Summary
Previous reviews of childhood obesity prevention have focused largely on schools and findings have been inconsistent. Funded by the US Agency for Healthcare Research and Quality (AHRQ) and the National Institutes of Health, we systematically evaluated the effectiveness of childhood obesity prevention programmes conducted in high-income countries and implemented in various settings. We searched MEDLINE®, Embase, PsycINFO, CINAHL®, ClinicalTrials.gov and the Cochrane Library from inception through 22 April 2013 for relevant studies, including randomized controlled trials, quasi-experimental studies and natural experiments, targeting diet, physical activity or both, and conducted in children aged 2–18 in high-income countries. Two reviewers independently abstracted the data. The strength of evidence (SOE) supporting interventions was graded for each study setting (e.g. home, school). Meta-analyses were performed on studies judged sufficiently similar and appropriate to pool using random effect models. This paper reported our findings on various adiposity-related outcomes. We identified 147 articles (139 intervention studies) of which 115 studies were primarily school based, although other settings could have been involved. Most were conducted in the United States and within the past decade. SOE was high for physical activity-only interventions delivered in schools with home involvement or combined diet–physical activity interventions delivered in schools with both home and community components. SOE was moderate for school-based interventions targeting either diet or physical activity, combined interventions delivered in schools with home or community components or combined interventions delivered in the community with a school component. SOE was low for combined interventions in childcare or home settings. Evidence was insufficient for other interventions. In conclusion, at least moderately strong evidence supports the effectiveness of school-based interventions for preventing childhood obesity. More research is needed to evaluate programmes in other settings or of other design types, especially environmental, policy and consumer health informatics-oriented interventions.
Keywords: Childhood, obesity, prevention, systematic review
Introduction
Childhood obesity persists as a serious threat to public health worldwide (1–5). In the United States, over two-thirds of adults and one-third of children are overweight or obese. Childhood obesity has many health consequences (6,7). Obesity is the result of biological, behavioural, social, environmental and economic factors and the complex interactions between them, which can produce a positive energy balance (8,9). Several leading health organizations and expert panels, including the World Health Organization (10) and Institute of Medicine (IOM), have recommended comprehensive interventions to combat childhood obesity (11,12).
Some prior systematic reviews have summarized findings of childhood obesity prevention studies (13–16); however, findings have been mixed and often limited either by the length of follow-up, exclusively focusing on a specific intervention setting (e.g. school) or certain outcomes (e.g. body mass index [BMI]), or by including only a small number of studies.
The present study aimed to systematically evaluate the effectiveness of all childhood obesity prevention programmes implemented in various settings or designs (e.g. school, home, primary care, childcare, community, consumer health informatics [CHI]) conducted in high-income countries. Our original systematic review that served as the basis for the present study was funded by the Agency for Healthcare Research and Quality (AHRQ) of the US Department of Health and Human Services. Our full 835-page research report for AHRQ includes a literature review for six intervention settings and designs and was published in June 2013 (17). (For the present study, we conducted a new literature search for studies published after the completion of our AHRQ report and included them in analyses.) We reviewed studies implemented in any setting (or design) that tested obesity prevention interventions targeting diet, physical activity (PA) or a combination of both behaviours.
In our original AHRQ-funded study, we assessed various key outcomes including certain adiposity-related measures, behaviours such as dietary consumption, PA and sedentary behaviours, and some other health markers such as blood lipid levels and blood pressure. The present study focuses on the effects of the interventions on adiposity outcomes and aims to provide the variety of readers (e.g. researchers, health professionals and policy makers) a refined, comprehensive review of findings to help guide future interventions and research, particularly in children of high-income countries.
The present study provides new knowledge and possesses additional features and strengths compared with previous reviews on childhood obesity prevention including our full AHRQ report published in June 2013. This study is more encompassing as it included studies set in various settings, it assessed a wide variety of outcome measures and it followed a rigorous protocol – that required of AHRQ-funded comparative effectiveness reviews. More details on our research methods and findings can be found in our full AHRQ report (17).
Methods
Our large research team consisted of epidemiologists, clinicians, nutritionists, biostatisticians and health policy researchers from multiple institutions. We followed standardized procedures developed by the AHRQ Effective Healthcare Program and benefited from the input of experts in the field, with the AHRQ and other stakeholders, throughout the project’s stages. For example, we developed our key questions (KQs) with the input of a key informant panel that included experts in childhood nutrition policy, academic clinicians treating obese children, representatives from public school systems, parents of obese children, representatives from professional societies focusing on nutrition and obesity, and AHRQ staff. In addition, we also formed a technical expert panel of leading experts and other stakeholders in the field, which provided input on the development of our study protocol. Our full report was reviewed by both experts and the public and improvements were made based on their feedback. Additional details are provided in the full AHRQ manuscript (17).
Search strategy and selection criteria
We searched MEDLINE®, EMBASE®, PsycINFO, CINAHL® and the Cochrane Library from inception through 22 April 2013. We developed a search strategy based on medical subject heading (MeSH®) terms and the text of key articles we had identified a priori. We reviewed the reference lists of all included articles and all pertinent review articles to identify articles the database searches may have missed. We uploaded all articles into DistillerSR (Evidence Partners, Ottawa, Ontario, Canada), a web-based software application developed for systematic review and data management. We also conducted a grey literature search in ClinicalTrials.gov to identify relevant unpublished research through 23 July 2012.
We identified studies conducted in high-income countries, defined as those with a very high human development index (18), that evaluated interventions to prevent obesity (or ‘excessive weight gain’) in children aged 2–18 years. We only included randomized controlled trials (RCTs), quasi-experimental studies and natural experiments that reported intervention effects on adiposity-related outcomes. The studies also needed to follow participants for at least 1 year from baseline measures, or for six or more months in school-based interventions (considering the length of the school year). Studies targeting only overweight or obese children or children with medical conditions (e.g. diabetes) were excluded.
Data extraction
Two independent reviewers conducted title, abstract and full article reviews to assess inclusion eligibility. Standardized forms were used for data abstraction. Each article was double reviewed during this phase: the second reviewer confirmed or corrected the first reviewer’s data abstractions for completeness and accuracy. Information on the study characteristics, subjects, eligibility criteria, intervention components, outcome measures and method of ascertainment regarding body weight status were abstracted.
Primary adiposity-related outcomes of interest were BMI, BMI z-score, BMI percentile, waist circumference (WC), percent body fat (%BF), skin-fold thickness and prevalence of overweight or obesity. Secondary outcomes (not reported on in this paper) were intermediate behavioural outcomes (i.e. dietary intakes, PA and sedentary behaviours) and obesity-related clinical outcomes (e.g. blood pressure and blood lipid levels).
Quality (risk of bias) assessment of individual studies
Two independent reviewers used the Downs and Black Checklist for Measuring Quality, summarized here, to assess risk of study bias (ROB) for each included study (19): (i) low ROB: when a study fulfilled all of the following: clearly stated the objective, described the main outcomes, described the characteristics of the enrolled subjects, clearly described the interventions, described the main findings, randomized the subjects to the intervention group, concealed the intervention assignment until recruitment was complete and had at least partially described the distributions of (potential) confounders in each treatment group; (ii) moderate ROB: if a study did not fulfil one of the aforementioned items, or if such could not be verified and (iii) high ROB: if a study did not fulfil more than one of the aforementioned items.
Data synthesis
For each intervention setting, we created a set of detailed evidence tables containing the information extracted from all eligible studies fitting that setting (or design). We aggregated the studies by the primary setting where the interventions took place. Within each setting, we grouped the interventions into three groups by strategy: (i) ‘diet-only interventions’, those who aimed to alter dietary intake only; (ii) ‘PA-only interventions’, those who aimed to increase PA and/or reduce sedentary activity only and (iii) ‘diet–PA combined interventions’, those who targeted both diet and PA for change.
When more than three comparable studies were available for a given intervention strategy and setting(s), we conducted meta-analyses using STATA (version 11.0; Stata Corp., College Station, TX, USA). We used random-effect models applying the DerSimonian and Laird approach due to the heterogeneity present among studies (20). A study was not included in the meta-analysis if it (i) was not an RCT; (ii) induced substantial heterogeneity when included in the analysis (i.e. I2 >50% or P-value <0.1 from chi-square tests assessing the heterogeneity of effect sizes across interventions) or (iii) did not report sufficient data.
Strength of the body of evidence
We graded the quantity, quality and consistency of the best available evidence of interventions for each setting by adapting an evidence-grading scheme recommended in the Methods Guide for Conducting Comparative Effectiveness Reviews (21). We assigned grades for all adiposity-related outcomes by first constructing a hierarchy of outcomes. Using the hierarchy, each study contributed only one (the highest ranked) adiposity-related measure for grading. We considered four domains in our evaluation of strength of evidence (SOE): ROB, direction of the body of evidence, consistency of outcomes across studies and precision of the pooled estimate or individual study estimates.
We determined an overall ROB for each setting and intervention target (i.e. diet, PA or both) combination based on where most studies in their respective groupings fell. We decided that all of the included studies provided evidence of a direct effect. We considered the body of studies to be consistent in direction if more than 70% of the studies in a grouping had an effect in the same direction. We considered an individual study to be precise if the results for the given outcome were significant (P < 0.05) or if estimates had narrow confidence intervals (CI) that excluded the null. If more than 70% of the individual studies were precise, we considered the body of evidence to be precise.
SOE was classified into four categories: (i) ‘high’, indicating high confidence that the evidence reflects the true effect and further research is very unlikely to change our confidence in the estimate of the effect; (ii) ‘moderate’, indicating moderate confidence and further research may change our confidence and the estimate; (iii) ‘low’, meaning low confidence and further research is likely to change our confidence and the estimate and (iv) ‘insufficient’, reflecting that either a body of evidence is unavailable or there was only one study for this setting and it had moderate or high ROB.
Results
Results of the literature search and intervention studies
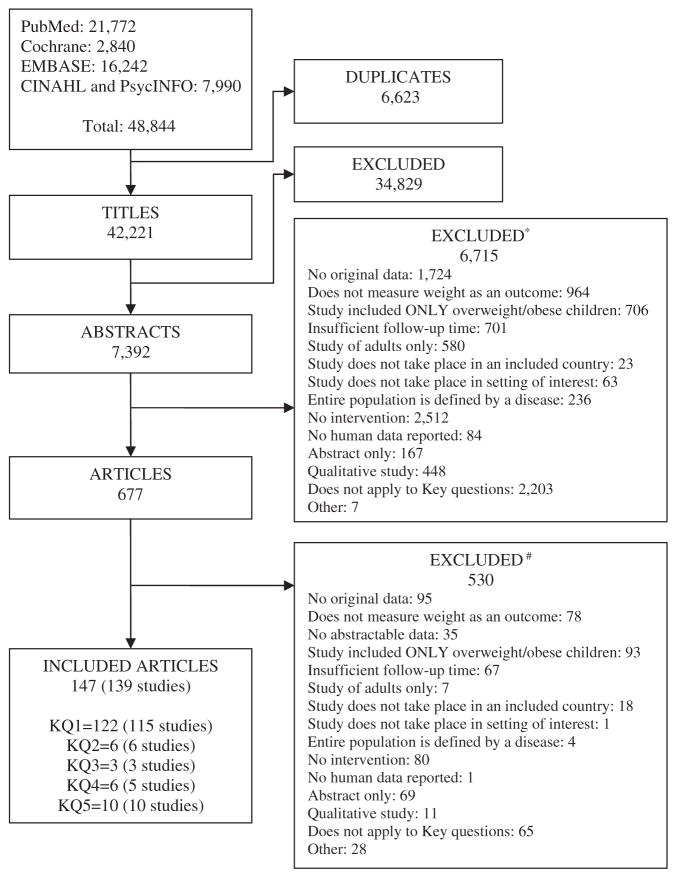
We identified 42,221 unique citations, which resulted in 7,392 abstracts and, later, 677 articles after screening. A final 139 intervention studies described in 147 articles (21.7%) met our inclusion criteria (Fig. 1). This included 115 studies that assessed school-based interventions, six home-based interventions, three primary care-based interventions, five child care-based interventions and 10 community-based interventions. Seven studies were interventions using CHI, which we combined and described under other intervention settings (see Fig. 1, Appendix A, Table 1). None of the unpublished studies met our selection criteria.
Figure 1.
Results of the literature search on childhood obesity prevention studies/interventions in high-income countries. *Sum of excluded abstracts exceeds 6,175 because reviewers were not required to agree on reasons for exclusion. #Sum of excluded abstracts exceeds 530 because reviewers were not required to agree on reasons for exclusion. The key questions (KQs) of this review were organized by study setting/design as follows: What is the comparative effectiveness of school-based interventions (KQ1), home-based interventions (KQ2), primary care-based interventions (KQ3), childcare setting-based interventions (KQ4) and community-based interventions (KQ5) for the prevention of obesity or overweight in children? Note that our original Agency for Healthcare Research and Quality study also included KQ6 ‘What is the comparative effectiveness of consumer health informatics applications for the prevention of obesity or overweight in children?’ and KQ7 ‘What is the comparative effectiveness of multi-setting interventions for the prevention of obesity or overweight in children?’, but, in the present study, the interventions previously classified under these headings were grouped into KQ1 or KQ2 based on if the intervention was primarily school or home based, or another KQ based on the key intervention setting. We merged KQ6 and KQ7 with the other KQ groups to help simplify the presentation of information and because of the relatively small number of studies originally grouped into KQ6 and KQ7.
Table 1.
Summary of the results of the 139 childhood obesity prevention studies on adiposity-related outcomes*†
| Setting | Type of intervention, number of studies |
Years of publication |
Enrolled participants | Studies with low/moderate/high risk of bias (n) |
% with favourable outcome (P < 0.05) |
% with favourable outcome (P < 0.05 not necessary) |
Risk of bias |
Consistency | Precision | Strength of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| School based | ||||||||||
| School only | D, 3 | 1995–2012 | 2,423 | 1/2/0 | 67 | 100 | Moderate | Consistent | Imprecise | Moderate |
| PA, 18 | 1993–2013 | 10,488 | 0/14/4 | 22 | 72 | Moderate | Consistent | Imprecise | Moderate | |
| C, 40 | 1985–2013 | 47,665 | 2/29/9 | 44 | 53 | Moderate | Inconsistent | Imprecise | Insufficient | |
| School and home | D, 1 | 1986 | 1,321 | 0/1/0 | 100 | 100 | Moderate | NA | Precise | Insufficient |
| PA, 3 | 1999–2010 | 1,654 | 1/2/0 | 100 | 100 | Moderate | Consistent | Precise | High | |
| C, 28 | 1991–2013 | 33,297 | 2/20/6 | 36 | 79 | Moderate | Consistent | Imprecise | Moderate | |
| School, home and community | PA, 1 | 2010 | 2,829 | 0/1/0 | 0 | 0 | Moderate | NA | Imprecise | Insufficient |
| C, 9 | 2008–2013 | 11,776 | 1/5/3 | 11 | 83 | Moderate | Consistent | Imprecise | High | |
| School and community | D, 1 | 2009 | 2,950 | 0/1/0 | 100 | 100 | Moderate | NA | Precise | Insufficient |
| PA, 1 | 2008 | 1,721 | 0/0/1 | 0 | 0 | High | NA | Imprecise | Insufficient | |
| C, 4 | 1997–2012 | 5,416 | 0/2/2 | 25 | 75 | High | Consistent | Imprecise | Moderate | |
| School and consumer health informatics (CHI) | PA, 2 | 2007–2012 | 1,335 | 0/2/0 | 0 | 0 | Moderate | Inconsistent | Imprecise | Insufficient |
| C, 3 | 2006–2013 | 2,280 | 0/3/0 | 33 | 33 | Moderate | Inconsistent | Imprecise | Insufficient | |
| School, home and CHI | C, 1 | 2011 | 589 | 0/0/1 | 0 | 0 | High | NA | Imprecise | Insufficient |
| Home based | ||||||||||
| Home only | D, 1 | 2004 | 59 | 0/1/0 | 0 | 0 | Moderate | NA | Imprecise | Insufficient |
| C, 3 | 2001–2012 | 262 | 0/2/1 | 0 | 33 | Moderate | Inconsistent | Imprecise | Low | |
| Home, school and community | C, 1 | 2009 | 1,323 | 0/0/1 | 0 | 0 | High | NA | Imprecise | Insufficient |
| Home, primary care and CHI | C, 1 | 2006 | 878 | 1/0/0 | 0 | Unable to determine | Low | NA | Imprecise | Insufficient |
| Primary care setting | ||||||||||
| Primary care | C, 1 | 2009 | 600 | 0/1/0 | 0 | 0 | Moderate | NA | Imprecise | Insufficient |
| Primary care and home | C, 2 | 2012 | 253 | 1/1/0 | 50 | 50 | Moderate | Inconsistent | Imprecise | Insufficient |
| Child care setting | ||||||||||
| Child care | P, 2 | 2007–2012 | 827 | 0/0/2 | 50 | 50 | High | Inconsistent | Imprecise | Insufficient |
| C, 3 | 2009–2012 | 2,393 | 1/2/0 | 33 | 33 | Moderate | Inconsistent | Imprecise | Low | |
| Community based | ||||||||||
| Community only | PA, 1 | 2010 | 46 | 0/1/0 | 0 | 0 | Moderate | NA | Imprecise | Insufficient |
| Community and school | C, 3 | 1997–2010 | 2,966 plus 24 schools (mean enrolment 1109) | 0/3/0 | 66 | 66 | Moderate | Inconsistent | Imprecise | Moderate |
| Community, school and home | C, 1 | 2007–2008 | 1,326 | 0/1/0 | 100 | 100 | Moderate | NA | Precise | Insufficient |
| Community and home | C, 2 | 2010 | 564 | 0/1/1 | 0 | 0 | High | Consistent | Imprecise | Insufficient |
| Community, home, primary care and child care | C, 1 | 2010 | 43,811 | 0/1/0 | 100 | 100 | Moderate | NA | Precise | Insufficient |
| Community, school, primary care and child care | D, 1 | 2010 | NR | 0/0/1 | 100 | 100 | High | NA | Precise | Insufficient |
| Community, home, school and child care | C, 1 | 2013 | 2,631 | 0/0/1 | 0 | 50 | High | NA | Imprecise | Insufficient |
Risk of bias: The Downs and Black Checklist for Measuring Quality was used to assess the risk of bias in the included studies.
Consistency: The body of evidence was considered to be consistent in direction if ≥70% of the studies had an effect in the same direction.
Precision: We considered the body of evidence precise if ≥70% of the studies reported statistically significant results (P < 0.05) or had narrow confidence intervals that excluded the null.
Strength of the evidence: We considered the four recommended domains: (i) risk of bias in the included studies; (ii) direction of the evidence; (iii) consistency across studies and (iv) precision of the pooled estimate or the individual study estimates. We identified all studies as providing direct evidence since all of the studied interventions directly affected one of the study’s primary outcomes of interest.
Adiposity-related outcomes: for example, body mass index (BMI), BMI z-score, waist circumference and skin-fold thickness.
Our original KQ6 focused on consumer health informatics-based interventions. These results are reported here under other KQs based on primary setting.
C, diet–PA combined interventions; D, diet-only intervention; NA, not applicable; NR, not reported; PA, PA-only intervention.
The majority of the 139 studies (104 or 75%) evaluated diet–PA combined interventions, 28 evaluated PA-only interventions and seven evaluated diet-only interventions (Table 2). As described in detail below, 76 of the 115 studies (66%) evaluating school-based interventions showed favourable intervention effects on adiposity-related outcomes, but only 42 of them (36%) were statistically significant. None of the home-based studies reported statistically significant favourable results. One out of three (33%) primary care-based studies, two out of five (40%) child care-based studies and five out of 10 (50%) community-based studies reported significant and favourable effects on adiposity-related outcomes (Table 2). Multi-setting studies had statistically significant favourable results more often than single-setting studies (44 vs. 35%) (Table 3).
Table 2.
Percentage (%) of childhood obesity prevention studies showing favourable adiposity-related outcomes by primary intervention setting and type of intervention*
| Setting | Type of intervention, number of studies |
% with statistically significant and favourable results (P < 0.05)
|
% with favourable results (P < 0.05 not necessary)
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Diet-only interventions |
PA-only interventions |
Combined diet–PA interventions |
Total | Diet-only interventions |
PA-only interventions |
Combined diet–PA interventions |
Total | ||
| School based | D, 5; PA, 25; C, 85; Total, 115 | 80 | 28 | 36 | 36 | 100 | 64 | 64 | 66 |
| Home based | D, 1; PA, 0; C, 5; Total, 6 | 0 | – | 0 | 0 | 0 | – | 20 | 17 |
| Primary care based | D, 0; PA, 0; C, 3; Total, 3 | – | – | 33 | 33 | – | – | 33 | 33 |
| Child care based | D, 0; PA, 2; C, 3; Total, 5 | – | 50 | 33 | 40 | – | 50 | 33 | 40 |
| Community based | D, 1; PA, 1; C, 8; Total, 10 | 100 | 0 | 50 | 50 | 100 | 0 | 63 | 60 |
| Total | D, 7; PA, 28; C, 104; Total, 139 | 71 | 29 | 35 | 36 | 86 | 61 | 60 | 62 |
Our original KQ6/setting focused on consumer health informatics-based interventions. These results are reported here under other KQs based on primary setting.
C, diet–PA combined interventions; D, diet-only intervention; PA, PA-only intervention.
Table 3.
Percentage (%) of childhood obesity prevention studies showing favourable adiposity-related outcomes by intervention setting(s) and type of intervention
| Setting(s) | Type of intervention, number of studies |
% with statistically significant and favourable results (P < 0.05)
|
% with favourable results (do not need to be P < 0.05)
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Diet-only interventions |
PA-only interventions |
Diet–PA combined interventions |
Total | Diet-only interventions |
PA-only interventions |
Diet–PA combined interventions |
Total | ||
| 1. Single setting interventions | |||||||||
| School only | D, 3; PA, 18; C, 40; Total, 61 | 67 | 22 | 44 | 39 | 100 | 72 | 53 | 61 |
| Home only | D, 1; PA, 0; C, 3; Total, 4 | 0 | – | 0 | 0 | 0 | – | 33 | 25 |
| Primary care only | D, 0; PA, 0; C, 1; Total, 1 | – | – | 0 | 0 | – | – | 0 | 0 |
| Child care only | D, 0; PA, 2; C, 3; Total, 5 | – | 50 | 33 | 40 | – | 50 | 33 | 40 |
| Community only | D, 0; PA, 1; C, 0; Total, 1 | – | 0 | – | 0 | – | 0 | – | 0 |
| All single setting interventions (overall) | D, 4; PA, 21; C, 47; Total, 72 | 50 | 24 | 39 | 35 | 75 | 67 | 49 | 56 |
| 2. Multiple setting interventions* | |||||||||
| School and home | D, 1; PA, 3; C, 28; Total, 32 | 100 | 100 | 36 | 44 | 100 | 100 | 79 | 81 |
| School and community | D, 1; PA, 1; C, 7; Total, 9 | 100 | 0 | 43 | 44 | 100 | 0 | 71 | 67 |
| Community and home | D, 0; PA, 0; C, 2; Total, 2 | – | 0 | – | 0 | – | 0 | – | 0 |
| School, home and community | D, 0; PA, 1; C, 11; Total, 12 | – | 0 | 18 | 17 | – | 0 | 77 | 71 |
| All multiple setting interventions (overall) | D, 2; PA, 5; C, 48; Total, 55 | 100 | 60 | 40 | 44 | 100 | 60 | 74 | 74 |
| Total | D, 6; PA, 26; C, 95; Total, 127 | 67 | 31 | 39 | 39 | 83 | 65 | 62 | 63 |
School and community, both ‘School and Community’ and ‘Community and School’ based interventions. School and home and community, ‘School, Home and Community’, ‘Home, School and Community’, and ‘Community, School and Home’ based interventions.
C, diet–PA combined interventions; D, diet-only intervention; PA, PA-only intervention.
Effectiveness of school-based interventions
School only-based interventions
Sixty-one studies (60,576 participants) took place in a school-only setting, including 40 RCTs and 21 non-RCTs. Most enrolled elementary or middle school-aged children. Three RCTs, described in four articles, evaluated diet-only interventions (22–25) and showed a decrease in BMIs or BMI z-scores. They were designed to prevent weight gain and focused on promoting a healthy diet and reducing the consumption of carbonated drinks.
Eighteen studies tested PA-only interventions (Appendix A1). PA-only interventions had an impact on BMI (26), WC in girls (27), skin-fold thickness (28) and %BF (29) in children. One study with a significant effect on %BF (29) enrolled pre-pubertal girls in daily physical education classes. Some of the PA interventions also affected clinical outcomes by lowering systolic blood pressure (30) or affected intermediate outcomes by increasing PA and reducing sedentary activities (31,32).
Forty studies assessed the effect of combined strategy interventions (Appendix A2). These included intensive classroom PA lessons led by trained teachers, moderate-to-vigorous PA sessions, distribution of nutritional education materials and provision of healthful foods. Children who participated in longer term intervention programmes generally showed significant improvements in physical performance (e.g. shuttle run minutes) (33–37), whereas shorter studies mostly had non-significant results.
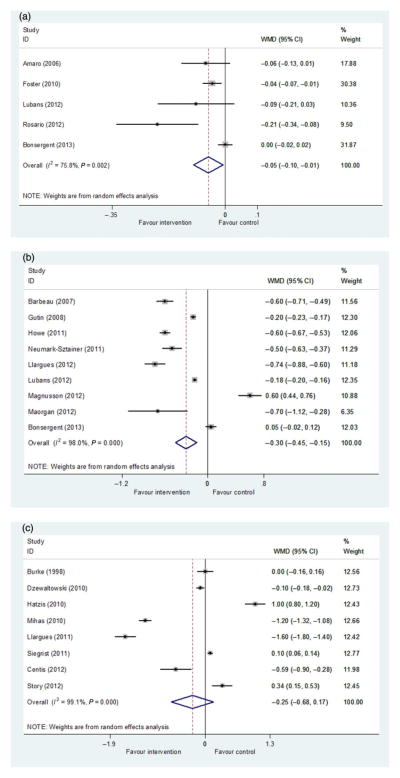
Five of the combined interventions were RCTs, reported BMI z-score as an outcome and had sufficient data for meta-analysis (38–42). Together, they showed an overall difference in BMI z-score of −0.05 (95% CI: −0.10, −0.01, P = 0.025) in favour of the intervention groups (Fig. 2a).
Figure 2.
Meta-analyses of changes in body mass index (BMI) and BMI z-score of school-based, diet–physical activity combined childhood obesity prevention studies. (a) Change in BMI z-score in studies taking place only in school. (b) Change in BMI in studies taking place only in school. (c) Change in BMI in studies taking place in school with a home-based intervention component.
WMD, weighted mean difference.
Nine of the combined interventions reported on BMI and were RCTs with sufficient data for meta-analysis (41–49). They showed an overall mean difference in BMI of −0.30 kg m−2 (95% CI: −0.45, −0.15, P < 0.001) in favour of the intervention (Fig. 2b).
Overall, SOE was moderate that interventions targeting diet or PA only in a school-only setting prevent obesity in children. SOE was presently insufficient that school only-based interventions using a combined strategy prevent obesity.
School-based interventions with a home component
Thirty-two studies (36,272 participants) implemented interventions in schools and included a home component, including 21 RCTs (Appendix A3). Only one study evaluated a diet-only intervention (50), where the most intensive of its two intervention arms showed a reduction in the prevalence of overweight and obesity. Three studies tested PA-only interventions (51–53). All four reported statistically significant beneficial effects of the intervention on adiposity-related outcomes.
Ten (36%) of the 28 studies that tested combined strategy interventions reported statistically significant beneficial effects (Table 1). Among the 18 studies that measured BMI change, 16 showed reduced BMI due to the intervention with differences ranging from −0.10 to −1.60 kg m−2. However, only in five studies were these changes statistically significant.
Only one of the 28 examined studies reported a significant, desirable intervention effect on the combined prevalence of overweight and obesity (adjusted odds ratio [OR] = 0.67; 95% CI: 0.47, 0.96, P < 0.03) (54). Another study found a statistically significant difference in the prevalence of both overweight (3.7%, P < 0.05) and obesity (2.3%, P < 0.05), again favouring the intervention (55).
Eight combined intervention studies reported sufficient data for meta-analysis of BMI (56–63). The weighted mean BMI difference was −0.25 kg m−2 (95% CI: −0.68, 0.17, P = 0.237) favouring the interventions (Fig. 2c).
SOE was insufficient that diet-only interventions prevent obesity when implemented in a school setting with a home component. SOE was high that PA-only interventions prevent obesity, but was moderate regarding diet–PA combined interventions.
School-based interventions with home and community components
We identified 10 studies (14,605 participants) that were school based and included both home and community components, including five RCTs (Appendix A4). Most of the combined interventions focused on providing education to improve diet and PA. SOE was insufficient that PA-only interventions prevent obesity as there was only one study found with a moderate ROB. SOE was high that combined interventions prevent obesity as the only study had a low ROB and the other studies, which mostly had moderate ROB, showed favourable intervention effects.
School-based interventions with a community component
Six studies (10,087 participants) were school-based with a community component, including three RCTs (Appendix A5). One RCT tested a diet-only intervention and showed significant improvements in BMI and obesity prevalence (64). Another RCT testing PA-only interventions found positive but insignificant improvements in triceps skin-fold thickness and body weight, but no improvements in BMI or %BF (65). Four studies evaluating combined interventions generally showed non-significant improvements in adiposity-related outcomes.
SOE was insufficient that diet- or PA-only interventions prevent obesity given only one study for each. SOE was moderate that combined interventions prevent obesity as two of the four studies with moderate ROB both showed favourable effects.
School-based interventions with a consumer health informatics component
We identified five studies (3,615 participants) that were school based with a CHI component (Appendix A6). One reported a significant difference in BMI between the intervention and control groups (66). SOE was insufficient regarding such interventions.
School-based interventions with home and consumer health informatics components
One non-RCT evaluated a combined intervention (589 participants) in a school setting with both home and CHI components, but detected no beneficial effects on adiposity-related outcomes (67). Hence, SOE was insufficient.
Key findings from non-school-based interventions
Home only-based interventions
We identified four home-based intervention studies (321 participants) and all were RCTs (Appendix A7). One examined a diet-only intervention and three tested combined interventions. None of the studies detected a statistically significant beneficial intervention effect on adiposity-related outcomes. SOE was insufficient for diet-only interventions. SOE was low that combined interventions at home to prevent obesity.
Home-based interventions with school and community components
We identified one RCT intervention study (1,323 participants), which was home based and included both school and community components. It reported no effect of a diet–PA combined intervention on BMI (68). SOE was insufficient that such interventions prevent obesity in these settings.
Home-based studies with primary care and consumer health informatics components
One RCT (878 participants) was home based with both primary care and CHI components. It reported no effect of a combined diet and PA intervention on BMI z-score (69). SOE was insufficient for this intervention strategy.
Primary care only-based interventions
We identified one quasi-experimental study (600 participants) that was only primary care based (70). It did not reduce obesity rates. Thus, SOE was insufficient regarding interventions in this setting.
Primary care-based interventions with a home component
Two RCTs (71,72) (253 participants) assessed the effect of combined interventions performed in a primary care setting with a home component. Only one found significant differences in BMI z-score in favour of the intervention group (72). Thus, SOE was insufficient for such interventions.
Child care centre only-based interventions
We identified five child care centre-based intervention studies (3,220 participants) (73–77), three of which were RCTs (73–75) and two non-RCTs. The two non-RCTs both assessed the effects of PA-only interventions. One of them found significant differences in BMI and %BF between the intervention and control groups (76). The other one found positive but insignificant differences in BMI between intervention and control (P = 0.09 for weight and intervention interaction). However, with only two studies, SOE was insufficient regarding the PA-only interventions.
The three RCT studies (73–75) all evaluated diet–PA combined interventions, but only one (75) showed significant beneficial effects on adiposity-related outcomes. SOE was low for combined interventions as these RCTs had moderate ROB and inconsistent results.
Community-based or environmental-level interventions
We identified 10 community-based or environmental-level intervention studies (Appendix A8). The strongest evidence came from three studies that took place in the community with school involvement (78–80). Two were RCTs with one conducted in the Netherlands (1,108 participants) (78) and the other in the United States (mean enrolment of 1,109 participants across 24 schools) (79). The third was a non-RCT in the United States (80). The US RCT (79) and the one non-RCT (80) detected statistically significant, beneficial intervention effects.
SOE was moderate that community-based, diet–PA combined interventions that include a school component prevent obesity. SOE was insufficient for interventions implemented in the community alone or with support from other settings.
Consumer health informatics interventions
Seven CHI studies were identified and they took place primarily in the school or home setting. Only one (66) school-based CHI study showed a significant reduction in BMI in the intervention group.
Discussion
To our knowledge, this is the most comprehensive study that has been performed to evaluate the success of various childhood obesity prevention programmes. We included 139 studies conducted in multiple settings in high-income countries over the past three decades, focusing on adiposity-related outcomes and SOE. The study followed the rigorous protocol required by the AHRQ for systematic reviews and provides important findings to help various stakeholders understand the effectiveness of obesity prevention programmes for children and to offer insights for future research and intervention development. This study has a number of principal strengths and makes some unique contributions to the field (see below). Our key findings include:
First, we find that a large number of childhood obesity prevention studies have been performed, but the majority are school based and conducted in the United States and within the most recent decade. In total, we identified 139 intervention studies, 115 (83%) of which were school based.
Second, we find at least moderate SOE to support the effectiveness of school-based interventions. About half of the studies reported statistically significant beneficial intervention effects for at least some of the adiposity-related measures. Interventions implemented in schools with home involvement had the highest proportion of studies with favourable results.
Third, overall, a greater proportion of multi-setting studies demonstrated significant and beneficial results compared with single-setting interventions. All settings combined, the highest proportion of significant and favourable impacts on adiposity-related outcomes was attributable to diet-only interventions while the lowest proportion of successes lies in PA-only interventions.
Fourth, the SOE varied by intervention strategy and setting. SOE for PA-only interventions delivered in schools with home involvement and diet–PA combined interventions delivered in schools with both home and community components to prevent obesity were high. SOE for school only-based interventions targeting either diet or PA, combined diet–PA school-based interventions with home or community components, and combined diet–PA community-based interventions with a school component to prevent obesity was moderate. SOE for combined interventions in a child care or home setting to prevent obesity was low. In general, some intervention groupings had low SOE due to the small number of relevant studies conducted of their type. The SOE for the effectiveness of interventions in other settings was insufficient due to the small number of published research found, the moderate or high ROB and conflicting results across studies.
In general, our main findings are consistent with previous systematic reviews that school-based interventions can help prevent obesity in children. This supports the IOM’s recommendations (12) that schools be the focal point for childhood obesity prevention. However, discrepancies between our findings and previous reviews exist, especially regarding the SOE and the magnitude of intervention effects. Although our study generally found an insufficient-to-moderate SOE supporting the intervention effects of school-based interventions (although there were a few exceptions of large intervention effects in some cases), the most recent Cochrane review found strong evidence to support the beneficial effects of school-based intervention programmes, particularly among children aged 6–12 (16). However, another systematic review of 18 controlled trials did not find any significant improvements in BMI with school-based PA interventions (81). The discrepancies may stem from differences in study selection criteria and, therefore, included studies, as well as from differences in the outcomes being examined.
Although some of the intervention studies we reviewed reported large effect sizes in changes in BMI and obesity/overweight prevalence, overall, our meta-analyses, which was based on all available studies meeting our inclusion criteria, suggest the effect size of these interventions to be small. For example, our findings presented in Fig. 2 imply improvements of about 0.05 z-score and 0.25 BMI. Especially compared with the increase in BMI and the rates of overweight and obesity over the last three decades in many countries, these intervention effects are slight. Thus, the effectiveness of interventions to reverse the tide of the epidemic is likely to be small as many large social and environmental changes are driving the trend towards increasing obesity. In general, our reported effect sizes were similar to those reported by other reviews of preventive interventions, although there are also reviews that did not find any significant improvements in BMI with school-based interventions (81).
Our findings have some important implications for clinical decision and policy making. This review can help clinical and public health practitioners, researchers and policy makers decide on appropriate intervention strategies with which to combat the prevailing obesity epidemic in developed countries. It may also help provide insights for future research. We need more research to test non-school-based interventions and those utilizing innovative designs and approaches. Strong, promising results suggest that school-based childhood obesity prevention programmes may fight the rise in childhood obesity. After careful review of the individual components of the successful studies, healthcare professionals may replicate the results in new settings, which could lead to broader implementation.
The cost-effectiveness of the interventions was infrequently studied. Only a few of our included studies mentioned such analyses and none of the studies we reviewed reported estimates of the resources used (costs) to achieve the observed effects. It is likely that few studies collected data on the costs associated with their interventions. Given the complexity of many programmes, it is understandably challenging to determine which costs should be accounted for (e.g. programme development, implementation, maintenance costs) and, subsequently, assessed and reported. Nevertheless, it would be important to know how stakeholders (e.g. parents, schools, public health professionals, government agencies) would calculate the real value of an intervention. It would also be important to figure out how researchers may help in such assessments. This is a critical gap in the current literature. In the future, we recommend researchers, journal editors and funding agencies to encourage the collection and reporting of data on the cost-effectiveness of interventions.
The sustainability of interventions and their beneficial effects are another important, albeit complex and controversial, issue that is less studied. Very few studies measured or showed that intervention effects were sustained beyond the active intervention period. More future research, including systematic reviews, is needed in this area.
Intervention programmes may also have potential harms, although few were reported. For example, programmes may unintentionally cause stigmas; most interventions achieved only small or no effects but weighed and measured many youth. Some of the youth may have anticipated improvement in their weight status, but could have experienced no significant improvements or benefits. Thus, it is foreseeable that some youth could feel a sense of failure with this or an associated loss in self-esteem. Although, we did not observe any reports of this in the literature. Nonetheless, future research into the potential harms of interventions would be useful.
In addition, it is possible that some intervention approaches may elicit the desire to respond favourably in some children, particularly those from families with higher educational attainment and/or greater financial resources. This may lead to disproportionate behavioural and weight improvements in these groups. Future research is needed to assess this possibility and better understand the issue to help enhance intervention effectiveness.
This study has several limitations. First, it was limited in scope by focusing only on studies from high-income countries. However, this restriction makes the findings all the more applicable to the examined population. Second, there was great heterogeneity in the included studies in terms of intervention setting, design, sample size and characteristics, intervention approach, primary measures used to assess intervention effects, length of follow-up, and statistical and analytical approaches taken. Such variability made it challenging for cross-comparisons. Third, given that we identified so few studies outside of the school setting, we were only able to conduct meta-analyses for KQ1 (school-based interventions) and only on a small number of studies at that.
Fourth, we stratified analyses first based on study setting and then by intervention strategy taken (diet, PA or both combined). However, due to limited sample sizes, we could not further stratify analyses – for example, to explore the comparative effectiveness of specific intervention approaches (e.g. educational interventions vs. environmental interventions) with pooled analyses or compare effects in specific intermediate outcomes (e.g. changes in fruit and vegetable intake vs. total energy intake).
Fifth, we used BMI and BMI-related measures, such as BMI z-score and BMI percentile, as well as the prevalence of overweight and obesity based on BMI cut-points, as the primary outcomes of interest. This was performed given its more common reporting across included studies. But, BMI has its limitations. It is an indirect measure of adiposity and not an ideal indicator for health risk. In addition, studies used different BMI cut-points to define overweight and obesity.
Sixth, related to study heterogeneity, another challenge was that studies assessed intervention effects in different ways. Some did so by comparing changes in the outcomes between the intervention and control groups while other studies compared between-group differences in weight outcomes only at follow-up. Still others reported on ORs of being overweight and/or obese and other studies did so on between-group difference in continuous outcome measures such as BMI. This again made comparing and pooling results challenging.
Seventh, we included some studies that did not state obesity prevention among their original intervention goals but rather stated they aimed to reduce cardiovascular risk. We kept these studies in the review because they also implemented diet and/or PA interventions and reported on body weight-related outcomes for their results. By employing similar strategies on similar outcomes, they could also shed some light on the potential effects of childhood obesity interventions. However, because of the differences in original study intents, these studies may differ slightly with those originally designed to primarily target childhood obesity.
Lastly, considering the comparability of studies conducted in different locales, we limited our review to only those studies conducted in high-income countries. Thus, our findings may not be generalizable to lower income countries. In addition, we decided to reduce the inclusion requirement for length of follow-up time to 6 months for school-based studies considering the usual length of school years. However, we recognize 6 months may be too short a time to observe intervention effects on weight-related outcomes.
Despite these many limitations, our study was systematic and rigorous. We followed standardized procedures from the AHRQ Effective Healthcare Program and utilized input from various experts and stakeholders in the field of childhood obesity prevention. Only experimental studies, quasi-experimental studies and natural experiments were included in our analyses to minimize confounding and maximize utilization of available evidence. Our study assessed the effects of the interventions on multiple adiposity-related outcomes while most other reviews have focused only on BMI or other select outcomes. We have also identified a number of future research priorities for the field (see Table 4 for our recommendations).
Table 4.
Recommendations for future research in childhood obesity prevention based on our systematic review
| Although we have found promising effects for school-based interventions for childhood obesity prevention, many questions still remain unanswered. We recommend additional research in the following areas: |
|---|
|
PA, physical activity.
In conclusion, a large number of childhood obesity intervention studies have been conducted in high-income countries, but they have been predominantly conducted in schools and in the United States. The following intervention points are supported by a body of evidence of at least a moderate level of strength to be effective for childhood obesity prevention: (i) schools are an important setting in which to implement effective intervention programmes and concomitant involvement of the home/family and community is desirable; (ii) improving access to PA facilities and healthful food choices such as fruits and vegetables both at school and home is effective and (iii) home or parental and family involvement is important. Overall, there is moderate-to-high SOE to support the idea that diet and/or PA interventions implemented in schools prevent obesity. However, the evidence on the effectiveness of interventions implemented in other settings is generally insufficient. Other analyses and findings from this systematic review on other outcomes such as on blood pressure and blood lipids can be found and were reported recently elsewhere (82,83).
Future research is needed to evaluate interventions conducted in settings other than in schools, especially those implementing wide-ranging changes through regional and national policy and environmental changes. Research into the delivery and effectiveness of innovative intervention strategies, such as those taking advantage of and applying new technologies and approaches (e.g. health communication and social marketing, urban planning), established behavioural theories and novel methodologies (e.g. systems science) is also of great importance.
Acknowledgments
This study was primarily funded under contract no. 290-2007-10061-I from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services. Youfa Wang, Yang Wu, LC and LJC’s efforts were also supported in part by research grants from the National Institute of Health (research grants 1R01HD064685-01A1 and U54HD070725 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development [NICHD]). The U54 project was co-funded by the NICHD and the Office of Behavioral and Social Sciences Research (OBSSR). LC also received support from the China Scholarship Council, Peking University and Johns Hopkins University for her research as a postdoctoral fellow working with Youfa Wang at Johns Hopkins University, who is the principal investigator of the project. The authors are fully responsible for the content of this report. Statements herein should not be construed as opinions of the funders. We thank Dr. Christine Chang from AHRQ for her steadfast support and assistance to the study. We also thank our technical experts and stakeholders for their contributions and feedback to our study through providing input on refining the key research questions, protocol and our full research report submitted to the AHRQ.
Appendix A References for studies cited in the Result section (A1–A8)
This systematic review included 147 articles, which described 139 intervention studies. Appendix A provided additional references that were not included in the paper due to the journal’s page limit.
Appendix A1 PA-only interventions implemented in a school only-based setting
- 1.Walther C, Gaede L, Adams V, et al. Effect of increased exercise in school children on physical fitness and endothelial progenitor cells: a prospective randomized trial. Circulation. 2009;120:2251–2259. doi: 10.1161/CIRCULATIONAHA.109.865808. [DOI] [PubMed] [Google Scholar]
- 2.Donnelly JE, Greene JL, Gibson CA, et al. Physical Activity Across the Curriculum (PAAC): a randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–341. doi: 10.1016/j.ypmed.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stenevi-Lundgren S, Daly RM, Linden C, Gardsell P, Karlsson MK. Effects of a daily school based physical activity intervention program on muscle development in prepubertal girls. Eur J Appl Physiol. 2009;105:533–541. doi: 10.1007/s00421-008-0932-2. [DOI] [PubMed] [Google Scholar]
- 4.Reed KE, Warburton DE, Macdonald HM, Naylor PJ, McKay HA. Action Schools! BC: a school-based physical activity intervention designed to decrease cardiovascular disease risk factors in children. Prev Med. 2008;46:525–531. doi: 10.1016/j.ypmed.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 5.Heelan KA, Abbey BM, Donnelly JE, Mayo MS, Welk GJ. Evaluation of a walking school bus for promoting physical activity in youth. J Phys Act Health. 2009;6:560–567. doi: 10.1123/jpah.6.5.560. [DOI] [PubMed] [Google Scholar]
- 6.Chiodera P, Volta E, Gobbi G, et al. Specifically designed physical exercise programs improve children’s motor abilities. Scand J Med Sci Sports. 2008;18:179–187. doi: 10.1111/j.1600-0838.2007.00682.x. [DOI] [PubMed] [Google Scholar]
- 7.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Hovell MF, Nader PR. Project SPARK. Effects of physical education on adiposity in children. Ann N Y Acad Sci. 1993;699:127–136. doi: 10.1111/j.1749-6632.1993.tb18844.x. [DOI] [PubMed] [Google Scholar]
- 8.Thivel D, Isacco L, Lazaar N, et al. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur J Pediatr. 2011;170:1435–1443. doi: 10.1007/s00431-011-1466-x. [DOI] [PubMed] [Google Scholar]
- 9.Lazaar N, Aucouturier J, Ratel S, Rance M, Meyer M, Duche P. Effect of physical activity intervention on body composition in young children: influence of body mass index status and gender. Acta Paediatr. 2007;96:1315–1320. doi: 10.1111/j.1651-2227.2007.00426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smolak L, Levine MP. A two-year follow-up of a primary prevention program for negative body image and unhealthy weight regulation. Eat Disord. 2001;9:313–325. doi: 10.1080/106402601753454886. [DOI] [PubMed] [Google Scholar]
- 11.Martinez Vizcaino V, Salcedo Aguilar F, Franquelo Gutierrez R, et al. Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children: a cluster randomized trial. Int J Obes (Lond) 2008;32:12–22. doi: 10.1038/sj.ijo.0803738. [DOI] [PubMed] [Google Scholar]
- 12.Resaland GK, Anderssen SA, Holme IM, Mamen A, Andersen LB. Effects of a 2-year school-based daily physical activity intervention on cardiovascular disease risk factors: the Sogndal school-intervention study. Scand J Med Sci Sports. 2011;21:e122–e131. doi: 10.1111/j.1600-0838.2010.01181.x. [DOI] [PubMed] [Google Scholar]
- 13.Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: switch-play. Int J Obes (Lond) 2008;32:601–612. doi: 10.1038/sj.ijo.0803805. [DOI] [PubMed] [Google Scholar]
- 14.Valdimarsson O, Linden C, Johnell O, Gardsell P, Karlsson MK. Daily physical education in the school curriculum in prepubertal girls during 1 year is followed by an increase in bone mineral accrual and bone width – data from the prospective controlled Malmo pediatric osteoporosis prevention study. Calcif Tissue Int. 2006;78:65–71. doi: 10.1007/s00223-005-0096-6. [DOI] [PubMed] [Google Scholar]
- 15.Bielec G, Peczak-Graczyk A, Waade B. Do swimming exercises induce anthropometric changes in adolescents? Issues Compr Pediatr Nurs. 2013;36:37–47. doi: 10.3109/01460862.2013.777818. [DOI] [PubMed] [Google Scholar]
- 16.Weeks BK, Beck BR. Twice-weekly, in-school jumping improves lean mass, particularly in adolescent boys. Pediatr Obes. 2012;7:196–204. doi: 10.1111/j.2047-6310.2011.00026.x. [DOI] [PubMed] [Google Scholar]
- 17.Robbins LB, Pfeiffer KA, Maier KS, Lo YJ, Wesolek Ladrig SM. Pilot intervention to increase physical activity among sedentary urban middle school girls: a two-group pretest-posttest quasi-experimental design. J Sch Nurs. 2012;28:302–315. doi: 10.1177/1059840512438777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandongen R, Jenner DA, Thompson C, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10- to 12-year-old children. Prev Med. 1995;24:9–22. doi: 10.1006/pmed.1995.1003. [DOI] [PubMed] [Google Scholar]
Appendix A2 Combined interventions implemented in a school only-based setting
- 18.Vandongen R, Jenner DA, Thompson C, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10- to 12-year-old children. Prev Med. 1995;24:9–22. doi: 10.1006/pmed.1995.1003. [DOI] [PubMed] [Google Scholar]
- 19.Bonsergent E, Agrinier N, Thilly N, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013;44:30–39. doi: 10.1016/j.amepre.2012.09.055. [DOI] [PubMed] [Google Scholar]
- 20.Foster GD, Linder B, Baranowski T, et al. A school-based intervention for diabetes risk reduction. N Engl J Med. 2010;363:443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosario R, Oliveira B, Araujo A, et al. The impact of an intervention taught by trained teachers on childhood overweight. Int J Environ Res Public Health. 2012;9:1355–1367. doi: 10.3390/ijerph9041355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amaro S, Viggiano A, Di Costanzo A, et al. Kaledo, a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: a pilot cluster randomized trial. Eur J Pediatr. 2006;165:630–635. doi: 10.1007/s00431-006-0153-9. [DOI] [PubMed] [Google Scholar]
- 23.Lubans DR, Morgan PJ, Okely AD, et al. Preventing obesity among adolescent girls: one-year outcomes of the Nutrition and Enjoyable Activity for Teen Girls (NEAT Girls) cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166:821–827. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 24.Gutin B, Yin Z, Johnson M, Barbeau P. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: the Medical College of Georgia Fitkid Project. Int J Pediatr Obes. 2008;3(Suppl 1):3–9. doi: 10.1080/17477160801896457. [DOI] [PubMed] [Google Scholar]
- 25.Barbeau P, Johnson MH, Howe CA, et al. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity (Silver Spring) 2007;15:2077–2085. doi: 10.1038/oby.2007.247. [DOI] [PubMed] [Google Scholar]
- 26.Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, Johannsson E, Sveinsson T. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ Res. 2012;27:484–494. doi: 10.1093/her/cys049. [DOI] [PubMed] [Google Scholar]
- 27.Morgan PJ, Saunders KL, Lubans DR. Improving physical self-perception in adolescent boys from disadvantaged schools: psychological outcomes from the Physical Activity Leaders randomized controlled trial. Pediatr Obes. 2012;7:e27–e32. doi: 10.1111/j.2047-6310.2012.00050.x. [DOI] [PubMed] [Google Scholar]
- 28.Busch V, De Leeuw RJ, Schrijvers AJ. Results of a multibehavioral health-promoting school pilot intervention in a Dutch secondary school. J Adolesc Health. 2013;52:400–406. doi: 10.1016/j.jadohealth.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 29.Neumark-Sztainer DR, Friend SE, Flattum CF, et al. New moves-preventing weight-related problems in adolescent girls a group-randomized study. Am J Prev Med. 2010;39:421–432. doi: 10.1016/j.amepre.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Llargues E, Recasens A, Franco R, et al. Medium-term evaluation of an educational intervention on dietary and physical exercise habits in schoolchildren: the Avall 2 study. Endocrinol Nutr. 2012;59:288–295. doi: 10.1016/j.endonu.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Howe CA, Harris RA, Gutin B. A 10-month physical activity intervention improves body composition in young black boys. J Obes. 2011;2011:358581. doi: 10.1155/2011/358581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manios Y, Kafatos A. Health and nutrition education in primary schools in Crete: 10 years follow-up of serum lipids, physical activity and macronutrient intake. Br J Nutr. 2006;95:568–575. doi: 10.1079/bjn20051666. [DOI] [PubMed] [Google Scholar]
- 33.Manios Y, Moschandreas J, Hatzis C, Kafatos A. Evaluation of a health and nutrition education program in primary school children of Crete over a three-year period. Prev Med. 1999;28:149–159. doi: 10.1006/pmed.1998.0388. [DOI] [PubMed] [Google Scholar]
- 34.Manios Y, Moschandreas J, Hatzis C, Kafatos A. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br J Nutr. 2002;88:315–324. doi: 10.1079/BJN2002672. [DOI] [PubMed] [Google Scholar]
- 35.Sollerhed AC, Ejlertsson G. Physical benefits of expanded physical education in primary school: findings from a 3-year intervention study in Sweden. Scand J Med Sci Sports. 2008;18:102–107. doi: 10.1111/j.1600-0838.2007.00636.x. [DOI] [PubMed] [Google Scholar]
- 36.Graf C, Koch B, Falkowski G, et al. School-based prevention: effects on obesity and physical performance after 4 years. J Sports Sci. 2008;26:987–994. doi: 10.1080/02640410801930176. [DOI] [PubMed] [Google Scholar]
- 37.Haerens L, Deforche B, Maes L, Stevens V, Cardon G, De Bourdeaudhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity (Silver Spring) 2006;14:847–854. doi: 10.1038/oby.2006.98. [DOI] [PubMed] [Google Scholar]
- 38.Kain J, Leyton B, Cerda R, Vio F, Uauy R. Two-year controlled effectiveness trial of a school-based intervention to prevent obesity in Chilean children. Public Health Nutr. 2009;12:1451–1461. doi: 10.1017/S136898000800428X. [DOI] [PubMed] [Google Scholar]
- 39.Trevino RP, Hernandez AE, Yin Z, Garcia OA, Hernandez I. Effect of the Bienestar Health Program on physical fitness in low-income Mexican American children. Hispanic J Behav Sci. 2005;27:120–132. [Google Scholar]
- 40.Kafatos A, Manios Y, Moschandreas J. Health and nutrition education in primary schools of Crete: follow-up changes in body mass index and overweight status. Eur J Clin Nutr. 2005;59:1090–1092. doi: 10.1038/sj.ejcn.1602216. [DOI] [PubMed] [Google Scholar]
- 41.Stock S, Miranda C, Evans S, et al. Healthy Buddies: a novel, peer-led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics. 2007;120:e1059–e1068. doi: 10.1542/peds.2006-3003. [DOI] [PubMed] [Google Scholar]
- 42.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123:e661–e667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 43.Newton RL, Jr, Han H, Anton SD, et al. An environmental intervention to prevent excess weight gain in African-American students: a pilot study. Am J Health Promot. 2010;24:340–343. doi: 10.4278/ajhp.08031224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Skybo TA, Ryan-Wenger N. A school-based intervention to teach third grade children about the prevention of heart disease. Pediatr Nurs. 2002;28:223–229. 235. [PubMed] [Google Scholar]
- 45.Walter HJ, Hofman A, Connelly PA, Barrett LT, Kost KL. Primary prevention of chronic disease in childhood: changes in risk factors after one year of intervention. Am J Epidemiol. 1985;122:772–781. doi: 10.1093/oxfordjournals.aje.a114160. [DOI] [PubMed] [Google Scholar]
- 46.Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323:1029–1032. doi: 10.1136/bmj.323.7320.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 48.Madsen J, Sallis JF, Rupp JW, et al. Relationship between self-monitoring of diet and exercise change and subsequent risk factor changes in children and adults. Patient Educ Couns. 1993;21:61–69. doi: 10.1016/0738-3991(93)90060-a. [DOI] [PubMed] [Google Scholar]
- 49.Bush PJ, Zuckerman AE, Theiss PK, et al. Cardiovascular risk factor prevention in black schoolchildren: two-year results of the ‘Know Your Body’ program. Am J Epidemiol. 1989;129:466–482. doi: 10.1093/oxfordjournals.aje.a115158. [DOI] [PubMed] [Google Scholar]
- 50.Bronikowski M, Bronikowska M. Will they stay fit and healthy? A three-year follow-up evaluation of a physical activity and health intervention in Polish youth. Scand J Public Health. 2011;39:704–713. doi: 10.1177/1403494811421059. [DOI] [PubMed] [Google Scholar]
- 51.Burguera B, Colom A, Pinero E, et al. ACTYBOSS: activity, behavioral therapy in young subjects – after-school intervention pilot project on obesity prevention. Obes Facts. 2011;4:400–406. doi: 10.1159/000333436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coleman KJ, Shordon M, Caparosa SL, Pomichowski ME, Dzewaltowski DA. The healthy options for nutrition environments in schools (Healthy ONES) group randomized trial: using implementation models to change nutrition policy and environments in low income schools. Int J Behav Nutr Phys Act. 2012;9:80. doi: 10.1186/1479-5868-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.DeBar LL, Schneider M, Drews KL, et al. Student public commitment in a school-based diabetes prevention project: impact on physical health and health behavior. BMC Public Health. 2011;11:711. doi: 10.1186/1471-2458-11-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fung C, Kuhle S, Lu C, et al. From ‘best practice’ to ‘next practice’: the effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. Int J Behav Nutr Phys Act. 2012;9:27. doi: 10.1186/1479-5868-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Klish WJ, Karavias KE, White KS, et al. Multicomponent school-initiated obesity intervention in a high-risk, Hispanic elementary school. J Pediatr Gastroenterol Nutr. 2012;54:113–116. doi: 10.1097/MPG.0b013e3182318b39. [DOI] [PubMed] [Google Scholar]
- 56.Lubans DR, Morgan PJ, Callister R. Potential moderators and mediators of intervention effects in an obesity prevention program for adolescent boys from disadvantaged schools. J Sci Med Sport. 2012;15:519–525. doi: 10.1016/j.jsams.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 57.Rush E, Reed P, McLennan S, Coppinger T, Simmons D, Graham D. A school-based obesity control programme: Project Energize. Two-year outcomes. Br J Nutr. 2012;107:581–587. doi: 10.1017/S0007114511003151. [DOI] [PubMed] [Google Scholar]
- 58.Tucker S, Lanningham-Foster L, Murphy J, et al. A school based community partnership for promoting healthy habits for life. J Community Health. 2011;36:414–422. doi: 10.1007/s10900-010-9323-9. [DOI] [PubMed] [Google Scholar]
- 59.Warren JM, Henry CJ, Lightowler HJ, Bradshaw SM, Perwaiz S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot Int. 2003;18:287–296. doi: 10.1093/heapro/dag402. [DOI] [PubMed] [Google Scholar]
- 60.Dämon S, Dietrich S, Widhalm K. PRESTO – Prevention Study of Obesity: a project to prevent obesity during childhood and adolescence. Acta Paediatr Suppl. 2005;94:47–48. doi: 10.1111/j.1651-2227.2005.tb02131.x. [DOI] [PubMed] [Google Scholar]
Appendix A3 Interventions implemented in schools and included a home component
- 61.Trevino RP, Yin Z, Hernandez A, Hale DE, Garcia OA, Mobley C. Impact of the Bienestar school-based diabetes mellitus prevention program on fasting capillary glucose levels: a randomized controlled trial. Arch Pediatr Adolesc Med. 2004;158:911–917. doi: 10.1001/archpedi.158.9.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–1038. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hendy HM, Williams KE, Camise TS. Kid’s Choice Program improves weight management behaviors and weight status in school children. Appetite. 2011;56:484–494. doi: 10.1016/j.appet.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 64.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 65.Manios Y, Kafatos A, Mamalakis G. The effects of a health education intervention initiated at first grade over a 3 year period: physical activity and fitness indices. Health Educ Res. 1998;13:593–606. doi: 10.1093/her/13.4.593. [DOI] [PubMed] [Google Scholar]
- 66.Burke V, Milligan RA, Thompson C, et al. A controlled trial of health promotion programs in 11-year-olds using physical activity ‘enrichment’ for higher risk children. J Pediatr. 1998;132:840–848. doi: 10.1016/s0022-3476(98)70315-4. [DOI] [PubMed] [Google Scholar]
- 67.Dzewaltowski DA, Rosenkranz RR, Geller KS, et al. HOP’N after-school project: an obesity prevention randomized controlled trial. Int J Behav Nutr Phys Act. 2010;7:90. doi: 10.1186/1479-5868-7-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Siegrist M, Lammel C, Haller B, Christle J, Halle M. Effects of a physical education program on physical activity, fitness, and health in children: the JuvenTUM project. Scand J Med Sci Sports. 2011;23:2241–2249. doi: 10.1111/j.1600-0838.2011.01387.x. [DOI] [PubMed] [Google Scholar]
- 69.Story M, Hannan PJ, Fulkerson JA, et al. Bright Start: description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity (Silver Spring) 2012;20:2241–2249. doi: 10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hatzis CM, Papandreou C, Kafatos AG. School health education programs in Crete: evaluation of behavioural and health indices a decade after initiation. Prev Med. 2010;51:262–267. doi: 10.1016/j.ypmed.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 71.Mihas C, Mariolis A, Manios Y, et al. Evaluation of a nutrition intervention in adolescents of an urban area in Greece: short- and long-term effects of the VYRONAS study. Public Health Nutr. 2010;13:712–719. doi: 10.1017/S1368980009991625. [DOI] [PubMed] [Google Scholar]
- 72.Llargues E, Franco R, Recasens A, et al. Assessment of a school-based intervention in eating habits and physical activity in school children: the AVall study. J Epidemiol Community Health. 2011;65:896–901. doi: 10.1136/jech.2009.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Centis E, Marzocchi R, Di Luzio R, et al. A controlled, class-based multicomponent intervention to promote healthy lifestyle and to reduce the burden of childhood obesity. Pediatr Obes. 2012;7:436–445. doi: 10.1111/j.2047-6310.2012.00079.x. [DOI] [PubMed] [Google Scholar]
- 74.Elinder LS, Heinemans N, Hagberg J, Quetel AK, Hagstromer M. A participatory and capacity-building approach to healthy eating and physical activity- SCIP-school: a 2-year controlled trial. Int J Behav Nutr Phys Act. 2012;9:145. doi: 10.1186/1479-5868-9-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rappaport EB, Daskalakis C, Sendecki JA. Using routinely collected growth data to assess a school-based obesity prevention strategy. Int J Obes (Lond) 2013;37:79–85. doi: 10.1038/ijo.2012.126. [DOI] [PubMed] [Google Scholar]
- 76.Shofan Y, Kedar O, Branski D, Berry E, Wilschanski M. A school-based program of physical activity may prevent obesity. Eur J Clin Nutr. 2011;65:768–770. doi: 10.1038/ejcn.2011.25. [DOI] [PubMed] [Google Scholar]
- 77.Danielzik S, Pust S, Muller MJ. School-based interventions to prevent overweight and obesity in prepubertal children: process and 4-years outcome evaluation of the Kiel Obesity Prevention Study (KOPS) Acta Paediatr Suppl. 2007;96:19–25. doi: 10.1111/j.1651-2227.2007.00165.x. [DOI] [PubMed] [Google Scholar]
- 78.Simonetti D’Arca A, Tarsitani G, Cairella M, et al. Prevention of obesity in elementary and nursery school children. Public Health. 1986;100:166–173. doi: 10.1016/s0033-3506(86)80030-0. [DOI] [PubMed] [Google Scholar]
- 79.Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Effect of a two-year obesity prevention intervention on percentile changes in body mass index and academic performance in low-income elementary school children. Am J Public Health. 2010;100:646–653. doi: 10.2105/AJPH.2009.165746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hoelscher DM, Springer AE, Ranjit N, et al. Reductions in child obesity among disadvantaged school children with community involvement: the Travis County CATCH Trial. Obesity (Silver Spring) 2010;18(Suppl 1):S36–S44. doi: 10.1038/oby.2009.430. [DOI] [PubMed] [Google Scholar]
- 82.Nader PR, Stone EJ, Lytle LA, et al. Three-year maintenance of improved diet and physical activity: the CATCH cohort. Child and Adolescent Trial for Cardiovascular Health. Arch Pediatr Adolesc Med. 1999;153:695–704. doi: 10.1001/archpedi.153.7.695. [DOI] [PubMed] [Google Scholar]
- 83.Lionis C, Kafatos A, Vlachonikolis J, Vakaki M, Tzortzi M, Petraki A. The effects of a health education intervention program among Cretan adolescents. Prev Med. 1991;20:685–699. doi: 10.1016/0091-7435(91)90064-b. [DOI] [PubMed] [Google Scholar]
- 84.Schetzina KE, Dalton WT, 3rd, Lowe EF, et al. A coordinated school health approach to obesity prevention among Appalachian youth: the Winning with Wellness Pilot Project. Fam Community Health. 2009;32:271–285. doi: 10.1097/FCH.0b013e3181ab3c57. [DOI] [PubMed] [Google Scholar]
- 85.Marcus C, Nyberg G, Nordenfelt A, Karpmyr M, Kowalski J, Ekelund U. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int J Obes (Lond) 2009;33:408–417. doi: 10.1038/ijo.2009.38. [DOI] [PubMed] [Google Scholar]
- 86.Brandstetter S, Klenk J, Berg S, et al. Overweight prevention implemented by primary school teachers: a randomised controlled trial. Obes Facts. 2012;5:1–11. doi: 10.1159/000336255. [DOI] [PubMed] [Google Scholar]
- 87.Lloyd JJ, Wyatt KM, Creanor S. Behavioural and weight status outcomes from an exploratory trial of the Healthy Lifestyles Programme (HeLP): a novel school-based obesity prevention programme. BMJ Open. 2012:2. doi: 10.1136/bmjopen-2011-000390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Williamson DA, Champagne CM, Harsha DW, et al. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity (Silver Spring) 2012;20:1653–1661. doi: 10.1038/oby.2012.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes (Lond) 2008;32:1489–1498. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 90.Foster GD, Sherman S, Borradaile KE, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794–e802. doi: 10.1542/peds.2007-1365. [DOI] [PubMed] [Google Scholar]
- 91.Speroni KG, Earley C, Atherton M. Evaluating the effectiveness of the Kids Living Fit program: a comparative study. J Sch Nurs. 2007;23:329–336. doi: 10.1177/10598405070230060501. [DOI] [PubMed] [Google Scholar]
- 92.Hopper CA, Munoz KD, Gruber MB, Nguyen KP. The effects of a family fitness program on the physical activity and nutrition behaviors of third-grade children. Res Q Exerc Sport. 2005;76:130–139. doi: 10.1080/02701367.2005.10599275. [DOI] [PubMed] [Google Scholar]
- 93.Coleman KJ, Tiller CL, Sanchez J, et al. Prevention of the epidemic increase in child risk of overweight in low-income schools: the El Paso coordinated approach to child health. Arch Pediatr Adolesc Med. 2005;159:217–224. doi: 10.1001/archpedi.159.3.217. [DOI] [PubMed] [Google Scholar]
Appendix A4 School-based interventions with home and community components
- 94.Angelopoulos PD, Milionis HJ, Grammatikaki E, Moschonis G, Manios Y. Changes in BMI and blood pressure after a school based intervention: the CHILDREN study. Eur J Public Health. 2009;19:319–325. doi: 10.1093/eurpub/ckp004. [DOI] [PubMed] [Google Scholar]
- 95.Greening L, Harrell KT, Low AK, Fielder CE. Efficacy of a school-based childhood obesity intervention program in a rural southern community: TEAM Mississippi Project. Obesity (Silver Spring) 2011;19:1213–1219. doi: 10.1038/oby.2010.329. [DOI] [PubMed] [Google Scholar]
- 96.Jansen W, Borsboom G, Meima A, et al. Effectiveness of a primary school-based intervention to reduce overweight. Int J Pediatr Obes. 2011;6:e70–e77. doi: 10.3109/17477166.2011.575151. [DOI] [PubMed] [Google Scholar]
- 97.De Coen V, De Bourdeaudhuij I, Vereecken C, et al. Effects of a 2-year healthy eating and physical activity intervention for 3–6-year-olds in communities of high and low socio-economic status: the POP (Prevention of Overweight among Pre-school and school children) project. Public Health Nutr. 2012;15:1737–1745. doi: 10.1017/S1368980012000687. [DOI] [PubMed] [Google Scholar]
- 98.Wright K, Giger JN, Norris K, Suro Z. Impact of a nurse-directed, coordinated school health program to enhance physical activity behaviors and reduce body mass index among minority children: a parallel-group, randomized control trial. Int J Nurs Stud. 2013;50:727–737. doi: 10.1016/j.ijnurstu.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.de Meij JS, Chinapaw MJ, van Stralen MM, van der Wal MF, van Dieren L, van Mechelen W. Effectiveness of JUMP-in, a Dutch primary school-based community intervention aimed at the promotion of physical activity. Br J Sports Med. 2010;45:1052–1057. doi: 10.1136/bjsm.2010.075531. [DOI] [PubMed] [Google Scholar]
- 100.Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes (Lond) 2008;32:1060–1067. doi: 10.1038/ijo.2008.79. [DOI] [PubMed] [Google Scholar]
- 101.Millar L, Kremer P, de Silva-Sanigorski A, et al. Reduction in overweight and obesity from a 3-year community-based intervention in Australia: the ‘It’s Your Move!’ project. Obes Rev. 2011;12(Suppl 2):20–28. doi: 10.1111/j.1467-789X.2011.00904.x. [DOI] [PubMed] [Google Scholar]
- 102.Naul R, Schmelt D, Dreiskaemper D, Hoffmann D, l’Hoir M. ‘Healthy children in sound communities’ (HCSC/gkgk) – a Dutch-German community-based network project to counteract obesity and physical inactivity. Fam Pract. 2012;29(Suppl 1):i110–i116. doi: 10.1093/fampra/cmr097. [DOI] [PubMed] [Google Scholar]
- 103.Tomlin D, Naylor PJ, McKay H, Zorzi A, Mitchell M, Panagiotopoulos C. The impact of Action Schools! BC on the health of Aboriginal children and youth living in rural and remote communities in British Columbia. Int J Circumpolar Health. 2012;71:17999. doi: 10.3402/ijch.v71i0.17999. [DOI] [PMC free article] [PubMed] [Google Scholar]
Appendix A5 School-based interventions with a community component
- 104.Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obes Facts. 2009;2:282–285. doi: 10.1159/000229783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Webber LS, Catellier DJ, Lytle LA, et al. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med. 2008;34:173–184. doi: 10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Crespo NC, Elder JP, Ayala GX, et al. Results of a multi-level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Ninos Study. Ann Behav Med. 2012;43:84–100. doi: 10.1007/s12160-011-9332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Macaulay AC, Paradis G, Potvin L, et al. The Kahnawake Schools Diabetes Prevention Project: intervention, evaluation, and baseline results of a diabetes primary prevention program with a native community in Canada. Prev Med. 1997;26:779–790. doi: 10.1006/pmed.1997.0241. [DOI] [PubMed] [Google Scholar]
- 108.Madsen KA, Thompson HR, Wlasiuk L, Queliza E, Schmidt C, Newman TB. After-school program to reduce obesity in minority children: a pilot study. J Child Health Care. 2009;13:333–346. doi: 10.1177/1367493509344823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Utter J, Scragg R, Robinson E, et al. Evaluation of the Living 4 Life project: a youth-led, school-based obesity prevention study. Obes Rev. 2011;12(Suppl 2):51–60. doi: 10.1111/j.1467-789X.2011.00905.x. [DOI] [PubMed] [Google Scholar]
Appendix A6 School-based interventions with a consumer health informatics component
- 110.Spiegel SA, Foulk D. Reducing overweight through a multi-disciplinary school-based intervention. Obesity (Silver Spring) 2006;14:88–96. doi: 10.1038/oby.2006.11. [DOI] [PubMed] [Google Scholar]
- 111.Ezendam NP, Brug J, Oenema A. Evaluation of the web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166:248–255. doi: 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 112.Schneider M, Dunton GF, Bassin S, Graham DJ, Eliakim AF, Cooper DM. Impact of a school-based physical activity intervention on fitness and bone in adolescent females. J Phys Act Health. 2007;4:17–29. doi: 10.1123/jpah.4.1.17. [DOI] [PubMed] [Google Scholar]
- 113.Prins RG, Brug J, van Empelen P, Oenema A. Effectiveness of YouRAction, an intervention to promote adolescent physical activity using personal and environmental feedback: a cluster RCT. PLoS One. 2012;7:e32682. doi: 10.1371/journal.pone.0032682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Whittemore R, Jeon S, Grey M. An internet obesity prevention program for adolescents. J Adolesc Health. 2013;52:439–447. doi: 10.1016/j.jadohealth.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Appendix A7 Home only-based interventions
- 115.Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res. 2001;9:171–178. doi: 10.1038/oby.2001.18. [DOI] [PubMed] [Google Scholar]
- 116.Lappe JM, Rafferty KA, Davies KM, Lypaczewski G. Girls on a high-calcium diet gain weight at the same rate as girls on a normal diet: a pilot study. J Am Diet Assoc. 2004;104:1361–1367. doi: 10.1016/j.jada.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 117.French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action – a group-randomized trial. Obesity (Silver Spring) 2011;19:2082–2088. doi: 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fitzgibbon ML, Stolley MR, Schiffer L, et al. Family-based hip-hop to health: outcome results. Obesity (Silver Spring) 2012;21:274–283. doi: 10.1038/oby.2012.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Appendix A8 Community-based or environmental-level interventions
- 119.Klesges RC, Obarzanek E, Kumanyika S, et al. The Memphis Girls’ health Enrichment Multi-site Studies (GEMS): an evaluation of the efficacy of a 2-year obesity prevention program in African American girls. Arch Pediatr Adolesc Med. 2010;164:1007–1014. doi: 10.1001/archpediatrics.2010.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Eiholzer U, Meinhardt U, Petro R, Witassek F, Gutzwiller F, Gasser T. High-intensity training increases spontaneous physical activity in children: a randomized controlled study. J Pediatr. 2010;156:242–246. doi: 10.1016/j.jpeds.2009.08.039. [DOI] [PubMed] [Google Scholar]
- 121.Singh AS, Chin A, Paw M, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–317. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- 122.Sallis JF, McKenzie TL, Conway TL, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. Am J Prev Med. 2003;24:209–217. doi: 10.1016/s0749-3797(02)00646-3. [DOI] [PubMed] [Google Scholar]
- 123.Chomitz VR, McGowan RJ, Wendel JM, et al. Healthy Living Cambridge Kids: a community-based participatory effort to promote healthy weight and fitness. Obesity (Silver Spring) 2010;18(Suppl 1):S45–S53. doi: 10.1038/oby.2009.431. [DOI] [PubMed] [Google Scholar]
- 124.Economos CD, Hyatt RR, Goldberg JP, et al. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity (Silver Spring) 2007;15:1325–1336. doi: 10.1038/oby.2007.155. [DOI] [PubMed] [Google Scholar]
- 125.Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;164:995–1004. doi: 10.1001/archpediatrics.2010.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91:831–840. doi: 10.3945/ajcn.2009.28826. [DOI] [PubMed] [Google Scholar]
- 127.Chang DI, Gertel-Rosenberg A, Drayton VL, Schmidt S, Angalet GB. A statewide strategy to battle child obesity in Delaware. Health Aff (Millwood) 2010;29:481–490. doi: 10.1377/hlthaff.2009.0742. [DOI] [PubMed] [Google Scholar]
- 128.Pettman T, Magarey A, Mastersson N, Wilson A, Dollman J. Improving weight status in childhood: results from the eat well be active community programs. Int J Public Health. 2014;59:43–50. doi: 10.1007/s00038-013-0455-4. [DOI] [PubMed] [Google Scholar]
Footnotes
Conflict of interest statement
No conflict of interest was declared.
Authors’ contributions
Youfa Wang is the study’s principal investigator. RFW is the project manager. Yang Wu is the project coordinator. Study concept and design were contributed by Youfa Wang, JS, LJC, RFW and Yang Wu. All authors and some other research team members were responsible for acquisition of data. All authors participated in the analysis and interpretation of data. Youfa Wang, RFW, Yang Wu, JS and LC drafted the manuscript. All authors were responsible for the critical revision of the manuscript for important intellectual content. LC, OF, BDL, RFW and Youfa Wang performed statistical analysis. Youfa Wang, RFW and JS conducted administrative, technical or material support. Study supervision was provided by Youfa Wang and RFW.
References
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States – gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control (CDC) [accessed August 2013];Vital Signs: Obesity among low-income, preschool-aged children – United States, 2008–2011. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6231a4.htm. [PMC free article] [PubMed]
- 3.Centers for Disease Control (CDC) [accessed August 2013];Childhood Overweight and Obesity. http://www.cdc.gov/obesity/childhood/index.html.
- 4.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24:176–188. doi: 10.3109/09540261.2012.688195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 7.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 8.Hampl SE, Summar MJ. ‘Weighing in’ on childhood obesity. Pediatr Ann. 2009;38:143–148. doi: 10.3928/00904481-20090301-07. [DOI] [PubMed] [Google Scholar]
- 9.Woolford SJ, Gebremariam A, Clark SJ, Davis MM. Incremental hospital charges associated with obesity as a secondary diagnosis in children. Obesity (Silver Spring) 2007;15:1895–1901. doi: 10.1038/oby.2007.224. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. [accessed May 2012];Global Strategy on Diet, Physical Activity, and Health. http://www.who.int/dietphysicalactivity/childhood_what_can_be_done/en/index.html.
- 11.Koplan JP, Liverman CT, Kraak VI. Preventing childhood obesity: health in the balance: executive summary. J Am Diet Assoc. 2005;105:131–138. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. National Academies Press; Washington, DC: 2012. [accessed May 2012]. http://www.iom.edu/Reports/2012/Accelerating-Progress-in-Obesity-Prevention.aspx. [PubMed] [Google Scholar]
- 13.Connelly JB, Duaso MJ, Butler G. A systematic review of controlled trials of interventions to prevent childhood obesity and overweight: a realistic synthesis of the evidence. Public Health. 2007;121:510–517. doi: 10.1016/j.puhe.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 14.Kamath CC, Vickers KS, Ehrlich A, et al. Clinical review: behavioral interventions to prevent childhood obesity: a systematic review and meta analyses of randomized trials. J Clin Endocrinol Metab. 2008;93:4606–4615. doi: 10.1210/jc.2006-2411. [DOI] [PubMed] [Google Scholar]
- 15.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity (Silver Spring) 2008;16:1009–1018. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 16.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;(12):CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Wu Y, Wilson RF, et al. [accessed June 2013];Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis. http://www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed]
- 18.United Nations. Human Development Reports. [accessed May 2012];Human Development Index. http://hdr.undp.org/en/statistics/hdi/
- 19.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 21.Owens DK, Lohr KN, Atkins D, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions – agency for healthcare research and quality and the effective health-care program. J Clin Epidemiol. 2010;63:513–523. doi: 10.1016/j.jclinepi.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 22.James J, Thomas P, Kerr D. Preventing childhood obesity: two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS) BMJ. 2007;335:762. doi: 10.1136/bmj.39342.571806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ. 2004;328:1237. doi: 10.1136/bmj.38077.458438.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vandongen R, Jenner DA, Thompson C, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10- to 12-year-old children. Prev Med. 1995;24:9–22. doi: 10.1006/pmed.1995.1003. [DOI] [PubMed] [Google Scholar]
- 25.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367:1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 26.Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: switch-play. Int J Obes (Lond) 2008;32:601–612. doi: 10.1038/sj.ijo.0803805. [DOI] [PubMed] [Google Scholar]
- 27.Lazaar N, Aucouturier J, Ratel S, Rance M, Meyer M, Duche P. Effect of physical activity intervention on body composition in young children: influence of body mass index status and gender. Acta Paediatr. 2007;96:1315–1320. doi: 10.1111/j.1651-2227.2007.00426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martinez Vizcaino V, Salcedo Aguilar F, Franquelo Gutierrez R, et al. Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children: a cluster randomized trial. Int J Obes (Lond) 2008;32:12–22. doi: 10.1038/sj.ijo.0803738. [DOI] [PubMed] [Google Scholar]
- 29.Valdimarsson O, Linden C, Johnell O, Gardsell P, Karlsson MK. Daily physical education in the school curriculum in prepubertal girls during 1 year is followed by an increase in bone mineral accrual and bone width – data from the prospective controlled Malmo pediatric osteoporosis prevention study. Calcif Tissue Int. 2006;78:65–71. doi: 10.1007/s00223-005-0096-6. [DOI] [PubMed] [Google Scholar]
- 30.Reed KE, Warburton DE, Macdonald HM, Naylor PJ, McKay HA. Action Schools! BC: a school-based physical activity intervention designed to decrease cardiovascular disease risk factors in children. Prev Med. 2008;46:525–531. doi: 10.1016/j.ypmed.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 31.Donnelly JE, Greene JL, Gibson CA, et al. Physical Activity Across the Curriculum (PAAC): a randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–341. doi: 10.1016/j.ypmed.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stenevi-Lundgren S, Daly RM, Linden C, Gardsell P, Karlsson MK. Effects of a daily school based physical activity intervention program on muscle development in prepubertal girls. Eur J Appl Physiol. 2009;105:533–541. doi: 10.1007/s00421-008-0932-2. [DOI] [PubMed] [Google Scholar]
- 33.Manios Y, Moschandreas J, Hatzis C, Kafatos A. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br J Nutr. 2002;88:315–324. doi: 10.1079/BJN2002672. [DOI] [PubMed] [Google Scholar]
- 34.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 35.Will JC, Massoudi B, Mokdad A, et al. Reducing risk for cardiovascular disease in uninsured women: combined results from two WISEWOMAN projects. J Am Med Womens Assoc. 2001;56:161–165. [PubMed] [Google Scholar]
- 36.Heelan KA, Abbey BM, Donnelly JE, Mayo MS, Welk GJ. Evaluation of a walking school bus for promoting physical activity in youth. J Phys Act Health. 2009;6:560–567. doi: 10.1123/jpah.6.5.560. [DOI] [PubMed] [Google Scholar]
- 37.Warren JM, Henry CJ, Lightowler HJ, Bradshaw SM, Perwaiz S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot Int. 2003;18:287–296. doi: 10.1093/heapro/dag402. [DOI] [PubMed] [Google Scholar]
- 38.Foster GD, Linder B, Baranowski T, et al. A school-based intervention for diabetes risk reduction. N Engl J Med. 2010;363:443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosario R, Oliveira B, Araujo A, et al. The impact of an intervention taught by trained teachers on childhood overweight. Int J Environ Res Public Health. 2012;9:1355–1367. doi: 10.3390/ijerph9041355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amaro S, Viggiano A, Di Costanzo A, et al. Kaledo, a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: a pilot cluster randomized trial. Eur J Pediatr. 2006;165:630–635. doi: 10.1007/s00431-006-0153-9. [DOI] [PubMed] [Google Scholar]
- 41.Lubans DR, Morgan PJ, Okely AD, et al. Preventing obesity among adolescent girls: one-year outcomes of the Nutrition and Enjoyable Activity for Teen Girls (NEAT Girls) cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166:821–827. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 42.Bonsergent E, Agrinier N, Thilly N, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013;44:30–39. doi: 10.1016/j.amepre.2012.09.055. [DOI] [PubMed] [Google Scholar]
- 43.Gutin B, Yin Z, Johnson M, Barbeau P. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: the Medical College of Georgia Fitkid Project. Int J Pediatr Obes. 2008;3(Suppl 1):3–9. doi: 10.1080/17477160801896457. [DOI] [PubMed] [Google Scholar]
- 44.Barbeau P, Johnson MH, Howe CA, et al. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity (Silver Spring) 2007;15:2077–2085. doi: 10.1038/oby.2007.247. [DOI] [PubMed] [Google Scholar]
- 45.Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, Johannsson E, Sveinsson T. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ Res. 2012;27:484–494. doi: 10.1093/her/cys049. [DOI] [PubMed] [Google Scholar]
- 46.Neumark-Sztainer DR, Friend SE, Flattum CF, et al. New moves-preventing weight-related problems in adolescent girls a group-randomized study. Am J Prev Med. 2010;39:421–432. doi: 10.1016/j.amepre.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Llargues E, Recasens A, Franco R, et al. Medium-term evaluation of an educational intervention on dietary and physical exercise habits in schoolchildren: the Avall 2 study. Endocrinol Nutr. 2012;59:288–295. doi: 10.1016/j.endonu.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 48.Howe CA, Harris RA, Gutin B. A 10-month physical activity intervention improves body composition in young black boys. J Obes. 2011;2011:358581. doi: 10.1155/2011/358581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morgan PJ, Saunders KL, Lubans DR. Improving physical self-perception in adolescent boys from disadvantaged schools: psychological outcomes from the Physical Activity Leaders randomized controlled trial. Pediatr Obes. 2012;7:e27–e32. doi: 10.1111/j.2047-6310.2012.00050.x. [DOI] [PubMed] [Google Scholar]
- 50.Simonetti D’Arca A, Tarsitani G, Cairella M, et al. Prevention of obesity in elementary and nursery school children. Public Health. 1986;100:166–173. doi: 10.1016/s0033-3506(86)80030-0. [DOI] [PubMed] [Google Scholar]
- 51.Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 53.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes (Lond) 2008;32:1489–1498. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 54.Foster GD, Sherman S, Borradaile KE, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794–e802. doi: 10.1542/peds.2007-1365. [DOI] [PubMed] [Google Scholar]
- 55.Marcus C, Nyberg G, Nordenfelt A, Karpmyr M, Kowalski J, Ekelund U. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int J Obes (Lond) 2009;33:408–417. doi: 10.1038/ijo.2009.38. [DOI] [PubMed] [Google Scholar]
- 56.Burke V, Milligan RA, Thompson C, et al. A controlled trial of health promotion programs in 11-year-olds using physical activity ‘enrichment’ for higher risk children. J Pediatr. 1998;132:840–848. doi: 10.1016/s0022-3476(98)70315-4. [DOI] [PubMed] [Google Scholar]
- 57.Dzewaltowski DA, Rosenkranz RR, Geller KS, et al. HOP’N after-school project: an obesity prevention randomized controlled trial. Int J Behav Nutr Phys Act. 2010;7:90. doi: 10.1186/1479-5868-7-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Siegrist M, Lammel C, Haller B, Christle J, Halle M. Effects of a physical education program on physical activity, fitness, and health in children: the JuvenTUM project. Scand J Med Sci Sports. 2013;23:323–330. doi: 10.1111/j.1600-0838.2011.01387.x. [DOI] [PubMed] [Google Scholar]
- 59.Story M, Hannan PJ, Fulkerson JA, et al. Bright Start: description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity (Silver Spring) 2012;20:2241–2249. doi: 10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hatzis CM, Papandreou C, Kafatos AG. School health education programs in Crete: evaluation of behavioural and health indices a decade after initiation. Prev Med. 2010;51:262–267. doi: 10.1016/j.ypmed.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 61.Mihas C, Mariolis A, Manios Y, et al. Evaluation of a nutrition intervention in adolescents of an urban area in Greece: short- and long-term effects of the VYRONAS study. Public Health Nutr. 2010;13:712–719. doi: 10.1017/S1368980009991625. [DOI] [PubMed] [Google Scholar]
- 62.Llargues E, Franco R, Recasens A, et al. Assessment of a school-based intervention in eating habits and physical activity in school children: the AVall study. J Epidemiol Community Health. 2011;65:896–901. doi: 10.1136/jech.2009.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Centis E, Marzocchi R, Di Luzio R, et al. A controlled, class-based multicomponent intervention to promote healthy lifestyle and to reduce the burden of childhood obesity. Pediatr Obes. 2012;7:436–445. doi: 10.1111/j.2047-6310.2012.00079.x. [DOI] [PubMed] [Google Scholar]
- 64.Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obes Facts. 2009;2:282–285. doi: 10.1159/000229783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Webber LS, Catellier DJ, Lytle LA, et al. Promoting physical activity in middle school girls: trial of activity for adolescent girls. Am J Prev Med. 2008;34:173–184. doi: 10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Spiegel SA, Foulk D. Reducing overweight through a multi-disciplinary school-based intervention. Obesity (Silver Spring) 2006;14:88–96. doi: 10.1038/oby.2006.11. [DOI] [PubMed] [Google Scholar]
- 67.Gorely T, Morris JG, Musson H, Brown S, Nevill A, Nevill ME. Physical activity and body composition outcomes of the GreatFun2Run intervention at 20 month follow-up. Int J Behav Nutr Phys Act. 2011;8:74. doi: 10.1186/1479-5868-8-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gentile DA, Welk G, Eisenmann JC, et al. Evaluation of a multiple ecological level child obesity prevention program: switch what you do, view, and chew. BMC Med. 2009;7:49. doi: 10.1186/1741-7015-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Patrick K, Calfas KJ, Norman GJ, et al. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2006;160:128–136. doi: 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- 70.Polacsek M, Orr J, Letourneau L, et al. Impact of a primary care intervention on physician practice and patient and family behavior: keep ME Healthy – the Maine Youth Overweight Collaborative. Pediatrics. 2009;123(Suppl 5):S258–S266. doi: 10.1542/peds.2008-2780C. [DOI] [PubMed] [Google Scholar]
- 71.Birken CS, Maguire J, Mekky M, et al. Office-based randomized controlled trial to reduce screen time in preschool children. Pediatrics. 2012;130:1110–1115. doi: 10.1542/peds.2011-3088. [DOI] [PubMed] [Google Scholar]
- 72.Slusser W, Frankel F, Robison K, Fischer H, Cumberland WG, Neumann C. Pediatric overweight prevention through a parent training program for 2–4 year old Latino children. Child Obes. 2012;8:52–59. doi: 10.1089/chi.2011.0060. [DOI] [PubMed] [Google Scholar]
- 73.Bayer O, von Kries R, Strauss A, et al. Short- and mid-term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster-randomized trial. Clin Nutr. 2009;28:122–128. doi: 10.1016/j.clnu.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 74.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity (Silver Spring) 2006;14:1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- 75.Puder JJ, Marques-Vidal P, Schindler C, et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. BMJ. 2011;343:d6195. doi: 10.1136/bmj.d6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Scheffler C, Ketelhut K, Mohasseb I. Does physical education modify the body composition?– results of a longitudinal study of pre-school children. Anthropol Anz. 2007;65:193–201. [PubMed] [Google Scholar]
- 77.Krombholz H. The impact of a 20-month physical activity intervention in child care centers on motor performance and weight in overweight and healthy-weight preschool children. Percept Mot Skills. 2012;115:919–932. doi: 10.2466/06.10.25.PMS.115.6.919-932. [DOI] [PubMed] [Google Scholar]
- 78.Singh AS, Chin A, Paw M, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–317. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- 79.Sallis JF, McKenzie TL, Conway TL, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. Am J Prev Med. 2003;24:209–217. doi: 10.1016/s0749-3797(02)00646-3. [DOI] [PubMed] [Google Scholar]
- 80.Chomitz VR, McGowan RJ, Wendel JM, et al. Healthy Living Cambridge Kids: a community-based participatory effort to promote healthy weight and fitness. Obesity (Silver Spring) 2010;18(Suppl 1):S45–S53. doi: 10.1038/oby.2009.431. [DOI] [PubMed] [Google Scholar]
- 81.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009;180:719–726. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cai L, Wu Y, Wilson RF, Segal JB, Kim MT, Wang Y. Effect of childhood obesity prevention programs on blood pressure: a systematic review and meta-analysis. Circulation. 2014;129:1832–1839. doi: 10.1161/CIRCULATIONAHA.113.005666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cai L, Wu Y, Cheskin LJ, Wilson RF, Wang Y. Effect of childhood obesity prevention programmes on blood lipids: a systematic review and meta-analysis. Obes Rev. 2014;15:933–944. doi: 10.1111/obr.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]