Abstract
Cervical cancer epitomizes the success of cancer prevention through the human papillomavirus (HPV) vaccine, but significant challenges remain in the treatment of advanced disease. We report the first three cases of cervical carcinoma harboring an FGFR3–TACC3 fusion, which serves as a novel therapeutic target. The fusion, identified by comprehensive genomic profiling, activates the FGFR pathway that has been implicated in HPV-driven carcinogenesis. One of the patients whose tumor contained the FGFR3–TACC3 fusion was treated with an investigational FGFR tyrosine kinase inhibitor. Concomitant molecular alterations involving the PI3K/AKT/mTOR and RAF/MEK pathways were also identified and suggest other treatment strategies that deserve investigation. This case series highlights the role of comprehensive genomic profiling in the identification of new therapeutic targets and in targeted therapy selection for patients with cervical cancer.
Keywords: FGFR translocations, FGFR-TACC3, FGFR inhibitors, Cervical carcinoma, Targeted therapy, Adenocarcinoma of the cervix
Highlights
-
•
The first cases of cervical carcinoma harboring an FGFR3–TACC3 fusion
-
•
One of patients whose tumor contained the FGFR3–TACC3 fusion received an investigational FGFR tyrosine kinase inhibitor
-
•
Manuscript highlights the role of genomic profiling identifying new therapeutic targets and targeted therapies
1. Introduction
Cervical cancer is a major health challenge with approximately 530,000 news cases and 270,000 deaths annually worldwide despite remarkable advances in screening and prevention through the development of human papillomavirus (HPV) vaccine. While the majority of cervical cancer cases can be potentially cured with surgery, chemoradiation or a combination of these strategies, treatment options for recurrent or metastatic disease are limited to pelvic exenteration or palliative chemotherapy. A recent phase III trial evaluating the combination of cisplatin, paclitaxel and bevacizumab (monoclonal antibody against vascular endothelial growth factor receptor) in the first-line treatment of metastatic disease elicited a 50% response rate and median overall survival (OS) of approximately 17 months (Tewari et al., 2014). Despite these relatively positive data that led to the approval of the first targeted therapy for this disease (bevacizumab), the median progression-free survival of 8 months demonstrates the aggressive behavior of this disease. Hence, there is an urgent need to advance the understanding of the molecular abnormalities driving cervical cancer pathogenesis that could lead to novel targeted therapies. Comprehensive genomic profiling of metastatic tumors is an increasingly relevant tool to identify somatic alterations leading to additional therapeutic options and a better understanding of tumor molecular pathogenesis. Herein, we describe the first three cases of cervical carcinoma harboring FGFR3–TACC3 fusions revealed by a next-generation sequencing assay able to detect all classes of genomic alterations including gene fusions. The fusion of the fibroblast growth factor receptor gene 3 (FGFR3) with the transforming acidic coiled-coil containing gene (TACC3) has been described in glioblastoma multiforme, bladder urothelial carcinoma, and non-small cell lung cancer (Wu et al., 2013). While FGFR mutations have been described in cervical carcinomas, the FGFR3–TACC3 fusion has not been reported previously (Cappellen et al., 1999). This fusion resulting in FGFR pathway activation provided the rationale for treating one of the patients with a FGFR tyrosine kinase inhibitor (TKI) in a clinical study setting and other molecular alterations involving the PI3K/AKT/mTOR pathway hold the potential to inform treatment decisions.
2. Case 1
The patient was diagnosed in 1997 at age 36 with stage IB1 adenocarcinoma of the cervix and underwent a modified radical hysterectomy, left salpingo-oophorectomy and bilateral pelvic lymphadenectomy. Adjuvant therapy was not indicated. Twelve years later she developed sudden, significant hemoptysis, and work-up revealed bilateral upper and lower lobe lung masses with left hilar adenopathy. She developed respiratory failure requiring intubation, two arterial embolizations and eventually palliative right middle lobectomy to ameliorate the persistent bleeding. Histopathologic examination of the resected lung mass revealed a carcinoma with mixed glandular and squamous features (adenosquamous carcinoma). The tumor cells were diffusely immunoreactive for p16 and were positive for HPV by PCR, consistent with recurrent cervical cancer. The original hysterectomy specimen was unavailable for comparison.
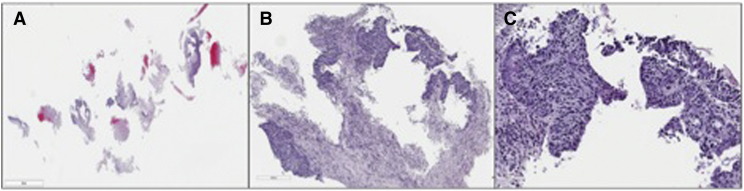
The patient received multiple palliative chemotherapy regimens (i.e., paclitaxel/carboplatin, cisplatin/topotecan, pemetrexed) as well as stereotactic body radiation therapy. Following two years of active surveillance, her PET/CT scans showed an enlarging left upper lobe mass (5.4 cm with SUV 12.6) causing destruction of the left third rib, and a pleural-based lesion in the right lung (SUV 2.9). Transbronchial lung biopsy of the left upper lobe mass revealed a tumor with both squamous and focal glandular differentiation (Fig. 1). The tumor cells were diffusely positive for p16, Pax8, and p63 by immunohistochemistry and HPV 16 by PCR. The morphology, immunohistochemical staining pattern, and HPV results were consistent with those of the right lung metastatic lesion resected 5 years previously. Comprehensive genomic profiling of the left upper lobe lung tumor was performed to identify additional therapeutic options. Hybridization capture of 236 cancer-related genes and 19 genes commonly rearranged in cancer (FoundationOne®) was applied to ≥ 50 ng of DNA extracted from archival formalin-fixed, paraffin embedded left upper lung tumor tissue and sequenced to high, uniform coverage. All classes of genomic alterations (base substitutions, small indels, rearrangements, copy number alterations) were determined and revealed the following: FGFR3–TACC3 fusion (breakpoints at FGFR3 intron 17 and TACC3 intron 10), AKT1 missense mutation (E17K), mTOR point mutation (P1312L), and ATRX truncating nonsense mutation (W1883*).
Fig. 1.
Left upper lobe lung transbronchial biopsy of cervical carcinoma metastasis utilized for comprehensive genomic profiling (A, H&E, 4 × mag). B) Representative tissue fragment is a mixture of metastatic carcinoma, reactive stroma, and inflammatory cells. Tumor nuclei account for approximately 30% of total nuclei (H&E, 20 × mag). C) Carcinoma demonstrates both squamous and glandular differentiation (H&E, 200 × mag).
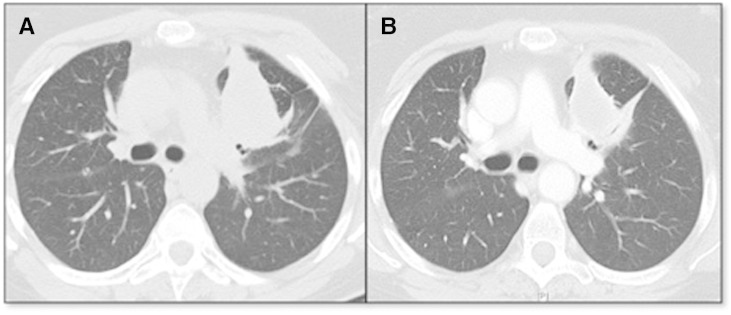
Based on the genomic profiling results, the patient was enrolled in a clinical study evaluating a multi-kinase TKI targeting FGFR (NCT1831726). The patient was treated with the study drug for four cycles with best response of stable disease suggesting expected target (FGFR) inhibition (Fig. 2). The treatment was complicated by skin rash and significant fatigue requiring suspension of therapy.
Fig. 2.
Chest computed tomography showing the tumor response to treatment with FGFR inhibitor. Panel A: baseline tumor measuring 61 mm. Panel B: tumor after 4 cycles measuring 54 mm.
3. Case 2
A 47 year-old female underwent investigation of abnormal uterine bleeding and a cervical biopsy showed an invasive well-differentiated keratinizing squamous cell carcinoma of the cervix. At the time of diagnosis pelvic soft tissue and pelvic lymph node involvement were demonstrated radiographically (FIGO stage IIIB), and she was treated with primary chemoradiation achieving remission. No additional tissue sampling or surgical procedures were performed at this time. The patient developed recurrent disease in the pelvis and adnexa 20 months later and was treated with carboplatin and paclitaxel with partial response after three cycles, receiving a total of five cycles. In July 2014, CT scans showed disease progression, and the patient was started on topotecan and bevacizumab, which was administered for 4 cycles before disease progression causing sigmoid colon involvement and ureteral obstruction. Pemetrexed was started resulting in relief of urinary tract obstruction, but also led to development of a colorectal fistula requiring a colostomy. The patient had excellent performance status and was evaluated for debulking surgery but was deemed not to be a candidate for pelvic exenteration. Comprehensive genomic profiling of the original cervical biopsy was pursued to identify additional therapeutic options and revealed the following: FGFR3–TACC3 fusion (breakpoints at FGFR3 intron 18 and TACC3 intron 7), BRAF 3′ tandem duplication (breakpoint in intron 9 with duplication of exons 10–18), activating PIK3CA missense mutation (E545K), CDNK2A loss, and subclonal activating missense mutations in KRAS (G12C), and HRAS (G13R). Recently, CT scans showed disease progression and the patient enrolled on a clinical trial evaluating a pan-FGFR inhibitor.
4. Case 3
A 33-year-old woman was diagnosed with stage II poorly differentiated non-keratinizing carcinoma of the cervix and she underwent a radical hysterectomy and bilateral salpingo-oophorectomy. The primary tumor measured 5.5 cm and invaded through the inner two-thirds of the cervix. The immunostain profile (positive: p16 and p63; negative: CK20, ER, PR, chromogranin and synaptophysin) was consistent with cervical squamous cell carcinoma. The patient developed rapid disease progression with intra-abdominal and lung metastases leading to palliative treatment with carboplatin/paclitaxel followed by gemcitabine. Comprehensive genomic profiling of the tumor from the hysterectomy specimen was pursued to identify additional therapeutic options, which revealed the following: FGFR3–TACC3 fusion (breakpoints at FGFR3 intron 17 and TACC3 intron 10), partial loss of STK11 (loss of exons 2–9), and RB1 loss (breakpoints in introns 6 and 12). The patient died of uterine hemorrhage 10 months after diagnosis before targeted therapy could be initiated.
5. Discussion
The FGFR family consists of four structurally related subtypes of tyrosine kinase receptors that play an important role in cell growth, differentiation and angiogenesis via binding of twenty different FGF family ligands (Wu et al., 2013). Ligand binding triggers activation of downstream pathways implicated in carcinogenesis, including the PI3K/AKT, RAS/MAPK, phospholipase Cγ, and STAT pathways. Anomalous signaling through FGFR can occur through overexpression of receptors, activating mutations, amplification of the wild type gene, or by FGFR-containing translocations. FGFR3 amplification or activating mutation may lead to activation of FGFR3 and may therefore confer sensitivity to FGFR family inhibitors. FGFR3–TACC3 fusions have been reported to transform rat fibroblasts and to induce tumors in mice.
FGFR3 mutations have been described in approximately 2–5% of cervical carcinomas in large studies (Cappellen et al., 1999, Rosty et al., 2005, Wu et al., 2000). In the COSMIC database, FGFR3 mutation has been found in 2 out of 120 cervical squamous cell carcinoma specimens. In the cervical squamous cell carcinoma and endocervical adenocarcinoma TCGA dataset, putative high-level amplification of FGFR3 was reported in < 1% (1/212) of samples analyzed (cBioPortal, Dec 2014). While transcriptome sequencing revealed rare FGFR3 fusions in glioblastoma, cholangiocarcinoma, breast, prostate, lung, bladder, head and neck, and thyroid cancers (Wu et al., 2013), FGFR3 fusions have not previously been described in cervical carcinoma. FGFR3 fusions are formed by both interchromosomal and intrachromosomal rearrangements, the latter typically involving the TACC3 locus, which is located within 150 kb of the FGFR3 gene on chromosome 4p16 (Still et al., 1999). Similar to the chromosomal proximity of FGFR3 and TACC3, TACC1 and TACC2 genes are also located near their respective FGFR1 and FGFR2 genes, leading to the suggestion that these gene families arose through duplication of a common ancestral FGFR/TACC gene pair.
TACC proteins have been implicated in regulation of mitosis and epithelial mesenchymal transition (EMT). TACC interacts with histone acetyltransferases, and drives proteins to the mitotic spindle via its distinctive coiled-coil domain at the C terminus. TACC3 transcript is overexpressed in cervical cancer human specimens compared to normal cervical tissue and mediates the epidermal growth factor (EGF)-induced EMT in cervical cancer cell lines through upregulation of PI3K/AKT and ERK pathways (Ha et al., 2013). In contrast, FGFR3–TACC3 fusion proteins appear to localize to spindle poles and cause disruption of chromosome segregation and aneuploidy by a mechanism dependent on FGFR tyrosine kinase activity. These preclinical results suggest a role for FGFR3–TACC3 fusion as an oncogenic-driver in multiple tumor types, worthy of target inhibition by small molecule kinase inhibitors. These preclinical results are supported by the observable clinical response in case 1 to FGFR signaling blockade.
In each of these three cases, additional clinically relevant alterations were detected coincident with the FGFR3–TACC3 fusion (Fig. 3). In addition to putative activation of FGFR signaling, each of the three cases displays co-occurring mutations predicted to activate the PI3K/AKT/mTOR pathway, which has been implicated in cervical tumorigenesis. PI3K/AKT/mTOR pathway activation can be mediated by activating mutations in PIK3CA, AKT1, or mTOR or loss of function of STK11. PIK3CA mutations are common in cervical carcinoma (up to 38%; 11% of COSMIC [Jan 2015] and 25% of TCGA [cBioPortal, Jan 2015] cervical cancer datasets). Less commonly, homozygous loss of STK11 (10% of COSMIC [July 2014] and 3% of TCGA [cBioPortal, Feb 2015]) and AKT1 activating mutations (not reported in COSMIC [March 2015]; observed in 2% (3/194) of TCGA [cBioPortal, May 2015]) have been reported in the cervical carcinoma datasets.
Fig. 3.
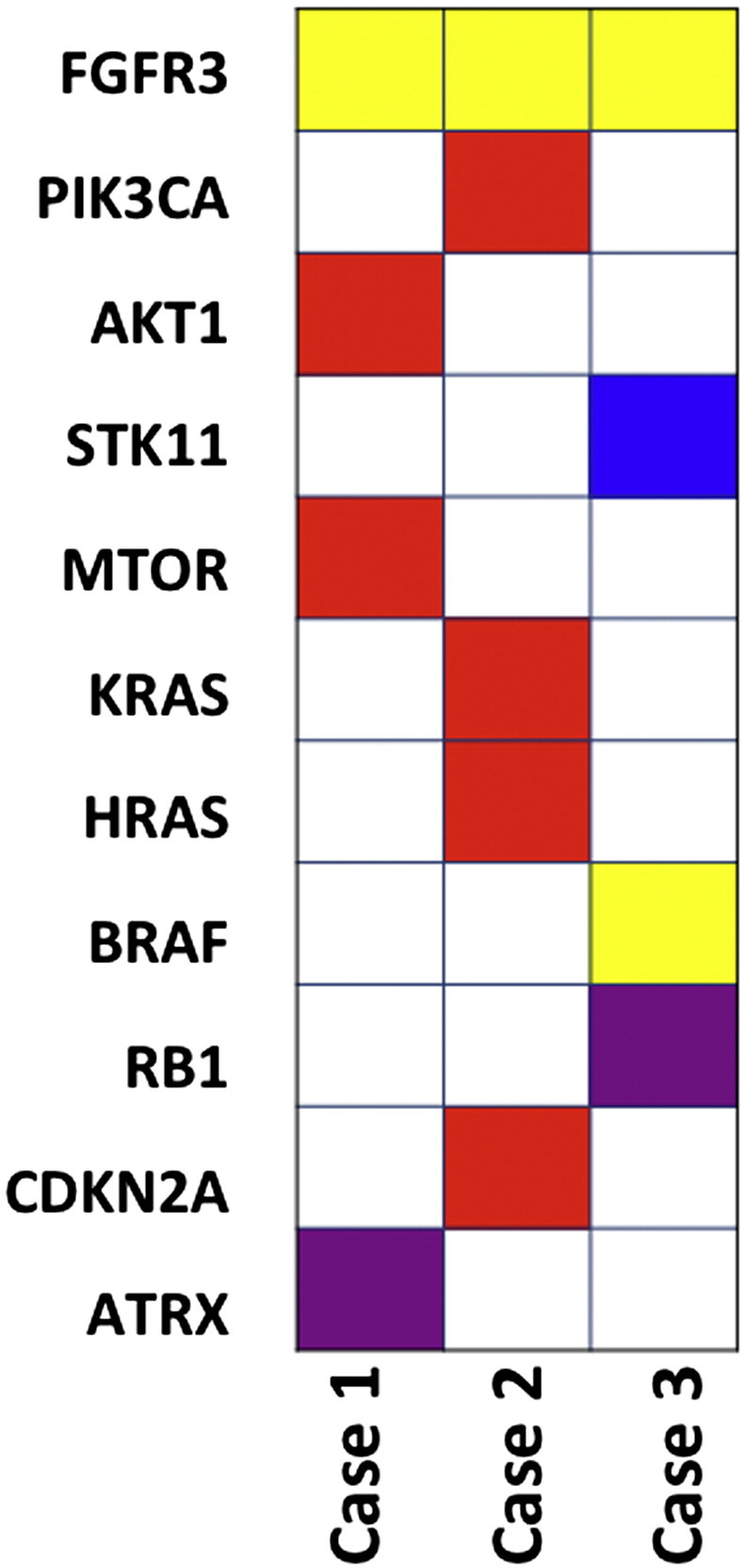
Tileplot comparing co-occurring clinically relevant genomic alterations observed in three cases of invasive cervical carcinoma with FGFR3–TACC3 fusions. Key: Base substitutions (red), homozygous deletions (blue), truncations (purple), and fusions (yellow).
PIK3CA encodes the p110-alpha catalytic subunit of PI3K. Base substitutions in the E545 hotspot codon located in the helical domain, such as observed in case 2, have been shown to be oncogenic (Kang et al., 2005). Activated PI3K converts phosphatidylinositol 4,5-biphosphate (PIP2) to phosphatidylinositol 3,4,5-triphosphate (PIP3), which in turn recruits AKT to the cell membrane for activation through phosphorylation. AKT is an intracellular serine/threonine kinase that promotes cell proliferation and survival by activating the mTOR pathway, interacting with cell-cycle proteins and apoptotic proteins. AKT E17K, observed in case 1, is a constitutively activating missense mutation within the AKT1 pleckstrin homology domain that causes PI3K-independent recruitment to the cell membrane. STK11 encodes serine/threonine-protein kinase 11, also known as Lkb1, that activates AMPK, and negatively regulates the mTOR pathway in response to cellular energy levels (Shaw et al., 2004). STK11 alterations that result in the partial or complete loss of the kinase domain, such as observed in case 3, are predicted to result in a loss of function.
Studies have shown an association of mTOR signaling with prognosis and response to chemotherapy and radiation therapy and the frequency of mutations activating this pathway provided the rationale for clinical studies evaluating the efficacy of mTOR inhibitors for the treatment of cervical cancer. A phase 2 study of single agent temsirolimus in patients with recurrent or metastatic cervical carcinoma reported partial response and stable disease rates of 3% (1/33) and 57% (19/33), respectively (Tinker et al., 2013). In a study of 23 patients with PIK3CA mutated breast or female gynecological cancers, treatment with PI3K/AKT/mTOR pathway inhibitors in combination with other drugs resulted in a partial response of 40% among five patients with advanced cervical SCC (Janku et al., 2012). Despite the small number of patients on these studies, the results suggest a higher efficacy when mTOR inhibitors are combined with inhibitors of other pathways that can circumvent feedback loops causing resistance.
The contribution of the additional co-occurring alterations in the RAF/MEK pathway and in tumor suppressor genes also deserves consideration, as they may be impacting the clinical course or be expected to alter responsiveness to single-agent therapy. In case 2, the BRAF 3′ tandem duplication may result in expression of the constitutively active BRAF kinase domain in the absence of the BRAF N-terminal autoinhibitory domain, and subsequent hyperactivation of the MAPK pathway (Sievert et al., 2013). Similarly, the subclonal missense mutations (codons 12 and 13) in the ‘G box’ domains of the Ras-family GTPases, KRAS and HRAS, also observed in case 2 are predicted to create proteins incapable of GTP hydrolysis and therefore constitutively activate MEK signaling. Finally, p53 and Rb somatic mutation is generally uncommon in HPV-associated cervical carcinomas as the high risk HPV early gene 6 and 7 proteins cause a functional loss of these master tumor suppressors. It seems reasonable to speculate that the unusual RB1 somatic loss observed in case 3 could have also contributed to the especially aggressive clinical course in this patient.
The identification of FGFR3–TACC3 fusion, in addition to previously observed genomic drivers, in these three cases of cervical carcinoma, supports preclinical evidence of the role of FGFR signaling in a subset of HPV-driven carcinogenesis. Specimens from cervical cancer xenograft models exhibit increased expression of FGF2 and FGFR1 genes, while HPV16 E6/E7 oncoproteins reduce their ligand-induced proliferation (Cheng et al., 2012). In addition, HPV E6 oncoprotein has been shown to induce the expression of fibroblast growth factor binding protein (FGF-BP), which regulates the bioavailability of FGF-1 and FGF-2 in the extracellular matrix, and thereby modulates tumor angiogenesis (Stoppler et al., 2001). These observations coupled with the clinical response observed in case 1 support FGFR signaling pathway as a potential therapeutic target in the treatment of cervical carcinoma. Results of ongoing clinical studies investigating potent and specific inhibitors of FGFR could provide a signal of efficacy in this disease. The potential utility of FDA-approved multikinase inhibitors such as pazopanib, lenvatinib and regorafenib in cervical carcinoma carrying FGFR molecular alterations also deserves investigation since these agents inhibit FGFR family members with distinct specificity. Pazopanib, FDA-approved for advanced soft tissue sarcoma and renal cell carcinoma, inhibits FGFR1 and 3; lenvatinib, FDA-approved for advanced radioactive iodine-refractory differentiated thyroid cancer, inhibits FGFR1, 2, 3 and 4; regorafenib, FDA-approved for metastatic colorectal cancer, inhibits FGFR1 and 2. However, at this time, there is no approved indication to use these agents for treatment of solid tumors harboring FGFR molecular aberrations.
This case series highlights the importance of a comprehensive genomic profiling approach able to detect all classes of genomic alterations including uncommon gene fusions to reveal potentially targetable somatic alterations for mutation-matched therapy selection. Case 1 provides proof of concept that treating with an FGFR inhibitor can result in clinical benefit in metastatic cervical cancer carrying FGFR3–TACC3 translocation in agreement with results observed in other malignancies. In a preliminary report, a patient with refractory bladder cancer and lung metastasis harboring a FGFR3–TACC3 fusion demonstrated a partial response to treatment with a pan-FGFR inhibitor, supporting this strategy in patients with similar translocations, irrespective of tumor histology (Bahleda et al., 2014). Cases 1 and 2 also highlight the importance of utilizing a molecular profiling approach able to detect all classes of genomic alterations (base substitutions, insertion/deletions, copy number alterations, and gene fusions) simultaneously on a small tissue sample. Based on the small amount of material available for testing, it is certain that this fusion would not have been detected by a sequential testing approach. These three cases also demonstrate a co-occurrence of more common genomic alterations in PI3K/AKT/mTOR pathway that might require combinatorial treatment strategies given the challenge in identifying the primary “driver” mutation for the tumor.
Acknowledgments
We would like to thank Dr. Paulo Campregher (Hospital Israelita Albert Einstein, Sao Paulo, Brazil) and Dr. Karina Vianna (Curitiba, Brazil) for their contributions to the case 3 clinical description.
Contributor Information
Benedito A. Carneiro, Email: benedito.carneiro@northwestern.edu.
Julia A. Elvin, Email: jelvin@foundationmedicine.com.
Suneel D. Kamath, Email: suneel.kamath@northwestern.edu.
Siraj M. Ali, Email: sali@foundationmedicine.com.
Ajit S. Paintal, Email: ajit.paintal@northwestern.edu.
Alvaro Restrepo, Email: Alvaro.Restrepo@USOncology.com.
Emily Berry, Email: eberry@nmff.org.
Francis J. Giles, Email: francis.giles@northwestern.edu.
Melissa L. Johnson, Email: meljohn22@hotmail.com.
References
- Bahleda R., Dienstmann R., Adamo B., Gazzah A., Infante J.R. Phase 1 study of JNJ-42756493, a pan-fibroblast growth factor receptor (FGFR) inhibitor, in patients with advanced solid tumors. J. Clin. Oncol. 2014;32 doi: 10.1200/JCO.2014.60.7341. (abstract 2501) [DOI] [PubMed] [Google Scholar]
- Cappellen D., De Oliveira C., Ricol D., de Medina S., Bourdin J., Sastre-Garau X. Frequent activating mutations of FGFR3 in human bladder and cervix carcinomas. Nat. Genet. 1999;23:18–20. doi: 10.1038/12615. [DOI] [PubMed] [Google Scholar]
- Cheng Y.M., Chou C.Y., Hsu Y.C., Chen M.J., Wing L.Y. The role of human papillomavirus type 16 E6/E7 oncoproteins in cervical epithelial–mesenchymal transition and carcinogenesis. Oncol. Lett. 2012;3:667–671. doi: 10.3892/ol.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha G.H., Park J.S., Breuer E.K. TACC3 promotes epithelial–mesenchymal transition (EMT) through the activation of PI3K/Akt and ERK signaling pathways. Cancer Lett. 2013;332:63–73. doi: 10.1016/j.canlet.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Janku F., Wheler J.J., Westin S.N., Moulder S.L., Naing A., Tsimberidou A.M. PI3K/AKT/mTOR inhibitors in patients with breast and gynecologic malignancies harboring PIK3CA mutations. J. Clin. Oncol. 2012;30:777–782. doi: 10.1200/JCO.2011.36.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S., Bader A.G., Vogt P.K. Phosphatidylinositol 3-kinase mutations identified in human cancer are oncogenic. Proc. Natl. Acad. Sci. U. S. A. 2005;102:802–807. doi: 10.1073/pnas.0408864102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosty C., Aubriot M.H., Cappellen D., Bourdin J., Cartier I., Thiery J.P. Clinical and biological characteristics of cervical neoplasias with FGFR3 mutation. Mol. Cancer. 2005;4:15. doi: 10.1186/1476-4598-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw R.J., Bardeesy N., Manning B.D., Lopez L., Kosmatka M., DePinho R.A. The LKB1 tumor suppressor negatively regulates mTOR signaling. Cancer Cell. 2004;6:91–99. doi: 10.1016/j.ccr.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Sievert A.J., Lang S.S., Boucher K.L., Madsen P.J., Slaunwhite E., Choudhari N. Paradoxical activation and RAF inhibitor resistance of BRAF protein kinase fusions characterizing pediatric astrocytomas. Proc. Natl. Acad. Sci. U. S. A. 2013;110:5957–5962. doi: 10.1073/pnas.1219232110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Still I.H., Vince P., Cowell J.K. The third member of the transforming acidic coiled coil-containing gene family, TACC3, maps in 4p16, close to translocation breakpoints in multiple myeloma, and is upregulated in various cancer cell lines. Genomics. 1999;58:165–170. doi: 10.1006/geno.1999.5829. [DOI] [PubMed] [Google Scholar]
- Stoppler H., Malerczyk C., Block K., Aigner A., Czubayko F. The human papillomavirus (HPV) 16 E6 oncoprotein leads to an increase in gene expression of the angiogenic switch molecule FGF-BP in non-immortalized human keratinocytes. Oncogene. 2001;20:7430–7436. doi: 10.1038/sj.onc.1204957. [DOI] [PubMed] [Google Scholar]
- Tewari K.S., Sill M.W., Long H.J., III, Penson R.T., Huang H., Ramondetta L.M. Improved survival with bevacizumab in advanced cervical cancer. N. Engl. J. Med. 2014;370:734–743. doi: 10.1056/NEJMoa1309748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinker A.V., Ellard S., Welch S., Moens F., Allo G., Tsao M.S. Phase II study of temsirolimus (CCI-779) in women with recurrent, unresectable, locally advanced or metastatic carcinoma of the cervix. A trial of the NCIC Clinical Trials Group (NCIC CTG IND 199) Gynecol. Oncol. 2013;130:269–274. doi: 10.1016/j.ygyno.2013.05.008. [DOI] [PubMed] [Google Scholar]
- Wu R., Connolly D., Ngelangel C., Bosch F.X., Munoz N., Cho K.R. Somatic mutations of fibroblast growth factor receptor 3 (FGFR3) are uncommon in carcinomas of the uterine cervix. Oncogene. 2000;19:5543–5546. doi: 10.1038/sj.onc.1203934. [DOI] [PubMed] [Google Scholar]
- Wu Y.M., Su F., Kalyana-Sundaram S., Khazanov N., Ateeq B., Cao X. Identification of targetable FGFR gene fusions in diverse cancers. Cancer Discov. 2013;3:636–647. doi: 10.1158/2159-8290.CD-13-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]