Summary
Adequate pre-dialysis care reduces mortality among end-stage renal disease (ESRD) patients. We tested the hypothesis that individuals with ESRD due to sickle cell disease (SCD–ESRD) receiving pre-ESRD care have lower mortality compared to individuals without pre-ESRD care. We examined the association between mortality and pre-ESRD care in incident SCD–ESRD patients who started haemodialysis between 1 June, 2005 and 31 May, 2009 using data provided by the Centers for Medicare and Medicaid Services (CMS). SCD–ESRD was reported for 410 (0·1%) of 442 017 patients. One year after starting dialysis, 108 (26·3%) patients with incident ESRD attributed to SCD died; the hazard ratio (HR) for mortality among patients with SCD–ESRD compared to those without SCD as the primary cause of renal failure was 2·80 (95% confidence interval [CI] 2·31–3·38). Patients with SCD–ESRD receiving pre-dialysis nephrology care had a lower death rate than those with SCD–ESRD who did not receive pre-dialysis nephrology care (HR = 0·67, 95% CI 0·45–0·99). The one-year mortality rate following an ESRD diagnosis was almost three times higher in individuals with SCD when compared to those without SCD but with ESRD and could be attenuated by pre-dialysis nephrology care.
Keywords: sickle cell disease, kidney disease, end-stage renal disease, mortality, disparities
Sickle cell disease (SCD) is a genetic disorder that occurs among approximately 1 in 365 Blacks or African Americans in the United States (Hassell, 2010). Prior to recent innovations in treatment protocols that have increased the life expectancy for this population, children born with SCD often died during early adolescence (Platt et al, 1994). Now, almost 94% of children with SCD are expected to become adults (Quinn et al, 2010). Chronic kidney disease (CKD) occurs among approximately 30% of these individuals and a proportion of them will develop end-stage renal disease (ESRD) (Powars et al, 1991). Renal replacement therapy (RRT) with dialysis (haemo or peritoneal) or kidney transplantation substantially extends the life expectancy of individuals with ESRD.
The first-year United States mortality rate among all patients using haemodialysis is quite high. However, appropriate medical care prior to the start of RRT decreases the risk of early death (Bradbury et al, 2007; McClellan et al, 2009). Appropriate medical care, defined by widely disseminated clinical practice guidelines, includes nephrology referral at least 6 months before the anticipated start of RRT and the placement of a functioning arteriovenous fistula (AVF) prior to the initiation of haemodialysis (National Kidney Foundation, 2001a, 2002). Despite the importance of early pre-ESRD care for patient well-being and survival, recent studies have reported that fewer than half of all patients with incident ESRD have seen a nephrologist and fewer than one in five have an AVF in place at the start of dialysis (Collins et al, 2009). For special populations, such as individuals with SCD, adequate precare prior to RRT might be particularly beneficial to lower their risk for adverse outcomes and improve survival.
The relationship between mortality and pre-ESRD care among individuals with SCD has not been examined previously. We tested the hypothesis that pre-ESRD care is associated with lower mortality among individuals with SCD.
Methods
Study design and population
We conducted a population-based cohort study of patients with incident ESRD with a diagnosis of SCD listed as their primary cause of renal failure. Dialysis facilities are required by federal law to provide the Centers for Medicare and Medicaid Services (CMS) with information on all patients receiving RRT. Patients starting RRT with haemodialysis as their initial treatment modality during the period from 1 June, 2005 to 31 May, 2009, were included in our cohort. Patients were included in the analysis if they were younger than 100 years of age. Mortality was ascertained from the start date of the initial haemodialysis treatment until death or the last day of follow up. This study was approved by the Emory University institutional review board.
Data sources
Participant information was obtained from the Form CMS-2728, which is completed for all patients at the start of incentre or home haemodialysis and confirmed as accurate by a physician. Data elements for this study included: age category (<65 years vs. ≥65 years), sex, race as recorded on the Form CMS-2728 (‘Black or African American’ versus ‘White’), height and weight used to calculate body mass index (BMI), the primary cause of ESRD, past medical history, the patient’s type of vascular access at the initiation of haemodialysis, and laboratory values for haemoglobin concentrations, serum, creatinine, and serum albumin before and after the start of dialysis. The race category was restricted to patients identified as ‘Black or African American’ or ‘White’ on the Form CMS-2728 because of the small numbers of patients in other racial groups. Form CMS-2728 contains information on pre-existing comorbid conditions that are not listed as the primary cause of ESRD, which include diabetes mellitus (DM), congestive heart failure (CHF), atherosclerotic cardiovascular disease (ASHD), cerebrovascular disease (CVA or TIA), peripheral vascular disease (PVD), and history of hypertension (HxHT). If a comorbid condition was not indicated on the Form CMS-2728, we assumed for the purposes of this analysis that it was not present. Functional status (amputation, inability to ambulate, needs assistance ambulating, and institutionalized at the start of haemodialysis), employment status 6 months prior to starting haemodialysis, and insurance status as assessed by dialysis facility staff were abstracted from the Form CMS-2728.
Study variables
Sickle cell disease
The attending nephrologist attested to the accuracy of the recorded primary diagnosis before Form CMS-2728 was submitted to CMS. We defined a patient as having a diagnosis of SCD-ESRD if ‘sickle cell disease/anaemia’ was designated on the Form CMS-2728 as the primary cause of renal failure.
Outcome
The outcome of our study was all-cause mortality following the start of haemodialysis. Follow-up for each patient began on the day of the first dialysis treatment and patients who did not die were censored (their follow-up ended) at the completion of the study period. Mortality was identified by monitoring death notification forms routinely submitted to CMS-funded ESRD Networks by dialysis facility staff.
Pre-ESRD care
Characteristics of pre-ESRD care recorded on the Form CMS-2728 included the presence and duration of nephrology care prior to starting dialysis and whether a functional AVF for vascular access was in place at the start of dialysis or a central venous catheter was used instead. Pre-ESRD nephrology care was ascertained on the Form CMS-2728 with the following question: ‘Prior to ESRD therapy: Was patient under care of a nephrologist?’ If the answer was ‘yes,’ the duration of care was indicated as either ‘6–12 months’ or >12 months. We defined two levels of nephrology care: (i) any pre-ESRD nephrology care as defined by ‘yes’ to the root of this question and (ii) pre-ESRD care with a duration of 6 or more months defined as the sum of those answering either answering ‘6–12 months’ or ‘>12 months’.
Arteriovenous fistula and catheter use at the start of haemodialysis was ascertained on pre-dialysis by asking, ‘What access was used on first outpatient dialysis?’ Possible responses were: (i) ‘AVF,’ (ii) ‘Graft,’ (iii) ‘Catheter,’ and (iv) ‘Other.’ We defined a functioning AVF or catheter to be present if the method of vascular access used on the first outpatient dialysis treatment was reported on the Form CMS-2728 to be an AVF or catheter, respectively.
Statistical analysis
Means and proportions were used to describe individual characteristics and chi-square tests and analysis of variance to test the associations among study variables. Using logistic regression, we examined the independent associations between SCD–ESRD and pre-ESRD care. We conducted general linear models to control for clustering within ESRD Network areas and assessed patient characteristics that were individually associated with a higher risk of death. In these analyses, we controlled for age, sex, race (‘Black or African American versus ‘White’), BMI, a set of comorbid conditions (DM, CHF, ASHD, PVD, and HxHT), and a set of functional status variables (amputation, inability to ambulate, and residence in an institutional setting), as well as unemployment and no health insurance prior to starting dialysis.
Kaplan–Meier (KM) survival curves were obtained using the log rank test to assess if survival for patients with or those without SCD as the primary cause of renal failure was statistically different. We then conducted Cox regression models to determine patient characteristics that were associated individually with higher risk of death, adjusting for potential confounding factors that included age category, sex, race, cause of ESRD, comorbid conditions, functional status, unemployment, health insurance status at the start of RRT, haemoglobin level, and ESRD Network. Our modelling strategy, to obtain the best model, was based on a priori consideration of bivariate analyses and clinical judgment to select the most important variables. The three most prevalent comorbidities were used for the final model. Given the small sample of SCD–ESRD patients and the large number of covariates, we also performed a model using back-ward elimination to achieve the most parsimonious model. We calculated adjusted hazard ratios (HRs) with their associated 95% confidence intervals (CIs) and checked the proportional hazard assumption using the graphical method. The precare analysis was performed without controlling for ESRD Network due to the insufficient numbers of patients across Networks. Finally, these analyses were repeated with only ‘Black or African American’ patients and the results were not changed substantively. These analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
There were 442 099 patients with incidental ESRD that received haemodialysis within the study time frame between 1 June, 2005 and 31 May, 2009. We excluded 80 patients with incomplete data, none of whom had SCD, resulting in a sample of 442 019 eligible ESRD incident haemodialysis patients. Of these, 410 individuals had a diagnosis of SCD–ESRD, representing 0·1% of all patients with incident ESRD that received haemodialysis. Fifty-three per cent of patients with SCD–ESRD were male. The mean age of those with SCD–ESRD was 42·8 [standard deviation (SD) = 12·6] years and 97·6% were identified as ‘Black or African American.’
Patients with SCD–ESRD were less likely to be 65 years of age or older compared with other haemodialysis patients with incident ESRD [odds ratio (OR) = 0·06, 95% CI 0·03–0·11] (Table I). Further, individuals with SCD–ESRD were less likely than other incident ESRD haemodialysis patients to have a history of treated DM (OR = 0·08 95% CI 0·05–0·12), ASHD (OR = 0·42, 95% CI 0·21–0·85), and HxHT (OR = 0·50, 95% CI 0·41–0·60) (Table I), but they were more likely than other patients with incident ESRD to have a history of CHF (OR = 1·72, 95% CI 1·39–2·13) and stroke (OR = 1·39, 95% CI 1·16–1·65). In contrast to their counterparts, patients with SCD–ESRD had significantly lower BMI (OR = 0·21, 95% CI 0·18–0·26). Further, patients with SCD–ESRD were more likely than the other ESRD patients to be unemployed (OR = 1·40, 95% CI 1·05–1·87), but less likely to be uninsured (OR = 0·23, 95% CI 0·17–0·31). Between those with and those without SCD–ESRD, there were significant differences in the level of anaemia at the time of the initiation of haemodialysis (mean haemoglobin, 79 vs. 100 g/l, P ≤ 0·0001) and mean serum creatinine (6·6 vs. 6·0 μmol/l, P ≤ 0·0001). The prevalence of severe anaemia (haemoglobin 70–90 g/l) was higher among individuals with SCD–ESRD, 70·9% of all subjects compared to 24·9% of the other ESRD patients.
Table I.
Characteristics of end-stage renal disease patients with and without sickle cell disease as the primary cause of renal failure, starting haemodialysis during the period 1June 1, 2005, to 31 May, 2009, N = 442 017.
| SCD–ESRD |
Non-SCD–ESRD |
OR (95% CI)* |
|||||
|---|---|---|---|---|---|---|---|
| All |
Black or African American |
White |
SCD–ESRD versus non-SCD–ESRD |
||||
| Characteristic | n | % | n | % | n | % | |
| 410 | 0·1 | 127 270 | 28·8 | 314 337 | 71·1 | ||
| Demographic characteristics | |||||||
| Age (years) | |||||||
| <65 | 396 | 96·6 | 82 138 | 64·5 | 145 829 | 46·4 | – |
| ≥65 | 14 | 3·4 | 45 114 | 35·5 | 168 469 | 53·6 | 0·06 (0·03–0·11) |
| Sex | |||||||
| Male | 219 | 53·4 | 65 710 | 51·6 | 182 100 | 57·9 | 0·85 (0·71–1·02) |
| Female | 191 | 46·6 | 61 560 | 48·4 | 132 237 | 42·1 | – |
| Race as shown on Form CMS-2728 | |||||||
| Black or African American | 400 | 97·6 | 127 270 | 100·0 | – | – | 81·51 (35·61–186·55) |
| White | 10 | 2·4 | – | – | 314 337 | 100·0 | |
| Comorbid conditions | |||||||
| DM | 18 | 4·4 | 58 546 | 46·0 | 148 264 | 47·2 | 0·08 (0·05–0·12) |
| CHF | 104 | 25·4 | 37 726 | 29·6 | 106 669 | 33·9 | 1·72 (1·39–2·13) |
| ASHD | 14 | 3·4 | 17 741 | 13·9 | 76 884 | 24·5 | 0·42 (0·21–0·85) |
| CVA | 33 | 8·1 | 12 710 | 10·0 | 29 353 | 9·3 | 1·39 (1·16–1·65) |
| PVD | 15 | 3·7 | 12 887 | 10·1 | 49 958 | 15·9 | 0·83 (0·48–1·43) |
| HxHT | 295 | 72·0 | 112 079 | 88·1 | 259 400 | 82·5 | 0·50 (0·41–0·60) |
| BMI (kg/m2) | |||||||
| <25 | 302 | 74·2 | 43 545 | 34·4 | 116 073 | 37·2 | – |
| ≥25 | 105 | 25·8 | 82 943 | 65·6 | 196 294 | 62·8 | 0·21 (0·18–0·26) |
| Amputation | 1 | 0·2 | 4004 | 3·2 | 10 091 | 3·2 | 0·19 (0·02–1·44) |
| Unable to ambulate | 9 | 2·2 | 8280 | 6·5 | 22 163 | 7·1 | 0·60 (0·30–1·19) |
| Needs assistance | 26 | 6·3 | 12 989 | 10·2 | 36 428 | 11·6 | −1·19 (0·87–1·64) |
| Institutionalized | 12 | 2·9 | 9096 | 7·2 | 25 092 | 8·0 | 0·63 (0·34–1·18) |
| Unemployment | 172 | 42·0 | 33 180 | 26·1 | 47 878 | 15·2 | 1·40 (1·05–1·87) |
| No health insurance | 23 | 5·6 | 14 082 | 11·1 | 18 947 | 6·0 | 0·23 (0·17–0·31) |
SCD, sickle cell disease; ESRD, end-stage renal disease; OR, odds ratio; CI, confidence interval; DM, diabetics mellitus; CHF, congestive heart failure; ASHD, atherosclerotic heart disease; CVA, cerebrovascular disease; PVD, peripheral vascular disease; HxHT, history of hypertension; BMI, body mass index.
OR adjusted for age category, sex, race (‘Black or African American’ versus ‘White’), DM, CHF, ASHD, CVA, PVD, HxHT, BMI, amputation, unable to ambulate, needs assistance, institutionalized, unemployed, no health insurance, and End Stage Renal Disease Network.
The majority of patients with SCD–ESRD (53·9%) reported seeing a nephrologist prior to starting haemodialysis, with fewer than half (43·9%) reporting being under the care of a nephrologist for 6 months or longer prior to starting haemodialysis (Table II). After controlling for all confounding factors, patients with SCD–ESRD were more likely than the other ESRD patients to have seen a nephrologist both prior to starting haemodialysis (OR = 1·24, 95% CI 1·04–1·48) and for 6 months or longer prior to the start of treatment (OR = 1·25, 95% CI 1·10–1·43) (Table II).
Table II.
Nephrology care among incident end-stage renal disease haemodialysis patients with and without sickle cell disease as the primary cause of renal failure, June 2005 to May 2009, N = 442 017.
| SCD–ESRD |
Non-SCD–ESRD |
OR (95% CI)* |
||
|---|---|---|---|---|
| All |
Black or African American |
White |
||
| Measure |
n = 410,% Receiving care |
n = 127 270,% Receiving care |
n = 314 337,% Receiving care |
SCD–ESRD versus Non-SCD–ESRD |
| Any pre-dialysis care | 53·9 | 54·5 | 59·7 | 1·24 (1·04–1·48) |
| Pre-dialysis care > 6 months | 43·9 | 44·0 | 48·5 | 1·25 (1·10–1·43) |
| Use of catheter at start of dialysis | 76·1 | 77·2 | 75·2 | 0·95 (0·74–1·22) |
| AVF at start of dialysis | 6·8 | 11·9 | 13·5 | 0·61 (0·40–0·92) |
SCD, sickle cell disease; ESRD, end-stage renal disease; OR, odds ratio; CI, confidence interval; AVF, arteriovenous fistula.
OR adjusted for age category, sex, race (‘Black or African American’ versus ‘White’), diabetics mellitus, congestive heart failure, atherosclerotic heart disease, cerebrovascular disease, peripheral vascular disease, history of hypertension, body mass index, amputation, inability to ambulate, institutionalized, unemployed, no health insurance, and End-Stage Renal Disease Network.
At the start of dialysis, a functioning AVF was reported present among 6·8% of patients with SCD–ESRD, 11·9% of ‘Black or African American’ patients without SCD–ESRD and 13·5% of ‘White’ patients without SCD–ESRD. Patients with SCD–ESRD were less likely to have started haemodialysis with an AVF than other ESRD patients (OR = 0·61, 95% CI 0·40–0·92). The majority of individuals with SCD–ESRD (76·1%) started dialysis with a central venous catheter, and were as likely to have a catheter for the first haemodialysis (OR = 0·95, 95% CI 0·74–1·22) as other incident patients (Table II).
During the 4·25 years of follow-up, there were 183 deaths among individuals with SCD–ESRD, accounting for 44·6% of all patients with SCD–ESRD. In contrast, there were 152 496 (34·5%) deaths among other incident ESRD patients. The median follow-up time for all patients with ESRD was 529·0 d (range: 0–1553 d; SD = 606·1). Further, among patients with ESRD attributed to SCD, the median follow-up was 467·5 d (range: 17–1545 d; SD = 574·0). The fully adjusted HR for mortality among patients with SCD–ESRD compared with those without SCD–ESRD was 2·95 (95% CI = 2·55–3·41).
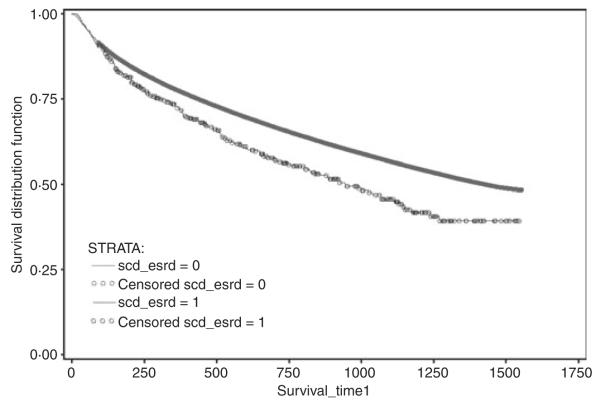
The rate of death during the study period was higher among patients with SCD–ESRD when compared to those without SCD-associated ESRD (log rank test: P < 0·0001) (Fig 1). Twenty-six per cent of patients with incident SCD–ESRD died within the first year of haemodialysis. In the first year of dialysis, the fully adjusted HR for mortality among patients with SCD–ESRD compared to those without SCD–ESRD was 2·80 (95% CI 2·31–3·38). In addition to SCD, patient characteristics independently associated with a higher rate of death were older age, males, ‘Black or African American’ race, and a higher BMI, as well as the presence of comorbid conditions (DM, CHF, CVA, PVD, and HxHT), decreased baseline glomerular filtration rate and haemoglobin levels, lower functional status (amputation, inability to ambulate, and institutionalized), being unemployed at the time of the ESRD, and having no insurance.
Fig 1.
Kaplan–Meier mortality survival curves (Up to 1,553 d (4·25 years) of survival) for incident end-stage renal disease (ESRD) haemodialysis patients with and without sickle cell disease as the primary cause of renal failure, (Log rank test: P < 0·0001) June 2005 to May 2009, N = 442 015. Incident ESRD patients without sickle cell disease (SCD) as the primary cause of renal failure, as recorded on Form CMS-2728. Incident ESRD patients with SCD as the primary cause of renal failure.
The associations between risk of death and individual variables of pre-ESRD care during the follow-up period are shown in Table III. In the non-SCD–ESRD cohort the risk of premature death within the study period among those receiving any pre-dialysis nephrology care was significantly lower by 33% (HR = 0·67, 95% CI 0·45–0·99). The risk of death among patients with SCD–ESRD receiving pre-dialysis care for ≥6 months was not statistically different from that of the group that received pre-dialysis care for <6 months (HR = 0·75, 95% CI 0·51–1·12). In contrast, among the ESRD haemodialysis population without SCD, early pre-dialysis care, defined as more than 6 months prior to the start of dialysis, was associated with a 22% (HR = 0·78, 95% CI 0·77-0·80) decrease in death when compared to receipt of pre-dialysis care for <6 months prior to dialysis.
Table III.
One year mortality risk* among incident end-stage renal disease (ESRD) haemodialysis patients with sickle cell disease as the primary cause of renal failure, by pre-ESRD care and race, June 2005 to May 2009, n = 410.
| Precare measure | HR (95% CI) for death† | HR (95% CI) for death‡ | HR (95% CI) for death§ |
|---|---|---|---|
| Any pre-dialysis nephrologist care | |||
| All | 0·73 (0·50–1·06) | 0·67 (0·45–0·99) | 0·75 (0·51–1·10) |
| Black or African American¶ | 0·68 (0·46–1·00) | 0·66 (0·44–0·97) | 0·72 (0·49–1·06) |
| Pre-dialysis nephrologist care ≥6 months | |||
| All | 0·81 (0·55–1·19) | 0·75 (0·51–1·12) | 0·84 (0·57–1·23) |
| Black or African American¶ | 0·75 (0·51–1·17) | 0·73 (0·49–1·08) | 0·79 (0·54–1·17) |
| Use of catheter at start of dialysis | |||
| All | 1·48 (0·91–2·40) | 1·34 (0·81–2·21) | 1·34 (0·82–2·18) |
| Black or African American¶ | 1·48 (0·91–2·43) | 1·32 (0·80–2·17) | 1·34 (0·82–2·19) |
| AVF at start of dialysis | |||
| All | 0·75 (0·33–1·71) | 0·79 (0·34–1·83) | 0·73 (0·32–1·66) |
| Black or African American¶ | 0·78 (0·33–1·79) | 0·79 (0·34–1·84) | 0·72 (0·31–1·64) |
HR, hazard ratio; CI, confidence interval; AVF, arteriovenous fistula.
Up to 1,553 d (4·25 years) of survival.
HR adjusted for age, sex, race (‘Black or African American’ versus ‘White’), diabetes mellitus, history of hypertension, and body mass index (Model with 3 most prevalent comorbidities).
HR adjusted for age category, sex, race (‘Black or African American’ versus ‘White’), diabetics mellitus, congestive heart failure, atherosclerotic heart disease, cerebrovascular disease, peripheral vascular disease, history of hypertension, body mass index, amputation; inability to ambulate, institutionalized, unemployed, and health insurance (Full model).
HR adjusted for congestive heart failure and inability to ambulate (Backward elimination model).
In the models with Black or African American only the variable race (‘Black or African American’ versus ‘White’) was dropped.
The type of venous access used for the first dialysis was not associated with survival of patients with SCD–ESRD. Having an AVF at the start of haemodialysis was not associated with a significant reduction in mortality (HR = 0·79, 95% CI 0·34–1·83), nor was the use of a central venous catheter associated with an increase in risk of early death among those with SCD–ESRD (HR = 1·34, 95% CI 0·81–2·21). Data regarding the cause of death were available for two of the four study years (2005 and 2007). The most frequent causes of death for those with SCD were arrhythmia (33·3%) and infections (9·1%).
Discussion
In this population-based, cohort study using national renal surveillance data, 26% of incident ESRD patients with SCD as the primary cause of renal failure died within the first year of haemodialysis and mortality within the first year among this population was 2·8 times that of other patients with ESRD beginning haemodialysis during the same time period. Further, similar to other patients with ESRD, the risk of death among patients with SCD–ESRD was attenuated among those who received pre-dialysis nephrology care for a period of 6 or more months. Our finding that CKD among patients with SCD was associated with high mortality is consistent with previously reported evidence (Platt et al, 1994) and the increased risk of mortality associated with late referral to nephrology care is consistent with a number of recent reports for dialysis patients without SCD–ESRD (Bradbury et al, 2007; McClellan et al, 2009). In our study, patients with SCD–ESRD had higher mortality compared with other patients with ESRD despite their younger average age and the lower prevalence of specific comorbid conditions, such as DM and ASHD, that are associated with lower survival in the general dialysis population. These findings suggest that detection and appropriate, evidence-based management of CKD among individuals with SCD might reduce the 26% 1 year death rate following the start of haemodialysis reported here.
A previous study of SCD–ESRD utilizing United States Renal Data System data noted increased mortality over longer periods of follow-up among individuals with ESRD due to SCD (National Kidney Foundation, 2001a) However, although SCD patients were less likely to be placed on the renal transplant waiting list and to receive a transplant, controlling for transplantation status eliminated the increased risk of death among SCD haemodialysis patients. We were unable to account for transplantation status in the current analysis but, given the low rates of transplantation in individuals with SCD and the prolonged waiting times experienced by those on the transplant waiting list, we believe that transplantation status is unlikely to account for the patterns of early mortality that we observed.
While CKD might not be diagnosed until adulthood, evidence suggests that renal injury associated with SCD might start during infancy. A recent randomized, double-blinded, placebo-controlled trial (Ware et al, 2010) showed that, at baseline, infants with SCD demonstrated significant glomerular hyperfiltration. A study of an infant SCD cohort (Piepsz et al, 2006) found that the average baseline quantitative glomerular filtration rate measurement, determined by diethylenetriaminepentaacetic acid clearance, was 125 ml/min/1·73 m2 (range from 40·2 to 300·9 ml/min/1·73 m2), a value considerably higher than the published normal value of 91·5 ml/min/1·73 m2 (10–90% range from 60 to 120 ml/min/1·73 m2) for this age group. Another group reported that 4·2% of 725 individuals with SCD who were followed for 25 years developed renal failure and had a 40% higher risk of death during follow-up than their counterparts without renal failure (Powars et al, 1991). Further, the occurrence of renal insufficiency generally was evident by early adulthood (23 years). Thus, recommendations to improve outcomes for renal disease among individuals with SCD should start with the paediatric population and continue with practice guidelines addressing the transition of care from adolescence to adulthood. One possible reason that current clinical practice guidelines for CKD and ESRD lack specific recommendations for SCD care is the low incidence of the disease (Collins et al, 2009). However, despite the overall small proportion of patients with SCD, as the primary cause of ESRD, quality improvement activities targeted to this population are needed to improve outcomes.
Patients with SCD have complex medical problems that complicate both pre-ESRD care and renal replacement therapy. Unfortunately, we did not have data on the prevalence of pulmonary hypertension, and the incidence of pain or acute chest syndrome that have been associated with mortality among patients with SCD. We could not determine the extent to which the prevalence of these co-morbidities may contribute to the high mortality in this population. Nevertheless, early referral to a nephrologist may decrease the risk of death for SCD patients with CKD. Additional studies are needed to understand the relationships between early ESRD mortality and common complications experienced by patients with SCD. The applicability of existing guidelines for the early detection and management of kidney disease (National Kidney Foundation, 2001b, 2002) should be examined in relation to SCD. Further, given the strong relationship between ESRD and mortality in the first year following diagnosis of ESRD, future studies addressing other co-morbidities associated with risk of death in SCD, such as elevated triscuspid jet velocity, must either exclude or adjust for the presence of ESRD so results may be comparable from one study to the next.
Additional limitations to our study should be noted. First, others have demonstrated that there is misclassification of AVF status in data collected on the CMS–2728 form at the start of ESRD therapy (Piepsz et al, 2006). However, we believe this is unlikely as both the presence of an AVF and early pre-nephrology care data collected on the Form CMS–2728 are strong predictors of improved survival. If individuals with SCD were consistently misclassified with respect to these measures (i.e. absent when actually present and the converse) then we would expect an attenuation of the risks observed in our study. The misclassification is likely to be non-differential, resulting in an underestimate of the strength of the association; therefore, our finding of a strong association may be an underestimate. We were not able to demonstrate statistically significant relationships for all of our outcomes. It is probable that the lack of statistical significance was due to the small number of patients in our study with SCD–ESRD (n = 410). However, the magnitude and direction of our point estimates were consistent with a large body of literature on mortality in the ESRD population. Additionally, we were not able to confirm the diagnosis of SCD in the study sample. Thus, misclassification of patients with incident ESRD and SCD might have occurred. To limit misclassification, we restricted our analysis to patients with a diagnostic code of SCD as their primary cause of ESRD and excluded patients with SCD who had comorbid conditions, such as diabetes, leading to ESRD. Consequently, the prevalence of comorbid conditions among patients with ESRD who have SCD is probably understated. Most critically, the results cannot be generalized to the population of SCD with ESRD but only to those for whom SCD is the direct cause of ESRD.
Also, we used all-cause mortality in our analysis, as opposed to identifying the primary and secondary reasons for death. Such information might have strengthened the evidence that prior ESRD care among individuals with SCD–ESRD improved survival. However, all-cause mortality has been used as an outcome after a diagnosis of ESRD in previous mortality studies (Pastan et al, 2002; McClellan et al, 2009), which enables comparisons across studies. Despite these limitations, our results are consistent with previous evidence that haemodialysis survival rates are increased with adequate pre-ESRD care.
In summary, ESRD patients with SCD as the primary cause of renal failure have a high rate of premature death, particularly in the first 12 months after the diagnosis, which might be attenuated with timely referral to a nephrologist. Further improvement in outcomes might be achieved by the development of evidence-based guidelines that are specific to the population with SCD. Future studies to identify risk factors for death should include the presence of ESRD as a potential confounder. Clinicians caring for this vulnerable population of patients should recognize the importance of early detection and appropriate management of CKD associated with SCD.
Acknowledgements
The analyses upon which this publication is based were performed under Contract Number HHSM-500-2010-005C, entitled ‘End Stage Renal Disease Networks Organization Number 5”, sponsored by the Centers for Medicare and Medicaid Services (CMS), Department of Health and Human Services.” This article is a direct result of the Health Care Quality Improvement Program initiated by CMS, which has encouraged identification of quality improvement projects derived from analysis of patterns of care, and therefore required no special funding on the part of this contractor. This research was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention, Division of Blood Disorders administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. We thank Dr. Steven Embury and Mrs. Deborah Jones for reviewing and editing the manuscript.
Footnotes
Author Contributions
A.M., M.D., and R.K. designed and performed research, analysed data and wrote the paper. E.H. and W.M. designed research, analysed data and wrote the paper. J.C.L. performed research, analysed data and wrote the paper. J.L. designed and performed research and wrote the paper. M.S. contributed to writing the paper. A.G. analysed data and wrote the paper. D.G. designed research and wrote the paper.
References
- Bradbury BD, Fissell RB, Albert JM, Anthony MS, Critchlow CW, Pisoni RL, Port FK, Gillespie BW. Predictors of early mortality among incident US hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Clinical Journal of American Society of Nephrology. 2007;2:89–99. doi: 10.2215/CJN.01170905. [DOI] [PubMed] [Google Scholar]
- Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, Murray A, St Peter W, Guo H, Li Q, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Wang C, Wein handl E, Zaun D, Arko C, Chen SC, Dalleska F, Daniels F, Dunning S, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L. United States Renal Data System 2008 Annual Data Report. American Journal of Kidney Diseases. 2009;53:S1–S374. doi: 10.1053/j.ajkd.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Hassell KL. Population estimates of sickle cell disease in the U.S. American Journal of Preventive Medicine. 2010;38:S512–S521. doi: 10.1016/j.amepre.2009.12.022. [DOI] [PubMed] [Google Scholar]
- McClellan WM, Wasse H, McClellan AC, Kipp A, Waller LA, Rocco MV. Treatment center and geographic variability in pre-ESRD care associate with increased mortality. Journal of the American Society of Nephrology. 2009;20:1078–1085. doi: 10.1681/ASN.2008060624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Kidney Foundation III. NKF-K/DOQI Clinical Practice Guidelines for Vascular Access: update 2000. American Journal of Kidney Diseases. 2001a;37:S137–181. doi: 10.1016/s0272-6386(01)70007-8. [DOI] [PubMed] [Google Scholar]
- National Kidney Foundation IV. NKF-K/DOQI Clinical Practice Guidelines for Anemia of Chronic Kidney Disease: update 2000. American Journal of Kidney Diseases. 2001b;37:S182–238. doi: 10.1016/s0272-6386(01)70008-x. [DOI] [PubMed] [Google Scholar]
- National Kidney Foundation K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. American Journal of Kidney Diseases. 2002;39:S1–266. [PubMed] [Google Scholar]
- Pastan S, Soucie JM, McClellan WM. Vascular access and increased risk of death among hemodialysis patients. Kidney International. 2002;62:620–626. doi: 10.1046/j.1523-1755.2002.00460.x. [DOI] [PubMed] [Google Scholar]
- Piepsz A, Tondeur M, Ham H. Revisiting normal (51)Cr-ethylenediaminetetraacetic acid clearance values in children. European Journal of Nuclear Medicine and Molecular Training. 2006;33:1477–1482. doi: 10.1007/s00259-006-0179-2. [DOI] [PubMed] [Google Scholar]
- Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, Klug PP. Mortality in sickle cell disease. Life expectancy and risk factors for early death. New England Journal of Medicine. 1994;330:1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- Powars DR, Elliott-Mills DD, Chan L, Niland J, Hiti AL, Opas LM, Johnson C. Chronic renal failure in sickle cell disease: risk factors, clinical course, and mortality. Annals of Internal Medicine. 1991;115:614–620. doi: 10.7326/0003-4819-115-8-614. [DOI] [PubMed] [Google Scholar]
- Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115:3447–3452. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware RE, Rees RC, Sarnaik SA, Iyer RV, Alvarez OA, Casella JF, Shulkin BL, Shalaby-Rana E, Strife CF, Miller JH, Lane PA, Wang WC, Miller ST. Renal function in infants with sickle cell anemia: baseline data from the BABY HUG trial. Journal of Pediatrics. 2010;156:66–70 e1. doi: 10.1016/j.jpeds.2009.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]