Abstract
Background
Diabetes mellitus (DM) is now prevalent in many countries in sub-Saharan Africa, with associated health and socioeconomic consequences. Adherence to antidiabetic medications has been shown to improve glycaemic control, which subsequently improves both the short- and long-term prognosis of the disease. The main objective of this study was to assess the level of adherence to antidiabetic drugs among outpatients in a teaching hospital in southwestern Nigeria.
Methods
A cross-sectional study was carried out using the eight-item Morisky Medication Adherence Scale (MMAS-8) among diabetic patients attending the medical outpatients' diabetes clinic of Ladoke Akintola University Teaching Hospital, in Ogbomosho, Oyo State in southwestern Nigeria, during a three-month period (October to December 2013).
Results
A total of 129 patients participated in the study with a male-to-female ratio of 1:1.5. Seventy-eight (60.5%) patients had systemic hypertension as a comorbid condition while the remaining were being managed for diabetes mellitus alone. Only 6 (4.7%) of the patients had type 1 DM while the remaining 123 (95.3%) were diagnosed with type 2 DM. Metformin was the most prescribed oral hypoglycaemic agent (n = 111, 58.7%) followed by glibenclamide (n = 49, 25.9%). Medication adherence was classified as good, medium, and poor for 52 (40.6%), 42 (32.8%), and 34 (26.6%) patients, respectively.
Medication costs accounted for 72.3% of the total direct cost of DM in this study, followed by the cost of laboratory investigations (17.6%).
Conclusion
Adherence of diabetes patients in the study sample to their medications was satisfactory. There is a need for the integration of generic medicines into routine care as a way of further reducing the burden of healthcare expenditure on the patients.
Introduction
Diabetes mellitus (DM) is now one of the most common non-communicable diseases affecting the global population, with increasing incidence in many emerging countries of the world1–3. In developing countries like Nigeria, the incidence of DM, especially the type 2 variant, is on the increase, with its attendant complications. According to the International Diabetic Federation (IDF), the prevalence of DM will increase by as much as 54% globally between 2010 and 2030 with projections for countries in sub-Saharan Africa close to 100%4. In Nigeria, studies from different parts of the country have recorded prevalence rates between 1% and 8%5–8.
The management of DM consists of lifestyle and dietary changes and pharmacotherapy. For patients with type 1 DM, insulin remains the mainstay of treatment while the different groups of oral hypoglycaemic agents (OHA) and insulin are used in treating patients with type 2 DM. Studies have shown that adequate glycaemic control will slow down or prevent the development of microvascular and macrovascular complications of both types of DM9–12. Adherence to anti-diabetic medications has been shown to improve glycaemic control, which augurs well for the long-term prognosis of the disease13,14. Medication adherence to antidiabetic agents has also been shown to be more cost-effective, as it may reduce hospitalization frequency and costs associated with both short- and long-trem complications15,16. Some of the reasons or predictors of poor adherence found in the literature include high pill burden, complexity of drug regimens forgetfulness, high cost of medications, presence or perceived fear of adverse effects, and poor knowledge about the disease condition17–19.
Worldwide, studies on medication adherence among diabetes patients have shown a wide variation. Ahmad et al. reported 53% non-adherence among diabetics in Malaysia; similar studies in India and Ethiopia have reported non-adherence rates of 42.3% and 25.4%, respectively19–21. Recent Nigerian studies using different instruments revealed non-adherence rates between 27.5% and 50%22–24. These Nigerian studies investigated medication adherence among diabetes patients and its association with the number of prescribed medications and glycaemic control. The relationship between cost of medications and adherence is well established in the literature15,25. The issue of cost of medications and indeed healthcare expenditure is especially germane in developing countries like Nigeria, where the majority of patients pay out of pocket26. The national health insurance scheme (NHIS), which has been operational for about a decade now, covers less than 10% of the country's population: mainly those in the formal sectors of the economy27, 28.
The principal objective of the study was to assess the level of adherence to OHAs and insulin among diabetes patients attending the medical outpatient clinics of a tertiary hospital in Nigeria. Secondary objectives included: the prescription pattern for OHAs, some components of direct costs, and the effects of various factors on medication costs.
Methods
Study setting
The study was carried out in the medical outpatients' diabetes clinic of a tertiary-level healthcare facility in Nigeria during a three-month period (October to December 2013). The study centre was Ladoke Akintola University Teaching Hospital in Ogbomosho, Oyo State in southwestern Nigeria. This site caters for the population of Oyo and its surrounding states. This teaching hospital is the major referral hospital in the northern part of Oyo State and draws its patient population from numerous private hospitals and primary and secondary healthcare facilities in the region. The medical outpatients' clinic is manned by a consultant endocrinologist physician, registrars (senior and junior) in internal medicine, and medical interns. The centre runs a weekly clinic with an average attendance between 30 and 60 patients.
Study population
Consecutive patients who had been diagnosed with type 1 and type 2 DM and who had been on treatment in the study centre were invited to participate in the study. Patients older than 18 years of age, who had been on medication for at least six months, and gave informed consent were included in the study. Patients younger than 18 years, those who refused to consent, and those with acute symptomatology were excluded from the study. All participating patients were paying out of pocket, as they were not enrolled under the national health insurance scheme of the country.
Sampling
Sample size
The number of patients needed for this study was calculated using the formula for descriptive studies:
Sample size (n) = [DEFF*Np(1−p)]/ [(d2/Z21-α/2*(N−1)+p*(1−p)]
Where, N = Population size (600)
p = prevalence of poor adherence (0.4)
d = Precision (0.1)
DEFF = Design effect (1.5)
Z1−α/2 = 1.96
The estimated prevalence of poor adherence of 40% was chosen based on results from two similar Nigerian studies with values of 27.5% and 50% respectively22, 24. An estimated minimum sample size of 129 was obtained using the aforementioned assumptions. A convenience sampling method was used, as consecutive patients presenting at the clinic were recruited.
Study Instrument
A cross-sectional study was done using a validated self-reported adherence tool (the eight-item Morisky Medication Adherence Scale (MMAS-8))29. The MMAS-8, a validated instrument with high reliability and validity, has been used for studies on medication adherence among diabetes patients in many countries19,30,31. In Nigeria, the MMAS has been used for studies on medication adherence among hypertensive and psychiatric patients32,33. A previous Nigerian study on medication adherence among diabetes patients used the modified MMAS-4 instrument34. It collects information on how frequently patients may forget to take their medications and the reasons for this using a binary (Yes/No) and a five-option response version (never/rarely/sometimes/often/always). The summary of the scoring interpretation is as follows: 0 (for high adherence), 1–2 (medium adherence) and > 2 (poor adherence). An additional questionnaire for collection of sociodemographic details, diagnoses, a list of prescribed medications, some components of direct costs (cost of medications, laboratory investigations, transportation to and from hospital, and consultation) and factors that may affect adherence was also administered. The additional questionnaire, a mixture of open- and closed-ended statements was developed by the authors for the purpose of this study and was pre-tested among ten diabetes patients who were attending another tertiary healthcare facility in Ekiti State, southwestern Nigeria. Necessary adjustments were made in the contents and structure before its administration. The questionnaires were administered by medical interns during clinic encounters after informed consent was obtained. Glycaemic control was assessed using the average of the two most recent fasting plasma glucose and/or glycosylated haemoglobin (HbA1c) measurements available. The blood glucose was done with capillary blood taken from the patients' finger and analyzed using a glucometer in the clinic early in the morning before consultation starts. The investigators ensured that there was no discrimination against those that refused participation in the study by attending to them promptly and professionally. Six months of medication use was chosen as the cut-off for inclusion into the study because most patients had appointments either monthly or every other month and would have had between three and six clinic appointments by the time they were recruited into the study. The monthly cost of the prescribed medications was calculated using the price list of the hospital pharmacy, while patients gave an estimate of their individual transport fares to and from the hospital. The consultation fee is a constant one charged by the hospital for a consulting encounter with a physician. Written consent was obtained from each patient during study recruiment. Ethical approval was obtained from the Research Ethics Committee of the hospital before commencement of the study.
Statistical Analysis
The information obtained from the general questionnaire was coded and entered using IBM SPSS version 19 (IBM Corporation, Armonk, NY, USA). The information from the MMAS-8 was interpreted using its keys and entered. General characteristics of the patients were analyzed using descriptive statistics. Demographic variables that were normally distributed were described by mean and standard deviation. The median and range were calculated for other demographic variables that were not normally distributed. Categorical variables are reported as frequency distributions and proportions with 95% confidence intervals and were compared using the chi-square test or Fisher's exact test. Comparisons of the means of some variables (age, fasting plasma glucose, HbA1c, monthly income, monthly medication cost) were done using analysis of variance (ANOVA) with a p-value of < 0.05 taken as the level of statistical significance.
Results
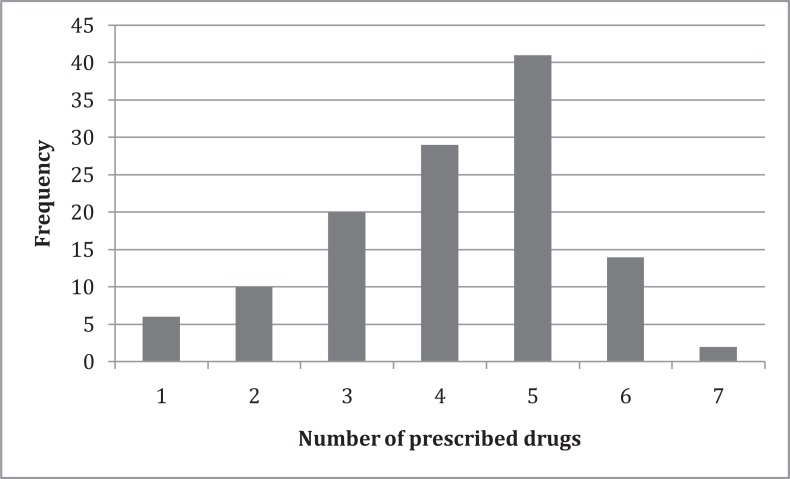
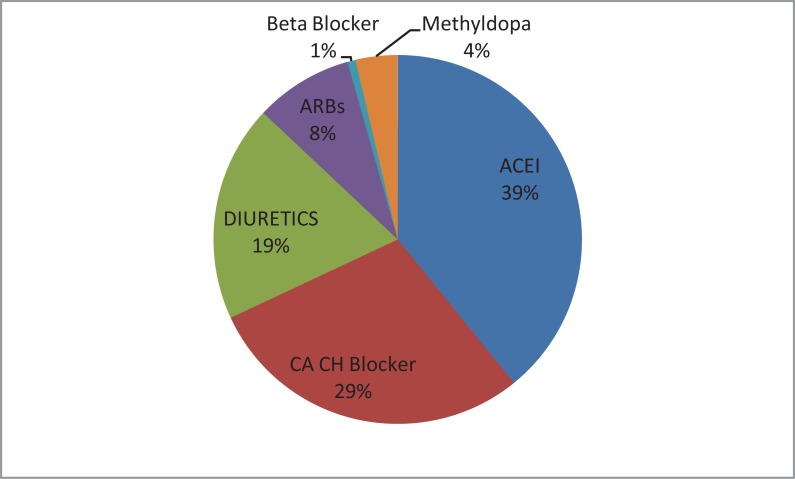
A total of 129 patients participated in the study with a male-to-female ratio of 1:1.5. The sociodemographic variables of the participants are shown in Table 1. Seventy-eight patients (60.5%) had systemic hypertension as a comorbid condition, while the remaining were being managed for DM alone. Only six (4.7%) of the patients had type 1 DM, while the remaining 123 (95.3%) were diagnosed with type 2 DM. The median duration of disease (time since initial diagnosis was made) was seven years, while the median duration of clinic attendance was three years. The average of the previous two fasting plasma glucose measurements (done on the morning of clinic appointments) of the patients was 8.2 ± 3.4 mmol/L while the mean HbA1c (done within the previous three months) was 7.5 ± 2.4%. On further analysis, only 45.9% (n = 50) of the patients had their fasting plasma glucose within the normal range (4 to 6.9 mmol/L), while 50% of those who had HbA1c done in the previous three months recorded values within normal range. Five hundred five medications were prescribed for the patients, with a mean number of 4.1 ± 1.4 prescribed per patient. The frequency distribution of number of prescribed drugs is shown in Figure 1. The breakdown of the drugs is as follows: 220 antidiabetic agents prescribed (43.6%), 163 antihypertensives (32.3%), 23 antilipemics (4.5%), and 42 anti-platelets (8.3%). Insulin usage either alone or in combination with oral hypoglycaemic agents was observed in 14.1% of patients, while the majority of patients (85.9%) had OHAs alone as antidiabetic agents. Metformin, with 111 prescriptions (58.7%), was the most prescribed oral hypoglycaemic agent followed by glibenclamide (49 prescriptions, 25.9%). Glimepiride, vildagliptin and pioglitazone were prescribed for 26 (13.8%), 2 (1.1%) and 1 (0.5%) of the patients respectively. Combination therapy of oral hypoglycaemic agents was prescribed in 74 (57.4%), oral hypoglycaemic agents and insulin in 18 (14%) and metformin alone 15 (11.6%). Lisinopril (37.4%) was the most prescribed antihypertensive, followed by nifedipine (16.6%) and hydrochlorothiazide (14.1%). The groups of prescribed antihypertensives are shown in Figure 2.
Table 1.
Sociodemographic data of study participants attending diabetes clinic at LAUTECH Teaching Hospital
| Frequency (n) | Percentage (%) | |
| SEX | ||
| Male | 51 | 39.5 |
| Female | 78 | 60.5 |
| EDUCATIONAL LEVEL | ||
| No Education | 22 | 17.6 |
| Primary Education | 30 | 24 |
| Secondary Education | 20 | 16 |
| Tertiary Education | 53 | 42.4 |
| EMPLOYMENT STATUS | ||
| Unemployed | 8 | 6.5 |
| Employed | 115 | 93.5 |
| AGE GROUP | ||
| < 30yrs | 2 | 1.6 |
| 31 – 44yrs | 5 | 4.1 |
| 45 – 64yrs | 61 | 49.6 |
| > 65yrs | 55 | 44.7 |
| MONTHLY INCOME | ||
| < 20,000 Naira | 50 | 43.1 |
| 20 – 50,000 Naira | 37 | 31.9 |
| 50 – 100,000 Naira | 22 | 19 |
| > 100,000 Naira | 7 | 6 |
₦165 Nigerian Naira = $1 US Dollar at the time of data collection
Figure 1.
Number of drugs prescribed to individual study participants at diabetes clinic at LAUTECH Teaching Hospital
Figure 2.
Percentages of prescribed antihypertensives by drug class at LAUTECH Teaching Hospital diabetes clinic
ARB = Angiotensin Receptor Blocker
ACI = Angiotensin-Converting Enzyme Inhibitor
CA CH Blocker = Calcium Channel Blocker
Medication adherence among the patients was grouped as follows: 52 good (40.3%), 43 medium (33.3%), and 34 poor (26.4%). The mean monthly cost of medications was N6557 ± N4463 Nigerian Naira (NGN) while the median monthly amount spent on transportation, investigations and consultations was NGN N400, N800 and N250, respectively (165 Nigerian Naira = 1 US Dollar, USD, at the time of data collection). The total amount (direct cost) expended monthly by patients was NGN N1,096,668, of which medications, laboratory investigations, transportation and consultation fees accounted for 72.3%, 17.6%, 7% and 3.1%, respectively. The descriptive statistics of the means of the different components of direct cost is shown in Table 4.
Table 4.
Descriptive statistics of components of direct costs for study participants at LAUTECH Teaching Hospital diabetes clinic
| n | Mean | Std. Deviation | Median | 95% Confidence Interval for Mean | Minimum | Maximum | p-value | |||
| Lower Bound | Upper Bound | |||||||||
| Monthly medication cost | Good | 49 | 6772.45 | 4804.102 | 5000 | 5392.55 | 8152.35 | 1000 | 20000 | .64 |
| Moderate | 39 | 6900.00 | 4140.303 | 5557.87 | 8242.13 | 1300 | 20000 | |||
| Poor | 32 | 5965.62 | 4353.390 | 4396.06 | 7535.19 | 1000 | 16500 | |||
| Total | 120 | 6598.75 | 4457.614 | 5793.00 | 7404.50 | 1000 | 20000 | |||
| Monthly cost of | Good | 44 | 1498.64 | 1891.121 | 800 | 923.68 | 2073.59 | 200 | 10000 | .81 |
| investigations | Moderate | 38 | 1772.89 | 2603.174 | 917.25 | 2628.54 | 150 | 10000 | ||
| Poor | 32 | 1807.81 | 2633.595 | 858.30 | 2757.32 | 200 | 11000 | |||
| Total | 114 | 1676.84 | 2345.813 | 1241.57 | 2112.12 | 150 | 11000 | |||
| Monthly transportation cost | Good | 48 | 609.79 | 709.232 | 400 | 403.85 | 815.73 | 60 | 3000 | .92 |
| Moderate | 42 | 641.19 | 869.853 | 370.13 | 912.26 | 10 | 4000 | |||
| Poor | 30 | 682.33 | 663.105 | 434.73 | 929.94 | 60 | 3000 | |||
| Total | 120 | 638.92 | 753.217 | 502.77 | 775.07 | 10 | 4000 | |||
| Consultation fees | Good | 34 | 223.53 | 105.339 | 250 | 186.77 | 260.28 | 100 | 500 | .24 |
| Moderate | 37 | 400.09 | 498.259 | 233.96 | 566.21 | 3 | 3000 | |||
| Poor | 26 | 404.05 | 737.844 | 106.03 | 702.07 | 5 | 4000 | |||
| Total | 97 | 339.26 | 495.978 | 239.30 | 439.22 | 3 | 4000 | |||
Prices in Nigerian Naira, ₦(₦165 Nigerian Naira = $1 US Dollar at the time of data collection)
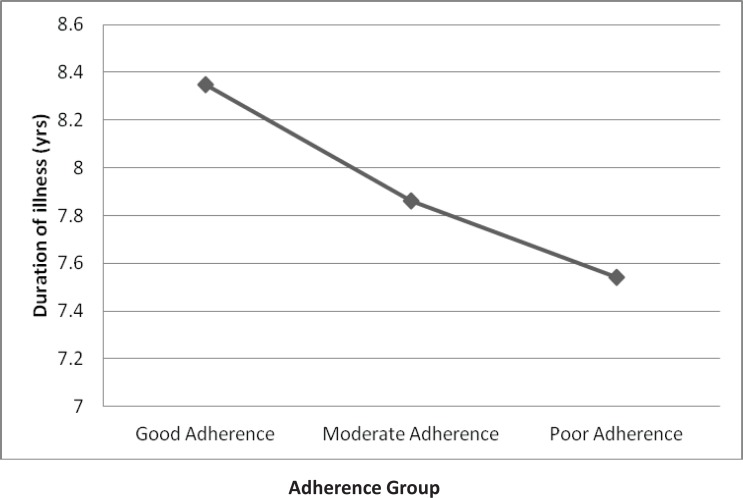
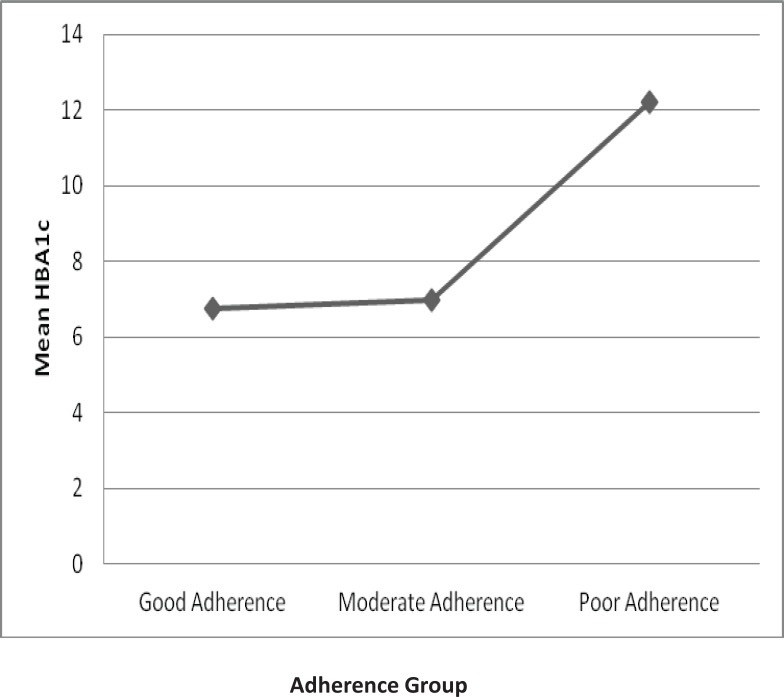
The relationship between medication adherence, sex, level of education, monthly income and other categories was explored using the chi-square.test (Table 2). The variation of the mean HbA1c levels among the three adherence groups was statistically significant (p = 0.003). Details of the comparison are shown in Table 3. The relationship between average duration of illness and the three adherence groups is shown in Figure 3, and Figure 4 depicts the the mean HbA1c levels of the three groups. The most common factors, according to the study participants, that may affect adherence to medications were cost of treatment (20.2%), lack of family support (11%), high pill burden (11%), cultural and religious beliefs (10%), inadequate information about therapy (10%) and non-availability of prescribed medications (10%).
Table 2.
Associations between study participant drug adherence and other variables at LAUTECH Teaching Hospital diabetes clinic
| Adherence level | X2 | df | p-value |
| Monthly Income | 5.25 | 2 | 0..51 |
| Sex | 3.39 | 2 | 0.18 |
| Level of Education | 6.2 | 6 | 0.40 |
| Age group | 5.06 | 6 | 0.54 |
|
Fasting Plasma Glucose (Normal/Elevated) |
0.05 | 2 | 0.98 |
|
HbA1c (Normal/Elevated) |
3.2 | 2 | 0.20 |
X2 = chi-square statistic
df = degrees of freedom
HbA1c = blood glycosylated haemoglobin concentration
Table 3.
Comparison of means of some variables between the three levels of adherence among study patients at LAUTECH Teaching Hospital
| Sum of Squares | df | Mean Square | F | p-value | ||
| HbA1c | Between Groups | 50.519 | 2 | 25.260 | 9.049 | .003 |
| Within Groups | 36.290 | 13 | 2.792 | |||
| Total | 86.809 | 15 | ||||
| Mean number of drugs | Between Groups | 2.846 | 2 | 1.423 | .785 | .458 |
| Within Groups | 213.848 | 118 | 1.812 | |||
| Total | 216.694 | 120 | ||||
| Fasting Plasma | Between Groups | 10.580 | 2 | 5.290 | .486 | .616 |
| Glucose | Within Groups | 1109.207 | 102 | 10.875 | ||
| Total | 1119.787 | 104 | ||||
| Cost of medications | Between Groups | 1.784E7 | 2 | 8922409.439 | .445 | .642 |
| Within Groups | 2.347E9 | 117 | 2.006E7 | |||
| Total | 2.365E9 | 119 | ||||
| Duration of illness | Between Groups | 12.259 | 2 | 6.130 | .161 | .851 |
| Within Groups | 4061.705 | 107 | 37.960 | |||
| Total | 4073.964 | 109 | ||||
| Monthly income | Between Groups | .798 | 2 | .399 | .462 | .631 |
| Within Groups | 96.733 | 112 | .864 | |||
| Total | 97.530 | 114 | ||||
| AGE | Between Groups | 377.306 | 2 | 188.653 | 1.741 | .180 |
| Within Groups | 12893.317 | 119 | 108.347 | |||
| Total | 13270.623 | 121 | ||||
HbA1c = blood glycosylated haemoglobin concentration
df = degrees of freedom
F = F-ratio
Figure 3.
Relationship between duration of DM and the three levels of adherence at LAUTECH Teaching Hospital diabetes clinic
Duration of Illness = time since first diagnoses of diabetes mellitus (DM) was made
Adherence groups were defined based on the level of diabetes patient adherence to medications according to the Morisky Medication Adherence Scale (MMAS-8) questionnaire results
Figure 4.
Relationship between mean HbA1c and three levels of adherence at LAUTECH Teaching Hospital diabetes clinic
HbA1c = blood glycosylated haemoglobin concentration
Adherence groups were defined based on the level of diabetes patient adherence to medications according to the Morisky Medication Adherence Scale (MMAS-8) questionnaire results
Discussion
The results above have described, in detail, the prescribing pattern of antidiabetic drugs, some direct costs, and adherence of patients to treatment. Female patients made up the larger proportion of patients in our study; this reflects the general trend from similar studies among diabetes patients worldwide35–37. The mean age of 61.4 ± 10.5 years found in this study is close to the 58.15 ± 9.16 years and 61 ± 12.3 years recorded in work from Malaysia and the USA31,38.
Achieving and keeping good glycaemic control (fasting plasma glucose < 110mg/dl or 6.1 mmol/L) is the goal of pharmacotherapy among diabetes patients, though this is not possible in a large percentage of them. Less than 50% of the study participants had good glycaemic control, similar to the 40.3% in another Nigerian study34. Studies conducted in Ethiopia and Nepal found glycaemic control rates of 41.8% and 49.5% respectively39,40. Of the 16 patients (12.4%) who were able to obtain (afford) HbA1c as a biomarker for glycaemic control, 50% of them had their values within normal limits. The mean plot for HbA1c (Figure 3) reveals a trend of higher values of HbA1c in poorly adherent patients. This supports the statistical significant difference found when the average HbA1c was compared between the three adherence groups. Though HbA1c was tested in a small number of patients (because of financial constraints), this trend shows the importance of HbA1c as a useful tool for monitoring medication adherence among diabetes patients.
The number of drugs prescribed for patients has been found to affect adherence to treatment. The average number of prescribed medications in this study was 4.1 ± 1.4; this is close to the 4.6 found in another Nigerian study and less than the 5.56 ± 2.52 in an Indian study24,41. Oral hypoglycaemic agents were the most prescribed drugs in our study, with metformin either alone or in combination with other hypoglycaemic agents. Yusuff et al. found that oral hypoglycaemic agents were prescribed in 86% of cases while a similar study involving 384 type 2 diabetes patients had over 91% of these patients prescribed oral hypoglycaemic drugs23,40. Oral agents from the thiazolidinedione and DPP4-inhibitor groups were prescribed for only three patients during the duration of this study; this is likely because of the higher cost of these drugs, their availability and potential safety issues. The cost of drugs formed a substantial part (72.3%) of the calculated direct costs in this study; this was higher than the 42.4% and 46% reported in studies from India and Pakistan42,43. The aggressive development and marketing of generic medicines in these two Asian countries may account for the significantly lesser medication costs. Taking a cue from the Asian examples, it may be necessary for authorities in Nigeria to aggressively promote the use of cheap and effective generic medicines to increase access and adherence to these medications. The mean cost of monthly medications of about NGN N6556.60 (USD $39.70) found in this study indicates that a large chunk of the patients' income is spent on drugs: over 70% of the patients in this study earned less than NGN N50,000 (USD $303) monthly. This mismatch obviously has the potential to negatively impact patients' medication adherence; however, the communal way of life in Nigerian society means that the family usually supports or sponsors healthcare expenditures of any ill member.
Using the MMAS-8, medication adherence was recorded as good (40.6%), moderate (32.8%), or poor (26.6%). Using the same study tool, Jamons et al. identified only 16.9% of patients as poorly adherent in a study among 131 Palestinian diabetic patients, while Abebe et al. recorded 45.9%, 28.7% and 25.4% with high, medium and low adherence, respectively19,44. A Nigerian study using another tool, the Adherence and Self-Management Monitoring Tool (ASMMT), found 59% of its sample diabetes patients to be non-adherent23. Ahmad et al. in a study among Malaysian diabetic patients found 53% to be non-adherent using the Medication Compliance Questionnaire, while a study using pill count and other self-reporting methods found adherence to be adequate in only 29% of patients20,45. The predictors of medication non-adherence shown in previous studies include disease and medication beliefs, poverty, service dissatisfaction, and using traditional medicines19,31,40,46,47. This study, in addition to some of these aforementioned factors, identified inadequate information about the pharmacotherapy of diabetes, high pill burden and non-availability of prescribed drugs as obstacles to medication adherence among diabetes patients.
Conclusion
This study identified a satisfactory level of adherence to diabetes medications in the population evaluated. There is a need for the integration of generic medicines into routine care as a way of further reducing the burden of healthcare expenditure on the patients. The role or influence of healthcare insurance on medical expenditure among diabetes patients in the Nigerian setting is a potential research topic for the future.
Study Limitations
The relatively small sample size and the fact that only one centre was used for the study were major limitations. This would mean that results of the study might not be representative of other regions of the country. Additionally, some respondents refused to disclose some sensitive information such as income level and age because of fear about possible use of their information for tax-related or other of ficial purposes. Though bias could arise from participant self-reporting and patients' recall ability, the standardization and validation of the data collection instruments used in the study act to mitigate such biases. Measuring adherence for all medications being taken by diabetes patients and not antidiabetic agents alone may pose some questions. DM is a multi-system disease, however, with a myriad of complications, and it therefore might not have been as practical to analyze only adherence to antidiabetic agents.
Acknowledgements
The authors are grateful to the entire staff of the medical outpatient department of the Ladoke Akintola University of Technology Teaching Hospital, Ogbomosho, Nigeria for their cooperation and support during the study period.
References
- 1.Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010 Jun 26;375(9733):2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 2.Ramachandran A, Snehalatha C. Current scenario of diabetes in India. J Diabetes. 2009 Mar;1(1):18–28. doi: 10.1111/j.1753-0407.2008.00004.x. [DOI] [PubMed] [Google Scholar]
- 3.Msyamboza KP, Mvula CJ, Kathyola D. Prevalence and correlates of diabetes mellitus in Malawi: population-based national NCD STEPS survey. BMC Endocr Disord. 2014;14:41. doi: 10.1186/1472-6823-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. The Lancet Diabetes & Endocrinology. 2014;2(1):56–64. doi: 10.1016/S2213-8587(13)70112-8. [DOI] [PubMed] [Google Scholar]
- 5.Owoaje EE, Rotimi CN, Kaufman JS, Tracy J, Cooper RS. Prevalence of adult diabetes in Ibadan, Nigeria. East Afr Med J. 1997 May;74(5):299–302. [PubMed] [Google Scholar]
- 6.Nyenwe EA, Odia OJ, Ihekwaba AE, Ojule A, Babatunde S. Type 2 diabetes in adult Nigerians: a study of its prevalence and risk factors in Port Harcourt, Nigeria. Diabetes Res Clin Pract. 2003 Dec;62(3):177–185. doi: 10.1016/j.diabres.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Dahiru T, Jibo A, Hassan AA, Mande AT. Prevalence of diabetes in a semi-urban community in Northern Nigeria. Niger J Med. 2008 Oct-Dec;17(4):414–416. doi: 10.4314/njm.v17i4.37423. [DOI] [PubMed] [Google Scholar]
- 8.Alebiosu OC, Familoni OB, Ogunsemi OO, Raimi TH, Balogun WO, Odusan O, et al. Community based diabetes risk assessment in Ogun state, Nigeria (World Diabetes Foundation project 08-321) Indian J Endocrinol Metab. 2013 Jul;17(4):653–658. doi: 10.4103/2230-8210.113756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000 Aug 12;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005 Dec 22;353(25):2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008 Oct 9;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 12.Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassai B, et al. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343:d4169. doi: 10.1136/bmj.d4169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu AP, Yu YF, Nichol MB. Estimating the effect of medication adherence on health outcomes among patients with type 2 diabetes-an application of marginal structural models. Value Health. 2010 Dec;13(8):1038–1045. doi: 10.1111/j.1524-4733.2010.00787.x. [DOI] [PubMed] [Google Scholar]
- 14.DiBonaventura M, Wintfeld N, Huang J, Goren A. The association between nonadherence and glycated hemoglobin among type 2 diabetes patients using basal insulin analogs. Patient Prefer Adherence. 2014;8:873–882. doi: 10.2147/PPA.S55550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Breitscheidel L, Stamenitis S, Dippel FW, Schoffski O. Economic impact of compliance to treatment with antidiabetes medication in type 2 diabetes mellitus: a review paper. J Med Econ. 2010 Mar;13(1):8–15. doi: 10.3111/13696990903479199. [DOI] [PubMed] [Google Scholar]
- 16.Wild H. The economic rationale for adherence in the treatment of type 2 diabetes mellitus. Am J Manag Care. 2012 Apr;18(3 Suppl):S43–S48. [PubMed] [Google Scholar]
- 17.Benner JS, Chapman RH, Petrilla AA, Tang SS, Rosenberg N, Schwartz JS. Association between prescription burden and medication adherence in patients initiating antihypertensive and lipid-lowering therapy. Am J Health Syst Pharm. 2009 Aug 15;66(16):1471–1477. doi: 10.2146/ajhp080238. [DOI] [PubMed] [Google Scholar]
- 18.Farsaei S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Adherence to glyburide and metformin and associated factors in type 2 diabetes in isfahan, iran. Iran J Pharm Res. 2011 Fall;10(4):933–939. [PMC free article] [PubMed] [Google Scholar]
- 19.Abebe SM, Berhane Y, Worku A. Barriers to diabetes medication adherence in North West Ethiopia. Springerplus. 2014;3:195. doi: 10.1186/2193-1801-3-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmad NS, Ramli A, Islahudin F, Paraidathathu T. Medication adherence in patients with type 2 diabetes mellitus treated at primary health clinics in Malaysia. Patient Prefer Adherence. 2013;7:525–530. doi: 10.2147/PPA.S44698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mukherjee S, Sharmasarkar B, Das KK, Bhattacharyya A, Deb A. Compliance to anti-diabetic drugs: observations from the diabetic clinic of a medical college in kolkata, India. J Clin Diagn Res. 2013 Apr;7(4):661–665. doi: 10.7860/JCDR/2013/5352.2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pascal IG, Ofoedu JN, Uchenna NP, Nkwa AA, Uchamma GU. Blood Glucose Control and Medication Adherence Among Adult Type 2 Diabetic Nigerians Attending A Primary Care Clinic in Under-resourced Environment of Eastern Nigeria. N Am J Med Sci. 2012 Jul;4(7):310–315. doi: 10.4103/1947-2714.98590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yusuff KB, Obe O, Joseph BY. Adherence to anti-diabetic drug therapy and self management practices among type-2 diabetics in Nigeria. Pharm World Sci. 2008 Dec;30(6):876–883. doi: 10.1007/s11096-008-9243-2. [DOI] [PubMed] [Google Scholar]
- 24.Adisa R, Fakeye TO. Effect of number and type of antidiabetes medications on adherence and glycemia of ambulatory type 2 diabetes patients in southwestern Nigeria. Pharm Pract (Granada) 2013 Jul;11(3):156–165. doi: 10.4321/s1886-36552013000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005 May;118 Suppl 5A:27S–34S. doi: 10.1016/j.amjmed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Odeyemi IA, Nixon J. Assessing equity in health care through the national health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. Int J Equity Health. 2013;12:9. doi: 10.1186/1475-9276-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Onoka CA, Hanson K, Hanefeld J. Towards universal coverage: a policy analysis of the development of the National Health Insurance Scheme in Nigeria. Health Policy Plan. 2014 Oct 21; doi: 10.1093/heapol/czu116. [DOI] [PubMed] [Google Scholar]
- 28.Onwujekwe O, Hanson K, Uzochukwu B. Examining inequities in incidence of catastrophic health expenditures on different healthcare services and health facilities in Nigeria. PLoS One. 2012;7(7):e40811. doi: 10.1371/journal.pone.0040811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008 May;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Lee WY, Ahn J, Kim JH, Hong YP, Hong SK, Kim YT, et al. Reliability and validity of a self-reported measure of medication adherence in patients with type 2 diabetes mellitus in Korea. J Int Med Res. 2013 Aug;41(4):1098–1110. doi: 10.1177/0300060513484433. [DOI] [PubMed] [Google Scholar]
- 31.Al-Qazaz H, Sulaiman SA, Hassali MA, Shafie AA, Sundram S, Al-Nuri R, et al. Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. Int J Clin Pharm. 2011 Dec;33(6):1028–1035. doi: 10.1007/s11096-011-9582-2. [DOI] [PubMed] [Google Scholar]
- 32.Ajayi EA, Adeoti AO, Ajayi IA, Ajayi AO, Adeyeye VO. Adherence to Antihypertensive Medications and Some of Its Clinical Implications in Patients Seen At a Tertiary Hospital in Nigeria [Google Scholar]
- 33.Adewuya AO, Owoeye OA, Erinfolami AR, Coker AO, Ogun OC, Okewole AO, et al. Prevalence and correlates of poor medication adherence amongst psychiatric outpatients in southwestern Nigeria. Gen Hosp Psychiatry. 2009 Mar-Apr;31(2):167–174. doi: 10.1016/j.genhosppsych.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Adisa R, Fakeye TO, Fasanmade A. Medication adherence among ambulatory patients with type 2 diabetes in a tertiary healthcare setting in southwestern Nigeria. Pharm Pract (Granada) 2011 Apr;9(2):72–81. doi: 10.4321/s1886-36552011000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rhee MK, Slocum W, Ziemer DC, Culler SD, Cook CB, El-Kebbi IM, et al. Patient adherence improves glycemic control. Diabetes Educ. 2005 Mar-Apr;31(2):240–250. doi: 10.1177/0145721705274927. [DOI] [PubMed] [Google Scholar]
- 36.Sweileh WM, Zyoud SH, Abu Nab'a RJ, Deleq MI, Enaia MI, Nassar SM, et al. Influence of patients' disease knowledge and beliefs about medicines on medication adherence: findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14:94. doi: 10.1186/1471-2458-14-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mafauzy M. Diabetes control and complications in public hospitals in Malaysia. Med J Malaysia. 2006 Oct;61(4):477–483. [PubMed] [Google Scholar]
- 38.Ahia CL, Holt EW, Krousel-Wood M. Diabetes care and its association with glycosylated hemoglobin level. Am J Med Sci. 2014 Mar;347(3):245–247. doi: 10.1097/MAJ.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 39.Shrestha SS, Shakya R, Karmacharya BM, Thapa P. Medication adherence to oral hypoglycemic agents among type II diabetic patients and their clinical outcomes with special reference to fasting blood glucose and glycosylated hemoglobin levels. Kathmandu Univ Med J (KUMJ) 2013 Jul-Sep;11(43):226–232. doi: 10.3126/kumj.v11i3.12510. [DOI] [PubMed] [Google Scholar]
- 40.Wabe NT, Angamo MT, Hussein S. Medication adherence in diabetes mellitus and self management practices among type-2 diabetics in Ethiopia. N Am J Med Sci. 2011 Sep;3(9):418–423. doi: 10.4297/najms.2011.3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Acharya KG, Shah KN, Solanki ND, Rana DA. Evaluation of antidiabetic prescriptions, cost and adherence to treatment guidelines: A prospective, cross-sectional study at a tertiary care teaching hospital. J Basic Clin Pharm. 2013 Sep;4(4):82–87. doi: 10.4103/0976-0105.121653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grover S, Avasthi A, Bhansali A, Chakrabarti S, Kulhara P. Cost of ambulatory care of diabetes mellitus: a study from north India. Postgrad Med J. 2005 Jun;81(956):391–395. doi: 10.1136/pgmj.2004.024299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khowaja LA, Khuwaja AK, Cosgrove P. Cost of diabetes care in outpatient clinics of Karachi, Pakistan. BMC Health Serv Res. 2007;7:189. doi: 10.1186/1472-6963-7-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jamous RM, Sweileh WM, Abu-Taha AS, Sawalha AF, Zyoud SH, Morisky DE. Adherence and satisfaction with oral hypoglycemic medications: a pilot study in Palestine. Int J Clin Pharm. 2011 Dec;33(6):942–948. doi: 10.1007/s11096-011-9561-7. [DOI] [PubMed] [Google Scholar]
- 45.Mateo JF, Gil-Guillen VF, Mateo E, Orozco D, Carbayo JA, Merino J. Multifactorial approach and adherence to prescribed oral medications in patients with type 2 diabetes. Int J Clin Pract. 2006 Apr;60(4):422–428. doi: 10.1111/j.1368-5031.2006.00799.x. [DOI] [PubMed] [Google Scholar]
- 46.Mann DM, Ponieman D, Leventhal H, Halm EA. Predictors of adherence to diabetes medications: the role of disease and medication beliefs. J Behav Med. 2009 Jun;32(3):278–284. doi: 10.1007/s10865-009-9202-y. [DOI] [PubMed] [Google Scholar]
- 47.Walz L, Pettersson B, Rosenqvist U, Deleskog A, Journath G, Wandell P. Impact of symptomatic hypoglycemia on medication adherence, patient satisfaction with treatment, and glycemic control in patients with type 2 diabetes. Patient Prefer Adherence. 2014;8:593–601. doi: 10.2147/PPA.S58781. [DOI] [PMC free article] [PubMed] [Google Scholar]