessments of static balance because they required no (or limited) movement of the participants base of support. Studies employing motion capture technology that were capable of quantifying the amount of postural sway circumference or CoP deviation, including posturographic measures, force plates, digital sway meters, virtual avatars, or Wii balance-board technology, were included as measures of PC.
We identified the TUG test, which involves the purposeful movement of the participants base of support, as a measure of dynamic balance. The TUG measures the total time (seconds) that an individual takes to rise from a chair, walk at a fast pace for 3-m, turn around, walk back and sit on the same chair (Podsiadlo and Richardson, 1991).
Data synthesis and analysis
A random effects meta-analysis was conducted with MedCalc Statistical Software v14.12.0 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org: 2015). Continuous measures extrapolation yielded standardized mean difference (SMD) results, which were used as a measure of effect size, along with 95% confidence intervals (CI). Heterogeneity across studies was tested based on I2 statistics, which indicates the percentage of variance that is attributable to study heterogeneity. Studies with I2 < 40% was considered to have low heterogeneity, I2 = 40–75% was considered to have moderate heterogeneity, and I2 > 75% was considered to have high heterogeneity. Fisher’s method of combining p-values was applied to test for overall effects for each outcome measure.
Results
Study selection
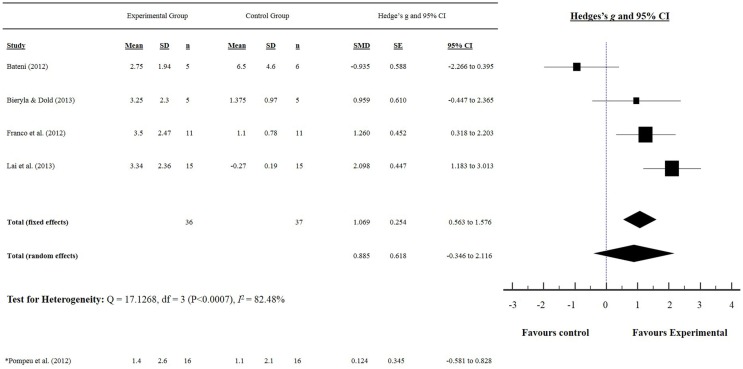
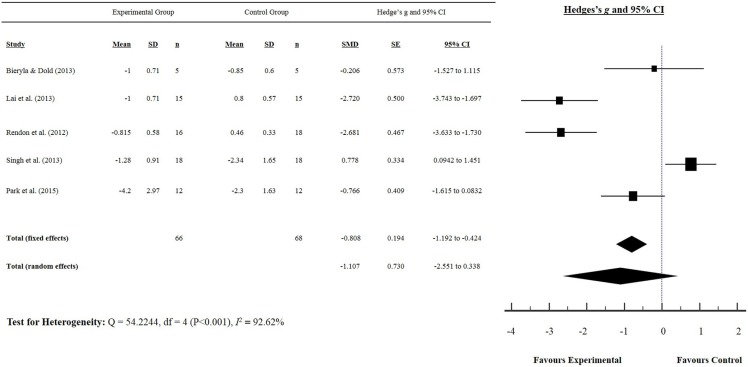
Our initial search yielded 303 articles. Following screening of the title and abstract, and removal of duplicates, 11 studies were included in our meta-analysis, and are summarized in Tables 1 and 2. Five studies reported a measurement of static balance (BBS) (Bateni, 2012; Franco et al., 2012; Pompeu et al., 2012; Bieryla and Dold, 2013; Lai et al., 2013) (Figure 2), and five studies reported a measurement of dynamic balance (TUG) (Rendon et al., 2012; Bieryla and Dold, 2013; Lai et al., 2013; Singh et al., 2013; Park et al., 2015) (Figure 3). Seven studies reported a measurement of PC (Yen et al., 2011; Bateni, 2012; Toulotte et al., 2012; Kim et al., 2013; Lai et al., 2013; Singh et al., 2013; Park et al., 2015) (Table 3).
Table 1.
Characteristics of exergaming randomized controlled trials studies among people with IPD.
| Author | Sample size, mean age (years) ± SD | Hoehn and Yahr stage | Medications | Duration (weeks) | Main outcome assessments | Intervention groups | Control group |
|---|---|---|---|---|---|---|---|
| Pompeu et al. (2012) | n = 32 VR and CON 67.4 ± 8.1 | 1 and 2 | Levodopa therapy-outcome measures and training interventions were performed during “on” phase | 7 | UPDRS-II | VR and cognitive training + global exercises (1 h, 2 sessions/week) | TBT |
| Static balance | • 10 min of warming, stretching and active exercises; 10 min of resistance exercises for limbs; and 10 min of exercises in diagonal patterns for trunk, neck and limbs | • 10 exercises (5 per session, 2 trials of each) that were equivalent to the motor demands of the Wii training group, but without the provision of external cues, feedback, and cognitive stimulation | |||||
| Dynamic balance | • 10 min dynamic balance: Table Tilt, Tilt City, Soccer Heading and Penguin Slide | ||||||
| • 10 min static balance: rhythm parade, obstacle course, basic step, and basic run | |||||||
| Yen et al. (2011) | n = 42 VR 70.4 ± 6.5; TBT 70.1 ± 6.9; CON 71.6 ± 5.8 | 2 and 3 | Levodopa therapy-outcome measures and interventions were performed during “on” phase | 6 | Postural control | VR balance training (30 min, 2 sessions/week) | NI |
| Verbal reaction time | • 10 min warm up | ||||||
| • VR training: 10 min of a 3D ball-rolling game and 10 min of indoor-outdoor virtual activities | |||||||
| TBT | |||||||
| • 10 min warm up, 20 min of TBT | |||||||
| • Static stance: participants stood on pieces of foam with eyes open or closed for approximately 60 s difficulty was increased by adding more foam pieces and reducing the base of support | |||||||
| • Dynamic weight shifting: a ball was thrown at patients from multiple directions, ball was caught after stepping forward and squatting | |||||||
| • Addition of a tilt board was used as external perturbation to facilitate postural reflexes under both static and dynamic conditions |
Table 2.
Characteristics of exergaming randomized controlled trials studies among older adults.
| Author | Participant number mean age (years) ± SD | Duration (weeks) | Main outcome assessed | Intervention groups | Control group |
|---|---|---|---|---|---|
| Bateni (2012) | n = 8 VR 79 ± 13; PA 72 ± 12; COMBI 68 ± 14 | 4 | Static balance | VR (3 sessions/wk) | NI |
| • Wii Fit games: Ski Slalom, Ski Jump and Table Tilt | |||||
| PA (3 sessions/wk) | |||||
| • Standard strength, balance and postural exercises | |||||
| COMB (3 sessions/wk) | |||||
| • Combination of both physical therapy and Wii Fit games | |||||
| Bieryla and Dold (2013) | n = 12 VR 82.5 ± 1.6; CON 80.5 ± 7.8 | 3 | Static balance | VR (30 min, 3 sessions/wk) | NI |
| • Training consisted of: half-moon, chair, warrior, torso twists, soccer heading and ski jump | |||||
| • All maneuvers were chosen from the yoga, aerobic and balance game modes | |||||
| Franco et al. (2012) | n = 32 VR 79.8 ± 4.7; CON 76.9 ± 6.3 | 3 | Static balance Dynamic balance Health and wellbeing |
VR (10–15 min, 5 separate sessions) • Wii Fit group: received Wii Fit balance training and completed supplemental home exercises |
Completed exercises from the MOB Program, administered by the staff exercise physiologist |
| Kim et al. (2013) | n = 32 VR 68.28 ± 3.7; CON 65.83 ± 3.7 | 8 | Hip muscle strength Ground reaction force |
VR (3 sessions/wk) • “Your Shape Fitness Evolved” software: includes movements derived from exercise programs based on Tai Chi and yoga • Bilateral shoulder abduction, and single-leg abduction • Abduction of the right (or left) arm to shoulder level with elbow flexion at 90°, and abduction of the ipsilateral leg with knee flexion at 90° • Abduction of the arms to shoulder level and flexion of both knees at 90° • Crossed arms in front of chest in a standing position with the feet splayed outward and the knees flexed at 90° |
NI |
| Lai et al. (2013) | n = 30 VR 70.6 ± 3.5; CON 74.5 ± 4.7 | 6 | Functional performance Static balance Stability confidence Postural control XMSS stepping test |
VR (3 sessions/wk) • Subjects performed following movements: quiet stance, sitting-to-standing, shifting weight and reaching, turning in place, standing on one leg, and maintaining a tandem stance • Virtual reality XMSS stepping test procedures |
NI |
| Park et al. (2015) | n = 24 VR 66.55 ± 8.1; BE 65.2 ± 7.9 | 8 | Static balance | VR (30 min, 3 sessions/wk) | BE (30 min, 3 sessions/wk) |
| Dynamic balance | • Participants spent 10 min on each of the Wii fit balance games including soccer heading, snowboard slalom, and table tilt | 20 min bouncing, pelvic tilting laterally, pelvic tilting anterior-posterior, and the pelvic circling while sitting on an exercise ball | |||
| 10 min tilting the body to the right and left sides while putting their feet on the ball in a supine position, bending the knees and performing a hamstring bridge | |||||
| Rendon et al. (2012) | n = 40 VR 85.7 ± 4.3; CON 83.3 ± 6.2 | 6 | Dynamic balance Static balance Balance confidence |
VR (35–45 min, 3 sessions/wk) • Lunges • Single-leg extensions • Twists |
NI |
| Singh et al. (2013) | n = 36 VR 61.12 ± 3.72; CB 64 ± 5.88 | 6 | Agility | VR (40 min, 2 sessions/wk) | TBT prescribed by Seidler and Martin (1997) |
| Dynamic balance | • Ski slalom | ||||
| Functional mobility | • Table tilt | ||||
| Postural control | • Penguin slide | ||||
| • Soccer heading | |||||
| • Tight rope walk | |||||
| • Perfect 10 | |||||
| • Tilt city | |||||
| Toulotte et al. (2012) | n = 36 VR 72.2 ± 8.6; CON 71.8 ± 8.0 | 20 | Static balance Dynamic balance “Wii Fitness” |
PA (1 h, 1 sessions/wk) • Exercises to increase step length, step height, the mobility of the cervical rachis and ocular mobility in order to develop muscular strength, proprioception, flexibility, static balance, and dynamic balance with eyes open and eyes closed VR (1 h, 1 session/wk) • Heading soccer, ski jumping, yoga, downhill skiing, game balls, and tight rope walker COMBI (30 min PA, 30 min VR, 1 session/wk) • Same PA and Wii Fit exercises as above, with half the repetitions of both groups |
NI |
PA, physical activity; NR, not reported; NI, no intervention; TBT traditional balance training; VR, virtual reality; COMB, combination of both; UPDRS, unified Parkinson’s disease rating scale; MOB, matter of balance; BE, ball exercise; wk, week.
Figure 2.
Static balance: Berg balance scale score. (*) indicates only IPD study that used the BBS as a measure of static balance.
Figure 3.
Dynamic balance: timed up and go test score for older adults.
Table 3.
Description of studies assessing postural control in older adults.
| Study | Assessment of postural control | VR intervention (n) | Control (n) | Total (n) | SMD | SE | 95% CI | t | p |
|---|---|---|---|---|---|---|---|---|---|
| Bateni (2012) | Wii Fit game (Bubble Test) pre-post score: requires participants to maneuver their center of body mass in a controlled manner within a VR environment | 5 | 6 | 11 | −0.960 | 0.590 | −2.294 to 0.375 | ||
| Kim et al. (2013) | Ground reaction force plate: backward step test with eyes open | 18 | 14 | 32 | 1.412 | 0.390 | 0.617–2.208 | ||
| Lai et al. (2013) | Catsys 2000 system: a platform with 3 orthogonal strain gage devices | 15 | 15 | 30 | 1.487 | 0.404 | 0.660–2.315 | ||
| Park et al. (2015) | Static postural sway length (mm) measurement system: “Biorescue” | 12 | 12 | 24 | 0.636 | 0.405 | −0.203 to 1.475 | ||
| Singh et al. (2013) | Intelligent balance board: combined scores to obtain an overall performance rating score | 18 | 18 | 36 | 1.328 | 0.362 | 0.593–2.063 | ||
| Toulotte et al. (2012) | Estimated a percentage of center of gravity score by using “Wii Fit” balance assessment VR tool | 9 | 9 | 18 | 1.578 | 0.520 | 0.475–2.681 | ||
| Total (fixed effects) | 77 | 74 | 151 | 0.826 | 0.174 | 0.481–1.170 | 4.738 | <0.001 | |
| Total (random effects) | 77 | 74 | 151 | 0.714 | 0.454 | −0.184 to 1.611 | 1.571 | 0.118 |
Participant characteristics
In total, 225 older adults (experimental = 115, control = 110) and 56 people with IPD (experimental = 28, control = 28) were assessed across 11 studies. The mean age ±SD for the older adults was 73.32 ± 7.35 (experimental 73.97 ± 8.19 years, control 72.67 ± 6.84 years), while the mean age for people with IPD was 69.8 ± 2.16 (experimental 68.9 ± 2.12, control 71.6 ± 5.8). The mean duration of IPD was 6.9 ± 1.27 years, and disease severity, as assessed by the Hoehn and Yahr scale (Hoehn and Yahr, 1998), ranged from 1 to 3 (mild to moderate disease severity).
Methodological quality
The scores for each criterion using the PEDro scale are presented in Table 5. The mean score for all 11 trials was 5.3 ± 1.5. Across the 11 studies, neither the participants nor the therapists administering the program were blinded to the intervention. Only one study concealed the allocation of all participants, used blinded assessors, and employed intention-to-treat analysis (Yen et al., 2011).
Table 5.
PEDro scale of quality for eligible randomized controlled trials.
| Study | Random allocation | Concealed allocation | Similar at baseline | Subjects blinded | Therapists blinded | Assessors blinded | <15% dropout | Intention-to-treat analysis | Between group comparisons | Point measures and variability data | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bateni (2012) | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 5 |
| Bieryla and Dold (2013) | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| Franco et al. (2012) | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Kim et al. (2013) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Lai et al. (2013) | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 4 |
| Park et al. (2015) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Pompeu et al. (2012) | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Rendon et al. (2012) | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Singh et al. (2013) | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Toulotte et al. (2012) | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 4 |
| Yen et al. (2011) | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
Static balance: Berg balance scale
The effects of exergaming on static balance were examined by pooling post-intervention data from the five studies that reported BBS results from older adults and people with IPD (experimental n = 52, control n = 53) (Figure 2). Overall, the pooled results showed a significant improvement in static balance for older adults, as evidenced by increased BBS scores post-intervention (SMD 1.069, 95% CI 0.563–1.576). Pompeu et al. (2012) was the only study to examine the effect of exergaming on the balance of people with IPD and showed a favorable effect (i.e., an improvement in BBS score) (SMD 0.124, 95% CI −0.581 to 0.828). Only Bateni (2012) showed a non-favorable effect (i.e., a reduction in BBS score) for the exergaming intervention group (SMD −0.935, 95% CI −2.266 to 0.395) of older adults.
Dynamic balance: Timed up and go test
The effects of exergaming on dynamic balance were examined by pooling post-intervention data from the five studies that reported TUG test results of older adults and people with IPD (experimental n = 66, control n = 68) (Rendon et al., 2012; Bieryla and Dold, 2013; Lai et al., 2013; Singh et al., 2013; Park et al., 2015) (Figure 3). Our findings showed a significant improvement in TUG (SMD −0.808, 95% CI −1.192 to −0.424), as indicated by a negative score (i.e., reduction in TUG time). Singh et al. (2013) was the only study to show a non-favorable effect following a 6-week exergaming intervention for older adults (SMD 0.778, 95% CI 0.0898–1.466).
Postural control
Tables 3 and 4 summarize each study and their effect sizes regarding exergaming and PC in older adults (Table 3) and people with IPD (Table 4). Collectively, our results suggest that exergaming improves PC in older adults (SMD 0.826, 95% CI 0.481–1.170). Only Bateni (2012) reported a non-favorable effect following a 4-week exergaming and physical therapy training intervention for older adults (SMD −0.960, 95% CI −2.294 to 0.375). Yen et al. (2011) was the only study to investigate exergaming and PC of people with IPD, and found a significant improvement in PC for people with IPD (SMD 2.576, 95% CI 1.534–3.599).
Discussion
This study is the first to cohesively present the effects of exergaming on the balance of older adults and people with IPD. Our systematic review of the literature found limited robust evidence for the effects of exergaming on the balance of older adults and people with IPD. Of the RCTs included in our meta-analysis, the methodologies are not comprehensive enough to definitively elucidate if exergaming affects the balance of older adults or people with IPD. Our meta-analysis showed that no RCTs used the TUG as a measure of dynamic balance of people with IPD, and only two RCTs measured static balance using the BBS (Pompeu et al., 2012) or PC measures (Yen et al., 2011) for people with IPD. However, we found exergaming improves the static (BBS and PC measures) and dynamic (TUG) balance of older adults, despite the variability in PC measures used. Therefore, while our meta-analysis might suggest that exergaming can improve the balance of older adults, it remains largely unknown if the same is true for people with IPD due to a lack of sufficient evidence.
Only Bateni (2012) and Singh et al. (2013) found the static and dynamic balance of older adults was not improved by exergaming. An explanation for this could arise from their respective methodologies; the control groups for both studies included exercise interventions that specifically targeted balance (i.e., one-leg standing, free leg swinging, and moving objects), which may have contributed to the lack of effects found. These results might indicate that exergaming can improve balance as much as balance-specific training among older adults, which has previously been reported (Bateni, 2012; Franco et al., 2012; Toulotte et al., 2012; Singh et al., 2013).
It is beyond the scope of this study to determine the mechanisms responsible for the improvements in balance indicated by our meta-analysis. However, we can speculate that exergaming might provide a novel setting conducive to enhancing an individual’s ability to learn and perform new skills. For people with IPD who experience difficulties learning new skills (Scandalis et al., 2001; Dos Santos Mendes et al., 2012), the stimulus provided by exergaming might be strong enough to induce implicit learning (Mirelman et al., 2011). Additionally, immediate biofeedback of performance may also account for the augmented balance improvements of older adults (Bisson et al., 2007; Heiden and Lajoie, 2010; Franco et al., 2012; Cho et al., 2014; Wuest et al., 2014). Caudron et al. (2014) postulated that visual immersion provides a strong biofeedback cue for improving PC for people with IPD, although the effects of biofeedback on the balance of people with IPD is not clear. However, speculation of the opposite that certain exergames considered too challenging (i.e., exergames requiring dual tasking or decisive movements) might impair balance improvements for people with IPD has also been suggested (Dos Santos Mendes et al., 2012; Galna et al., 2014). Moreover, many interventions conducted in the clinical setting are unlikely to be replicated in the home setting, highlighting the importance of selecting appropriate exergames so that people with IPD can safely and effectively perform the tasks from home.
We have identified that static balance, indicative of PC changes, among older adults can be improved by exergaming, and Yen et al. (2011) demonstrated improvements in the PC of people with IPD. Interestingly, there were inconsistencies in effect sizes seen in both IPD studies compared with the pooled effects of older adults, with Yen et al. (2011) having a much larger effect size compared with Pompeu et al. (2012). To provide some explanations, Pompeu et al. (2012) contrasted an exergaming group against a traditional balance training group, while Yen et al. (2011) did not adopt an intervention for their control group providing a sound reason for the disparate results. Yen and colleagues used a combination of exergaming and traditional balance training in their intervention group. Furthermore, it is likely that the study by Yen and colleagues used participants that are between Hoehn–Yahr stages II and III, which may have allowed for the larger balance effects seen in Yen et al. (2011). Finally, IPD participants in both studies were using medication at the time of intervention, which can improve functional balance in the early stages of the disease (Nova et al., 2004), potentially reducing the effects of exergaming on balance in Pompeu et al. (2012).
The use of simplistic assessments to quantify static and dynamic balance presents as a limitation in the current exergaming literature, with posturography not commonly used. Posturography provides a more valid tool for effectively measuring static and dynamic balance, but can be costly and inaccessible for many clinicians. Alternatively, Wii balance-board technology is commercially accessible, and has previously shown high validity and reliability in mapping CoP deviation for older adults during static stance (Clark et al., 2010; Chang et al., 2013), but no evidence exists validating Wii balance-board technology and CoP deviation for people with IPD.
Our average PEDro score of 5.3 suggests that the studies included were of moderate methodological quality (Moseley et al., 2002). A lack of concealed allocation of participants, double blinding, and intention-to-treat analysis present as limitations of the methodology of the current exergaming literature. Furthermore, non-English studies were excluded here, and this presents as another limitation in the applicability of non-English exergaming literature. Lastly, only two of the studies included targeted people with IPD. Resultantly, our findings may not represent the larger community of people with IPD. Nevertheless, we deliberately included only RCT studies in an attempt to raise the standard of methodological quality. As such, while the IPD studies included were underwhelming, we have shown that there is a need for more robust, comprehensive studies on exergaming for people with IPD.
Our systematic review and meta-analysis demonstrates that exergaming can improve the balance of older adults. However, with the current available studies, the efficacy of exergaming cannot be sufficiently determined for people with IPD. While a non-favorable training effect was identified in two studies included in our meta-analysis, both studies implemented balance-specific training interventions for the control group. We interpret this to indicate exergaming has similar effects on balance as balance-specific training. Whether or not this training response is caused by physiological adaptation or neural adaptation is unknown, with the effects of exergaming on balance for people with IPD speculative to this point. As such, more robust RCT evidence is required to validate our findings.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Source
This study was supported by the Central Research Grant Scheme (RM29471) and the School of Exercise and Nutrition Sciences, Deakin University. TR is supported by an Alfred Deakin Postdoctoral Fellowship. LJ is supported by the Australian Government’s Collaborative Research Networks program. MM is supported by a Labex NUMEV Fellowship (Digital and Hardware Solutions, Environmental and Organic Life Modeling, ANR-10-LABX-20).
Acknowledgments
All authors are acknowledged for their contributions to this study.
References
- Agmon M., Perry C., Phelan E., Demiris G., Nguyen H. (2011). A pilot study of Wii Fit exergames to improve balance in older adults. J. Geriatr. Phys. Ther. 34, 161–167. 10.1519/JPT.0b013e3182191d98 [DOI] [PubMed] [Google Scholar]
- Barry G., Galna B., Rochester L. (2014). The role of exergaming in Parkinson’s disease rehabilitation: a systematic review of the evidence. J. Neuroeng. Rehabil. 11, 1–17. 10.1186/1743-0003-11-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateni H. (2012). Changes in balance in older adults based on use of physical therapy vs the Wii Fit gaming system: a preliminary study. Physiotherapy 98, 211–216. 10.1016/j.physio.2011.02.004 [DOI] [PubMed] [Google Scholar]
- Berg K. (1989). Measuring balance in the elderly: preliminary development of an instrument. Physiother. Can. 41, 304–311. 10.3138/ptc.41.6.304 [DOI] [Google Scholar]
- Berg K. O., Wood-Dauphinee S. L., Williams J. I., Maki B. (1991). Measuring balance in the elderly: validation of an instrument. Can. J. Public Health 83, S7–S11. [PubMed] [Google Scholar]
- Betker A. L., Desai A., Nett C., Kapadia N., Szturm T. (2007). Game-based exercises for dynamic short-sitting balance rehabilitation of people with chronic spinal cord and traumatic brain injuries. Phys. Ther. 87, 1389–1398. 10.2522/ptj.20060229 [DOI] [PubMed] [Google Scholar]
- Bieryla K. A., Dold N. M. (2013). Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clin. Interv. Aging 8, 775. 10.2147/CIA.S46164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisson E., Contant B., Sveistrup H., Lajoie Y. (2007). Functional balance and dual-task reaction times in older adults are improved by virtual reality and biofeedback training. Cyberpsychol. Behav. 10, 16–23. 10.1089/cpb.2006.9997 [DOI] [PubMed] [Google Scholar]
- Black F. O. (2001). Clinical status of computerized dynamic posturography in neurotology. Curr. Opin. Otolaryngol. Head Neck Surg. 9, 314–318. 10.1097/00020840-200110000-0001111710483 [DOI] [Google Scholar]
- Bloem B. R., Beckley D. J., Van Dijk J. G., Zwinderman A. H., Remler M. P., Roos R. A. (1996). Influence of dopaminergic medication on automatic postural responses and balance impairment in Parkinson’s disease. Mov. Disord. 11, 509–521. 10.1002/mds.870110506 [DOI] [PubMed] [Google Scholar]
- Bloem B. R., Grimbergen Y. A., Cramer M., Willemsen M., Zwinderman A. H. (2001). Prospective assessment of falls in Parkinson’s disease. J. Neurol. 248, 950–958. 10.1007/s004150170047 [DOI] [PubMed] [Google Scholar]
- Caudron S., Guerraz M., Eusebio A., Gros J. P., Azulay J. P., Vaugoyeau M. (2014). Evaluation of a visual biofeedback on the postural control in Parkinson’s disease. Clin. Neurophys 44, 77–86. 10.1016/j.neucli.2013.10.134 [DOI] [PubMed] [Google Scholar]
- Chang W.-D., Chang W.-Y., Lee C.-L., Feng C.-Y. (2013). Validity and reliability of Wii Fit balance board for the assessment of balance of healthy young adults and the elderly. J. Phys. Ther. Sci. 25, 1251. 10.1589/jpts.25.1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao Y.-Y., Scherer Y. K., Montgomery C. A. (2014). Effects of using Nintendo Wii™ exergames in older adults: a review of the literature. J. Aging Health. 27, 379–402. 10.1177/0898264314551171 [DOI] [PubMed] [Google Scholar]
- Cho G. H., Hwangbo G., Shin H. S. (2014). The effects of virtual reality-based balance training on balance of the elderly. J. Phys. Ther. Sci. 26, 615–617. 10.1589/jpts.26.615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R. A., Bryant A. L., Pua Y., Mccrory P., Bennell K., Hunt M. (2010). Validity and reliability of the Nintendo Wii balance board for assessment of standing balance. Gait. Posture 31, 307–310. 10.1016/j.gaitpost.2009.11.012 [DOI] [PubMed] [Google Scholar]
- Dibble L. E., Nicholson D. E., Shultz B., Macwilliams B. A., Marcus R. L., Moncur C. (2004). Maximal speed gait initiation of healthy elderly individuals and persons with Parkinson disease. J. Neurol. Phys. Ther. 28, 2–11. 10.1097/01.NPT.0000284772.09932.dc [DOI] [PubMed] [Google Scholar]
- Dos Santos Mendes F. A., Pompeu J. E., Lobo A. M., Da Silva K. G., De Paula Oliveira T., Zomignani A. P., et al. (2012). Motor learning, retention and transfer after virtual-reality-based training in Parkinson’s disease – effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy 98, 217–223. 10.1016/j.physio.2012.06.001 [DOI] [PubMed] [Google Scholar]
- Duque G., Boersma D., Loza-Diaz G., Hassan S., Suarez H., Geisinger D., et al. (2013). Effects of balance training using a virtual-reality system in older fallers. Clin. Interv. Aging 8, 257–263. 10.2147/cia.s41453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco J. R., Jacobs K., Inzerillo C., Kluzik J. (2012). The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol. Health Care 20, 95–115. 10.3233/THC-2011-0661 [DOI] [PubMed] [Google Scholar]
- Galna B., Jackson D., Schofield G., Mcnaney R., Webster M., Barry G., et al. (2014). Retraining function in people with Parkinson’s disease using the microsoft kinect: game design and pilot testing. J. Neuroeng. Rehabil. 11, 60. 10.1186/1743-0003-11-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiden E., Lajoie Y. (2010). Games-based biofeedback training and the attentional demands of balance in older adults. Aging Clin. Exper. Res. 22, 367–373. 10.3275/6733 [DOI] [PubMed] [Google Scholar]
- Hely M. A., Morris J. G., Reid W. G., Trafficante R. (2005). Sydney multicenter study of parkinson’s disease: non-L-dopa-responsive problems dominate at 15 years. Mov Disord 20, 190–199. [DOI] [PubMed] [Google Scholar]
- Hoehn M. M., Yahr M. D. (1998). Parkinsonism: onset, progression, and mortality. Neurology 50, 318–318. 10.1212/WNL.50.2.318 [DOI] [PubMed] [Google Scholar]
- Holmes J. D., Gu M. L., Johnson A. M., Jenkins M. E. (2013). The effects of a home-based virtual reality rehabilitation program on balance among individuals with Parkinson’s disease. Phys. Occup. Ther. Geriatr. 31, 241–253. 10.3109/02703181.2013.814743 [DOI] [Google Scholar]
- Hung J. W., Chou C. X., Hsieh Y. W., Wu W. C., Yu M. Y., Chen P. C., et al. (2014). Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch. Phys. Med. Rehabil. 95, 1629–1637. 10.1016/j.apmr.2014.04.029 [DOI] [PubMed] [Google Scholar]
- Kahlbaugh P. E., Sperandio A. J., Carlson A. L., Hauselt J. (2011). Effects of playing Wii on well-being in the elderly: physical activity, loneliness, and mood. Activ. Adapt Aging 35, 331–344. 10.1080/01924788.2011.625218 [DOI] [Google Scholar]
- Kim J., Son J., Ko N., Yoon B. (2013). Unsupervised virtual reality-based exercise program improves hip muscle strength and balance control in older adults: a pilot study. Arch. Phys. Med. Rehabil. 94, 937–943. 10.1016/j.apmr.2012.12.010 [DOI] [PubMed] [Google Scholar]
- Lai C.-H., Peng C.-W., Chen Y.-L., Huang C.-P., Hsiao Y.-L., Chen S.-C. (2013). Effects of interactive video-game based system exercise on the balance of the elderly. Gait Posture 37, 511–515. 10.1016/j.gaitpost.2012.09.003 [DOI] [PubMed] [Google Scholar]
- Lees A. J., Hardy J., Revesz T. (2009). Parkinson’s disease. Lancet 373, 2055–2066. 10.1016/S0140-6736(09)60492-X [DOI] [PubMed] [Google Scholar]
- Lindholm B., Hagell P., Hansson O., Nilsson M. H. (2015). Prediction of falls and/or near falls in people with mild Parkinson’s disease. Plos one 10, e0117018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher C. G., Sherrington C., Herbert R. D., Moseley A. M., Elkins M. (2003). Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys ther 83, 713–721. [PubMed] [Google Scholar]
- Meldrum D., Glennon A., Herdman S., Murray D., Mcconn-Walsh R. (2012). Virtual reality rehabilitation of balance: assessment of the usability of the Nintendo Wii((R)) Fit plus. Disabil. Rehabil. Assist. Technol. 7, 205–210. 10.3109/17483107.2011.616922 [DOI] [PubMed] [Google Scholar]
- Mhatre P. V., Vilares I., Stibb S. M., Albert M. V., Pickering L., Marciniak C. M., et al. (2013). Wii Fit balance board playing improves balance and gait in Parkinson disease. PM R 5, 769–777. 10.1016/j.pmrj.2013.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K. J., Adair B. S., Pearce A. J., Said C. M., Ozanne E., Morris M. M. (2014). Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: a systematic review. Age Ageing 43, 188–195. 10.1093/ageing/aft194 [DOI] [PubMed] [Google Scholar]
- Mirelman A., Maidan I., Herman T., Deutsch J. E., Giladi N., Hausdorff J. M. (2011). Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J. Gerontol. A Biol. Sci. Med. Sci. 66, 234–240. 10.1093/gerona/glq201 [DOI] [PubMed] [Google Scholar]
- Moore D. J., West A. B., Dawson V. L., Dawson T. M. (2005). Molecular pathophysiology of Parkinson’s disease. Annu. Rev. Neurosci. 28, 57–87. 10.1146/annurev.neuro.28.061604.135718 [DOI] [PubMed] [Google Scholar]
- Moseley A. M., Herbert R. D., Sherrington C., Maher C. G. (2002). Evidence for physiotherapy practice: a survey of the physiotherapy evidence database (PEDro). Aust. J. Phys. 48, 43–49. 10.1016/S0004-9514(14)60281-6 [DOI] [PubMed] [Google Scholar]
- Nova I. C., Monica R. P., Henrique B. F. (2004). Levodopa effect upon functional balance of Parkinson’s disease patients. Park. Rel. Dis. 10, 411–415. 10.1016/j.parkreldis.2004.04.004 [DOI] [PubMed] [Google Scholar]
- Park E.-C., Kim S.-G., Lee C.-W. (2015). The effects of virtual reality game exercise on balance and gait of the elderly. J. Phys. Ther. Sci. 27, 1157–1159. 10.1589/jpts.27.1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D., Richardson S. (1991). The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39, 142–148. 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- Pompeu J. E., Dos Santos Mendes F. A., Da Silva K. G., Lobo A. M., De Paula Oliveira T., Zomignani A. P., et al. (2012). Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: a randomised clinical trial. Physiotherapy 98, 196–204. 10.1016/j.physio.2012.06.004 [DOI] [PubMed] [Google Scholar]
- Ravenek K. E., Wolfe D. L., Hitzig S. L. (2015). A scoping review of video gaming in rehabilitation. Disabil. Rehabil. Assist. Technol. 1–9. 10.3109/17483107.2015.1029538 [DOI] [PubMed] [Google Scholar]
- Rendon A. A., Lohman E. B., Thorpe D., Johnson E. G., Medina E., Bradley B. (2012). The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 41, 549–552. 10.1093/ageing/afs053 [DOI] [PubMed] [Google Scholar]
- Scandalis T. A., Bosak A., Berliner J. C., Helman L. L., Wells M. R. (2001). Resistance training and gait function in patients with Parkinson’s disease. Am J Phys Med Rehab 80, 38–43. [DOI] [PubMed] [Google Scholar]
- Seidler R. D., Martin P. E. (1997). The effects of short term balance training on the postural control of older adults. Gait Posture 6, 224–236. 10.1016/S0966-6362(97)00012-X [DOI] [Google Scholar]
- Singh D. K., Rajaratnam B. S., Palaniswamy V., Raman V. P., Bong P. S., Pearson H. (2013). Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric 16, 141–146. 10.3109/13697137.2012.664832 [DOI] [PubMed] [Google Scholar]
- Singh N., Pillay V., Choonara Y. E. (2007). Advances in the treatment of Parkinson’s disease. Prog. Neurobio. 81, 29–44. 10.1016/j.pneurobio.2006.11.009 [DOI] [PubMed] [Google Scholar]
- Thorbahn L. D. B., Newton R. A. (1996). Use of the Berg balance test to predict falls in elderly persons. Phys. Ther. 76, 576–583. [DOI] [PubMed] [Google Scholar]
- Toulotte C., Toursel C., Olivier N. (2012). Wii Fit® training vs. adapted physical activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin. Rehabil. 26, 827–835. 10.1177/0269215511434996 [DOI] [PubMed] [Google Scholar]
- Wood B., Bilclough J., Bowron A., Walker R. (2002). Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. J. Neurol. Neurosurg. Psych. 72, 721–725. 10.1136/jnnp.72.6.721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuest S., Borghese N. A., Pirovano M., Mainetti R., Van De Langenberg R., De Bruin E. D. (2014). Usability and effects of an exergame-based balance training program. Games Health J. 3, 106–114. 10.1089/g4h.2013.0093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen C. Y., Lin K. H., Hu M. H., Wu R. M., Lu T. W., Lin C. H. (2011). Effects of virtual reality-augmented balance training on sensory organization and attentional demand for postural control in people with Parkinson disease: a randomized controlled trial. Phys. Ther. 91, 862–874. 10.2522/ptj.20100050 [DOI] [PubMed] [Google Scholar]
- Zettergren K., Franca J., Antunes M., Lavallee C. (2011). The effects of Nintendo Wii Fit training on gait speed, balance, functional mobility and depression in one person with Parkinson’s disease. Med. Health Sci. J. 9, 18–24. 10.15208/mhsj.2011.174 [DOI] [Google Scholar]