Abstract
While early detection through screenings for breast, cervical, and colorectal cancer is essential in improving cancer survival, it is not evenly utilized across class, race, ethnicity, or nativity. Given that utilization of early detection through screenings is not evenly distributed, immigrants who have much lower rates of health insurance coverage are at a disadvantage. We use National Health Interview Survey data linked with the Medical Expenditures Panel Survey to examine the trend in screening rates for breast, cervical, and colorectal cancer from 2000 to 2010, comparing U.S.-born natives, foreign-born citizens, and foreign-born non-citizens. We find that citizenship is clearly advantageous for the foreign-born, and that screening rates are higher among citizens compared to non-citizens overall, but uninsured non-citizens sometimes have higher screening rates that uninsured natives. Health insurance is pivotal for higher screening rates with clear differences among the insured and uninsured. Policies aimed at reducing disparities in cancer screening need to take into account nativity, citizenship, and access to health insurance.
Keywords: Cancer screening, Immigrants, Health insurance, Health policy
Introduction
The foreign born made up 13 % of the United States population in 2010, but they are often marginalized in the health care system due to lack of access. Cancer prevalence is high for certain foreign-born groups compared to U.S.-born natives, which may only increase as the foreign born population is aging. For instance, cancer was the second leading cause of death for all foreign-born residents in the U.S. in 2000 [1], and became the leading cause of death for Latinos, the largest minority group in the U.S. in 2012 [2]. While breast, cervical, and colorectal cancer screening rates have increased overall for the U.S. population [2], the uninsured and the foreign-born are still disadvantaged.
Though early detection through regular screenings has led to a reduction in mortality from breast cancer [3], its utilization is not evenly distributed across class, race, ethnicity, or nativity. Disparities in cancer prevention through screenings previously thought to be race-based are partially attributable to nativity differences, though some are also explained by access to care, including health insurance coverage, number of doctor visits, and usual source of care [4]. Evidence shows that the foreign born are less likely to have received a mammogram in the past 2 years than U.S.-born natives, with mixed findings that nativity differences persist even after controlling for socio-demographics [5]. Although fewer studies look at clinical breast exams, a similar disadvantage for the foreign born has been found, with health insurance as the strongest predictor of who gets screened [6].
A simple dichotomy of foreign-born/native comparison overlooks the role of citizenship, especially in terms of eligibility for federally funded programs. A majority of the foreign born are non-citizens, and they have lower rates of health insurance, a major predictor in preventive screenings, than both native and naturalized citizens [5, 7–9]. Length of residence for foreign-born in the U.S. has mixed support and duration in the U.S. may be more important for some foreign-born groups more than others [10–13]. The ability and preference of speaking English is also associated with higher rates of cancer screening among the foreign born [11, 12, 14]. Although some may examine these language issues as a proxy for acculturation, the possibility that these measures may be capturing a separate mechanism, such as access, deserves further consideration [15]. Cultural factors, such as mistrust in the medical system, poor doctor-patient communication, health literacy are also important when considering differences between foreign-born and native-born individuals [16].
Citizenship also enables different levels of health insurance access for the foreign born: Lawfully present immigrants are eligible for state insurance exchanges and tax credits with the introduction of the Patient Protection and Affordable Care Act (PPACA); legal permanent residents are still not eligible for federally provided Medicaid their first 5 years in the U.S.; and undocumented foreign-born residents will continue to not be eligible. Therefore many foreign-born may still not have health insurance coverage. It is estimated that after all mandates are implemented, about a quarter of the uninsured population will be undocumented foreign-born residents which make up nearly half of the noncitizen foreign-born population [17, 18]. The foreign born that are diagnosed with cancer are often diagnosed at later stages which puts a greater financial burden on the health care system and reduces life expectancy [19, 20].
Healthy People 2010 cancer prevention goals, the benchmark 10-year health objectives set by the U.S. Department of Health and Human Services during collection of the majority of these data, are used as a reference point for this study [21]. Among the cancers most effectively prevented through early detection [22], we examine how foreign-born citizens and foreign-born non-citizens compare to the U.S.-born natives in accessing screening utilization services. Our study will provide a comprehensive overview of screening rates among the foreign born compared to U.S.-born natives from 2000 to 2010 using nationally representative data to examine the trend in screening rates for breast, cervical, and colorectal cancer for different citizenship groups stratified by insurance status. We then evaluate if trends in the utilization of cancer screenings have changed significantly overtime and if the gaps between citizenship groups are narrowing.
Methods
Data
This study used the linked Medical Expenditure Panel Survey (MEPS)–National Health Interview Survey (NHIS) survey datasets for the years 2000–2010. MEPS collects nationally representative estimates of health care use for the U.S. civilian non-institutionalized population, and is described in detail elsewhere [23]. The NHIS provides information on health behaviors, demographics, and other health information. NHIS also provides the sampling frame for MEPS. Merging the two datasets allowed unique items from both surveys to be analyzed for the subset of NHIS respondents that were interviewed in MEPS. To increase the sample size and allow the study of time trends, we created a stacked dataset pooling 11 years of MEPS data (2000–2010). Analytic sample sizes ranged from 73,475 to 91,711 based on age and gender requirements as well as those who have complete information for the screening and citizenship. Missing data on individual items ranged from 2.5 to 5.5 % of the MEPS sample within each age range.
Measures
We examined four dependent variables, each representing a different screening for three types of cancer according to the recommendation of the United States Preventative Services Task Force (USPSTF). For each type of cancer, we used the screening recommendation that was used for the majority of the 11 year observation period. For breast cancer screening, we analyzed breast cancer screenings among women over the age 40 in accordance with the USPSTF guidelines up to 2009 [24]. Those who had a mammogram in the past 2 years were compliant, and those who had never had a screening or it had been more than 2 years were coded as not meeting screening guidelines. We also analyzed clinical breast exams among women 40 and older. Those that had a clinical breast exam within the past 2 years were categorized as meeting recommendations, although clinical breast exams are no longer included in USPSTF recommendations. For cervical cancer screening, we analyzed papanicolaou tests among women age 21–65 that had not had a hysterectomy in accordance with the current USPSTF screening recommendations as of 2003 [25]. Those who had a screening in the past 3 years were compliant and otherwise coded as 0. For colon cancer, we analyzed both fecal occult blood test (FOBT) and sigmoidoscopy and colonoscopy rates among adults age 50 and over in line with the 2002 USPSTF guidelines, which were in use for a majority of the years, until changes in 2008 that called for screenings to stop at age 75 [26]. Those that had an endoscopy in the past 5 years or FOBT in the last year are categorized as compliant with the guidelines. Health insurance was a dichotomous measure of having any health insurance at some point during the year. A combined measure of foreign-born and citizenship was used to classify citizenship into three categories: natives, born in the U.S. and automatically citizens; foreign-born citizens, individuals that have migrated to the U.S. and gained citizenship through naturalization; and non-citizens, individuals that have migrated to the U.S. and have not naturalized—these individuals may have migrated to the U.S. legally or illegally. Education was measured as the highest education level attained with four categories, less than high school, high school, some college, and bachelors or higher. Income was calculated as family income adjusted for household size, grouped into quintiles.
Analysis
Descriptive statistics averaged across all time points for each sub-sample of those recommended to get each screening are provided. Screening rates for mammograms, clinical breast exams, papanicolaou tests, and combined endoscopy and FOBT were calculated by nativity and citizenship status and stratified by insurance and plotted over time. Absolute differences by nativity and citizenship noted in the figures were calculated using logistic regression controlling for year, age, education, and income. Screening rates at the beginning of the time period and end, as well as trend differences were calculated. Significant differences among initial screening rates were noted in the first column. Differences in trends between 2000 and 2010 for each citizenship group were calculated as well, indicating the yearly trend in screening rates controlling for age, education, and income. Trend differences compared to natives for foreign-born citizens and non-citizens using logistic regression are calculated, indicating if the gap was narrowed a significant amount [27]. For each screening type, citizenship group screening rates in 2010 are compared to the Health People 2010 goals. All analyses were conducted using the survey weights provided by MEPS to make the results nationally representative for each year, and adjustments for the complex survey design of MEPS were also taken into account using the survey procedures in Stata 12.
Results
Sample descriptive statistics are presented in Table 1. Older individuals are more likely to have health insurance and among the foreign-born more likely to be citizens. Across all three groups recommended to get screened, noncitizens have the lowest rate of health insurance coverage by as much as 25 % lower coverage rates compared to foreign-born citizens. The gap between natives and foreign-born citizens is smaller with natives generally having about 5–6 % higher health insurance rates. Screening rates among those recommended to get each screening are highest for papanicolaou tests, and then clinical breast exams, followed by mammograms, and are the lowest for colorectal cancer screenings.
Table 1.
Descriptive statistics by Recommended Cancer Screening Groups, 2000–2010
| Women aged 40 +
|
Women aged 21–65
|
Men and women aged 50–80
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| %/Mean | Median | SD | %/Mean | Median | SD | %/Mean | Median | SD | |
| Age | 58.06 | 55 | 12.8 | 41.87 | 41 | 11.9 | 61.76 | 60 | 8.6 |
| Female | 53 % | ||||||||
| Native | 87 % | 84 % | 88 % | ||||||
| Foreign-born citizen | 8 % | 7 % | 8 % | ||||||
| Non-Citizen | 5 % | 8 % | 4 % | ||||||
| Health insurance | 91 % | 86 % | 92 % | ||||||
| Native | 91 % | 86 % | 92 % | ||||||
| Foreign-born citizen | 86 % | 80 % | 87 % | ||||||
| Non-citizen | 62 % | 55 % | 68 % | ||||||
| Mammogram | 74 % | ||||||||
| Clinical breast exam | 80 % | ||||||||
| Papanicolaou tests | 87 % | ||||||||
| CRC screening | 48 % | ||||||||
| N | 73,475 | 91,711 | 80,811 | ||||||
Source: MEPS–NHIS 2000–2010
Mammogram Screenings
For mammography there is little overall change in adherence rates, but a clear stratification between those with health insurance and those without health insurance is evident (Fig. 1). Among only those with health insurance, non-citizens have the lowest rate of mammograms by a significant margin. In 2000, the U.S.-born natives have the highest rate of mammograms; however, in 2006, insured foreign-born citizens start having screening rates higher than U.S.-born natives. The trends among the uninsured are less clear, in general, both foreign-born groups appear to get screened at similar or higher rates than uninsured U.S.-born natives.
Fig. 1.
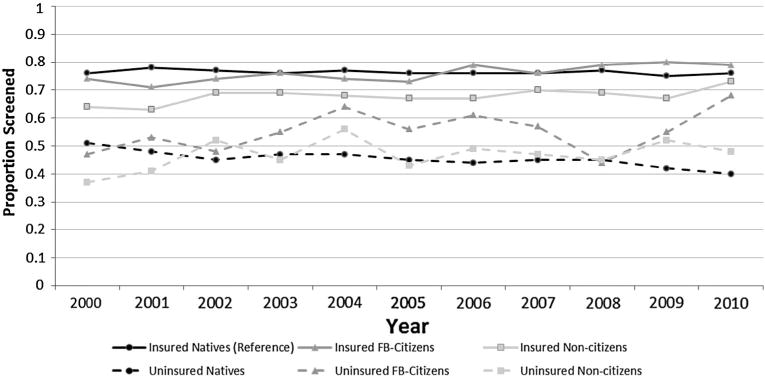
Mammogram trends by citizenship and health insurance from 2000 to 2010
Table 2 shows the change in screening rates by citizenship, indicating that while overall there was almost no change, both foreign-born citizens and non-citizens significantly increased their screening rates. The odds of getting a mammogram increased by 3.9 % each year for foreign-born citizens and by 1.5 % for foreign-born non-citizens. Natives on the other hand significantly decreased their rate of screening adherence overtime. This increase for the foreign-born and decrease for natives significantly narrows the gap. Despite narrowing the gap, rates for non-citizens in 2010 still fail to meet the HP2010 goal of 70 %.
Table 2.
Screening rates trend analysis from 2000 to 2010
| 2000a (%) | 2010 (%) | Trendb | Trend differencec | Met HP2010 goal | |
|---|---|---|---|---|---|
| Mammogram | |||||
| Natives | 74 | 73 | −.015** | (Ref) | Yes |
| Foreign-born citizen | 71*** | 78 | .039*** | Converge | Yes |
| Non-Citizens | 57*** | 64 | .0145*** | Converge | No |
| Total | 73 | 73 | −.009* | Yes | |
| Clinical breast exam | |||||
| Natives | 82 | 79 | −.030*** | (Ref) | – |
| Foreign-born citizen | 81* | 81 | .007** | Converge | – |
| Non-citizens | 68*** | 72 | .004** | Converge | – |
| Total | 82 | 78 | −.025*** | – | |
| Papanicolaou tests | |||||
| Natives | 89 | 86 | −.0417*** | (Ref) | No |
| Foreign-born citizen | 92 | 84 | −.025*** | Coincident | No |
| Non-Citizens | 82*** | 85 | .006*** | Converge | No |
| Total | 89 | 85 | −.035*** | No | |
| CRC screening | |||||
| Natives | 39 | 56 | .111*** | (Ref) | Yes |
| Foreign-born citizen | 41*** | 52 | .160*** | Converge | Yes |
| Non-citizens | 20*** | 34 | .190*** | Converge | No |
| Total | 39 | 55 | .116*** | Yes |
Source: MEPS–NHIS 2000–2010
p<.05
p<.01
p<.001
Indicate initial differences in screening rate
The yearly trend in screening rate from 2000 to 2010
This indicates if the gap in trends between groups is closing at a significant level overtime, foreign-born citizens and noncitizens referencing natives calculated from logistic regression models
Clinical Breast Exam
Clinical breast exam rates decline slightly from 2000 to 2010, with the odds of having a clinical breast exam declining by 2.5 % every year (Table 2). The patterns are very similar to those for mammography in that it is stratified by health insurance (Fig. 2). Among the insured, noncitizens have the lowest rate of clinical breast exams. In 2006, insured foreign-born citizens overtake insured U.S.-born natives and have a higher rate of clinical breast exams. Foreign-born citizens have the highest overall rate of mammography among the uninsured. The uninsured natives and uninsured non-citizens have similarly low rates of clinical breast exams. Non-citizens are the only group that increases in the rate of coverage over time. Trend differences by citizenship show initial differences are evident and converge overtime at a significant rate (Table 2).
Fig. 2.
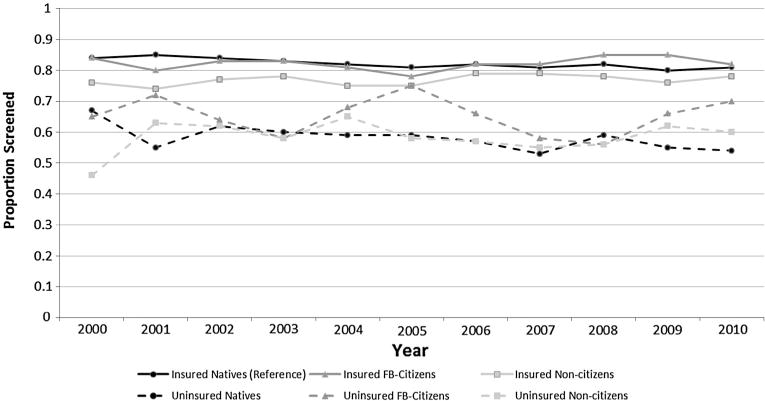
Clinical breast exam trends by citizenship and health insurance from 2000 to 2010
Cervical Cancer Screening
The rates of papanicolaou tests decrease from 2000 to 2010. The differences in the rate of papanicolaou tests between the insured and uninsured are much smaller than other screenings, only 15–20 % lower for uninsured compared to the 40 % differences found for mammograms; however, the uninsured still have noticeably lower rates overall than the insured (Fig. 3). From 2000 to 2006 U.S.-born natives have the highest rate, followed by the insured foreign-born citizens, and lastly the insured non-citizens. From 2007 to 2009 foreign-born citizens have the highest rate of screenings. However, in 2010, the pattern changes again such that insured non-citizens have the highest rate followed closely by insured natives, and then insured foreign-born citizens. Among the uninsured the non-citizens generally have the highest rate of screenings. Uninsured natives have the lowest and the greatest decline in papanicolaou tests. Between 2000 and 2010 the odds of a foreign-born citizen getting a papanicolaou test declines by 2.5 %, natives’ odds declines by 4.2 % each year, and non-citizens actually increase slightly. Natives and foreign-born citizens have similar rates across the entire time period. Non-citizens however significantly narrow the gap with natives’ overtime. All citizenship groups fail to meet the HP2010 goal of 90 % screening rate.
Fig. 3.
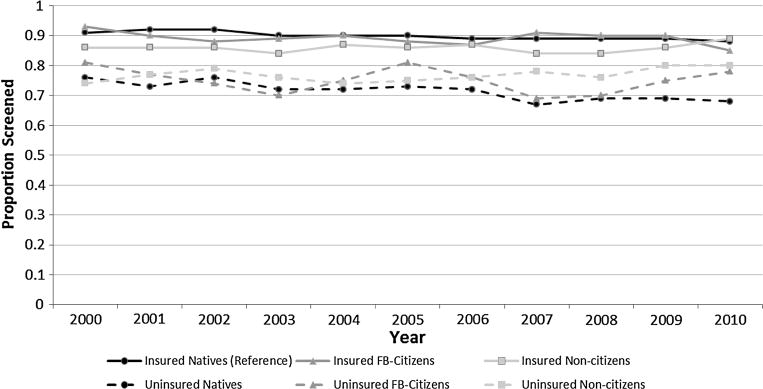
Papanicolaou test trends by citizenship and health insurance from 2000 to 2010
Colorectal Cancer Screening
The rate of colorectal cancer screenings increases for all groups from 2000 to 2010 (Fig. 4). Insured foreign-born citizens are slightly lower than insured natives with a similar increase over time. From 2000 to about 2006 insured non-citizens appear to have colorectal screening rates similar to the uninsured, but from 2007 to 2010 the health insurance stratification is visible for all groups. Uninsured U.S.-born natives have the highest rate of colorectal screenings among the uninsured, followed closely by uninsured foreign-born citizens. Uninsured non-citizens have the lowest rate by far with the rate dipping below 5 % in some years. Overall the odds of colorectal screening increases by 11.6 % each year from 2000 to 2010, with most of this coming from increases among the U.S.-born natives. Both foreign-born groups have significantly lower starting rates of colorectal cancer screening than natives, but significantly narrow the gap by 2010. Both U.S.-born natives and foreign-born citizens meet the HP2010 goal of 50 % screening rate; however, non-citizens are still far below this goal with a screening rate of 34 % in 2010.
Fig. 4.
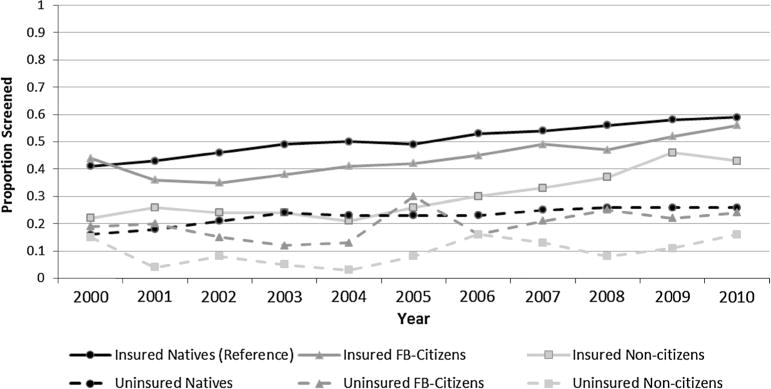
Colorectal screening trends by citizenship and health insurance from 2000 to 2010
Discussion
Individuals without health insurance are at a clear disadvantage in obtaining recommended screenings, and noncitizens are more likely to be uninsured than both citizen groups. While most of the HP2010 goals were met, noncitizens do not make any of the HP2010 goals. Citizenship offers clear benefits to the foreign born in terms of their cancer screening rates: foreign-born citizens have higher or similar rates of screenings as U.S.-born natives. While differences by citizenship still exist, looking at the trend from 2000 to 2010 is hopeful in many ways. The gaps in coverage differences have narrowed for all cancer screenings. Non-citizens had large initial differences to overcome, if this pattern continues differences in screenings could become insignificant overtime. Additionally, much of the screening differences for non-citizens are related to lower rates of health insurance coverage for non-citizens. For all screenings except colorectal cancer screenings, foreign-born groups were able to narrow the gap because natives had a decreasing rate. While much ground has been made in encouraging cancer screenings, it is important to maintain the high rates of compliance. Some of the reasons for a decrease among natives may be related to the economic crisis from 2008 to 2009, which significantly increased unemployment rates. From the start of the recession in 2008 the proportion of uninsured individuals in the U.S. increased and remained high well past 2010 [28]. Given the stratification of screening rates by insurance, it is possible this decrease is a result of the recession given health insurance and employment status are highly correlated.
Overall, a clear pattern based on the ease of the screening exists. That is, the highest rates of screening are found for papanicolaou tests and then for clinical breast exams, which are both less burdensome, lower-cost, in-office procedures. Mammograms have the next highest rate, which are not as easily conducted because mammograms are usually conducted on a second visit that includes a radiologist. Either endoscopy or FOBT has the lowest rates, and as the most difficult to administer, endoscopy requires not only a separate appointment but extensive patient preparation before the procedure. FOBT may be easier but still requires more of the patient than other screenings. Not only are overall screening rates higher for screenings with lower patient burden, but the disparity by health insurance and between citizenship groups decreases with the ease of the procedure. In 2010, the greatest inequalities in screening rates were for colorectal cancer screening and then mammograms. Making all screenings easier and more accessible, such as performing mammograms without requiring a second visit when feasible, will help substantially increase screening rates. These differences may also be related to variation in costs of these screenings, which may make obtaining services without health insurance more difficult, for example a colonoscopy costs on averages over $1,000 [29]. Additionally, increasing health insurance coverage rates will also be vital in increasing screening rates.
It is important to consider the cancer screening rates of the foreign born because the proportion of foreign-born residents in the older age ranges is increasing, which are those who are recommended to be screened for breast and colorectal cancer. In 2007, the mean age of the foreign-born population was 40—driven largely by younger Latino populations, and just barely reaching the age cut-off for breast cancer screenings [30]. Given that large numbers of immigrants will soon reach the age for screening recommendation, it is essential to understand the behavior of these groups. This study helps to pinpoint the demographic differences in screening rates over time. As the number of foreign born recommended to get screened increases, it is clear that targeted intervention to increase the screening rates of non-citizens is needed.
Screening rates for colorectal cancer are improving for all groups; however, gaps by citizenship still exist, which is similar to previous research. Variations in provider recommendations for mammography and endoscopies may be related to some of the citizenship disparities. A study of safety-net clinics in high immigrant areas found low rates of physician recommendations for colorectal screenings [31]. The first step to improving the screening rates, especially among vulnerable populations such as the foreign born, is to make sure providers are recommending guideline concordant screenings to all patients. Computerized medical records have been shown to be effective at increasing screening rates through the use of physician and patient reminders [32], and will play an increasingly important role in explicitly decreasing health disparities in these vulnerable populations.
Congruent with previous research, mammography rates are relatively steady, with non-citizens lagging behind. Clinical breast exam and papanicolaou tests rates have declined from 2000 to 2010; some of the decline may be a result of revised guidelines. Physicians may want to continue providing clinical breast exams for these vulnerable groups, perhaps with increased frequency for high-risk women if rates of mammograms among the foreign-born non-citizens remains low and rates of premenopausal breast cancer rise [33]. Additionally, the comparatively high rates of papanicolaou tests, clinical breast exams, and mammograms points to the preventive mindset of gynecologists, and their gatekeeper role as promoters of women’s health.
While smaller studies have found heterogeneity among foreign-born groups by country of origin, using this nationally representative data we are unable to analyze the foreign born by country of origin [34–36]. Another limitation of this study is that we are unable to identify undocumented immigrants, which may have screening rates much lower than legal permanent residents. Future studies should continue to examine the foreign born by citizenship status and health insurance status, but may also want to stratify by type of health insurance, public or private.
Despite the above mentioned caveats, this study makes a significant contribution by looking at screening trends by citizenship type, which has relevant and timely implications for eligibility for health insurance. With the passage of the PPACA, many of the stratifications by health insurance will be reduced; however, many non-citizen immigrants will remain uninsured even after the full implementation of the PPACA. This is especially true for the undocumented non-citizens; however, if legislation passes that facilitates a pathway to becoming a legal permanent resident with access to healthcare, disparities could decrease. Not being a citizen is a barrier to cancer screening, and without major policy changes, citizenship will continue to add to the existing disparity affecting the uninsured.
Acknowledgments
This material is based upon work supported by the National Science Foundation under Grant No. DGE1255832 and an infrastructure grant to the Population Research Institute at Pennsylvania State University by the National Institutes of Health (2R24HD041025-11). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation. The authors would also like to acknowledge funding from Penn State Hershey Cancer Institute, Social Science Research Institute, and Clinical and Translational Science Institute.
Footnotes
Conflict of interest None.
Contributor Information
Adriana M Reyes, Email: amr5763@psu.edu, Department of Sociology, The Pennsylvania State University, 211 Oswald Tower, University Park, PA 16802, USA.
Patricia Y Miranda, Email: pym1@psu.edu, Department of Health Policy and Administration, The Pennsylvania State University, 604 Ford Building, University Park 16802, PA, USA.
References
- 1.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91(3):392–9. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin. 2012;62(5) doi: 10.3322/caac.21153. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Cancer Screening—United States. 2010;2012 [Google Scholar]
- 4.Goel MS, Wee CC, McCarthy EP, Davis RB, Ngo-Metzger Q, Phillips RS. Racial and ethnic disparities in cancer screening—the importance of foreign birth as a barrier to care. J Gen Intern Med. 2003;18(12):1028–35. doi: 10.1111/j.1525-1497.2003.20807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Billmeier TM, Dallo FJ. Nativity status and mammography use: results from the 2005 National Health Interview Survey. J Immigr Minor Health. 2011;13(5):883–90. doi: 10.1007/s10903-010-9334-8. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez MA, Ward LM, Perez-Stable EJ. Breast and cervical cancer screening: impact of health insurance status, ethnicity and nativity of Latinas. Ann Fam Med. 2005;3(3):235–41. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Alba I, Hubbell FA, McMullin JM, Sweningson JM, Saitz R. Impact of US citizenship status on cancer screening among immigrant women. J Gen Intern Med. 2005;20(3):290–6. doi: 10.1111/j.1525-1497.2005.40158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Echeverria SE, Carrasquillo O. The roles of citizenship status, acculturation, and health insurance in breast and cervical cancer screening among immigrant women. Med Care. 2006;44(8):788–92. doi: 10.1097/01.mlr.0000215863.24214.41. [DOI] [PubMed] [Google Scholar]
- 9.Shih YCT, Elting LS, Levin B. Disparities in colorectal screening between US-born and foreign-born populations: evidence from the 2000 National Health Interview Survey. J Cancer Educ. 2008;23(1):18–25. doi: 10.1080/08858190701634623. [DOI] [PubMed] [Google Scholar]
- 10.Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000;18(1):62–8. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- 11.Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites - Cultural influences or access to care? Cancer. 2006;107(1):184–92. doi: 10.1002/cncr.21968. [DOI] [PubMed] [Google Scholar]
- 12.Maxwell AE, Danao LL, Crespi CM, Antonio C, Garcia GM, Bastani R. Disparities in the receipt of fecal occult blood test versus endoscopy among Filipino American immigrants. Cancer Epidemiol Biomark Prev. 2008;17(8):1963–7. doi: 10.1158/1055-9965.EPI-07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and non-Latino whites. Cancer. 2005;104(12):2940–7. doi: 10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jandorf L, Ellison J, Villagra C, et al. Understanding the barriers and facilitators of colorectal cancer screening among low income immigrant Hispanics. J Immigr Minor Health. 2010;12(4):462–9. doi: 10.1007/s10903-009-9274-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099–106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 16.Franzini L, Fernandez-Esquer ME. Socioeconomic, cultural, and personal influences on health outcomes in low income Mexican-origin individuals in Texas. Soc Sci Med. 2004;59(8):1629–45. doi: 10.1016/j.socscimed.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Passel J, Cohn DV. Unauthorized immigrant population: national and state trends, 2010. Washington, DC: Pew Research Center; 2011. [Google Scholar]
- 18.Buettgens M, Hall MA. Who Will Be Uninsured After Health Insurance Reform? Urban Institue. 2011 [Google Scholar]
- 19.Hedeen AN, White E. Breast cancer size and stage in Hispanic American women, by birthplace: 1992–1995. Am J Public Health. 2001;91(1):122–5. doi: 10.2105/ajph.91.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hedeen AN, White E, Taylor V. Ethnicity and birthplace in relation to tumor size and stage in Asian American women with breast cancer. Am J Public Health. 1999;89(8):1248–52. doi: 10.2105/ajph.89.8.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Services USDoHaH Healthy people 2010: understanding and improving health. 2nd. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 22.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 23.Ezzati-Rice TM, Rohde F, Greenblatt J. Sample design of the Medical Expenditure Panel Survey household component, 1998–2007. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 24.U.S. Preventive Services Task Force. U.S. Preventive Services Task Force: recommendations and rationale. Am Fam Physician. 2002;65(12) [Google Scholar]
- 25.U.S. Preventive Services Task Force. U.S. Prevetative Services Task Force: recommendations and rational: screening for cervical cancer. Am Fam Physician. 2003;67(8) [Google Scholar]
- 26.U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventative Services Task Force recommendation statement. Ann Intern Med. 2008;149 doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 27.Firebaugh G. Sage university paper series on quantitative applications in the social sciences. Thousand Oaks, CA: Sage; 1997. Analyzing repeated surveys; pp. 7–115. [Google Scholar]
- 28.Fronstin P. Tracking health insurance coverage by month: Trends in employment-based coverage among workers, and access to coverage among uninsured workers, 1995–2012. Employee Benefit Research Institute; 2013. [Google Scholar]
- 29.Healthcare Bluebook. 2014:2014. https://www.healthcarebluebook.com/page_Default.aspx.
- 30.Passel J, Cohn DV. A portrait of unauthorized immigrants in the United States. Washington, DC: Pew Research Center; 2009. [Google Scholar]
- 31.Lopez-Class M, Luta G, Noone A-M, et al. Patient and provider factors associated with colorectal cancer screening in safety net clinics serving low-income, urban immigrant Latinos. J Health Care Poor Underserved. 2012;23(3):1011. doi: 10.1353/hpu.2012.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmittdiel J, McMenamin SB, Halpin HA, et al. The use of patient and physician reminders for preventive services: results from a National Study of Physician Organizations. Prev Med. 2004;39(5):1000–6. doi: 10.1016/j.ypmed.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 33.Johnson Rh, CFLBA INcidence of breast cancer with distant involvement among women in the united states, 1976 to 2009. JAMA. 2013;309(8):800–5. doi: 10.1001/jama.2013.776. [DOI] [PubMed] [Google Scholar]
- 34.Lee HY, Ju E, Vang PD, Lundquist M. Breast and cervical cancer screening among Asian American women and Latinas: does race/ethnicity matter? J Womens Health. 2010;19(10):1877–84. doi: 10.1089/jwh.2009.1783. [DOI] [PubMed] [Google Scholar]
- 35.Samuel PS, Pringle JP, James NW, Fielding SJ, Fairfield KM. Breast, cervical, and colorectal cancer screening rates amongst female Cambodian, Somali, and Vietnamese immigrants in the USA. Int J Equity Health. 009:8. doi: 10.1186/1475-9276-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu TY, West B, Chen YW, Hergert C. Health beliefs and practices related to breast cancer screening in Filipino, Chinese and Asian-Indian women. Cancer Detect Prev. 2006;30(1):58–66. doi: 10.1016/j.cdp.2005.06.013. [DOI] [PubMed] [Google Scholar]


