Abstract
Objective
This report presents national estimates of the use of complementary health approaches among children aged 4–17 years in the United States. Selected modalities are compared for 2007 and 2012 to examine changes over time.
Methods
Data from the 2007 and 2012 National Health Interview Survey (NHIS) were analyzed for this report. The combined sample included 17,321 interviews with knowledgeable adults about children aged 4–17 years. Point estimates and estimates of their variances were calculated using SUDAAN software to account for the complex sampling design of NHIS. Differences between percentages were evaluated using two-sided significance tests at the 0.05 level.
Results
The use of complementary health approaches among children did not change significantly since 2007 (from 12.0% in 2007 to 11.6% in 2012). However, one approach, the use of traditional healers, showed a statistically significant decrease in use, from 1.1% in 2007 to 0.1% in 2012. No other significant decreases were identified. An increase in the use of yoga was observed during this period (from 2.3% in 2007 to 3.1% in 2012). Nonvitamin, nonmineral dietary supplements; chiropractic or osteopathic manipulation; and yoga, tai chi, or qi gong were the most commonly used complementary health approaches in both 2007 and 2012. Also consistent between 2007 and 2012 was that complementary health approaches were most frequently used for back or neck pain, head or chest cold, anxiety or stress, and other musculoskeletal conditions.
Keywords: complementary and alternative medicine, chiropractic manipulation, dietary supplements, fish oil
Introduction
Complementary health approaches include a group of diverse medical and health care interventions, practices, products, and disciplines that are not generally considered part of conventional medicine (1). Use of complementary health approaches in children has not been studied extensively at the national level. However, the available data suggest higher rates of use among children with chronic health conditions, including anxiety, musculoskeletal conditions, and recurrent headaches compared with those without these conditions (2–4). This is similar to what is seen in adult populations (5–7). Previous reports have found that the specific sociodemographic and health factors associated with children’s use of complementary health approaches—higher parental education, higher family income, living in the Western region, having more health conditions, and having more doctor visits in the past 12 months—mirror those for adults (5,8). These similarities may be partly explained by the fact that parents are the gatekeepers of health care for their children. Reflecting this role, research has found that the strongest predictor of the use of complementary health approaches by children is use by their parents (2,3,5).
Data from population-based surveys on the use of complementary health approaches in the United States now span 20 years (5,9,10). The 2007 National Health Interview Survey (NHIS) provided the first population-based estimate of children’s use of complementary health approaches. Recognizing that factors such as awareness and health insurance benefits may change over time, this report aims to update the findings from 2007 to provide the most current and comprehensive picture of U.S. children’s use of complementary health approaches. In addition, estimates on the use of complementary health approaches by selected demographic characteristics and the use of complementary health approaches to treat selected conditions are presented in this report.
Methods
Data source
Data in this report come primarily from the 2007 and 2012 Child Complementary and Alternative Medicine (CAL) supplement of NHIS, with demographic, family characteristics, and other health information from the Person, Sample Child Core, and Family Core components of NHIS. NHIS is a household survey conducted continuously throughout the year for the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics by interviewers from the U.S. Census Bureau. Interviews are primarily conducted in person, but follow-ups to complete interviews may be conducted over the telephone. NHIS collects detailed health-related information and some demographic information from a sample of the civilian noninstitutionalized U.S. population.
The Sample Child Core obtains additional information on the health of one randomly selected child (the sample child) in the family. For sample children, information is provided by a knowledgeable adult family member residing in the household. In 2007, the CAL supplement included all sample children under age 18, while in 2012, the supplement only included sample children aged 4–17 years. To enable comparisons, for this report 2007 data were restricted to children aged 4–17 years, yielding final sample sizes of 7,103 children in 2007 and 10,218 children in 2012. A detailed description of the NHIS sample design and the survey questionnaires for specific years are available from NHIS survey description documents (11,12).
The processes used to develop the CAL supplements have been previously described (13). In brief, the questionnaire content for both the 2007 and 2012 CAL supplements was based on literature reviews, feedback from the scientific community, expert input and workshops, and cognitive testing. Although specific modalities included in the three questionnaires varied slightly by year, the following practices were asked about in both the 2007 and 2012 CAL supplements: acupuncture; Ayurveda; biofeedback; chelation therapy; chiropractic or osteopathic manipulation; energy healing therapy; hypnosis; massage; naturopathy; nonvitamin, nonmineral dietary supplements; homeopathy; diet-based therapies; yoga; tai chi; qi gong; meditation; and other relaxation techniques. For both years, information was collected on whether the sample child used each modality in the past 12 months; whether the sample child had seen a provider or practitioner for the modality; whether the modality was used to treat a specific health problem or condition, and, if so, what health problems or conditions were treated; and whether the modality was used to improve athletic or sports performance. In 2012, the CAL supplement was enhanced to collect further information on lifetime use of the modality, the number of times the sample child had seen a practitioner for the modality, and the costs related to modality use (13).
Although no changes were made in how the survey was administered, several modifications were made between the 2007 and 2012 CAL supplements. Noteworthy modifications include: a) the restriction of the survey to children aged 4–17 years; b) the addition of items to determine whether deep breathing or meditation was used in conjunction with the practice of yoga, tai chi, or qi gong and if a class was taken or formal training was received; c) meditation was categorized as mantra, mindfulness, or spiritual; d) the number of nonvitamin, nonmineral dietary supplements included on the flashcard was reduced from 44 products in 2007 to 21 products in 2012, although only the 2012 survey allowed for the inclusion of products not listed on the flashcard; e) names of traditional healers were modified and consolidated; f) Zone and South Beach were eliminated from the list of special diets; and g) deep-breathing exercise was removed as an independent health practice for 2012, but collected as a component of other approaches. These changes likely influenced the overall prevalence rates, and the 2012 data were recoded to be consistent with 2007 for the analysis presented in this report. Given these changes, results should be interpreted with caution when comparing modalities that are impacted by questionnaire revisions.
Due to the lack of sufficient sample sizes and the inability to compare modalities across survey years, this report only covers a selection of complementary health approaches, including: nonvitamin, nonmineral dietary supplements; acupuncture; naturopathy; homeopathy; chiropractic or osteopathic manipulation; biofeedback; massage therapy; special diets (vegetarian or vegan, macrobiotic, Atkins, Pritikin, and Ornish); traditional healers (Curandero, Espiritista, Hierbero or Yerbera, Shaman, Botanica, Native American Healer or Medicine Man, Sobador, Machi, Parchero, Yerbero, Hierbista, and Huesero); movement therapies (Feldenkrais, Alexander technique, Pilates, and Trager psychophysical integration); energy healing therapy; and hypnosis. Information presented in this report for both 2007 and 2012 was obtained via a knowledgeable adult proxy as part of the in-person interview.
Demographic and other variables used in the analysis
Demographic characteristics of children presented in this report include: sex, age group, Hispanic or Latino origin and race, parent’s highest level of education, poverty status, and health insurance coverage. All demographic characteristics are based on the knowledgeable adult’s report on behalf of the child. Age groups of 4–11 and 12–17 years were assigned based on the child’s age at the time of interview. Hispanic or Latino origin and race are determined based on two separate questions. For this reason, a child may have been identified as Hispanic or Latino origin regardless of race. The text and tables in this report use shorter versions of the 1997 Office of Management and Budget race and Hispanic origin terms for conciseness. For example, the category “Not Hispanic or Latino, black or African American, single race” is referred to as “non-Hispanic black.” Due to insufficient sample size, Non-Hispanic Asian, Non-Hispanic Other Pacific Islander, and Non-Hispanic American Indian or Alaska Native were combined to form the category Non-Hispanic all other races.
Parent’s education was defined as the highest grade completed by the child’s mother or father who was living in the household, regardless of that parent’s age. This measure did not take into account a parent’s education if they did not live in the same household as the child.
Poverty status was based on the family income and family size using the U.S. Census Bureau’s poverty thresholds. Children who are categorized as “Poor” have a ratio less than 1.0; that is, their family income was strictly below the poverty threshold. “Near poor” children have family incomes of 100% to less than 200% of the poverty threshold, and “not poor” children have family incomes that are 200% of the poverty threshold or greater.
Respondents were asked about the child’s health insurance coverage at the time of the interview. Respondents reported whether the child was covered by private insurance (obtained through the employer or workplace, purchased directly, or through a local or community program); Medicare; Medigap (supplemental Medicare coverage); Medicaid; State Children’s Health Insurance Program (SCHIP); Indian Health Service (IHS); military coverage (including VA, TRICARE, and CHAMP–VA); a state-sponsored health plan; another government program; or any single service plan. This information was used to form a health insurance hierarchy that consisted of three mutually exclusive categories. Persons with more than one type of health insurance were assigned to the first appropriate category in the following hierarchy: private coverage; public coverage (includes persons with Medicare, Medigap, Medicaid, SCHIP, military coverage, a state-sponsored health plan, or another government program); and uninsured (also includes persons who are only covered by IHS or only have a single service plan).
The “any complementary health approach use” category was defined as a “yes” response to any of the following: chelation therapy; nonvitamin, nonmineral dietary supplements; special diet; acupuncture; Ayurveda; homeopathic treatment; naturopathy; traditional healer; chiropractic or osteopathic manipulation; massage; Feldenkrais; Alexander technique; Pilates; Trager psychophysical integration; biofeedback; mantra meditation; Transcendental Meditation; relaxation response; clinically standard meditation; spiritual meditation; guided imagery; progressive relaxation; yoga, tai chi, or qi gong (with deep breathing); hypnosis; or energy healing.
Statistical analysis
Estimates in this report were calculated using weighted data and are representative of the U.S. noninstitutionalized population of children aged 4–17 years. Data weighting procedures are described in more detail elsewhere (14). Point estimates, and estimates of their variances, were calculated using SUDAAN software, version 10 (15), a software package designed to account for the complex sampling design of NHIS. Estimates were age-adjusted and weighted using the sample child weight. Unless otherwise specified, the denominator used was all children aged 4–17 years. Reliability of estimates was evaluated using the relative standard error (RSE), which is the standard error divided by the point estimate. Estimates were considered reliable if the RSE was less than or equal to 30%; estimates that were greater than 30% and less than or equal to 50% were considered unreliable. Estimates with RSEs of greater than 50% are not shown. Differences between estimates were evaluated using two-tailed significance tests at the 0.05 level. Terms such as “greater than” and “less than” indicate a statistically significant difference. Terms such as “similar” or “no difference” indicate that the estimates being compared were not significantly different. Due to the cross-sectional nature of the data collected in NHIS, an association between two variables does not indicate a causal relationship.
Strengths and limitations of the data
A major strength of the NHIS CAL supplement data is that they were collected for a nationally representative sample of U.S. children, allowing for population estimates. The large sample size allows for estimation of the use of complementary health approaches by a wide variety of population subgroups. The large sample size also facilitates investigation of the association between complementary health approaches and a wide range of other self-reported health characteristics collected in NHIS.
NHIS data have several limitations. First, estimates are based on responses from a child’s knowledgeable adult and therefore may be subject to recall bias. Although considerable effort is made to ensure accurate reporting, information from the knowledgeable adult may be inaccurate because the respondent is unaware of relevant information, has forgotten it, does not wish to reveal it to an interviewer, or does not understand the intended meaning of the question. Lastly, although the overall sample size was large, the number of children that used many of the selected complementary health approaches presented in this report was low. However, the findings reported here are within the range of previous reports (5).
Results
Children’s use of complementary health approaches during the past 12 months, 2007 and 2012
Complementary health approaches encompass a wide range of modalities. Table 1 breaks out selected modalities used among all children aged 4–17 years for 2007 and 2012. The percentages of individual modalities range from 0.1%–4.9% of children reporting use in the past 12 months.
Table 1.
Frequencies and age-adjusted percentages of children aged 4–17 years who used or saw a practitioner, took a class, or received formal training for selected complementary and alternative medicine modalities during the past 12 months, by type of therapy: United States, 2007 and 2012
| 2007 |
2012 |
||||
|---|---|---|---|---|---|
| Therapy | Number (in thousands) |
Age- adjusted percent (standard error) |
Number (in thousands) |
Age- adjusted percent (standard error) |
p
value1 |
| Nonvitamin, nonmineral dietary supplements2 | 2,452 | 4.3 (0.38) | 2,753 | 4.9 (0.29) | † |
| Chiropractic or osteopathic manipulation | 1,742 | 3.0 (0.29) | 1,854 | 3.3 (0.26) | † |
| Yoga, tai chi, or qi gong (any) | 1,414 | 2.5 (0.23) | 1,820 | 3.2 (0.24) | ¶ |
| Yoga (any) | 1,312 | 2.3 (0.22) | 1,741 | 3.1 (0.23) | ¶ |
| Tai chi (any) | ‡113 | ‡0.2 (0.06) | 139 | 0.2 (0.05) | † |
| Qi gong (any) | ‡ | ‡ | 40 | ‡0.1 (0.03) | † |
| Deep-breathing exercises3 | 1,533 | 2.7 (0.28) | 1,531 | 2.7 (0.21) | † |
| Deep breathing as part of mantra, mindful, or spiritual meditation; guided imagery; or progressive relaxation |
--- | --- | 360 | 0.6 (0.09) | --- |
| Deep breathing as part of yoga, tai chi, or qi gong | --- | --- | 1,387 | 2.5 (0.21) | --- |
| Homeopathy treatment4 | 686 | 1.2 (0.26) | 1,007 | 1.8 (0.19) | † |
| Homeopathy (practitioner based) | --- | --- | 123 | 0.2 (0.06) | --- |
| Meditation5 | 725 | 1.3 (0.16) | 927 | 1.6 (0.16) | † |
| Mantra, mindful, or spiritual meditation | --- | --- | 323 | 0.6 (0.09) | --- |
| Meditation as part of yoga, tai chi, or qi gong | --- | --- | 760 | 1.3 (0.15) | --- |
| Massage | 579 | 1.0 (0.14) | 385 | 0.7 (0.10) | † |
| Special diets6 | 404 | 0.7 (0.12) | 419 | 0.7 (0.12) | † |
| Progressive relaxation | 327 | 0.6 (0.11) | 216 | 0.4 (0.07) | † |
| Guided imagery | 293 | 0.5 (0.11) | 239 | 0.4 (0.08) | † |
| Movement therapies7 | 266 | 0.5 (0.08) | 239 | 0.4 (0.09) | † |
| Energy healing therapy | 110 | 0.2 (0.05) | 102 | 0.2 (0.05) | † |
| Naturopathy | ‡158 | ‡0.3 (0.10) | ‡130 | 0.2 (0.07) | † |
| Craniosacral therapy | --- | --- | ‡95 | ‡0.2 (0.07) | † |
| Acupuncture | 96 | 0.2 (0.05) | ‡79 | ‡0.1 (0.05) | § |
| Traditional healers8 | 619 | 1.1 (0.20) | ‡69 | ‡ 0.1 (0.05) | § |
| Biofeedback | ‡73 | ‡0.1 (0.04) | ‡21 | ‡0.0 (0.02) | ¶ |
| Hypnosis | ‡ | ‡ | ‡ | ‡ | † |
| Ayurveda | 34 | ‡0.1 (0.03) | ‡ | ‡ | † |
Difference is not statistically significant.
Estimates are considered unreliable. Data have a relative standard error (RSE) greater than 30% and less than or equal to 50% and should be used with caution. Data not shown have an RSE greater than 50%.
--- Data not available.
p value less than 0.01.
0.0 Quantity more than zero but less than 0.05.
p value less than 0.05.
p value for differences across years.
While questions were asked about nonvitamin, nonmineral dietary supplements in 2007 and 2012, the data should be interpreted with caution due to question order and the specific nonvitamin, nonmineral dietary supplements covered.
Deep-breathing exercises in 2012 included deep-breathing exercises as part of hypnosis, biofeedback, mantra meditation (including Transcendental Meditation, relaxation response, and clinically standardized meditation), mindfulness meditation (including vipassana, Zen Buddhist meditation, mindfulness-based stress reduction, and mindfulness-based cognitive therapy), spiritual meditation (including centering prayer and contemplative meditation), guided imagery, progressive relaxation, yoga, tai chi, or qi gong, while deep-breathing exercises in 2007 asked broadly about the use of deep breathing and did not distinguish between deep breathing used as part of other complementary health approach modalities.
Homeopathy questions in 2007 did not distinguish between practitioner based and self-care. Therefore, estimates presented in 2012 also do not take this into account.
Meditation in 2012 includes mantra meditation (including Transcendental Meditation, relaxation response, and clinically standardized meditation), mindfulness meditation (including vipassana, Zen Buddhist meditation, mindfulness-based stress reduction, and mindfulness-based cognitive therapy), spiritual meditation (including centering prayer and contemplative meditation), and meditation as part of yoga, tai chi, or qi gong. In 2007, meditation was asked broadly and did not specify subgroups of meditation.
Special diets in 2007 and 2012 include vegetarian (including vegan), macrobiotic, Atkins, Pritikin, and Ornish diets.
Movement therapies in 2007 and 2012 include Feldenkrais, Alexander technique, Pilates, and Trager psychophysical integration.
Traditional healers in 2007 include Curandero, Espiritista, Hierbero and Yerbera, Shaman, Botanica, Native American Healer or Medicine Man, and Sobador. Traditional healers in 2012 include Curandero, Machi, or Parchero; Yerbero or Hierbista; Shaman; Native American Healer or Medicine Man; Sobador; and Huesero.
NOTES: Estimates are based on household interviews of a sample of the civilian noninstitutionalized population. Estimates were age-adjusted using the projected 2000 U.S. population as the standard population and using two age groups: 4–11 and 12–17. The denominators for statistics shown exclude persons with unknown complementary health approach use information.
SOURCE: CDC/NCHS, National Health Interview Survey, 2007, 2012.
There was a statistically significant decrease in the use of traditional healers between 2007 (1.1%) and 2012 (0.1%). Due to questionnaire modifications, this should be interpreted with caution.
Nonvitamin, nonmineral dietary supplements were the most commonly used modality in both 2007 and 2012.
Any homeopathy was used by about 1.8% of children in 2012, while practitioner-based homeopathy was used by only 0.2% of children.
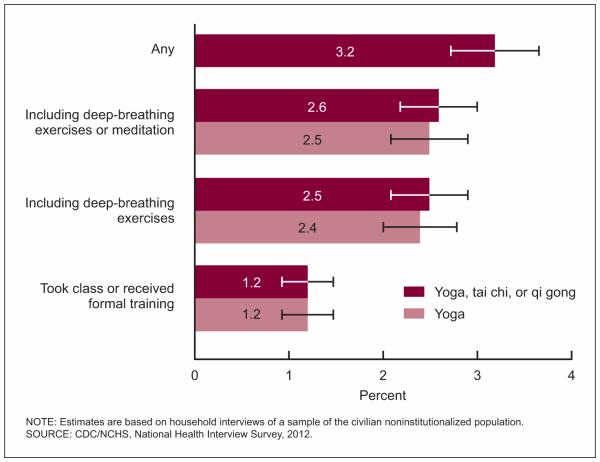
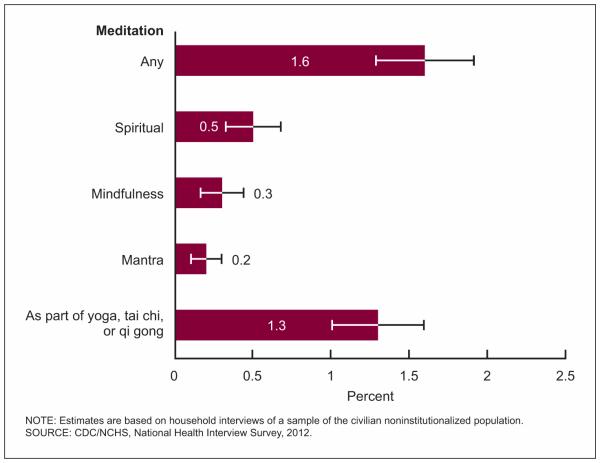
Yoga, tai chi, and qi gong are movement therapies that are often performed in classes with instructors. Deep breathing and meditation are often used with these movement therapies. For the 2012 survey, respondents were asked more detailed questions about the use of yoga, tai chi, and qi gong such as if deep-breathing exercises and meditation were used with the practice and if formal training was received or a class was taken. Figure 1 illustrates the use of yoga, tai chi, and qi gong among all children in 2012 and differentiates the percentage of children who use breathing exercises and meditation as part of their practice. Figure 2 provides detailed information about children’s use of different types of meditation.
Figure 1.
Age-adjusted percentages of children aged 4–17 years who used yoga, tai chi, or qi gong during the past 12 months: United States, 2012
Figure 2.
Age-adjusted percentages of children aged 4–17 years who used selected meditation techniques during the past 12 months: United States, 2012
There was a statistically significant increase in the use of any yoga, tai chi, or qi gong between 2007 (2.5%) and 2012 (3.2%). Most of this increase can be attributed to the increased use of yoga (2.3% to 3.1%) (Table 1).
In 2012, 2.6% of children used yoga, tai chi, or qi gong that included deep-breathing exercises or meditation in the past 12 months (Figure 1).
In 2012, 1.2% of children took yoga classes or received formal training (Figure 1).
Spiritual, mindfulness, and mantra meditation were each used by less than 0.5% of children (Figure 2).
Meditation as part of yoga, tai chi, or qi gong was used by about 1.3% of children in 2012 (Table 1).
Overall use of any complementary health approaches, by selected characteristics, 2007 and 2012
Table 2 shows the percentages of all children aged 4–17 years in 2007 and in 2012 who had used any complementary health approach in the past 12 months by selected characteristics. Just as the overall percentage of children aged 4–17 years using any complementary health approaches remained stable from 2007 to 2012, use among subgroups of sociodemographic characteristics also did not change for most groups.
Table 2.
Age-adjusted percentages of children aged 4–17 years who used any complementary health approaches during the past 12 months, by selected characteristics: United States, 2007 and 2012
| Any complementary health approach use1 |
p value for differences across years |
||
|---|---|---|---|
| Selected characteristic | 2007 | 2012 | |
| Age-adjusted percent2 (standard error) |
Age-adjusted percent2 (standard error) |
||
| Total | 12.0 (0.54) | 11.6 (0.46) | |
| Sex | |||
| Boys | 10.5 (0.77) | 9.7 (0.56) | † |
| Girls | 13.5 (0.69) | 13.5 (0.67) | † |
| Age (years)3 | |||
| 4–11 | 9.8 (0.67) | 9.3 (0.53) | † |
| 12–17 | 15.0 (0.86) | 14.7 (0.75) | † |
| Hispanic origin and race | |||
| Hispanic | 8.2 (0.87) | 6.1 (0.54) | ‡ |
| Non-Hispanic white, single race | 14.7 (0.82) | 14.9 (0.70) | † |
| Non-Hispanic black or African American, single race | 5.5 (0.84) | 5.5 (0.77) | † |
| Non-Hispanic all other races | 13.6 (1.62) | 14.2 (1.50) | † |
| Parent’s education4 | |||
| Less than high school diploma | 4.1 (0.74) | 2.1 (0.43) | ‡ |
| High school diploma or GED5 | 8.1 (0.89) | 6.9 (0.77) | † |
| More than high school | 15.2 (0.76) | 15.0 (0.62) | † |
| Poverty status6 | |||
| Poor | 7.0 (0.96) | 5.7 (0.69) | † |
| Near poor | 8.5 (0.95) | 9.1 (0.81) | † |
| Not poor | 14.9 (0.80) | 14.8 (0.67) | † |
| Health insurance7 | |||
| Private | 14.1 (0.73) | 14.6 (0.66) | † |
| Public | 8.1 (0.76) | 7.6 (0.55) | † |
| Uninsured | 10.4 (1.44) | 8.4 (1.20) | † |
Difference is not statistically significant.
p value less than 0.01.
Complementary health approach definition was a “yes” response to chelation therapy; nonvitamin, nonmineral dietary supplements; vegetarian or vegan diet; macrobiotic diet; Atkins diet; Pritikin diet; Ornish diet; acupuncture; Ayurveda; homeopathic treatment; naturopathy; Native American or Medicine Man; Shaman; Curandero, Machi, or Parchero; Yerbero or Hierbista; Sobador; Huesero; chiropractic or osteopathic manipulation; massage; Feldenkrais; Alexander technique; Pilates; Trager psychophysical integration; biofeedback; mantra meditation; Transcendental Meditation; relaxation; clinically standard meditation; spiritual meditation; guided imagery; progressive relaxation; yoga, tai chi, or qi gong (with deep breathing); hypnosis; and energy healing.
The denominator used in the calculation of percentages was all sample children.
Estimates for age groups are not age-adjusted.
Refers to the education level of the parent with the higher level of education, regardless of that parent’s age.
GED is General Educational Development high school equivalency diploma.
Based on family income and family size using the U.S. Census Bureau’s poverty thresholds for the previous calendar year. “Poor” persons are defined as below the poverty threshold. “Near poor” persons have incomes of 100% to less than 200% of the poverty threshold. “Not poor” persons have incomes that are 200% of the poverty threshold or greater.
Based on a hierarchy of mutually exclusive categories. Children with more than one type of health insurance were assigned to the first appropriate category in the hierarchy. “Uninsured” includes children who had no coverage as well as those who had only Indian Health Service coverage or had only a private plan that paid for one type of service such as accidents or dental care.
NOTES: Estimates are based on household interviews of a sample of the civilian noninstitutionalized population. Estimates are age-adjusted using the projected 2000 U.S. population as the standard population and using two age groups: 4–11 and 12–17.
SOURCE: CDC/NCHS, National Health Interview Survey, 2007, 2012.
Overall, there was not a statistically significant change in the prevalence of any complementary health approach between 2007 and 2012 (12.0% and 11.6%, respectively).
In 2012, there was a statistically significant decrease in the use of any complementary health approach for Hispanic children, and among children whose parents had less than a high school diploma.
Similar to the pattern seen in 2007, in 2012, older children (aged 12–17) were more likely to use any complementary health approach compared with younger children (aged 4–11) (p < 0.001).
In 2012, children whose parents had more than a high school education were seven times more likely to use any complementary health approach (15.0%) as children whose parents had less than a high school diploma (2.1%) (p < 0.001). This is similar to 2007, when 15.2% of children whose parents were in the highest education group and 4.1% of children whose parents were in the lowest education group used any complementary health approach (p < 0.01).
In both 2007 and 2012, children who were not poor were two to three times more likely to use any complementary health approach (14.9% and 14.8%, respectively) as children who were poor (7.0% and 5.7%, respectively) (p < 0.001).
Use of selected complementary health approaches, by selected characteristics, 2012
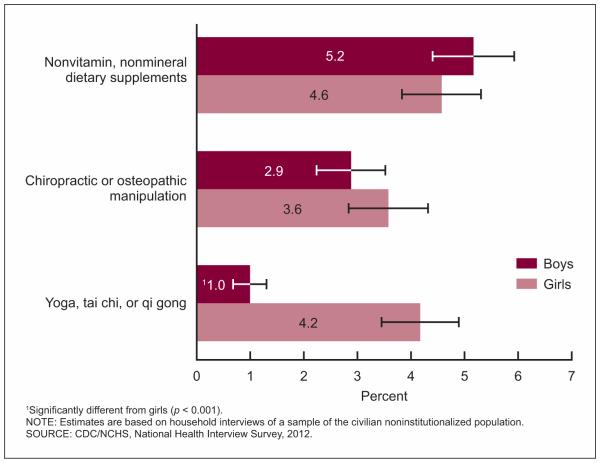
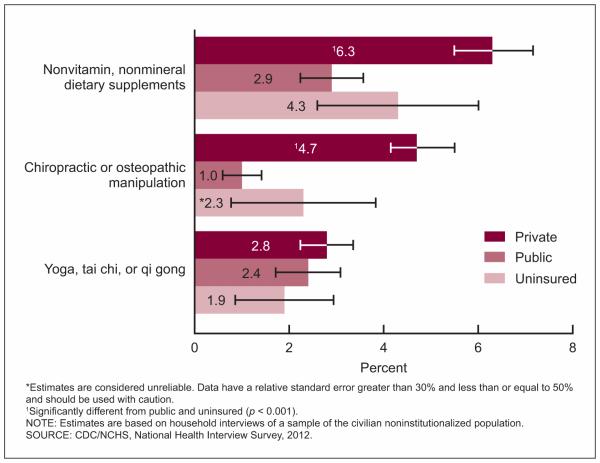
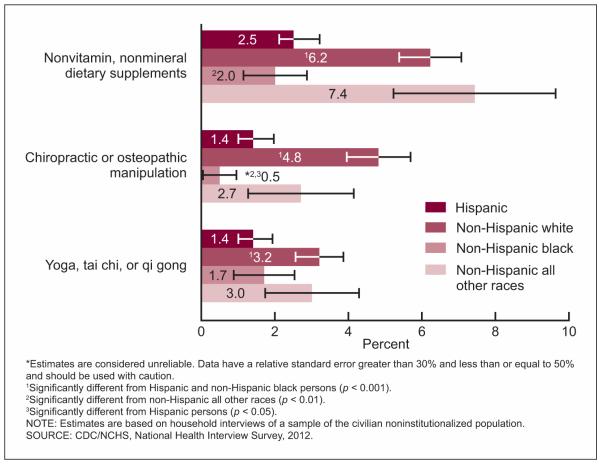
Differences in the percentages of children who used nonvitamin, nonmineral dietary supplements; chiropractic or osteopathic manipulation; and yoga, tai chi, or qi gong by sex, race and ethnicity, and health insurance status among all children aged 4–17 years for 2012 are presented in Figures 3–5.
Figure 3.
Age-adjusted percentages of children aged 4–17 years who used selected complementary health approaches during the past 12 months, by sex: United States, 2012
Figure 5.
Age-adjusted percentages of children aged 4–17 years who used selected complementary health approaches during the past 12 months, by health insurance status: United States, 2012
In 2012, girls were more likely to use yoga, tai chi, or qi gong in the past 12 months (4.2%) compared with boys (1.0%). Sex did not have a significant association with the use of nonvitamin, nonmineral dietary supplements and chiropractic or osteopathic manipulation (Figure 3).
Non-Hispanic white children were more likely than Hispanic and Non-Hispanic black children to use nonvitamin, nonmineral dietary supplements; chiropractic or osteopathic manipulation; and yoga, tai chi, or qi gong in the past 12 months (Figure 4).
In 2012, the prevalence of nonvitamin, nonmineral dietary supplement and chiropractic or osteopathic manipulation use in the past 12 months was higher for children with private health insurance than for children with public coverage. Insurance status had no impact on the use of yoga, tai chi, or qi gong (Figure 5).
Figure 4.
Age-adjusted percentages of children aged 4–17 years who used selected complementary health approaches during the past 12 months, by race and ethnicity: United States, 2012
Use of selected nonvitamin, nonmineral dietary supplements, 2007 and 2012
Little is known about the possible benefits or adverse effects of nonvitamin, nonmineral dietary supplements in children. The use of nonvitamin, nonmineral dietary supplements was the most common complementary health approach used in both 2007 and 2012. Table 3 provides greater detail on the specific types of supplements used among all children in the 30 days prior to the survey interview. Overall, there was a change in the ranking of the top three supplements used. Respondents could report using more than one dietary supplement.
Table 3.
Frequencies and age-adjusted percentages of children aged 4–17 years who used selected types of nonvitamin, nonmineral dietary supplements for health reasons in the past 30 days, by type of product used: United States, 2007 and 2012
| Used selected nonvitamin, nonmineral dietary supplements1 |
|||||
|---|---|---|---|---|---|
| 2007 |
2012 |
||||
| Nonvitamin, nonmineral dietary supplements | Number (in thousands) |
Age- adjusted percent2 (standard error) |
Number (in thousands) |
Age- adjusted percent2 (standard error) |
p
value |
| Fish oil3 | 394 | 0.7 (0.17) | 664 | 1.1 (0.13) | † |
| Melatonin | ‡87 | ‡0.1 (0.05) | 419 | 0.7 (0.11) | § |
| Probiotics or prebiotics | † | ‡0.3 (0.15) | 294 | 0.5 (0.09) | † |
| Echinacea | 434 | 0.8 (0.13) | 205 | 0.4 (0.08) | § |
| Garlic supplements | ‡78 | ‡0.1 (0.04) | ‡80 | ‡0.1 (0.04) | † |
| Combination herb pill | ‡290 | ‡0.5 (0.15) | ‡68 | ‡0.1 (0.04) | ¶ |
| Ginseng | ‡ | ‡ | ‡63 | ‡0.1 (0.05) | † |
| Cranberry (pills, capsules) | ‡33 | ‡0.1 (0.03) | ‡31 | ‡0.1 (0.02) | † |
| Glucosamine or chondroitin | ‡ | ‡ | ‡42 | ‡0.1 (0.03) | † |
Difference is not statistically significant.
Estimates are considered unreliable. Data have a relative standard error (RSE) greater than 30% and less than or equal to 50% and should be used with caution. Data not shown have an RSE greater than 50%.
p value less than 0.01.
p value less than 0.05.
Respondents may have used more than one nonvitamin, nonmineral dietary supplement.
The denominator used in the calculation of percentages was all sample children.
In 2007, fish oil was described as fish oil or omega-3 or DHA fatty acid. In 2012, fish oil was described as fish oil or omega-3 or DHA or EPA fatty acid.
NOTES: Estimates are based on household interviews of a sample of the civilian noninstitutionalized population. Estimates were age-adjusted using the projected 2000 U.S. population as the standard population and using two age groups: 4–11 and 12–17.
SOURCE: CDC/NCHS, National Health Interview Survey, 2007, 2012.
Echinacea was the most commonly used supplement in 2007, while fish oil was most commonly used in 2012.
There was a significant increase in the use of melatonin among children, from 0.1% in 2007 to 0.7% in 2012.
Use of combination herb pills decreased from 0.5% in 2007 to 0.1% in 2012.
Fish oil and probiotics or prebiotics were among the top three nonvitamin, nonmineral dietary supplements used in 2012. There was no statistical difference between 2007 use and 2012 use.
In 2012 and 2007, garlic supplements, combination herb pills, ginseng, cranberry, and glucosamine or chondroitin were used by about 0.1% of children.
Reason for complementary health approach use, 2007 and 2012
Respondents for children who used or saw a practitioner for any complementary health approach in the past 12 months were asked if the modality was used to treat a specific health problem or condition. The frequencies and percentages of children who used selected complementary health approaches to treat a specific health problem or condition are shown in Table 4.
Table 4.
Frequencies and age-adjusted percentages of children aged 4–17 years who used selected types of complementary health approaches to treat a condition among those who used any complementary health approach in the past 12 months: United States, 2007 and 2012
| 2007 |
2012 |
||
|---|---|---|---|
| Complementary health approach | Age-adjusted percent (standard error)1 |
Age-adjusted percent (standard error)1 |
p
value |
| Any complementary health approach | 44.2 (2.66) | 45.6 (2.16) | † |
| Acupuncture | 53.9 (14.71) | 70.1 (17.83) | † |
| Naturopathy | ‡50.0 (17.70) | 66.0 (6.47) | † |
| Homeopathy treatment | 88.8 (4.07) | 62.9 (5.26) | § |
| Chiropractic or osteopathic manipulation | 59.8 (5.21) | 62.1 (3.86) | † |
| Biofeedback | 42.1 (16.36) | 59.7 (21.93) | † |
| Massage therapy | 40.0 (8.77) | 42.6 (8.70) | † |
| Nonvitamin, nonmineral dietary supplements | 49.4 (5.59) | 35.5 (3.47) | § |
| Special diets2 | ‡ | 25.9 (7.36) | † |
| Traditional healers3 | ‡14.4 (4.61) | ‡23.5 (8.85) | † |
| Movement therapies4 | ‡ | ‡11.1 (3.98) | † |
| Energy healing therapy | 57.9 (13.44) | ‡ | † |
| Hypnosis | 78.3 (19.11) | ‡ | † |
Difference is not statistically significant.
Estimates are considered unreliable. Data have a relative standard error (RSE) greater than 30% and less than or equal to 50% and should be used with caution. Data not shown have an RSE greater than 50%.
p value less than 0.001.
The denominators used in the calculation of percentages were children who used each selected type of complementary health approach.
Special diets include vegetarian (including vegan), macrobiotic, Atkins, Pritikin, and Ornish diets for both 2007 and 2012.
Traditional healers in 2007 include Curandero, Espiritista, Hierbero or Yerbera, Shaman, Botanica, Native American Healer or Medicine Man, and Sobador. Traditional healers in 2012 include Curandero, Machi, or Parchero; Yerbero or Hierbista; Shaman; Native American Healer or Medicine Man; Sobador; and Huesero.
Movement therapies include Feldenkrais, Alexander technique, Pilates, and Trager psychophysical integration for both 2007 and 2012.
NOTES: Estimates are based on household interviews of a sample of the civilian noninstitutionalized population. Estimates are age-adjusted using the projected 2000 U.S. population as the standard population and using two age groups: 4–11 and 12–17.
SOURCE: CDC/NCHS, National Health Interview Survey, 2007, 2012
Overall, among children who used any complementary health approach, 44.2% used it to treat a specific health problem or condition in 2007 and 45.6% in 2012.
Among children who used nonvitamin, nonmineral dietary supplements, the percentage using these products to treat a specific health condition decreased from 49.4% in 2007 to 35.5% in 2012. A similar decrease was seen for homeopathy (88.8% to 62.9%, respectively).
In 2012, acupuncture was the modality that had the highest percentage of users reporting use for treatment of a condition (70.1%). In 2007, homeopathy was the modality that had the highest percentage of users reporting use for treatment of a condition (88.8%).
Medical conditions treated with complementary health approaches, 2007 and 2012
Complementary health approaches are often used to treat a specific health problem or condition. Among children who used any complementary health approach, Table 5 presents selected health problems and conditions for which they were used.
Table 5.
Frequencies and age-adjusted percentages of children aged 4–17 years who used complementary health approaches in the past 12 months for specific conditions, among those who used complementary health approaches, by the condition for which it was used: United States, 2007 and 2012
| 2007 |
2012 |
||||
|---|---|---|---|---|---|
| Disease or condition1 | Number (in thousands) |
Age-adjusted percentage2 (standard error) |
Number (in thousands |
Age-adjusted percentage2 (standard error) |
p
value |
| Back or neck pain | 686 | 8.8 (1.12) | 602 | 8.9 (1.14) | † |
| Head or chest cold | 409 | 6.5 (1.38) | 294 | 5.1 (0.92) | † |
| Other musculoskeletal conditions | 345 | 5.0 (0.99) | 416 | 6.0 (0.98) | † |
| Anxiety or stress | 293 | 4.4 (0.94) | 221 | 3.4 (0.72) | † |
| ADHD or ADD3 | 150 | 2.3 (0.52) | 131 | 2.2 (0.59) | † |
| Insomnia or trouble sleeping | 134 | 2.0 (0.59) | 110 | 1.7 (0.43) | † |
| Constipation | ‡ | ‡ | 70 | 1.2 (0.38) | † |
| Respiratory allergy | ‡68 | ‡1.2 (0.53) | ‡69 | ‡1.0 (0.39) | † |
| Sore throat other than strep or tonsillitis | ‡94 | ‡1.4 (0.59) | ‡50 | ‡0.9 (0.42) | † |
| Sinusitis | ‡117 | ‡2.0 (0.78) | ‡45 | ‡0.7 (0.31) | † |
| Abdominal pain | ‡66 | ‡1.0 (0.39) | ‡44 | ‡0.6 (0.26) | † |
| Depression | ‡178 | ‡0.9 (0.28) | ‡41 | ‡0.6 (0.23) | † |
| Asthma | 112 | ‡1.8 (0.65) | ‡34 | ‡0.5 (0.21) | † |
Difference is not statistically significant.
Estimates are considered unreliable. Data have a relative standard error (RSE) greater than 30% and less than or equal to 50% and should be used with caution. Data not shown have an RSE greater than 50%.
Respondents may have used more than one modality to treat a disease or condition, but were counted only once under each disease or condition treated. The questions about using a modality to treat a disease or condition were only asked of respondents who had used the modality within the past 12 months. The exception to this is the questions about using nonvitamin, nonmineral dietary supplements to treat a disease or condition, which were only asked of respondents who had used nonvitamin, nonmineral dietary supplements within the past 30 days.
The denominator used in the calculation of percentages was the number of children who used complementary health approaches within the past 12 months, excluding persons with unknown information about whether a complementary health approach was used to treat the specified condition.
ADHD is attention deficit hyperactivity disorder and ADD is attention deficit disorder.
NOTES: Estimates are based on household interviews of a sample of the civilian noninstitutionalized population. Estimates are age-adjusted using the 2000 U.S. population as the standard population and using two age groups: 4–11 and 12–17.
SOURCE: CDC/NCHS, National Health Interview Survey, 2007 and 2012.
No statistically significant differences were seen between 2007 and 2012 in the proportion of individuals using complementary health approaches to treat or manage any of the conditions queried.
In 2007 and 2012, complementary health approaches were most often used for back or neck pain, head or chest cold, other musculoskeletal conditions, anxiety or stress, and attention deficit hyperactivity disorder (ADHD).
Conclusion
This report presents data from the 2007 and 2012 NHIS on the use of complementary health approaches among children aged 4–17 years in the United States. It focuses on the use of specific modalities in the past 12 months; the use of nonvitamin, nonmineral dietary supplements in the past 30 days; and complementary health approaches used to treat health problems or conditions. Further, it explores characteristics of children who use complementary health approaches and makes comparisons between 2007 and 2012. Although prevalence rates for overall use of complementary health approaches in 2007 and 2012 are presented, the 2012 questionnaire was substantially different from the 2007 questionnaire (13). For instance, a lower number of response options were included on the flashcard for nonvitamin, nonmineral dietary supplements, two diet-based modalities were eliminated, the list of traditional healers was modified, and deep-breathing exercise was removed as an independent health practice, all of which likely influenced the overall prevalence rate. Thus, while the prevalence of children using any complementary health approach did not change significantly (from 12.0% in 2007 to 11.6% in 2012), this finding must be viewed cautiously. When looking at individual approaches, there was a statistically significant decrease in the use of traditional healers and a significant increase in the use of yoga, tai chi, or qi gong. However, the decrease in the use of traditional healers may be due, in part, to the modification of the questionnaire (a decrease in the types of traditional healers that could be selected).
This report presents unique data examining the practices of yoga, meditation, and homeopathy in children. Children, like adults, substantially increased the practice of yoga between 2007 and 2012 (16). Within this same 5-year period, industry data suggest a 7.8% annual growth in the number of yoga instructors (17). The low cost (18) and the ability to practice in one’s own home may contribute to yoga’s growing popularity. Furthermore, public school systems are beginning to incorporate yoga into their fitness programs (19), which may accelerate use by children in the future.
Most children who practiced yoga incorporated meditation, deep-breathing exercises, or both into their practice; that is, traditional forms of yoga were practiced, not simply yoga as a type of exercise (20). Only about one-third of children who practiced yoga had taken a class or received formal training in the past 12 months. It is not clear what proportion of the remaining children had taken a class or received formal training prior to the past 12 months.
More than 900,000 children used meditation in 2012; of these, 760,000 (just over 80%) practiced meditation as a part of yoga, tai chi, or qi gong. Only about one-third of children who meditated participated in mantra, mindfulness, or spiritual meditation. Thus, meditation as a part of movement therapies is more common among children than meditation alone (20).
Of those children who had received homeopathic treatments, only a small proportion had seen a practitioner of homeopathy, suggesting that most use is self-care. This self-care use of homeopathy treatments is also reflected in industry sales data that show steady growth in the sales of homeopathic products over the last 10 years, with about 80% of sales occurring at retailers such as big box stores, grocery stores, and drug stores (21). To the best of the authors’ knowledge, there are no data assessing whether self-care with homeopathic products is equivalent to care from a trained homeopath. However, the Food and Drug Administration’s oversight of over-the-counter homeopathic products is far less stringent than for pharmaceuticals, and serious adverse events with the use of homeopathic over-the-counter remedies have been reported (22).
Similar to the results for adults (5), the use of nonvitamin, nonmineral dietary supplements; yoga, tai chi, or qi gong; and chiropractic or osteopathic manipulation varied considerably by demographic characteristics (e.g., sex, race and ethnicity, and insurance status). Looking at individual approaches, unique changes were seen over time in the frequencies with which these approaches were used to treat specific health conditions. For instance, there were large decreases in the percentage of children who used either nonvitamin, nonmineral dietary supplements or homeopathy to treat a specific health condition, but no changes for all other approaches.
Consistent with previous reports (5), the use of complementary health approaches in children, both overall and for individual modalities, is low compared with that seen in adults (16). For instance, while nonvitamin, nonmineral dietary supplements are the most common approach used by both adults and children, the use by children is almost one-quarter of the use by adults (4.9% compared with 17.7%).
In 2007, the most common nonvitamin, nonmineral dietary supplements used by children in the past 30 days were echinacea (0.8%), fish oil (0.7%), and combination herb pills (0.5%). There was a significant increase in fish oil use from 0.7% in 2007 to 1.1% in 2012. However, the use of echinacea and combination herb pills decreased such that the top three nonvitamin, nonmineral dietary supplements shifted slightly in 2012 to be fish oil (1.1%), melatonin (0.7%), and probiotics or prebiotics (0.5%). These changes in use patterns coincide to some degree with the publication of results from clinical trials. For instance, since the mid-2000s, several well-designed clinical trials have not seen any benefit of taking echinacea to treat or prevent the common cold (23,24). During this same time period, data supporting the use of fish oil for heart health have been accumulating (25); however, more recent work has been published that questions the magnitude of this effect (26). There is also some evidence that omega-3 fatty acid supplementation may have benefit for the treatment of ADHD in children (27).
Between 2007 and 2012, there was not much change in the top diseases or conditions treated with complementary health approaches. In fact, for both years, the use of complementary health approaches was most frequently reported for back or neck pain, head or chest cold, anxiety or stress, and other musculoskeletal conditions. As shown previously, back or neck pain is by far the most prevalent condition for which these approaches are used in children (16). This high use may reflect current best practice guidelines for the treatment of back pain issued jointly by the American College of Physicians and the American Pain Society (28).
Taken together, the breadth and depth of the 2012 NHIS child supplement on complementary health approaches provides the most comprehensive snapshot of the use of these approaches. The descriptive statistics and highlights presented in this report are the foundation for future studies of complementary health approaches. This report also reveals interesting relationships between the use of complementary health approaches in children over the span of 5 years. The expanded set of questions in the survey addressing the reasons children use these approaches, as well as perceived outcomes associated with their use, may help explain some of the observed variation in the use of individual approaches by population subgroups.
Technical Notes
Sample design
The National Health Interview Survey (NHIS) is a cross-sectional household interview survey of the U.S. civilian noninstitutionalized population. Data are collected continuously throughout the year in all 50 states and the District of Columbia. NHIS uses a multistage clustered sample design to produce national estimates for a variety of health indicators. Information on basic health topics is collected for all household members, if necessary by proxy, from one adult family member. Additional information is collected for one randomly selected adult and one randomly selected child in each family. Self-response is required for the Sample Adult questionnaire except in rare cases where sample adults are physically or mentally incapable of responding for themselves. Interviews are conducted in the home using computer-assisted personal interview techniques, with telephone interviewing permitted for follow-up if necessary. Starting in 2006, the sample design included Asian persons in the oversampling of minority populations in NHIS; previously, only households with non-Hispanic black and Hispanic persons were oversampled.
Response rate
In 2007, NHIS interviews were completed in 29,266 households, which yielded 75,764 persons in 29,914 families; the household response rate was 87.1%. The Sample Child questionnaire was completed for 9,417 children. The final response rate (which takes into account household and family nonresponse) for the 2007 sample child files was 76.5% (11). In 2012, NHIS interviews were completed in 42,366 households, which yielded 108,131 persons in 43,345 families; the household response rate was 77.6%. The Sample Child questionnaire was completed for 12,275 children. The final response rate (which takes into account household and family nonresponse) for the 2012 sample child files was 69.7% (12).
Procedures used in calculating response rates are described in detail in Appendix I of the NHIS Survey Description Document (11,12).
Age adjustment
Unless otherwise specified, percentages shown in this report were age-adjusted using the projected 2000 U.S. population provided by the U.S. Census Bureau as the standard population (29,30). Age adjustment was used to allow comparison among various population subgroups that have different age structures. This is particularly important for demographic characteristics such as race, ethnicity, and parent’s education. Age-adjusted percentages should also be used when assessing changes in prevalence over time when the age distribution of the population is changing. The following age groups were used for age adjustment: 4–11 and 12–17 years. Estimates were calculated using software for statistical analysis of correlated data (SUDAAN) (15). The SUDAAN procedure PROC DESCRIPT was used to produce age-adjusted percentages and their standard errors.
Using different age groups for age adjustment may result in slightly different percentages. For this reason, age-adjusted percentages for health characteristics in this report may not match age-adjusted percentages for the same health characteristics in other reports. Frequencies in this report are not age-adjusted.
For more information on the derivation of age-adjustment weights for use with National Center for Health Statistics survey data, see Klein and Schoenborn (30).
Tests of significance
Statistical reliability and hypothesis tests
Statistical tests performed to assess the significance of year-to-year differences in the estimates were two-tailed tests with no adjustments made for multiple comparisons. The test statistic used to determine statistical significance of the difference between two percentages was
where Xa and Xb are the two percentages being compared, and Sa and Sb are the SUDAAN-calculated standard errors of those percentages. The critical value used for two-sided tests at the 0.05 level of significance was 1.96.
Relative standard error
Standard errors, produced by using the SUDAAN statistical package, are shown for all percentages in the tables. Estimates with a relative standard error (RSE) greater than 30% and less than or equal to 50% should be used with caution as they do not meet standards of reliability or precision. Estimates with an RSE greater than 50% are not shown. RSEs are calculated as:
where SE is the standard error of the estimate, and Est is the estimate (percentage). The reliability of frequencies and their corresponding percentages is determined independently, so it is possible for a particular frequency to be reliable and its associated percentage unreliable, and vice versa. In most instances, however, both estimates were reliable (or unreliable).
Definition of terms related to complementary health approaches
Acupuncture
A family of procedures involving stimulation of anatomical points on the body by a variety of techniques. American practices of acupuncture incorporate medical traditions from China, Japan, Korea, and other countries. The acupuncture technique that has been most scientifically studied involves penetrating the skin with thin, solid, metallic needles that are manipulated by the hands or by electrical stimulation.
Alexander technique
A practice that uses guidance and education on ways to improve posture and movement. The intent is to teach a person how to use muscles more efficiently to improve the overall functioning of the body. Examples of the Alexander technique as a complementary health approach are using it to treat low-back pain and the symptoms of Parkinson’s disease.
Alternative provider or practitioner
Someone who is knowledgeable about a specific alternative health practice. This person provides care or gives advice about its use and usually receives payment for his or her services.
For some practices, the provider may have received formal training and been certified by a licensing board or related professional association. For example, a practitioner of biofeedback (biofeedback therapist) has usually received training in psychology and physiology and may be certified by the Biofeedback Certification International Alliance (formerly the Biofeedback Certification Institute of America).
Atkins diet
Emphasizes a drastic reduction in the daily intake of carbohydrates (40 grams or fewer), countered by an increase in protein and fat.
Ayurveda
A medical system that originated in India several thousand years ago. In the United States, Ayurveda is based on theories of health and illness, and on ways to prevent, manage, or treat health problems. Ayurveda aims to integrate and balance the body, mind, and spirit (thus, some view it as holistic). This balance is believed to lead to contentment and health and to help prevent illness. A chief aim of Ayurvedic practices is to cleanse the body of substances that can cause disease, and this is believed to help reestablish harmony and balance.
Biofeedback
A technique that uses simple electronic devices to teach clients how to consciously regulate bodily functions, such as breathing, heart rate, and blood pressure, to improve overall health. Biofeedback is used to reduce stress, eliminate headaches, recondition injured muscles, control asthma attacks, and relieve pain.
Botanica
A traditional healer who supplies healing products, sometimes associated with spiritual interventions.
Chelation therapy
A chemical process in which a substance is used to bind molecules, such as metals or minerals, and hold them tightly so that they can be removed from a system, such as the body. In medicine, chelation has been scientifically proven to rid the body of excess or toxic metals. For example, a person who has lead poisoning may be given chelation therapy to bind and remove excess lead from the body before it can cause damage.
Chiropractic manipulation
A form of health care that focuses on the relationship between the body’s structure, primarily the spine, and its function.
Craniosacral therapy
A body-based practice in which practitioners use light touch and manipulation focused on the skull and spine, with the intent of sensing and removing what they refer to as blockages or imbalances that may be contributing to a health condition.
Curandero, Machi, or Parchero
Types of traditional folk healers. Originally found in Latin America, these healers specialize in treating illness through the use of supernatural forces, herbal remedies, and other natural medicines.
Deep-breathing exercises
An active process that involves conscious control over breathing in and out. This may involve controlling the way in which air is drawn in (for example, through the mouth or nostrils), the rate (for example, quickly or over a length of time), the depth (for example, shallow or deep), and the control of other body parts (for example, relaxation of the stomach).
Energy healing therapy
A technique that involves channeling healing energy through the hands of a practitioner into the client’s body to restore a normal energy balance and, therefore, health. Energy healing therapy has been used to treat a wide variety of ailments and health problems, and it is often used with other alternative and conventional medical treatments.
Espiritista
A traditional healer who assesses a patient’s condition and recommends herbs or religious amulets to improve physical or mental health or to help overcome a personal problem.
Feldenkrais
A method of education in physical coordination and movement. Practitioners use verbal guidance and light touch to teach the method through one-on-one lessons and group classes. The intent is to help the person become more aware of how the body moves through space and to improve physical functioning.
Guided imagery
Used for healing or health maintenance and involves a series of relaxation techniques followed by the visualization of detailed images, usually calm and peaceful in nature. If used for treatment, the individual will visualize their body free of the specific problem or condition. Sessions are typically 20 to 30 minutes in length, and may be practiced several times a week.
Hierbero, Yerbero, or Hierbista
A practitioner with knowledge of the medicinal qualities of plants.
Homeopathic treatment
A system of medical practices based on the theory that any substance that can produce symptoms of disease or illness in a healthy person can cure those symptoms in a sick person.
Huesero
A “bone setter” (in Hispanic folk healing) who specializes in bone ailments, mainly lesions and fractures.
Hypnosis
An altered state of consciousness characterized by increased responsiveness to suggestion. This hypnotic state is attained by first relaxing the body, then shifting attention toward a narrow range of objects or ideas as suggested by the hypnotist or hypnotherapist. The procedure is used to effect positive changes and to treat numerous health conditions including ulcers, chronic pain, respiratory ailments, stress, and headaches.
Macrobiotic diet
A diet low in fat that emphasizes whole grains and vegetables, and restricts the intake of fluids. Of particular importance is the consumption of fresh, nonprocessed foods.
Mantra meditation
A type of meditation in which the meditator focuses on a mantra (a specially chosen word, sound, or phrase that is repeated silently).
Massage
Therapists manipulate muscle and connective tissue to enhance function of those tissues and promote relaxation and wellbeing.
Meditation
A group of techniques, most of which started in Eastern religious or spiritual traditions. In meditation, individuals learn to focus their attention and suspend the stream of thoughts that normally occupy the mind. This practice is believed to result in a state of greater physical relaxation, mental calmness, and psychological balance. Practicing meditation can change how a person relates to the flow of emotions and thoughts in the mind.
Mindfulness meditation
A type of meditation based on the concept of being mindful or having increased awareness of the present. It uses breathing methods, guided imagery, and other practices to relax the body and mind and help reduce stress. It is also known as mindfulness relaxation and mindfulness-based stress reduction.
Native American Healer or Medicine Man
A traditional healer who uses information from the spirit world to benefit the community. People see Native American healers for a variety of reasons, especially to find relief from or a cure for illness or to find spiritual guidance.
Naturopathy
An alternative medical approach based on the belief that there is a healing power in the body that establishes, maintains, and restores health. Practitioners work with the patient with a goal of supporting this power through treatments such as nutrition and lifestyle counseling, dietary supplements, medicinal plants, exercise, homeopathy, and treatments from traditional Chinese medicine.
Nonvitamin, nonmineral dietary supplements
Taken by mouth and contain a dietary ingredient intended to supplement the diet other than vitamins and minerals. Examples include herbs or herbal medicine (as single herbs or mixtures), other botanical products such as soy or flax products, and dietary substances such as enzymes and glandulars. Among the most popular are echinacea, ginkgo biloba, ginseng, feverfew, garlic, kava kava, and saw palmetto. Garlic, for example, has been used to treat fevers, sore throats, digestive ailments, hardening of the arteries, and other health problems and conditions.
Ornish diet
A high-fiber, low-fat vegetarian diet that promotes weight loss and health by controlling what one eats, not by restricting the intake of calories. Fruits, beans, grains, and vegetables can be eaten at all meals, while nonfat dairy products such as skim milk, nonfat cheeses, and egg whites are to be eaten in moderation. Products such as oils, avocados, nuts and seeds, and meats of all kind are avoided.
Osteopathic manipulation
A full-body system of hands-on techniques to alleviate pain, restore function, and promote health and wellbeing.
Pilates
A method of physical exercise used to strengthen and build control of muscles, especially those used for posture. Awareness of breathing and precise control of movements are integral components of Pilates. Special equipment, if available, is often used.
Pritikin diet
A diet low in fat that emphasizes the consumption of foods with large volumes of fiber and water, including many vegetables; fruits; beans; and natural, unprocessed grains. Meat is allowed.
Progressive relaxation
A technique used to relieve tension and stress by systematically tensing and relaxing successive muscle groups.
Qi gong
An ancient Chinese discipline combining the use of gentle physical movements, mental focus, and deep breathing directed toward specific parts of the body. Performed in repetitions, the exercises are normally performed two times or more a week for 30 minutes at a time.
Shaman
Said to act as a medium between the invisible spiritual world and the physical world. Most gain knowledge through contact with the spiritual world and use the information to perform tasks such as divination, influencing natural events, and healing the sick or injured.
Sobador
Uses massage and rubbing techniques to treat patients.
Spiritual meditation
May be performed according to the practices of one of the major religions or within a spiritual tradition. The techniques used may be the same as in other types of meditation (for example, Transcendental Meditation), but the focus is on spirituality (such as repeating a spiritual, meditative phrase).
Tai chi
A mind-body practice that originated in China as a martial art. Individuals doing tai chi move their bodies slowly and gently, while breathing deeply and meditating (tai chi is sometimes called moving meditation). Many practitioners believe that tai chi helps the flow throughout the body of a proposed vital energy called “qi.” Individuals practicing tai chi move their bodies in a slow, relaxed, and graceful series of movements. One can practice alone or in a group. The movements make up what are called forms (or routines).
Traditional healer
Someone who employs any one of a number of ancient medical practices that are based on indigenous theories, beliefs, and experiences handed down from generation to generation, often orally. The methods employed by each type of traditional healer have evolved to reflect the different philosophical backgrounds and cultural origins of the healer.
Trager psychophysical integration
A therapy in which practitioners apply a series of gentle, rhythmic rocking movements to the joints. They also teach physical and mental self-care exercises to reinforce the proper movement of the body. The intent is to release physical tension and increase the body’s range of motion. An example of Trager psychophysical integration therapy is using it to treat chronic headaches.
Vegetarian diet
A diet that does not include any meat. There are, however, numerous variations on the nonmeat theme. For example, some vegetarian diets (called vegan diets) are restricted to plant products only, while others may include eggs and dairy products. Another variation limits consumption to raw fruit, sometimes supplemented with nuts and vegetables. Finally, a number of vegetarian diets prohibit alcohol, sugar, caffeine, or processed foods.
Yoga
A combination of breathing exercises, physical postures, and meditation to calm the nervous system and balance the body, mind, and spirit.
References
- 1.National Center for Complementary and Alternative Medicine . Exploring the science of complementary and alternative medicine: Third strategic plan: 2011–2015. U.S. Department of Health and Human Services, National Institutes of Health, National Center for Complementary and Alternative Medicine; Washington, DC: 2011. NIH Publication number 11–7643, D458. [Google Scholar]
- 2.Birdee GS, Phillips RS, Davis RB, Gardiner P. Factors associated with pediatric use of complementary and alternative medicine. Pediatrics. 2010;125(2):249–56. doi: 10.1542/peds.2009-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bethell C, Kemper KJ, Gombojav N, Koch TK. Complementary and conventional medicine use among youth with recurrent headaches. Pediatrics. 2013;132(5):e1173–83. doi: 10.1542/peds.2013-1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simkin DR, Popper CW. Alternative and complementary therapies for children with psychiatric disorders, Part 1. Child and Adolesc Psychiatr Clin N Am. 2013;22(3) doi: 10.1016/j.chc.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National Center for Health Statistics; Hyattsville, MD: 2008. National health statistics reports; no 12. Available from: http://www.cdc.gov/nchs/data/nhsr/nhsr012.pdf. [PubMed] [Google Scholar]
- 6.Wells RE, Bertisch SM, Buettner C, Phillips RS, McCarthy EP. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51(7):1087–97. doi: 10.1111/j.1526-4610.2011.01917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quandt SA, Chen H, Grzywacz JG, Bell RA, Lang W, Arcury TA. Use of complementary and alternative medicine by persons with arthritis: Results of the National Health Interview Survey. Arthritis Rheum. 2005;53(5):748–55. doi: 10.1002/art.21443. [DOI] [PubMed] [Google Scholar]
- 8.Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern Ther Health Med. 2005;11(1):42–9. [PubMed] [Google Scholar]
- 9.Astin JA. Why patients use alternative medicine: Results of a national study. JAMA. 1998;279(19):1548–53. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 10.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA. 1998;280(18):1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 11.National Center for Health Statistics 2007 National Health Interview Survey (NHIS): Public use data release. NHIS survey description. 2007 Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2007/srvydesc.pdf.
- 12.National Center for Health Statistics . NHIS survey description. 2012. 2012 National Health Interview Survey (NHIS): Public use data release. Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2012/srvydesc.pdf. [Google Scholar]
- 13.Stussman BJ, Bethell CD, Gray C, Nahin RL. Development of the adult and child complementary medicine questionnaires fielded on the National Health Interview Survey. BMC Complement Altern Med. 2013;13:328. doi: 10.1186/1472-6882-13-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parsons VL, Moriarity C, Jonas K, et al. Design and estimation for the National Health Interview Survey, 2006–2015. National Center for Health Statistics. Vital Health Stat. 2014;2(165) [PubMed] [Google Scholar]
- 15.RTI International SUDAAN (Release 11.0.0) [computer software] 2009 [Google Scholar]
- 16.Clarke TC, Black LI, Stussman BJ, et al. Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Center for Health Statistics; Hyattsville, MD: 2015. National health statistics reports; no 79. [PMC free article] [PubMed] [Google Scholar]
- 17.Moldvay C. IBISWorld industry report OD4185: Pilates & yoga studios in the US. IBISWorld, Inc.; Los Angeles, CA: 2012. [Google Scholar]
- 18.Nahin RL, Barnes PM, Stussman BJ, Bloom B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. National Center for Health Statistics; Hyattsville, MD: 2009. National health statistics reports; no 18. Available from: http://www.cdc.gov/NCHS/data/nhsr/nhsr018.pdf. [PubMed] [Google Scholar]
- 19.Abcarian R. Yoga in public schools is exercise, not religion. Los Angeles Times; Jul 1, 2013. [Google Scholar]
- 20.Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, et al. Meditation practices for health: State of the research. Evid Rep Technol Assess (Full Rep) 2007;155:1–263. [PMC free article] [PubMed] [Google Scholar]
- 21.Nutrition Business Journal . Supplement business report. Penton Media, Inc.; Boulder, CO: 2013. [Google Scholar]
- 22.Kuehn BM. Despite health claims by manufacturers, little oversight for homeopathic products. JAMA. 2009;302(15):1631–2. doi: 10.1001/jama.2009.1476. [DOI] [PubMed] [Google Scholar]
- 23.Barrett B, Brown R, Rakel D, Mundt M, Bone K, Barlow S, Ewers T. Echinacea for treating the common cold: A randomized trial. Ann Intern Med. 2010;153(12):769–77. doi: 10.7326/0003-4819-153-12-201012210-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turner RB, Bauer R, Woelkart K, Hulsey TC, Gangemi JD. An evaluation of Echinacea angustifolia in experimental rhinovirus infections. N Engl J Med. 2005;353(4):341–8. doi: 10.1056/NEJMoa044441. [DOI] [PubMed] [Google Scholar]
- 25.Marik PE, Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: A systematic review. Clin Cardiol. 2009;32(7):365–72. doi: 10.1002/clc.20604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kotwal S, Jun M, Sullivan D, Perkovic V, Neal B. Omega-3 fatty acids and cardiovascular outcomes: Systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2012;5(6):808–18. doi: 10.1161/CIRCOUTCOMES.112.966168. [DOI] [PubMed] [Google Scholar]
- 27.Bloch MH, Qawasmi A. Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomology: Systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2011;50(10):991–1000. doi: 10.1016/j.jaac.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 29.Day JC. Population projections of the United States by age, sex, race, and Hispanic origin: 1995 to 2050. U.S. Government Printing Office; Washington, DC: 1996. U.S. Bureau of the Census, Current Population Reports, P25–1130. [Google Scholar]
- 30.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. National Center for Health Statistics; Hyattsville, MD: 2001. Healthy People Statistical Notes, no. 20. Available from: http://www.cdc.gov/nchs/data/statnt/statnt20.pdf. [PubMed] [Google Scholar]
- 31.Office of Management and Budget Revisions to the standards for the classification of federal data on race and ethnicity. Fed Regist. 1997;62(210):58781–90. [Google Scholar]