INTRODUCTION
Child and adolescent mental health (CAMH) problems are largely neglected in the wider realm of global public health, and this lack of attention has implications for young people's health, well-being, and longevity. The World Health Organization (WHO) estimates that more than 800,000 people committed suicide in 2012. Suicide is the second leading killer of people aged 15 to 29 years,1 and in regions of the world where targeted interventions have successfully reduced rates of maternal mortality, it is the leading killer of young women aged 15 to 19 years.2 Within countries, suicide rates differ among subpopulations, and young people in some communities are distinctly vulnerable. A regional analysis of suicide from 1999 to 2009 among Alaska Native and American Indian populations showed particularly high rates among Alaska Native communities and suicide rate among people younger than 44 years was 5 times the suicide rate of White Americans in the United States.3 In Nunavut, the northernmost territory of Canada, around 65% of suicides among the Inuit population between 1999 and 2014 occurred among people aged 10 to 24 years.4
Evidence-based interventions implemented through regional, national, and global suicide prevention plans provide one example of how health systems can use data to generate strategies for control and to stimulate policy responses from decision makers. The WHO's Comprehensive Mental Health Action Plan 2013–2020 sets a global target of 10% reduction in suicides by 2020 across member states and calls for strengthened information systems, evidence, and research on mental health.5 In the United States, the Prioritized Research Agenda for Suicide Prevention calls for a 20% reduction in suicides over the next 5 years and 40% reduction over the next 10 years.6 The investigators note, “A research document alone cannot reduce suicide deaths or attempts; rather, its intent is to identify the research needed to guide practice and inform policy decisions across many areas.”6
These efforts call attention to the role that research can play in supporting and stimulating a public health agenda. Research provides the evidence base for successful interventions, data for monitoring progress, and, over the long run, makes solutions available to complex problems. Globally, research is needed to spur public health action to reduce the mortality and morbidity associated with poor mental health in childhood and adolescence. Children, adolescents, and youth represent more than one-third of the world's population. In 2010, 35.4% of the world's population was aged between 0 and 19 years and 44.3% was aged between 0 and 24 years.7 In the least developed countries, these populations represent 51.6% and 60.8% of the total population, respectively.
Most mental and substance use disorders begin during childhood and adolescence,8 with 75% of cases beginning before the age of 25 years in the United States.9 Developmental disabilities, conduct disorder, attention deficit-hyperactivity disorder, anxiety, and depression confer the greatest burden of disease for children younger than 10 years10; these are disabling disorders of youth across continents with vastly different health profiles and remain the leading causes for disability worldwide.11 At the same time, the periods of infancy, childhood, and adolescence represent opportune times for interventions to reduce risk for mental disorders and enhance social, emotional, and cognitive functioning.12 Researchers seeking to understand developmental trajectories of brain development and their relationship to mental disorders increasingly view these disorders as neurodevelopmental.13 Researchers are exploring how changes in neural architecture correspond to developmental stages and respond to contextual and environmental exposures.12 This work opens the door to better understanding risk and protective factors and to the development of effective multilevel interventions.
Optimizing this research enterprise to ensure global representation has been challenging. The 10/90 research gap, which refers to the inequity in distribution of research investments and activities, highlighted 20 years ago by the Commission on Health Research for Development,14 is particularly striking in the area of child mental health. Although 90% of the world's children live in developing countries, only 10% of randomized controlled trials testing mental health interventions for children occurred in LMICs.15 Even fewer studies address psychosocial and combined interventions for children's mental health problems.15 Nevertheless, a key function (and challenge) for health systems everywhere is the use of research findings and implementation of research-based interventions for CAMH in routine practice.16 For these reasons, research is an integral part of the global health system.17 Developing an agenda and the associated priorities lead this process, followed by financing and resource allocation, research and development, implementation and delivery of services, as well as monitoring and evaluation, while ensuring that means for learning from the knowledge gained are built into the process.17,18
In this article, the authors use selected findings from a recent research priority-setting exercise, the Grand Challenges in Global Mental Health, to organize the presentation of priorities for global CAMH research and public health action. The initiative articulates a set of challenges with particular relevance to children and adolescents that, if addressed in a coordinated manner, have the potential to improve outcomes in early child development (ECD) and mental health. For each challenge, the authors describe existing research-informed initiatives with national and global reach that can contribute to solving the challenges, and they also discuss the research capacity building needed to undertake these challenges.
RESEARCH PRIORITY SETTING FOR GLOBAL MENTAL HEALTH
Over the past decade, Grand Challenge initiatives focused on global health priorities have mobilized global cooperation, resource allocation, and research in efforts to solve intractable problems.19,20 In 2010, the National Institute of Mental Health and partners, including the Global Alliance for Chronic Disease, launched the Grand Challenges in Global Mental Health.21 The initiative convened more than 400 researchers, clinicians, and advocates from 60 countries to identify priorities for research that, if addressed, could make an impact on the lives of people with mental, neurologic, and substance use disorders worldwide.
Unlike previous priority-setting exercises,22–24 the initiative identified challenges for HICs and LMICs and focused on mental, neurologic, and substance use disorders. Three rounds of a Delphi procedure, a structured consensus-building process, yielded 40 challenges. The top 25 challenges were categorized across 6 goals that spanned the range of science—from discovery research to policy research.21 In addition, the following 4 cross-cutting themes emerged from the data:
Researchers and decision makers must adopt a life course approach to carry out research and action on these issues.
Approaches to mental, neurological, and substance use (MNS) disorders cannot solely be addressed within siloed health care, but must be addressed across the health system and across sectors.
Interventions must be evidence based.
Context matters—the impact of environmental exposures and experience on risk, resilience, and interventions should be understood.
The authors focus on 5 challenges relevant to CAMH that are associated with Goal B: Advance prevention and implementation of early interventions (Box 1).
Box 1 Grand challenge goal B: advance prevention and implementation of early interventions.
Challenge 1: Support community environments that promote physical and mental well-being throughout life
Challenge 2: Develop interventions to reduce the long-term negative impact of low childhood socioeconomic status on cognitive ability and mental health
Challenge 3: Develop locally appropriate strategies to eliminate childhood abuse and enhance child protection
Challenge 4: Develop an evidence-based set of primary prevention interventions for a range of mental, neurologic, and substance use disorders
Challenge 5: Reduce the duration of untreated illness by developing culturally sensitive early interventions across settings
Adapted from Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health.
Nature 2011;475:27–30
Challenge 1: Support Community Environments that Promote Physical and Mental Well-Being Throughout Life
Scientific discussions of the interplay between biological factors (nature) and environmental factors (nurture) have been going on for centuries.25 Multiple levels of environmental exposures affect child development and well-being, including intrauterine exposures and the postnatal and early life influences of nutrition, infectious disease, and exposure to toxic agents.26–28 Socioeconomic status also drives exposure to risk and protective factors that have a significant impact on children's physical, social, and cognitive development.29–32 Neighborhoods, usually a function of socioeconomic status, matter, too. Concentrated disadvantage in wealthy countries is associated with violence, depression, and increased mortality.33 An urban US study among 5- to 11-year-old children demonstrated increasing prevalence of mental health problems across neighborhoods with increasing levels of poverty. Collective efficacy, a neighborhood social process the researchers measured, was associated with better mental health outcomes and mediated the effects of concentrated disadvantage.34
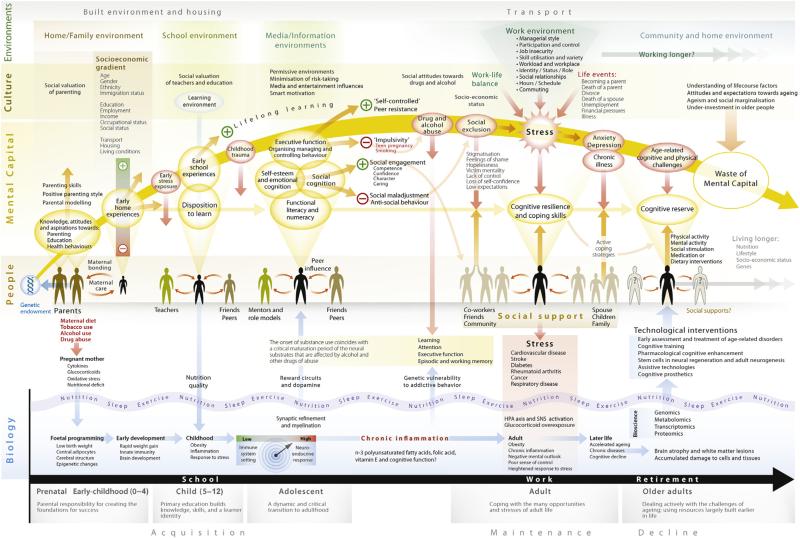
Research findings such as these have the potential to inform public health policy and practice. The UK Government Office for Science sponsored a nationwide research program to examine the contextual exposures that influence well-being over the life course: the Foresight Project on Mental Capital and Wellbeing.35,36 The project organizers convened a multidisciplinary group of investigators and policy makers in order to provide recommendations to the government on how best to achieve mental well-being, develop mental capital, and ultimately create a flourishing society in the United Kingdom over the next 20 years. They defined mental development in terms of mental capital and mental well-being. Mental capital represents cognitive and emotional resources (cognitive ability, flexibility and efficiency at learning, emotional intelligence, and social skills), and mental well-being refers to an individual's ability to develop his or her potential, work productively, and creatively build strong and positive relationships with others and contribute to the community.35 Adopting a life course approach, the organizers outlined biological, relational, cultural, and environmental exposures across the developmental trajectory that increase the risk for poor mental and physical health outcomes and enhance mental capital and well-being. (Fig. 1) depicts these interactions over the life span. Perhaps most importantly, the project poses questions relevant to implementation—“to what extent should policy choices take account of mental capital and well-being”—and highlights existing government initiatives informed by the project's synthesis.36
Fig. 1.
Positive and negative influences on mental capital and mental well-being over the life course. (From Foresight Mental Capital and Wellbeing Project. Final project report: executive summary. London: The Government Office for Science; 2008. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/292453/mental-capital-wellbeing-summary.pdf.)
Challenge 2: Develop Interventions to Reduce the Long-Term Negative Impact of Low Childhood Socioeconomic Status on Cognitive Ability and Mental Health
Experiences and genes build the neural architecture of the developing brain.12 Cognitive, emotional, physical, and social health potential emerges from the complex integrative processes of the brain as it continuously interacts with the social and environmental context.12 Poverty is associated with reduced access to basic services, poor sanitation and associated risks for infection, and undernutrition—factors that adversely affect growth and neurodevelopment, cognition, and mental health. Not surprisingly, people living in poverty disproportionately experience mental disorders and their sequelae.37,38 Although the number of people living in extreme poverty decreased from 1.9 billion in 1990 to 1.2 billion in 2010,39 children younger than 13 years are among the poorest population group in developing countries.40 These children constitute 34% of those living in extreme poverty, and they make up 50% of the poor in low-income countries.40
In 2012, a United Nations study showed that 1 in 7 children younger than 5 years, or approximately 99 million worldwide, were underweight for age.39 Although on the decline in most regions of the world, 1 in 4 children in the world—an estimated 162 million—are stunted and thus at risk for impaired cognitive and physical development and related consequences such as poor school performance.39,41 In one analysis, for every 10% increase in stunting, the proportion of children reaching the final grade of primary school dropped by 7.9%.41
Several international efforts are underway to use the current state of the evidence on ECD to move health systems, governments, and funders to appropriate implementation of health and social interventions. In 2013, United Nations Children's Fund published the Handbook of Early Child Development Research and its Impact on Global Policy, a text that synthesizes research evidence that these major threats—poverty, conflict, and disease—endanger children's chances of achieving their potential. The Institute of Medicine (IOM) launched a forum in 2014, Investing in Young Children Globally, which will convene key stakeholders from LMICs and HICs over 3 years to “translate evidence into sound and strategic investments in policies and practices” for the benefit of children and families.42 The World Bank has translated the evidence for investing in ECD into a free e-learning format so that decision makers can educate themselves about ECD, prioritize needs for their settings, and finance, implement, and monitor intersectoral interventions.43
Challenge 3: Develop Locally Appropriate Strategies to Eliminate Childhood Abuse and Enhance Child Protection
An estimated 681,000 children in the United States were victims of abuse and neglect in 2011,44 and the United States is not alone. Violence inflicted on children and youth occurs in various forms and can be deadly. Around the world, approximately 95,000 people younger than 20 years died of homicides in 2012.45 Globally, about 120 million girls experience some form of coerced sex at least once in their lifetimes.45 Inadequate social protections and social norms that condone some forms of violence collude to keep children at risk.45 Child abuse has long-term effects that include elevated risk of drug and alcohol abuse, sexual risk-taking behaviors, perpetuation of violence in subsequent generations, and poor educational outcomes.46 Despite the global nature of violence against children, only 1 prevention study from LMICs was published between 1995 and 2011.46 The authors present examples of intervention components and study findings in Table 1. Effective evidence-based interventions to reduce child abuse have long existed,47 but access to such interventions is not universal.
Table 1.
Summary of selected findings for mental disorder prevention and mental health promotion interventions
| Intervention Category | Intervention Components | Exemplary Outcome Measures (List) | Global Distribution of Research (Yes or No) | Main Findings | Research Gaps |
|---|---|---|---|---|---|
| Child abuse prevention | ECHV (provide support, education, improve child health & caregiving) PE (provide education, improve child-rearing skills) School-based CSA programs (education) MCT (family support, parenting skills, preschool education) |
Child maltreatment (hospital visits, parental report, referrals to protective services) Parenting skills Parental employment & reliance on social services |
No 0.6% of research from LMICs Reviewed in Skeen and Tomlinson,46 2013 and Mikton and Butchart,89 2009 |
ECHV: reduced risk factors for child maltreatment Only clear evidence of reduced actual maltreatment: Nurse-family partnership (USA) PE: some small to medium effects for reduction in risk factors and actual maltreatment, others only on reduced risk factors CSA: mixed—increased knowledge, no clear evidence of reduced abuse MCT: moderate effects in some studies, mixed evidence regarding reduction of risk factors in others |
Improve methodological quality in HIC studies (use of control groups, internal validity, randomized controlled designs) Overall prevention interventions in LMICs |
| Early childhood education | Parent training: 1.Improving parenting practices (eg, increased sensitive responsive interactions and early stimulation) 2.Emotional support for parents Center based: 1. Training teachers/caregivers in behavior management and greater social, emotional, and coping skills |
Observation of child behavior Assessment of child attachment Assessment of child mental health Assessment of caregiver practices (eg, measures of parenting) Assessment of caregiver mental health |
Yes Reviewed in Baker-Henningham,90 2014 |
Overall improvements in child mental health outcomes, and behavioral outcomes (both in short term [12/16 studies] and long term [6/6 studies]) Benefits in caregiver practices (21/25 studies) and caregiver mental health (6/9 studies) |
Need more long-term follow-up studies Discern optimal timing and duration Assess benefit to other children in the family Effect of booster interventions during later part of childhood |
| Mental health promotion interventions | Cognitive behavioral frameworks to structure building socioemotional skills, problem solving, and increased positive behaviors Physical, reproductive, and psychological health education Stress reduction techniques |
Emotional and behavioral well-being (eg, self-esteem, self-efficacy, coping skills, prosocial behaviors) Mental health assessment (anxiety, depression, PTSD, anger, hyperactivity symptoms) |
Yes Reviewed in Barry et al,70 2013 |
Positive effects for children living in conflict areas Mixed results in other interventions with differential gender and age group effects Positive effects in life skill and resilience-building programs |
Discern optimal components of intervention (age, individual/group, timing, duration) Need more research in low-income countries and in younger age groups (5-10 y) Assess cost-effectiveness |
| School-based mental health interventions | Health promotion: see mental health promotion intervention components and outcome measures described above Prevention and treatment (can be universal, selective and indicated): Cognitive behavioral techniques Creative arts and relaxation techniques Multimodal (including family and community components) |
Health promotion: see mental health promotion intervention components and outcomes described above Prevention and treatment: mental health assessment (anxiety, depression, PTSD, anger, hyperactivity symptoms) |
Yes Reviewed in Barry et al,70 2013 and Fazel et al,69 2014 |
In LMICs: most positive effects on PTSD symptoms Mixed effects on depression, grief, behaviors, and conduct symptoms Differential sex effects as well as differential effects depending on symptom severity |
Discern optimal components of intervention Develop outcome measures that integrate mental health and academic outcomes Assessment fidelity of interventions Need more long-term follow-up studies |
| Early intervention for psychosis | Prodromal symptoms: CBT Specialized teama Medications Omega-3 fatty acids Transition to psychosis: CBT vs supportive counseling Omega-3 fatty acids Improving outcome of first-episode psychosis: Medications CBT Family therapy Specialized team Vocational training |
Transition to psychosis Adherence to treatment Number of hospitalizations and number of days hospitalized Living independently Working or studying |
No (1 study in China, the rest in HICs) Reviewed in Marshal and Rathbone,92 2011; Stafford et al,93 2013 |
Prodromal symptoms: No effects of antipsychotics or CBT alone. Short-term effects of combination of all 3 over specialized team alone. Not sustained at 1 year Possible benefit of Omega-3 fatty acids Reduced transition to psychosis: Moderate-quality evidence in favor of CBT vs supportive counseling Low-quality evidence in favor of omega-3 fatty acids vs placebo Improving outcome of first-episode psychosis: Some support for vocational training and family therapy in addition to medications |
Rigorous randomized controlled trials Studies in LMICs Improved characterization of the role of a specialized team and the intervention components |
Abbreviations: CBT, cognitive behavioral therapy; CSA, child sexual abuse; ECHV, early childhood home visitation; MCT, multicomponent; PE, parent education; PTSD, posttraumatic stress disorder.
Specialized team is a multidisciplinary psychiatric team specializing in the treatment of patients with first-episode psychosis.
In response to these challenges, the United States Agency for International Development convened an Evidence Summit in 2011 to assess the available research that could inform strategies for policies and programs supporting child protection in LMIC. The Action Plan on Children in Adversity emerged from this process as a means of integrating sound practices into development initiatives.48 The plan uses existing evidence to promote strategies that support child development, prevent family separation, and promote safe and permanent family care, and to protect children from violence and abuse. The implementation of the plan calls for interagency collaboration within the US government as well as in the collaborating countries, which will aim to achieve progress toward these goals by 2017. At the same time, the US Centers for Disease Control and Prevention's Violence Against Children Survey permits countries supported by the President's Emergency Plan for AIDS Relief (PEPFAR) to measure the prevalence of violence as a first step toward applying remedies.
Challenge 4: Develop an Evidence-Based Set of Primary Prevention Interventions for a Range of Mental, Neurologic, and Substance Use Disorders
Understanding the multiple causes of mental disorders and developing effective interventions to prevent them remain grand challenges. Existing prevention interventions typically focus on a specific disorder and can be classified as universal (targeting the entire eligible population), selective (targeting a population at risk for illness), or indicated (targeting a population with subthreshold symptoms of disease).49 The IOM and National Research Council's 2009 report, Preventing Mental, Emotional and Behavioral Disorders in Young People, synthesizes the evidence for prevention and encourages an expanded focus that moves beyond preventing illness to include promoting wellness, collaborating between neuroscience and prevention science, using an interagency approach, being responsive to community priorities, focusing on dissemination and implementation research, including cost analyses, and concurrent screening and intervention activities.50
Although sometimes overshadowed by treatment-focused research, the global evidence base for preventive interventions for mental disorders is varied and expanding.15,51–53 Most intervention studies come from HICs and are disease focused, targeting common mental disorders in childhood such as depression,54–56 anxiety,57–60 conduct disorder,61–64 and substance abuse.65–68 A few of these are universal, whereas the majority have been conducted in high-risk populations. The settings for the interventions range from schools/preschools, homes, and clinics and are delivered by a range of providers: teachers, clinicians, parents, and community leaders. The duration of the interventions vary, as do the delivery (individual vs group) and the intervention content. Many use cognitive behavioral frameworks, social skills training, and parent training. Some interventions target youth directly, and others focus on parents and primary caregivers. Recent systematic reviews on the effectiveness of mental health promotion interventions in youth in LMICs found good evidence for the effectiveness of selected interventions to reduce anxiety and depressive symptoms and enhance self-esteem, self-efficacy, and motivation in youth69,70 (see Table 1). Schools emerged as an important context for interventions focused on children affected by conflict, but a sizable number of interventions had no effect.
Although more research is needed to clarify targets for preventive interventions, existing effective interventions merit attention for scaling up. One of the 4 objectives of the WHO Comprehensive Mental Health Action Plan 2013–2020 is to “implement strategies for prevention and promotion in mental health.” The World Health Assembly adopted the plan in 2013, and the plan, with its accompanying resolution, was an assertion of commitment from WHO's 194 member states to achieve the plan's objectives.71
Challenge 5: Reduce the Duration of Untreated Illness by Developing Culturally Sensitive Early Interventions Across Settings
Psychotic disorders may be among the most widely recognized mental illnesses worldwide, and they frequently begin in adolescence. A significant body of mental health research on the duration of untreated illness focuses on these disorders. Data from HICs suggest, however, that psychotic symptoms, per se, are not uncommon, occurring in 4% to 8% of the general population, and the prevalence may be higher among children and adolescents.72 A community study of youth aged 14 to 29 years from Kenya reported that 45% of the sample endorsed at least 1 psychotic risk symptom.73 These experiences do not necessarily predict the onset of a psychotic disorder; rather, they are apt to be indicators of risk for a variety of mental disorders (including depression, bipolar disorder, and sometimes schizophrenia). Even when psychotic symptoms do represent a prodrome for psychotic disorders (usually schizophrenia spectrum disorders), approximately 18% to 36% of people defined as high risk go on to transition to a mental disorder, with the risk of transition increasing over time.72 Once the transition occurs, a minority of patients achieve recovery, and a longer duration of untreated psychosis (DUP) is associated with greater morbidity. Identifying who is at risk to transition to a psychotic disorder, and intervening early, remains a critical area for investigation. Efforts to harmonize data across research sites in HICs enrich these research activities, but questions remain about the validity of commonly used measures to assess those who may be at high risk for psychosis in low-income country settings73 (see Table 1).
Among those who do develop a psychotic disorder, the DUP is associated with more severe symptoms, decreased remission rates, poor social functioning, and poorer overall functioning and quality of life among individuals in HIC and LMIC.74–76 The mean duration of untreated illness differs significantly between HICs and LMICs with almost double the duration in the latter.77 A recent UK study showed higher DUP among adolescents, and within that group, Asians had the lowest DUP, followed by black participants, and then white adolescents.78 Studies in Indonesia79 and China80 have reported increased mortality associated with prolonged duration of untreated illness. In these examples, the lack of available mental health services likely contributes to the chronicity and morbidity associated with psychotic disorders. The WHO Comprehensive Mental Health Action Plan 2013–2020 identifies a 20% increase in service coverage for severe mental disorders by 2020 as a target,5 but identifying and integrating evidence-based interventions for the prevention of psychosis into these services will require additional research.
BUILDING RESEARCH CAPACITY
Meeting the grand challenges relevant to CAMH requires a skilled global, collaborative, multidisciplinary research workforce with the capacity to translate research findings to practice settings in health, education, and other relevant sectors. Although several training programs in global mental health have emerged over the past 5 years, developing and sustaining a global cadre of CAMH researchers will require that several interacting factors be addressed.18 Countries must provide training and capacity-building opportunities for the development of skills in the basic, translational, and implementation sciences; the necessary research infrastructure; adequate financial resources; and environments that facilitate the conduct of research in order to address research priorities.18 In LMICs, the dearth of mental health clinical providers contributes to limited mental health research activity, as do the lack of graduate programs and the pressing need for clinical service providers to devote their energies to patient care.81
Other barriers curtail traditional research career trajectories. Once trained, new researchers must be mentored and retained. In LMICs, clinical and teaching responsibilities limit the available time to conduct research and clinical faculty seldom receive salaries to conduct research.18 The brain drain, that is, the loss of an already limited skilled workforce to higher resourced organizations or countries, demands innovative retention efforts. When trainees from LMICs receive research training in HICs, sufficient infrastructure must exist in the home institution in order to make returning worthwhile. Initiatives such as the Medical Education Partnership Initiative (MEPI), funded by the US National Institutes of Health and the President's Emergency Plan for AIDS Relief (PEPFAR), address some of these concerns. MEPI aims to enhance medical education so that health systems function effectively to deliver services in countries supported by PEPFAR. The initiative's specific aims are to build clinical capacity, retain clinicians, and stimulate and support contextually relevant research by building research capacity.82 MEPI provides funds to extend and reform clinical training approaches in 12 African countries, while also exposing students and trainees to research opportunities.82
MEPI programs in Kenya and Zimbabwe provide mental health research training opportunities, specifically linked to larger medical education efforts. The University of Zimbabwe's initiative, Improving Mental Health Education and Research capacity in Zimbabwe offered scholarships to develop new academic psychiatrists, master classes taught by international experts in child psychiatry and other underrepresented areas of training, and research training and mentoring opportunities.83 Among the lessons learned, the team noted the importance of building clinical service training and research experiences around needs in the local context. Mentorship by external experts was valued and best accomplished through teamwork and skills transfer in person with continuity through electronic communications. The program experienced a 4-fold increase in psychiatry faculty over 4 years and witnessed growth in its postgraduate training program.
Mentorship plays an important role in faculty development and success in every setting. Mentors guide trainees or junior faculty to resources and model skills not formally taught (eg, time management, perseverance).18 Mentors provide the “road-map of a research career and help to correct naïve assumptions” and assist with informed decision making about alternate career paths.18,84 Here again, the limited number of researchers in mental health, globally, also limits the number of available mentors. The challenge of finding a mentor is not restricted to LMICs; early career researchers in North America also face the small number of North American researchers focused on global mental health themes. Existing faculty must carve out time for mentorship amid competing priorities. In both high-income and low-income settings, up and coming researchers can experience isolation because of the dearth of investigators with shared or overlapping interests.18
Are there incentives for mentorship in LMIC academic institutions? Many of these institutions face challenges analogous to those faced by non–research-intensive institutions in the United States, where heavy teaching or administrative responsibilities compete with opportunities for research. Collins and colleagues18 note that in institutions without a culture of research or a strong research infrastructure, the senior faculty expected to mentor students and the junior faculty may not have received adequate training in research methods and grant writing or may not have strong publication records. Partnering with research-intensive institutions or experienced teams can help solve this problem. The National Institute of Mental Health-supported Collaborative Hubs for International Research on Mental Health provide one such example (http://www.nimh.nih.gov/about/organization/od/globalhubs/index.shtml). These 5 collaborative research teams conduct research aimed at reducing the mental health treatment gap in LMICs. Each funded hub consists of collaborating teams from 4 or more countries in a given region; they serve as regional resources for research training opportunities that occur through short courses, research mentorship, and on-the-job training for research assistants and coordinators.
Research partnerships also provide opportunities for researchers to develop skills for equitable collaboration. In the context of collaboration, teams confront the realities of differential resource distribution in the form of salaries, expertise, access to funding, and research human resources. How will these differences influence relationships across teams? How will pressures related to career maintenance, funding acquisition, advancement, and promotion among HIC investigators influence decision making? Will collaborations result in the development of new research leaders among the teams with fewer resources? Such teams are more frequently represented among LMIC organizations or institutions in HICs that are less research intensive.
Researchers working across cultural and economic contexts also confront the need for careful attention to ethical research practices. Research with children and other vulnerable populations—often made more vulnerable in the context of poverty—requires oversight by ethics committees or institutional review boards. As researchers obtain informed consent for research participation, they will need to understand and be sensitive to decision-making processes in the local context and meanings of privacy and confidentiality.85 Ruiz-Casares85 recommends that research teams “create safe spaces for reflection and dialogue on the scientific and ethical principles relevant to mental health research and the cultural, social, and other factors that may facilitate or hinder the conditions under study.”
Skills for ethical and equitable collaboration can also be operationalized through learning to prepare and disseminate research findings. Kohrt and colleagues86 outline procedures for collaborative writing that results in equitable representation of collaborators from LMICs on academic publications. The investigators observe that a key component involves “distributing lead authorship for different outputs at the same time as having mechanisms in place (eg, mentoring, workshops, coursework) to develop skills needed to adequately perform the role of lead author.”
In addition to writing skills for academic publications, global mental health research teams can benefit from learning to translate and disseminate research findings to local stakeholders and decision makers. The diversity of member roles on collaborative research teams, which likely include clinicians and other practitioners (eg, teachers, peers, lay health workers) as well as other community members, is a distinct advantage. Building research capacity affords opportunities to train nontraditional researchers in research methods. Teams can craft research training as a route to educate mental health service users. Teams can also train health system decision makers on the applications of research to meet public health needs. Initiatives like the Mental Health Leadership and Advocacy Program in West Africa do precisely this.87 The project teaches mental health care providers, government officials, policy-makers, and organizations representing service users and caregivers about mental health and builds skills for advocating for mental health service development among key stakeholders.87 The leaders that emerge from such programs are ideal candidates for research training. Although they may not conduct research, understanding the sources and uses of local data can further empower them.
SUMMARY
The 5 challenges discussed here demand more than multidisciplinary research efforts. These challenges require coordinated efforts across science, policy, and many domains of practice (education, nutrition, mental health, justice, etc.). The authors have described specific programs that attempt to mobilize the diverse skills of multiple stakeholders to tackle these problems. Can a larger effort be mounted? The global effort to expand access to treatment and care for human immunodeficiency virus infection is a good example of a public health effort that garnered large, targeted investments and rapidly linked new evidence to clinical practice, making use of partnerships among funders, governments, scientists, clinicians, advocates, and community organizations.88 There are surely lessons for mental health researchers and other interested parties. The stakes are high: they carry the life chances of millions of children worldwide for whom research is critical and the capacity to move relevant research to action, essential.
KEY POINTS.
Research plays an essential role in global mental health.
The knowledge and interventions generated by research must be translated to action to achieve public health impact.
Global research relevant to child and adolescent mental health requires multidisciplinary collaboration and the capacity to conduct research activities that range from basic neuro-science to health policy research.
Equitable research collaborations can facilitate research capacity building and ensure full participation of high-income country (HIC) and low- and middle-income country (LMIC) researchers to solve problems.
Footnotes
The authors have no disclosures.
The viewpoints expressed in this article do not necessarily reflect the views of the National Institute of Mental Health.
REFERENCES
- 1.WHO . Preventing suicide: a global perspective. World Health Organization; Geneva (Switzerland): 2014. [Google Scholar]
- 2.WHO . Health for the World's adolescents: a second chance in the second decade, summary. World Health Organization; Geneva (Switzerland): 2014. [Google Scholar]
- 3.Herne MA, Bartholomew ML, Weahkee RL. Suicide mortality among American Indians and Alaska natives, 1999-2009. Am J Public Health. 2014;104:S336–42. doi: 10.2105/AJPH.2014.301929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hicks J. Statistical data on death by suicide by Nunavut Inuit, 1920 to 2014. Report prepared for Nunavut Tunngavik Inc. 2015 [Google Scholar]
- 5.WHO . Mental health action plan 2013-2020. World Health Organization; Geneva (Switzerland): 2013. [Google Scholar]
- 6.National Action Alliance for Suicide Prevention . Research prioritization task force. a prioritized research agenda for suicide prevention: an action plan to save lives. National Institute of Mental Health and the Research Prioritization Task Force; Rockville (MD): 2014. [Google Scholar]
- 7.United Nations Department of Economic and Social Affairs, Population Division . World population prospects: the 2012 revision. DVD Edition United Nations; New York: 2013. [Google Scholar]
- 8.Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20:359–64. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 10.Murray C, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 11.Vos T, Flaxman A, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shonkoff JP, Richter L. The powerful reach of early childhood development: a science-based foundation for sound investment. In: Britto PR, Engle PL, Super CM, editors. Handbook of early childhood development research and its impact on global policy. Oxford University Press; New York: 2013. pp. 24–34. [Google Scholar]
- 13.Insel TR. Mental disorders in childhood: shifting the focus from behavioral symptoms to neurodevelopmental trajectories. JAMA. 2014;311:1727–8. doi: 10.1001/jama.2014.1193. [DOI] [PubMed] [Google Scholar]
- 14.Commission on Health Research for Development . Health Research: essential link to equity in development. Oxford University Press; New York: 1990. [Google Scholar]
- 15.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378:1515–25. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 16.Hoagwood K, Olin S. The NIMH blueprint for change report: research priorities in child and adolescent mental health. J Am Acad Child Adolesc Psychiatry. 2002;41:760–7. doi: 10.1097/00004583-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Moon S, Szlezák NA, Michaud CM, et al. The global health system: lessons for a stronger institutional framework. PLoS Med. 2010;7:e1000193. doi: 10.1371/journal.pmed.1000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collins PY, Tomlinson M, Kakuma R, et al. Research priorities, capacity, and networks in global mental health. In: Patel V, Minas H, Cohen A, et al., editors. Global mental health principles and practice. Oxford University Press; New York: 2013. pp. 425–49. [Google Scholar]
- 19.Varmus H, Klausner R, Zerhouni E, et al. Grand challenges in global health. Science. 2003;302:398–9. doi: 10.1126/science.1091769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daar AS, Singer PA, Persad DL, et al. Grand challenges in chronic noncommunicable diseases. Nature. 2007;450:494–6. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 21.Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health. Nature. 2011;475:27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lancet Mental Health Group. Chisholm D, Flisher AJ, et al. Scale up services for mental disorders: a call for action. Lancet. 2007;370:1241–52. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]
- 23.Sharan P, Gallo C, Gureje O, et al. Mental health research priorities in low- and middle-income countries of Africa, Asia, Latin America and the Caribbean. Br J Psychiatry. 2009;195:354–63. doi: 10.1192/bjp.bp.108.050187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tomlinson M, Rudan I, Saxena S, et al. Setting priorities for global mental health research. Bull World Health Organ. 2009;87:438–46. doi: 10.2471/BLT.08.054353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galton F. English men of science: their nature and nurture. Macmillan & co; London: 1874. [Google Scholar]
- 26.Rees S, Harding R. Brain development during fetal life: influences of the intrauterine environment. Neurosci Lett. 2004;361:111–4. doi: 10.1016/j.neulet.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Irner TB, Teasdale TW, Olofsson M. Cognitive and social development in pre-school children born to women using substances. J Addict Dis. 2012;31:29–44. doi: 10.1080/10550887.2011.642766. [DOI] [PubMed] [Google Scholar]
- 28.Perera FP, Rauh V, Whyatt RM, et al. A summary of recent findings on birth outcomes and developmental effects of prenatal ETS, PAH, and pesticide exposures. Neurotoxicology. 2005;26:573–87. doi: 10.1016/j.neuro.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 29.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–99. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- 30.Hackman DA, Farah MJ, Meaney MJ. Socioeconomic status and the brain: mechanistic insights from human and animal research. Nat Rev Neurosci. 2010;11:651–9. doi: 10.1038/nrn2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walker SP, Wachs TD, Gardner JM, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007;369:145–57. doi: 10.1016/S0140-6736(07)60076-2. [DOI] [PubMed] [Google Scholar]
- 32.Berkman DS, Lescano AG, Gilman RH, et al. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002;359:564–71. doi: 10.1016/S0140-6736(02)07744-9. [DOI] [PubMed] [Google Scholar]
- 33.Sampson RJ. The neighborhood context of well-being. Perspect Biol Med. 2003;46:S53–64. [PubMed] [Google Scholar]
- 34.Xue Y, Leventhal T, Brooks-Gunn J, et al. Neighborhood residence and mental health problems of 5- to 11-year-olds. Arch Gen Psychiatry. 2005;62:554–63. doi: 10.1001/archpsyc.62.5.554. [DOI] [PubMed] [Google Scholar]
- 35.Beddington J, Cooper CL, Field J, et al. The mental wealth of nations. Nature. 2008;455:1057–60. doi: 10.1038/4551057a. [DOI] [PubMed] [Google Scholar]
- 36.Foresight mental capital and wellbeing project . Final project report. The Government Office for Science; London: 2008. [Google Scholar]
- 37.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 38.Lund C, De Silva M, Plagerson S, et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet. 2011;378:1502–14. doi: 10.1016/S0140-6736(11)60754-X. [DOI] [PubMed] [Google Scholar]
- 39.United Nations . The millennium development goals report. United Nations; New York: 2014. [Google Scholar]
- 40.Olinto P, Beegle K, Sobrado C, et al. The state of the poor: Where are the poor, where is extreme poverty harder to end, and what is the current profile of the world's poor? [November 22, 2014];Economic Premise. 2013 Available at: http://www.worldbank.org/economicpremise.
- 41.Grantham-McGregor S, Cheung YB, Cueto S, et al. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.IOM (Institute of Medicine), National Research Council . The cost of inaction for young children globally: workshop summary. National Academies Press; Washington, DC: 2014. [PubMed] [Google Scholar]
- 43.The World Bank [November 22, 2014];Education Staff Development Program: Early Childhood Development for Policymakers and Practitioners. 2014 Available at: http://einstitute.worldbank.org/ei/course/education-staff-development-program-early-childhood-development-policymakers-and-practitioner.
- 44.U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children Youth and Families, Children's Bureau, Child Maltreatment 2011 [November 22, 2014];2012 Available at: http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment.
- 45.United Nations Children's Fund . Hidden in Plain Sight: a statistical analysis of violence against children. UNICEF; New York: 2014. [Google Scholar]
- 46.Skeen S, Tomlinson M. A public health approach to preventing child abuse in low- and middle-income countries: a call for action. Int J Psychol. 2013;48:108–16. doi: 10.1080/00207594.2012.737467. [DOI] [PubMed] [Google Scholar]
- 47.Olds DL, Henderson J, Charles R, et al. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78:65–78. [PubMed] [Google Scholar]
- 48.USAID [November 22, 2014];United States Government Action Plan on Children In Adversity: A Framework for International Assistance: 2012-2017. 2012 Available at: http://www.usaid.gov/sites/default/files/documents/1860/United States Action Plan on Children in Adversity.pdf.
- 49.Gordon RS., Jr An operational classification of disease prevention. Public Health Rep. 1983;98:107–9. [PMC free article] [PubMed] [Google Scholar]
- 50.Institute of Medicine, National Research Council . Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- 51.Jane-Llopis E, Barry M, Hosman C, et al. Mental health promotion works: a review. Promot Educ. 2005;(Suppl 2):9–25. 61, 67. doi: 10.1177/10253823050120020103x. [DOI] [PubMed] [Google Scholar]
- 52.World Health Organization . Promoting mental health: concepts, emerging evidence, practice: summary report/a report from the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. World Health Organization; Geneva, Switzerland: 2004. [Google Scholar]
- 53.Hosman C, Lopis J. International Union for Health Promotion and Education, IUHPE. Jouve Composition & Impression; Paris: 1999. Political challenges 2: Mental health. The Evidence of Health Promotion Effectiveness: Shaping Public Health in a New Europe. pp. 29–41. [Google Scholar]
- 54.Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program's effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042–54. doi: 10.1037/a0017671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Clarke GN, Hawkins W, Murphy M, et al. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry. 1995;34:312–21. doi: 10.1097/00004583-199503000-00016. [DOI] [PubMed] [Google Scholar]
- 56.Arnarson EÖ, Craighead WE. Prevention of depression among Icelandic adolescents. Behav Res Ther. 2009;47:577–85. doi: 10.1016/j.brat.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 57.Barrett PM, Farrell LJ, Ollendick TH, et al. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: an evaluation of the friends program. J Clin Child Adolesc Psychol. 2006;35:403–11. doi: 10.1207/s15374424jccp3503_5. [DOI] [PubMed] [Google Scholar]
- 58.Dadds MR, Roth JH. Prevention of anxiety disorders: results of a universal trial with young children. J Child Fam Stud. 2008;17:320–35. [Google Scholar]
- 59.Stallard P. Mental health prevention in UK classrooms: the FRIENDS anxiety prevention programme. Emot Behav Diffic. 2010;15:23–35. [Google Scholar]
- 60.Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study. Behav Change. 2001;18:36–50. [Google Scholar]
- 61.Webster-Stratton C, Jamila Reid M, Stoolmiller M. Preventing conduct problems and improving school readiness: evaluation of the incredible years teacher and child training programs in high-risk schools. J Child Psychol Psychiatry. 2008;49:471–88. doi: 10.1111/j.1469-7610.2007.01861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Slough NM, McMahon RJ, Bierman KL, et al. Preventing Serious conduct problems in school-age youths: the fast track program. Cogn Behav Pract. 2008;15:3–17. doi: 10.1016/j.cbpra.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McCord J, Tremblay RE, Vitaro F, et al. Boys’ disruptive behaviour, school adjustment, and delinquency: the Montreal prevention experiment. Int J Behav Dev. 1994;17:739–52. [Google Scholar]
- 64.Ialongo N, Poduska J, Werthamer L, et al. The distal impact of two first-grade preventive interventions on conduct problems and disorder in early adolescence. J Emot Behav Disord. 2001;9:146–60. [Google Scholar]
- 65.Palinkas LA, Atkins CJ, Miller C, et al. Social skills training for drug prevention in high-risk female adolescents. Prev Med. 1996;25:692–701. doi: 10.1006/pmed.1996.0108. [DOI] [PubMed] [Google Scholar]
- 66.Griffin KW, Botvin GJ, Nichols TR, et al. Effectiveness of a universal drug abuse prevention approach for youth at high risk for substance use initiation. Prev Med. 2003;36:1–7. doi: 10.1006/pmed.2002.1133. [DOI] [PubMed] [Google Scholar]
- 67.Pantin H, Prado G, Lopez B, et al. A randomized controlled trial of Familias Unidas for Hispanic adolescents with behavior problems. Psychosom Med. 2009;71:987–95. doi: 10.1097/PSY.0b013e3181bb2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Arch Gen Psychiatry. 2010;67:85–93. doi: 10.1001/archgenpsychiatry.2009.173. [DOI] [PubMed] [Google Scholar]
- 69.Fazel M, Patel V, Thomas S, et al. Mental health interventions in schools in low-income and middle-income countries. Lancet Psychiatry. 2014;1:388–98. doi: 10.1016/S2215-0366(14)70357-8. [DOI] [PubMed] [Google Scholar]
- 70.Barry MM, Clarke AM, Jenkins R, et al. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health. 2013;13:835. doi: 10.1186/1471-2458-13-835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saxena S, Funk M, Chisholm D. World health assembly adopts comprehensive mental health action plan 2013–2020. Lancet. 2013;381:1970–1. doi: 10.1016/S0140-6736(13)61139-3. [DOI] [PubMed] [Google Scholar]
- 72.Fusar-Poli P, Borgwardt S, Bechdolf A, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–20. doi: 10.1001/jamapsychiatry.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mamah D, Mbwayo A, Mutiso V, et al. A survey of psychosis risk symptoms in Kenya. Compr Psychiatry. 2012;53:516–24. doi: 10.1016/j.comppsych.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Penttila M, Jaaskelainen E, Hirvonen N, et al. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2014;205:88–94. doi: 10.1192/bjp.bp.113.127753. [DOI] [PubMed] [Google Scholar]
- 75.Marshall M, Lewis S, Lockwood A, et al. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62:975–83. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 76.Farooq S, Large M, Nielssen O, et al. The relationship between the duration of untreated psychosis and outcome in low-and-middle income countries: a systematic review and meta analysis. Schizophr Res. 2009;109:15–23. doi: 10.1016/j.schres.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 77.Large M, Farooq S, Nielssen O, et al. Relationship between gross domestic product and duration of untreated psychosis in low- and middle-income countries. Br J Psychiatry. 2008;193:272–8. doi: 10.1192/bjp.bp.107.041863. [DOI] [PubMed] [Google Scholar]
- 78.Fraguas D, Merchán-Naranjo J, del Rey-Mejías Á , et al. A longitudinal study on the relationship between duration of untreated psychosis and executive function in early-onset first-episode psychosis. Schizophr Res. 2014;158:126–33. doi: 10.1016/j.schres.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 79.Kurihara T, Kato M, Kashima H, et al. Excess mortality of schizophrenia in the developing country of Bali. Schizophr Res. 2006;83:103–5. doi: 10.1016/j.schres.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 80.Ran MS, Chen EY, Conwell Y, et al. Mortality in people with schizophrenia in rural China: 10-year cohort study. Br J Psychiatry. 2007;190:237–42. doi: 10.1192/bjp.bp.106.025155. [DOI] [PubMed] [Google Scholar]
- 81.Thornicroft G, Cooper S, Bortel TV, et al. Capacity building in global mental health research. Harv Rev Psychiatry. 2012;20:13–24. doi: 10.3109/10673229.2012.649117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mullan F, Frehywot S, Omaswa F, et al. The Medical Education Partnership Initiative: PEPFAR's effort to boost health worker education to strengthen health systems. Health Aff. 2012;31:1561–72. doi: 10.1377/hlthaff.2012.0219. [DOI] [PubMed] [Google Scholar]
- 83.Mangezi WO, Nhiwatiwa SM, Cowan FM, et al. Improving psychiatric education and research capacity in Zimbabwe. Med Educ. 2014;48:1132. doi: 10.1111/medu.12554. [DOI] [PubMed] [Google Scholar]
- 84.The Royal Society . Knowledge, networks and nations: global scientific collaboration in the 21st century. The Royal Society; London: 2011. [Google Scholar]
- 85.Ruiz-Casares M. Research ethics in global mental health: advancing culturally responsive mental health research. Transcult Psychiatry. 2014;51:790–805. doi: 10.1177/1363461514527491. [DOI] [PubMed] [Google Scholar]
- 86.Kohrt BA, Upadhaya N, Luitel NP, et al. Authorship in global mental health research: recommendations for collaborative approaches to writing and publishing. Ann Glob Health. 2014;80:134–42. doi: 10.1016/j.aogh.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Adbdulmalik J, Fadahunsi W, Kola L, et al. The Mental Health Leadership and Advocacy Program (mhLAP): a pioneering response to the neglect of mental health in Anglophone West Africa. Int J Ment Health Syst. 2014;8:5. doi: 10.1186/1752-4458-8-5. Available at: http://www.ijmhs.com/content/8/1/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.De Cock K, El-Sadr W, Ghebreyesus T. Game changers: why did the scale-up of HIV treatment work despite weak health systems? J Acquir Immune Defic Syndr. 2011;57:S61–3. doi: 10.1097/QAI.0b013e3182217f00. [DOI] [PubMed] [Google Scholar]
- 89.Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bull World Health Organ. 2009;87:353–61. doi: 10.2471/BLT.08.057075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baker-Henningham H. The role of early childhood education programmes in the promotion of child and adolescent mental health in low- and middle-income countries. Int J Epidemiol. 2014;43:407–33. doi: 10.1093/ije/dyt226. [DOI] [PubMed] [Google Scholar]
- 91.Fazel M, Hoagwood K, Stephan S, et al. Mental health interventions in schools in high-income countries. Lancet Psychiatry. 2014;1:377–87. doi: 10.1016/S2215-0366(14)70312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev. 2011;(6):CD004718. doi: 10.1002/14651858.CD004718.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stafford MR, Jackson H, Mayo-Wilson E, et al. Early interventions to prevent psychosis: systematic review and meta-analysis. Br Med J. 2013;346:f185. doi: 10.1136/bmj.f185. [DOI] [PMC free article] [PubMed] [Google Scholar]