Abstract
Background
Functional improvements have been seen in stroke patients who have received an increased intensity of physiotherapy. This requires additional costs in the form of increased physiotherapist time.
Objectives
The objective of this economic analysis is to determine the cost-effectiveness of increasing the intensity of physiotherapy (duration and/or frequency) during inpatient rehabilitation after stroke, from the perspective of the Ontario Ministry of Health and Long-term Care.
Data Sources
The inputs for our economic evaluation were extracted from articles published in peer-reviewed journals and from reports from government sources or the Canadian Stroke Network. Where published data were not available, we sought expert opinion and used inputs based on the experts' estimates.
Review Methods
The primary outcome we considered was cost per quality-adjusted life-year (QALY). We also evaluated functional strength training because of its similarities to physiotherapy. We used a 2-state Markov model to evaluate the cost-effectiveness of functional strength training and increased physiotherapy intensity for stroke inpatient rehabilitation. The model had a lifetime timeframe with a 5% annual discount rate. We then used sensitivity analyses to evaluate uncertainty in the model inputs.
Results
We found that functional strength training and higher-intensity physiotherapy resulted in lower costs and improved outcomes over a lifetime. However, our sensitivity analyses revealed high levels of uncertainty in the model inputs, and therefore in the results.
Limitations
There is a high level of uncertainty in this analysis due to the uncertainty in model inputs, with some of the major inputs based on expert panel consensus or expert opinion. In addition, the utility outcomes were based on a clinical study conducted in the United Kingdom (i.e., 1 study only, and not in an Ontario or Canadian setting).
Conclusions
Functional strength training and higher-intensity physiotherapy may result in lower costs and improved health outcomes. However, these results should be interpreted with caution.
PLAIN LANGUAGE SUMMARY
Physiotherapy plays an important role in patients' recovery after stroke. Studies have shown that patients who get more physiotherapy (either longer or more frequent sessions) may have greater improvement. However, this involves the added cost of more physiotherapist hours.
In this economic analysis, we explored whether increased physiotherapy for stroke patients could be cost-effective for Ontario's health care system. Specifically, we looked at the early phase after stroke (during inpatient rehabilitation). We did a literature search for articles published in peer-reviewed journals. We found additional data in government reports and statistics, and from the Canadian Stroke Network. When information wasn't available otherwise, we sought expert opinion.
We balanced the additional cost against the number of quality-adjusted life years that patients would gain. A quality-adjusted life-year (QALY) is calculated by taking the number of years someone is expected to gain as the result of a treatment, and adjusting it based on the quality of life they are expected to have. We used a Markov model (a type of decision analysis that allows for movement between different health states over time) to develop a basic scenario. We then changed some of the variables, to consider multiple other scenarios.
Overall, we found that increased physiotherapy for stroke patients could be cost-effective in Ontario. It could improve health outcomes and also reduce costs for the health care system. This is because patients who received more physiotherapy would have a shorter stay in rehabilitation facilities. These reductions could more than offset the extra physiotherapist hours.
However, it should be noted that we had limited data in some areas and were unsure about the quality of data in other areas. These findings should therefore be treated with uncertainty and caution.
BACKGROUND
The Toronto Health Economics and Technology Assessment (THETA) Collaborative was commissioned by Health Quality Ontario to evaluate the cost-effectiveness of increased intensity of physiotherapy during rehabilitation after stroke. Published economic evaluations are reviewed, and the structure and inputs of the economic model used to estimate cost-effectiveness are summarized. The results of the economic analyses are presented for increased-intensity versus conventional physiotherapy, and the budget impact of implementing each intervention is estimated.
Health Quality Ontario conducts full evidence-based analyses, including economic analyses, of health technologies being considered for use in Ontario. These analyses are then presented to the Ontario Health Technology Advisory Committee, whose mandate it is to examine proposed health technologies in the context of available evidence and existing clinical practice, and to provide advice and recommendations to Ontario health care practitioners, the broader health care system, and the Ontario Ministry of Health and Long-Term Care.
DISCLAIMER: Health Quality Ontario uses a standardized costing method for its economic analyses. The main cost category and associated methods of retrieval from the province's perspective are described below.
Hospital costs: The cost of additional physiotherapy care was provided by the wage report presented by the Workplace Partnership Directorate, Government of Canada, and from clinical trial data. The cost of inpatient rehabilitation was extracted from a report published by the Ontario Stroke Network. It was assumed that there were no additional hospital cost differences between the intervention and comparator.
Non-hospital costs: It was assumed that there were no non-hospital cost differences between intervention and comparator.
Discounting: For cost-effectiveness analyses, a discount rate of 5% is applied (to both costs and effects/QALYs), as recommended by economic guidelines.
Downstream costs: It was assumed that there were no downstream cost differences between intervention and comparator.
The economic analysis represents an estimate only, based on the assumptions and costing methods explicitly stated above. These estimates will change if different assumptions and costing methods are applied to the analysis.
NOTE: Numbers may be rounded to the nearest decimal point, as they may be reported from an Excel spreadsheet.
Objective of Analysis
The objective is to determine the cost-effectiveness of increasing the intensity (duration and/or frequency) of physiotherapy during inpatient rehabilitation for people with stroke, from the perspective of the Ontario Ministry of Health and Long-Term Care.
Clinical Need and Target Population
Description of Disease/Condition
A stroke occurs when there is an interruption in blood flow to the brain (ischemic stroke) or a blood- vessel rupture in the brain (hemorrhagic stroke). (1) It causes brain cells (neurons) in the affected area to die, resulting in an immediate loss of brain function. The impact depends on the location of brain injury and extent of damage. A stroke can affect a person's memory, sight, speech, reasoning, motor function, and ability to read and write.
Prevalence and Incidence
In Ontario, more than 22,000 cases of confirmed or suspected stroke or transient ischemic attack (TIA, also called “mini-stroke”) were discharged from acute care facilities between April 1, 2010, and March 31, 2011. (2) In Canada, more than 300,000 people in the community reportedly suffer from the effects of a stroke. (3)
Intervention Under Evaluation
In a review of the clinical evidence for physiotherapy (PT) for stroke patients, Van Peppen and colleagues concluded that studies “support the use of physical therapy to improve performance as well as the capacity to perform regular daily activities after stroke.” (4) The largest improvements were observed for sit-to-stand transfer training, glenohumeral subluxation neuromuscular stimulation, and gait and treadmill training with external auditory rhythms. The smallest statistically significant improvements were seen in studies supporting increased intensity of exercise training.
For this analysis, the intervention of interest is increased intensity of PT for stroke rehabilitation. This will be compared to the standard level of PT received by the average stroke patient. Intensity has numerous meanings in rehabilitation medicine. It can be defined from a biomechanical perspective that observes the amount of work or energy exerted to perform a specific task or set of tasks. (5) It can also be viewed as the frequency of repetitions of a task or the duration of time dedicated to the task. (5) Most studies have evaluated the latter. (5) For this analysis, intensity means the total amount of PT time provided to a stroke patient; increased intensity means any PT time beyond the typical amount a patient is expected to receive.
ECONOMIC ANALYSIS
Research Question
What is the cost-effectiveness of increasing the intensity (duration and/or frequency) of physiotherapy during inpatient rehabilitation for people with stroke? The question will be considered from the perspective of the Ontario Ministry of Health and Long-Term Care.
Economic Literature Review
Research Methods
Literature Search
Search Strategy
Economic literature searches were performed from November 12, 2013 to December 3, 2013, using Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid Embase, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), and Wiley Cochrane Library databases for studies published from the earliest record of each database to November 12, 2013 for MEDLINE, and December 2, 2013 for Embase and Cochrane. (Appendix 1 provides details of the search strategies.) Titles and abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. The reference lists of all full-text articles were also examined for any additional relevant studies not identified in the original search.
Inclusion Criteria
English-language full-text publications
published between January 1, 2000, and November 12, 2013/December 3, 2013 (see Search Strategy, above)
full economic evaluations: cost-utility analyses, cost-effectiveness analyses, cost-benefit analyses
economic evaluations reporting incremental cost-effectiveness ratios (i.e., reporting cost per quality-adjusted life-year [QALY], per life-year gained, or per event avoided)
studies of patients with stroke
studies reporting on an intervention that increases the intensity of PT delivered to the patient
Exclusion Criteria
studies where the patients in the conventional intervention do not receive any PT
studies evaluating a multidisciplinary team rehabilitation model
Results of Economic Literature Review
The database search yielded 254 citations (with duplicates removed). A total of 247 articles were excluded after the title and abstract review. The full texts of the remaining 7 articles were extracted for a more detailed review (6–12) and none met the inclusion criteria. A review of the reference lists did not result in any other potential articles.
Primary Economic Evaluation
Because our literature review did not identify any published studies on the cost-effectiveness of increased PT intensity for stroke rehabilitation, we conducted a primary economic evaluation.
Research Methods
Type of Analysis
Parallel to this report, Health Quality Ontario conducted a clinical review on the same topic (an evidence-based analysis [EBA]). (13) The EBA found that statistically significant improvements were observed when PT after stroke was more intensive, according to specific functional measures. It concluded that available evidence supports the use of higher-intensity PT for the improvement of limb activities and function and activities of daily living (ADL). For quality of life, however, 3 studies were identified in the EBA that reported only non-statistically significant improvements with more intensive PT. Quality of life was a secondary outcome in these studies, so it is likely that they were underpowered to detect these differences. To explore this issue and to determine the economic impact of increased PT intensity after stroke, we chose to conduct our primary economic evaluation as a full cost-utility analysis, using Markov modelling.
Intervention Evaluated
As stated earlier, the intervention being evaluated is higher-intensity PT for stroke rehabilitation compared with standard levels of PT; and higher intensity is defined in this analysis as a greater quantity of PT time. There is no minimum threshold at which an increased amount of PT time is deemed “higher intensity.” Thus, we have taken the boundaries of the term from the intervention described in the clinical trial which we have included in our analysis. (14) This clinical trial was conducted in an inpatient setting during the rehabilitation period after stroke, so we have limited the PT intervention in our economic evaluation to the same period. Functional strength training (FST) was also evaluated in the same clinical trial. This intervention involved additional PT, focused on resistive exercises of the paretic lower limb to improve muscle strength and the ability to perform functional activities. Since this intervention is similar to higher-intensity PT, it is included in our economic evaluation.
Perspective
The analysis was conducted from the perspective of the Ontario Ministry of Health and Long-Term Care.
Discounting and Time Horizon
An annual discount rate of 5% was applied to both costs and quality-adjusted life-years (QALYs), as recommended by the Canadian Agency for Drugs and Technologies in Health (CADTH). (15) A lifelong time horizon was used in all analyses. A half-cycle correction was included to address the concern that transitions occur only at the beginning or end of each cycle. (15)
Target Population
The hypothetical target population of this analysis is recent stroke patients who require PT rehabilitation in Ontario. They would have a mean age of 73, as reported in an Ontario stroke audit, (16) and 50 % would be female. (17)
Variability and Uncertainty
As will be shown, there is uncertainty in the input parameters of our model, with some of our major inputs based on expert panel consensus or expert opinion. Given this level of uncertainty, we conducted probabilistic sensitivity analyses, using assigned distributions on point estimates where possible. Randomly sampling from each distribution, we ran the model repeatedly to provide a range of possible outcomes. The results inform the probability of cost-effectiveness through a range of willingness-to-pay values.
Generalizability
The generalizability of this study is limited to a population similar to the patient population represented in the clinical study by Cooke and colleagues, (14) from which we extracted the utilities. The results may be used by Health Quality Ontario to help guide decision-making for similar patient populations.
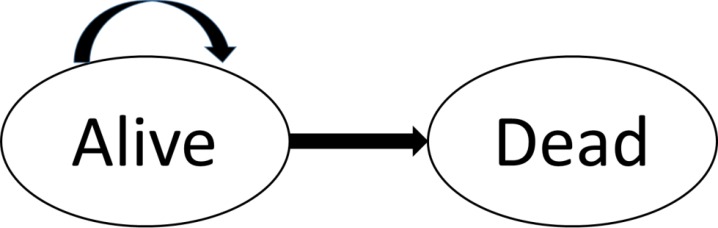
Model Structure
The clinical literature showed that the functional improvements associated with higher-intensity PT were not linked to any downstream improvements, i.e., did not result in changes to the stroke disease trajectory in terms of disease progression, risk for other co-morbidities, or risk of future strokes, in either the short term or long term. Therefore, the Markov model we developed to model lifetime outcomes comprised 2 states only (Figure 1).
Figure 1: Schematic Diagram of Model Structure for 2-State Markov Model.
Cost differentials are anticipated between intervention and comparator. This is because of additional physiotherapist visits on one hand, and a reduced length of stay in inpatient rehabilitation on the other. However, we assume that there will be no downstream costs associated with the intervention. This assumption is supported by expert opinion. (Personal communication, Clinical Expert, February 7, 2014) Improvements in QALY (utilities), on the other hand, are expected to last more than a year. (Personal communication, Clinical Expert, February 7, 2014) Therefore the mortality of a cohort of stroke patients will need to be modelled over time, to calculate QALYs.
Model Input Parameters
Model inputs for this analysis can be categorized into clinical outcomes such as life tables, standardized mortality ratios for stroke, utility values, and cost outcomes including physiotherapist wages and cost of inpatient rehabilitation.
Clinical Outcomes—Quality of Life with Higher-Intensity PT (intervention utilities)
Note was made earlier of 3 studies, included in the parallel EBA on this topic, (13) that evaluated high-intensity PT and included quality-of-life outcomes. In 1 of these studies, Harris and colleagues (18) compared quality-of-life measures between treatment arms, using the 12–Item Short Form Survey (SF-12). The authors noted that no differences were observed, but did not present any numbers. For this reason, we excluded their study from our economic analysis. In another of the 3 studies, the Glasgow Augmented Physiotherapy Study group (19) used the EuroQol-5D (EQ-5D) visual analogue scale to evaluate quality of life at baseline and 6 months. The authors observed a non-statistically significant increase in score for the higher-intensity PT group. Unfortunately, the EQ-5D visual analogue scale cannot be mapped into utility values. So we excluded the results of this study too.
The third study, by Cooke and colleagues (14), is included in our analysis. Its quality-of-evidence evaluation can be found in the above-mentioned EBA. (13) A randomized controlled trial (RCT) conducted in the United Kingdom, this study compared higher-intensity PT with conventional PT, and also FST in addition to PT with conventional PT. (14) There were 109 participants, with 36 receiving FST and conventional PT, 35 receiving higher-intensity PT, and 38 receiving conventional PT only. People randomized to the intervention arm received up to 1 extra hour of therapy (PT or FST) 4 days a week for 6 weeks. A follow-up was conducted at 18 weeks. The EQ-5D measurement was taken at baseline, 6 weeks, and at follow-up. For this analysis, we used the utilities recorded at 6 weeks because of our concern that the 18–week utilities might not be representative, since a greater number of participants were lost to follow-up in the conventional PT arm. In estimating the duration of effect, we assumed that the differences at 6 weeks would be sustained at 1 year and then gradually decline. The EQ-5D results at baseline and 6 weeks are presented in Table 1.
Table 1:
Results of Included RCT—Utility Differences at Baseline and 6 Weeks
| EQ-5D (standard deviation) | ||
|---|---|---|
| Baseline | 6 Weeks | |
| FST + conventional physiotherapy | 0.38 (0.39) | 0.59 (0.32) |
| Higher-intensity physiotherapy | 0.40 (0.36) | 0.54 (0.30) |
| Conventional physiotherapy | 0.39 (0.33) | 0.47 (0.31) |
Abbreviations: EQ-5D, EuroQol-5D; FST, functional strength training.
Data source: Cooke et al. (13)
Clinical Outcomes—Duration of Treatment Effect
The literature search that was conducted in the parallel EBA (13) found no evidence of long-term effects associated with higher-intensity PT in stroke patients. Thus, beyond the trial period observed by Cooke and colleagues, potential differences in utility scores are unknown. To estimate the duration of treatment effect, we solicited the opinion of a clinical expert. (Personal communication, Clinical Expert, February 7, 2014) Based on the expert opinion, we estimated the duration of effect of higher-intensity PT as 2 years of higher utility values, with the difference in values gradually decreasing to 0 over this period.
Clinical Outcomes—Probability of Mortality Over Time
Ontario stroke mortality rates for up to 1 year post-stroke are reported in the Ontario Stroke Evaluation Report. (20) The results based on the calculation from the years 2009/2010 to 2010/2011 are presented in Table 2.
Table 2:
Ontario Stroke Mortality Rate for 2009/2010 to 2010/2011
| Mean Adjusted Rate (95% CI) | |
|---|---|
| Ontario 1–year mortality rate | 25.3 (24.8–25.7) |
Abbreviation: CI, confidence interval.
Data source: Ontario Stroke Evaluation Report. (20)
Ontario stroke mortality rates beyond the first year are not reported. So, for this analysis, we used Statistics Canada life tables and standardized mortality ratios from literature to estimate the long-term mortality rates of stroke (over lifetime). From the most recent published life tables (2009 to 2010) (21), we extracted probability of mortality over time in the general population. From this, we selected the probability-of-mortality figures for Canadians aged 74 to 100 years (Table 3), since these ages are in keeping with our hypothetical cohort. We finally multiplied these figures by the increase in mortality risk associated with stroke (Table 4).
Table 3:
General Population Life-Table Inputs Used in Primary Economic Evaluation
| Age | Female | Male | ||
|---|---|---|---|---|
| Probability of Mortality | 95% Confidence Interval | Male | 95% Confidence Interval | |
| 74 | 0.019 | 0.019–0.020 | 0.030 | 0.029–0.031 |
| 75 | 0.021 | 0.021–0.022 | 0.033 | 0.032–0.034 |
| 76 | 0.024 | 0.023–0.024 | 0.037 | 0.036–0.037 |
| 77 | 0.027 | 0.026–0.027 | 0.040 | 0.039–0.041 |
| 78 | 0.030 | 0.029–0.030 | 0.044 | 0.044–0.045 |
| 79 | 0.033 | 0.032–0.033 | 0.049 | 0.048–0.050 |
| 80 | 0.037 | 0.036–0.037 | 0.054 | 0.053–0.055 |
| 81 | 0.041 | 0.040–0.042 | 0.059 | 0.058–0.060 |
| 82 | 0.046 | 0.045–0.046 | 0.065 | 0.064–0.067 |
| 83 | 0.051 | 0.050–0.052 | 0.072 | 0.071–0.073 |
| 84 | 0.057 | 0.056–0.058 | 0.080 | 0.078–0.081 |
| 85 | 0.063 | 0.062–0.064 | 0.088 | 0.086–0.089 |
| 86 | 0.071 | 0.070–0.072 | 0.097 | 0.095–0.099 |
| 87 | 0.079 | 0.078–0.081 | 0.107 | 0.105–0.109 |
| 88 | 0.089 | 0.088–0.090 | 0.118 | 0.116–0.120 |
| 89 | 0.100 | 0.098–0.101 | 0.130 | 0.127–0.133 |
| 90 | 0.112 | 0.110–0.114 | 0.143 | 0.140–0.146 |
| 91 | 0.125 | 0.123–0.128 | 0.158 | 0.154–0.162 |
| 92 | 0.140 | 0.137–0.142 | 0.173 | 0.169–0.178 |
| 93 | 0.155 | 0.153–0.158 | 0.189 | 0.184–0.194 |
| 94 | 0.172 | 0.169–0.175 | 0.206 | 0.200–0.212 |
| 95 | 0.189 | 0.185–0.192 | 0.218 | 0.211–0.226 |
| 96 | 0.207 | 0.202–0.211 | 0.235 | 0.227–0.244 |
| 97 | 0.226 | 0.220–0.231 | 0.253 | 0.243–0.263 |
| 98 | 0.245 | 0.239–0.252 | 0.271 | 0.258–0.284 |
| 99 | 0.266 | 0.257–0.274 | 0.289 | 0.273–0.306 |
| 100 | 0.287 | 0.277–0.297 | 0.308 | 0.290–0.326 |
Data source: Statistics Canada. (21)
Table 4:
Increase in Mortality Rates for Stroke Survivors, Compared With General Population, Used in Primary Economic Evaluation
| Years After Stroke | Standardized Mortality Ratio (95% Confidence Interval) | |
|---|---|---|
| Men | Women | |
| 1–5 | 1.92 (1.68–2.18) | 2.05 (1.81–2.30) |
| 5–10 | 1.89 (1.56–2.27) | 1.99 (1.67–2.36) |
| 10–15 | 2.49 (1.48–3.93) | 1.67 (1.08–2.47) |
Source: Bronnum-Hansen et al. (22)
To determine the increased mortality risk associated with stroke, we extracted standardized mortality ratios from the results of a Danish cohort study of more than 4,000 people (Table 4). (22) Ratios were presented for people 70 years of age and greater for up to 15 years after stroke. Since life tables are stratified by sex and total population mortality risk was not reported, we also extracted results for standardized mortality ratios stratified by sex. Study follow-up was limited to 15 years. For our analysis, we assumed that standardized mortality ratio values for stroke patients who live beyond 15 years are identical to the values observed for 10–to-15 years post-stroke. Since first-year mortality rates for stroke patients in Ontario are available, the standardized mortality ratio for years 0 to 1 after stroke was not used in the base case, but was explored in the sensitivity analysis.
Cost Outcomes—Physiotherapist Hours
The total mean time spent by physiotherapists for each intervention was also presented in the study by Cooke and colleagues (14), and we used it as a measure of the additional physiotherapist time required to administer higher-intensity PT (see Table 5). According to expert opinion, the total number of hours of conventional PT reported by Cooke and colleagues is similar to that which is experienced on average in Ontario. (Personal communication, Clinical Experts, February 7, 2014 and February 10, 2014) The total number of hours of FST and higher-intensity PT are also similar to what would be expected in Ontario if these interventions were implemented. (Personal communication, Clinical Expert, February 10, 2014)
Table 5:
Physiotherapist Hours Spent on Conventional PT, Higher-Intensity PT, and FST Plus Conventional PT
| Total Mean Number of Physiotherapist Hours (standard deviation) | |
|---|---|
| Functional strength training + conventional physiotherapy | 23.5 (10.0) |
| Higher-intensity physiotherapy | 23.0 (10.4) |
| Conventional physiotherapy | 9.2 (6.9) |
Abbreviations: FST, functional strength training; PT, physiotherapy.
Data source: Cooke et al. (14)
We extracted the average wage of a physiotherapist in Ontario from a wage report compiled by the federal government's Workplace Partnerships Directorate. (23) We used the median wage of $35.02 per hour, compiled from 10 different regions of the province. A median wage of $36.70 was reported for the Windsor-Sarnia region; we excluded this from the base case. To calculate the cost of physiotherapist time for the 3 intervention arms, we multiplied the number of PT hours by the median wage. Table 6 shows the results.
Table 6:
Cost of Physiotherapist Time for Conventional PT, Higher-Intensity PT, and FST Plus Conventional PT
| Total Cost for Physiotherapist Time | |
|---|---|
| Functional strength training + conventional physiotherapy | $822.97 |
| Higher-intensity physiotherapy | $805.46 |
| Conventional physiotherapy | $322.18 |
Cost Outcomes—Inpatient Rehabilitation Length of Stay
In a report on the impact of instituting best stroke rehabilitation practices in Ontario, Meyer and colleagues (24) analyzed the impact of increasing rehabilitation therapy from 5 to 7 days per week. The authors suggested that higher-intensity PT could, conservatively speaking, reduce inpatient rehabilitation length of stay by 1 day for every week of therapy (a 14% reduction). Therefore, we took the mean length of stay for 2011/2012 (extracted from the Ontario Stroke Evaluation Report) (20) and multiplied it by 0.86 (calculated by subtracting 1 by 0.14 reduction in inpatient rehabilitation length of stay). We assumed that the improvement in outcomes for FST plus PT would be the same as for higher-intensity PT, and that the length-of-stay standard deviation for the other 2 interventions would be the same as it is for conventional PT. The results are presented in Table 7.
Table 7:
Length of Stay in Inpatient Rehabilitation for Conventional PT, Higher-Intensity PT, and FST Plus Conventional PT
| Mean Length of Stay (standard deviation) | |
|---|---|
| Functional strength training + conventional physiotherapy | 28.63 days (22.9) |
| Higher-intensity physiotherapy | 28.63 days (22.9) |
| Conventional physiotherapy | 33.4 days (22.9) |
Abbreviations: FST, functional strength training; PT, physiotherapy.
Data source: Ontario Stroke Evaluation Report. (20)
The Meyer and colleagues report (24) included the average cost per bed day for inpatient rehabilitation. This was presented in 2008 Canadian dollars, which we inflated to 2013 Canadian dollars for our analysis, using the Consumer Price Index for medical and personal care as reported by Statistics Canada. (25) The resulting cost per bed day included the cost of physiotherapist time per day ($9.65), which we subtracted to avoid double counting. (To calculate it, we took the total cost of physiotherapist time for conventional PT [$322.18], as presented in Table 6, and divided it by the mean length of stay [33.4], as presented in Table 7.) Table 8 shows the cost per inpatient rehabilitation bed day, excluding physiotherapist time.
Table 8:
Cost per Inpatient Rehabilitation Bed Day
To calculate the total cost for inpatient rehabilitation less physiotherapist time, we multiplied the mean length of stay by the bed cost per day. The results are presented in Table 9.
Table 9:
Cost of Inpatient Rehabilitation, Less Physiotherapist Time, for Conventional PT, Higher-Intensity PT, and FST Plus Conventional PT
| Total Cost | |
|---|---|
| Functional strength training + conventional physiotherapy | $18,494.98 |
| Higher-intensity physiotherapy | $18,494.98 |
| Conventional physiotherapy | $21,576.40 |
Key Assumptions
The following assumptions were made for this analysis, due to uncertainty:
No additional costs are associated with the increased-therapy interventions (higher-intensity PT; FST plus conventional PT) beyond physiotherapist time and inpatient rehabilitation costs.
The additional physiotherapist time associated with the interventions is physiotherapist— not physiotherapy assistant—time.
No downstream costs are associated with the interventions.
The disease model will stop at age 100, at which time most people in the cohort will have died.
The utility improvements observed at 6–weeks follow-up will be maintained for up to 2 years.
For the remainder of the model (i.e., after the up-to-2–year duration of effect) there will be no differences in utility scores between interventions and comparator.
The improvement in inpatient rehabilitation length of stay is the same for both of the increased-therapy interventions (higher-intensity PT; FST plus conventional PT).
Base Case Analysis
To calculate the mean change in total costs and QALYs of higher-intensity PT and of FST plus conventional PT, compared with conventional PT, we ran 10,000 simulations of the Markov model. This allows the results to be presented as a mean, with standard deviation.
Sensitivity Analyses
To explore the uncertainty surrounding the base case analysis (as outlined in the Key Assumptions list, above), we conducted several one-way sensitivity analyses. Each of these showed the effect that changing a single model input would have on the overall outcome. We also conducted a probabilistic sensitivity analysis to investigate the uncertainty of the point estimate of model inputs.
The variables modified for the one-way sensitivity analyses are summarized in Table 10.
Table 10:
Variables Modified for One-Way Sensitivity Analyses
| Variable | Base Case | Modified Value | Comment |
|---|---|---|---|
| Duration of effect | 2 years | 1 year | |
| Duration of effect | 2 years diminishing effect | 2 years sustained effect | Patients would receive 2 years of sustained effect with the 2 interventions and then experience no difference in effect, compared with conventional treatment. |
| Physiotherapist wage | $35.02 | $36.70 | The modified value is the median wage of physiotherapists in Windsor-Sarnia (23) |
| Involvement of physiotherapy assistant | 0 | 50% | Observe changes in results if 50% of additional physiotherapist time is provided by a physiotherapy assistant (median wage $17 per hour) |
| First-year mortality rate | Ontario Stroke Evaluation Report | Statistics Canada Life Tables and published standardized mortality ratios | Observe changes in results if mortality rate in first year is calculated by multiplying the mortality rate reported in Statistics Canada Life Tables (21) with published standardized mortality ratios for stroke patients. (22) |
| Discount rate | 5% | 0% | Observe effect of not applying the CADTH-recommended discount. (15) |
| Discount rate | 5% | 3% | Observe effect of reducing the CADTH-recommended discount to 3%. (15) |
| Utility values | 6-week study follow-up results | 18-week study follow-up results | 0.64 for functional strength training plus conventional physiotherapy, 0.56 for higher-intensity physiotherapy, 0.6 for conventional physiotherapy. |
| Inpatient rehabilitation length of stay | 14% reduction | No reduction |
Abbreviation: CADTH, Canadian Agency for Drugs and Technologies in Health.
For the probabilistic sensitivity analysis, we incorporated the uncertainty of the model inputs, as reported through the confidence intervals or standard deviations of the mean results, into the Markov model. From this information, a distribution could be constructed for each of the inputs where there was uncertainty, allowing for repeated runs of the model. Given the wide levels of uncertainty, we conducted 10,000 simulations of the model. The distributions used for the model inputs are presented in Table 11.
Table 11:
Variables Modified for Probabilistic Sensitivity Analysis
| Model Input | Reported Result | Distribution |
|---|---|---|
| Utilities (baseline and follow-up) | Mean and standard deviation | Beta distribution |
| Standardized mortality ratios | Mean and confidence intervals | Normal distribution |
| Mortality rate of general population | Mean and confidence intervals | Normal distribution |
| Total hours of physiotherapy treatment | Mean and standard deviation | Beta distribution |
Results of Primary Economic Evaluation
Base Case Results
The result of 10,000 simulations of the Markov model was an average reduction in lifetime costs, both for higher-intensity PT and for FST plus conventional PT. The results are presented in Table 12. Note that the high standard deviations emphasize the significant level of uncertainty with the inputs.
Table 12:
Change in Costs for Higher-Intensity PT and for FST Plus Conventional PT, Compared With Conventional PT
| Intervention | Mean Change in Total Costs (standard deviation) |
|---|---|
| Higher-intensity physiotherapy | −$2,616.66 ($20,811.59) |
| Functional strength training + conventional physiotherapy | −$2,355.91 ($21,090.56) |
Abbreviations: FST, functional strength training; PT, physiotherapy.
An average increase in QALYs was observed for both interventions, compared with conventional PT, after 10,000 simulations of the Markov model. The results are presented in Table 13.
Table 13:
Difference in QALYs for Higher-Intensity PT and for FST Plus Conventional PT, Compared With Conventional PT
| Intervention | Mean Increase [decrease] in QALYs (standard deviation) |
|---|---|
| Higher-intensity physiotherapy | 0.05 (0.69) |
| Functional strength training + conventional physiotherapy | 0.12 (0.68) |
Abbreviations: FST, functional strength training; PT, physiotherapy; QALYs, quality-adjusted life-years.
As shown, a reduction in estimated lifetime costs and an increase in QALYs was seen for higher-intensity PT and for FST plus conventional PT. Therefore, these 2 interventions dominated conventional PT in the base case.
One-Way Sensitivity Analyses Results
The results for the one-way sensitivity analyses are presented in Tables 14 and 15.
Table 14:
Differences in Incremental Cost-Effectiveness Ratios for Higher-Intensity PT Compared With Conventional PT, Resulting From Changes to Model Inputs
| Variable | Base Case | Modified Value | Modified Incremental Cost-Effectiveness Ratio |
|---|---|---|---|
| Duration of effect | 2 years | 1 year | Dominates conventional PT |
| Duration of effect | 2 years diminishing effect | 2 years sustained effect | Dominates conventional PT |
| Physiotherapist wage Involvement of physiotherapy assistant | $35.02 0 | $36.70 50% | Dominates conventional PT Dominates conventional PT |
| First-year mortality rate | Ontario Stroke Evaluation Report | Statistics Canada Life Tables and published standardized mortality ratios | Dominates conventional PT |
| Discount rate | 5% | 0% | Dominates conventional PT |
| Discount rate | 5% | 3% | Dominates conventional PT |
| Utility values | 6–week study follow-up results | 18–week study follow-up results | Lower costs and lower overall QALYs |
| Inpatient rehabilitation length of stay | 14% reduction | No reduction | $13,772.66 per QALY |
Abbreviations: PT, physiotherapy; QALY, quality-adjusted life-year.
Table 15:
Differences in Incremental Cost-Effectiveness Ratios for FST Plus Conventional PT, Compared With Conventional PT, Resulting From Changes to Model Inputs
| Variable | Base Case | Modified Value | Modified Incremental Cost-Effectiveness Ratio |
|---|---|---|---|
| Duration of effect | 2 years | 1 year | Dominates conventional PT |
| Duration of effect | 2 years diminishing effect | 2 years sustained effect | Dominates conventional PT |
| Physiotherapist wage | $35.02 | $36.70 | Dominates conventional PT |
| Involvement of physiotherapy assistant | 0 | 50% | Dominates conventional PT |
| First-year mortality rate | Ontario Stroke Evaluation Report | Statistics Canada Life Tables and published standardized mortality ratios | Dominates conventional PT |
| Discount rate | 5% | 0% | Dominates conventional PT |
| Discount rate | 5% | 3% | Dominates conventional PT |
| Utility values | 6–week study follow-up results | 18–week study follow-up results | Dominates conventional PT |
| Inpatient rehabilitation length of stay | 14% reduction | No reduction | $8,528.04/QALY |
Abbreviations: PT, physiotherapy; QALY, quality-adjusted life-year.
Probabilistic Sensitivity Analysis Results
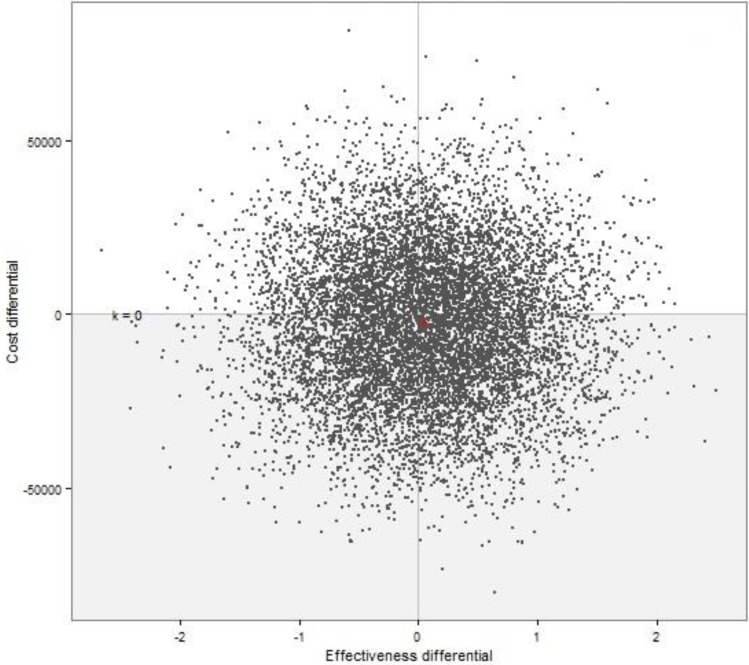
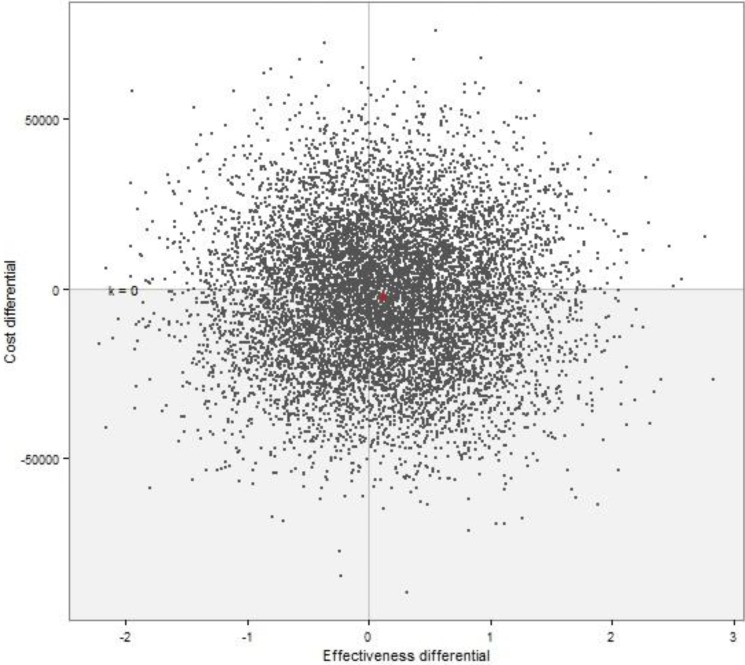
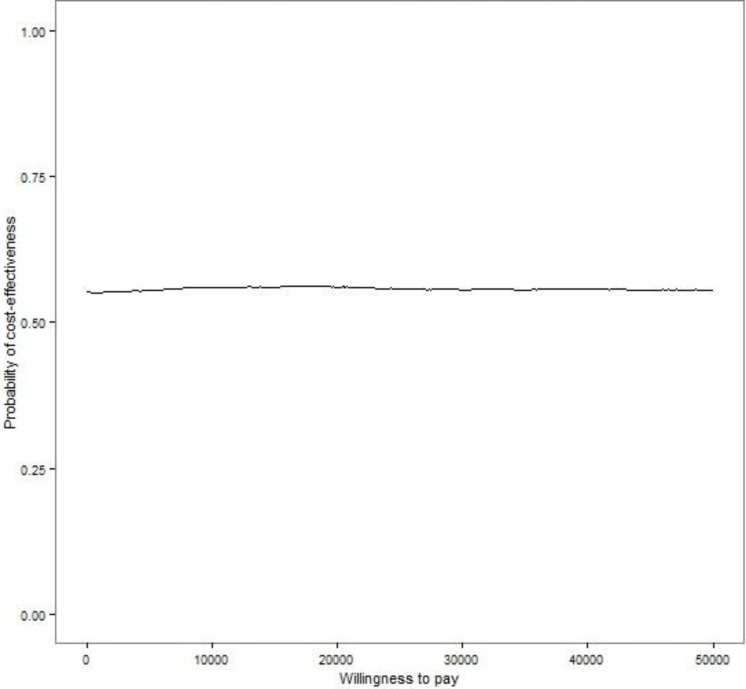
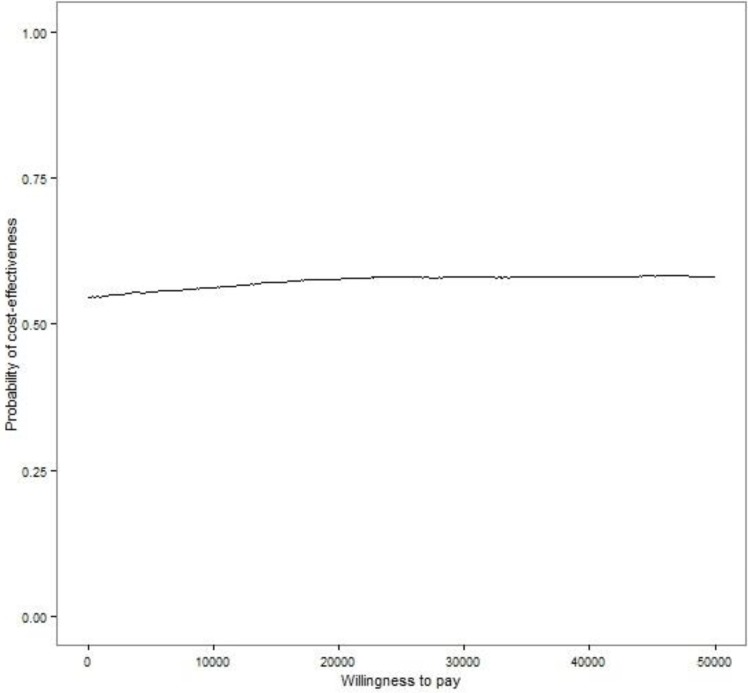
In running the total of 10,000 simulations of the Markov model, we used random draws of certain model parameters within the selected distributions. The result—a range of incremental cost-effectiveness ratios—is presented in a cost-effectiveness plane (see Figure 2 and Figure 3 for higher-intensity PT and FST plus conventional PT, respectively). For the cost-effectiveness acceptability curve for different levels of willingness to pay by the decision-makers, see Figure 4 for higher-intensity PT and Figure 5 for FST plus conventional PT.
Figure 2: Cost-Effectiveness Plane Showing Incremental Cost-Effectiveness Ratios for Higher-Intensity PT Versus Conventional PT.
Abbreviation: PT, physiotherapy.
Figure 3: Cost-Effectiveness Plane Showing Incremental Cost-Effectiveness Ratios for FST Plus Conventional PT, Versus Conventional PT.
Abbreviations: FST, functional strength training; PT, physiotherapy.
Figure 4: Cost-Effectiveness Plane Showing Cost-Effectiveness Acceptability Curve for Higher-Intensity PT Versus Conventional PT.
Abbreviation: PT, physiotherapy.
Figure 5: Cost-Effectiveness Plane Showing Cost-Effectiveness Acceptability Curve for FST Plus Conventional PT, Versus Conventional PT.
Abbreviations: FST, functional strength training; PT, physiotherapy.
Budget Impact Analysis
A budget impact analysis was conducted from the perspective of the Ontario Ministry of Health and Long-Term Care to determine the estimated cost burden of higher-intensity PT, and of FST in addition to PT, during inpatient rehabilitation for stroke patients. All costs are reported in 2014 Canadian dollars.
Research Methods
Incident Population
According to the Ontario Stroke Evaluation Report 2013, there were 3,351 inpatient rehabilitation admissions for stroke in fiscal year 2009/2010; 3,428 in 2010/2011; and 3,472 in 2011/2012. (20) For this analysis, we took the average of these 3 years (3,417) as the total incident population, i.e., the number of people who would receive higher-intensity PT or FST plus conventional PT.
Resources
The higher-intensity PT and the FST intervention would both result in additional physiotherapist time per stroke rehabilitation case. It is also assumed that no additional resources would be required for these interventions in Ontario, e.g., no additional rehabilitation facilities or training of additional physiotherapists to accommodate the increased workload. This analysis also assumes that no downstream costs are associated with implementing higher-intensity PT or FST plus conventional PT.
Canadian Costs
Assuming that the additional time required for both the higher-intensity PT and the FST intervention was identical to that observed in the RCT by Cooke and colleagues (14), and that the reduction in inpatient rehabilitation length of stay is realized and sustained, the costs per patient would be reduced by the figure that was shown in Base Case Results, Table 12: $2,616.66 +/− $20,811.59 for higher-intensity PT; $2,355.91 +/− 21,090.56 for FST plus conventional PT.
Results of Budget Impact Analysis
In Ontario, the total estimated cost savings each year would be almost $8.8 million +/− $71.2 million if higher-intensity PT was standard practice; $7.9 million +/− $71.8 million if FST plus conventional PT was standard practice.
Limitations
This economic analysis has several limitations. First, the primary clinical outcome that informs it comes from a single clinical trial conducted in the United Kingdom. The patient population in the RCT by Cooke and colleagues differs from the Ontario population in some important ways. First, the mean age of patients in the RCT's conventional PT and higher-intensity PT arms (66.37 years and 67.46 years, respectively) (14) was younger than the mean age of Ontario patients admitted to inpatient rehabilitation (71.6 years). (20) (Note that the mean age of patients in the RCT's FST arm—71.17 years—was more in line with Ontario patients.) Second, for all 3 arms of the RCT, the mean time since stroke was almost double the mean time in Ontario (more than 30 days, compared with 16.4 days). These differences may point to the possibility of better quality-of-life outcomes for Ontario patients, compared with those in the RCT. However, there is unfortunately no evidence to confirm this.
Also, Ontario stroke patients receive, on average, about 12 to 15 hours of PT during their inpatient rehabilitation—about 30 to 45 minutes about 5 days a week for an average stay of about 33 days. (20) This is a slightly higher intensity of PT than the baseline values in the RCT by Cooke and colleagues; and it is possible, though not certain, that this too may limit the RCT's generalizability to an Ontario population. Finally, another concern is that patients in different jurisdictions may respond differently to a PT intervention because of different concurrent health services and interventions.
As outlined in the EBA that accompanies this analysis, (13) there is also an issue with the RCT itself that may limit the external validity of its quality-of-life outcomes. This is a concern about risk of bias given that more participants were lost to follow-up in one arm than in the other 2. (There would be little risk of bias if the loss to follow-up was random.) The number of people lost to follow-up because they were unwell was similar in all arms, but the number who withdrew was much larger in the conventional PT arm (7 people, versus 1 in the higher-intensity PT and 2 in the FST arm).
Another limitation of our economic analysis is that several inputs into our model lacked clinical evidence. Specifically, we found no published studies observing additional cost impacts of higher-intensity PT beyond physiotherapist time, downstream cost impacts, and duration of PT effect. Thus, we relied on expert opinion to inform these model inputs, and this gave our results a level of uncertainty. We conducted several one-way sensitivity analyses to determine the robustness of the results if certain variables were changed to other plausible values. In almost all cases, there was no change in the dominance of the 2 interventions compared with conventional PT. The only exception was when the inpatient rehabilitation length-of-stay benefit was reduced to zero. Then, both higher-intensity PT and the FST intervention showed a higher cost than conventional PT. This suggested that the base-case result observed in this analysis is appropriate only if there is a reduction in inpatient rehabilitation length of stay.
An ad hoc analysis was conducted to further investigate length of stay. The dominance results appear to be sustained down to a half-a-day reduction in rehabilitation length of stay; any less than that results in a higher cost for the 2 interventions. Thus, it may be safe to say that either intervention—higher-intensity PT or FST plus conventional PT—results in cost savings if it reduces rehabilitation length of stay. This comes as no surprise, given that inpatient rehabilitation is the largest cost item in our analysis. The estimated reduction in length of stay was based on the consensus of a group of Ontario stroke experts, but, on its own, this constitutes a very low level of evidence. A large-cohort observational study or RCT to investigate this question would help reduce the uncertainty of this key input in our model.
Discussion
The 2 interventions dominated conventional PT in our base-case analysis because of the reduction in incremental cost, and also because a small incremental gain in QALY was observed in people receiving either intervention. This gain in QALY is a result of the higher improvement in utility values observed by Cooke and colleagues in their RCT. They saw a 0.06 improvement in utility values at follow-up for higher-intensity PT and a 0.13 improvement at follow-up for FST plus conventional PT, compared with conventional PT. We decreased this improvement over a short duration of effect. As a result, the total utility improvement and resulting QALY associated with higher-intensity PT and FST in our analysis is almost the same as in the RCT.
In most of the one-way sensitivity analyses that we conducted, the dominance of the 2 increased-intensity interventions remained. One exception was when we replaced the 6–week utility values observed in the RCT with the 18–week follow-up values. In this scenario, higher-intensity PT had lower costs, but also lower QALYs compared with conventional PT. The only other exception was when the inpatient rehabilitation length of stay was set to ‘no reduction.’ In this scenario we observed close to $14,000 per QALY for higher-intensity PT and $8,500 per QALY for FST plus conventional PT. These costs per QALY were observed because, once the benefit gained by reduced length of stay is removed, all that remains are the increased costs associated with increased hours of physiotherapist time. The high level of model uncertainty is easy to see in the probability sensitivity analysis when the standard deviation information is incorporated into the model and 10,000 simulations are plotted on a cost-effectiveness plane. The resulting scatter of incremental cost-effectiveness ratios is centred close to the origin of the effectiveness-differential x-axis, both for higher-intensity PT and for conventional treatment plus FST. In other words, the results of the sensitivity analyses suggest that higher-intensity PT and the FST intervention are just as likely as conventional PT to result in improved QALYs. This interpretation is strengthened by the results of the cost-effectiveness acceptability curves that show both higher-intensity PT and the FST intervention as having a 50% or lower probability of being cost-effective, compared with conventional treatment, at all levels of willingness to pay. Therefore, the base-case analysis shows that both higher-intensity PT and FST in addition to PT are cost-effective and this remains the case for most of the one-way sensitivity analyses we conducted. However, the probabilistic sensitivity analyses suggest that these results should be interpreted with caution, due to the high level of uncertainty in the clinical data.
The budget impact for the Ontario Ministry of Health and Long-term Care is estimated as nearly $9 million in annual cost savings if higher-intensity PT were implemented, or about $8 million in annual cost savings if FST plus conventional PT were implemented. We expect that these costs would remain stable, assuming that the incidence of stroke in Ontario did not change. This estimate does not include any potential implementation costs or any downstream effects. Most of the cost savings are a result of the reduced rehabilitation length of stay. This would be of further benefit if the freed-up beds allowed other patients to receive rehabilitation earlier, or gave appropriate patients a chance to receive rehabilitation when they otherwise would not. Unfortunately, this estimate of cost savings has a high level of uncertainty and should therefore be interpreted with caution.
The results of this cost-effectiveness analysis suggest that increasing the intensity of rehabilitation therapy for stroke patients, either through higher-intensity PT or through FST in addition to conventional PT, may result in cost savings and improvement in quality-adjusted life-years. However, as noted previously, these results have a high level of uncertainty and should be interpreted with caution.
Additional clinical studies that evaluate the impact of higher-intensity PT and FST on inpatient rehabilitation length of stay, changes in utility scores, long-term outcomes, and downstream costs—these would help reduce the uncertainty of the economic evaluation and provide a more definitive answer on the cost-effectiveness of increasing the intensity of PT.
CONCLUSIONS
Higher-intensity physiotherapy provided during inpatient rehabilitation after stroke appears to result in a reduction in costs and improvements in quality-adjusted life-years.
Functional strength training of the paretic lower limb in addition to the conventional physiotherapy provided during inpatient rehabilitation after stroke appears to result in a reduction in cost and improvements in quality-adjusted life-years.
These results of the economic evaluation appear to be driven by the potential reductions in inpatient rehabilitation length of stay.
There is a great level of uncertainty surrounding the cost-effectiveness analysis.
Many of the important model inputs were based on very low-level evidence.
Results of this economic evaluation must be interpreted with caution given the uncertainty and very low-level evidence of some model inputs.
ACKNOWLEDGEMENTS
Editorial Staff
Sue MacLeod, BA
Medical Information Services
Corinne Holubowich, BEd, MLIS
Kellee Kaulback, BA(H), MISt
Joanna Bielecki, BSc, MISt (THETA)
APPENDICES
Appendix 1: Literature Search Strategies
Table 1A:
MEDLINE search strategy and results. Database(s): Ovid MEDLINE(R) 1946 to October Week 5 2013, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations November 12, 2013
| # | Searches | Results | Description |
|---|---|---|---|
| 1 | exp Stroke/ or exp brain ischemia/ or exp intracranial hemorrhages/ or (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct∗ or brain infarct∗ or CVA or (brain adj2 isch?emia) or (cerebral adj2 isch?emia) or (intracranial | 263993 | Stroke Terms |
| 2 | exp Rehabilitation/ or exp Rehabilitation Nursing/ or exp Rehabilitation Centers/ or exp Stroke/rh or exp Physical Therapy Modalities/ or (rehabilitat∗ or habilitat∗ or movement therap∗ or physiotherap∗ or physical therap∗ or exercis∗ or occupational therap∗ or mobilization or mobilisation or strength train∗).ti,ab. | 551925 | Rehablitation Terms |
| 3 | exp Time/ or ((time∗ or interval∗ or intens∗ or duration or augment∗ or dose-response or dose or dosing or dosage or frequency or enhance∗ or amount∗ or quantit∗) adj4 (rehabilitat∗ or habilitat∗ or movement therap∗ or physiotherap∗ or physical therap∗ or exercis∗ or occupational therap∗ or mobilization or mobilisation or strength train∗)).ti,ab. | 1189948 | Time to Treatment Terms |
| 4 | economics/ or exp “costs and cost analysis”/ or economics, dental/ or exp “economics, hospital”/ or economics, medical/ or economics, nursing/ or economics, pharmaceutical/ or (economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. or (expenditure$ not energy).ti,ab. or (value adj1 money).ti,ab. or budget$.ti,ab. | 596596 | Econnomic Evalaluation Filter: NHS EED MEDLINE best sensitivity from Glanville and colleagues |
| 5 | (((energy or oxygen) adj cost) or (metabolic adj cost) or ((energy or oxygen) adj expenditure)).ti,ab. | 20767 | |
| 6 | 4 not 5 | 591881 | |
| 7 | (Letter or Editorial or Historical article).pt. or (Animals/ not humans/) | 5389991 | |
| 8 | 6 not 7 | 529759 | |
| 9 | 1 and 2 and 3 and 8 | 174 |
Data sources: Glanville et al (26)
Table 1B:
Embase search strategy and results. Database(s): Embase 1980 to 2013 Week 48
| # | Searches | Results | Description |
|---|---|---|---|
| 1 | exp cerebrovascular accident/ or exp brain ischemia/ or exp brain hemorrhage/ or exp stroke patient/ or (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct$ or brain infarct$ or CVA or (brain adj2 isch?emia) or (cerebral adj2 isch?emia) or (intracranial adj2 hemorrhag$) or (brain adj2 hemorrhag$)).ti,ab. | 344847 | Stroke Terms |
| 2 | exp Rehabilitation/ or exp Rehabilitation Nursing/ or exp rehabilitation center/ or exp rehabilitation medicine/ or exp rehabilitation research/ or exp rehabilitation care/ or exp Stroke/rh or exp physical medicine/ or exp mobilization/ or (rehabilitat$ or habilitat$ or movement therap$ or physiotherap$ or physical therap$ or exercis$ or occupational therap$ or mobilization or mobilisation or strength train$).ti,ab. | 923550 | Rehabilitation Terms |
| 3 | exp Time/ or exp dose response/ or exp treatment duration/ or exp exercise intensity/ or ((time$ or interval$ or intens$ or duration or augment$ or dose-response or dose or dosing or dosage or frequency or enhance$ or amount$ or quantit$) adj4 (rehabilitat$ or habilitat$ or movement therap$ or physiotherap$ or physical therap$ or exercis$ or occupational therap$ or | 979352 | Time to Treatment Terms |
| 4 | ((Cost adj effectiveness).ab. or (Cost adj effectiveness).ti. or (Life adj years).ab. or (Life adj year).ab. or Qaly.ab. or ((Cost or costs).ab. and Controlled Study/) or (Cost and costs).ab.) and ((health economics/ or exp economic evaluation/ or exp health care cost/ or exp pharmacoeconomics/ or (econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. or (expenditure$ not energy).ti,ab. or (value adj2 money).ti,ab. or budget$.ti,ab.) not ((metabolic adj cost) or ((energy or oxygen) adj cost) or ((energy or oxygen) adj expenditure)).ti,ab.) | 135424 | Economic Evaluation Filter: EMBASE G filter AND NHS EED filter; best optimization of sensitivity and precision from Glanville and |
| 5 | 1 and 2 and 3 and 4 | 89 | |
| 6 | limit 5 to english language | 81 |
Data sources: Glanville et al (26)
Table 1C:
Cochrane database search strategy and results. Database(s): Cochrane Library databases, December, 2013: Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register, Database of Abstracts of Reviews of Effects, Health Technology Assessment, NHS Economic Evaluation Database
| ID | Search | Hits | Description |
|---|---|---|---|
| #1 | MeSH descriptor: [Stroke] explode all trees | 4580 | Stroke Terms |
| #2 | MeSH descriptor: [Brain Ischemia] explode all trees | 2076 | |
| #3 | MeSH descriptor: [Intracranial Hemorrhages] explode all trees | 1209 | |
| #4 | stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct∗ or brain infarct∗ or CVA or (brain adj2 isch?emia) or (cerebral adj2 isch?emia) or (intracranial adj2 hemorrhag∗) or (brain adj2 hemorrhag∗):ti,ab,kw (Word variations have been searched) | 20421 | |
| #5 | #1 or #2 or #3 or #4 | 21681 | |
| #6 | MeSH descriptor: [Rehabilitation] explode all trees | 13131 | Rehabilitation Terms |
| #7 | MeSH descriptor: [Rehabilitation Nursing] explode all trees | 37 | |
| #8 | MeSH descriptor: [Rehabilitation Centers] explode all trees | 538 | |
| #9 | MeSH descriptor: [Physical Therapy Modalities] explode all trees | 13680 | |
| #10 | MeSH descriptor: [Stroke] explode all trees and with qualifiers: [Rehabilitation – RH] | 1072 | |
| #11 | rehabilitat∗ or habilitat∗ or movement therap∗ or physiotherap∗ or physical therap∗ or exercis∗ or occupational therap∗ or mobilization or mobilisation or strength train∗:ti,ab,kw (Word variations have been searched) | 53776 | |
| #12 | #6 or #7 or #8 or #8 or #9 or #10 or #11 | 63029 | |
| #13 | MeSH descriptor: [Time] explode all trees | 50534 | Time to Treatment Terms |
| #14 | (time∗ or interval∗ or intens∗ or duration or augment∗ or dose-response or dose or dosing or dosage or frequency or enhance∗ or amount∗ or quantit∗) adj4 (rehabilitat∗ or habilitat∗ or movement therap∗ or physiotherap∗ or physical therap∗ or exercis∗ or occupational therap∗ or mobilization or mobilisation or strength train∗):ti,ab,kw (Word variations have been searched) | 0 | |
| #15 | #13 or #14 | 50534 | |
| #16 | MeSH descriptor: [Economics] this term only | 53 | Economic Evaluation Filter: EMBASE G filter AND NHS EED filter; best optimization of sensitivity and precision from Glanville and colleagues |
| #17 | MeSH descriptor: [Costs and Cost Analysis] explode all trees | 20621 | |
| #18 | MeSH descriptor: [Economics, Dental] this term only | 3 | |
| #19 | MeSH descriptor: [Economics, Hospital] explode all trees | 1501 | |
| #20 | MeSH descriptor: [Economics, Medical] this term only | 36 | |
| #21 | MeSH descriptor: [Economics, Nursing] this term only | 15 | |
| #22 | MeSH descriptor: [Economics, Pharmaceutical] this term only | 225 | |
| #23 | (economic∗ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic∗) or (expenditure∗ not energy) or (value near/1 money) or budget∗:ti,ab,kw (Word variations have been searched) | 38910 | |
| #24 | #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 | 38988 | |
| #25 | ((energy or oxygen) near cost) or (metabolic near cost) or ((energy or oxygen) near expenditure):ti,ab,kw (Word variations have been searched) | 1976 | |
| #26 | #24 not #25 | 38539 | |
| #27 | letter or editorial or historical article:pt (Word variations have been searched) | 5894 | |
| #28 | #26 not #27 | 38459 | |
| #29 | MeSH descriptor: [Animals] explode all trees | 6334 | |
| #30 | MeSH descriptor: [Humans] explode all trees | 1080 | |
| #31 | #29 not (#29 and #30) | 5254 | |
| #32 | #28 not #31 | 38300 | |
| #33 | #5 and #12 and #15 and #32 | 18 |
Data sources: Glanville et al (26)
Table 1D:
CINAHL database search strategy and results. Database: Cumulative Index to Nursing and Allied Health database December, 2013
| # | Query | Results | Terms |
|---|---|---|---|
| S20 | S15 not S18 | 62 | Limiters |
| S19 | S15 not S18 | 66 | |
| S18 | S16 not (S16 and S17) | 23,369 | |
| S17 | (MH “Human”) | 800,575 | |
| S16 | (MH “Animals”) | 25,171 | |
| S15 | S13 not S14 | 66 | |
| S14 | PT Letter or Editorial or Historical article | 151,973 | |
| S13 | S3 AND S6 AND S9 AND S12 | 67 | |
| S12 | S10 OR S11 | 109,571 | Economic evaluations terms |
| S11 | (MH “Economics”) OR (MH “Economics, Dental”) OR (MH “Economics, Pharmaceutical”) OR (MH “Costs and Cost Analysis”) OR (MH “Health Care Costs”) OR (MH “Nursing Costs”) OR (MH “Health Facility Costs”) | 36,766 | |
| S10 | TI ((economic∗ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic∗) or (expenditure∗ NOT energy) or (value N1 money) or budget∗) OR AB ((economic∗ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic∗) or (expenditure∗ not energy) or (value N1 money) or budget∗) | 89,687 | |
| S9 | S7 OR S8 | 85,901 | Timing & intensity terms |
| S8 | (time∗ or interval∗ or intens∗ or duration or augment∗ or dose-response or dose or dosing or dosage or frequency or enhance∗ or amount∗ or quantit∗) N4 (rehabilitat∗ or habilitat∗ or movement therap∗ or physiotherap∗ or physical therap∗ or exercis∗ or occupational therap∗ or mobilization or mobilisation or strength train∗) | 14,359 | |
| S7 | (MH “Time+”) OR (MH “Treatment Duration”) | 73,182 | |
| S6 | S4 OR S5 | 255,469 | Rehabilitation terms |
| S5 | (rehabilitat∗ or habilitat∗ or movement therap∗ or physiotherap∗ or physical therap∗ or exercis∗ or occupational therap∗ or mobilization or mobilisation or strength train∗) | 209,977 | |
| S4 | (MH “Rehabilitation+”) OR (MH “Rehabilitation Centers+”) OR (MH “Rehabilitation Nursing”) OR (MH “Stroke+/RH”) OR (MH “Physical Medicine”) | 146,796 | |
| S3 | S1 OR S2 | 51,264 | Stroke terms |
| S2 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct∗ or brain infarct∗ or CVA or (brain N2 isch?emia) or (cerebral N2 isch?emia) or (intracranial N2 hemorrhag∗) or (brain N2 hemorrhag∗)) | 46,112 | |
| S1 | (MH “Stroke”) OR (MH “Cerebral Ischemia+”) OR (MH “Intracranial Hemorrhage+”) OR (MH “Intracranial Hemorrhage+”) OR (MH “Stroke Patients”) | 38,734 |
Appendix 2: Literature Search Results
A total of 7 articles were selected for complete review. The list of these articles and the reasons for exclusion are presented in Table 2A.
Table 2A:
Articles Selected for Full Review and Reasons for Exclusion
| Author, Year | Reason for Exclusion |
|---|---|
| Annemans et al, 2007 (6) | Not related to PT intensity |
| Bjorkdahl et al, 2006 (7) | Not an economic evaluation |
| French et al, 2008 (8) | Not related to PT intensity |
| Hillier et al, 2011 (9) | Study protocol |
| von Koch et al, 2001 (10) | Not related to PT intensity |
| Rodgers et al, 2003 (11) | Not related to PT intensity |
| van de Port et al, 2009 (12) | Study protocol |
REFERENCES
- (1).Heart and Stroke Foundation. What is a stroke? [Internet]. Ottawa, ON: Heart and Stroke Foundation; 2012. [updated 2014 July]. Available from: http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3483935/k.736A/Stroke__What_is_Stroke.htm [Google Scholar]
- (2).Hall R, Khan F, O'Callaghan C, Kapral MK, Hodwitz K, Fang J, et al. Ontario Stroke Evaluation Report 2012: Prescribing System Solutions to Improve Stroke Outcomes [Internet]. Toronto, ON: Institute for Clinical Evaluative Sciences; 2012. Available from: http://www.ices.on.ca/webpage.cfm?site_id=1&org_id=68&morg_id=0&gsec_id=0&item_id=7543&type=report
- (3).Public Health Agency of Canada. Tracking Heart Disease and Stroke in Canada – Stroke Highlights 2011 [Internet]. Ottawa, ON: Public Health Agency of Canada; 2011. Available from: http://www.phac-aspc.gc.ca/cd-mc/cvd-mcv/sh-fs-2011/index-eng.php [Google Scholar]
- (4).Van Peppen RP, Kwakkel G, Wood-Dauphinee S, Hendriks HJ, Van der Wees PJ, Dekker J. The impact of physical therapy on functional outcomes after stroke: what's the evidence? Clin Rehabil. 2004; 18(8): 833–62. [DOI] [PubMed] [Google Scholar]
- (5).Kwakkel G, Kollen B, Twisk J. Impact of time on improvement of outcome after stroke. Stroke. 2006; 37(9): 2348–53. [DOI] [PubMed] [Google Scholar]
- (6).Annemans L, Lamotte M, Clarys P, Van den Abeele E. Health economic evaluation of controlled and maintained physical exercise in the prevention of cardiovascular and other prosperity diseases. Eur J Cardiovasc Prev Rehabil. 2007; 14(6): 815–24. [DOI] [PubMed] [Google Scholar]
- (7).Bjorkdahl A, Nilsson AL, Grimby G, Sunnerhagen KS. Does a short period of rehabilitation in the home setting facilitate functioning after stroke? A randomized controlled trial. Clin Rehabil. 2006; 20(12): 1038–49. [DOI] [PubMed] [Google Scholar]
- (8).French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al. A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness. Health Technol Assess. 2008; 12(30):iii, ix-x, 1–117. [DOI] [PubMed] [Google Scholar]
- (9).Hillier S, English C, Crotty M, Segal L, Bernhardt J, Esterman A. Circuit class or seven-day therapy for increasing intensity of rehabilitation after stroke: protocol of the CIRCIT trial. Int J Stroke. 2011; 6(6): 560–5. [DOI] [PubMed] [Google Scholar]
- (10).von Koch L, de Pedro-Cuesta J, Kostulas V, Almazan J, Widen HL. Randomized controlled trial of rehabilitation at home after stroke: one-year follow-up of patient outcome, resource use and cost. Cerebrovasc Dis. 2001; 12(2): 131–8. [DOI] [PubMed] [Google Scholar]
- (11).Rodgers H, Mackintosh J, Price C, Wood R, McNamee P, Fearon T, et al. Does an early increased-intensity interdisciplinary upper limb therapy programme following acute stroke improve outcome? Clin Rehabil. 2003; 17(6): 579–89. [DOI] [PubMed] [Google Scholar]
- (12).van de Port IG, Wevers L, Roelse H, van Kats L, Lindeman E, Kwakkel G. Cost-effectiveness of a structured progressive task-oriented circuit class training programme to enhance walking competency after stroke: the protocol of the FIT-Stroke trial. BMC Neurol. 2009; 9: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Sehatzadeh S. Effect of Increased Intensity of Physical Therapy on Patient Outcomes After Stroke: An Evidence-Based Analysis (in press). Toronto: [PMC free article] [PubMed] [Google Scholar]
- (14).Cooke EV, Tallis RC, Clark A, Pomeroy VM. Efficacy of functional strength training on restoration of lower-limb motor function early after stroke: phase I randomized controlled trial. Neurorehabil Neural Repair. 2010; 24(1): 88–96. [DOI] [PubMed] [Google Scholar]
- (15).Canadian Agency for Drugs and Technologies in Health. Guidelines for the Economic Evaluation of Health Technologies: Canada. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 46 p. [Google Scholar]
- (16).Kapral MK, Hall R, Stamplecoski M, Meyer S, Asllani E, Fang J, et al. Registry of the Canadian Stroke Network – Report on the 2008/09 Ontario Stroke Audit. Toronto, ON: Institute for Clinical Evaluative Sciences; 72 p. [Google Scholar]
- (17).Canadian Stroke Network. The Quality of Stroke Care in Canada 2011 [Internet]. Ottawa, ON: Canadian Stroke Network; 2011. [updated 2011]. Available from: http://www.canadianstrokenetwork.ca/index.php5/news/the-quality-of-stroke-care-in-canada-2011/ [Google Scholar]
- (18).Harris JE, Eng JJ, Miller WC, Dawson AS. A self-administered Graded Repetitive Arm Supplementary Program (GRASP) improves arm function during inpatient stroke rehabilitation: a multi-site randomized controlled trial. Stroke. 2009; 40(6): 2123–8. [DOI] [PubMed] [Google Scholar]
- (19).Glasgow Augmented Physiotherapy Study (GAPS) group. Can augmented physiotherapy input enhance recovery of mobility after stroke? A randomized controlled trial. Clin Rehabil. 2004;18 (5): 529–37. [DOI] [PubMed] [Google Scholar]
- (20).Hall R, Khan F, O'Callaghan C, Kapral MK, Hodwitz K, Kapila S, et al. Ontario Stroke Evaluation Report 2013: Spotlight on Secondary Stroke Prevention and Care. [Internet]. Toronto, ON: Institute for Clinical Evaluative Sciences; 2013. Available from: http://www.ices.on.ca/webpage.cfm?site_id=1&org_id=68&morg_id=0&gsec_id=0&item_id=7543&type=report
- (21).Statistics Canada. Life Tables, Canada, Provinces and Territories, 2009 to 2011 [Internet]. Ottawa, ON: Statistics Canada; 2013. Available from: http://www.statcan.gc.ca/pub/84-537-x/84-537-x2013005-eng.htm [Google Scholar]
- (22).Bronnum-Hansen H, Davidsen M, Thorvaldsen P. Long-term survival and causes of death after stroke. Stroke. 2001; 32(9): 2131–6. [DOI] [PubMed] [Google Scholar]
- (23).Workplace Partnerships Directorate: Government of Canada. Explore Careers – Wage Report [Internet]. Ottawa, ON: Workplace Partnerships Directorate; 2013. Available from: http://www.workingincanada.gc.ca/LMI_report_bynoc.do?&noc=3142&reportOption=wage [Google Scholar]
- (24).Meyer M, O'Callaghan C, Kelloway L, Hall R, Teasell R, Meyer S, et al. The Impact of Moving to Stroke Rehabilitation Best Practices in Ontario. Ontario: Ontario Stroke Network; 66 p. [Google Scholar]
- (25).Statistics Canada. Consumer Price Index, health and personal care, by province [Internet]. Ottawa, ON: Statistics Canada; 2014. Available from: http://data.gc.ca/data/en/dataset/07e78ed3-1c15-4e44-89e0-e11a9930bcfd# [Google Scholar]
- (26).Glanville J, Fleetwood K, Yellowlees A, Kaunelis D, Mensinkai S. Development and Testing of Search Filters to Identify Economic Evaluations in MEDLINE and EMBASE. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 90 p. [Google Scholar]