Abstract
The current study examined the latent factor structure of posttraumatic stress disorder (PTSD) based on DSM-5 criteria in a sample of participants (N = 374) recruited for studies on trauma and health. Confirmatory factor analyses (CFA) were used to compare the fit of the previous 3-factor DSM-IV model of PTSD to the 4-factor model specified in DSM-5 as well as to a competing 4-factor “dysphoria” model (Simms, Watson, & Doebbeling, 2002) and a 5-factor (Elhai et al., 2011) model of PTSD. Results indicated that the Elhai 5-factor model (re-experiencing, active avoidance, emotional numbing, dysphoric arousal, anxious arousal) provided the best fit to the data, although substantial support was demonstrated for the DSM-5 4-factor model. Low factor loadings were noted for two of the symptoms in the DSM-5 model (psychogenic amnesia and reckless/self-destructive behavior), which raises questions regarding the adequacy of fit of these symptoms with other core features of the disorder. Overall, the findings from the present research suggest the DSM-5 model of PTSD is a significant improvement over the previous DSM-IV model of PTSD.
Keywords: DSM-5, posttraumatic stress disorder, latent factor structure, CFA
With the recent publication of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013), several changes have been made to the diagnosis of posttraumatic stress disorder (PTSD; for a description, see Calhoun et al., 2012; Friedman, 2013; Miller et al., 2013). These changes include: (1) alteration of the stressor criterion (Criterion A), (2) the addition of three new symptoms, (3) revisions or clarifications of several existing symptoms, and (4) the reorganization of symptoms from a three-factor model in DSM-IV to include four clusters of symptoms in DSM-5.
Several of these changes may impact estimations of the latent structure of PTSD symptoms. In particular, the total number of symptoms included in the diagnosis has increased from 17 to 20. In addition, symptoms are now organized under four clusters, rather than the three clusters included in DSM-IV. The five symptoms included in DSM-5 Criterion B remain largely the same as those in the DSM-IV re-experiencing cluster, with the exception of changes in wording intended to emphasize the intrusive (rather than ruminative) nature of these symptoms (Friedman, 2013). However, DSM-5 PTSD Criterion C is now comprised of only two items reflecting effortful avoidance, while DSM-5 PTSD Criterion D contains symptoms of negative alterations in cognitions and mood. Of the seven symptoms now included in Criterion D, two are new symptoms that were added to DSM-5 to capture distorted blame of self or others about the cause or consequence of the traumatic event and pervasive negative emotional state. Additionally, the DSM-IV symptom of sense of foreshortened future has been modified to reflect persistent and exaggerated negative expectations about self, others, or the world. Finally, DSM-5 PTSD Criterion E is comprised of six symptoms reflecting alterations in arousal and reactivity associated with the traumatic event (previously DSM-IV hyperarousal symptoms). Criterion E contains one new symptom, which captures reckless or self-destructive behavior. Additionally, the symptom of irritability and outbursts of anger has been modified to focus exclusively on irritable or aggressive behavior (with irritable and angry feelings subsumed under the negative mood symptom in Criterion D). A diagnosis of PTSD in DSM-5 requires one symptom each from Clusters B and C and two symptoms each from Clusters D and E, each of which must begin following exposure to a qualifying Criterion A event.
An overarching goal of a psychiatric classification system is to “carve nature at its joints” by defining valid and discrete groupings of symptoms that can be used for organizing research and treatment on mental disorders (Meehl, 1992; Widiger & Clark, 2000). DSM-5 diagnostic criteria now define the specific groupings of symptoms that will be studied and treated under the category of PTSD and which will be excluded from the diagnosis. For example, an individual who reports one symptom each from clusters B and C and two symptoms each from Clusters D and E following a traumatic event will be diagnosed with DSM-5 PTSD, and eligible for inclusion in research studies and treatments for the disorder. However, an individual who experiences the same symptoms across clusters B, C, and E but reports no symptoms from cluster D will not - although they may have met DSM-IV criteria for a PTSD diagnosis. Our evolving understanding of the underlying factor structure of PTSD affects the way that we define the groupings of symptoms required for a diagnosis (Friedman, 2013) and therefore may have fundamental implications for the way in which we classify, study, and treat the psychological consequences of trauma. In particular, improved knowledge of the underlying factor structure of PTSD may promote more accurate theoretical models of the nature and origins of the disorder, facilitate more appropriate research questions and methodological designs, and lead to improved treatment approaches by improving the reliability and validity of the diagnosis
Although DSM criteria have historically been generated by empirically-informed expert consensus, our evolving classification system, and DSM-5 in particular, is increasingly based on empirical findings regarding the underlying structure of mental disorders (Friedman, 2013; Widiger & Clark, 2000). In order to continue improving upon our classification system, it will be important to continue to empirically examine the performance of DSM diagnostic criteria. Confirmatory factor analysis (CFA) is well-suited to this purpose, as it enables researchers to assess the degree to which data fit a hypothesized measurement model.
There is now a large literature examining the factor structure of DSM-IV PTSD (for reviews, see Elhai & Palmieri, 2011; Yufik & Simms, 2010). Overall, this research has not supported the three-factor model presented in DSM-IV (Cluster B reexperiencing, Cluster C avoidance, Cluster D hyperarousal), but rather provides consistent support for two similar four-factor models (King, Leskin, King & Weathers, 1998; Simms, Watson, & Doebbeling, 2002). The “emotional numbing” model (King et al., 1998) separates symptoms of active avoidance (e.g., avoiding reminders of trauma) from emotional numbing (e.g., restricted range of affect), retaining the reexperiencing and hyperarousal factors as they are presented in DSM-IV. The “dysphoria” model (Simms et al., 2002) similarly retains the reexperiencing factor, along with an active avoidance factor. However, it includes a broadened version of the emotional numbing factor, in which emotional numbing symptoms are combined with symptoms of sleep disturbance, irritability, and difficulty concentrating to form a factor reflecting general distress or dysphoria. In this model, the hyperarousal factor contains only two items (hypervigilance and exaggerated startle). More recently, a five-factor model has been introduced and has found some preliminary support (Elhai et al., 2011). The five-factor model consists of reexperiencing, active avoidance, and emotional numbing factors, but separates symptoms of sleep disturbance, irritability, and concentration difficulties into a separate dysphoric arousal factor. The two remaining hyperarousal symptoms comprise an anxious arousal factor.
Consistent with factor analytic research supporting these models, research has shown that avoidance and numbing symptoms are clinically distinct from one another in terms of response to treatment and relationships with other forms of psychopathology (Asmundson, Stapleton, & Taylor, 2004). In fact, the separation of active avoidance (Criterion C) from negative alterations in cognitions and mood (Criterion D) in DSM-5 was in part intended to reflect these important statistical and clinical distinctions between effortful avoidance and numbing symptoms (Friedman, 2013). However, very little research to date has examined the factor structure of the new DSM-5 PTSD diagnosis. We are aware of only two recent studies using CFA to examine the latent structure of the new symptom set. Both studies used internet-based surveys to assess symptoms and found an adequate fit to the data in nonclinical college student (Elhai et al., 2012) and US adult and veteran samples (Miller et al., 2013).
The primary aim of the present study was to examine the latent structure of the DSM-5 symptom set in data obtained using an interview-based method to assess symptoms of PTSD. Interview based methods are considered the most valid approach to diagnostic assessment of psychiatric diagnosis and PTSD (Jablensky, 2002; McDonald & Calhoun, 2010; Miller, 2005). CFA was used to evaluate and compare the structural fit of four models: the three-factor model defined by the DSM-IV, the four-factor model proposed by the DSM-5, Simms and colleagues’ (2002) “dysphoria” model, and Elhai and colleagues’ (2011) five-factor model. Consistent with previous research evaluating similar models with DSM-IV data, we hypothesized that Elhai and colleagues’ (2011) model would provide the best overall fit to the data. In addition, given the dearth of descriptive data currently available on the DSM-5 model of PTSD, we also report here the internal consistency for each of the DSM-5 clusters as well as the endorsement rates for each of the DSM-5 PTSD symptoms (Table 4).
Table 4.
DSM-5 Symptom Endorsement and Item-Cluster Correlations
| Item-cluster severity correlations (r) | |||||||
|---|---|---|---|---|---|---|---|
|
DSM-5 symptoms |
Endorsed % (n) |
Mean sx severity (SD) |
B (α = .82) |
C (α = .77) |
D (α = .81) |
E (α = .79) |
Scale α if item removed |
| B-1 | 72% (269) | 1.62 (1.26) | .80 | .67 | .65 | .58 | .76 |
| B-2 | 49% (181) | 1.44 (1.61) | .75 | .48 | .48 | .57 | .80 |
| B-3 | 29% (109) | 0.71 (1.19) | .70 | .43 | .43 | .42 | .80 |
| B-4 | 66% (244) | 1.53 (1.29) | .78 | .55 | .52 | .46 | .77 |
| B-5 | 56% (207) | 1.39 (1.41) | .78 | .56 | .54 | .55 | .77 |
| C-1 | 66% (245) | 1.52 (1.31) | .69 | .90 | .66 | .61 | - |
| C-2 | 56% (209) | 1.38 (1.37) | .58 | .90 | .65 | .60 | - |
| D-1 | 26% (95) | 0.71 (1.30) | .21 | .23 | .44 | .27 | .83 |
| D-2 | 53% (199) | 1.32 (1.39) | .50 | .47 | .74 | .52 | .77 |
| D-3 | 44% (164) | 1.02 (1.33) | .41 | .50 | .67 | .45 | .79 |
| D-4 | 57% (212) | 1.40 (1.39) | .56 | .58 | .74 | .57 | .77 |
| D-5 | 50% (186) | 1.16 (1.31) | .53 | .60 | .69 | .57 | .78 |
| D-6 | 57% (213) | 1.50 (1.43) | .58 | .59 | .81 | .65 | .75 |
| D-7 | 47% (173) | 1.18 (1.39) | .47 | .50 | .69 | .58 | .78 |
| E-1 | 60% (223) | 1.91 (1.70) | .54 | .51 | .55 | .75 | .75 |
| E-2 | 14% (52) | 0.37 (1.01) | .28 | .28 | .34 | .47 | .80 |
| E-3 | 55% (204) | 1.33 (1.34) | .54 | .48 | .56 | .72 | .75 |
| E-4 | 47% (174) | 1.08 (1.23) | .50 | .49 | .63 | .74 | .74 |
| E-5 | 64% (238) | 1.67 (1.43) | .53 | .56 | .60 | .78 | .73 |
| E-6 | 48% (177) | 1.15 (1.34) | .43 | .44 | .47 | .69 | .76 |
Note. Cluster scores based on sum of corresponding item severity scores. Intercriterion item-cluster r-values are bolded.
Method
Participants
The present sample was drawn from 374 participants (n = 210 with a current DSM-IV diagnosis of PTSD, n = 230 with a lifetime diagnosis) who were initially recruited for studies on trauma and health conducted at a VA medical center and an academic medical center in the southeastern United States between August 2010 and July 2013. To be eligible for the current analyses, participants had to: (1) consent to allow their research data to be included in a trauma research database, (2) be English-speaking, (3) be 18 years of age or older, and (4) have completed the measures described below. Thus, all participants included in the current analyses provided informed consent to participate in both a primary research study and a trauma research database. All study procedures were approved by the affiliated Institutional Review Boards. Participant characteristics are listed in Table 1. The average age of the sample was 38.5 years. Based on the Hollingshead index, the sample on average fell in the lower-middle class. The sample was almost evenly split among men and women (47% female). Note, data (including endorsement rates of DSM-5 criteria) for a portion (n = 185; 49%) of the current sample have been previously reported in a paper comparing differences in PTSD prevalence rates based on DSM-IV and proposed DSM-5 criteria (Calhoun et al., 2012).
Table 1.
Sample Characteristics
| Mean (SD) | Freq (%) | |
|---|---|---|
| Age | 38.54 (12.58) | |
| Female | 179 (48%) | |
| Minority | 205 (55%) | |
| SESa | 50.82 (14.23) | |
| Veterans | 157 (42%) | |
| Pre-Vietnam | 1 (1%) | |
| Vietnam | 35 (22%) | |
| Gulf War | 69 (44%) | |
| OEF/OIF | 17 (11%) | |
| Missing | 35 (22%) | |
| CAPS total | 46.24 (28.96) | |
| Current MDD | 69 (20%) |
Note. SES = socioeconomic status; OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; MDD = major depressive disorder.
SES measured via the Hollingshead index (Hollingshead & Redlich, 1958).
Measures
Demographics
Information about age, gender, ethnicity, education, military service, and employment was collected. Level of education and current occupation was summarized as an overall measure of socioeconomic status (SES) in the Hollingshead Index score (Hollingshead & Redlich, 1958). Lower scores on the Hollingshead Index indicate higher SES.
Trauma Exposure
Trauma exposure was assessed with the 22-item Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) which assesses exposure to and reactions to traumatic events. The TLEQ has demonstrated reliability and content validity (Dedert et al., 2009; Kubany et al., 2000).
Clinician-Administered PTSD Scale
All participants were assessed for the presence of DSM-IV-based PTSD symptoms using the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995), a structured clinical interview that evaluates the frequency and intensity of the 17 symptoms of PTSD as defined in the DSM-IV. To diagnose current PTSD status, presence of each symptom was determined using the frequency ≥ 1/intensity ≥ 2 rule (Blake et al., 1995; Weathers, Keane, & Davidson, 2001), which requires a symptom to be endorsed at a frequency of at least once per month and intensity of at least moderate impairment or distress to be counted as present. The CAPS interview has excellent reliability and validity within multiple trauma populations and is widely accepted as the state of the art method for PTSD assessment (Weathers et al., 2001; Weathers, Ruscio, & Keane, 1999). Fourteen interviewers administered the CAPS after receiving intensive training. All interviewers participated in regular diagnostic supervision sessions. Interrater reliability among the raters across five training tapes showed excellent agreement for diagnosis of current PTSD, Fleiss’ kappa = 1.0 (Fleiss & Cohen, 1973). Training tapes included cases with and without current PTSD from childhood sexual trauma, combat trauma, interpersonal violence, and motor vehicle accidents. Following CAPS instructions, current symptoms (past month) for up to three traumatic events were queried. In each case, participants were first queried about their worst traumatic event, that is, the event that was disturbing them most now. In some cases, where an individual did not meet DSM-IV criteria for their “worst traumatic event,” up to two other qualifying DSM-IV traumatic events were explored to see if they would meet DSM-IV PTSD criteria for another trauma. If an individual met DSM-IV criteria for an event other than their worst, it was recorded as their index traumatic event.
Items to Assess New DSM-5 Criteria
Interviewers rated whether or not each individual’s index traumatic event met the new definition of a qualifying traumatic event based on DSM-5 Criterion A. In order to assess newly revised DSM-5 symptoms of PTSD that did not overlap with DSM-IV CAPS items, four additional items were constructed and administered via clinical interview. These items included measurement of DSM-5 Criteria D2 (formally DSM-IV C7), D3, D4, and E2. These new items are provided in Calhoun et al. (2012).
Structured Clinical Interview for DSM-IV
Presence of comorbid major depressive disorder (MDD) and substance misuse (alcohol or drug abuse or dependence) was assessed using the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1997). Eight diagnostic raters performed the SCID and interrater reliability on the SCID across seven SCID training videos was excellent, mean Fleiss’ kappa = 0.92 (Fleiss & Cohen, 1973).
Data Analysis
Confirmatory factor analysis (CFA) was used to evaluate and compare the structural fit of four models: the three-factor model defined by the DSM-IV, the four-factor model proposed by the DSM-5, Simms and colleagues’ (2002) “dysphoria” model, and Elhai and colleagues’ (2011) five-factor model. Each of the four models was constructed using 16 of the 17 CAPS items (dropping item C7) plus the 4 newly constructed DSM-5 items. In the Simms model, the dysphoria factor was comprised of all of the DSM-5 D and E symptoms, with the exception of the hypervigilance and exaggerated startle items (Miller et al., 2013). These two items comprised a separate hyperarousal factor. The remaining B and C symptoms loaded on their respective factors. In the Elhai model, the hypervigilance and exaggerated startle items loaded on one factor, and the remaining hyperarousal items loaded on a “dysphoric arousal” factor. The remaining B, C, and D symptoms loaded on their respective factors (see Table 2 for symptom-scale assignments for each model).
Table 2.
Symptom-Scale Assignments across PTSD Models
| Models | ||||
|---|---|---|---|---|
| DSM-5 symptoms | DSM-IV | DSM-5 | Simms | Elhai |
| (B-1) intrusive recollections | R | R | R | R |
| (B-2) distressing dreams | R | R | R | R |
| (B-3) dissociative reactions (e.g., flashbacks) | R | R | R | R |
| (B-4) psychological distress at exposure to cues | R | R | R | R |
| (B-5) physiological reactivity on exposure to cues | R | R | R | R |
| (C-1) avoidance of internal reminders | A/N | A | A | A |
| (C-2) avoidance of external reminders | A/N | A | A | A |
| (D-1) inability to recall important aspects of trauma | A/N | NA | D | NA |
| (D-2) negative expectations about self/others/world | A/N | NA | D | NA |
| (D-3) distorted blame of self or others | A/N | NA | D | NA |
| (D-4) pervasive negative emotional state | A/N | NA | D | NA |
| (D-5) diminished interest in activities | A/N | NA | D | NA |
| (D-6) detachment or estrangement | A/N | NA | D | NA |
| (D-7) inability to experience positive emotions | A/N | NA | D | NA |
| (E-1) irritable or aggressive behavior | H | H | D | DA |
| (E-2) reckless or self-destructive behavior | H | H | D | DA |
| (E-3) hypervigilance | H | H | H | AA |
| (E-4) exaggerated startle response | H | H | H | AA |
| (E-5) problems with concentration | H | H | D | DA |
| (E-6) difficulty falling or staying asleep | H | H | D | DA |
Note. R, reexperiencing; A = avoidance; N = numbing; H = hyperarousal; NA = negative alterations; D = dysphoria; DA = dysphoric arousal; AA = anxious arousal.
Analyses were conducted on the 5-point intensity ratings for symptoms experienced at least once within the past month. If a given symptom was not endorsed within the past month (i.e., frequency = 0), it was assigned an intensity rating of 0.1 Given non-normal data, CFA was performed using robust maximum likelihood, available through Mplus 7. Model fit was evaluated using standard fit criteria (Hoyle, 1995; Hu & Bentler, 1999): root mean square error of approximation (RMSEA) ≤ .05, comparative fit index (CFI) ≥ .90, and standardized root mean square residual (SRMR) ≤ .08. To accommodate the non-normal data, the Satorra-Bentler scaled chi-square test of difference was used to compare nested models (Curran, West, & Finch, 1996). Akaike (1987) and Bayesian (Schwartz, 1978) information criteria (AIC and BIC, respectively) were also reported to aid in comparison of non-nested models. For these latter two statistics, lower values reflect superior model fit. For comparison of BIC values in particular, a 10-point difference can be interpreted as “very strong” evidence (i.e., p < .05) of the superiority of the model with the smaller BIC (Kass & Raftery, 1995; Raftery, 1995). A difference of 6 to 9 points may be interpreted as “strong” support for a meaningful difference between the models.
Results
Forty-four percent of participants reported a history of military service. Trauma exposure was highly prevalent in the sample with 99% (n = 372) reporting one or more traumatic events on the TLEQ. TLEQ data for the remaining two participants was missing. Twenty-nine percent (n = 110) of the sample endorsed exposure to childhood physical assault and 36% (n = 135) reported a history of childhood sexual assault on the TLEQ. Exposure to a natural disaster or serious accident (84%, n = 313) and exposure to adult physical violence (77%, n = 289) were common. Fewer participants endorsed adult sexual trauma (17%, n = 64) and service in a warzone (30%, n = 111).
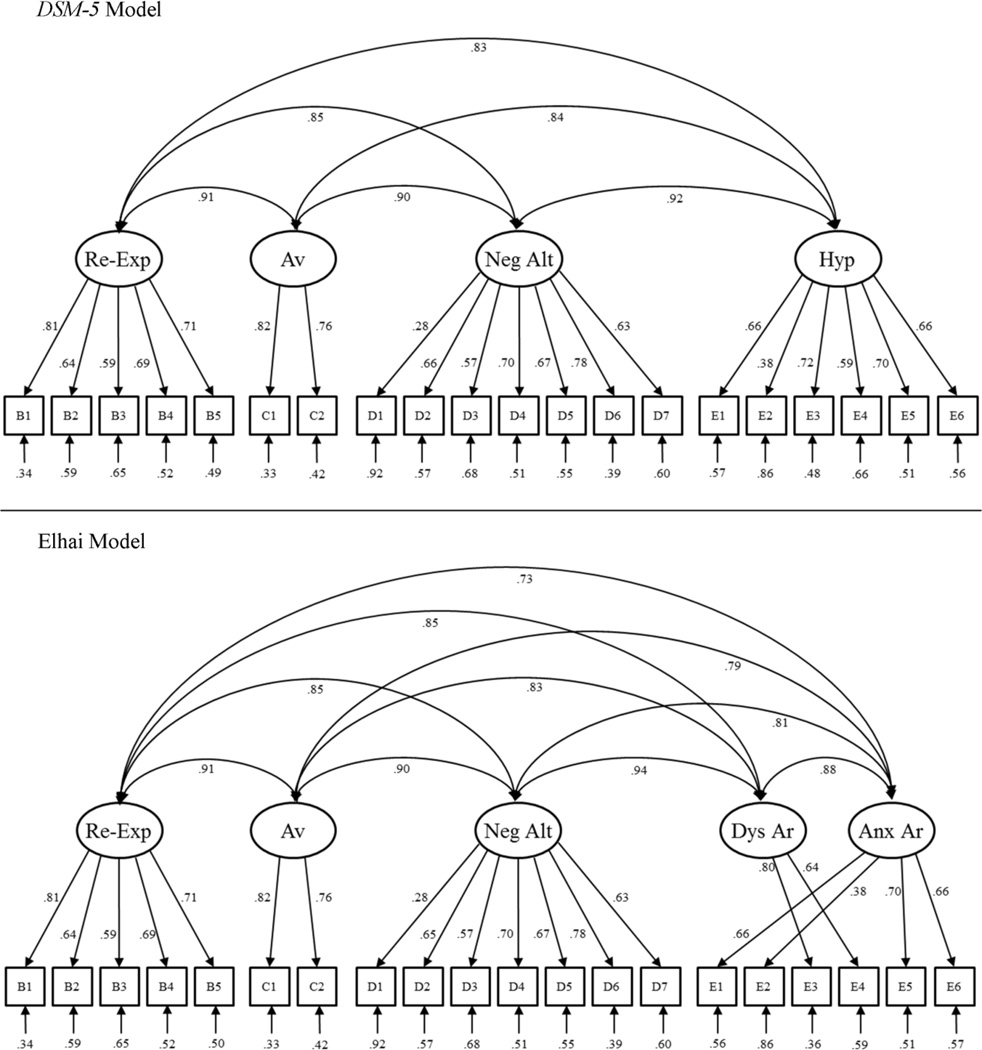
CFA was used to evaluate and compare the structural fit for four competing models. The model fit statistics for the four CFA models are listed in Table 3. Of the four models, the three-factor DSM-IV model demonstrated the weakest fit according to the Satorra-Bentler test of difference, ps < .01, the Elhai model, the strongest, ps ≤ .02. The fit of the DSM-5 and Simms models fell between these two, with the Simms model offering a negligible degree of improvement over the DSM-5 model according to the AIC and BIC indices. As can be seen in Figure 1, in general, factor loadings for the DSM-5 and Elhai models were high (rs ≥ .57), with the lowest factor loadings occurring for the D1 (.28) and E2 (.38) symptoms. Nevertheless, it should still be noted that the DSM-5 model demonstrated excellent fit according to the RMSEA, CFI, and SRMR.
Table 3.
Confirmatory Factor Analysis (CFA) Fit Statistics
| Model | Χ2 (df) | RMSEA | CFI | SRMR | AIC | BIC |
|---|---|---|---|---|---|---|
| DSM-IV (3 factors) | 303.24 (167) | .047 | .947 | .039 | 22348.036 | 22594.074 |
| DSM-5 (4 factors) | 279.35 (164) | .044 | .955 | .038 | 22324.618 | 22582.372 |
| Simms (4 factors) | 277.52 (164) | .043 | .955 | .038 | 22322.874 | 22580.628 |
| Elhai (5 factors) | 264.76 (160) | .042 | .959 | .037 | 22314.794 | 22588.169 |
Note. RMSEA = root means square error of approximation; CFI = comparative fit index; SRMR = standardized root mean square residual; AIC = Akaike information criterion; BIC = Bayesian information criterion.
Figure 1.
Confirmatory factor analysis of PTSD symptomatology proposed by the DSM-5 and Elhai et al. (2011). All estimates are standardized.
Focusing on the DSM-5 model, internal reliability was high for each of the clusters (see Table 4); however, two of the symptoms, D1 (inability to recall important aspects of trauma) and E2 (reckless or self-destructive behavior), loaded poorly on their respective cluster factors (see Figure 1). Otherwise, the remaining symptoms loaded strongly on their corresponding factors (rs ≥ .57). Examination of the modification indices suggested that specifying several cross-loadings—namely, criteria B1 (intrusive recollections) and D5 (diminished interest in activities) on the avoidance factor and B2 (distressing dreams) and B4 (psychological distress at exposure to cues) on the hyperarousal factor—would significantly improve the model. The model demonstrated metric invariance (i.e., factor loadings did not significantly vary) across individuals exposed to a traumatic event prior to age 18 that resulted in fear, helplessness, and horror (n = 302) and those who were not (n = 63), p = .11.
Discussion
The primary objective of the present study was to examine the latent factor structure of the DSM-5 PTSD symptom set in data obtained from a sample using a gold-standard structured clinical interview. As hypothesized, we found that Elhai and colleagues’ (2011) model provided the best overall fit to the data. In addition, as expected, we also found that the DSM-5 and the dysphoria models were superior to the DSM-IV model of the structure of PTSD. Taken together, these findings suggest that that while the DSM-5 model of PTSD is a significant improvement over the previous DSM-IV model of PTSD, it is still may not be the most accurate description of the underlying latent factor structure of the disorder.
The DSM-5 model did, however, perform fairly well overall in the analyses. For example, while the DSM-5 model did not demonstrate the best overall fit to the data, the global fit indices indicated that it still provided excellent fit to the data (e.g., RMSEA = .044, CFI = .955). The latter finding is consistent with two previous internet-based studies of DSM-5 PTSD symptom structure, which also found the proposed DSM-5 model to exhibit good fit to the data. Importantly, though, the current findings are the first to demonstrate that the DSM-5 model provides adequate fit to the data using symptom-level data obtained from an interview based assessment method, which is considered to be the gold-standard for the assessment of PTSD.
The factor loadings for the DSM-5 model were also relatively high (avg. factor loading = .65), although two notable exceptions to this finding were the factor loadings for the psychogenic amnesia (.28) and reckless/self-destructive behavior (.38) symptoms. This finding is, however, consistent with those of Miller and colleagues (2013), who also found low factor loadings for psychogenic amnesia (.41, .48) and reckless/self-destructive behavior (.41, .41) in two internet-based studies (community sample, veteran sample, respectively).
The finding that psychogenic amnesia has a low factor loading is also consistent with factor analytic studies of DSM-IV PTSD symptoms (e.g., King et al., 1998; Simms et al., 2002). There is also some evidence that psychogenic amnesia may be more likely to be endorsed by individuals with more severe symptomatology (Miller et al., 2013) and severe dissociative symptoms (Wolf et al., 2012), leading some researchers to suggest the possibility that this symptom should be dropped from the core symptoms of PTSD in DSM-5 and instead be used as a potential marker of a dissociative subtype of PTSD (Miller et al., 2013). However, rather than add a dissociative subtype, the new DSM-5 criteria include a “with dissociative symptoms” specifier that requires the individual to experience either persistent depersonalization or persistent derealization (American Psychiatric Association, 2013). While additional research on the new DSM-5 PTSD symptom set is still needed, the low factor loading (.28) and low item-cluster correlation (.44) suggest that the psychogenic amnesia item has a fairly low association with the negative alterations cluster of PTSD symptoms (i.e., Cluster D). Moreover, the low endorsement rate (26%) of this item that was observed in the current study lends further support to the idea that this symptom is not a core feature of the typical PTSD presentation.
In contrast with the relatively well-established literature on psychogenic amnesia, the reckless/self-destructive behavior symptom is one of the new symptoms introduced in DSM-5. The present research and that of Miller and colleagues (2013) and Elhai and colleagues (2012) are the only studies that we are aware of that have examined the performance of this symptom within a factor-analytic framework. Both the present study and Miller et al. (2013) observed low factor loadings (less than .42 across all three samples) and low endorsement rates for this item (less than 15% for past month across all three samples). In contrast, Elhai et al. (2012) reported a high factor loading (.84) for the reckless/self-destructive behavior item among a sample of college students collected through the internet. Thus, there appear to be substantial differences in the performance of this item, possibly due to differences in methodology and sample composition. Clearly, more research on the DSM-5 symptom set in other trauma samples will be necessary to determine how well the reckless/self-destructive symptom performs; however, it is important to note that the majority of evidence to date [i.e., the present study and the two studies reported by Miller et al. (2013)] suggests that this item may perform poorly as well.
Limitations and Future Directions
The current study had several limitations that should be noted when interpreting the findings. First, while a clinical interview was used to assess PTSD symptoms, it should be noted that we used a modified version of the original DSM-IV based CAPS interview. The CAPS-5 is still under development by Dr. Frank Weathers and a team of investigators at the VA National Center for PTSD, so it is unclear the degree to which the current findings will differ from those obtained after the CAPS and other clinical measures are updated and finalized to reflect the new DSM-5 criteria. It is possible that differences in the wording of items designed to assess DSM-5 criteria could have some impact on the results of item endorsement. A second limitation concerns the composition of the sample in the current study. Specifically, because the sample was derived from multiple trauma studies, the trauma types are not homogenous, as is often the case in studies of traumatized populations. Thus, while a benefit of this approach is that the trauma sample in the present sample was quite diverse, the degree to which the findings from the current study will relate to other more homogenous trauma samples (e.g., rape survivors, veteran samples, domestic violence victims) is unclear.
Summary and Conclusion
The primary objective of the present research was to examine the latent structure of the DSM-5 PTSD symptom set in data obtained using a structured clinical interview to assess symptoms of PTSD. CFA was used to evaluate and compare the structural fit of four models: the three-factor model defined by the DSM-IV, the four-factor model proposed by the DSM-5, Simms and colleagues’ (2002) “dysphoria” model, and Elhai and colleagues’ (2011) five-factor model. As hypothesized, Elhai and colleagues’ (2011) 5-factor model provided the best overall fit to the data, although the DSM-5 model also performed well in the analyses. Particularly low factor loadings were noted for two of the symptoms in the DSM-5 model (psychogenic amnesia and reckless/self-destructive behavior). Overall, the findings from the present research suggest that that while the DSM-5 model of PTSD is a significant improvement over the previous DSM-IV model of PTSD, it may not be the most accurate description of the underlying latent factor structure of the disorder. Additional research on the factor structure of DSM-5 PTSD symptomatology is warranted.
Acknowledgements
Preparation of this manuscript was supported, in part, by grants R01MH062482 from the National Institute of Mental Health, K24DA016388 from the National Institute on Drug Abuse and R21CA128965 from the National Cancer Institute. This work was also supported by resources and facilities at the VA Mid-Atlantic MIRECC, Durham VA Medical Center; by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment; and by the Clinical Science Research and Development Service of the VA Office of Research and Development. Dr. Kimbrel was supported by a Career Development Award (IK2 CX000525) from the Clinical Science Research and Development Service of the VA Office of Research and Development. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Alternative CFA modeling of the sum of frequency and intensity ratings yielded similar results.
References
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: Author; 2013. [Google Scholar]
- Asmundson GJ, Stapleton JA, Taylor S. Are avoidance and numbing distinct PTSD symptom clusters? Journal of Traumatic Stress. 2004;17:467–475. doi: 10.1007/s10960-004-5795-7. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered posttraumatic stress disorder scale. Journal of Traumatic Stress. 1995;8:75–80. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Hertzberg JS, Kirby AC, Dennis MF, Hair LP, Dedert EA, Beckham JC. The effect of draft DSM-V criteria on posttraumatic stress disorder prevalence. Depression and Anxiety. 2012;29:1032–1042. doi: 10.1002/da.22012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods. 1996;1:16–29. [Google Scholar]
- Dedert EA, Green KT, Calhoun PS, Toash-Gantz R, Taber KH, Mumford MM, Beckham JC. Association of trauma exposure with psychiatric morbidity in military veterans who have served since September 11, 2001. Journal of Psychiatric Research. 2009;43:830–836. doi: 10.1016/j.jpsychires.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Biehn TL, Armour C, Klopper JJ, Frueh BC, Palmieri PA. Evidence for a unique PTSD construct represented by PTSD’s D1-D3 symptoms. Journal of Anxiety Disorders. 2011;25:340–345. doi: 10.1016/j.janxdis.2010.10.007. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Miller ME, Ford JD, Biehn TL, Palmieri PA, Frueh BC. Posttraumatic stress disorder in DSM-5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. Journal of Anxiety Disorders. 2012;26:58–64. doi: 10.1016/j.janxdis.2011.08.013. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Palmieri PA. The factor structure of posttraumatic stress disorder: A literature update, critique of methodology, and agenda for future research. Journal of Anxiety Disorders. 2011;25:849–854. doi: 10.1016/j.janxdis.2011.04.007. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. Washington, DC: American Psychiatric Press, Inc.; 1997. [Google Scholar]
- Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educational and Psychological Measurement. 1973;33:613–619. [Google Scholar]
- Friedman M. Finalizing PTSD in DSM-5: Getting here from there and where to go next. Journal of Traumatic Stress. 2013;26:548–556. doi: 10.1002/jts.21840. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB, Redlich RL. Social class and mental illness. New York, NY: John Wiley; 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle RH. Structural equation modeling. Thousand Oaks, CA: Sage Publications, Inc.; 1995. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jablensky A. Research methods in psychiatric epidemiology: An overview. Australian and New Zealand Journal of Psychiatry. 2002;36:297–310. doi: 10.1046/j.1440-1614.2002.01035.x. [DOI] [PubMed] [Google Scholar]
- Kass RE, Raftery AE. Bayes factors. Journal of the American Statistical Association. 1995;90:773–795. [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence of the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD checklist: A critical review. Clinical Psychology Review. 2010;30:976–987. doi: 10.1016/j.cpr.2010.06.012. [DOI] [PubMed] [Google Scholar]
- Meehl PE. Factors and taxa, traits and types, differences of degree and differences in kind. Journal of Personality. 1992;60:117–174. [Google Scholar]
- Miller AB. General principles of screening. In: Ahrens W, Krickeberg K, Pigeot I, editors. Handbook of epidemiology. Berlin: Berlin Springer Science & Business Media; 2005. pp. 1268–1300. [Google Scholar]
- Miller MW, Wolf EJ, Kilpatrick D, Resnick H, Marx BP, Holowka DW, Rosen RC. The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:501–512. [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–196. [Google Scholar]
- Schwartz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–746. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. [Google Scholar]
- Widiger TA, Clark LA. Toward DSM-V and the classification of psychopathology. Psychological Bulletin. 2000;126:946–963. doi: 10.1037/0033-2909.126.6.946. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, Freund R. A latent class analysis of dissociation and posttraumatic stress disorder: Evidence for a dissociative subtype. JAMA Psychiatry. 2012;69:698–705. doi: 10.1001/archgenpsychiatry.2011.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yufik T, Simms LJ. A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. Journal of Abnormal Psychology. 2010;119:764–776. doi: 10.1037/a0020981. [DOI] [PMC free article] [PubMed] [Google Scholar]