Abstract
Introduction:
The Affordable Care Act increases health insurance options, yet many Americans may struggle to consistently maintain coverage. While health care providers have traditionally not been involved in providing insurance enrollment support to their patients, the ability for them to do so now exists. We propose that providers could capitalize on the expansion of electronic health records (EHRs) and the advances in health information exchanges (HIEs) to improve their patients’ insurance coverage rates and continuity.
Evidence for Argument:
We describe a project in which we are building strategies for linking, and thus improving synergy between, payer and EHR data. Through this effort, care teams will have access to new automated tools and increased EHR functionality designed to help them assist their patients in obtaining and maintaining health insurance coverage.
Suggestion for the Future:
The convergence of increasing EHR adoption, improving HIE functionality, and expanding insurance coverage options, creates new opportunities for clinics to help their patients obtain public health insurance. Harnessing this nascent ability to exchange information between payers and providers may improve synergies between HIE and EHRs, and thus support clinic-based efforts to keep patients continuously insured.
Keywords: access, health information technology, health policy, health information exchange
Introduction
Continuous health insurance has significant benefits,1–4 yet many patients eligible for Medicaid and other public plans have been unable to obtain or consistently retain coverage.5–7 The Affordable Care Act (ACA) increases health insurance options for millions of Americans, but many may still struggle to maintain coverage; for example, it is estimated that half of adults will experience a change in eligibility status within a year of gaining Medicaid.8 Health insurance coverage gaps might be prevented if patients had timely access to eligibility and reenrollment information. We propose that such information could be made available in electronic health records (EHRs) through automated exchanges of information about coverage, and used by care providers to help keep eligible patients continuously insured. To demonstrate this concept, we present an example from our work synergizing the exchange of health insurance information and EHRs to support patients’ Medicaid insurance maintenance.
An Opportunity to Improve Synergy Between Health Information Exchange and EHRs to Increase Continuous Insurance
Currently, most health insurance coverage information is contained in insurance payer data systems, and EHRs have, at best, limited linkages to these data. Usually their only interfaces are outbound messages: billing data sent from the EHR to the payer. Some EHRs import insurance status, generally limited to patient matching data (e.g., name, date of birth), binary coverage status (i.e., insured, not insured), and sometimes the name of the insurance plan and/or coverage “start date.” Despite recent advances in health information exchange (HIE) focused on interoperability of clinical systems,9–11 payer-EHR interfaces rarely exchange certain key information needed to enable point-of-care health insurance support. For example, health insurance “end date” data could be used in EHR tools that alert a social worker, care manager, clinic-based insurance specialist, and/or front desk staff to a patient’s potential upcoming insurance expiration date; such alerts would enhance clinics’ ability to assist patients in maintaining continuous coverage. An important opportunity now exists to improve HIE to better enable clinic insurance enrollment support, arising from the unique confluence of recent federal programs supporting the rapid evolution of health information technology (HIT) and changes in insurance systems and the health care ecosystem.12–16 This opportunity is timely, as 7.2 million new Medicaid enrollees, enrolled through the ACA, will need to verify eligibility every 6 to 12 months after enrollment.17
Evidence for Argument
To capitalize on expanding HIT capabilities and increased health insurance options, we partnered with eight community health centers (CHCs) that share an EHR through membership in the OCHIN community health information network (described elsewhere).18,19 Like most EHRs, payer and coverage status information is manually entered into the OCHIN EHR system; using external state portals, clinics can determine if a patient is insured by Medicaid on the appointment date (but not beyond that date). However, this information is not tracked or recorded over time. Coverage data may also come from the patient’s insurance card (if available), or from patient self-reports. Front desk staff do not confirm insurance status from these sources.
We conducted 95 hours of clinic observation and engaged 31 staff and 20 families from the OCHIN CHCs in interviews designed to identify their needs related to patient insurance data.20 A workflow redesign process identified gaps in the data that must be addressed to facilitate clinic-based insurance-enrollment support services. We then engaged six staff in user-centered design processes (wireframe prototyping, and “Think Aloud” usability testing21–24) to further develop and fine-tune suggested EHR enhancements and data tools for linking Medicaid and EHR data more closely. Our goal in linking these data sources was to increase the synergy between HIE and the CHCs’ EHR.
Through these processes, the CHC staff identified the following needs: patients’ health insurance “end date;” automated systems to identify patients eligible for coverage but not enrolled, or those nearing reenrollment; and a method to record and track attempts to help patients obtain or keep coverage. To address this need, we developed six strategies for increasing HIE between Medicaid coverage data and the OCHIN EHR. Table 1 lists these strategies and associated data tool prototypes, and provides examples of the CHC feedback that indicated the need for each. These strategies included creating workflows, both during and outside clinic visits, to assist patients with keeping their health insurance coverage up-to-date.
Table 1.
Tool Strategies Created with Quotes from Community Health Center (CHC) Staff about Need
| STRATEGY | QUOTE FROM CHC STAFF THAT DEMONSTRATES NEED |
|---|---|
| 1. Oregon’s Medicaid office sends OCHIN a monthly update of health insurance status data that are made available in the EHR. (Figure 1) | “if we could cut all of that and have the [EHR] system itself… interface with…the State [insurance data] somehow, then we would be able to know when a patient’s insurance was due to lapse.” |
| 2. A drop-down menu option under coverage verification to indicate insurance coverage may end soon. | “So I think it would be a good idea to know at least when it will expire. Or we can kind of give it a reminder to the patients: Don’t forget to apply. We can schedule you an appointment. That would be nice.” |
| 3. A message to alert front desk staff at check-in if the patient’s insurance coverage may end soon. (Figure 2) | “It will be nice [if] something pops out when you’re checking patients in.” |
| 4. A tracking form to capture data about insurance application status. | “Maybe what there should be is a flag for anybody that doesn’t have coverage. Oh look, doesn’t look like you put any coverage in for this person. Are you sure they don’t qualify? And then, you know, they could do the screening.” |
| 5. A report to identify clinicpatients with an appointment in the next 30 days and have lost or may soon lose coverage. (Figure 3) | “So it will be nice…something that we can see ahead of time, so that way we can call them. Or we can schedule the appointment with insurance specialist. We can try to help before they actually come in.” |
| 6. A report to identify the clinic’s uninsured patients, and those who may soon lose insurance. | “If we could have something that identified when this patient’s coverage is going to lapse, so that we can be proactive and get them an appointment with an insurance specialist and do all that stuff, that would be great.” |
Next Steps
Our team will use mixed methods to assess the feasibility of implementing these strategies and the effectiveness of doing so. Qualitative methods will determine the acceptability of the tools, CHC staff members’ experience with use of the tools, and how the tools fit into the clinics’ workflow processes. Quantitative methods will determine which tools are being used and how often. We will also assess children’s coverage continuity data in intervention versus control clinics before and after the study tools were implemented to test the hypothesis that children seen at CHCs that use the tools will have improved insurance coverage rates and fewer coverage gaps compared to children in other CHCs.
As shown in Table 2, most of the pediatric patients seen in the study CHCs have Medicaid coverage, but >20% are uninsured. Thus, developing tools and strategies to improve the health insurance coverage continuity of pediatric CHC patients has the potential to have a large impact at the study sites; if proven effective, the impact could be much greater if strategies are implemented in additional OCHIN network CHCs. As OCHIN has a track record of creating and rolling out customized EHR tools to its member clinics, if the tools prove effective and are perceived as useful we will make them available to all interested network CHCs. We will also provide clinics with recommendations for their use within clinic workflows. The tools could also be adapted as needed to meet changing practice and policy demands.
Table 2.
Child Health Insurance Type at OCHIN Community Health Centers (CHCs)
| MEDICAID % | UNINSURED % | COMMERCIAL COVERAGE % | |
|---|---|---|---|
| OCHIN network CHCs | 68.1 | 19.8 | 12.1 |
| OCHIN Oregon CHCs | 64.1 | 23.7 | 12.2 |
| Study site CHCs* | 73.1 | 21.4 | 5.5 |
Source: OCHIN Electronic Health Record Data
Note:
Average across study sites
Suggestions for the Future
We present one example of how synergizing nascent HIE and EHR capabilities could support clinics in helping patients obtain and maintain health insurance coverage. In this example, increasing the coverage information exchanged with an EHR, and building tools that capitalize on this increased HIE could help patients maximally benefit from recent expansions in health insurance access.26 Health impacts are likely: when patients maintain continuous coverage, they are more likely to receive essential healthcare services,1–4 whereas patients with even short lapses in coverage have higher rates of unmet healthcare needs.27,28 For providers and delivery systems with per-member-per-month reimbursement, or those in accountable care organizations, keeping all patient panel members insured helps support the provision of vital, evidence-based care, leading to improved patient outcomes.29 Further, preventing insurance lapses could decrease patients’ out-of-pocket expenses, and could stabilize clinics’ revenue streams. Thus, the strategies presented here,—and other efforts to improve synergy between HIEs and EHRs,—will help patients and providers access and use coverage data. The meaningful use and effective exchange of these data will be essential to achieving the healthcare Triple Aim: improved population health, better individual patient care, and lower cost.30
Although there are potential weaknesses in the design of any EHR-based tools, the overall concept presented here is sound and generalizable.12,31,32 However, in any such intervention, numerous assumptions must be met. The proposed strategies depend on access to payer data via an interface. Many patients experience frequent gaps in coverage6,7 or change health insurance plans frequently.8,33 Thus, interoperability with payer data systems—be they public or private—will be necessary, and payer data must be up-to-date and accurate. Patient-matching algorithms needed to link payer and EHR data are usually <90% effective,34 limiting the utility of linkage automation. Some EHRs may not be able to appropriately accept and store inbound data; this functionality could be improved in future EHR designs and standards. Once the data are in the EHR, workflows can fail; EHR pop-up alerts are often ignored.35 Such system improvements need dedicated staff time to help patients obtain and maintain insurance, but movement toward global payment models (e.g., per-member-per-month capitation) may make the investment worthwhile.
Conclusions
The convergence of increasing EHR adoption, improving HIE functionality, and expansions in health insurance coverage options creates new opportunities for clinics to help patients obtain and maintain public health insurance. This emergent ability to exchange health information between payers and providers must be harnessed to improve synergies between HIE and EHRs, in support of keeping patients continuously insured.
Figure 1.
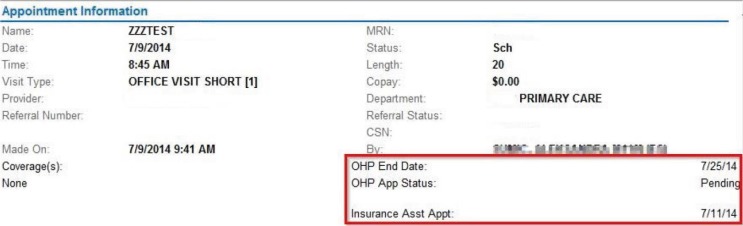
New Data Fields in the Appointment Information Box
Figure 2.
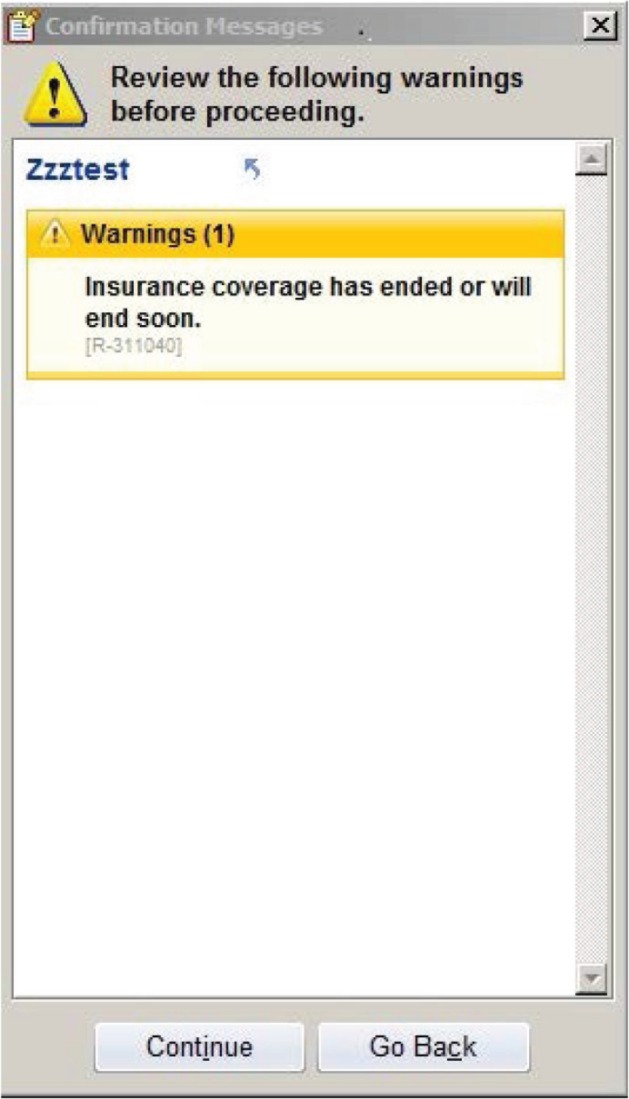
Expiration Warning That Pops Up When You Close the Registration Page of, Schedule an Appointment for, or Check in a Patient Whose Insurance May End Soon
Figure 3.
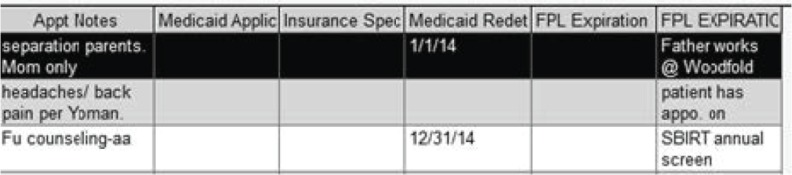
Detailed Report Created to Highlight Loss of Health Insurance in Aggregate
Note: © 2014 Epic Systems Corporation. Used with permission.
Acknowledgments
This work was financially supported by the Agency for Healthcare Research and Quality (AHRQ) grant number (1 R01 HS018569), the Patient-Centered Outcomes Research Institute (PCORI), National Cancer Institute (NCI) of the National Institutes of Health grant number (1 R01 CA181452 01), and the Oregon Health & Science University Department of Family Medicine.
Footnotes
Disciplines
Health Information Technology | Health Services Research | Primary Care
References
- 1.Cassedy A, Fairbrother G, Newacheck PW. The impact of insurance instability on children’s access, utilization, and satisfaction with health care. Ambulatory Pediatrics. 2008;8(5):321–8. doi: 10.1016/j.ambp.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Sudano JJ, Baker DW. Intermittent lack of health insurance coverage and use of preventive services. American Journal of Public Health. 2003;93(1):130–137. doi: 10.2105/ajph.93.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoffman C, Paradise J. Health insurance and access to health care in the United States. Ann N Y Acad Sci. 2008;1136:149–60. doi: 10.1196/annals.1425.007. [DOI] [PubMed] [Google Scholar]
- 4.Courtemanche CJ, Zapata D. Does universal coverage improve health? The Massachusetts experience. Journal of Policy Analysis & Management. 2014;33(1):36–69. doi: 10.1002/pam.21737. [DOI] [PubMed] [Google Scholar]
- 5.Sommers BD. Why millions of children eligible for Medicaid and SCHIP are uninsured: poor retention versus poor take-up. Health Affairs. 2007;26(5):w560–w567. doi: 10.1377/hlthaff.26.5.w560. [DOI] [PubMed] [Google Scholar]
- 6.Short PF, Graefe DR, Schoen C. In: Churn, Churn, Churn: How Instability of Health Insurance Shapes America’s Uninsured Problem. Fund TC, editor. 2003. [PubMed] [Google Scholar]
- 7.Fairbrother G, et al. Churning in Medicaid managed care and its effect on accountability. Journal of Health Care for the Poor & Underserved. 2004;15(1):30–41. doi: 10.1353/hpu.2004.0003. [DOI] [PubMed] [Google Scholar]
- 8.Sommers BD, Rosenbaum S. Issues In Health Reform: How Changes In Eligibility May Move Millions Back And Forth Between Medicaid And Insurance Exchanges. Health Affairs. 2011;230(2):228–236. doi: 10.1377/hlthaff.2010.1000. [DOI] [PubMed] [Google Scholar]
- 9. HealthIT.gov Health Information Exchange (HIE): What is HIE? 2014. [cited 2014 February 20]; Available from: http://healthit.gov/providers-professionals/health-information-exchange/what-hie.
- 10.Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. J Am Med Inform Assoc. 2010;17(3):288–94. doi: 10.1136/jamia.2010.003673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011;18(5):678–82. doi: 10.1136/amiajnl-2010-000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rudin RS, Bates DW. Let the left hand know what the right is doing: a vision for care coordination and electronic health records. J Am Med Inform Assoc. 2014;21(1):13–6. doi: 10.1136/amiajnl-2013-001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiner JP, Yeh S, Blumenthal D. The impact of health information technology and e-health on the future demand for physician services. Health Affairs. 2013;32(11):1998–2004. doi: 10.1377/hlthaff.2013.0680. [DOI] [PubMed] [Google Scholar]
- 14.Blumenthal D. Implementation of the federal health information technology initiative. N Engl J Med. 2011;365(25):2426–31. doi: 10.1056/NEJMsr1112158. [DOI] [PubMed] [Google Scholar]
- 15.Shaffer ER. The affordable care act: the value of systemic disruption. American Journal of Public Health. 2013;103(6):969–72. doi: 10.2105/AJPH.2012.301180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buntin MB, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Affairs. 2011;30(3):464–71. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- 17.Medicaid and CHIP Medicaid/CHIP Renewal: Opportunities, Strategies and Considerations. SOTA All State Call. 2014 [Google Scholar]
- 18.Devoe JE, Sears A. The OCHIN community information network: bringing together community health centers, information technology, and data to support a patient-centered medical village. Journal of the American Board of Family Medicine. 2013;26(3):271–8. doi: 10.3122/jabfm.2013.03.120234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeVoe JE, et al. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-based Research Network (SNW-PBRN) Journal of the American Board of Family Medicine. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeVoe JE, et al. Use of Qualitative Methods and User-Centered Design to Develop Customized Health Information Technology Tools Within Federally Qualified Health Centers to Keep Children Insured. Journal of Ambulatory Care Management. 2014;37(2):148–154. doi: 10.1097/JAC.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 21.Jaspers MW. A comparison of usability methods for testing interactive health technologies: methodological aspects and empirical evidence. Int J Med Inform. 2009;78(5):340–53. doi: 10.1016/j.ijmedinf.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Kushniruk AW, Patel VL. Cognitive and usability engineering methods for the evaluation of clinical information systems. J Biomed Inform. 2004;37(1):56–76. doi: 10.1016/j.jbi.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Jaspers MW, et al. The think aloud method: a guide to user interface design. Int J Med Inform. 2004;73(11–12):81–95. doi: 10.1016/j.ijmedinf.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Johnson CM, Johnson TR, Zhang J. A user-centered framework for redesigning health care interfaces. J Biomed Inform. 2005;38(1):75–87. doi: 10.1016/j.jbi.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Likumahuwa S, et al. IMPACCT Kids’ Care: a real-world example of stakeholder involvement in comparative effectiveness research. Journal of Comparative Effectiveness Research. in press. [DOI] [PMC free article] [PubMed]
- 26.Shoen C, et al. Affordable Care Act Reforms Could Reduce The Number Of Uninsured US Adults By 70 Percent. Health Affairs. 2011;30(9):1762–1771. doi: 10.1377/hlthaff.2011.0335. [DOI] [PubMed] [Google Scholar]
- 27.Olson LM, Tang S-fS, Newacheck PW. Children in the United States with Discontinuous Health Insurance Coverage. N Engl J Med. 2005;353(4):382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- 28.Gold R, et al. Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage. J Am Board Fam Med. 2012;25(1):42–9. doi: 10.3122/jabfm.2012.01.110142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fromer L. Implementing chronic care for COPD: planned visits, care coordination, and patient empowerment for improved outcomes. Int J Chron Obstruct Pulmon Dis. 2011;6:605–614. doi: 10.2147/COPD.S24692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affairs. 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 31.Lassetter JK. Building a solid infrastructure for ACOs. Use an HIE to leverage existing information systems. Health Manag Technol. 2011;32(1):32. [PubMed] [Google Scholar]
- 32.HRSA Meaningful Use and Care Coordination. Health Information Technology and Quality Improvement. 2014. [cited 2014 January 7]; Available from: http://www.hrsa.gov/healthit/toolbox/HealthITAdoptiontoolbox/MeaningfulUse/meaningfuluseandcarecoord.html.
- 33.Hwang A, Rosenbaum S, Sommers BD. Creation of state basic health programs would lead to 4 percent fewer people churning between Medicaid and exchanges. Health Affairs. 2012;31(6):1314–20. doi: 10.1377/hlthaff.2011.0986. [DOI] [PubMed] [Google Scholar]
- 34.Wang X, Ling J. Multiple valued logic approach for matching patient records in multiple databases. Journal of Biomedical Informatics. 2012;45(2):224–230. doi: 10.1016/j.jbi.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 35.Van der Sijs H, et al. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;13(2):138–47. doi: 10.1197/jamia.M1809. [DOI] [PMC free article] [PubMed] [Google Scholar]


