Abstract
Background and Objectives:
Human T-cell lymphotropic virus type-I (HTLV-I) infection is considered as a public health challenge in endemic areas. The virus is associated with severe diseases, such as adult T-cell leukemia/lymphoma, and HTLV-I-associated myelopathy/tropical spastic paraparesis. One of the major routes of the HTLV-I transmission includes blood transfusion. Sabzevar is located in the endemic region of HTLV-I infection. The aim of the present study was to determine the seroprevalence of HTLV-I infection in the blood donors in Sabzevar.
Materials and Methods:
A total of 35,067 blood donors in Sabzevar from March 2009 to April 2012 who were screened with HTLV-I on the enzyme-linked immunosorbent assay screening test were included in this survey. Reactive samples that confirmed by western blot were considered to be seropositive cases. The required data were obtained from blood donors’ database of blood transfusion service.
Results:
The overall prevalence of HTLV-1 based on the positive result of western blot test was 0.14%. The seropositive donors aged 17–59 years with a mean age of 38.10 ± 11.82. The prevalence rates of HTLV-I infection in 3 years of study were 0.19%, 0.14%, and 0.09%, respectively. A significant relation between age, sex, educational level, and history of blood donation was observed with seropositivity of HTLV-I.
Conclusion:
The improvement of donor selection and laboratory screening caused a decline in the prevalence of infection in blood donors. Given the lower prevalence of infection in regular donors with lower age and higher educational level, more efforts should be done to attract blood donors from these populations.
Keywords: Blood donors, human T-cell lymphotropic virus type-I, Sabzevar, seroprevalence, Iran
Introduction
Human T-cell lymphotropic virus type-I (HTLV-I) is a deltavirus of retroviridae family and about 15–20 million people worldwide are infected with HTLV-I. Although most infected individuals remain asymptomatic, about 5% of infected individuals are infected by HTLV-I related diseases including adult T-cell leukemia/lymphoma and tropical spastic paraparesis.[1,2,3] HTLV-I is distributed worldwide. However, HTLV-I infection is endemic in some regions such as Japan, Taiwan, Caribbean Basin, Central and South Africa, the Middle East, the southern United States and northeastern Iran.[3,4] According to Azarpazhooh et al., the prevalence of HTLV-I infection in the general population of Sabzevar was 1.66%.[4] In the only study conducted on blood donors in Sabzevar in 2007-2008, the prevalence of HTLV-I infection was 0.26%.[5] According to the recent studies in Mashhad (the capital of Khorasan Razavi province), the prevalence rates of HTLV-I infection in the general population and blood donors were 2.12% and 0.18%, respectively.[6,7] The prevalence of HTLV-I infection in blood donors in Chaharmahal-Bakhtiari, West Azerbaijan, Ilam, Hormozgan, and Bushehr was 0.62%, 0.34%, 0.21%, 0.18%, and 0.01%, respectively.[8,9,10,11,12]
Human T-cell lymphotropic virus type-I is mainly transmitted through sexual contact with an infected person, from mother to child through breastfeeding and cell-containing blood products.[1,2] HTLV-I transmission through blood products containing white blood cells is about 44%. However, there is no report on the HTLV-I transmission through cell-free blood products like plasma. Therefore, it is necessary to screen donated blood in endemic areas to limit the spread of HTLV-I infection. The laboratory screening of HTLV-I/II on blood donations began in northeastern Iran since 1995.[6,13] HTLV-I infection is considered as a public health challenge in the world, especially in endemic areas. Given the burden of disease caused by HTLV-I infection as well as unpleasant psychological and social impacts of infection on seropositive individuals, it is necessary to determine the prevalence of infection to take necessary measures to prevent and control HTLV-I infection. Sabzevar is a historic and ancient city and the second largest city in Khorasan Razavi province. Sabzevar is considered as one of endemic regions of HTLV-I infection in the world. Continuous epidemiological studies in endemic areas lead to continuous monitoring of infection changes in the community while updating information about HTLV-I infection. Accordingly, continuous studies on the prevalence of HTLV-I infection are required. In addition, such studies will reveal the prevalence and distribution pattern of the infection changes over time. It leads to more awareness of public health managers to control the spread of HTLV-I infection. The aim of the present study is to review the prevalence of HTLV-I infection in blood donors in Sabzevar from March 2009 to April 2012.
Materials and Methods
This is a cross-sectional study. The required data were collected from blood donors’ database of Sabzevar Blood Transfusion Center from March 2009 to April 2012 using census method. All samples were detected by enzyme-linked immunosorbent assay (ELISA) screening test using standard kits approved by the Iranian Blood Transfusion Organization. All the donors who were positive for anti-HTLV-I/II on the ELISA screening test (double check) using the (Adaltis Srl, viaDurini, Italy) kit and the Western blot confirmatory test using (Mp Biomedical Asia Pacific Pte. Ltd., Singapore), were considered positive cases of HTLV-I infection. The demographic characteristics including age, gender, marital status, educational level, and the history of blood donation. The data were recorded in the database. A total of 100 blood donors with normal laboratory results were randomly selected as a control group at the same study period, and their data were entered into the database. The collected data were analyzed using descriptive and inferential statistical techniques (Chi-square test and t-test) by using computer software (SPSS, SPSS Inc., IL, USA).
Results
Following initial screening by a physician, 35,067 volunteers donated blood at Sabzevar Blood Transfusion Center. Of this, 31,581 (90.1%) were male and 3486 (9.9%) were female. According to western blot confirmatory test, 50 blood donors were seropositive in terms of anti-HTLV-I/II.
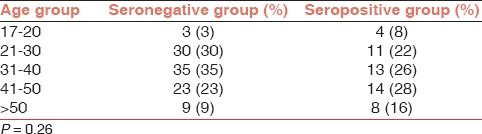
The overall prevalence of HTLV-I infection was 0.14%. The seropositive donors aged 17-59 years with a mean age of 38.10 ± 11.82 years. The control group aged 19–62 years with a mean age of 35.77 ± 10.47. The population was divided into five age groups of 17-20, 21–30, 31-40, 41-50, and older than 50 years. Most of infected donors aged 41–50 years (28%). According to t-test results, the age distribution of two groups was significantly different (P = 0.26). On other words, the older individuals showed higher positive HTLV-I antibody levels [Table 1].
Table 1.
Age distribution in two compared groups
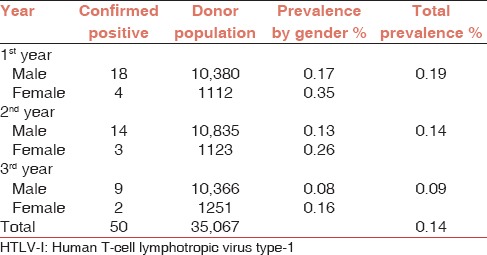
The seropositive population consisted of 41 (82%) men and 9 (18%) women. The seronegative group consisted of 91 (91%) men and 9 (9%) women (P = 0.11). The seropositive group consisted of 8 (16%) single and 42 (84%) married cases. The seronegative group consisted of 18 (18%) single and 82 (82%) married individuals (P = 0.76). Among seropositive blood donors, 43 cases (86%) had a high school diploma, or lower educational level and 7 (14%) had an academic degree. The corresponding values in the seronegative group were 69 (69%) and 31 (31%), respectively (P = 0.02). In terms of blood donations, 49 seropositive donors (98%) were first-time donors and 1 (2%) was a regular blood donor. In the seronegative donors, 22 donors (22%) were first-time donors and 78 donors (78%) were regular blood donors (P < 0.001). The infection rate including the overall prevalence and prevalence in terms of gender during the study period was calculated [Table 2].
Table 2.
Number of HTLV-I positive cases in Sabzevar blood donors
Discussion
According to the results, the overall prevalence of HTLV-I infection in blood donors in Sabzevar was 0.14%. This is lower than the prevalence (0.26%) found in a study on blood donors of Sabzevar in 2007-2008. According to studies on blood donors in Iran, the seroprevalence rates of infection in Chaharmahal-Bakhtiari, West Azerbaijan, Ilam, Mashhad, Hormozgan, Southern Khorasan, and Bushehr were 0.62%, 0.34%, 0.21%, 0.18%, 0.18%, 0.04%, and 0.01%, respectively.[7,8,9,10,11,12,14] The different prevalence rates may be attributed to the differences in the geographical area, social and demographic composition, behavioral patterns of the studied population and insufficient sample size in some studies.[15] The prevalence of HTLV-I infection in blood donors in neighboring countries, Turkmenistan (northeast of Iran) and Turkey (northwest of Iran) was 0.27% and 0%, respectively.[16,17] The prevalence of HTLV-I infection in blood donors in southern neighbors, Saudi Arabia and Kuwait was 0.006% and 0.016%, respectively.[18,19] The prevalence of HTLV-I infection in Japanese blood donors (1.9%) is higher than in the present study.[15] The prevalence of infection in Brazilian and Senegalese blood donors was 0.12% and 0.14%, respectively which is close to the prevalence rate obtained in the present study.[20,21] The prevalence of infection among blood donors in nonendemic Asian countries such as Lebanon, Korea, and Taiwan was 0.028%, 0.007%, and 0.058%, respectively which is lower than that obtained in the present study.[22,23,24] The prevalence of infection among donors in France (0.004%), Denmark (0.003%), Sweden (0.002%), Norway (0.002%), Spain (0.001%), and Belgium (0%) was much lower than in our study.[25,26,27,28]
The HTLV-I prevalence in blood donors shows a declining trend from 2009 to 2011. In another study on blood donors in Sabzevar in 2007-2008, the prevalence rates of HTLV-I infection were 0.30% and 0.22%, respectively.[5] It appears the main reasons for declining prevalence in blood donors include improved selection of blood donors and increased awareness of the blood donors and the general population about the high-risk behaviors and transmission ways of HTLV-I. In addition, the increased number of regular donations, development of deferral registry of blood donors software, as well as specialized training courses for staff in blood transfusion centers resulted in effective screening of blood donors.[29]
According to study on the general population of Sabzevar in 2008, the overall prevalence of infection was 1.66%.[4] The prevalence of the HTLV-I infection in the general population of Mashhad was estimated 2.12% in 2009.[6] As can be seen, the prevalence of HTLV-I infection in blood donors is far less than the general population. On the other hand, since blood donors are considered as people with fewer behavioral risks, the low prevalence of HTLV-I infection in blood donors than the general population seems reasonable.
According to the results, the positive rate of HTLV-I antibody increased with increasing age. This is consistent with most studies in this area. This may be due to cumulative effects of multiple exposures in endemic areas.[3,6] The higher prevalence rate in females is consistent with most studies and could be due to the higher possibility of male to female transmission during sexual contact.[2,3,28] In this study, the prevalence of HTLV-I infection in married individuals (84%) was higher than in single people (16%). However, the difference was not statistically significant. This could be due to the higher average age of married people and thus the higher exposure to the virus infection through sexual transmission.[2,3] In general, older age, female gender, and lower socioeconomic status were associated with higher infection rates in both endemic and non-endemic areas of HTLV-I infection.[28] The higher prevalence of HTLV-I infection in the first-time donors than regular donors may be emphasized that regular donor are safer than first-time donors. A national study in the country showed that the regular donation was associated with high levels of altruistic motives.[30]
Conclusion
Despite the endemic study region, the prevalence of HTLV-I infection in blood donors in Sabzevar was low with a declining trend. The factors involved in declining the prevalence of HTLV-I infection among blood donors include improved clinical screening methods, using deferral registry in blood transfusion centers and increased the percentage of regular donation. Due to the lower frequency of infection in blood donors with lower age and higher educational level, more efforts should be done to attract regular blood donors among young age groups with higher educational levels.
Acknowledgment
This study was supported by Khorasan Razavi Blood Transfusion Centre.
Footnotes
Source of Support: Razavi Khorasan Blood Transfusion Centre
Conflicting Interest: None declared.
References
- 1.Verdonck K, González E, Van Dooren S, Vandamme AM, Vanham G, Gotuzzo E. Human T-lymphotropic virus 1: Recent knowledge about an ancient infection. Lancet Infect Dis. 2007;7:266–81. doi: 10.1016/S1473-3099(07)70081-6. [DOI] [PubMed] [Google Scholar]
- 2.Bittencourt AL, Primo J, Oliveira MF. Manifestations of the human T-cell lymphotropic virus type I infection in childhood and adolescence. J Pediatr (Rio J) 2006;82:411–20. doi: 10.2223/JPED.1573. [DOI] [PubMed] [Google Scholar]
- 3.Edlich RF, Hill LG, Williams FM. Global epidemic of human T-cell lymphotrophic virus type-I (HTLV-I): An update. J Long Term Eff Med Implants. 2003;13:127–40. doi: 10.1615/jlongtermeffmedimplants.v13.i2.70. [DOI] [PubMed] [Google Scholar]
- 4.Azarpazhooh MR, Hasanpour K, Ghanbari M, Rezaee SA, Mashkani B, Hedayati-Moghaddam MR, et al. Human T-lymphotropic virus type 1 prevalence in northeastern Iran, Sabzevar: An epidemiologic-based study and phylogenetic analysis. AIDS Res Hum Retroviruses. 2012;28:1095–101. doi: 10.1089/AID.2011.0248. [DOI] [PubMed] [Google Scholar]
- 5.Jamili P, Safabakhsh H, Marvi M, Shakeri M, Bazargani R. Seroepidemiology of HTLV-I infection in Sabzevar blood donors from 2007 to 2008. J Sabzevar Univ Med Sci. 2014;20:464–71. [Google Scholar]
- 6.Rafatpanah H, Hedayati-Moghaddam MR, Fathimoghadam F, Bidkhori HR, Shamsian SK, Ahmadi S, et al. High prevalence of HTLV-I infection in Mashhad, Northeast Iran: A population-based seroepidemiology survey. J Clin Virol. 2011;52:172–6. doi: 10.1016/j.jcv.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Safabakhsh H, Jalalian M, Karimi G. The prevalence of HTLV-1 infection in blood donation volunteers in Mashhad. Glob J Health Sci. 2014;6:99–104. doi: 10.5539/gjhs.v6n5p99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karimi A, Nafici MR, Imani K. Comparison of human T-cell leukemia virus type 1 seroprevalence in high risk patients (thalassemia and hemodialysis) and healthy individuals from Charmahal-Bakhtiari province, Iran. Kuwait Med J. 2007;39:259–61. [Google Scholar]
- 9.Khameneh ZR, Baradaran M, Sepehrvand N. Survey of the seroprovalence of HTLV I/II in hemodialysis patients and blood donors in Urmia. Saudi J Kidney Dis Transpl. 2008;19:838–41. [PubMed] [Google Scholar]
- 10.Falahi S, Sabahi F, Zeynali M, Kiani J, Ranjbar J. Incidence of human T- lymphotropic virus type-1 (HTLV1) among blood donors from Ilam, Iran. Iran J Virol. 2008;1:11–4. [Google Scholar]
- 11.Abedi F, Yavarian M, Shakibzadeh A, Khalvati B, Asadi AH. A pilot Seroepidemiologic study of HTLV in thalassemia, hemophilia, and hemodialysed patients in Hormozgan. Med J Hormozgan Univ. 2009;13:75–80. [Google Scholar]
- 12.Karim MR, Pour GH, Zandi K, Roustaei MH. Prevalence of anti-HTLV-I & anti-HTLV-II antibodies in blood donors in Bushehr province. Iran S Med J. 2004;2:164–1. [Google Scholar]
- 13.Rafatpanah H, Farid R, Golanbar G, Jabbari Azad F. HTLV-I infection: Virus structure, immune response to the virus and genetic association studies in HTLV-I-infected individuals. Iran J Allergy Asthma Immunol. 2006;5:153–66. [PubMed] [Google Scholar]
- 14.Ghafouri M, Ameli MR. Transfusion transmitted viral infections in blood donors of South Khorasan. Sci J Iran Blood Transfus Organ. 2011;7:242–8. [Google Scholar]
- 15.Chaudhari SC, Shah T, Misra SC. Prevalence of human T cell leukaemia virus amongst blood donors. Med J Armed Forces India. 2009;65:38–40. doi: 10.1016/S0377-1237(09)80052-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Senyuta N, Syrtsev A, Yamashita M, Stepina V, Susova O, Scherbak L, et al. Sero-epidemiologic and phylogenetic studies of HTLV-I infection in 2 countries of the Caspian Sea region. Int J Cancer. 1998;77:488–93. doi: 10.1002/(sici)1097-0215(19980812)77:4<488::aid-ijc2>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 17.Sertöz R, Turhan A, Bozkurt H, Samlioglu P, Degirmenci A, Aydinok Y, et al. Investigation of anti-HTLV I/II seroprevalence in healthy blood donors in Izmir region, Turkey. Mikrobiyol Bul. 2010;44:579–84. [PubMed] [Google Scholar]
- 18.Ul-Hassan Z, Al-Bahrani AT, Panhotra BR. Prevalence of human T-lymphotropic virus type I and type II antibody among blood donors in Eastern Saudi Arabia. Saudi Med J. 2004;25:1419–22. [PubMed] [Google Scholar]
- 19.Al-Mufti S, Voevodin A, Ahmed S, Al Hamdan S, Al-Basheer AA. Seroprevalence of human T-cell leukemia/lymphoma virus type I and type II (HTLV-I/HTLV-II) infection among volunteer blood donors in Kuwait. Med Princ Pract. 1999;8:45–50. [Google Scholar]
- 20.Carneiro-Proietti AB, Sabino EC, Leão S, Loureiro P, Sarr M. HTLV-1/2 prevalence in Brazilian blood donors: Regional and demographic variation. Retrovirology. 2011;8(Suppl 1):A83. [Google Scholar]
- 21.Diop S, Calattini S, Abah-Dakou J, Thiam D, Diakhaté L, Gessain A. Seroprevalence and molecular epidemiology of human T-cell leukemia virus type 1 (HTLV-1) and HTLV-2 in blood donors from Dakar, Senegal. J Clin Microbiol. 2006;44:1550–4. doi: 10.1128/JCM.44.4.1550-1554.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tamim H, Musharrafieh U, Ramia S, Almawi WY, Al-Jisr T, Ayoub T, et al. Is seroprevalence of HTLV-I/II among blood donors in Lebanon relevant? Am J Infect Control. 2004;32:220–3. doi: 10.1016/j.ajic.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 23.Kwon SY, Lim AH, Park JY, Han SH, Cho NS. Seroprevalence of human T-lymphotropic virus type 1 and 2 in Korean blood donors. J Med Virol. 2008;80:1864–7. doi: 10.1002/jmv.21260. [DOI] [PubMed] [Google Scholar]
- 24.Lu SC, Kao CL, Chin LT, Chen JW, Yang CM, Chang JH, et al. Seroprevalence and demographic characteristics of HTLV-I among blood donors in Taiwan: 1996-1999. Int J Hematol. 2001;74:333–7. doi: 10.1007/BF02982070. [DOI] [PubMed] [Google Scholar]
- 25.Couroucé AM, Pillonel J, Lemaire JM, Maniez M, Brunet JB. Seroepidemiology of HTLV-I/II in universal screening of blood donations in France. AIDS. 1993;7:841–7. doi: 10.1097/00002030-199306000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Stigum H, Magnus P, Samdal HH, Nord E. Human T-cell lymphotropic virus testing of blood donors in Norway: A cost-effect model. Int J Epidemiol. 2000;29:1076–84. doi: 10.1093/ije/29.6.1076. [DOI] [PubMed] [Google Scholar]
- 27.Toro C, Rodés B, Aguilera A, Caballero E, Benito R, Tuset C, et al. Clinical impact of HTLV-1 infection in Spain: Implications for public health and mandatory screening. J Acquir Immune Defic Syndr. 2002;30:366–8. doi: 10.1097/00126334-200207010-00016. [DOI] [PubMed] [Google Scholar]
- 28.Proietti FA, Carneiro-Proietti AB, Catalan-Soares BC, Murphy EL. Global epidemiology of HTLV-I infection and associated diseases. Oncogene. 2005;24:6058–68. doi: 10.1038/sj.onc.1208968. [DOI] [PubMed] [Google Scholar]
- 29.Abolghasemi H, Maghsudlu M, Amini Kafi-Abad S, Cheraghali A. Introduction to Iranian Blood Transfusion Organization and blood safety in Iran. Iran J Public Health. 2009;38(Suppl 1):82–7. [Google Scholar]
- 30.Maghsudlu M, Nasizadeh S. Iranian blood donors’ motivations and their influencing factors. Transfus Med. 2011;21:247–52. doi: 10.1111/j.1365-3148.2011.01077.x. [DOI] [PubMed] [Google Scholar]


