Abstract
Aim
To conduct a systematic review on the prevalence, risk factors, treatments and outcomes of Coronary Artery Disease (CAD) in Indians.
Methods and results
We conducted a systematic review of studies in Indians with CAD from Jan 1969 to Oct 2012.
Initial search yielded 3885 studies and after review 288 observational studies were included. The prevalence of CAD in urban areas was 2.5%–12.6% and in rural areas, 1.4%–4.6%. The prevalence of risk factors was: smoking (8.9–40.5%), hypertension (13.1–36.9%) and diabetes mellitus (0.2–24.0%). The median time to reach hospital after an MI was 360 min. In hospital rates of drug use were: antiplatelets 68%–97.9%, beta blockers 47.3%–65.8% and ACEIs 27.8–56.8%.
Conclusions
In this first systematic review of CAD in India, prevalence of risk factors is high, treatments delayed and use of evidence based treatments variable.
Keywords: Coronary artery disease, Prevalence, Risk factors, Outcomes, India
1. Introduction
The burden of cardio vascular disease (CVD) is on the rise globally. Cardiovascular deaths account for 30% of deaths world wide.1 The burden of CVD is projected to be the highest in India by the year 2020, as compared to other countries.2 In the WHO-PREMISE study, the proportion of coronary heart disease (CHD) among patients less than 50 years of age, was highest in India (22.6% in males and 3% in females).3 In the Million Death Study (2009) the authors determined that cardiovascular diseases are the leading cause of death (20.3% in males and 16.9% in females) among Indian adults (age 25–69 years).4 Yet it is difficult to get a comprehensive picture of the epidemiology and disease burden of coronary artery disease (CAD) in India. One systematic review of 31 studies in India reported that the prevalence of CAD is higher in urban as compared to the rural areas (Men 35–90/1000 vs. 17–45/1000; Women 28–93/1000 vs. 13–43/1000).5
In order to implement nation-wide policies to control CAD, we need a comprehensive view of its different aspects such as the disease burden, manifestations, treatment patterns and outcomes of the condition. We therefore conducted a systematic review of all the observational studies to record the available evidence on the epidemiology, risk factors, clinical presentations, management and outcomes of coronary artery disease among Indians residing in India.
2. Methods
A systematic review of all studies in Asian Indians with coronary artery disease addressing the epidemiology, risk factors, clinical presentations, management or outcomes of CAD among Indians.
2.1. Studies included
We included all studies from January 1969 to October 2012, pertaining to coronary artery disease and its treatments. The diagnosis of coronary artery disease was not uniform across different studies. The diagnosis was based on history of angina or myocardial infarction or electrocardiographic findings. Treatment of CAD included both prescribed drugs (in hospital based studies) and self-reported use of medications (in community based studies). We only included studies in English. As English is the primary medium of scientific communication in India, we are confident that we have been able to include all the relevant studies in this review. Amongst the studies that were excluded were: articles without original data (letters to the editor, comment and narrative review); studies conducted among Indians residing outside India and international studies without separate data on Indians.
2.2. Search strategy and data extraction
Two independent reviewers conducted a systematic search of Medline as well as extensive hand searches using the following pre-specified MeSH terms and search strategies: Search #1: Heart diseases OR myocardial ischemia OR coronary disease OR coronary artery disease OR coronary arteriosclerosis OR coronary atherosclerosis OR Ischemic Heart Disease; Search # 2: India OR Indians OR South Asia; and Search #3: combined #1 and # 2.
Duplicates were removed using Reference Manager (version 12). Relevant studies were selected for data extraction based on pre-specified eligibility criteria. Disagreements between the two reviewers on the selection of articles were resolved by discussions with a third reviewer.
We assessed study quality using parameters specified in the STROBE statement.6 The parameters for different observational study designs were specified and are described here. For cohort studies we used indicators of eligibility criteria, source of cohort, methods of selection, and methods of follow up. The maximum score was 4 and minimum was 0. For case–control and cross-sectional studies the parameters included were as follows: eligibility criteria, ascertainment of cases and controls and the rationale for the choice of cases and controls. For cross sectional studies, eligibility specified, ascertainment of cases and rationale for inclusion of cases, were the parameters. The maximum score possible was 3 and the minimum was 0. Using a structured format, the following data were independently extracted: year, type of study, sample size, patient characteristics, incidence, prevalence, risk factors, manifestations, treatments and outcomes of CAD.
3. Results
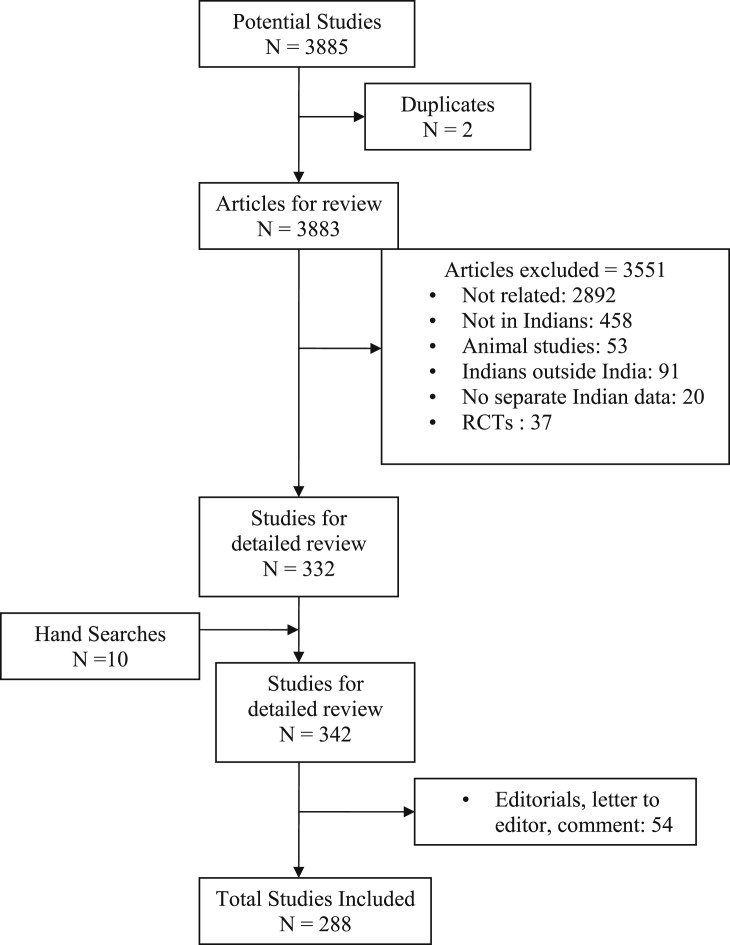
The initial search yielded 3885 studies. Of these, a total of 111 studies were excluded as they were either studies with Indians combined with other South Asians (20) or studies conducted among Indians living outside India (91). We found 37 RCTs in our search and none of them looked at clinical outcomes. After removing duplicates and reviewing the title and abstract for relevance, 342 observational studies were identified. Fifty four of the 342 articles were editorials, letter to the editor, comment and did not contain original data. We extracted data from 288 observational studies (cohort 12 [4.2%], case control 57 [19.8%], cross sectional 180 [62.5%] and mixed methods 39 [13.5%]) (Fig. 1). Of these there were sufficient data in 59 studies for further analyses (Chi-squared and time trend analysis).
Fig. 1.
Flow chart of included studies.
3.1. Quality of the studies included (Table 1)
Table 1.
Summary of Quality scores of Observational studies.
| Quality score | Observational studies n = 194 (%) |
|---|---|
| 4 | 2(1.03) |
| 3 | 49(25.2) |
| 2 | 131(67.5) |
| 1 | 12(6.1) |
Among the observational studies (288), we were able to assess the quality for 194 (68.3%) studies that had evaluable data. The data were insufficient to assess the quality in other studies. Of the 194 studies, 131 (67.5%) studies scored 2, and only 2 studies (1.0%) obtained the maximum score of 4.
3.2. Incidence and prevalence of CAD
There were two community based studies that had data on the incidence of CAD. The study by Chadha et al in 1993 conducted in urban Delhi included 4151 subjects (25–64 years of age) and followed up for 3 years, reported an incidence of CAD as 19.7/1000 (male 17.3 and female 21.0).7 The study by Trivedi et al in rural population of Gujarat included 714 subjects (30–62 years of age), followed up for 5 years estimated the CAD incidence of 25.1/1000.8
There were 18 cross sectional studies conducted in various parts of India between 1990 and 2012. In 12 of these studies from urban areas among adults aged above 20 years (1990–2012, sample size [SS] from 534 to 13,723), the prevalence ranged from 2.5% to 12.6%. In 7 of these studies in rural areas (1993–2009, SS from 812 to 3148), the prevalence ranged from 1.4% to 4.6%. The prevalence of CAD among males in urban areas was 2.8 %–7.9% in 11 studies and 2.2%–15.8% among females in 9 studies (1990–2012). In rural areas the prevalence was 3.1%–6.9% in males and 1.7%–4.6% in females (1994–2009). There was a significant positive trend in the overall prevalence of CAD in urban (Mantel–Haenszel Chi squared value 299.99, p < 0.0001) and rural areas (Mantel–Haenszel Chi squared value 19.74, p < 0.0001). The diagnosis of CAD in these studies was not uniform. It was based on past history, ECG changes or the Rose questionnaire (Table 2). Prevalence of CAD as reported by ECG changes, were low: 5.2% in urban areas9 and 3.1–4.4% in rural areas.10–12
Table 2.
Studies reporting prevalence of CHD and criteria for diagnosis by year.
| Authors | Year | Place | S size | Age (yrs) | CHD % | Male | Female | cCHD diagnosis criteria |
|---|---|---|---|---|---|---|---|---|
| Urban (U) | ||||||||
| Chadha SL38a | 1990 | Delhi | 13723 | 25–64 | 3.2 | 3.9 | 2.5 | Clinical history |
| Chadha SL39a | 1992 | Delhia | 1317 | 25–64 | 2.5 | 2.8 | 2.2 | Clinical history |
| Gupta R9 | 1995 | Jaipur | 2212 | ≥20 | 7.6 | 6.0 | 10.4 | Past doc, Rose q or ECG changes |
| 5.2 | 3.5 | 8.4 | Q, ST or T wave | |||||
| bGupta R18 | 1996 | Rsthan | 3397 | NA | 4.5 | 6.0-U 3.4-R |
NA | Clinical history and ECG |
| RChdrn A40a | 1998 | Chennai | 953 | ≥40 | 3.9 | 3.5 | 4.5 | Clinical history or ECG (Q wave, ST changes) |
| Mohan V41a | 2001 | Chennai | 1175 | ≥20 | 11 | NA | NA | Clinical history or ECG (ST,T and Q changes |
| Gupta R42a | 2002 | Jaipur | 1123 | ≥20 | NA | 6.2 | 10.1 | Clinical history ± ECG (ST,T and Q changes) |
| Gupta R43a | 2002 | Rsthan | 2212 | >20 | NA | 7.1 H 1.8 M |
10.4 H 6.6 M |
Clinical history or ECG (ST and T changes) |
| D Prabhakaran28 | 2005 | Delhi | 2122 | 20–59 | NA | 7.3 | NA | Clinical history or ECG (ST, T and Q changes) |
| Latheef SA44a | 2007 | Tirupathi | 1519 | >20 M 42.5 ± 9.4 F 38.8 ± 11.2 |
12.6 | 6.8 | 15.8 | Clinical history & ECG (ST or Q wave changes or T changes) |
| bKamili M45a | 2007 | Kashmiris | 3128 | ≥40 | 7.5 8.4 U 6.7 R |
7.9 | 6.6 | Past doc, Rose q or ECG (ST and T changes) |
| Murthy PD46a | 2012 | AndraP | 534 | ≥20 | 5.4 | 7.7 | 3.6 | History or ECG (ST or Q wave changes) |
| Rural(R) | ||||||||
| Kutti VR10 | 1993 | Tpuram | 1130 | >25 | 1.4 | NA | NA | Definitive evidence of CHD |
| Gupta R11 | 1994 | C Rsthan | 1150 | 53 ± 4.6 | 4.6 | 4.6 | 4.6 | Clinical history ± ECG ST and T wave changes ± Rose Q |
| Wander GS12 | 1994 | Punjab | 1100 | >30 | 3.2 | 3.1 | 3.4 | History, ECG and TMT |
| Gupta R47a | 1997 | Rsthan | 3148 | ≥20 | NA | 3.4 | 3.7 | Clinical + ECG (Q, ST or T changes) |
| Clara Chow48a | 2007 | AndraP | 345 | 20–90 | 2.5 | NA | NA | previous heart attack, stroke or angina |
| Rajeev B49a | 2009 | H Pradesh | 812 | >30 | 4.1 | 6.9 | 1.7 | Hosp. records, TMT,ECG changes, Cor. Angiography |
(Mantel–Haenszel Chi squared value for urban 299.99, p < 0.0001) (Mantel–Haenszel Chi squared value for Rural 19.74, p < 0.0001). NA: Not Available, H: Hindus, M: Muslims.
Rsthan – Rajasthan, C Rsthan – Central Rajasthan, Tpuram – Tiruvananthapuram, AndraP – Andhra Pradesh, H Pradesh – Himachal Pradesh.
Reference numbers 38a–49a are provided in the supplementary data.
Gujaratis.
Includes both urban and rural areas.
Studies used different criteria for the diagnosis of CHD.
3.3. Risk factors (Table 3)
Table 3.
Prevalence (in %) of risk factors for CHD among community and patients from various studies.
| Risk factors | Prevalence in community % | No. of studies | Prevalence in patients from CS studies | No. of studies |
|---|---|---|---|---|
| Hypercholesterolemia | 7.0–30.0 | 99,12,28,44a,50a−53a,65a,66a | 15.0–46.2 | 643a,55a−58a,63a |
| Decreased HDL | 31.0–55.0 | 542a,44a,51a,53a,66a | NA | |
| Increased TG | 29.2–45.9 | 542a,44a,51a,53a,66a | NA | |
| Increased LDL | −21.5–41.5 | 342a,53a,66a | NA | |
| Smoking | 8.9–40.5 | 89,10,12,28,47a,48a,52a,53a,65a,66a | 16.5–87.0 | 1022,24,25,57a−59a,61a,63a,64a,67a |
| Hypertension | 13.1–36.9 | 1110,12,28,42a,44a,47a,48a,51a−53a,65a,66a | 15.0–54.3 | 422,24,25,57a |
| Diabetes | 0.2–24.0 | 119,10,12,28,42a,44a,47a,48a,52a,53a,65a,66a | 5.0–44.6 | 522,24,25,57a,67a |
| Positive family history | 17.0–19.4 | 252a,54a | 8.0–40.0 | 357a,63a,68a |
NA: Not Available.
CS: Cross sectional.
Reference numbers 42a,44a,47a,48a,50-59a,61a,63a,67–68a are provided in the supplementary data.
The studies reporting the prevalence of risk factors were from 1976 to 2012. Hence the definition for each of the risk factors is different across various studies. The risk factor rates are thus reported as minimum to maximum percentages in this study. The prevalence of common risk factors in the community from cross sectional studies were as follows: hypercholesterolemia (7.0–30.0%; 10 studies 1994–2012), hypertension (13.1–36.9%; 12 studies 1993–2012) diabetes mellitus (0.2–24.0%; 12 studies 1993–2012) and smoking (8.9–40.5%; 10 studies 1993–2012). Cross sectional studies among CAD patients report the prevalence of risk factors as follows: hypercholesterolemia 15.0–46.2% (6 studies 1970–2004), smoking 16.5–87.0% (10 studies 1987–2008), hypertension 15.0–54.3% (4 studies in 1987–2008) and diabetes mellitus 5.0–44.6% (5 studies 1987–2008). There was a significant positive trend with common risk factors like smoking, hypertension, diabetes mellitus and dyslipidemia in males and females when prevalence from studies with uniform definition of risk factors were analyzed. Mantel–Haenszel Chi squared values for males: Smoking 145.52, p < 0.0001, Hypertension 103.99, p < 0.0001, Diabetes mellitus 12.64, p = 0.0004, Dyslipidemia 161.09, p < 0.0001. Mantel–Haenszel Chi squared values for females: Smoking 35.84, p < 0.0001, Hypertension 35.59, p < 0.0001, Diabetes mellitus 11.19, p = 0.0008, Dyslipidemia 12.12, p = 0.0005 (Table 4).
Table 4.
Prevalence of major risk factors (%) for CAD in community from studies with similar definitions for risk factor.
| Author | Year | Sample size | Age | Smoking |
Hypertension |
Diabetes |
Dyslipidemia |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | ||||||
| R Gupta9 | 1995 | 2212 | ≥20 | 39 | 19 | 30 | 34 | NA | NA | NA | NA |
| R Gupta47a | 1997 | 3148 | ≥20 | 51 | 5 | 24 | 17 | NA | NA | NA | NA |
| Reddy N K52a | 2002 | 3307 | 43.12 ± 9.5 | 27 | 2 | 28 | 19 | 26 | 9 | 59 | 45 |
| R Gupta53a | 2003 | 1123 | NA | 40.5 | 20.5 | 33.7 | 33.7 | 7.8 | 7.3 | 37.4 | 43.1 |
| R Gupta65a | 2007 | 1127 | ≥20 | 37 | 2.1 | 57.9 | 48.9 | 25.9 | 21.1 | 32.6 | 39.5 |
| R Gupta66a | 2012 | 739 | 20–59 | 21.1 | 4.2 | 39.5 | 24.6 | 15.5 | 10.8 | 33 | 32.7 |
NA: Not Available.
Reference numbers 47a, 52-53a, 65–66a are provided in the supplementary data.
Definitions of the risk factors.
Smoking: Users of all types of tobacco products and present & past smokers are included in studies 53a, 65a and 66a. Other studies do not mention the definitions.
Hypertension: Blood pressure of >140/90 was considered as hypertension. Diabetes mellitus: Past history or fasting blood sugar level of >126 mg%.
Dyslipidemia: Total blood cholesterol levels ≥200 mg/dl.
Mantel–Haenszel Chi squared values for males: Smoking 145.52, p < 0.0001, Hypertension 103.99, p < 0.0001, Diabetes mellitus 12.64, p = 0.0004, Dyslipidemia 161.09, p < 0.0001.
Mantel–Haenszel Chi squared values for females: Smoking 35.84, p < 0.0001, Hypertension 35.59, p < 0.0001, Diabetes mellitus 11.19, p = 0.0008, Dyslipidemia 12.12, p = 0.0005.
Of the 55 case–control studies, the key risk factors (odds ratio) were, diabetes mellitus (2.7–8.9; 5 studies 1996–2008),13–17 hypertension (2.0–4.6; 4 studies 1994–2005)11,13,14,16 and smoking (1.3–4.4; 6 studies 1994–2005).11,13–16,18 On the other hand vegetarianism (0.3; 1 study, 1996) and higher socioeconomic status (0.32 vs lower; 1 study 1996)13 were found to be protective for CAD.
3.4. Studies on acute coronary syndrome (ACS)
We identified 19 studies on different aspects of acute coronary syndrome. The studies included 51,077 patients with myocardial infarction (minimum sample size [SS] 5519 and maximum SS 25,74820) between 1972 and 2012.
3.5. Presentation and treatment
The mean age for the presentation of an acute myocardial infarction (AMI) ranged from 47 to 60 yrs in 6 studies. Anterior wall MI was the commonest presentation (50.5–71.7%, 3 studies, 1970–2008) and antero-inferior wall infarction was the least common (2.2–3.9%, 2 studies 2004–2008) (Table 5).
Table 5.
Data reporting the involvement and location of myocardial wall in patients with myocardial infarction.
| Myocardial wall | Percentage of patients |
|---|---|
| Anterior wall MI55a,24,25 | 50.5%–71.7% |
| Inferior wall MI24,25 | 39.1%–47.3% |
| Ass. right ventricular or Posterior wall MI55a,24,25 | 13.3 %–62.7% |
| Antero-inferior wall MI24,25 | 2.2%–3.9% |
Reference number 55a is provided in the supplementary data.
The time taken for onset of symptoms to reach hospital was reported to be over 24 h from a study conducted as early as 1972 (Gupta RN, SS 165).21 This interval has considerably decreased in recent studies to a median of 360 min (Xavier D 2008, SS 20,468).22 The door to needle time also has decreased over time from 210 min (Chopra KL 1990, SS 330)23 to 50 min (Xavier D 2008, SS 20,468).22 Table 6.
Table 6.
Symptoms to hospital and door to needle time in the treatment of acute myocardial infarction.
| Study | Sample | Time to hospital | Door to needle |
|---|---|---|---|
| Gupta RN 197221 | 165 | 24 H to 7 D | NM |
| Gupta SP 198169a | 158 | 4 H 55 min | NM |
| Chopra KL 199023 | 330 | NM | 210 ± 64 min. |
| Anand SS 199770a | 87 | 330(50–5760)min | 30 (17–100) min |
| Malhotra S 200371a | 104 | 8.5 ± 0.8 H | 1.2 ± 0.1 H |
| Jose VJ 200425 | 1320 | 10.8 ± 12.4 h | NM |
| Achari V 200824 | 862 | 29.2 ± 10.8 H | NM |
| Xavier D 200822 | 20,468 | 360 min | 50 (25–68) min |
NM: Not Mentioned, H: hours, D: days.
Reference numbers 69a-71a are provided in the supplementary data.
Drug use in acute MI was reported since 1997 in 6 studies. They included thrombolytics 24.7–73.0%, antiplatelets 68.0–97.9%, beta blockers 47.3–65.8%, angiotensin-converting enzyme inhibitors (ACEI) 27.8–56.8%, nitrates 59.0–86.6% and anticoagulants 70.0–81.3% (Table 7). The rates of percutaneous coronary intervention (PCI) were as follows: overall rates 7.5–11.9%20,22 and in STEMI patients 1.4–12.9%.20,22,24
Table 7.
In-hospital and post discharge drug use in patients with MI.
| Drug | Utilization in % | Year |
|---|---|---|
| Thrombolytics22,24,67a,70a,72a,20 | 24.7–73 | 1997–2012 |
| Beta blockers22,70a,72a,20 | 47.3–65.8 | 1997–2012 |
| ACE inhibitors22,70a,72a,20 | 27.8–56.8 | 1997–2012 |
| Aspirin22,70a,72a,20 | 68.0–97.9 | 1997–2012 |
| Nitrates70a,20 | 59.0–86.6 | 1997,2012 |
| Anticoagulants22,70a,20 | 70.0–81.3 | 1997,2012 |
Reference numbers 67a,70a and 72a are provided in the supplementary data.
3.6. Outcomes (Table 8)
Table 8.
Outcomes reported among AMI patients.
| Study | Year | S size | Outcome | In hospital | 30 day | 6–36 months |
|---|---|---|---|---|---|---|
| Gupta RN21 | 1972 | 165 | All cause mortality | 13.8% | NM | NM |
| Chopra KL23 | 1990 | 330 | Mortality | 4.8% | NM | NM |
| Reinfarction | NM | NM | 4.0% | |||
| Late mortality | NM | NM | 1.8% | |||
| E. George72a | 1999 | 1072 | Death | 13.6% | NM | NM |
| Cardiac failure | 15.5% | NM | NM | |||
| Reinfarction | 11.4% | NM | NM | |||
| II/III degree block | 9.2% | NM | NM | |||
| Arrhythmia | 7.2% | NM | NM | |||
| Kaul U19 | 2002 | 57 | Composite of death, MI or revascularization | NM | 12.7% | NM |
| aJose VJ25 | 2004 | 1320 | Mortality | 16.9% | NM | NM |
| Composite of death, MI, Recurrent angina | NM | 18.8% | NM | |||
| Xavier D22 | 2008 | 20468 | Death | NM | 6.7% | NM |
| Reinfarction | NM | 1.9% | ||||
| Stroke | NM | 0.5% | ||||
| a Achari V24 | 2008 | 862 | Mortality | 12.4 | NM | NM |
| PP Mohanan20 | 2012 | 25748 | Death | 3.9 | NM | NM |
| Reinfarction | 0.5 | NM | ||||
| Stroke | 0.3 | NM |
NM: Not Mentioned.
Reference number 72a is provided in the supplementary data.
Studies included only patients with STEMI.
Our systematic review identified 8 studies from 1972 to 2012 with data on clinical outcomes in patients with MI. The earliest study21(Gupta RN 1972, SS 165) reported a 13.8% in-hospital mortality and a 2012 study reported 3.9%.20 Studies in patients with STEMI reported all cause mortality of 16.9%24 in 2004 and 8.2% in 2012.20 D Xavier et al in a large study reported the following rates of outcomes: death 6.7%, reinfarction 1.9% and stroke 0.5% at the end of one month after AMI.22
3.7. Secondary prevention of CAD
There were 4 studies that reported the drug utilization in secondary prevention of CAD from 2005 to 2009. Three of these studies reported drug utilization in outpatients while the fourth was a survey in the community. The use of aspirin 82.5–94.5% vs. 14.0% and statins 38.4–69.0% vs. 5.0% was higher among outpatients as compared to that in the community. The use of beta blockers ranged from 48.1 to 69.0% and ACE inhibitors or ARBs 15.5–82.0% in outpatients (Table 9).
Table 9.
Drug use for secondary prevention of CAD.
| Study | Year | S size | Drugs | % Patients (CI) |
|---|---|---|---|---|
| Mendis S3 Bulletin of WHO (PREMISE) |
2005 | 1013 | Aspirin Beta blockers ACEI Statins |
94.5% 48.1% 41.3% 38.4% |
| Gupta R73a Outpatients |
2009 | 406 | Aspirin Beta Blockers ACEI Statins |
82.5% (78.2–86.2) 53% (48.1–57.9) 15.55 (12–19) 69% (61–77) |
| Joshi R74a ≥30 yrs Community survey |
2009 | 4535 | Aspirin BP lowering Lipid lowering |
14%(10–18) 41%(36–47) 5%(3–7) |
| Sharma K75a Stable CAD patients |
2009 | 2993 | Aspirin Beta Blockers ACEI/ARBs Statins |
91% 69% 82% 69% |
Reference numbers 73–75a are provided in the supplementary data.
4. Discussion
In a comprehensive systematic review of CAD studies from India published over 40 years, we reviewed 288 studies that fulfilled the criteria for inclusion. Multinational studies including patients from India but not reporting separate data on Indians were not included.
We used the STROBE criteria to assess quality of the studies. Overall the quality of the studies was poor. About two-thirds of the observational studies had a score of 2 and just 1.0% obtained a maximum score of 4.
We identified only 2 community based studies that reported the incidence of CAD. Chadha (1985–87)7 reported an annual incidence of 19.7/1000 over 3 years, and Trivedi8 (1987–92) reported 25.1/1000 over 5 years. These studies were done in 2 regions (Delhi and Gujarat) and thus the findings may not be applicable to the entire country.
We identified 18 studies on the prevalence of CAD (11 urban, 6 rural and 1 in both areas) conducted over 22 years (1990–2012). During this time period, we note an increase in the prevalence of CAD, both in urban (3.2% in 1990 to 12.6% in 2007) and rural areas (1.4% in 1993 to 4.0% in 2009). The increase is seen in both males and females. Even though there is an increased prevalence of CAD over the years, this data has limitations as all these studies were confined to single regions and none representative of the country. On comparison of this prevalence data with the reports from US and the UK, we found that rates are lower than those reported in Indian studies. The American Heart Association Statistics Committee and Stroke Statistics Subcommittee reports an overall prevalence of CHD in the US as 7.9% (9.1% in males and 7.0% in females) in 2006.26 In England, the British Heart Foundation reported a prevalence of 6.5% in males and 4.0% in females in 2006.27 The mean age of patients with MI in India is also lower. The studies reported the age ranging from 55.0 to 58.2 years in males and 55.7–60 years in females. The US studies reported an average age of the first MI of 65.8 for men and 70.4 years for women.26
The common risk factors identified were smoking, hypercholesterolemia, hypertension and diabetes. Even though the studies are not representative of the country, we note an increase in the prevalence of these risk factors in the community from 199310 to 2005.28
Between 1993 and 2005 we see an increase in the prevalence of smoking in communities from 21.9 to 36.0%. The European Heart Survey (EHS)29 reported a prevalence of tobacco smoking of 29.4% in 2004 for the European Region and Heart and Strokes updates 2010 reports 20.6% in 2008 in the US.30 The prevalence rate of smoking in India is higher, even in comparison with data from a developing country like the Republic of Seychelles (17.5%).31 Prevalence of hypercholesterolemia (30%, Prabhakaran D 2005) among Indians was higher compared to Seychelles (24.2%) but lower compared to 46.8% in the US.30 Hypertension (30.0%) among Indians was lower as compared to reports from other regions (39.6% in Seychelles 2004, 33.6% in the US). The prevalence of diabetes mellitus has not only increased almost 4 folds over 12 years in India (4–15%, 1993–2005) but also is higher as compared to other regions (9.3% in Seychelles in 2004 and 7.7% in the US 2006).
The data from patients with CAD, as reported in a recent study (Xavier D 2008), showed a higher prevalence of smoking (40.2%) and diabetes mellitus (30.4%) as compared to Euro Aspire III (smoking 17.0% and 25.0% diabetes) while the prevalence of hypertension is lower (37.7% vs. 56.0%).32
In patients with MI, the time from onset of symptoms to reach the hospital and door to needle has reduced considerably over the years (1972–2008) from 24 h21 to 6 h22 and from 21023 to 50 min22 respectively. These intervals are still longer as compared to recent reports from other countries (170 min and 40 min in European Heart Survey 1, 2002,33 145 min and 37 min in EHS 2, 200434 and 139 min in STEMI and 191 min in NSTEMI patients in GRACE registry 200235).
The utilization of drugs among CAD patients in hospital was reported in 6 studies. The use of antiplatelets was good (68.0–97.9%) whereas the use of other drugs like beta blockers 47.3–65.8% and ACEIs 27.8–56.8% were low in India when compared to other countries (beta blockers 81.0%, ACEIs 66.0%).35
The utilization of drugs for secondary prevention is also low in India. A study at the community level (Joshi R, 2009) reports utilization of aspirin at 14.0% and lipid lowering drugs at 5.0% for secondary prevention. This is low as compared to the overall rates of drug use among patients with CHD from the PURE study36 (antiplatelets 25.8% and statins 16.7%). PURE study also reports low rates of drug use in participants from low income countries which include India (antiplatelet drugs 11.0%, ACE inhibitors or ARBs 6.5% and statins 4.5%).
There were very few studies with data on outcomes in patients with MI. In-hospital mortality after MI has decreased from 13.3% in 1972, 13.6% in 1999 to 3.9% in 2012. Mortality in STEMI patients was reported to be 12.4% in 200824 which decreased to 8.2% in 2012.20 The mortality rates have reduced over the years, but studies from developed countries report lower mortality rates. A follow up of the patients in the GRACE registry reported a decline in hospital mortality from 8.4% in 1999 to 4.6% in 2005.37
There are limitations in our systematic review. The search was limited to PubMed. There is therefore a possibility that we missed identifying some studies. Though 288 observational studies were reviewed, collation and analysis of data could be conducted only from 59 studies. This is because data from other studies were either incomplete or were primarily from patients with other conditions (eg. diabetes, rheumatic heart disease etc.) with only a mention of CAD. Even though these studies looked at various aspects of CAD, the objectives and the patient population included were different in each study.
5. Conclusions
This is the first systematic review of CAD in India that is comprehensive and covers a wide range of issues. We have found that single centre and regional studies report a high prevalence of CAD and high rates of risk factors. Patients take a long time to get to hospital, treatment for ACS is delayed, in-hospital use of evidence-based treatments is variable and post discharge rates of drug use are low. Hospital and short term mortality rates in ACS patients are high in observational studies. There are only a few high quality studies, and none representative of the country. There are no long-term studies to inform chronic management of CAD. Therefore to counter the burgeoning epidemic of CAD in India, we urgently need high quality, representative and long term studies addressing different issues. These studies should lead to programs for the reduction of risk factors and improved treatments to reduce the burden of CAD in India.
Funding
This work was supported by an unrestricted educational grant from AstraZeneca, India and partly funded by the Division of Clinical Research and Training (DCRT), St. John's Research Institute, Bangalore.
Conflicts of interest
Possible conflicts of interest (including financial and other relationships) for each author include the following: Drs. Xavier, Pais and Sigamani have received research funds from AstraZeneca, India. Dr. Pais has received consultancy fees from AstraZeneca. All three of them received these funds in to the Institution (St. John’s) account. Other authors declare no conflict of interest.
Acknowledgments
The authors gratefully acknowledge the contribution of Ms. Puneet Kaur and Ms. Nidhi Rai, from the DCRT, St. John's Research Institute for assistance in literature search and data extraction. We thank Ms. Nisha George for statistical assistance and that of Dr. Annalakshmi J. at St John's Medical College, Bangalore for support with manuscript preparation.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2015.05.003.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J.L., editors. Global Burden of Disease and Risk Factors. Oxford University Press; New York: 2006. [Google Scholar]
- 2.Murray C.J., Lopez A.D. Investing in Health Research and Development: Report of the Ad Hoc Committee on Health Research Relating to Future Intervention Options. World Health Organization; Geneva, Switzerland: 1996. Global patterns of cause of death and burden of disease in 1990, with projections to 2020; pp. 133–186. [Google Scholar]
- 3.Mendis S., Abegunde D., Yusuf S. WHO study on Prevention of REcurrences of Myocardial Infarction and StrokE (WHO-PREMISE) Bull World Health Organ. 2005;83:820–829. [PMC free article] [PubMed] [Google Scholar]
- 4.Office of Registrar General, India. Ministry of Home Affairs, New Delhi . 16 April 2013. Report on Causes of Death in India 2001–2003.http://www.cghr.org/wordpress/wpcontent/uploads/Causes_of_death_2001-03.pdf [Google Scholar]
- 5.Ahmad N., Bhopal R. Is coronary heart disease rising in India? A systematic review based on ECG defined coronary heart disease. Heart. 2005;91:719–725. doi: 10.1136/hrt.2003.031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007 Oct 20;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 7.Chadha S.L., Ramachandran K., Shekhawat S., Tandon R., Gopinath N. A 3-year follow-up study of coronary heart disease in Delhi. Bull World Health Organ. 1993;71:67–72. [PMC free article] [PubMed] [Google Scholar]
- 8.Trivedi D.H., Sharma V., Pandya H. Longitudinal epidemiological study of coronary heart disease in a rural population of Kheda district, Gujarat, India. Soz Praventivmed. 1996;41:373–379. doi: 10.1007/BF01324287. [DOI] [PubMed] [Google Scholar]
- 9.Gupta R., Prakash H., Majumdar S., Sharma S., Gupta V.P. Prevalence of coronary heart disease and coronary risk factors in an urban population of Rajasthan. Indian Heart J. 1995;47:331–338. [PubMed] [Google Scholar]
- 10.Kutty V.R., Balakrishnan K.G., Jayasree A.K., Thomas J. Prevalence of coronary heart disease in the rural population of Thiruvananthapuram district, Kerala, India. Int J Cardiol. 1993;39:59–70. doi: 10.1016/0167-5273(93)90297-t. [DOI] [PubMed] [Google Scholar]
- 11.Gupta R., Gupta H.P., Keswani P., Sharma S., Gupta V.P., Gupta K.D. Coronary heart disease and coronary risk factor prevalence in rural Rajasthan. J Assoc Physicians India. 1994;42:24–26. [PubMed] [Google Scholar]
- 12.Wander G.S., Khurana S.B., Gulati R. Epidemiology of coronary heart disease in a rural Punjab population–prevalence and correlation with various risk factors. Indian Heart J. 1994;46:319–323. [PubMed] [Google Scholar]
- 13.Pais P., Pogue J., Gerstein H. Risk factors for acute myocardial infarction in Indians: a case-control study. Lancet. 1996;348:358–363. doi: 10.1016/s0140-6736(96)02507-x. [DOI] [PubMed] [Google Scholar]
- 14.Pais P., Fay M.P., Yusuf S. Increased risk of acute myocardial infarction associated with beedi and cigarette smoking in Indians: final report on tobacco risks from a case-control study. Indian Heart J. 2001;53:731–735. [PubMed] [Google Scholar]
- 15.Patil S.S., Joshi R., Gupta G., Reddy M.V., Pai M., Kalantri S.P. Risk factors for acute myocardial infarction in a rural population of central India: a hospital-based case-control study. Natl Med J India. 2004;17:189–194. [PubMed] [Google Scholar]
- 16.Guha S., Ghosh A., Chatterjee N. Risk factors for coronary heart disease in Indians: a case-control study from Eastern India. Indian Heart J. 2005;57:738–740. [PubMed] [Google Scholar]
- 17.Jain P., Jain P., Bhandari S., Siddhu A. A case-control study of risk factors for coronary heart disease in urban Indian middle-aged males. Indian Heart J. 2008;60:233–240. [PubMed] [Google Scholar]
- 18.Gupta R. Lifestyle risk factors and coronary heart disease prevalence in Indian men. J Assoc Physicians India. 1996;44:689–693. [PubMed] [Google Scholar]
- 19.Kaul U., Gupta R.K., Haridas K.K. Platelet glycoprotein IIb/IIIa inhibition using eptifibatide with primary coronary stenting for acute myocardial infarction: a 30-day follow-up study. Catheter Cardiovasc Interv. 2002;57:497–503. doi: 10.1002/ccd.10351. [DOI] [PubMed] [Google Scholar]
- 20.Mohanan Padinhare Purayil, Mathew Rony, Harikrishnan Sadasivan, on behalf of the Kerala ACS Registry Investigators Presentation, management, and outcomes of 25748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013 Jan;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gupta R.N., Nagar K.S., Shah J.R. Observations on 165 patients with cardiac infarction treated in a coronary care unit. J Assoc Physicians India. 1972;20:283–287. [PubMed] [Google Scholar]
- 22.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 23.Chopra K.L., Chopra H.K., Aggarwal K.K. Intravenous streptokinase in acute evolving myocardial infarction–six to thirty-six months follow up. Indian Heart J. 1990;42:13–25. [PubMed] [Google Scholar]
- 24.Achari V., Prakash S., Sinha A.K., Thakur A.K. Short-term mortality and complications in ST elevation myocardial infarction–the Heart Hospital experience. J Indian Med Assoc. 2008;106:650–654. [PubMed] [Google Scholar]
- 25.Jose V.J., Gupta S.N. Mortality and morbidity of acute ST segment elevation myocardial infarction in the current era. Indian Heart J. 2004;56:210–214. [PubMed] [Google Scholar]
- 26.Thom T., Haase N., Rosamond W., American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics–2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006 Feb 14;113:e85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [Epub 2006 Jan 11] [DOI] [PubMed] [Google Scholar]
- 27.Peter Scarborough, Prachi Bhatnagar, Kremlin Wickramasinghe, Kate Smolina, Colin Mitchell and. Mike Rayner. British Heart Foundation Health Promotion Research Group. Department of Public Health, University of Oxford. Coronary Heart Disease Statistics. 2010 Edition. British Heart Foundation Statistics Database, www.heartstats.org.
- 28.Prabhakaran D., Shah P., Chaturvedi V., Ramakrishnan L., Manhapra A., Reddy K.S. Cardiovascular risk factor prevalence among men in a large industry of northern India. Natl Med J India. 2005;18:59–65. [PubMed] [Google Scholar]
- 29.Scholte op Reimer W.J.M., Gitt A.K., Boersma E., Simoons M.L., editors. Cardiovascular Diseases in Europe. Euro Heart Survey – 2006. European Society of Cardiology; Sophia Antipolis: 2006. [Google Scholar]
- 30.Lloyd-Jones D., Adams R.J., Brown T.M., American Heart Association Statistics Committee and Stroke Statistics Subcommittee Executive summary: heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010 Feb 23;121:948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 31.Bovet Pascal, Shamlaye Conrad, Gabriel Anne, Riesen Walter, Paccaud Fred. Prevalence of cardiovascular risk factors in a middle-income country and estimated cost of a treatment strategy. BMC Public Health. 2006;6:9. doi: 10.1186/1471-2458-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kotseva K., Wood D., De Backer G., De Bacquer D., Pyörälä K., Keil U., EUROASPIRE Study Group EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil. 2009 Apr;16:121–137. doi: 10.1097/HJR.0b013e3283294b1d. [DOI] [PubMed] [Google Scholar]
- 33.Hasdai D., Behar S., Wallentin L. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS) Eur Heart J. 2002;23:1190–1201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 34.Mandelzweig L., Battler A., Boyko V. Euro Heart Survey Investigators. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 35.Steg Philippe Gabriel, Goldberg Robert J., Gore Joel M., for the GRACE Investigators Baseline characteristics, management Practices, and in-hospital outcomes of patients Hospitalized with acute coronary syndromes in the Global registry of acute coronary Events (GRACE) Am J Cardiol. 2002;90:358–363. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 36.Yusuf S., Islam S., Chow C.K. Prospective Urban Rural Epidemiology (PURE) Study Investigators. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011 Oct 1;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [Epub 2011 Aug 26] [DOI] [PubMed] [Google Scholar]
- 37.Fox K.A., Steg P.G., Eagle K.A. GRACE Investigators. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007;May 2;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.