Abstract
Background
Relative accuracy of the various currently available cardiovascular (CV) risk assessment algorithms in Indian patients is not known.
Methods
This study included 194 consecutive patients (mean age 49.6 ± 10.3 years, 84.5% males) attending a CV disease prevention clinic at a tertiary center in north India. Four risk assessment models [Framingham Risk score (RiskFRS), American College of Cardiology/American Heart Association pooled cohort equations (RiskACC/AHA), the 3rd iteration of Joint British Societies' risk calculator (RiskJBS) and the World Health Organization/International Society of Hypertension risk prediction charts (RiskWHO)] were applied. The estimated risk scores were correlated with carotid intima-media thickness (CIMT) and coronary calcium score (CCS) using nonparametric statistics (Chi-square test, Kruskal–Wallis test and Spearman rank correlation).
Results
Overall, RiskACC/AHA and RiskWHO significantly underestimated CV risk as compared to RiskJBS and RiskFRS, with RiskJBS being the least likely to underestimate the risk (patients with coronary artery disease who were found to have ≥20% CV risk- 21.4% with RiskACC/AHA, 17.9% with RiskWHO, 41.4% with RiskFRS, and 58.6% with RiskJBS). Further, only RiskJBS and RiskFRS, but not RiskACC/AHA and RiskWHO, demonstrated consistent relationship with CIMT and CCS (Spearman rho 0.45 and 0.46 for RiskJBS and 0.39 and 0.36 for RiskFRS for CIMT and CCS respectively, all p values < 0.001).
Conclusions
The present study shows that in Indian subjects RiskJBS appears to provide the most accurate estimation of CV risk. It least underestimates the risk and has the best correlation with CIMT and CCS. However, large-scale prospective studies are needed to confirm these findings.
Keywords: Atherosclerotic cardiovascular disease, Primary prevention, Risk stratification
1. Introduction
Estimation of the risk of future atherosclerotic cardiovascular (CV) events is an important step in the management of the patients requiring primary prevention of CV disease. The ability to quantify CV risk allows objective assessment of the ‘seriousness’ of the illness, provides a means to communicate the same to the patient and his family, and most importantly, forms the basis on which a number of important therapeutic decisions are taken.1,2
A number of CV risk scoring systems are currently available for use in different population groups, such as Framingham risk score (RiskFRS),3,4 Prospective Cardiovascular Munster Score (PROCAM),5 Systemic Coronary Risk Evaluation (SCORE),6 World Health Organization/International Society of Hypertension (WHO/ISH) CV disease risk prediction charts (RiskWHO)7 and the more recently developed American College of Cardiology/American Heart Association (ACC/AHA) pooled cohort equations (RiskACC/AHA)8 and the 3rd iteration of Joint British Societies' risk calculator (RiskJBS).9 However, as these risk algorithms are based on epidemiological data, they are applicable only to those populations from which the data has been derived. Unfortunately, none of the currently available risk prediction models is based on Indian data or has been prospectively validated in Indians. Although a few studies have attempted to evaluate the relative accuracy of these western CV risk scores in Indians, the evidence remains grossly limited.10,11 We, therefore, sought this study to compare the accuracy of four clinically relevant CV risk assessment algorithms- RiskFRS, RiskJBS, RiskACC/AHA abd RiskWHO- in a north Indian population. The risk estimates derived using these four algorithms were correlated with carotid intima-media thickness (CIMT) and coronary calcium score (CCS)- the two well established measures of subclinical atherosclerosis and reliable predictors of future risk of CV events.
2. Methods
This cross-sectional study included consecutive subjects attending a CV disease prevention clinic at a tertiary care center in north India. The subjects were eligible to be included in the present study if they-
-
•
were ≥30 years of age,
-
•
had undergone computed tomographic (CT) coronary angiography along with CCS estimation,
-
•
did not have previously known coronary artery disease (CAD), and
-
•
did not have any other concomitant major cardiac illness.
Thus, a total of 194 subjects were included in the study. All subjects underwent clinical evaluation, biochemical investigations and measurement of CIMT. In addition, as mentioned above, all subjects had already undergone CCS estimation.
The clinical evaluation included history regarding the presence or absence of CV risk factors, duration of CV risk factors, symptoms suggestive of CAD etc. Physical examination included height, weight & blood pressure (BP) measurement and the examination of CV system. BP was measured in the right arm in supine position, using a standard sphygmomanometer. Biochemical investigations included a fasting lipid profile and fasting & 2-h post-prandial blood glucose estimation.
For the purpose of the present study, hypertension was defined according to Joint National Committee (JNC) 7 guidelines as systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg or previous history of hypertension or self reported use of anti-hypertensive medications.12 Diabetes mellitus was defined as fasting blood glucose ≥126 mg/dl or 2-h postprandial blood glucose ≥200 mg/dl or pharmacological treatment for diabetes or previous history of diabetes mellitus. Family history was considered positive if a coronary event had occurred in a male first degree relative before the age of 55 years or a female first degree relative before the age of 65 years. Smoking or tobacco use in any form during the preceding month was also considered to be a CV risk factor.
2.1. Estimation of CV risk
Based on the information collected, 10-year risk of having a major CV event [CV death, myocardial infarction (MI) or stroke] was calculated for each patient using RiskFRS, RiskJBS, RiskACC/AHA and RiskWHO. However, as RiskACC/AHA and RiskWHO limit 10-year risk estimation only to the individuals ≥40 years of age, those <40 years of age (n = 37) were excluded when calculating 10-year risk estimates using these two algorithms. Similarly, RiskFRS could not be applied in 2 patients as they were >74 years of age and RiskJBS could not be applied in 3 patients because their body-mass index values were not available.
RiskFRS and the RiskACC/AHA calculators are available for download from the websites https://www.framinghamheartstudy.org/risk-functions/cardiovascular-disease/10-year-risk.php# and http://my.americanheart.org/professional/StatementsGuidelines/Prevention-Guidelines_UCM_457698_SubHomePage.jsp respectively. RiskJBS is available as an online calculator at www.jbs3risk.com. The WHO/ISH risk prediction charts are included as part of the ‘Guideline for assessment and management of cardiovascular risk’ available at the WHO website (http://www.who.int/cardiovascular_diseases/publications/Prevention_of_Cardiovascular_Disease/en/). The chart applicable for South-East Asian region D (which includes Bangladesh, Bhutan, Democratic People's Republic of Korea, India, Maldives, Myanmar and Nepal) was used in the present study.
Using these risk assessment models, 10-year absolute CV risk estimates were derived and divided in to the following three categories – <10%, 10–19.9% and ≥20%. RiskWHO, however, only provides range estimates and not the absolute risk estimates.
2.2. CIMT assessment
CIMT measurement was performed following the standard protocol.13 Distal common carotid artery (CCA) was imaged on both sides with a 7.5 MHz frequency linear array transducer, attached to any standard vascular ultrasound machine. The artery was imaged in a longitudinal plane to obtain optimal angle of incidence, defined as the plane in which the bifurcation of the carotid bulb into the internal and external carotid arteries can be visualized simultaneously with the bulb and distal CCA (also known as ‘tuning fork’ view). Once this view was obtained, finer adjustments in the transducer position were done to ensure distal CCA was perfectly horizontal on the screen and ‘double lines’ of intima and adventitia were clearly visualized in the far wall of the CCA (‘double-line’ sign). From this view, CIMT was measured as the distance between the lumen-intima interface and the media-adventitia interface. Plaques, defined as ≥50% localized thickening of the intima compared to the rest of the wall, were included in the measurement of CIMT if present within the distal 1 cm of CCA.
The CCA was then imaged from two additional complimentary angles, approximately 45° anterior and posterior to the first image and the CIMT measurement was performed. The six values thus obtained (three for each side) were averaged and used for analysis.
Reproducibility of CIMT measurement in our lab has already been documented previously.14
2.3. Coronary calcium scoring
Multi-detector CT of the heart was performed using dual source dual energy Somatom Definition Flash (Siemens Healthcare, Germany) with 128 × 0.6 mm collimation, rotation time 75 ms and tube voltage of 80 & 140 kV. In a single breath-hold, images were acquired from the level of tracheal bifurcation to the base of the heart using prospective ECG-triggering with the centre of the acquisition at 70% of the R–R interval. From the raw data, the images were reconstructed with standard kernel in 3 mm thick axial, non-overlapping slices and 25 cm field of view. All image analyses were performed on a dedicated workstation (MMWP and Syngovia Siemens, Germany). A coronary calcified lesion was defined as an area with a density >130 Hounsfield units and covering at least 6 pixels. The Agatston method was used to determine the coronary calcium score (CCS) by multiplying each lesion area by a weighted CT attenuation score in the lesion.15
3. Statsitical analysis
The data were managed on Microsoft excel spreadsheet (version 2007, Microsoft Corp, Seattle, Washington) and analyzed using SPSS for Windows (release 15.0, SPSS Inc, Chicago, IL, USA). Standard descriptive analysis was performed. The categorical variables were expressed as actual numbers with percentages and the continuous variables as mean ± standard deviation (for normally distributed data) or as median with interquartile ranges (for CIMT and CCS, which were not normally distributed). The comparisons among different risk groups and disease groups were performed using Chi-square test for categorical variables and one-way analysis of variance or Kruskal–Wallis test, as appropriate, for continuous variables. Spearman rho (ρ) was estimated to assess the relationship between various risk estimates and the measures of subclinical atherosclerosis. A p value <0.05 was considered statistically significant.
4. Results
A total of 194 subjects were included in the study. The mean age of the study subjects was 49.6 ± 10.3 years and 164 (84.5%) were males. Nearly two-thirds (67.5%) had hypertension, one third (32.0%) had diabetes and another third (30.9%) were smokers. The mean body-mass index was 28.4 ± 4.2 kg/m2.
4.1. CT angiographic extent of CAD and its relationship with CV risk factors and risk estimates (Tables 1 and 2)
Table 1.
Clinical and biochemical characteristics of the study population according to presence or absence of coronary artery disease.
| Parameter | No CAD (n = 117) | Non-critical CAD (n = 47) | CAD (n = 30) | p Value |
|---|---|---|---|---|
| Age (years) | 46.2 ± 9.3 | 54.7 ± 9.7 | 54.9 ± 9.5 | <0.001 |
| Male gender, n (%) | 97 (82.9) | 40 (85.1) | 27 (90.0) | 0.63 |
| Hypertension, n (%) | 75 (64.1) | 32 (68.1) | 24 (80.0) | 0.25 |
| Diabetes mellitus, n (%) | 33 (28.2) | 19 (40.4) | 10 (33.3) | 0.31 |
| Current smokers, n (%) | 39 (33.3) | 8 (17.0) | 13 (43.3) | 0.04 |
| Body mass index (kg/m2) | 28.5 ± 4.1 | 28.1 ± 3.5 | 28.7 ± 5.8 | 0.81 |
| Systolic blood pressure (mmHg) | 132.1 ± 18.5 | 133.0 ± 15.4 | 132.2 ± 13.1 | 0.95 |
| Diastolic blood pressure (mmHg) | 81.9 ± 9.6 | 81.7 ± 9.3 | 83.0 ± 8.2 | 0.80 |
| Fasting blood glucose (mg/dL) | 105.7 ± 24.3 | 121.5 ± 43.1 | 109.0 ± 26.3 | 0.03 |
| Total cholesterol (mg/dL) | 192.5 ± 47.7 | 173.1 ± 39.2 | 179.3 ± 39.0 | 0.03 |
| Serum triglycerides (mg/dL) | 164.2 ± 97.4 | 134.4 ± 55.2 | 149.2 ± 92.6 | 0.15 |
| HDL-cholesterol (mg/dL) | 42.3 ± 12.1 | 43.4 ± 12.2 | 43.3 ± 11.7 | 0.83 |
| LDL-cholesterol (mg/dL) | 117.5 ± 43.3 | 100.8 ± 38.5 | 107.0 ± 31.1 | 0.047 |
*All values are mean ± standard deviation or actual number with percentages in parentheses.
CAD, coronary artery disease; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Table 2.
Estimated cardiovascular risk and measures of subclinical atherosclerosis according to presence or absence of coronary artery disease.
| Parameter | No CAD (n = 117) | Non-critical CAD (n = 47) | CAD (n = 30) | p Value |
|---|---|---|---|---|
| Framingham risk score (n = 192) | ||||
|
13.0 ± 9.4 | 17.7 ± 10.1 | 20.0 ± 9.5 | <0.001 |
|
23/117 (19.7) | 17/46 (37.0) | 12/29 (41.4) | 0.014 |
| JBS3 risk score (n = 191) | ||||
|
12.2 ± 11.2 | 18.3 ± 12.5 | 24.3 ± 13.7 | <0.001 |
|
23/116 (19.8) | 14/46 (30.4) | 17/29 (58.6) | <0.001 |
| ACC/AHA risk score (n = 157) | ||||
|
7.8 ± 7.7 | 11.7 ± 10.9 | 12.1 ± 7.7 | 0.02 |
|
7/86 (8.1) | 7/43 (16.3) | 6/28 (21.4) | 0.13 |
| WHO/ISH risk score (n = 157) | ||||
|
11/86 (12.8) | 6/43 (14.0) | 5/28 (17.9) | 0.80 |
| Carotid intima-media thickness (mm) | ||||
|
0.60 (0.5, 0.79) | 0.75 (0.60, 0.80) | 0.75 (0.65, 0.90) | 0.004 |
| Coronary calcium score | ||||
|
0 (0, 0) | 18.1 (1.0, 63.2) | 67.1 (21.2, 268.5) | <0.001 |
| ||||
| ‘0’ score, n (%) | 93 (79.5) | 10 (21.3) | 5 (16.7) | |
| 1–99, n (%) | 23 (19.7) | 31 (66.0) | 12 (40.0) | <0.001 |
| 100–399, n (%) | 1 (0.9) | 5 (10.6) | 9 (30.0) | |
| ≥400, n (%) | 0 (0) | 1 (2.1) | 4 (13.3) | |
ACC, American College of Cardiology; AHA, American Heart Association; CAD, coronary artery disease; JBS3, 3rd iteration of the Joint British Societies.
For the purpose of analysis, the study population was divided in to 3 groups based on CT coronary angiography findings-
-
○
No CAD group (n = 117)- normal coronaries
-
○
Non-critical CAD group (47)- those with <50% stenotic plaque(s) in any one or more of the major epicardial coronary arteries or their major branches
-
○
CAD group (n = 30)- those who had ≥50% stenotic lesion(s) in any one or more of the major epicardial coronary arteries or their major branches
The patients with CAD were older (p < 0.001) and were more likely to be smokers (p 0.04) than the other two groups (Table 1) whereas total cholesterol and low-density lipoprotein cholesterol were higher in those with normal coronary arteries (p values 0.03 and 0.047, respectively).The 10-year CV risk estimates derived using all the risk scores showed progressive increase with increasing extent of CAD. However, RiskACC/AHA and RiskWHO provided lower risk estimates as compared to RiskFRS and RiskJBS. Moreover, using the traditional threshold of ≥20% 10-year risk to define high CV risk, only RiskFRS and RiskJBS could adequately discriminate among different CAD categories (p values 0.014 and < 0.001, respectively; Table 2). RiskACC/AHA and RiskWHO significantly underestimated CV risk with only 21.4% and 17.9% of those in the CAD group found to have ≥20% CV risk using these risk algorithms. In comparison, RiskFRS identified 41.4% and RiskJBS 58.6% of these patients as at ‘high CV risk’.
4.2. CT angiographic extent of CAD and its relationship with CIMT and CCS
Both CIMT and CCS progressively increased as the CT angiographic extent of CAD increased (p value 0.004 for CIMT and <0.001 for CCS; Table 2). In addition, zero calcium score was seen in 79.5% of the patients with normal coronaries but only 16.7% of those with CAD (p < 0.001). These findings reinforce the validity of CIMT and CCS as surrogate measures of atherosclerosis.
4.3. CV risk estimates and their relationship with CIMT and CCS (Table 3, Figs. 1 and 2)
Table 3.
Carotid intima-media thickness and coronary calcium scores according to the estimated cardiovascular risk categories.
| Risk algorithm | 10-year risk categories | Carotid intima-media thickness (mm) |
Coronary calcium score |
||
|---|---|---|---|---|---|
| Median (interquartile range) | p Value | Median (interquartile range) | p Value | ||
| Framingham risk score | <20% (n = 140) | 0.60 (0.55, 0.76) | 0.002 | 0 (0, 18.8) | 0.008 |
| ≥20% (n = 52) | 0.74 (0.60, 0.90) | 7.5 (0, 64.1) | |||
| JBS3 risk score | <20% (n = 137) | 0.60 (0.55, 0.75) | <0.001 | 0 (0, 12.5) | <0.001 |
| ≥20% (n = 54) | 0.80 (0.65, 0.90) | 21.4 (0, 127.5) | |||
| ACC/AHA risk score | <20% (n = 137) | 0.65 (0.60, 0.80) | 0.02 | 0.2 (0, 48.6) | 0.13 |
| ≥20% (n = 20) | 0.85 (0.64, 1.0) | 16.6 (0, 208.2) | |||
| WHO/ISH risk score | <20% (n = 135) | 0.65 (0.60, 0.80) | 0.004 | 0.7 (0, 58.1) | 0.90 |
| ≥20% (n = 22) | 0.90 (0.65, 1.00) | 1.1 (0, 68.1) | |||
ACC, American College of Cardiology; AHA, American Heart Association; JBS3, 3rd iteration of the Joint British Societies.
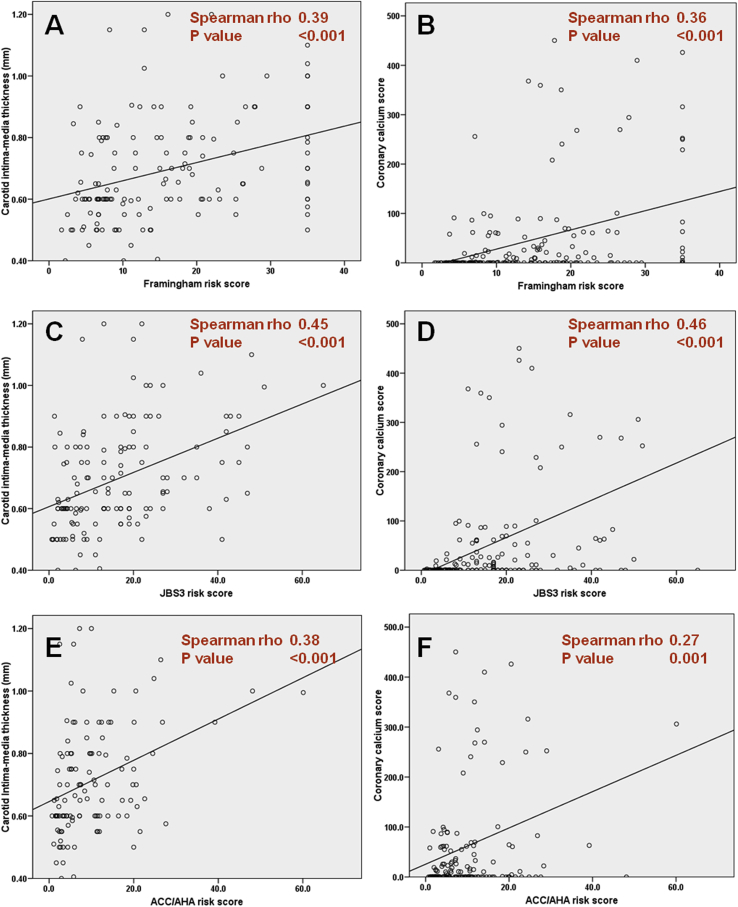
Fig. 1.
Correlations between the 10-year cardiovascular risk estimates derived using various risk scores and carotid intima-media thickness (left-side panels) and coronary calcium score (right-side panels). A, B- Framingham risk score; C, D- 3rd Iteration of the Joint British Societies (JBS3) risk score; and E, F- American College of Cardiology/American Heart Association (ACC/AHA) risk score.
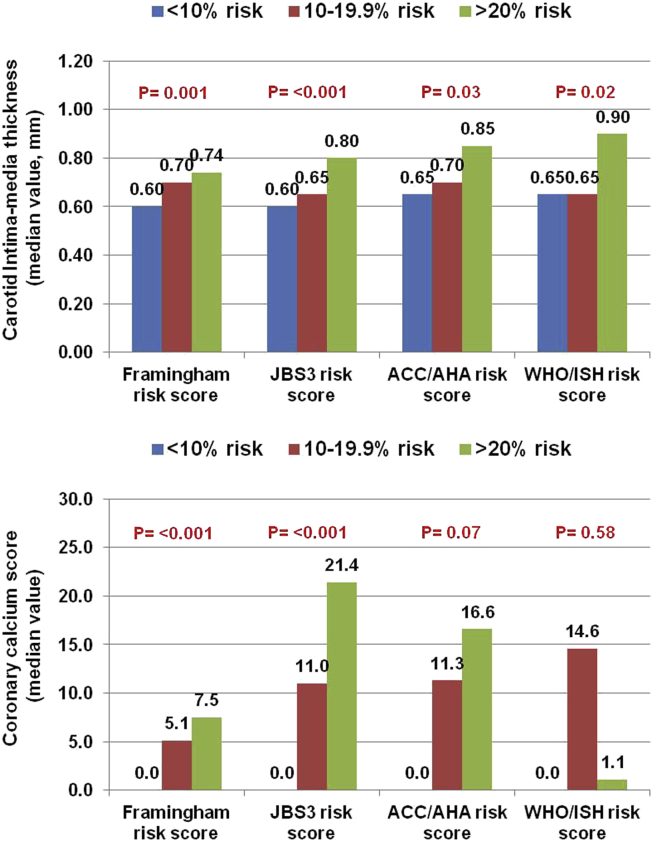
Fig. 2.
Median values of carotid intima-media thickness (upper panel) and coronary calcium scores (lower panel) according to the estimated 10-year cardiovascular risk categories. ACC, American College of Cardiology; AHA, American Heart Association; ISH, International Society of Hypertension; JBS3, 3rd iteration of the Joint British Societies, WHO, World Health Organization.
Correlations between CIMT and CCS and the absolute CV risk estimates derived using RiskFRS, RiskJBS and RiskACC/AHA were assessed using Spearman rank correlation (a similar analysis could not be performed for RiskWHO because it only provided risk ranges and not the absolute risk estimates). Statistically significant correlations were found between CIMT and CCS and all the three scoring systems (RiskFRS- ρ 0.39 and 0.36, both p values <0.001; RiskJBS- ρ 0.45 and 0.46, both p values <0.001; and RiskACC/AHA- ρ 0.38 and 0.27, p values <0.001 and 0.001, respectively) (Fig. 1). However, as evident, RiskJBS demonstrated stronger relationship as compared to the other two risk scores, whereas RiskACC/AHA had the weakest relationship (esp. with CCS). When the study subjects were categorized into various risk categories based on their 10-year CV risk estimates (i.e. <10%, 10–19.9% and ≥20%), there was progressive increase in CIMT and CCS with increasing risk categories based on RiskFRS and RiskJBS, with RiskJBS demonstrating stronger relationship as compared to RiskFRS. In contrast, RiskACC/AHA and RiskWHO showed a relationship only with CIMT and not with CCS (Fig. 2, Table 3).
5. Discussion
The salient findings of the present study are - 1) RiskACC/AHA and RiskWHO significantly underestimate CV risk in Indian patients. RiskJBS and RiskFRS are more accurate, with RiskJBS being the least likely to underestimate the risk; and 2) RiskJBS and RiskFRS, but not RiskACC/AHA and RiskWHO, demonstrate consistent relationship with the measures of subclinical atherosclerosis (i.e. CIMT and CCS). The strength of the association appears to be stronger for RiskJBS than the same for RiskFRS.
5.1. CV risk estimation in Indians
In the current era of evidence-based medicine, all our decisions need to be based on robust scientific evidence. The current guidelines recommend that the use of statins and aspirin should be linked to the anticipated CV risk in the given individual. Hence, it is essential to assess CV risk in every patient in whom a statin or aspirin is prescribed for primary prevention of CV disease. The estimation of CV risk has an added advantage that it provides an objective measure of the ‘seriousness’ of the illness and may help improve patient compliance to the treatment.
The major challenge to CV risk estimation in Indian patients is the lack of a prospectively validated, ethnic specific CV risk assessment algorithm for Indian population. As Indians are known to have considerable differences in the CV disease epidemiology as compared to the western populations,16–22 the risk scoring systems based on the western data may not be directly applicable to them. Consistent with this, several previous studies have shown that the currently available western risk assessment models tend to underestimate the risk in South Asians, including Indians.17,20,21,23,24
Several different approaches have been tried to overcome this challenge. Chow et al utilized data derived as part of the Andhra Pradesh Rural Health Initiative and demonstrated that it was feasible to recalibrate RiskFRS to render it applicable to a given ethnic/regional group.25 However, the study also showed that reliable local CV epidemiology data was required to achieve accurate recalibration of RiskFRS.
An alternate approach is to apply multiple scoring systems in the same population group and compare their accuracy to determine which one is likely to be more accurate. As an example, Kanjilal et al10 compared 3 different risk scoring systems- RiskFRS, SCORE and an older version of JBS risk score in the family members of the patients with CV disease. It was found that despite significantly elevated levels of lipids, pro-inflammatory, pro-thrombotic, and serological markers, all 3 risk scores identified <5% population as being at ‘high-risk’. In a more recent study involving patients presenting with acute MI, we compared the same four risk scores as evaluated in the present study.11 It was found that RiskJBS was the most likely to correctly identify these individuals as ‘at high-risk’ whereas RiskWHO most underestimated the risk. However, a major limitation of this study was that retrospective risk estimation was performed in patients who had already presented with a major CV event.
Therefore, in the present study, we included out-patients undergoing primary or secondary prevention of CV disease. Once again, we found that RiskJBS had the best accuracy for assessing atherosclerosis burden. In comparison, RiskFRS had lower, albeit comparable, accuracy whereas RiskACC/AHA and RiskWHO were much inferior. These two studies together provide the evidence to support that RiskJBS is perhaps the most suited CV risk assessment tool for use in Indians at present.
There could be several explanations why RiskJBS was found to be more accurate in our study. First, RiskJBS is the only risk assessment model that includes data derived from ethnic Indians, even though non-resident ones. Second, RiskJBS is a more comprehensive risk assessment model and takes in to account several additional risk factors such as obesity and family history of premature CV disease. Inclusion of these risk factors is likely to enhance the accuracy of risk prediction.
5.2. CIMT and CCS as surrogate measures of subclinical atherosclerosis
CIMT and CCS are established measures of subclinical atherosclerosis and are being widely used in epidemiological studies as well as in research on atherosclerosis.13,26–34 Numerous studies have demonstrated that both CIMT and CCS are excellent predictors of future CV risk and have incremental predictive value over conventional risk factors and risk assessment algorithms.13,26–28,30–32,34 Several studies performed in Indian subjects have also documented that CIMT and CCS are associated with the presence of CV risk factors and CV disease.33,35–42 In the present study also, CIMT and CCS correlated with the extent of coronary disease as assessed by CT coronary angiography, which further reinforces their value as reliable measures of atherosclerotic vascular disease.
Of all the currently available measures of subclinical atherosclerosis, CCS appears to be the most robust.29,34,43 It has been shown to have excellent accuracy to predict risk of adverse CV outcomes in a wide-variety of clinical settings, including asymptomatic patients with CV risk factors, patients with stable CAD as well as those presenting with an acute coronary event.29,34
6. Limitations
The main limitations of our study were its cross-sectional nature and the small sample size. As the clinical risk algorithms are meant only for estimating future risk of CV events, the only appropriate method to test their accuracy is to conduct a large-scale prospective study. While the need to have a large-scale prospective study cannot be overemphasized, performing such a study may not be feasible due to the obvious logistic constraints, particularly in a country like ours. Given these constraints, our study explores an alternate strategy to assess predictive accuracy of the different CV risk assessment algorithms in Indian subjects. We utilized CIMT and CCS as a surrogate for future risk of CV events, based on the enormous evidence generated from large-scale epidemiological studies. However, we do agree that a larger sample size would have enhanced the validity of our study findings.
Some of our patients were already on statins and angiotensin converting enzyme inhibitors which must have altered the relationship between various risk scores and CIMT and CCS. However, it is unlikely to have appreciably affected our study's main findings. Most of the patients who were on these therapies were only recently initiated on the treatment. Although significant lowering of cholesterol values may occur even with a short course of statin, CIMT and CCS change only gradually, taking several months to years to demonstrate any measurable change. Therefore, the use of statins could only lead to underestimation of CV risk by various risk algorithms, thereby weakening their relationships with CIMT and CCS. However, as total cholesterol is included in all the four risk scores evaluated in the present study, it is unlikely that statins would have differentially affected one risk score more than the other.
Finally, we only measured CIMT and did not specifically assess carotid plaques in the present study. The available evidence suggests that carotid plaques are more predictive of future CV events as compared to elevated CIMT.44 However, we had included multiple measures of subclinical atherosclerosis, including CCS which has been shown to be more robust than carotid ultrasound imaging.
7. Conclusions
The present study shows that in Indian subjects, RiskFRS and RiskJBS demonstrate better correlation with various measures of subclinical atherosclerosis than RiskACC/AHA and RiskWHO. Further, RiskJBS is the least likely to underestimate CV risk in these individuals. These findings suggest that RiskJBS may be the most appropriate CV risk assessment algorithm for use in Indians at present. However, large-scale prospective studies are needed to confirm these findings.
Conflicts of interest
The authors have none to declare.
Acknowledgment
We sincerely thank Mr Arun Rawat and Mr Ravinder Negi, clinical research coordinators, for their help in data collection and compilation.
Footnotes
Place of work: Medanta – The Medicity, Sector 38, Gurgaon 122001, India.
References
- 1.Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel iii) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 2.Stone N.J., Robinson J.G., Lichtenstein A.H. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129:S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 3.Wilson P.W., D'Agostino R.B., Levy D., Belanger A.M., Silbershatz H., Kannel W.B. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 4.D'Agostino R.B., Sr., Vasan R.S., Pencina M.J. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 5.Assmann G., Cullen P., Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular munster (procam) study. Circulation. 2002;105:310–315. doi: 10.1161/hc0302.102575. [DOI] [PubMed] [Google Scholar]
- 6.Conroy R.M., Pyorala K., Fitzgerald A.P. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the score project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 7.World health organization . WHO; Geneva: 2007. Prevention of Cardiovascular Disease Guidelines for Assessment and Management of Cardiovascular Risk. [Google Scholar]
- 8.Goff D.C., Jr., Lloyd-Jones D.M., Bennett G. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129:S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 9.Joint British societies' consensus recommendations for the prevention of cardiovascular disease (JBS3) Heart. 2014;100:ii1–ii67. doi: 10.1136/heartjnl-2014-305693. [DOI] [PubMed] [Google Scholar]
- 10.Kanjilal S., Rao V.S., Mukherjee M. Application of cardiovascular disease risk prediction models and the relevance of novel biomarkers to risk stratification in Asian Indians. Vasc Health Risk Manag. 2008;4:199–211. doi: 10.2147/vhrm.2008.04.01.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bansal M., Kasliwal R.R., Trehan N. Comparative accuracy of different risk scores in assessing cardiovascular risk in Indians: a study in patients with first myocardial infarction. Indian Heart J. 2014;66:580–586. doi: 10.1016/j.ihj.2014.10.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chobanian A.V., Bakris G.L., Black H.R. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the jnc 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 13.Stein J.H., Korcarz C.E., Hurst R.T. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American society of echocardiography carotid intima-media thickness task force endorsed by the society for vascular medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Kasliwal R.R., Agrawal S., Bansal M. Carotid intima-media thickness and brachial artery flow-mediated dilatation in patients with and without metabolic syndrome. Indian Heart J. 2006;58:42–46. [PubMed] [Google Scholar]
- 15.Agatston A.S., Janowitz W.R., Hildner F.J., Zusmer N.R., Viamonte M., Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 16.Enas E.A., Garg A., Davidson M.A., Nair V.M., Huet B.A., Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1996;48:343–353. [PubMed] [Google Scholar]
- 17.Anand S.S., Yusuf S., Vuksan V. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the study of health assessment and risk in ethnic groups (share) Lancet. 2000;356:279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 18.McKeigue P.M., Miller G.J., Marmot M.G. Coronary heart disease in south Asians overseas: a review. J Clin Epidemiol. 1989;42:597–609. doi: 10.1016/0895-4356(89)90002-4. [DOI] [PubMed] [Google Scholar]
- 19.Joshi P., Islam S., Pais P. Risk factors for early myocardial infarction in south Asians compared with individuals in other countries. JAMA. 2007;297:286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 20.Perumal L., Wells S., Ameratunga S. Markedly different clustering of cvd risk factors in New Zealand Indian and European people but similar risk scores (predict-14) Aust N. Z J Public Health. 2012;36:141–144. doi: 10.1111/j.1753-6405.2011.00808.x. [DOI] [PubMed] [Google Scholar]
- 21.Bhopal R., Fischbacher C., Vartiainen E., Unwin N., White M., Alberti G. Predicted and observed cardiovascular disease in south Asians: application of Finrisk, Framingham and score models to newcastle heart project data. J public health (Oxford, England) 2005;27:93–100. doi: 10.1093/pubmed/fdh202. [DOI] [PubMed] [Google Scholar]
- 22.Liem S.S., Oemrawsingh P.V., Cannegieter S.C. Cardiovascular risk in young apparently healthy descendents from Asian Indian migrants in the Netherlands: the Shiva study. Neth Heart J. 2009;17:155–161. doi: 10.1007/BF03086238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeemon P., Prabhakaran D., Huffman M.D. Distribution of 10-year and lifetime predicted risk for cardiovascular disease in the Indian sentinel surveillance study population (cross-sectional survey results) BMJ Open. 2011;1:e000068. doi: 10.1136/bmjopen-2011-000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bansal M., Shrivastava S., Mehrotra R., Agarwal V., Kasliwal R.R. Low Framingham risk score despite high prevalence of metabolic syndrome in asymptomatic North-Indian population. J Assoc Physicians India. 2009;57:17–22. [PubMed] [Google Scholar]
- 25.Chow C.K., Joshi R., Celermajer D.S., Patel A., Neal B.C. Recalibration of a Framingham risk equation for a rural population in India. J Epidemiol Community Health. 2009;63:379–385. doi: 10.1136/jech.2008.077057. [DOI] [PubMed] [Google Scholar]
- 26.Chambless L.E., Heiss G., Folsom A.R. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the atherosclerosis risk in communities (aric) study, 1987–1993. Am J Epidemiol. 1997;146:483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 27.O'Leary D.H., Polak J.F., Kronmal R.A., Manolio T.A., Burke G.L., Wolfson S.K., Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 28.van der Meer I.M., Bots M.L., Hofman A., del Sol A.I., van der Kuip D.A., Witteman J.C. Predictive value of noninvasive measures of atherosclerosis for incident myocardial infarction: the Rotterdam study. Circulation. 2004;109:1089–1094. doi: 10.1161/01.CIR.0000120708.59903.1B. [DOI] [PubMed] [Google Scholar]
- 29.Greenland P., Bonow R.O., Brundage B.H. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American college of cardiology foundation clinical expert consensus task force (ACCF/AHA writing committee to update the 2000 expert consensus document on electron beam computed tomography) developed in collaboration with the society of atherosclerosis imaging and prevention and the society of cardiovascular computed tomography. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Greenland P., LaBree L., Azen S.P., Doherty T.M., Detrano R.C. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 31.Arad Y., Goodman K.J., Roth M., Newstein D., Guerci A.D. Coronary calcification, coronary disease risk factors, c-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis heart study. J Am Coll Cardiol. 2005;46:158–165. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- 32.Detrano R., Guerci A.D., Carr J.J. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 33.Kasliwal R.R., Bansal M., Gupta H., Agrawal S. Association of carotid intima-media thickness with left main coronary artery disease. Indian Heart J. 2007;59:50–55. [PubMed] [Google Scholar]
- 34.Pletcher M.J., Tice J.A., Pignone M., Browner W.S. Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis. Arch Intern Med. 2004;164:1285–1292. doi: 10.1001/archinte.164.12.1285. [DOI] [PubMed] [Google Scholar]
- 35.Mohan V., Gokulakrishnan K., Sandeep S., Srivastava B.K., Ravikumar R., Deepa R. Intimal media thickness, glucose intolerance and metabolic syndrome in Asian Indians–the Chennai urban rural epidemiology study (cures -22) Diabet Med. 2006;23:845–850. doi: 10.1111/j.1464-5491.2006.01898.x. [DOI] [PubMed] [Google Scholar]
- 36.Mohan V., Ravikumar R., Shanthi Rani S., Deepa R. Intimal medial thickness of the carotid artery in south Indian diabetic and non-diabetic subjects: the Chennai urban population study (cups) Diabetologia. 2000;43:494–499. doi: 10.1007/s001250051334. [DOI] [PubMed] [Google Scholar]
- 37.Ravikumar R., Deepa R., Shanthirani C., Mohan V. Comparison of carotid intima-media thickness, arterial stiffness, and brachial artery flow mediated dilatation in diabetic and nondiabetic subjects (the Chennai urban population study [cups-9]) Am J Cardiol. 2002;90:702–707. doi: 10.1016/s0002-9149(02)02593-6. [DOI] [PubMed] [Google Scholar]
- 38.Rema M., Mohan V., Deepa R., Ravikumar R. Association of carotid intima-media thickness and arterial stiffness with diabetic retinopathy: the Chennai urban rural epidemiology study (cures-2) Diabetes Care. 2004;27:1962–1967. doi: 10.2337/diacare.27.8.1962. [DOI] [PubMed] [Google Scholar]
- 39.Chow C.K., McQuillan B., Raju P.K. Greater adverse effects of cholesterol and diabetes on carotid intima-media thickness in south Asian Indians: comparison of risk factor-imt associations in two population-based surveys. Atherosclerosis. 2008;199:116–122. doi: 10.1016/j.atherosclerosis.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 40.Hansa G., Bhargava K., Bansal M., Tandon S., Kasliwal R.R. Carotid intima-media thickness and coronary artery disease: an Indian perspective. Asian Cardiovasc Thorac Ann. 2003;11:217–221. doi: 10.1177/021849230301100308. [DOI] [PubMed] [Google Scholar]
- 41.Shrivastava S., Agrawal V., Kasliwal R.R. Coronary calcium and coronary artery disease: an Indian perspective. Indian Heart J. 2003;55:344–348. [PubMed] [Google Scholar]
- 42.Wasnik A., Raut A., Morani A. Coronary calcium scoring in asymptomatic Indian population: correlation with age, gender and risk factors–a prospective study on 500 subjects. Indian Heart J. 2007;59:232–238. [PubMed] [Google Scholar]
- 43.Simon A., Chironi G., Levenson J. Comparative performance of subclinical atherosclerosis tests in predicting coronary heart disease in asymptomatic individuals. Eur Heart J. 2007;28:2967–2971. doi: 10.1093/eurheartj/ehm487. [DOI] [PubMed] [Google Scholar]
- 44.Belcaro G., Nicolaides A.N., Ramaswami G. Carotid and femoral ultrasound morphology screening and cardiovascular events in low risk subjects: a 10-year follow-up study (the cafes-cave study(1)) Atherosclerosis. 2001;156:379–387. doi: 10.1016/s0021-9150(00)00665-1. [DOI] [PubMed] [Google Scholar]