Abstract
Context:
Bombay blood group although rare is found to be more prevalent in the Western and Southern states of India, believed to be associated with consanguineous marriage.
Aims:
To estimate the prevalence of the Bombay blood group (Oh) in the urban population of Puducherry. To find the effect of urbanization on consanguineous marriage and to establish whether consanguinity plays a part in the prevalence of Oh group. To compare Oh group prevalence with that of other neighboring states, where population is not predominantly urban.
Settings and Design:
This is a descriptive study in a tertiary care hospital in Puducherry, over a period of 6 years.
Materials and Methods:
All blood samples showing ‘O’ group were tested with anti-H lectin. Specialized tests like Adsorption Elution Technique, inhibition assay for determination of secretor status were performed on Oh positive cases. Any history of consanguineous marriage was recorded.
Statistical Analysis Used:
All variables were categorical variable and percentage and proportions were calculated manually.
Results:
Analysis of the results of 35,497 study subjects showed that the most common group was ‘O’ group constituting 14,164 (39.90%) of subjects. Only three “Oh” that is, Bombay phenotype (0.008%) were detected. Consanguinity was observed in two cases (66.66%).
Conclusions:
This study shows the prevalence of Bombay blood group representing the urban population of Puducherry, to be high (0.008%) and associated with consanguineous marriage (66.66%). Thus, consanguinity is still an important risk factor present, even in an urban population in Southern India.
Keywords: Anti-H antibody, Bombay blood group, H antigen
Introduction
The prevalence of Bombay blood group is high in South India and is believed to be associated with high incidence of consanguineous marriage. Consanguinity is expected to be more in rural population than in urban population.[1] The population of Puducherry is predominantly urban according to census 2011, while the population in the neighboring states of Tamil Nadu is both urban and rural and Karnataka and Andhra Pradesh is predominantly rural.[2] We, thus expected the prevalence of Bombay blood group as well as consanguineous marriage to be less in the urban population of Puducherry.
Materials and Methods
This is a descriptive study in a tertiary care hospital in Puducherry, covering its urban population, screened at its blood bank. Both the recipients and donor subjects were included in the study over a period of 6 years. Donors were selected as per the blood banking norms. The ABO and Rh-D typing were performed according to the blood transfusion manual, 2nd Edition; 2003, issued by Directorate General of Health Services (DGHS), Government of India.[3] Both cell and serum grouping were done. Red cell typing was done with commercial anti-sera. Serum grouping was done using known cells from freshly pooled AB and O blood units.
All blood samples showing ‘O’ group were tested for Bombay blood group by slide and tube method. In slide method, one drop each of commercial anti-H lectin (Tulip Diagnostics Ltd.) and negative control (normal saline) was placed on a slide, mixed and checked for agglutination. In tube method, one drop of anti-H lectin and one drop of 5% red cell suspension, washed in isotonic saline solution were mixed, shaken to homogenize, then centrifuged and checked for agglutination.
Bombay blood group was confirmed by Adsorption Elution Technique, to rule out para Bombay phenotype which carry weak subgroups of A or B. Red cells of Bombay blood group patients were washed, reagent antibody added (anti-A or -B), mixed, incubated and packed. After washing thoroughly eight times, it was eluted and elute was tested with A or B cells.
To check the secretory status of the Bombay blood group, inhibition test was performed. Fresh saliva of these patients were collected, boiled, centrifuged, and the supernatant used for testing. In two tubes marked one and two, two drops each of anti-H lectin was taken. Saliva and normal saline (each 100 μl) were taken in each tube, mixed well and incubated. To this, 50 μl of 5% cell suspension of known ‘O’ red cells were added, mixed, incubated, and centrifuged. All the procedures were done according to AABB and DGHS Technical Manual.[3,4]
History of any consanguineous marriage was recorded in the index cases. All relatives who volunteered to participate in the study were checked for the presence of Bombay phenotype.
Results
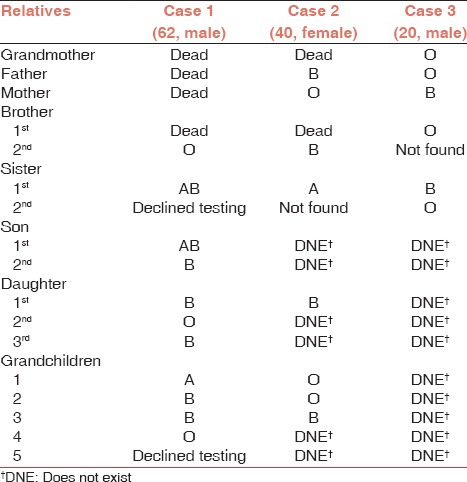
Analysis of the results of 35,497 study subjects showed that the most common group was ‘O’ group constituting 14,164 (39.90%) of subjects. Only three “Oh” that is, Bombay phenotypes (0.008%) were detected in the entire study group. Among O blood group subjects detected on routine blood grouping, as many as 0.02% had Bombay blood group. In Absorption Elution Technique, there was no agglutination with A or B cells confirming it to be Bombay and not para Bombay phenotype. Saliva testing of these cases by inhibition assay showed agglutination and proved them to be nonsecretor of H antigen. Second degree consanguineous marriage was observed in two cases out of three (66.66%). All the three cases were recipients and two of them needed blood transfusion. Bombay blood group could not be detected in any other relatives who participated in our study [Table 1].
Table 1.
Depicting the family tree of the three positive cases with their blood group result confirmed in our institute
Discussion
The discovery of this rare blood group, “Bombay phenotype” in three unrelated individuals in Mumbai by Bhende et al. was an important event in the field of immune-hematology.[5] These individuals had antibodies in plasma reacting with all red cells ABO phenotypes. This phenotype was characterized by the absence of A, B, and H antigens on red cells. The serum of these persons had anti-A, anti-B, and anti-H. These individuals were, therefore, genetically termed as homozygous recessive “hh” or Bombay phenotype. They phenotype as blood Group ‘O’ on normal ABO grouping but on cross matching shows incompatibility to ‘O’ blood group. They are Lewis antigen positive (a+).[5]
The H locus contains the FUT1 gene, which is expressed on red blood cells. The Se locus contains the FUT2 gene, which is expressed in secretory glands. FUT1 and FUT2 gene are located on chromosome 19q13.3. FUT1 and FUT2 are tightly linked, being only 35 kb apart. Kaneko et al. found out that the H null Bombay phenotype depends on a nonsense mutation at position 695 from G to A (G695A) of the FUT1or h1 gene.[6] Their salivary nonsecretor phenotype is due to a point mutation in C357T in FUT2 gene. The red cell H weak Reunion phenotype or para Bombay phenotype is due to four inactivated H gene alleles, h2, h3, h4, h5.[6]
In Bombay Blood group people, without fucose, neutrophils lack sialyl Lex and thus cannot roll and ingest bacteria. Thus, these patients can have high white blood cell count and severe recurrent infections. This condition is called leukocyte adhesion deficiency II or congenital disorder of glycosylation II.[7] In our cases, only the third case, gave some history of recurrent but infrequent lower respiratory tract infections, but not significantly.
If patients with anti-H in their circulation receive transfusions of blood that contains the H antigen (e.g., blood group O), they are at risk of suffering an acute hemolytic transfusion reaction.[5] Two cases in our series needed transfusion; one was managed through autologous transfusion while another received transfusion from a Bombay blood group individual through record of rare donors. The maternal production of anti-H during pregnancy in an Oh phenotype mother could cause hemolytic disease in a fetus who did not inherit the mother's Bombay phenotype.[8] In our case series, one 40-year female patient with Bombay blood group had one issue with normal delivery but she did not give any history of any complication during child birth or thereafter.
The probability of finding a person with Bombay phenotype is one for every 250,000 people worldwide. India has the highest number with one Bombay blood type per 7600 people.[9] After its discovery in1952,[5] Bombay blood group has been reported by various other workers in different parts of India and even in other Asian and European countries.[10] According to Sathe et al., 179 cases of Bombay phenotype were detected of which 112 was found in Maharashtra, followed by 14 cases in Karnataka, 8 cases in Andhra Pradesh, 6 cases in Goa, 5 cases in Gujarat and so on in decreasing order. All the cases were hospital cases and random population screening was not done.[11]
Balgir did extensive study among the Bhuyan tribe in Orissa and found incidence of Bombay blood group one in 278.[9] He also studied the Kutia Kondh tribe in the Kandhamal district of Orissa and found 1 in 33 incidence of Bombay phenotype.[12] He concluded that the high prevalence of Bombay Blood group in these tribes was due to the practice of endogamy and consanguinity. Consanguinity results in increased homozygous expression of rare recessive genetic characters like the Bombay phenotype. Thus, the incidence is higher in those states of India where consanguineous mating is more prevalent especially in Southern and Western states like Andhra Pradesh, Tamil Nadu, Karnataka, Maharashtra, Gujrat etc., than other states.[9,12,13]
Among the Southern states, a study by Geetha et al. in Karnataka covering urban as well as rural population found six Bombay phenotype among 37,117 people screened with consanguinity observed in four out of six cases.[13] Another study by Verma et al. in Andhra Pradesh found 13 Bombay phenotype among 26,638 subjects with consanguinity among parents in ten cases. Their study group was also a mixed population of urban and rural.[14] Another study by Periyavan et al. in and around Bangalore found two O group among 36,964 donors.[15]
Among the western states of India, Bhatia and Sanghvi found Bombay phenotype 1 in 13,000 cases,[16] Bhatia and Sathe found incidence 1 in 7600,[17] both in the urban population of Mumbai. Gorakshakar et al. after screening the rural population of Maharashtra found 1 in 4500 incidence.[18] Prevalence in the North Indian states is rarer. A case report by Kaur et al. in Chandigarh found Bombay phenotype in two North Indian brothers.[19]
The Bombay phenotype was also detected in other Asian countries like Japan,[6] Malaysia,[11] Sri Lanka,[20] Thailand.[21] Ravanparvar et al. studied three different population in Tehran, first Indian, second two families with Bombay phenotype history and the third voluntary donors.[22] They found one Bombay blood type among them. Yunis et al. found seven individuals in USA with Bombay phenotype in two generations of an Indian family.[23] Sathe et al. in reported 24 cases of Bombay blood group in South Africa in 11 families presumed to be hailing from Andhra Pradesh or Tamil Nadu.[11] Recently, a large series of H deficient individuals around 1:1000 were found in Reunion Island near Madagascar indicating Bombay blood group in mostly confined to South East Asian countries.[24]
This study shows the prevalence of Bombay blood group in and urban population of Puducherry to be high 0.008%. The high prevalence is also related to the high rate of consanguineous marriage. The neighboring states of Tamil Nadu and Karnataka with predominant rural population did not have such high prevalence, Tamil Nadu-0.004%, Karnataka - 0.005%. However, another neighboring state like Andhra Pradesh also with predominant rural population showed high prevalence-0.05%.[14] Thus the prevalence of Bombay blood group does not depend on urbanization. High prevalence is found wherever consanguineous mating is still highly followed, which remains a dominant risk factor. More random population-based studies are required on this subject to ascertain the prevalence of this blood group in the population so that even basic health care services in urban as well as rural population should have the facility to test for Bombay Blood Group.
Acknowledgements
We would like to acknowledge the contribution of all the technical staff of our blood bank who very patiently and sincerely did their job. We would also like to thank the concerned faculty and staff of the Department of Gynaecology, Urology and Orthopaedics who helped us gain information about the concerned cases as well as contacting the relatives of these people. Also, our heartfelt gratitude goes to all the faculty and PG's of our own Pathology Department. Last but not the least, our thanks to the management of our institution who always encourages and promotes such studies.
Footnotes
Source of Support: Nil
Conflicting Interest: None declared.
References
- 1.Verma IC, Prema A, Puri RK. Health effects of consanguinity in Pondicherry. Indian Pediatr. 1992;29:685–92. [PubMed] [Google Scholar]
- 2.Indiafacts. India census 2011. [Last accessed on 2013 Mar 16]. Available from: http://www.indiafacts.in/india-census-2011/urban-rural-population-o-india .
- 3.Brecher ME, editor. 15th ed. Bethesda, Maryland, USA: American Association of Blood Banks; 2005. AABB, Technical Manual. [Google Scholar]
- 4.Saran RK. 2nd ed. New Delhi, India: Directorate General of Health Services (DGHS); 2003. Transfusion Medicine: Technical Manual. [Google Scholar]
- 5.Bhende YM, Deshpande CK, Bhatia HM, Sanger R, Race RR, Morgan WT, et al. A “new” blood group character related to the ABO system. Lancet. 1952;1:903–4. [PubMed] [Google Scholar]
- 6.Kaneko M, Nishihara S, Shinya N, Kudo T, Iwasaki H, Seno T, et al. Wide variety of point mutations in the H gene of Bombay and para-Bombay individuals that inactivate H enzyme. Blood. 1997;90:839–49. [PubMed] [Google Scholar]
- 7.Etzioni A, Tonetti M. Leukocyte adhesion deficiency II-from A to almost Z. Immunol Rev. 2000;178:138–47. doi: 10.1034/j.1600-065x.2000.17805.x. [DOI] [PubMed] [Google Scholar]
- 8.Bhattacharya S, Makar Y, Laycock RA, Gooch A, Poole J, Hadley A. Outcome of consecutive pregnancies in a patient with Bombay (Oh) blood group. Transfus Med. 2002;12:379–82. doi: 10.1046/j.1365-3148.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 9.Balgir RS. Identification of a rare blood group, “Bombay (Oh) phenotype,” in Bhuyan tribe of Northwestern Orissa, India. Indian J Hum Genet. 2007;13:109–13. doi: 10.4103/0971-6866.38985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan MQ. Bombay blood Group: A case report. Pac J Sci Technol. 2009;10:333–7. [Google Scholar]
- 11.Sathe MS, Vasantha K, Mhaisalkar P, Gorakshakar AC. Distribution of Bombay (Oh) phenotypes in India. J Indian Anthropol Soc. 1988;23:277–80. [Google Scholar]
- 12.Balgir RS. Detection of a rare blood group “Bombay (Oh) phenotype” among the Kutia Kondh primitive tribe of Orissa, India. Int J Hum Genet. 2005;5:193–8. [Google Scholar]
- 13.Geetha R, Kavitha GU, Deepti P, Anitha MR, Vijayanath V. Prevalence of Bombay blood group in a tertiary health care centre, Karnataka. Elixir Pharm 31A (2011); 1980. [Last accessed on 2013 Mar 16]. Available from: http://www.elixirpublishers.com/articles/1349860432_31A%20(2011)%201980.pdf .
- 14.Verma A, Vani KG, Chaitanya Kumar IS, Jothi Bai DS. Prevalence of Bombay blood group in a tertiary care hospital, Andhra Pradesh, India. Asian J Transfus Sci. 2011;5:57–8. doi: 10.4103/0973-6247.76006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Periyavan S, Sangeetha SK, Marimuthu P, Manjunath BK, Seema DM. Distribution of ABO and Rhesus-D blood groups in and around Bangalore. Asian J Transfus Sci. 2010;4:41. doi: 10.4103/0973-6247.59391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhatia HM, Sanghvi LD. Rare blood groups and consanguinity: (Bombay) phenotype. Vox Sang. 1962;7:245–8. doi: 10.1111/j.1423-0410.1962.tb03250.x. [DOI] [PubMed] [Google Scholar]
- 17.Bhatia HM, Sathe MS. Incidence of “Bombay” (Oh) phenotype and weaker variants of A and B antigen in Bombay (India) Vox Sang. 1974;27:524–32. doi: 10.1111/j.1423-0410.1974.tb02450.x. [DOI] [PubMed] [Google Scholar]
- 18.Gorakshakar AC, Sathe MS, Shirsat SR, Bhatia HM. Genetic studies in Ratnagiri and Sindhudurg Districts of Maharashtra: Incidence of ABO, Rho(D), Inª antigens, G6PD deficiency and abnormal haemoglobins. J Indian Anthropol Soc. 1987;22:38–46. [Google Scholar]
- 19.Kaur P, Basu S, Bedi RK, Kaur G. Bombay phenotype in two North Indian brothers: A case report. Indian J Pathol Microbiol. 2007;50:919–21. [PubMed] [Google Scholar]
- 20.de Zoysa NS. Bombay (Oh) phenotype among Sinhalese in Sri Lanka. Ceylon Med J. 1985;30:29–36. [PubMed] [Google Scholar]
- 21.Sringarm S, Sombatpanich B, Chandanayingyong D. A case of Oh (Bombay) blood found in a Thai-Muslim patient. Vox Sang. 1977;33:364–8. doi: 10.1111/j.1423-0410.1977.tb02258.x. [DOI] [PubMed] [Google Scholar]
- 22.Ravanparvar N, Samiee SH, Asadi G, Sahebjamme M, Lotfi P, Taherian D. The survey of prevalence of rare Bombay (Oh) blood group among 3 different population in Tehran. Sci J Blood Transfus Organ. 2004;1:43–9. [Google Scholar]
- 23.Yunis EJ, Svardal JM, Bridges RA. Genetics of the Bombay phenotype. Blood. 1969;33:124–32. [PubMed] [Google Scholar]
- 24.Le Pendu J, Gerard G, Vitrac D, Juszczak G, Liberge G, Rouger P, et al. H-deficient blood groups of Reunion island. II. Differences between Indians (Bombay Phenotype) and whites (Reunion phenotype) Am J Hum Genet. 1983;35:484–96. [PMC free article] [PubMed] [Google Scholar]


