Abstract
Background
Pulmonary rehabilitation (PR) is a comprehensive intervention of exercise training, education, and behaviour change to improve the physical and psychological condition of people with chronic respiratory disorders, such as chronic obstructive pulmonary disease (COPD) and to promote long-term adherence to health-enhancing behaviours. Although PR is considered the standard of care for patients with COPD who remain symptomatic despite bronchodilator therapies, current evidence suggests that only 1.15% of COPD patients across Canada have access to PR facilities for care.
Objectives
The objectives of this study were to identify the number of health care facilities across Ontario providing PR services for patients with COPD, describe the scope of those services, and determine the province's current capacity to provide PR services relative to need, for the province as a whole and by local health integration network (LHIN).
Methods
The Pulmonary Rehabilitation Programs in Ontario (PRO) Survey was a province-wide, descriptive, cross-sectional survey of health care facilities (hospitals, family health teams, and community health centres). It was distributed to 409 facilities to collect information on various aspects of PR services in the province.
Results
Between April 2013 and February 2014, 187 facilities responded to the survey (46% response rate). Most responding centres (144) did not offer PR services, and only 43 were full PR sites providing a comprehensive program. Hospital-based programs made up the majority of sites offering full PR services (67%), followed by programs based at family health teams (19%) and community health centres (14%). More than 90% of PR programs are outpatient-based. The average wait time for outpatient PR was 6.9 weeks, and 58% of programs provide services 5 days per week. More than 80% of patients attending PR complete the full program. Across all program types, the total estimated provincial capacity for PR outpatient care is 4,524 patients per year, or 0.66% to 1.78% of patients with COPD, depending on the estimated prevalence of disease.
Limitations
These results are representative of 12 of the 14 LHINs in Ontario due to low response rates in facilities in 2 LHINs.
Conclusions
Although some increase in capacity has occurred since a similar survey in 2005, PR resources in Ontario are insufficient to support the delivery of care to people with COPD in accordance with clinical practice guideline recommendations.
PLAIN LANGUAGE SUMMARY
Pulmonary rehabilitation is a treatment program tailored for people with chronic lung disease who have difficulty breathing even though they take medication. It is recommended that everyone who needs this type of program have the opportunity to participate. The program provides exercise training and education about living with the disease. It helps people reduce flare-ups and have the best possible quality of life.
Health Quality Ontario commissioned a survey to identify and describe the pulmonary rehabilitation programs in Ontario. This report also describes the programs available in each of Ontario's local health integration networks (LHINs).
The survey shows that the province has relatively few program spaces compared to the number of people who could use them. A total of 43 health care facilities in the province provide pulmonary rehabilitation for approximately 4,500 people per year. More than 700,000 people in Ontario have chronic lung disease. The facilities currently available in this province can support only about 1% to 2% of the people who could potentially benefit from pulmonary rehabilitation.
Since 2005, when a similar national survey was conducted, pulmonary rehabilitation in Ontario has expanded to include more centres (43 vs. 21), more programs with maintenance or follow-up components (68% vs. 22%), more centres where staff are certified educators for this type of program (86% vs. 66%), and a shorter average wait time for outpatient programs (6.9 weeks vs. 11 weeks).
Most of Ontario's programs are located in hospitals, but they are generally for outpatients. These programs can be effectively run in community settings instead of hospitals. Moving these programs to community settings, such as community health centres and family health teams, might be one way for Ontario to make pulmonary rehabilitation available to more people. However, more research is needed to understand whether such a change would make a positive difference.
BACKGROUND
Study Objectives
This study had 3 objectives: to identify the number of health care facilities across Ontario providing pulmonary rehabilitation (PR) services for patients with chronic obstructive pulmonary disease (COPD); to describe the scope of those services; and to determine the province's capacity to provide PR services relative to need, for the province as a whole and for each local health integration network (LHIN).
Clinical Need and Target Population
Description of Condition
Chronic obstructive pulmonary disease is a group of respiratory disorders largely caused by smoking and characterized by persistent airway obstruction and difficulty breathing. (1) Emphysema and chronic bronchitis are among the common conditions that fall under COPD. (2) The disease is progressive, but treatment can help control symptoms and prevent further lung damage. (2) The condition affects patients' daily lives—their quality of life, general health, mental health, and mobility, and their ability to participate in employment, and recreational activities. (3) In addition, COPD exacerbations (flare-ups) cost the Canadian economy an estimated $646 million to $736 million (Cdn, 2006) per year. (4)
Results from the 2011 Canadian census revealed that 4% of Canadians age 35 years and older reported having chronic bronchitis, emphysema, or COPD diagnosed by a health care professional. (5) However, this estimated prevalence of COPD is likely an underestimate. In the 2009 to 2011 Canadian Health Measures Survey, 13% of Canadians over age 35 were measured by spirometry as having an airflow obstruction consistent with COPD, according to standards from the Global Initiative for Chronic Obstructive Lung Disease. (6) The Institute for Clinical Evaluative Sciences (ICES), using administrative data, estimated a lower prevalence of COPD in Ontario of 9.5% in 2007. (7) The 2–fold (5.5%) difference in prevalence estimates between the Statistics Canada and ICES data, which are based on self-report and medical records respectively, requires that both estimates be examined when estimating health care capacity for programs supporting individuals in Ontario with COPD.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive intervention of exercise training, education, and behaviour change to improve the physical and psychological condition of people with chronic respiratory disorders, such as COPD. (8) It has been described as any inpatient, outpatient, or home-based rehabilitation program of at least 4 weeks' duration that includes exercise therapy with or without any form of education and/or psychological support delivered to patients with exercise limitation attributable to COPD. (9) PR programs in Canada vary in duration, from 4 weeks to 20 weeks or more. (10) Some programs add a maintenance or follow-up component to monitor patients after the initial PR program. The duration of maintenance programs also varies and some programs may last up to 18 months. (11) People with either stable COPD or recent acute exacerbations can benefit from PR, which has been shown to improve exercise capacity and health-related quality of life. (12)
Current recommendations from the Canadian Thoracic Society state that the disease can be treated by education, smoking cessation, pharmacotherapy, and annual influenza vaccination to prevent acute exacerbations. (1) The recommendations also specify that “clinically stable patients who remain dyspneic [short of breath] and limited in their exercise capacity despite optimal pharmacotherapy should be referred for supervised pulmonary rehabilitation.” (1) In addition, the society's clinical practice guidelines state, “It is strongly recommended that patients with moderate, severe and very severe COPD participate in PR.” (11) While PR may not be effective in all cases, the program should not be considered a last resort. Rather, PR has been found to be most effective when used in conjunction with other treatment strategies. For example, self-management in the absence of exercise does not impact health-related quality of life or exercise capacity. (11)
Ontario Context
Although pulmonary rehabilitation is considered the standard of care for patients with COPD who remain symptomatic despite the use of bronchodilator therapies, (11) evidence indicates that PR is underutilized. A 2005 study estimated that approximately 1.2% of individuals with COPD in Canada had access to PR programs, based on the estimated prevalence of disease and program capacity. (10) Similarly, more recent data suggest that 1.15% of COPD patients are able to access PR across the nation. (13) A 2012 evidence review conducted by Health Quality Ontario explored PR as a component of care for COPD patients in the province. (12) That report found that PR within 1 month of hospital discharge is cost-effective at $18,000 per quality-adjusted life-year compared with usual care. In addition, “moderate quality evidence showed that pulmonary rehabilitation also led to a clinically and statistically significant improvement in functional exercise capacity compared with usual care.” (12) Based on this analysis, the Ontario Health Technology Advisory Committee (OHTAC) recommended the following regarding outpatient PR: 1) ongoing access to existing PR for the management of people with moderate to severe COPD in stable patients, and 2) use of PR within 1 month of hospital discharge, in patients following an acute exacerbation of COPD. (14)
Due to the low quality of evidence available on the cost-effectiveness of PR maintenance programs, OHTAC recommended that a field evaluation of PR programs be conducted to collect primary data in Ontario. (14) Prior to a field evaluation, it was necessary to accurately identify the existing programs in the province and describe their scope, which was the purpose of this study.
SURVEY DEVELOPMENT
Methods
Study Design
To locate examples of surveys intended to characterize pulmonary rehabilitation (PR) programs, we conducted a search of international literature published over the last 25 years. This search resulted in 16 relevant publications (10;15–29) of 15 reports of individual surveys and their updates. Surveys were administered in more than 20 countries; two-thirds of them were carried out in Canada and the United States. The majority of the surveys (11 of 15) were conducted on a national basis, (10;16–26) and response rates varied from 12.7% (20) to 100% (23) in the 13 of 16 studies that reported it.
Following the review of surveys from other jurisdictions, we developed a descriptive, cross-sectional survey based on a previous Canadian national survey of PR programs published by Brooks et al in 1999 (18) and 2007. (10) Additional information from the Canadian Thoracic Society and from the literature review was incorporated into the survey to satisfy the scope of the current project.
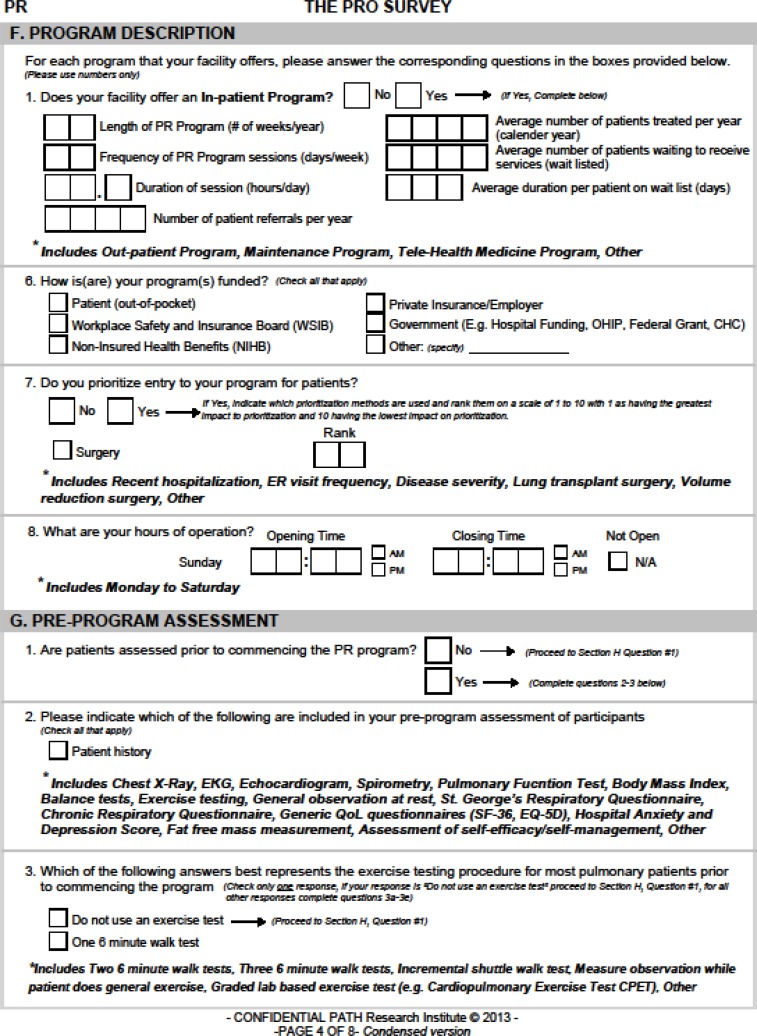
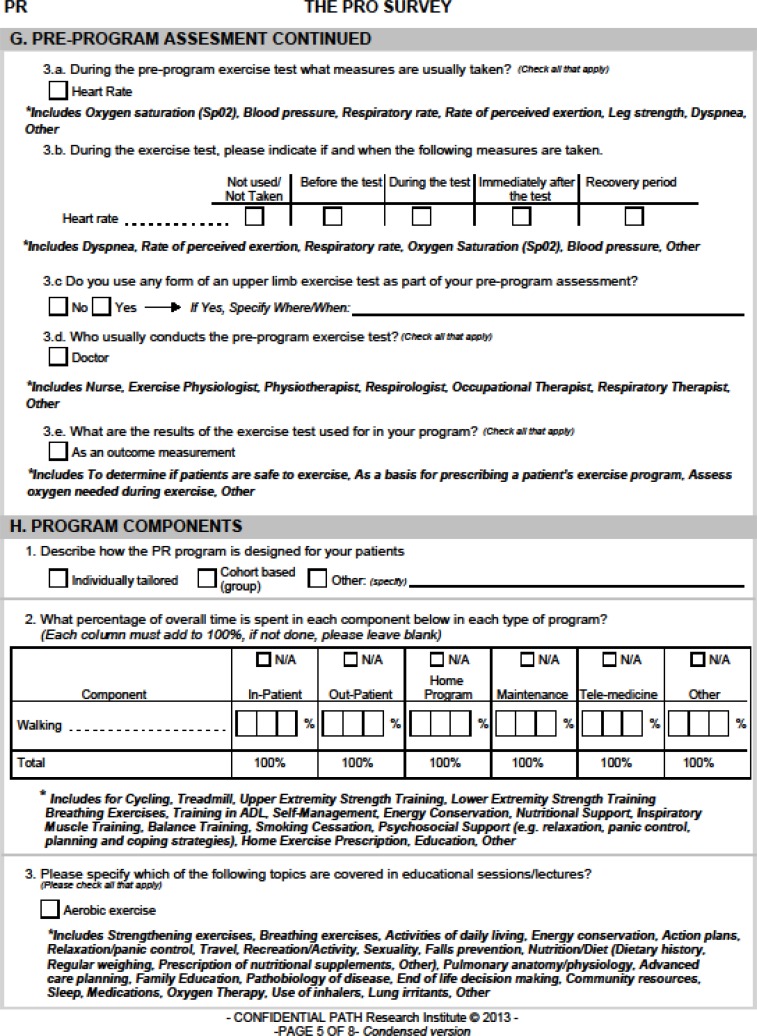
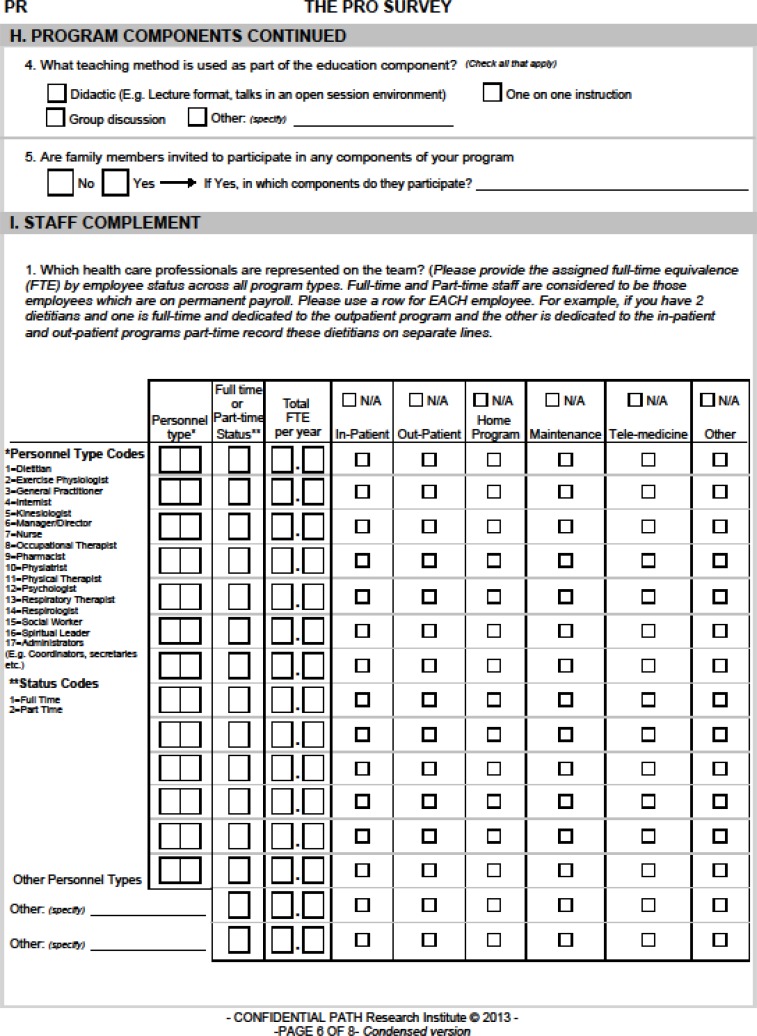
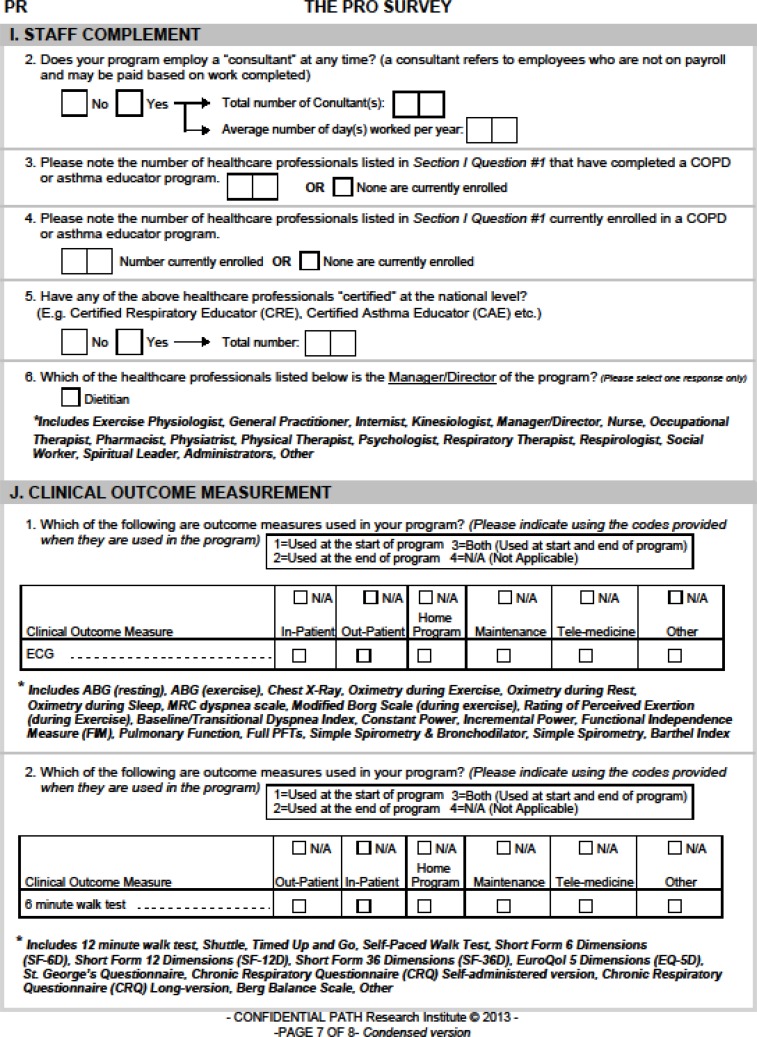
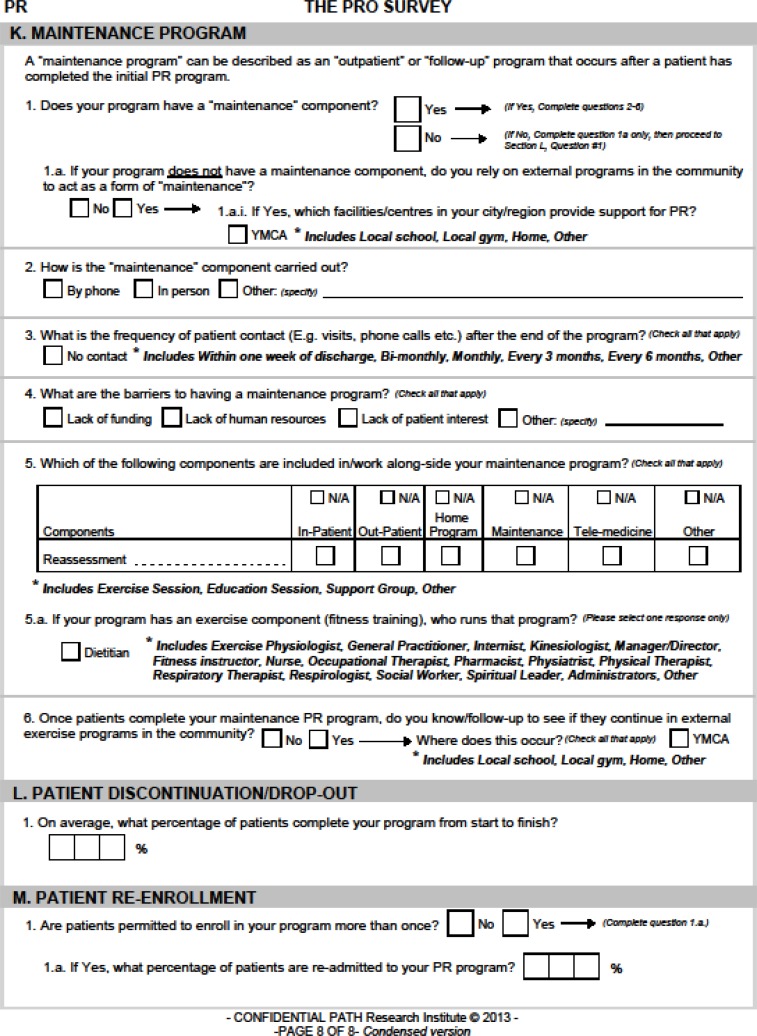
A study working group was created composed of physicians, respiratory health care practitioners, researchers, and a representative from an Ontario LHIN. These professionals reviewed the proposed survey to ensure that it included the pertinent factors to assess the capacity of PR programs in Ontario. This collaboration resulted in the Pulmonary Rehabilitation Programs in Ontario (PRO) Survey, which contains questions on the following aspects of full PR services in health care facilities or other sites: number of sites per LHIN; description of facilities; patient population; program description, components and capacity; pre-program patient assessment and clinical outcome measurements; staffing; specific maintenance activities; and follow-up. Table 1 defines full PR services, and Appendix A provides a condensed version of the survey.
Table 1:
Site Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Facility is a family health team, community health centre, or hospital. | Facility provides only long-term care. |
| Facility serves COPD patients. | Facility solely serves pediatric populations. |
| Facility offers a full PR program defined as an exercise training program for a minimum of 4 weeks, plus 1 or more of the following services: strength and breathing training, psychosocial/psychological support, self-management support, nutritional support, smoking cessation counselling, education, or other services. |
Abbreviations: COPD, chronic obstructive pulmonary disease; PR, pulmonary rehabilitation.
Site Consent
Sites interested in participating were asked to consent to the disclosure of information upon decision to enrol in the study. Each survey was assigned a unique identification number, which was used to track responses. The study protocol was approved by the Hamilton Integrated Research Ethics Board.
Site Recruitment
This was a province-wide survey of health care facilities in Ontario, including hospitals, family health teams (FHTs), and community health centres (CHCs). Using 2012 facility lists from the Ministry of Health and Long-Term Care, we identified 445 potential sites, along with 17 sites referred by survey respondents, for a total of 462 recommended sites (see Table 1 for detailed inclusion and exclusion criteria).
After removal of duplicate and irrelevant sites, the remaining 409 sites were categorized by LHIN and invited to participate in the study. Prior to distributing the surveys, either by mail or electronically (fax or email), we telephoned each institution to validate the list and identify the key contact(s) to ensure that the surveys would be sent directly to the people who would be able to supply PR program information.
Using a snowball approach, we continued recruitment beyond the minimum estimate described under “Sampling Size Calculation,” below. Sites that did not meet the inclusion criteria were invited to recommend other PR facilities in the province, and these sites were added to the target list, if not already present, and asked to participate.
Study Population
Each site was given 2 to 8 weeks to complete the survey. Sites without full PR services were asked to return only the first 3 pages of the survey. Their responses were used to calculate the proportions of facilities in the province providing full PR, other rehabilitation services or no rehabilitation services. Sites that met the criteria for a full PR centre (see Appendix A, part D, question 7) were instructed to continue and complete the remainder of the survey. Participating sites were given an honorarium (gift card) for taking time to complete the survey, and they were given the option of being notified of the final results.
Sites that did not respond by the end of Week 2 were reminded by postcard or email. If they had still not responded by the end of Week 4, we made several follow-up phone calls: first to verify or update the contact information for the site and then to request consent to participate from the new contacts. On consent, sites were then sent the survey electronically or by mail. Multiple follow-up attempts were made to contact sites that did not respond to phone messages. After 6 weeks, survey non-responders were sent a paper copy of the survey and a letter reminding them that they were still eligible to participate. Sites that did not respond within 2 weeks of the letter (end of Week 8) were deemed lost to follow-up. To estimate response rate from PR centres across Ontario, a full list of potential PR sites was compiled from the publicly available webpages of COPD Canada and the Canadian Lung Association, (30;31) and this list was used as a reference to identify all PR centres in the province. As of July 2012, 44 centres were identified as providing PR services.
We maintained a log to track responses by site and to identify sites that completed the full version of the survey. Survey distribution, recruitment of sites, and data collection began in April 2013 and ended in February 2014.
Sample Size Calculation
Based on previous research and COPD prevalence data, we determined the minimum number of sites in Ontario that should be recruited into the study to estimate the percentage of people with COPD receiving PR services in each LHIN. The Canadian Agency of Drugs in Technology and Health has estimated that only 1.15% of patients with COPD receive PR services in Canada. (13) As noted, we identified 445 institutions as possibly providing PR services in Ontario. Using the average number of COPD patients per province (13) and applying the average to each LHIN, (32) we determined that to achieve the targeted 95% confidence interval around the estimate of 1.15%, a minimum of 42 institutions should be targeted. This would represent services provided to an estimated 42,924 people (based on a calculated 1,022 patients per PR centre by LHIN), or a 9.4% sample of the Ontario COPD population. These calculations took non-response and post-hoc cluster effects into account. Table 2 provides the estimated minimum number of sites to produce representative survey results, by LHIN.
Table 2:
Sample Size Calculations, by LHIN
| LHIN Number | LHIN Name | Minimum Targeted Sites per LHIN, n |
|---|---|---|
| 1 | Erie St. Clair | 2 |
| 2 | South West | 4 |
| 3 | Waterloo Wellington | 2 |
| 4 | Hamilton Niagara Haldimand Brant | 4 |
| 5 | Central West | 1 |
| 6 | Mississauga Halton | 1 |
| 7 | Toronto Central | 5 |
| 8 | Central | 2 |
| 9 | Central East | 3 |
| 10 | South East | 3 |
| 11 | Champlain | 5 |
| 12 | North Simcoe Muskoka | 1 |
| 13 | North East | 5 |
| 14 | North West | 3 |
| Total | 42 |
Abbreviations: LHIN, local health integration network.
Data Collection
Sites were required to record their responses on either a paper or Adobe PDF survey form and return them by fax or email to the study coordination centre (Programs for Assessment of Technology in Health [PATH] Research Institute, St. Joseph's Healthcare Hamilton). Sites also had the opportunity to complete portions of the survey over the phone if they needed the assistance of a study coordinator.
LHIN Summaries
Responses from the PR centres were assembled into their respective LHINs and analyzed for program components. The capacity of each LHIN to provide PR services to patients with COPD was determined as a range, from “worst-case scenario” to “best-case scenario.” For the higher estimate of capacity, the total number of patients treated per year by all PR programs within a LHIN was divided by the Statistics Canada estimate of the population with COPD in that LHIN. This was used as our best-case scenario because the census is self-reported and therefore the prevalence is more likely to be lower than actual. For the lower estimate of capacity (worst case), we used COPD prevalence data for each LHIN reported by the ICES; (33) those prevalence estimates are based on administrative data and are higher than those reported by Statistics Canada. A provincial weighted average capacity was calculated for each scenario, to account for differences in PR services across the LHINs. The LHIN summaries (Appendix B) highlight survey results on key program elements that may play a role in local capacity.
RESULTS
Response Rates
A total of 187 responses were received from April 14, 2013, to February 5, 2014 (overall response rate, 46%). Of these, 43 centres reported offering full PR services and 144 reported offering other or no rehabilitation services for patients with COPD. Table 3 shows the survey response numbers and rates by LHIN. Response rates were highest from the South West LHIN (69%) and lowest from the Toronto Central LHIN (26%).
Table 3:
Survey Response Numbers and Rates, by LHIN
| LHIN Number | LHIN Name | Total Sites Contacted, n | Total Sites Responding, n (%) | Full Pulmonary Rehabilitation Sites, n |
|---|---|---|---|---|
| 1 | Erie St. Clair | 18 | 12 (67) | 4 |
| 2 | South West | 39 | 27 (69) | 4 |
| 3 | Waterloo Wellington | 22 | 12 (55) | 4 |
| 4 | Hamilton Niagara Haldimand Brant | 34 | 21 (62) | 4 |
| 5 | Central West | 11 | 6 (55) | 2 |
| 6 | Mississauga Halton | 14 | 8 (57) | 4 |
| 7 | Toronto Central | 39 | 10 (26) | 2 |
| 8 | Central | 18 | 5 (28) | 2 |
| 9 | Central East | 26 | 8 (31) | 2 |
| 10 | South East | 27 | 13 (48) | 1 |
| 11 | Champlain | 54 | 22 (41) | 6 |
| 12 | North Simcoe Muskoka | 13 | 6 (46) | 3 |
| 13 | North East | 61 | 22 (36) | 4 |
| 14 | North West | 33 | 15 (46) | 1 |
| Totals | 409 | 187(46) | 43 |
Abbreviations: LHIN, local health integration network.
Pulmonary Rehabilitation Programs in Ontario
Description of Facilities
Table 4 characterizes the survey responses by size and type of facility. About one-third of all respondents (35%) identified themselves as working in a centre serving between 10,000 and 50,000 people, and family health teams were the most common type of facility among survey respondents (41%). However, among the 43 full PR sites responding, the majority were hospital-based (67%) and were more likely to be located in major or regional centres serving populations of 100,000 or more (63%).
Table 4:
Total Survey Responses and Full Pulmonary Rehabilitation Sites, by Facility Size and Type
| Facility | Total Sites Responding, n (%) | Full Pulmonary Rehabilitation Sites, n (%) |
|---|---|---|
| Facility Size | ||
| Major centre serving > 200,000 people | 32 (17.11) | 16 (37.21) |
| Regional centre serving 100,000–200,000 people | 24 (12.83) | 11 (25.58) |
| Centre serving 50,000–100,000 people | 21 (11.23) | 5 (11.63) |
| Centre serving 10,000–50,000 people | 65 (34.76) | 7 (16.28) |
| Centre serving < 10,000 people | 36 (19.25) | 3 (6.98) |
| None of the above | 5 (2.67) | 0 (0) |
| No response | 4 (2.14) | 1 (2.33) |
| Totals | 187 (100) | 43 (100) |
| Facility Type | ||
| Hospital-based | 59 (31.55) | 29 (67.44) |
| Family health team | 77 (41.18) | 8 (18.61) |
| Community health centre | 33 (17.65) | 6 (13.95) |
| Other | 14 (7.49) | 0 (0) |
| No response | 4 (2.14) | 0 (0) |
| Totals | 187 (100) | 43 (100) |
Patient Referral, Entry, and Follow-Up
All 43 full PR sites reported on who refers patients to their program. Most sites receive referrals from respirologists (36 sites, 84%) and general practitioners (34 sites, 79%), and none from physiatrists.
About half of the sites said they prioritize patients for program entry (21 of 40 sites reporting, 53%). Important factors in prioritization include recent hospitalization (90%), frequency of emergency department visits (81%), and severity of disease (76%).
Most sites (78%) permit current smokers to participate in their program (40 sites reporting), and current smokers account for approximately 1 in 5 patients (22%) in those programs. Centres also reported that the majority of patients in outpatient (66%) and maintenance (70%) programs had a primary diagnosis of COPD at the time of referral.
Common potential barriers to patient participation (40 sites reporting) include weather, transportation, and the distance to the program (34 sites reported for each barrier, 85%). On average, 80% of patients complete the PR program from start to finish and, at centres that allow readmission and re-enrolment, just over 10% of patients are repeat clients (42 sites reporting).
PR Program Description, Components, and Capacity
The number of full PR programs, by program type and LHIN, is shown in Table 5. The vast majority of survey respondents reported offering programs on an outpatient basis (93%). One centre in the South West LHIN and 2 centres in the Mississauga Halton LHIN offer specific additional programming or referrals, such as referring patients to centres for aging or local gyms for external maintenance programs and COPD education.
Table 5:
Number of Full Pulmonary Rehabilitation Programs, by LHIN and Program Type
| LHIN Number | LHIN Name | Inpatient Programs, na | Outpatient Programs, nb | Maintenance Programs, nb | Telehealth Medicine Programs, nc | Total Programs per LHIN, n |
|---|---|---|---|---|---|---|
| 1 | Erie St. Clair | 0 | 4 | 4 | 1 | 9 |
| 2 | South West | 0 | 4 | 1 | 0 | 5 |
| 3 | Waterloo Wellington | 0 | 4 | 3 | 0 | 7 |
| 4 | Hamilton Niagara Haldimand Brant | 1 | 4 | 1 | 0 | 6 |
| 5 | Central West | 1 | 2 | 2 | 1 | 6 |
| 6 | Mississauga Halton | 1 | 4 | 1 | 1 | 7 |
| 7 | Toronto Central | 1 | 2 | 1 | 1 | 5 |
| 8 | Central | 0 | 1 | 2 | 1 | 4 |
| 9 | Central East | 0 | 2 | 2 | 0 | 4 |
| 10 | South East | 1 | 1 | 1 | 0 | 3 |
| 11 | Champlain | 0 | 4 | 2 | 0 | 6 |
| 12 | North Simcoe Muskoka | 0 | 3 | 2 | 0 | 5 |
| 13 | North East | 0 | 4 | 0 | 2 | 6 |
| 14 | North West | 0 | 1 | 1 | 0 | 2 |
| Totals (%) | 5 (12) | 40 (93) | 23 (54) | 7 (16) |
Abbreviations: LHIN, local health integration network.
42 out of 43 submitted surveys responded to this question.
41 out of 43 submitted surveys responded to this question.
34 out of 43 submitted surveys responded to this question.
Table 6 displays the total mean number of COPD patients treated in each type of full PR program annually, by LHIN. Outpatient PR programs serve the largest number of patients (3,280), and just under one-fifth of patients are being managed through maintenance programs (849). Program capacity varies across the province, with the North East LHIN reporting the largest overall volume (> 900 per year) and the lowest capacity in North Simcoe Muskoka.
Table 6:
Average Annual Number of Patients Treated per Full Pulmonary Rehabilitation Program, by LHIN and Program Type
| LHIN Number | LHIN Name | Inpatient Patients, na | Outpatient Patients, nb | Maintenance Patients, nc | Telehealth Medicine Patients, nd | Total Patients per LHIN, n |
|---|---|---|---|---|---|---|
| 1 | Erie St. Clair | NA | 175 | 85 | NR | 260 |
| 2 | South West | NA | 115 | NR | NA | 115 |
| 3 | Waterloo Wellington | NA | 314 | 150 | NA | 464 |
| 4 | Hamilton Niagara Haldimand Brant | 100 | 290 | 27 | NA | 417 |
| 5 | Central West | NR | 80 | 28 | NR | 108 |
| 6 | Mississauga Halton | NR | 295 | 30 | NR | 325 |
| 7 | Toronto Central | 165 | 280 | 80 | UNK | 525 |
| 8 | Central | NA | 160 | 200 | NR | 360 |
| 9 | Central East | NA | 170 | 95 | NA | 265 |
| 10 | South East | 25 | 70 | 30 | NA | 125 |
| 11 | Champlain | NA | 370 | 64 | NA | 434 |
| 12 | North Simcoe Muskoka | NA | 94 | NA | NA | 94 |
| 13 | North East | NA | 807 | 0 | 105 | 912 |
| 14 | North West | NA | 60 | 60 | NA | 120 |
| Totals (%) | 290 (6) | 3,280 (73) | 849 (19) | 105 (2) | 4,524 (100) |
Abbreviations: LHIN, local health integration network; NA, not applicable; NR, not reported; UNK, unknown.
3 out of 6 relevant surveys responded to this question.
32 out of 39 relevant surveys responded to this question.
20 out of 23 relevant surveys responded to this question.
1 out of 7 relevant surveys responded to this question.
Tables 7 and 8 present the total estimated capacity of full PR programs by LHIN for our best-case scenario (using self-reported COPD prevalence data) and our worst-case scenario (using prevalence estimates from administrative data). Using self-reported COPD prevalence, the province's overall weighted mean capacity to deliver full PR programs is 1.78%. In comparison, based on the higher prevalence estimates from administrative data, the province-wide capacity to accommodate COPD patients in PR programs is 0.66%. Appendix B presents a more extensive analysis of the program characteristics that contribute to program capacity in each LHIN.
Table 7:
Capacity of Pulmonary Rehabilitation Programs, by LHIN, “Best-Case Scenario”
| LHIN Number | LHIN Name | 2011 Population (≥ 35 y), n (32) | 2011 Census COPD Estimate, n (%) (34)a | Total Patients Treated per LHIN, n | Total PR Capacity, % |
|---|---|---|---|---|---|
| 1 | Erie St. Clair | 368,596 | 21,378 (5.8) | 260 | 1.22 |
| 2 | South West | 545,899 | 27,294 (5.0) | 115 | 0.42 |
| 3 | Waterloo Wellington | 408,301 | 19,190 (4.7) | 464 | 2.42 |
| 4 | Hamilton Niagara Haldimand Brant | 817,103 | 43,306 (5.3) | 417 | 0.96 |
| 5 | Central West | 453,105 | 8,155 (1.8) | 108 | 1.32 |
| 6 | Mississauga Halton | 628,800 | 13,204 (2.1) | 325 | 2.46 |
| 7 | Toronto Central | 667,460 | 13,349 (2.0) | 525 | 3.93 |
| 8 | Central | 975,460 | 17,558 (1.8) | 360 | 2.05 |
| 9 | Central East | 894,346 | 36,668 (4.1) | 265 | 0.72 |
| 10 | South East | 297,796 | 17,569 (5.9) | 125 | 0.71 |
| 11 | Champlain | 712,103 | 26,347 (3.7) | 434 | 1.65 |
| 12 | North Simcoe Muskoka | 270,492 | 15,147 (5.6) | 94 | 0.62 |
| 13 | North East | 345,070 | 21,049 (6.1) | 912 | 4.33 |
| 14 | North West | 137,754 | 5,647 (4.1) | 120 | 2.13 |
| Ontario | 7,522,285 | 4,524 | 1.78 |
Abbreviations: COPD, chronic obstructive pulmonary disease; LHIN, local health integration network; y, years of age.
The health profile for each LHIN was selected from the online database and the LHIN-specific percentages of self-reported COPD were used to estimate the number of individuals with COPD in the LHIN.
Table 8:
Capacity of Pulmonary Rehabilitation Programs, by LHIN, “Worst-Case Scenario”
| LHIN Number | LHIN Name | 2011 Population (≥ 35 y), n (32) | 2011 ICES COPD Estimate, n (%) (33)a | Total Patients Treated per LHIN, n | Total PR Capacity, % |
|---|---|---|---|---|---|
| 1 | Erie St. Clair | 368,596 | 49,760 (13.5) | 260 | 0.52 |
| 2 | South West | 545,899 | 58,411 (10.7) | 115 | 0.20 |
| 3 | Waterloo Wellington | 408,301 | 33,072 (8.1) | 464 | 1.40 |
| 4 | Hamilton Niagara Haldimand Brant | 817,103 | 83,344 (10.2) | 417 | 0.50 |
| 5 | Central West | 453,105 | 33,529 (7.4) | 108 | 0.32 |
| 6 | Mississauga Halton | 628,800 | 45,902 (7.3) | 325 | 0.71 |
| 7 | Toronto Central | 667,460 | 61,406 (9.2) | 525 | 0.86 |
| 8 | Central | 975,460 | 75,110 (7.7) | 360 | 0.48 |
| 9 | Central East | 894,346 | 92,117 (10.3) | 265 | 0.29 |
| 10 | South East | 297,796 | 35,735 (12.0) | 125 | 0.35 |
| 11 | Champlain | 712,103 | 72,634 (10.2) | 434 | 0.60 |
| 12 | North Simcoe Muskoka | 270,492 | 30,836 (11.4) | 94 | 0.31 |
| 13 | North East | 345,070 | 46,239 (13.4) | 912 | 1.97 |
| 14 | North West | 137,754 | 16,805 (12.2) | 120 | 0.71 |
| Ontario | 7,522,285 | 4,524 | 0.66 |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; y, years of age.
The age- and sex-adjusted rate of COPD in each LHIN was used to calculate the estimated number of individuals with COPD in the LHIN.
The mean number of days that patients spend on a wait list for entry into each type of full PR program varied considerably across LHINs (Table 9). The South East and Champlain LHINs reported the highest number of wait days for outpatient PR programs (120 and 105 days, respectively).
Table 9:
Wait Times for Full Pulmonary Rehabilitation, by LHIN and Program Type
| LHIN Number | LHIN Name | Wait Time, Mean, Days | ||
|---|---|---|---|---|
| Inpatienta | Outpatientb | Maintenancec | ||
| 1 | Erie St. Clair | NA | 35 | 0 |
| 2 | South West | NA | 15 | NR |
| 3 | Waterloo Wellington | NA | 85 | 15 |
| 4 | Hamilton Niagara Haldimand Brant | 14 | 35 | 30 |
| 5 | Central West | NR | 25 | 0 |
| 6 | Mississauga Halton | NR | 40 | 0 |
| 7 | Toronto Central | 21 | 7 | 10 |
| 8 | Central | NA | 14 | 30 |
| 9 | Central East | NA | 70 | 0 |
| 10 | South East | 30 | 120 | 0 |
| 11 | Champlain | NA | 105 | 45 |
| 12 | North Simcoe Muskoka | NA | 40 | 0 |
| 13 | North East | NA | 43 | 0 |
| 14 | North West | NA | 35 | NR |
| Means | 22 | 48 | 11 | |
Abbreviations: LHIN, local health integration network; NA, not applicable; NR, not reported.
3 out of 6 relevant surveys responded to this question.
32 out of 39 relevant surveys responded to this question.
14 out of 23 relevant surveys responded to this question.
Of the 40 PR centres reporting their hours of operation, 22 (55%) offer services 5 days per week or more, and 8 (20%) operated outside of regular business hours (before 8:00 AM or after 5:00 PM). The remaining 18 centres ran part-time, (4, 3, or 2 days per week for 5, 4, and 8 sites, respectively), and only 1 of these included after-hours services. Only 1 program, in the Mississauga Halton LHIN, reported having weekend hours, and these were specifically for access to a local gym 24 hours per day, 7 days per week.
Among outpatient programs, the most commonly reported components were education (a mean of 22% of all program time was spent on this activity) and treadmill (16% of program time). For maintenance programs, cycling and treadmill accounted for the largest component (each 20%). The least amount of time was spent on nutritional support in both outpatient and maintenance programs (almost 6% and 3% of time spent, respectively).
Many sites reported offering various other rehabilitation services in addition to PR services (43 sites reporting). These include cardiac (11 sites, 26%), heart failure (6 sites, 14%), and general rehabilitation services (13 sites, 30%). A majority of PR facilities (72%) offer smoking cessation programs in-house, and just over half of facilities that do not offer cessation programs (55%) report that they refer patients to external programs or resources.
In addition to exercise training, types of PR support services that the 43 responding sites offer include self-management (95%), psychosocial (83%), strength and breathing (83%), nutrition (80%), smoking cessation (80%), management of other chronic conditions (78%), exercise training/education lasting less than 4 weeks (48%), and a variety of other supports on a less common basis.
Among the full PR sites that reported on their educational topics (37 centres), all cover breathing exercises, energy conservation, and medications. The second most popular topics, covered in 95% of programs, are action plans, relaxation/panic control, and use of inhalers.
The most common structure for the instructional components of PR is programming tailored for individual patients (51% of 37 sites responding), followed by a combination of individualized and group programming (26%) and group programs only (23%). Nearly all programs (97%) invite family members to participate in program components.
Patient Pre-Program Assessment and Clinical Outcome Measurements
Among sites reporting that they assess patients prior to beginning the PR program (40 centres responding), most routinely include patient history (95%), heart rate and oxygen saturation testing (88%), and blood pressure testing at rest (78%) in their pre-program assessment. Quality of life questionnaires, more commonly the St. George's Respiratory Questionnaire and the Chronic Respiratory Questionnaire, are used by 9 (23%) and 19 (48%) of the centres, respectively. No sites used fat free mass measurement as a pre-assessment methods, and only 1 reported using a generic quality of life questionnaire such as the Short Form 36 Dimensions (SF-36) or EuroQol 5 Dimensions (EQ-5D) (3%).
Staffing
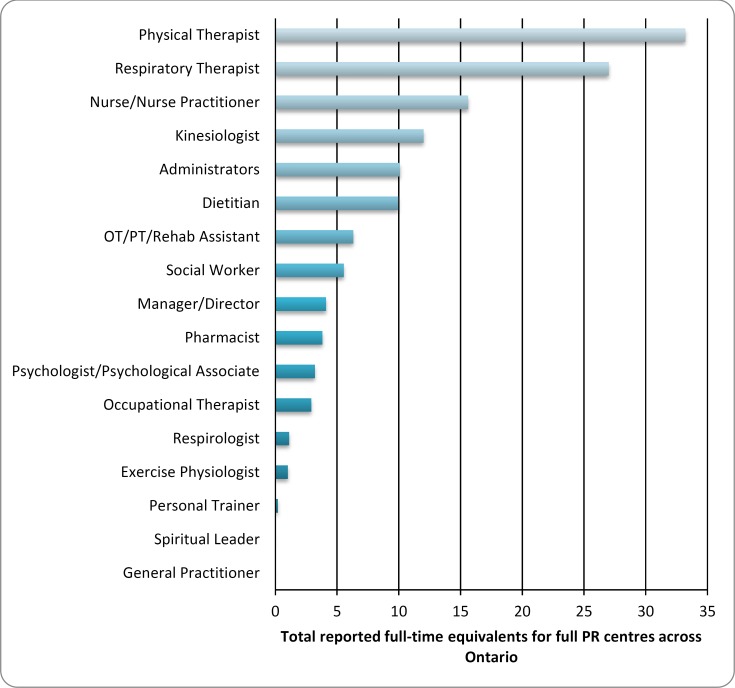
The total composition of staff for full PR programs in Ontario is summarized in Figure 1. The health care professionals most widely employed at PR centres across the province are physical therapists, at just over 33 full-time equivalents (FTE), and respiratory therapists, at 27 FTE.
Figure 1: Total Staff Complement for Pulmonary Rehabilitation in Ontario, by Personnel Type.
Abbreviations: OT, occupational therapist; PR, pulmonary rehabilitation; PT, physical therapist.
Although no respondents provided an FTE measurement for spiritual leaders and general practitioners, these professions are each available in one PR centre.
Some sites reported having access to specific professionals, without indicating their status in terms of FTE. Table 10 presents the number of full PR sites, by LHIN, that have access to various types of professionals. Again, the health care professionals most commonly involved in PR programs are physical therapists (67% of centres) and respiratory therapists (61%).
Table 10:
Full Pulmonary Rehabilitation Centres With Access to Health Care Personnel, by LHIN
| Personnel Typea | Total Full PR Centres With Access to Health Care Personnel, by LHIN Numberb, n | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total (%) | |
| Physical Therapist | 3 | 2 | 2 | 3 | 2 | 4 | 2 | 1 | 2 | 1 | 3 | 1 | 2 | 1 | 29 (67) |
| Respiratory Therapist | 3 | - | 1 | 2 | 2 | 4 | 1 | 1 | 2 | - | 5 | 2 | 2 | 1 | 26 (61) |
| Dietitian | 1 | 1 | 3 | 2 | 2 | 2 | - | 1 | - | - | 2 | 3 | 1 | - | 18 (43) |
| Nurse | 2 | 2 | 1 | 1 | - | 1 | - | - | 2 | 1 | 3 | 1 | 2 | - | 16 (38) |
| Social Worker | 1 | 1 | 2 | 1 | - | 2 | - | 1 | - | 1 | 3 | 2 | 1 | - | 15 (36) |
| Administrators | 3 | - | 3 | 2 | - | - | 1 | 1 | 1 | 1 | 2 | - | 1 | - | 15 (35) |
| Pharmacist | 1 | 2 | - | 1 | 2 | 2 | 1 | - | - | - | 1 | 3 | - | - | 13 (30) |
| Respirologist | - | 2 | 2 | - | 2 | 1 | 1 | - | - | 1 | 2 | 1 | - | - | 12 (28) |
| Occupational Therapist | 1 | 1 | 1 | 2 | 2 | 1 | - | - | - | 1 | 1 | 1 | - | - | 11 (26) |
| Kinesiologist | 1 | 1 | 1 | - | - | 1 | - | - | - | - | 2 | 1 | 2 | - | 9 (21) |
| OT/PT/Rehab Assistant | - | - | 2 | 1 | - | 1 | 1 | - | 1 | 1 | - | - | - | 1 | 8 (19) |
| Manager/ Director | 1 | - | 2 | - | - | - | - | 1 | 1 | - | 1 | - | 1 | - | 7 (17) |
| Psychologist/Psychological Associate | - | - | - | 1 | - | - | - | - | - | - | 1 | - | 1 | - | 3 (7) |
| General Practitioner | - | 1 | - | - | - | - | - | - | - | - | - | - | 1 | - | 2 (5) |
| Personal Trainer | - | - | - | - | - | - | - | - | - | - | - | - | 1 | - | 1 (2) |
| Spiritual Leader | - | 1 | - | - | - | - | - | - | - | - | - | - | - | - | 1 (2) |
| Exercise Physiologist | - | - | - | 1 | - | - | - | - | - | - | - | - | - | - | 1 (2) |
| Total Centres Respondingc | 3 | 4 | 3 | 4 | 2 | 4 | 2 | 1 | 2 | 1 | 6 | 3 | 4 | 1 | 40 (93) |
Abbreviations: LHIN, local health integration network; OT, occupational therapist; PR, physical rehabilitation; PT, physical therapist.
No respondents indicated that they had access to either internists or physiatrists.
By name and number, the LHINs are as follows: 1, Erie St. Clair; 2, South West; 3, Waterloo Wellington; 4, Hamilton Niagara Haldimand Brant; 5, Central West; 6, Mississauga Halton; 7, Toronto Central; 8, Central; 9, Central East; 10, South East; 11, Champlain; 12, North Simcoe Muskoka; 13, North East; 14, North West.
Some respondents indicated they had access to specific professionals without designating the FTE complement(s).
Only hospitals (18 of 28 hospital sites) and community health centres (4 of 6 CHC sites) reported having access to both physical and respiratory therapists. Sites that only had access to nurses were based at family health teams (4 of 7 sites), hospitals (2 of 7 sites), and CHCs (1 of 7 sites); the remaining site having access only to a nurse classified their facility as “other,” with no description.
No sites reported having access to either internists or physiatrists, and although no respondents provided an FTE measurement for spiritual leaders and general practitioners (Figure 1), these professions are available in a few PR centres (Table 10).
Staff Certification
A total of 37 full PR sites reported having health care professionals on staff who had completed a COPD or asthma educator program (mean of almost 2 staff members per site in LHINs where someone had completed this training). Eight sites reported that at least 1 employee was currently enrolled in a COPD or asthma educator program, and 29 sites reported having at least 1 health care professional on staff with national certification, such as Certified Respiratory Educator or Certified Asthma Educator.
Program Management
Based on the 40 sites that provided the profession of the program's manager/director, full PR programs in Ontario are most commonly headed by nurses (25%) or physical therapists (23%). Program medical directors are most commonly respirologists (54%) or general practitioners (16%), according to 37 sites reporting.
Maintenance Activities
Most full PR centres (68%, or 27 of 40 sites responding) offer an in-house maintenance or follow-up component to their program. Of the remaining 13 centres, more than two-thirds (69%) rely on community programs to provide maintenance opportunities for their clients. These external programs typically take place in local gyms and “other” centres, such as lung association sites, (56%, 5 of 9) or local schools and community centres (44%, 4 of 9). The majority of maintenance activities are carried out in person (65%, 26 of 40 sites reporting). We found no clear pattern on the frequency of patient contact after the end of the maintenance program.
Dominant barriers to running a maintenance program include lack of funding (49%, 19 of 39 sites responding) and human resources (44%, 17 of 39). Exercise sessions are the most popular components of maintenance programs (some exercise components are integrated, others are external) and education sessions are least popular. Of the 31 sites that reported having an exercise or fitness training component to their maintenance program, 35% (11 of 31) of these programs are run by physical therapists. About half of respondents (55%, 17 of 31) reported that they follow-up with patients to see if they continue with post-maintenance exercise programs in the community; those exercise programs typically operate at a local gym (53%, 9 of 17) or community centre (41%, 7 of 17).
DISCUSSION
This is the first in-depth survey to investigate pulmonary rehabilitation services (PR) for patients with chronic obstructive pulmonary disease (COPD) in Ontario specifically. The most recent national survey data, collected by Brooks et al (10) in 2005, identified 41 PR programs in the province. In our survey, 187 sites responded (response rate, 46%), including 43 that offer full PR services. Based on our knowledge of the number and location of programs in Ontario, this represents a response rate of more than 95% by full PR services. The remaining 144 centres reported offering other or no rehabilitation services that could potentially support people with COPD.
Program Setting
Centres offering full PR services in Ontario primarily serve large urban centres, with populations greater than 200,000 (37%) or populations between 100,000 and 200,000 (26%). Full PR centres are largely located in hospitals (67%), a finding similar to that of studies from other countries, including Australia (19) and the United States, (17) which found that 66% and 74% of PR programs, respectively, were hospital-based. However, one-third of the full PR programs we identified in Ontario are based at either family health teams (FHT, 19%) or community health centres (CHC, 14%). This suggests that there is the ability in this province to decentralize PR programs from hospitals.
The necessity for hospitals to be the primary providers of pulmonary rehabilitation can be questioned, as the vast majority of PR programs are delivered on an outpatient basis (93%). Only 12% were reported as inpatient, 54% as maintenance, and 16% as telehealth medicine programs (percentages exceed 100 because some centres offer more than one type of program). In 2010, the Canadian Thoracic Society found that functional outcomes—health-related quality of life, exercise tolerance, and reductions in dyspnea—did not differ between patients completing non-hospital and hospital-based PR programs. (11) Similarly, previous studies in the United Kingdom, (26) United States, (17) and Canada (10) have found that most PR programs are conducted on an outpatient basis (99%, 94%, and 57%, respectively). A 2013 study by Spruit et al (35) investigated the characteristics of PR programs worldwide and also found that most programs in North America were structured as outpatient programs (72%), followed by maintenance (23%), and inpatient (4%). Each of these program types, except for those serving an inpatient population, could easily be supported by a family health team or community health centre, enabling a shift from primarily hospital-based to more community-based PR programs in Ontario.
Program Entry and Wait Times
Half of Ontario's PR sites (53%, 21 of 40 sites responding) report prioritizing patients for entry into their program, and 90% said recent hospitalization was important in how patients are queued. The most commonly cited sources of referrals were respirologists (84% of sites) and general practitioners (GP) (79%). This result is similar to the 2005 Canadian study that also showed respirologists and GPs were the primary sources of referrals and the worldwide study by Spruit et al, which showed that most referrals came from chest physicians and GPs. (10;35)
In the 2005 national survey, Brooks et al (10) found a mean wait time of 11 weeks. In our survey, the total mean wait time for outpatient programs across all Ontario LHINs was 6.9 weeks, which suggests substantial improvement. This is also shorter than the 2004 national mean of 9 weeks in the United Kingdom. (26) However, the Ontario mean is skewed by outlying wait times in 5 LHINs: Toronto Central (1 week), Central (2 weeks), Waterloo Wellington (12.1 weeks), Champlain (15 weeks), and South East (17.1 weeks). These wait times fall outside the 99% confidence interval for the population. If the wait times for these 5 LHINs were removed from the calculation, then the mean provincial wait time decreases to 5.5 weeks. This would indicate that the wait time for PR outpatient programs in Ontario has, on average, been cut in half since 2005.
Current Program Capacity and Limiting Factors
The survey results show that the capacity of PR programs in Ontario to accommodate patients with COPD continues to be severely limited. Overall, the mean capacity in the province ranged from 0.66% of COPD patients treated (based on the higher COPD prevalence from ICES) to 1.78% (using the lower COPD prevalence from census data). This is in keeping with the 2010 national estimate, by the Canadian Agency for Drugs and Technologies in Health, (13) that 1.15% of the COPD population had access to PR services. While we found that the LHIN-specific capacities fluctuated above and below the 1% mark, the LHIN with the lowest capacity was South West (0.19%–0.42%) and the highest capacity was in North East LHIN (1.97%–4.33%). Raising this capacity across the province would bring Ontario closer to practices supported by current evidence and recommendations. A recent report by Health Quality Ontario found evidence that PR, compared with usual care, leads to clinically and statistically significant improvements in health-related quality of life, as well as improved exercise capacity, reduced hospital admissions, and greater cost-effectiveness. (14) Similarly, the Canadian Thoracic Society clinical practice guidelines for PR recommend that all COPD patients have access to pulmonary rehabilitation, regardless of program site. (11)
Access to PR services in Ontario is limited by a number of factors. Relative to the need, few health care personnel are dedicated to PR across the province. Only 22 (55%) of the 40 full PR centres that reported on their hours of operation offer services 5 days per week or more, and only 8 (20%) of these have hours outside of regular business hours. The remaining 18 centres operate only on a part-time basis (2, 3, or 4 days per week) and only 1 of those includes after-hours services. More flexible program hours (e.g., evenings and weekends) and types of services (e.g., external gym partnership) would likely increase the accessibility of the programs. Local facilities such as schools, community centres, churches, cultural centres, and gyms/recreational centres may be able to provide venues for PR maintenance activities; these facilities could provide access to structured exercise programs, in partnership with the PR programs, outside of regular business hours for outpatient hospital services. In addition, we found that only 68% of sites reported offering an in-house maintenance program and that 9 (69%) of the 13 sites without an in-house maintenance program reported utilizing external community programs to support clients after they completed their initial PR. Although this is a marked improvement since 2005 when only 22% of Canadian programs were found to offer a maintenance component, (10) a substantial proportion of PR programs in Ontario are unable to routinely follow-up with clients. The most commonly cited barriers to operating a maintenance program are lack of funding (49%) and lack of human resources (44%).
Staffing
Thirty-seven of the 43 sites (86%) reported having personnel who had completed a COPD or asthma educator program. This is slightly lower than for Australian PR programs, which reported 95% of staff had completed post-graduate training or certification in pulmonary rehabilitation. (19) However, our findings show considerable improvement over the 2005 national study, which found only 66% of PR programs across Canada had at least one health care professional who had completed a respiratory educator program. (10) Increasing recognition of the value of Certified Respiratory Educators (CREs) is apparent and helps to meet the needs of people with respiratory disorders. We found that PR program managers/directors in Ontario are most often nurses (25%) or physical therapists (23%). This differs somewhat from the United States, where programs are more commonly headed by registered respiratory therapists (38%) or registered nurses (24%). (17)
Program Components
PR program offer a wide range of PR services in addition to exercise training. We found that most Ontario centres offered self-management programs (95%), psychosocial support (83%), strength and breathing counselling (83%), nutritional support (80%), and chronic disease management programs (78%). Breathing exercises, energy conservation, medications, action plans, relaxation/panic control, and use of inhalers were offered as educational topics in more than 95% of programs. Other countries have reported similar PR services: exercise training is the major focus of most programs (99% of programs in the United Kingdom and Australia), followed by education. (19;26) The educational topics that we found were similar to those reported earlier in Canada (10) and the United Kingdom. (26)
In Ontario, most reporting centres allow family participation, a beneficial practice as involving families in the learning process increases participants' social support and their chances of successful rehabilitation. (36) In addition, we found that 78% of Ontario sites permit current smokers to enter the PR program and that 80% of facilities offer smoking cessation counselling. This acceptance of current smokers is comparable to programs in the United Kingdom and United States, where 90% and 83% of PR sites, respectively, accept current smokers. However, unlike in Ontario, only half of PR programs in the United Kingdom (50%) and the United States (52%) report offering smoking cessation counselling. (17;26)
Pre-program Assessments
While most PR programs responding to our survey conduct basic physical pre-program assessments (patient history, 95%; oxygen saturation testing, 88%; blood pressure testing, 78%), only 3% of programs reported using generic quality of life questionnaires. The clinical outcome measures that Ontario programs most often use are oximetry during exercise, oximetry during rest, Modified Borg scale during exercise, and a rating of perceived exertion during exercise. The Shuttle Walk test and or 6- and 12-Minute Walk test were the most commonly used physical measures; similarly, the 6–Minute Walk test was found to be the most common measure in Canada in 2005. (10) Use of each of these measures was considerably more common in outpatient programs compared to inpatient. Compared to other countries, Ontario programs use fewer measures and capture a narrower spectrum of outcomes. For example, quality of life questionnaires such as the Chronic Respiratory Disease Questionnaire and St. George's Respiratory Questionnaire, as well as generic quality of life measures such as the 36–item Short Form Health Survey (SF-36), are commonly used in both pre- and postprogram assessments in the United Kingdom, (26) Northern Ireland, (23) Australia, (19) and the United States. (17) These countries also commonly use the hospital anxiety and depression scale. While using more outcome measures will undoubtedly provide more information, and perhaps a more comprehensive overview of a patient's progress from rehabilitation, it could also be argued that standardizing outcome measures and ensuring the completion of pre- and postprogram assessments would allow the centres to compare the incremental changes associated with the PR programs at both the patient and program level.
LIMITATIONS
Our survey identified pulmonary rehabilitation programs from public sources, and the overall response rate from the full PR centres was more than 95%. However, for some LHINs (Central and Toronto Central) response rates were less than 30%, limiting the ability of the survey to describe PR services in these areas. Factors that may have contributed to the lower response rate in some LHINs include the time required to complete the survey (it ran 18 pages and covered multiple domains), timing (the initial survey was conducted during the summer), and challenges in identifying the appropriate people to complete the survey (the complexity of the survey may have made it difficult for a single person at each site to complete it, without consulting various colleagues). Fatigue due to the length of the survey may also have affected the precision of responses; for some of the later questions, the survey was returned, but responses were not provided.
CONCLUSIONS
Program capacity in Ontario to provide pulmonary rehabilitation (PR) services for people with chronic obstructive pulmonary disease (COPD) is limited. An estimated 0.66% to 1.78% of the population with COPD participate in PR programs in a given year. Although some increase in capacity has occurred since a similar national survey in 2005, PR resources in Ontario are insufficient to support practice that meets clinical practice guideline recommendations.
While the majority of PR programs are conducted on an outpatient basis in a hospital setting, evidence suggests that delivering PR in non-hospital settings would not impact patient outcomes. More research is needed to understand whether a shift to greater use of community-based settings would improve program capacity and utilization. Since the 2005 national survey, pulmonary rehabilitation in Ontario has expanded to include more centres (43 vs. 21), more programs with maintenance components (68% vs. 22%), a higher number of centres reporting personnel with COPD certification (86% vs. 66%), and a shorter average wait time for outpatient programs (6.9 weeks vs. 11 weeks).
ACKNOWLEDGEMENTS
The authors thank the staff at each of the contributing sites for their participation in the survey. We also thank Dr. Les Levin, Health Quality Ontario, and the Ontario Health Technology Advisory Committee for their support of the study and for their comments. The authors would like to thank Jathishinie Jegathisawaran for her work in summarizing the previous completed national pulmonary rehabilitation surveys.
Funding from the Ontario Ministry of Health and Long-Term Care was acquired through an independent Health Technology Assessment and Economic Evaluation Program research grant awarded to Professor Ron Goeree and research team (Grant 06129) at the Programs for Assessment of Technology in Health (PATH) Research Institute, St. Joseph's Healthcare Hamilton.
Study Working Group Members
| Dr. Dina Brooks | University of Toronto |
| Ann Bartlett | St. Joseph's Healthcare Hamilton |
| James Bowen | Programs for Assessment of Technology in Health |
| Dr. Andrea Gershon | University of Toronto |
| Dr. Roger Goldstein | West Park Healthcare Centre |
| Dr. Alan Kaplan | Representative for the Ontario College of Physicians |
| Shelley Prevost | St. Joseph's Hospital, Thunder Bay |
| Lorelei Samis | Providence Care – St. Mary's of the Lake Hospital, Kingston |
| Kiran Chandra | Programs for Assessment of Technology in Health; Health Quality Ontario |
| Angela Jacobs | Executive Lead, Mississauga/Halton LHIN |
| Vincent Pileggi | Health Quality Ontario |
| Ron Goeree | Programs for Assessment of Technology in Health |
APPENDIX A: PRO SURVEY – CONDENSED VERSION
This appendix contains a condensed version of the full Pulmonary Rehabilitation Programs in Ontario (PRO) Survey that was sent to potential pulmonary rehabilitation centres across the province. The full survey is available on request from PATH Research Institute.
The full survey was 18 pages. This condensed version covers all domains and sample questions in the order they appeared in the full survey. Formatting has been altered.
APPENDIX B: LHIN PROFILES
This appendix summarizes the PRO Survey findings on key elements of pulmonary rehabilitation (PR) services for people with chronic obstructive pulmonary disease (COPD) in each Ontario local health integration network (LHIN).
Each LHIN profile is based on responses received from centres with full PR programs. For LHINs with fewer responses, it was difficult for us to accurately describe the PR services; we have noted this limitation in the individual profiles.
Each profile contains the following LHIN-specific information:
Demographics (see tables)
census population ≥ 35 years of age
-
“best-case” estimated population with COPD (Statistics Canada data, based on self-reports)
-
–
estimated COPD prevalence (from Statistics Canada data)
-
▪
estimated COPD population
-
▪
-
–
-
“worst-case” estimated population with COPD
-
–
estimated COPD prevalence (from Ontario administrative data, provided by the Institute for Clinical Evaluative Sciences [ICES])
-
▪
estimated COPD population
-
▪
-
–
LHIN and PR program characteristics (see tables)
number of responding PR centres
types of programs at the responding centres
size of catchment area of responding centres
typical hours of operation of responding centres
mean wait time (days) for outpatient programs
mean outpatient program length
number of COPD patients through all combined programs annually
percentage of COPD population participating in PR programs annually
LHIN and PR program characteristics (see text portion of profiles)
types of facilities where the responding programs are based (e.g., hospital, family health team [FHT], community health centre [CHC])
geographic distribution within the LHIN of all responding PR centres
“current smoker” acceptance
program funding
-
staff dedicated to PR as indicated by serving on the LHIN's PR team(s)
-
–
typical staffing hours (e.g., full-time, part-time)
-
–
total full-time equivalents (FTE) of dedicated PR personnel
-
–
survey response rate of all centres within the LHIN (including PR centres and non-PR sites)
structured COPD services offered by non-PR sites
referral patterns of non-PR sites
LHIN Profile 1: Erie St. Clair
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 368,596 | 21,378 (5.8) | 49,760 (13.5) |
| LHIN Characteristic | Value | |
| Responding PR centres | 4 | |
| Program types (outpatient, inpatient, maintenance) | 4 outpatient, 4 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 1 of 4 responding centres | |
| A regional centre serving a population of 100,000–200,000 | 1 of 4 responding centres | |
| A centre serving a population of 50,000–100,000 | 1 of 4 responding centres | |
| A centre serving a population of 10,000–50,000 | 1 of 4 responding centres | |
| Typical hours of operation | 3 full-time, 1 part-time (12:30–16:00 Mon, Wed, Fri) | |
| Mean outpatient program wait time, days | 35 days | |
| Mean outpatient program length | 11 weeks | |
| Reported COPD patients through programs annually | 26 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.52%–1.21% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Erie St. Clair LHIN has a higher prevalence of COPD than the 3.8% mean for Ontario. (37) The PR programs vary in length (from 8 to 16 weeks for outpatient services) as the PR centres run several outpatient programs each year. However, maintenance programs typically run for most of the year (2 sites reported lengths greater than 50 weeks and 1 site did not report a length, though it did report that the total number of referrals each year equalled the number of patients). The PR programs are spread across all types of facilities: 1 is hospital-based, 1 is based at a family health team, and 2 are based at community health centres. In addition, the 4 responding PR centres are spread evenly across the LHIN with 3 in the soutern, more populated half, and 1 in the northern, more rural half. While program hours of operation did vary between sites, 2 sites reported full-time operation (Monday to Friday, 8 hours/day) and 1 reported operating 3 days a week (Monday, Wednesday, Friday) in the afternoon. Seventy-five percent of centres that offer PR within this LHIN accept current smokers into their programs. The same proportion (75%) is government funded, and 1 program is funded by patients through participation fees. All centres reported having a maintenance component that is self-sustaining (i.e., they do not generally use community resources/infrastructure such as local gyms or activity centres).
Physical therapists and respiratory therapists were reported as full-time members of the PR teams at 75% of sites. Designated administrators, nurses, and manager/directors were also reported as members of the PR team; most of these are full-time positions. The total reported full-time equivalent of dedicated PR personnel across the LHIN was 25.
Of the 18 sites contacted in the Erie St. Clair LHIN, 12 responded to our survey (response rate of 67%). Of these, 8 do not have a PR program. However, 4 of these non-PR sites did report having some structured services for patients with COPD. Services common to all of these sites include chronic disease management, nutritional support, self-management, psychosocial support, and smoking cessation counselling. Strength and breathing training is also offered by 50% of non-PR centres. The non-PR sites all refer patients to the 4 PR centres that we captured; there were no extra sites not captured in our survey.
With responses from 4 PR centres and 8 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the Erie St. Clair LHIN.
LHIN Profile 2: South West
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 545,899 | 27,294 (5.0) | 58,411 (10.7) |
| LHIN Characteristic | Value | |
| Responding PR centres | 4 | |
| Program types (outpatient, inpatient, maintenance) | 3 outpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 2 of 4 responding centres | |
| A centre serving a population of 10,000–50,000 | 1 of 4 responding centres | |
| A centre serving a population < 10,000 | 1 of 4 responding centres | |
| Typical hours of operation | 1 full-time, 3 part-time (Mon, Wed; Tue, Thu; Mon, Wed, Thu, Fri) | |
| Mean outpatient program wait time, days | 15 days | |
| Mean outpatient program length | 10 weeks | |
| Reported COPD patients through program annually | 115 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.19%–0.42% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The South West LHIN has a higher prevalence of COPD than the 3.8% provincial mean. (37) There are 3 outpatient programs in the LHIN running 6, 8, and 16 weeks. Seventy-five percent of the centres run on a part-time basis, and only 1 centre has full-time hours. Despite the limited hours and the fact that more than one-third of the LHIN's total population resides within one urban centre, the mean wait time is only 15 days for the LHIN. The 4 PR centres in the South West LHIN are all located in the southern-most third of the geographical region. This reflects the difficulties in maintaining a PR program: “transportation” and “distance in location” were the top barriers reported for all sites. All of the centres within the LHIN are government funded, and all 4 centres allow current smokers to enter their programs. Three of the 4 programs in this LHIN are hospital-based, and 1 is based out of a family health team. All programs in the LHIN reported being supported by their communities; for maintenance activities, they utilize local gyms, the YMCA, and centres for activity and aging.
In 75% of the PR sites, PR team members reported working part-time, although there are a wide variety of personnel including nurse, respirologist, physical therapist, social worker, dietitian, kinesiologist, pharmacist, and general practitioner. The total reported full-time equivalent of dedicated PR personnel across the LHIN could not be determined as this was not reported for more than 80% of listed staff.
Of the 39 sites contacted in the South West LHIN, 27 responded to our survey (response rate of 69%). Of these, 23 do not have a PR program. However, 17 did report having at least one of several structured services for patients with COPD. While no services were reported to be offered universally, the 3 services most commonly offered by non-PR centres are smoking cessation counselling, self-management, and nutritional support. Services least offered include psychosocial support, strength and breathing training, and exercise training/education. The non-PR sites reported referring patients to 2 of the PR centres that we captured in our survey, as well as 2 other PR centres from neighbouring LHINs (the Hamilton Niagara Haldimand Brant and Mississauga Halton LHINs).
With responses from 4 PR centres and 23 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the South West LHIN.
LHIN Profile 3: Waterloo Wellington
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 408,301 | 19,190 (4.7) | 33,072 (8.1) |
| LHIN Characteristic | Value | |
| Responding PR centres | 4 | |
| Program types (outpatient, inpatient, maintenance) | 4 outpatient, 3 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 2 of 4 responding centres | |
| A regional centre serving a population of 100,000–200,000 | 1 of 4 responding centres | |
| A centre serving a population of 10,000–50,000 | 1 of 4 responding centres | |
| Typical hours of operation | 4 full-time | |
| Mean outpatient program wait time, days | 85 days | |
| Mean outpatient program length | 10 weeks | |
| Reported COPD patients through program annually | 464 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 1.40%–2.42% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Waterloo Wellington LHIN has a higher prevalence of COPD than the 3.8% Ontario mean, but the COPD patient capacity of 1.4% annually is greater than the previous provincial estimate of 1.15%. (37) The outpatient program lengths were 8 and 12 weeks with maintenance having a wider range of 12 to 52 weeks. All facilities within this LHIN operate on a full-time basis: 5 days a week with regular working hours. The mean wait time for the LHIN is 85 days. Three of the programs are government funded and 1 program is funded entirely through patient participation fees. Seventy-five percent of sites in the LHIN responded that the lack of availability of private transportation is a barrier to patients accessing a PR program and rated it at the highest importance. Compounding the problem of transportation is the distance that patients must travel to sites that offer PR, as 78% of the LHIN's population, and all 4 PR sites, are located in the southern-most third of the geographical range. All 4 programs are hospital-based and have a maintenance component that is self-sustaining (i.e., they do not generally make use of other community infrastructure such as local gyms or activity centres).
Seventy-five percent of the sites reported that the members of their PR teams are primarily part-time; only 1 site had any full-time staff. Managers and directors were reported for all teams in the LHIN and other common PR personnel, reported by more than 50% of sites, included dietitians, physical therapists, respirologists, and administrators. Thirty percent of reported PR personnel did not have an FTE reported with their position. The total reported full-time equivalent of dedicated PR personnel across the LHIN was 3.36.
Of the 22 sites contacted in the Waterloo Wellington LHIN, 12 responded to our survey (response rate of 55%). Of these, 8 do not have a PR program. However, 7 did report having some structured services for patients with COPD. While there were no services that are offered by all sites, the 2 most commonly offered are smoking cessation counselling and chronic disease management. The 2 least offered are strength and breathing training and exercise training/education. The non-PR sites refer to all 4 of the PR centres that responded to our survey. In addition, 2 of the non-PR sites reported referring patients to one of the other non-PR sites.
With responses from 4 PR centres and 8 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services in the Waterloo Wellington LHIN.
LHIN Profile 4: Hamilton Niagara Haldimand Brant
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 817,103 | 43,306 (5.3) | 83,344 (10.2) |
| LHIN Characteristic | Value | |
| Responding PR centres | 4 | |
| Program types (outpatient, inpatient, maintenance) | 4 outpatient, 1 inpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 2 of 4 responding centres | |
| A regional centre serving a population of 100,000–200,000 | 2 of 4 responding centres | |
| Typical hours of operation | 2 full-time, 2 part-time (13:00–15:00 Mon, Wed; 13:30–15:30 Tue, Thu) | |
| Mean outpatient program wait time, days | 35 days | |
| Mean outpatient program length | 15 weeks | |
| Reported COPD patients through program annually | 417 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.50%–0.96% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Hamilton Niagara Haldimand Brant (HNHB) LHIN has a higher COPD prevalence than the 3.8% provincial mean. (37) Outpatient program lengths vary from 6 to 40 weeks. The inpatient program is 6 weeks long and the maintenance program is 12 weeks long. The programs are primarily hospital-based (75%); the other 25% are based out of a CHC. The programs are all located within large catchment areas and the northern half of the LHIN's geographic range; this more densely populated half is home to more than 70% of the LHIN's population. Only 50% of the programs across the LHIN operate on a full-time basis and the other half are only open 2 and 3 days per week, for only 2 hours each day. All the sites in the LHIN allow current smokers to participate in their PR programs. Most (75%) are funded by the government; 1 program is funded by a private source. None of the programs have participation fees but 75% report that public and private transportation are out-of-pocket expenses for patients and thus a barrier to their maintaining participation in a PR program. All sites in the LHIN use community resources and infrastructure as the basis or a part of the maintenance component. Local YMCAs, gyms, community centres, and BreathWorks/Lung Association programs were all reported to be a means of maintenance.
Physical therapists are members of the PR team at 75% of sites. Physical therapists, occupational therapists, and dietitians were also frequently reported members of the PR teams across the LHIN. There is an equal mix of full-time and part-time staff as 1 program has entirely part-time, 1 has entirely full-time, and 1 has a mix. (One site did not report on this.) The total reported full-time equivalent of dedicated PR personnel across the LHIN was 14.1.
Of the 34 sites contacted in the HNHB LHIN, 21 responded to our survey (response rate of 62%). Of these, 17 do not have a PR program. However, 15 did report having some structured services for patients with COPD. For non-PR sites, there are no universally offered services, but the most commonly offered are smoking cessation counselling and chronic disease management, and the least offered are exercise training/education and strength and breathing training. The non-PR sites refer to all 4 of the PR centres that responded to our survey. In addition, the non-PR sites reported referring patient to 1 PR centre in an adjacent LHIN, 1 other non-PR site, and 2 sites that did not respond to our survey.
With responses from 4 PR centres and 17 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the HNHB LHIN.
LHIN Profile 5: Central West
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 453,105 | 8,155 (1.8) | 33,529 (7.4) |
| LHIN Characteristic | Value | |
| Responding PR centres | 2 | |
| Program types (outpatient, inpatient, maintenance) | 2 outpatient, 1 inpatient, 2 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 2 of 2 responding centres | |
| Typical hours of operation | 1 full-time, 1 part-time (13:00–15:00 Tue, Fri) | |
| Mean outpatient program wait time, days | 25 days | |
| Mean outpatient program length | 8 weeks; 40 weeks | |
| Reported COPD patients through program annually | 108 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.32%–1.32% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Central West LHIN has a lower prevalence of COPD than the 3.8% mean for the province. (37) The 2 outpatient programs differ in length: 8 and 40 weeks. One of the maintenance programs runs 47 weeks and the other does not have a set length; participants are invited to continue as long as they wish. The 2 sites operate on different schedules: 1 full-time and the other only 2 days per week. Compared to other LHINs, Central West has a short mean wait time (25 days). The programs are based in hospitals and CHCs and are funded through several different means: government, patient (out-of-pocket), private insurance, and non-insured health benefits. Lack of private transportation and distance from location are the 2 most common and important barriers for patients in the programs, and both have maintenance components that do not generally use community resources or infrastructure. The responding sites are located in the southern-most quarter of the geographical range, which is home to half of the population.
Both sites reported that their PR staff are part-time employees, and both have the same personnel: dietitian, occupational therapist, pharmacist, physical therapist, respiratory therapist, and respirologist. One site reported that their team members operate primarily on a consultation basis; they attend in-person only several hours a year but are available to answer questions by email. The total reported full-time equivalent of dedicated PR personnel across the LHIN was 2.2.
Of the 11 sites contacted in the Central West LHIN, 6 responded to our survey (response rate of 55%). Of these, 4 do not have a PR program. However, 2 did report having some structured services for patients with COPD. Smoking cessation counselling and nutritional support are offered by both non-PR sites; none offer exercise training/education. The non-PR sites reported referring patients to 1 of the 2 PR centres that responded to our survey.
We received responses from 2 PR centres and 4 non-PR centres, all clustered in the southern-most quarter of the LHIN's geographical range. Since we have no responses from a large part of the LHIN, even though most of the population was captured in our survey, we cannot conclude that our findings provide an accurate depiction of the PR services within the Central West LHIN.
LHIN Profile 6: Mississauga Halton
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 628,800 | 13,204 (2.1) | 45,902 (7.3) |
| LHIN Characteristic | Value | |
| Responding PR centres | 4 | |
| Program types (outpatient, inpatient, maintenance) | 4 outpatient, 1 inpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 3 of 4 responding centres | |
| A centre servicing a population of 10,000–50,000 | 1 of 4 responding centres | |
| Typical hours of operation | 2 full-time, 2 part-time (11:30–15:30 Tue, Thu; 12:35–15:15 Wed, Fri) | |
| Mean outpatient program wait time, days | 40 days | |
| Mean outpatient program length | 10 weeks | |
| Reported COPD patients through program annually | 325 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.71%–2.46% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Mississauga Halton LHIN has a lower prevalence of COPD than the 3.8% mean for the province. (37) All 4 outpatient programs are 10 weeks in duration and all are hospital-based. The maintenance program runs for 52 weeks, but the inpatient program varies in length as it is conducted based on the needs of each participant. Two of the PR sites offer full-time services and 2 sites operate 2 days a week, only a few hours each day. The mean wait time for patients in the LHIN is 40 days. Programs are primarily funded by the government (75% of programs) and 1 program is funded by the hospital's global budget. Availability of transportation and parking fees were reported as the 2 biggest barriers to patient participation. Half the programs responded that they make use of community centres in a maintenance portion of their programs. The responding centres are spread out across most of the LHIN, and only the northern-most geographic region is a considerable distance from a PR site.
All sites reported having a physical therapist and respiratory therapist on staff, either full-time or part-time. The next most common personnel on the PR teams in the Mississauga Halton LHIN are dietitians, pharmacists, and social workers. Overall, the PR personnel in the LHIN are primarily part-time employees. The total reported full-time equivalent of dedicated PR personnel across the LHIN was 3.36.
Of the 14 sites contacted in the Mississauga Halton LHIN, 8 responded to our survey (response rate of 57%). Of these, 4 do not have a PR program. However, 3 did report having some structured services for patients with COPD. Chronic disease management, self-management, psychosocial support, and smoking cessation counselling are all offered by all non-PR centres that reported on their services. Strength and breathing training are not offered by any sites, and exercise training/education is only offered by 1. All 4 of the PR centres that responded to our survey receive referrals from the non-PR centres. In addition, 1 non-PR site refers to a PR centre in an adjacent LHIN.
With responses from 4 PR centres and 4 non-PR centres across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the Mississauga Halton LHIN.
LHIN Profile 7: Toronto Central
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 667,460 | 13,349 (2.0) | 61,406 (9.2) |
| LHIN Characteristic | Value | |
| Responding PR centres | 2 | |
| Program types (outpatient, inpatient, maintenance) | 2 outpatient, 1 inpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 2 of 2 responding centres | |
| Typical hours of operation | Full-time | |
| Mean outpatient program wait time, days | 7 days | |
| Mean outpatient program length | 52 weeks; 6 weeks | |
| Reported COPD patients through program annually | 525 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.86%–3.93% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Toronto Central LHIN has a lower prevalence of COPD than the 3.8% mean for the province. (37) Two sites that provide full PR services responded to our survey, so the summary of PR services in the Toronto LHIN is based on these 2 centres. The centres that responded offer 2 outpatient programs, 1 inpatient program, and 1 maintenance program with lengths of 52 weeks (for 1 of the PR programs) and 6 weeks for the rest. Both centres operate full-time and the mean wait time is 7 days. The programs are funded by the government and report that availability of private transportation, distance in location, and weather are the 3 most important barriers to patient participation in the program. The programs do not accept patients who currently smoke, and 50% do not offer any maintenance after their program has completed.
The PR centres reported having different health care professionals on their PR teams. The teams are primarily full-time with some part-time employees and include the following personnel: physical therapists, administrators, respiratory therapists, pharmacists, respirologists, nurses, and a physical therapy assistant. The total reported full-time equivalent of dedicated PR personnel across the LHIN is 13.
Of the 39 sites contacted in the Toronto Central LHIN, 10 responded to our survey (response rate of 26%). Of these, 8 do not have a PR program. However, 6 did report having some structured services for patients with COPD. While no PR services are offered universally, chronic disease management, nutritional support, and smoking cessation counselling are the most common offerings. None of the non-PR sites offer exercise training/education or strength and breathing education. Both of the PR centres that responded to our survey receive referrals from the non-PR sites that responded. In addition, the non-PR sites reported referring patients to 1 other PR centre that we did not capture in our survey.
Due to the limited response rate from centres that offer PR, it is not likely that our findings provide an accurate depiction of the PR services within the Toronto Central LHIN.
LHIN Profile 8: Central
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 975,460 | 17,558 (1.8) | 75,110 (7.7) |
| LHIN Characteristic | Value | |
| Responding PR centres | 2 | |
| Program types (outpatient, inpatient, maintenance) | 1 outpatient, 2 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A regional centre serving a population of 100,000–200,000 | 1 of 2 responding centres | |
| A centre serving a population < 10,000 | 1 of 2 responding centres | |
| Typical hours of operation | Part-time (8:00–16:00 Mon, Wed, Fri) | |
| Mean outpatient program wait time, days | 14 days | |
| Mean outpatient program length | 6 weeks | |
| Reported COPD patients through program annually | 360 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.48%–2.05% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Central LHIN has a lower prevalence of COPD than the 3.8% mean for the province. (37) While we received responses from 2 centres that offer pulmonary rehabilitation, 1 centre's response was only partially completed, thus our summary and most of our analyses for this LHIN are based on a single centre's response. The outpatient and maintenance programs both run for 6 weeks and are based at a hospital or a family health team. Funding for the LHIN's PR programs comes from the government and from participation fees that patients pay. The lack of availability of public and private transportation was reported as a barrier to patient participation in the PR programs. Out-of-pocket fees are also a potential barrier to participation. Both PR programs allow current smokers and both offer smoking cessation services. Both centres in the LHIN report having a maintenance component, though neither reported using community resources for their programs. The responding PR centres are spread across the LHIN covering most of the geographic range and population.
Employment in PR programs in the Central LHIN is primarily part-time. The PR teams have fulltime managers and directors, and nurses, dietitians, respiratory therapists, and social workers are on staff part-time. The total reported full-time equivalent of dedicated PR personnel across the LHIN is 17.
Of the 18 sites contacted in the Central LHIN, 5 responded to our survey (response rate of 28%). Of these, 3 do not have a PR program. However, all 3 did report having some structured services for patients with COPD. Smoking cessation counselling is offered by all 3 non-PR sites and self-management was offered by 2. No non-PR sites in the LHIN offer nutritional support, exercise training/education, psychosocial support, and strength and breathing services. One of the responding PR centres receives referrals from multiple non-PR sites; the other does not receive referrals from any non-PR site. In addition, the non-PR sites reported that they referred patients to 2 other PR centres in adjacent LHINs: 1 in the Toronto Central LHIN and 1 in the Central East LHIN.
With responses from 2 PR centres, 1 of which was mostly incomplete, and 3 non-PR centres across the LHIN, we are not confident that our findings provide an accurate depiction of PR services within the Central LHIN.
LHIN Profile 9: Central East
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 894,346 | 36,668 (4.1) | 92,117 (10.3) |
| LHIN Characteristic | Value | |
| Responding PR centres | 2 | |
| Program types (outpatient, inpatient, maintenance) | 2 outpatient, 2 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 1 of 2 responding centres | |
| A centre serving a population of 50,000–100,000 | 1 of 2 responding centres | |
| Typical hours of operation | Full-time | |
| Mean outpatient program wait time, days | 70 days | |
| Mean outpatient program length | 12 weeks; 51 weeks | |
| Reported COPD patients through program annually | 265 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.29%–0.72% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The prevalence of COPD in the Central East LHIN is marginally higher than the 3.8% mean for the province. (37) There are 2 outpatient pulmonary rehabilitation programs and they differ in length (8 and 40 weeks). The maintenance programs are more similar in length (48 and 51 weeks), and all programs are hospital-based. Both sites operate full-time but have different wait times for patient enrolment; the wait-list duration at 1 site's outpatient program is 21 days while the other's is 120 days. Funding for the PR programs in the Central East LHIN comes primarily from the government, although patient fees provide supplementary funding. All the sites reported that distance in location, parking, and weather are the most important barriers to patient participation. Availability of private and public transportation was also reported as very important. The maintenance components of each centre are self-contained; they do not generally use community resources or infrastructure. The responding sites are located in the southern half of the LHIN's geographical distribution and serve more than half of the population.
Nurses, physical therapists, and respiratory therapists are the most common members of PR teams in the Central East LHIN. Employment numbers are split evenly between full-time and part-time staff members. The total reported full-time equivalent of dedicated PR personnel across the LHIN is 3.7.
Of the 26 sites contacted in the Central East LHIN, 8 responded to our survey (response rate of 31%). Of these, 6 do not have a PR program. However, 5 did report having some structured services for patients with COPD. All 5 non-PR sites that reported offering some services to patients with COPD provide chronic disease management and nutritional support. Smoking cessation counselling is the next most commonly offered. Only 1 offers exercise training/education and strength and breathing training. The non-PR sites did report referring patients to 1 of the PR centres that responded to our survey. The other responding PR centre does not receive referrals from non-PR sites.
With responses from 2 PR centres and 6 non-PR centres across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the Central East LHIN.
LHIN Profile 10: South East
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 297,796 | 17,569 (5.9) | 35,735 (12.0) |
| LHIN Characteristic | Value | |
| Responding PR centres | 1 | |
| Program types (outpatient, inpatient, maintenance) | 1 outpatient, 1 inpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A regional centre serving a population of 100,000–200,000 | 1 of 1 responding centres | |
| Typical hours of operation | Part-time (11:00–15:30 or 12:30–14:30 Mon, Wed, Thu, Fri) | |
| Mean outpatient program wait time, days Mean outpatient program length | 120 days 12 weeks | |
| Reported COPD patients through program annually | 125 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.35%–0.71% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The South East LHIN has a higher COPD prevalence than the 3.8% mean for the province. (37) Of the 27 sites contacted in the LHIN, only 1 PR centre responded and thus our analysis and summary of PR services within the South East LHIN are based on this site. The facility that responded offers an inpatient program of 3 weeks' duration and outpatient and maintenance programs of 12 weeks' duration. The hours of operation are part-time, from 11:00 AM to 3:30 PM, 3 days of the week, and from 12:30 PM to 2:30 PM, 1 day of the week. The programs have a high total wait time for patients, 120 days, and are government funded. The most important barrier to patient participation reported is distance from the program site, followed by the availability of public and private transportation. The programs accept current smokers. The maintenance component is self-contained and does not generally use community resources or infrastructure.
The health care professionals on the PR team include several physical therapists, administrators, a respirologist, a nurse, a pharmacist, and a social worker. There is a mix of fulltime and part-time staff. The total reported full-time equivalent of dedicated PR personnel is 1.9.
Of the 27 sites contacted in the South East LHIN, 13 responded to our survey (response rate of 48%). Of these, 12 do not have a PR program. However, 8 did report having some structured services for patients with COPD. While no services are offered universally, smoking cessation counselling and nutritional support were the most commonly reported services. Strength and breathing training is offered by 1 site, and no sites offer exercise training/educational services. All of the non-PR sites reported that they refer patients to only 2 PR centres, including the PR centre that responded to our survey. The other centre that the non-PR sites refer to did not respond to our survey.
Despite having only 1 PR centre's response to use for analysis of this LHIN, we received a good response from non-PR sites across the LHIN; therefore, we can compare patient referrals and offered services, and we can conclude that our findings provide an accurate depiction of the PR services within the South East LHIN.
LHIN Profile 11: Champlain
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 712,103 | 26,347 (3.7) | 72,634 (10.2) |
| LHIN Characteristic | Value | |
| Responding PR centres | 6 | |
| Program types (outpatient, inpatient, maintenance) | 5 outpatient, 2 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A major centre serving a population > 200,000 | 1 of 6 responding centres | |
| A centre serving a population of 50,000–100,000 | 2 of 6 responding centres | |
| A centre serving a population of 10,000–50,000 | 2 of 6 responding centres | |
| Typical hours of operation | 3 full-time, 2 part-time (2–4 hours Tue, Wed, Thu, Fri; 2 hours Mon, Wed) | |
| Mean outpatient program wait time, days | 105 days | |
| Mean outpatient program length | 19 weeks | |
| Reported COPD patients through program annually | 434 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.60%–1.65% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The Champlain LHIN has a prevalence of COPD very similar to the 3.8% mean for Ontario. (37) One survey response was returned with several questions incomplete. The outpatient PR programs vary in length; the majority are 12 weeks or less in duration, and 1 is 50 weeks. The maintenance programs were both at least 50 weeks long. The PR programs are spread across all types of facilities: 3 in hospitals, 1 in a family health team, and 2 in community health centres. The PR centres are spread across the LHIN, and 50% operate on a full-time schedule; the part-time sites operate 2 or 4 days per week for only a few hours each day. Eighty percent of the sites allow current smokers entry to their programs. Four of the 6 programs are funded by government, and 1 is funded by the Champlain LHIN itself. Some of the PR centres reported having maintenance components to their programs. Of these, there was a mix of centres that did and did-not make use of community resources and infrastructure, such as local gyms, YMCA, community centre, and local schools. The PR centres without a maintenance component have a similar mix of use and non-use of community resources.
The PR centres with fewer employees prefer to have either entirely full-time or entirely part-time staff, while the PR centres with many employees have a mix of full-time and part-time. More than 80% of centres employ respiratory therapists; physical therapists and nurses are the next most common personnel on PR teams (50%). The total reported full-time equivalent of dedicated PR personnel across the LHIN is 15.8.
Of the 54 sites contacted in the Champlain LHIN, 22 responded to our survey (response rate of 41%). Of these, 16 do not have a PR program. However, 10 of these reported having some structured services for patients with COPD. The most commonly reported services are smoking cessation counselling, chronic disease management, and nutritional support. The least commonly offered services are strength and breathing training and exercise training/education, offered by only 1 or 2 sites across the LHIN. Of the 6 PR centres that we captured in our survey, 4 receive referrals and 2 do not. In addition, the non-PR sites reported referring patients to 3 other centres that did not respond to our survey.
With responses from 6 PR centres and 16 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the Champlain LHIN.
LHIN Profile 12: North Simcoe Muskoka
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 270,492 | 15,147 (5.6) | 30,836 (11.4) |
| LHIN Characteristic | Value | |
| Responding PR centres | 3 | |
| Program types (outpatient, inpatient, maintenance) | 3 outpatient, 2 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A regional centre serving a population of 100,000–200,000 | 1 of 3 responding centres | |
| A centre serving a population of 50,000–100,000 | 1 of 3 responding centres | |
| A centre serving a population of 10,000–50,000 | 1 of 3 responding centres | |
| Typical hours of operation | Full-time | |
| Mean outpatient program wait time, days | 40 days | |
| Mean outpatient program length | 14 weeks | |
| Reported COPD patients through program annually | 94 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.31%–0.62% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The North Simcoe Muskoka LHIN has a higher COPD prevalence than the 3.8% provincial mean. (37) The outpatient programs range from 7 to 24 weeks long, and the maintenance programs run for almost a year (48 weeks). Sixty-six percent of the programs are based in family health teams, while the others are based in hospitals. The PR centres are spread across the LHIN's geographic distribution and they are each located in different catchment sizes. All programs operate full-time and all sites allow current smokers to participate. The programs are primarily government funded; 1 supplements this through patient participation fees. Distance in location and availability of private transportation were reported to be the 2 most important barriers to patient participation. Weather also plays a significant role in preventing patients from participating in 2 of the centres. The PR programs do not generally use community resources or infrastructure in their maintenance components.
Respiratory therapists, pharmacists, and dietitians are members of the PR teams at all the centres. Other personnel found on the PR teams of the LHIN are nurses, respirologists, social workers, and physical therapists. The PR centres reported a mix of part-time and full-time staff. We could not determine the total reported full-time equivalent of dedicated PR personnel across the LHIN as this information was missing for more than 60% of staff listed in the survey responses.
Of the 13 sites contacted in the North Simcoe Muskoka LHIN, 6 responded to our survey (response rate of 46%). Of these, 3 do not have a PR program. However, 2 of these did report offering some structured services to patients with COPD. Both sites offer services on chronic disease management, self-management, nutritional support, psychosocial support, and smoking cessation counselling. Neither offer exercise training/education or strength and breathing services. The non-PR sites reported referring patients to 1 of the full PR centres that responded to our survey, and there were no extra sites that the survey did not capture. However, we did receive responses from 2 other full PR centres that were not referred to by the non-PR sites.
With responses from 3 PR centres and 3 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the North Simcoe Muskoka LHIN.
LHIN Profile 13: North East
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 345,070 | 21,049 (6.1) | 46,239 (13.4) |
| LHIN Characteristic | Value | |
| Responding PR centres | 4 | |
| Program types (outpatient, inpatient, maintenance) | 4 outpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A regional centre serving a population of 100,000–200,000 | 3 of 4 responding centres | |
| A centre serving a population of 10,000–50,000 | 1 of 4 responding centres | |
| Typical hours of operation | 3 full-time, 1 part-time (2–3 hours Mon, Wed, Thu) | |
| Mean outpatient program wait time, days | 43 days | |
| Mean outpatient program length | 6–46 weeks | |
| Reported COPD patients through program annually | 912 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 1.97%–4.33% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The North East LHIN has a higher prevalence of COPD than the 3.8% mean for the province. (37) However, the PR programs of the North East LHIN report serving a higher percentage of patients (2.70%) compared to the previous provincial estimate (1.15%). (13) The PR outpatient programs vary in length from 6 to 46 weeks. The maintenance program runs for 16 weeks. Half of the outpatient programs are hospital-based and the other half are based in family health teams. They are primarily located in larger catchment areas in the southern half of the LHIN's geographic distribution. Seventy-five percent of centres operate full-time, while 25% are only open a few days each week. All the PR centres allow current smokers to participate in their programs. Funding for the programs comes through several sources: government, patient fees, private insurance, and proceeds from other services (e.g., continuous positive airway pressure and oxygen treatment). Most centres reported that lack of public or private transportation is a barrier to participation; other barriers reported to be important were wait times due to shortage of staff, organization capacity, patient fees, and distance that patients must travel. Seventy-five percent of centres do not have a maintenance component, and those that do have a maintenance component generally do not make use of community resources.
Nurses, kinesiologists, and physical therapists are the most common health care professionals represented on the PR teams within the LHIN. A wide range of other team members were reported, including nurse practitioners, dietitians, general practitioners, social workers, and physiotherapists. Employment in the LHIN is a mix of full-time and part-time. The total reported full-time equivalent of dedicated PR personnel across the LHIN is 27.
Of the 61 sites contacted in the North East LHIN, 22 responded to our survey (response rate of 38%). Of these, 18 do not have a PR program. However, 14 non-PR sites did report having some structured services for patients with COPD. There were no universally offered services by non-PR sites, but the most commonly offered are smoking cessation counselling and self-management, and the least offered are exercise training/education and strength and breathing training. The non-PR sites reported referring patients to only 1 of the PR centres that responded to our survey. The non-PR sites reported referring patients to other LHINs (Champlain and Toronto Central).
With responses from 4 PR centres and 18 non-PR centres spread across the LHIN, we can conclude that our findings likely provide an accurate depiction of the PR services within the North East LHIN.
LHIN Profile 14: North West
| 2011 Canadian Census Estimated Population ≥ 35 Years of Age | 2011 Census COPD Estimate, n (%) | 2011 ICES COPD Estimate, n (%) |
|---|---|---|
| 137,754 | 5,647 (4.1) | 16,805 (12.2) |
| LHIN Characteristic | Value | |
| Responding PR centres | 1 | |
| Program types (outpatient, inpatient, maintenance) | 1 outpatient, 1 maintenance | |
| Catchment sizes of responding centres in LHIN | ||
| A regional centre serving a population of 100,000–200,000 | 1 of 1 responding centres | |
| Typical hours of operation | Part-time (afternoons Mon, Tue, Wed, Fri) | |
| Mean outpatient program wait time, days | 35 days | |
| Mean outpatient program length | 8 weeks | |
| Reported COPD patients through program annually | 120 | |
| Range of LHIN's COPD capacity (% COPD population in PR) | 0.71%–2.13% | |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICES, Institute for Clinical Evaluative Sciences; LHIN, local health integration network; PR, pulmonary rehabilitation.
The North West LHIN has a higher prevalence of COPD than the 3.8% mean for the province. (37) Only 1 site that provides PR responded to our survey, so the summary of PR services within the North West LHIN is based on this site. The centre that responded offers an outpatient program with a length of 8 weeks and a maintenance program with no reported length. The programs operate part-time, primarily in the afternoon for 4 days per week, and they have a total patient wait time of 35 days. The program is funded by government and out-of-pocket participation fees from the patients. Availability of private and public transportation, distance in location, cost of gas, and parking were all reported to be very important barriers to patient participation in the program. The program does not accept patients who currently smoke. The site offers maintenance once patients have completed the program, but it does not generally use community resources or infrastructure for maintenance activities.
The health care professions represented on the PR team were reported as respiratory therapist, physical therapist, and rehabilitation assistant. The team employment is split into full-time and part-time. The total reported full-time equivalent of dedicated PR personnel of the LHIN is 1.4.
Of the 33 sites contacted in the North West LHIN, 15 responded to our survey (response rate of 46%). Of these, 14 do not have a PR program. However, 9 non-PR sites did report having some structured services for patients with COPD. While no PR services are offered universally, chronic disease management, smoking cessation counselling, and nutritional support are offered most often. None of the non-PR sites offer exercise training/education or strength and breathing education. The 1 PR centre that responded to our survey receives referrals from the non-PR sites that responded.
The non-PR centres of the LHIN did not report referring patients to any PR centres that the survey did not capture. This, in conjunction with the geographic distribution of responding sites across the LHIN, allows us to conclude that our findings provide an accurate depiction of the PR services within the North West LHIN.
REFERENCES
- (1).O'Donnell DE, Hernandez P, Kaplan A, Aaron S, Bourbeau J, Marciniuk D, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2008 update – highlights for primary care [Internet]. Can Respir J. 2008. Jan;15 Suppl A: 1–8A. [cited 2013 Sep 9]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2802325/pdf/crj15001a.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Mayo Clinic Staff. Diseases and conditions: COPD [Internet]. Mayo Foundation for Medical Education and Research; [updated 2014; cited 2014 Aug 10]. Available from: http://www.mayoclinic.org/diseases-conditions/copd/basics/definition/con-20032017 [Google Scholar]
- (3).Fast facts about chronic obstructive pulmonary disease (COPD) 2011 [Internet]. Ottawa: Public Health Agency of Canada; 2012. [cited 2013 Feb 11]. Available from: http://www.phac-aspc.gc.ca/cd-mc/publications/copd-mpoc/ff-rr-2011–eng.php. [Google Scholar]
- (4).Mittmann N, Kuramoto L, Seung SJ, Haddon JM, Bradley-Kennedy C, Fitzgerald JM. The cost of moderate and severe COPD exacerbations to the Canadian healthcare system. Respir Med. 2008. Mar; 102(3): 413–21. [DOI] [PubMed] [Google Scholar]
- (5).Health Statistics Division, Statistics Canada. Chronic obstructive pulmonary disease in Canadians, 2009 to 2011 [Internet]. Ottawa: Minister of Industry; 2012. [cited 2014 Jul 17]. Available from: http://www.statcan.gc.ca/pub/82-625-x/2012001/article/11709-eng.pdf. [Google Scholar]
- (6).Statistics Canada. Chart 1, Self-reported versus measured COPD, by sex, household population aged 35 to 79, Canada, 2009 to 2011 [Internet]. Ottawa: Statistics Canada; 2013. [cited 2014 Jul 6]. Available from: http://www.statcan.gc.ca/pub/82-625-x/2012001/article/c-g/desc/11709-01-desc-eng.htm. [Google Scholar]
- (7).Gershon AS, Wang C, Wilton AS, Raut R, To T. Trends in chronic obstructive pulmonary disease prevalence, incidence, and mortality in Ontario, Canada, 1996 to 2007: a population-based study [Internet]. Arch Intern Med. 2010. Mar 22; 170(6): 560–5. [cited 2014 Jul 6]. Available from: http://dx.doi.org/10.1001/archinternmed.2010.17. [DOI] [PubMed] [Google Scholar]
- (8).Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013. Oct 15; 188(8): e13–64. [DOI] [PubMed] [Google Scholar]
- (9).Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006; (4): CD003793. [DOI] [PubMed]
- (10).Brooks D, Sottana R, Bell B, Hanna M, Laframboise L, Selvanayagarajah S, et al. Characterization of pulmonary rehabilitation programs in Canada in 2005 [Internet]. Can Respir J. 2007. Mar; 14(2): 87–92. [cited 2013 Jul 25]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2676378/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Marciniuk DD, Brooks D, Butcher S, Debigare R, Dechman G, Ford G, et al. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease–practical issues: a Canadian Thoracic Society Clinical Practice Guideline [Internet]. Can Respir J. 2010. Jul; 17(4): 159–68. [cited 2013 Sep 9]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2933771/pdf/crj17159.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).OHTAC COPD Collaborative. Chronic obstructive pulmonary disease (COPD) evidentiary framework [Internet]. Ont Health Technol Assess Ser. 2012;12 (2): 1–97. [cited 2013 Sep 9]. Available from: http://www.hqontario.ca/en/mas/tech/pdfs/2012/rev_COPD_Framework_March.pdf. [PMC free article] [PubMed] [Google Scholar]
- (13).Hailey D, Jacobs P, Stickland M, Chuck A, Marciniuk DD, Mayers I. et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease: clinical, economic, and budget impact analysis [Internet]. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2010. [cited 2013 Sep 9]. Available from: http://www.cadth.ca/media/pdf/H0482_COPD_tr_e.pdf. [Google Scholar]
- (14).Ontario Health Technology Advisory Committee (OHTAC). OHTAC recommendation: chronic obstructive pulmonary disease (COPD) [Internet]. Toronto, ON: Queen's Printer for Ontario; 2012; [cited 2013 Sep 9]. Available from: http://www.hqontario.ca/en/mas/pdfs/COPD_OHTACRecommendation_March2012.pdf. [Google Scholar]
- (15).Kida K, Jinno S, Nomura K, Yamada K, Katsura H, Kudoh S. Pulmonary rehabilitation program survey in North America, Europe, and Tokyo. J Cardiopulm Rehabil. 1998. Jul; 18(4): 301–8. [DOI] [PubMed] [Google Scholar]
- (16).Bickford LS, Hodgkin JE. National pulmonary rehabilitation survey. J Cardiopulmonary Rehabil. 1988. Nov; 8(11): 473–91. [PubMed] [Google Scholar]
- (17).Bickford LS, Hodgkin JE, McInturff SL. National pulmonary rehabilitation survey. Update. J Cardiopulm Rehabil. 1995. Nov; 15(6): 406–11. [DOI] [PubMed] [Google Scholar]
- (18).Brooks D, Lacasse Y, Goldstein RS. Pulmonary rehabilitation programs in Canada: national survey. Can Respir J. 1999. Jan; 6(1): 55–63. [PubMed] [Google Scholar]
- (19).Johnston CL, Maxwell LJ, Alison JA. Pulmonary rehabilitation in Australia: a national survey. Physiotherapy. 2011. Dec; 97(4): 284–90. [DOI] [PubMed] [Google Scholar]
- (20).Garvey C, Fullwood MD, Rigler J. Pulmonary rehabilitation exercise prescription in chronic obstructive lung disease: US survey and review of guidelines and clinical practices. J Cardiopulm Rehabil Prev. 2013. Sep; 33(5): 314–22. [DOI] [PubMed] [Google Scholar]
- (21).Levack WM, Weatherall M, Reeve JC, Mans C, Mauro A. Uptake of pulmonary rehabilitation in New Zealand by people with chronic obstructive pulmonary disease in 2009 [Internet]. N Z Med J. 2012. Jan 20; 125(1348): 23–33. [cited 2013 Sep 11]. Available from: http://journal.nzma.org.nz/journal/125-1348/5018/content.pdf. [PubMed] [Google Scholar]
- (22).Motegi T, Yamada K, Ishii T, Gemma A, Kida K. Long-term management of chronic obstructive pulmonary disease: a survey of collaboration among physicians involved in pulmonary rehabilitation in Japan. Respir Investig. 2012. Sep; 50(3): 98–103. [DOI] [PubMed] [Google Scholar]
- (23).O'Neill B, Elborn J, MacMahon J, Bradley JM. Pulmonary rehabilitation and follow-on services: a Northern Ireland survey. Chron Respir Dis. 2008; 5(3): 149–54. [DOI] [PubMed] [Google Scholar]
- (24).Puhan M, Koller M, Brandli O, Steurer J. Pulmonary rehabilitation of COPD in Switzerland–an assessment of current status [in German]. Praxis (Bern 1994). 2003. Jan 22; 92(4): 111–6. [DOI] [PubMed] [Google Scholar]
- (25).Wadell K, Janaudis FT, Arne M, Lisspers K, Stallberg B, Emtner M. Hospital-based pulmonary rehabilitation in patients with COPD in Sweden–a national survey. Respir Med. 2013. Aug; 107(8): 1195–200. [DOI] [PubMed] [Google Scholar]
- (26).Yohannes AM, Connolly MJ. Pulmonary rehabilitation programmes in the UK: a national representative survey. Clin Rehabil. 2004. Jun; 18(4): 444–9. [DOI] [PubMed] [Google Scholar]
- (27).Weiser PC, Ryan KP. Tri-State Regional Pulmonary Rehabilitation Survey. Program characteristics and practices. J Cardiopulm Rehabil. 1995. May; 15(3): 197–208. [DOI] [PubMed] [Google Scholar]
- (28).Weiser PC, Ryan KP. Tri-state region pulmonary rehabilitation survey. Delivery of exercise conditioning services. The Pulmonary Rehabilitation Committee, Tri-State Society for Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehabil. 1996. May; 16(3): 175–82. [DOI] [PubMed] [Google Scholar]
- (29).Deturk WE, Scott LB. Physical therapists as providers of care: exercise prescriptions and resultant outcomes in cardiac and pulmonary rehabilitation programs in New York state [Internet]. Cardiopulm Phys Ther J. 2008. Jun; 19(2): 35–43. [cited 2013 Sep 11]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2845219/. [PMC free article] [PubMed] [Google Scholar]
- (30).Canadian Lung Association. Find a pulmonary rehabilitation program [Internet]. Ottawa: The Association; 2012. [cited 2014 Jul 17]. Available from: http://www.lung.ca/respDB/search-pulmonary-rehabilitation_e.php. [Google Scholar]
- (31).Whitaker J. Pulmonary rehabilitation programs (for COPD) in Canada [Internet]. COPD Canada. 2013. [cited 2014 Jul 17]. Available from: http://copdcanada.ca/Pulmonary%20Rehabilitation%20Facilities%20for%20COPD%20in%20Canada.htm.
- (32).Statistics Canada. Table 109-5325. Estimates of population (2006 Census and administrative data), by age group and sex for July 1, Canada, provinces, territories, health regions (2011 boundaries) and peer groups annual (number), CANSIM (database) [Internet]. Ottawa: Statistics Canada; 2013. [cited 2013 Feb 11]. Available from: http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=1095325&paSer=&pattern=&stByVal=1&p1=1&p2=1&tabMode=dataTable&csid=. [Google Scholar]
- (33).Gershon A, To T, Guan J, Victor C, Wilton A, Ho M. et al. Prevalence of chronic obstructive pulmonary disease, Ontario 1996/97 to 2009/10 [Internet]. Toronto: Institute for Clinical Evaluative Sciences (ICES); 2010. [cited 2014 Feb 14]. Available from: http://www.ices.on.ca/file/COPD_Prevalence_Statistics_96to09_final.pdf.
- (34).Health profile – select from a list [Internet]. Ottawa: Statistics Canada; 2013. [cited 2014 Jan 26]. Available from: http://www12.statcan.gc.ca/health-sante/82-228/search-recherche/lst/page.cfm?Lang=E&GeoLevel=PR&GEOCODE=35. [Google Scholar]
- (35).Spruit MA, Pitta F, Garvey C, Zuwallack RL, Roberts CM, Collins EG, et al. Differences in content and organisational aspects of pulmonary rehabilitation programmes. Eur Respir J. 2014. May; 43(5): 1326–37. [DOI] [PubMed] [Google Scholar]
- (36).Gilmartin ME. Pulmonary rehabilitation. Patient and family education. Clin Chest Med. 1986. Dec; 7(4): 619–27. [PubMed] [Google Scholar]
- (37).Health profile, December 2013 [Internet]. Ottawa: Statistics Canada; 2013. [cited 2014 Jan 26]. Available from: http://www12.statcan.gc.ca/health-sante/82-228/index.cfm?Lang=E. [Google Scholar]