Abstract
Chronic pain conditions are the top reason patients seek care, the most common reason for disability and addiction, and the biggest driver of healthcare costs; their treatment costs more than cancer, heart disease, dementia, and diabetes care. The personal impact in terms of suffering, disability, depression, suicide, and other problems is incalculable. There has been much effort to prevent many medical and dental conditions, but little effort has been directed toward preventing chronic pain. To address this deficit, a massive open online course (MOOC) was developed for students and healthcare professionals. “Preventing Chronic Pain: A Human Systems Approach” was offered by the University of Minnesota through the online platform Coursera. The first offering of this free open course was in the spring of 2014 and had 23 650 participants; 53% were patients or consumers interested in pain. This article describes the course concepts in preventing chronic pain, the analytic data from course participants, and postcourse evaluation forms.
Key Words: Chronic pain, pain, online education, massive open online course, MOOC
摘要
慢性疼痛疾病是寻求医疗护理的 第一大原因、残疾和成瘾的最常 见原因,以及推动医疗护理成本 升高的最大原因,且慢性疼痛疾 病 治 疗 的 费 用 多 于 癌 症 、 心 脏 病、老年痴呆症和糖尿病。但无 法 计 算 患 病 的 痛 苦 、 残 疾 、 抑 郁、自杀和其他问题对人产生的 影响。为预防许多医学和牙科疾 病,我们已作出了许多努力,但 直接针对预防慢性疼痛的努力仍 很少。为弥补此不足,我们为学 生和医疗保健专业人员开展了一 项大型网络公开课 (MOOC)。明尼 苏达大学通过 www.Coursera.org 提供了“预防慢性疼痛:一种人 类系统法”公开课。此免费公开 课于 2014 年春天首次开播,有 23650 人参加学习;其中 53% 的 参加者是患者或关注疼痛治疗的 消费者。本文描述了预防慢性疼 痛的课程理念、课程参与者的分 析数据和课后评价表。
SINOPSIS
Las afecciones de dolor crónico son el principal motivo de búsqueda de asistencia sanitaria, la causa más frecuente de discapacidad y toxicomanía, y el factor generador de costos sanitarios más importante, con un coste mayor al generado por el cáncer, la cardiopatía, la demencia y la diabetes. Las repercusiones en cuanto a sufrimiento, discapacidad, depresión, suicidio y otros problemas son incalculables. Se han consagrado grandes esfuerzos a la prevención de muchas enfermedades médicas y dentales, pero no se han dirigido los suficientes hacia la prevención del dolor crónico. Para hacer frente a este déficit, se ha desarrollado un curso en línea masivo y abierto (massive open online course, MOOC) para estudiantes y profesionales sanitarios. La Universidad de Minnesota ofreció el curso “Prevención del dolor crónico: enfoque de un sistema humanista” a través del sitio www.Coursera.org. La primera oferta de este curso abierto y gratuito se hizo en primavera de 2014 y acogió a 23 650 participantes; de los cuales un 53 % eran pacientes o clientes interesados en el dolor. En este artículo se describen los conceptos del curso en la prevención del dolor crónico, los datos analíticos de los participantes y los formularios de evaluación posteriores al curso.
INTRODUCTION
Chronic pain conditions are the most prevalent chronic conditions and the primary driver of healthcare, costing more than diabetes, cancer, and heart disease.1-4 With at least 120 million US adults suffering from chronic pain including headaches, back and neck pain, and orofacial pain, pain has become the primary reason patients seek healthcare. Over half of all physician visits are attributed to some type of chronic pain.4 Chronic pain is also the most common cause of work loss, disability, and opioid dependency leading to more deaths than motor vehicle accidents in some states.5-11 On a community level, the prevalence and cost burden of chronic pain is staggering; however, the personal cost of chronic pain can be even more devastating with loss of function, depression, suicide, addiction, overdosing, and lower quality of life.12-13
While major efforts are underway to prevent other major health conditions such as heart disease and diabetes, preventing chronic pain remains overlooked by the public, neglected by the healthcare system, and omitted by the scientific community.11-13 Thus, a massive open on-line course (MOOC) sponsored by the University of Minnesota and entitled “Preventing Chronic Pain: A Human Systems Approach” was offered through www.Coursera.org, a MOOC platform.14 The first offering of the course in the spring of 2014 had 23 650 participants. We were surprised to find that 53% of them were patients or consumers interested in chronic pain, attesting to the great interest by those who suffer from it. This paper describes the course concepts in preventing chronic pain, the analytic data from the course, the course participants' pain assessments, and postcourse evaluation forms.
Rationale for the Course
Despite the societal and personal impact, the plight of the patient with chronic pain seeking healthcare is profound. If initial efforts to improve pain fail, care often escalates to higher-cost, higher-risk passive interventions such as ongoing opioid analgesics, polypharmacy, implantable devices, injections, physical therapies, and surgeries.1-3,15-19 Most people with pain after 30 days still have pain 5 years later despite extensive treatment.16-17 Research suggests that risk such as repetitive strain, fear avoidance, depression, poor sleep, stress, maladaptive postures, and ergonomic factors are the major causes of delayed recovery and failed treatment.18-24 Despite recognition that many of these factors can be improved with self-management strategies, they are often not addressed in routine pain care leading to pain persisting for years.1-2,23,26,27 Thus chronic pain has become a major healthcare problem primarily due to our lack of engaging, empowering, and educating patients in reducing the risk factors and enhancing the protective factors to help prevent chronic pain.25-40
New Approach to Chronic Pain
To address the chronic pain problem, a focus on prevention and early intervention of chronic pain is recommended.28,29 A broader conceptual model of chronic pain, new strategies for care delivery, and better ways to educate health professionals are needed. A human systems approach provides a broader understanding of the role of diverse lifestyle risk factors and protective factors in perpetuating chronic pain through recursive feedback cycles that are self-sustaining. These factors can either lead to or prevent progression from acute pain where peripheral tissues such as muscle, joints, and nerves are sensitized to chronic pain or where the brain and the central nervous system become sensitized.39-48 A transformative care model integrates personalized assessments, robust self-management training, and evidence-based treatments to help patients reduce risk factors, enhance protective factors, and reverse the perpetuation of chronic pain.1-3 This can best be implemented through an interdisciplinary integrative team to help support patients in implementing lifestyle changes and long-term improvement in preventing chronic pain. However, these changes require transformation of the healthcare system that would be a challenge for even the most innovative healthcare professional. A first step in this process is to simply teach these new concepts to a broader population of health professionals and patients. The development of MOOCs provides a new avenue for widespread dissemination of this knowledge.
Development of Massive Open Online Courses
Over the past few years, universities have embraced MOOCs as a strategy to spread knowledge, accommodate more students, and lower the cost of higher education.49,50 Table 1 compares teaching strategies between traditional courses and the MOOCs. Traditional online courses charge tuition, carry credit, and limit enrollment to improve interaction with instructors. In contrast, MOOCs are free high-quality noncredit courses that are scalable and open to anyone with an internet connection. As a result, enrollment can accommodate thousands of students at a time, and in this case, thousands of patients and consumers. Since it is massive and open in size, it is a challenge to respond to participant needs on an individual basis, which leads to a poor retention rate. Because of the number of participants, special care in course design, presentation of material, and interactive strategies are important to engage participants.
Table 1.
Differences Between Massive Open Online Course (MOOC) and Traditional Online Course in the Healthcare Curriculum
| Traditional Online Course | MOOC | |
|---|---|---|
| Registrants | 10 to 30 participants | Thousands of participants |
| Teaching method | 45 to 60 minutes lecture | Five to seven 10-minute lecture segments per module |
| Discussion | Interaction with faculty is high | Online discussion forum with other participants; faculty and teaching assistants contribute |
| Homework | Homework is often readings assigned for each lecture | Homework is experiential with videos showing how exercises or other activities are done |
| Timing of course | 1 to 3 hour-long lectures per week | Two self-paced modules presented per week over 10 weeks |
| Cost | Cost per credit | No cost or small cost for continuing education credit |
| Completion rate | 90% | 10% to 20% |
One reason cited for the poor completion rate for MOOCs is the difficulty in effectively achieving student engagement and the ease in enrollment and discontinuing the course.49,50 One avenue to increase active participation is the use of discussion forums and study groups. To date, there has been little evidence collected that would allow an assessment of whether MOOCs can provide a cost-effective mechanism for producing desirable educational outcomes, particularly in healthcare. Furthermore, there have been few MOOCs directed at healthcare providers and even fewer directed to patients to improve their understanding of medical conditions and how to manage them. Thus the team that developed this MOOC on preventing chronic pain considered these goals and evaluated the positive and negative aspects of the initial offering of the course.
METHODS
The MOOC entitled “Preventing Chronic Pain: A Human Systems Approach” was developed to blend clinical and scientific knowledge with didactic, creative, and experiential teaching strategies to help participants better understand chronic pain and how a human systems approach improve prevention and management. There were 4 major objectives to the course. Participants would learn to
understand the prevalence, personal impact, and healthcare dilemma associated with chronic pain;
recognize the clinical characteristics and underlying etiology of several common pain conditions and the peripheral, central, and genetic mechanisms of chronic pain;
analyze the literature associated with risk and protective factors that occur in each aspect of our lives and learn specific strategies that can be employed daily to prevent chronic pain and enhance wellness; and
appreciate the value of a human systems approach to healthcare and how it can provide a basis for integrative, interdisciplinary, and individualized care to preventing pain and enhancing wellness.
The course included 4 sections that corresponded with the objectives. The MOOC was 18 modules, which have been expanded to 20 modules in the follow-up course. Each module provided about 1 hour of instruction and 1 hour of experiential learning per week. Each module consisted of 10 to 15–minute video segments and interactive experiential components. The course completion was defined as participation in each of the 18 modules. The structure of the discussion forums included participants responding to a topic presented by the faculty of the module. The experiential exercise(s) included homework assignments for each module such as assessments and lifestyle changes such as posture, stress, sleep, and diet. A quiz was offered at the end of each module that included about 10 multiple-choice questions that could be completed at any time during the course. A homework essay was also assigned at the end of the course to ask participants to summarize the daily lifestyle changes they made to support preventing chronic pain.
An experienced, interdisciplinary group of faculty from areas of medicine, dentistry, basic science, nursing, public health, and physical therapy served as guest lecturers to discuss their different perspectives on preventing chronic pain. A rich set of strategies that included assessment tools, exercises, and experiential practices were provided. Creative strategies using music videos from the novel The Last Scroll (iUniverse, 2013) by James Fricton were also used to introduce each module in an attempt to broaden engagement and present nonacademic concepts such as balance and moderation in health and wellness.
New Epistemology for Chronic Pain
A new epistemology to understand broader concepts of chronic pain was presented in the course. It follows the assumption that humans are complex, multidimensional, and dynamic and live within an ever-changing social and physical environment. In contrast, the traditional biomedical model is based on a scientific paradigm that is unidimensional, reductionistic, and inflexible, based primarily on understanding the underlying pathophysiology. Healthcare professionals tend to see what they treat and treat what they see. If they see only the pathophysiology, recognition of the complex set of risk and protective factors that interact and play a powerful role in the onset, perpetuation, and progression of an illness may be missed. As a result, success of treatment can be compromised by limited approaches that address only part of the problem. For example, systematic reviews of biomedical treatments for chronic pain have found that even with the most efficacious treatments, improvement is only slightly above that obtained with placebo.36,37 When evidence-based biomedical treatments are combined with robust patient training to reduce risk factors and enhance protective factors, the potential of transforming a person from illness to health and wellness is enhanced.38-40 This is the basis for a transformative model of care.
Transformative Care
The Institute of Medicine's (IOM) 2011 monograph, Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research emphasizes the need for us to transform our current passive model of doctor-centered care into one that is patient-centered.1 The document states, “Health care provider organizations should take the lead in developing educational approaches for people with pain and their families that promote and enable self-management.”1 Transformative care integrates robust self-management training with the best and safest evidence-based treatments. Clinical trials of self-management strategies that activate the patient through exercise and cognitive and behavioral changes have equal or better efficacy than passive treatments in preventing or alleviating chronic pain.27-40 However, when self-management is combined with these evidenced-based biomedical treatments, the outcomes can be dramatically improved while also reducing the patient's dependency on the healthcare system.33,34 Thus, a transformative care model can help transform not only the patient's life but also improve the healthcare system.
Human Systems Approach
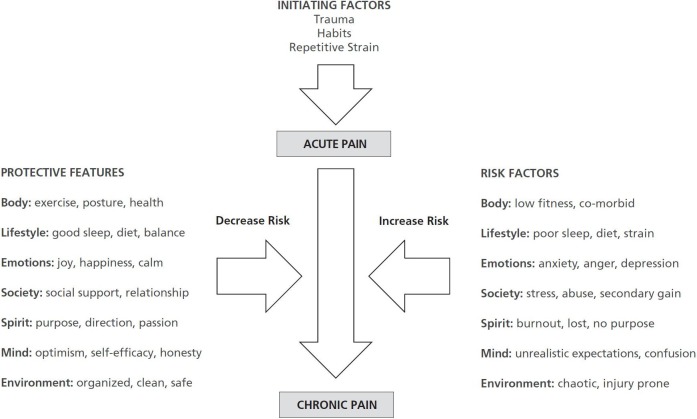
A broader conceptual basis is required for transformative care that includes understanding how different realms of our lives can interact and contribute to chronic pain. A human systems approach includes concepts of neuroplasticity, mind-body connectedness, cybernetics, chaos theory, social psychology, and cognitive-behavioral science to explain this delicate balance between health and illness as described in Table 2 and illustrated in the Figure.40-46 Human systems theory (HST) stems from research in general systems theory and originated in ecology out of the need to explain the interrelatedness of organisms in ecosystems.40-46 While many distinct pathophysiological mechanisms may occur in chronic pain conditions, HST suggest that it is the complex interaction of diverse lifestyle factors that can predispose, initiate, perpetuate, or result from chronic pain or, conversely, protect from and help prevent chronic pain.45,46 HST views a person as a whole with the interrelationship between different realms of their life contributing to this balance as illustrated in the Figure. These realms are not static and independent but rather are dynamic, evolving, and interrelated processes.
Table 2.
Comparison of the Traditional Biomedical Model and a Human Systems Model
| Concept | Biomedical Model | Human Systems Model |
|---|---|---|
| Conceptual basis | Reductionistic, mechanistic, inflexible | Holistic, fluid, flexible |
| Application of scientific methods | Relies on objective physical measures, single brief interventions, and randomized controlled trials | Relies on objective and subjective measures, multiple interventions over longer periods, and pragmatic clinical trials |
| Etiology | Pathophysiological etiology based on single static etiology (eg, infectious agent, structural change, cancer) | Multifactoral dynamic etiology of chronic illness (eg, influence of risk and protective factors on physical tissues) |
| Problem list | Identify chief complaint and diagnoses in the physical or psychiatric realm | Identify chief complaints, diagnoses, and contributing factors in each aspect of life (body, mind, spirit, lifestyle, emotions, environment, and society) |
| Treatment strategy | Unidimensional that encourages single sequential treatments | Multidimensional that integrates multiple interventions with self-management of risk and protective factors |
| Providers | Single clinician providing single intervention that is easy to implement: may lead to fragmented approaches. | Interdisciplinary, integrative team of clinicians that address multiple levels of contributing factors: more complex to implement. |
| Reimbursement | Well supported by traditional healthcare delivery system with an economic model that rewards procedures over process | Will be supported by an evolving healthcare delivery system with economic incentives for patient-centered care |
| Outcomes | Good outcomes with acute conditions. Poor outcomes with chronic illness due fragmentation of multiple single treatments and lack of patient engagement. | Good outcomes with chronic illness due to use of transformative care model with self-management, biomedical interventions, and a team approach to engage patients. |
Figure.
The impact of risk and protective factors in the progression from acute to chronic pain.
The clinical application of transformative care involves identifying and reducing risk factors for chronic pain while also training the patients in improving protective factors (Figure). Transformative care includes the use of personalized assessments to identify risk and protective factors as part of a “whole person” problem list. Personalized care strategies include integrative teams that can be supported by health coaches, social support networks, and consumer-based health information technology for both patient training and documenting outcomes. Since patients often expect to have a passive role in care, these new paradigms need to be conveyed to the patient as part of the evaluation including self-responsibility, education, personal motivation, self-efficacy, social support, strong provider/patient relationships, and long-term change. These paradigms will shift the balance of care from one of a passive, dependent patient to an empowered, engaged, and educated patient.1-2 Ultimately, this shift will not only improve the quality of care but will enhance pain and functional outcomes as well as significantly reduce healthcare costs. In the process, the Institute for Healthcare Improvement's triple aim of improving population health, enhancing the patient care experience (including quality, access, and reliability), and controlling or reducing cost of care will be acheived.47
Data Collection
As part of this MOOC, data were collected to evaluate the characteristics of the MOOC from different perspectives. The online platform Coursera presents a course analytics dashboard that included demographics, geographic location, and background of participants. In addition, educational assessments administered online were used in the course to identify participants' current pain conditions, the status of their risk, and protective factors in each of 7 areas or “realms” of life (body, mind, spirit, lifestyle, emotions, environment, and society), and the goals and strategies to prevent pain, if present. The pain assessment measures were generated based on recommendations from the Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) consortium found at www.immpact.org, which developed consensus recommendations for improving clinical trials of treatment for pain conditions.48 In this study, pain intensity, frequency, duration, and impact were assessed. In addition, scope of symptoms, onset event, frequency of healthcare visits, and self-care strategies were assessed. Finally, a course evaluation was completed after the course to evaluate whether the course met its goals and the quality of the teaching strategy. Each of these provided a dataset for analysis to better understand the impact and function of the course. The University of Minnesota Institutional Review Board approved the secondary use of data for this analysis.
Data Analysis
Characteristics of the participants based in course analytics, educational assessments, and course evaluations were analyzed descriptively. Mean values with standard deviation or frequency distribution were calculated. The brief course evaluation including qualitative data analyzed for key themes addressing use, satisfaction, knowledge, and potential for implementation including challenges and benefits.
RESULTS
The Coursera dashboard showed that 23 650 participants registered for the first version of the course. The registrants who participated in the course included
15 184 who reviewed course material (66.2%),
11 579 who completed at least 1 module including the quiz (49.0%),
5219 who participated in the discussion forums (22.2%),
4352 who participated in an experiential exercise (18.4%),
2435 who participated in the Seven Realms Assessment,
2112 who completed all of the modules (9.0%),
1893 who completed a quiz for each module (8.0%), and
771 who completed the full course evaluation (3.2%).
This significant drop in participations rates does reflect the characteristics of MOOCs in general and limits full data analysis. Yet this sample size is still much larger than traditional university courses and provides some relevant and interesting data.
Demographics
The Coursera dashboard demonstrated that the participants were from nearly every part of the world including 179 different countries (92% of all 195 countries in the world) including 5934 (25%) from emerging and developing countries that do not have broad-based access to higher education courses. Participant demographic data are presented in Table 3. Although the course was predominantly aimed at healthcare professionals and students, it was surprising to discover that the participants also included patients or consumers who were interested in the topic. Thus the participants taking the course included a mix of both health professionals (47%) and patient or consumers interested in pain (53%). The consumers or patients had hoped that the course would provide insight into chronic pain conditions. The inclusion of consumers and patients may have also changed the participant mix. For example, the Coursera dashboard showed a slight majority of participants were female at 57% compared to all other Coursera MOOCs where males (60%) outnumber females (40%). Age distribution included a wide range with most (59%) under the age of 44 years. Most participants (73%) also had a college degree, including 42% with advanced degrees.
Table 3.
Demographic Distribution of Massive Open Online Course Participants
| Gender | Female (57%), male (43%) |
|---|---|
| Age, y | 18-24 (13%) 25-34 (27%) 35-44 (19%) 44-54 (18%) 55-64 (13%) >65 (9%) |
| Education | Doctorate or professional degree (17%) Master's degree (25%) Bachelor's degree (31%) Associate's degree or some college (17%) High school diploma or less (10%) |
| Reason for taking the course | Patient with pain (27%) Health professional (21%) Student of health professions (9%) Researcher interested in pain (6%) Consumer interested in pain (10%) Interested person (27%) Other reason (1%) |
| Top countries represented | United States (36%) Canada (6%) United Kingdom (5%) India (5%) Australia (3%) China (3%) Brazil (2%) Spain (2%) Germany (2%) Greece (2%) Russia (1%) 168 other countries (34%) Emerging Economies (24%) |
Pain Characteristics
Since over half of the participants were patients/consumers, we were able to conduct an analysis of the pain characteristics for the 2435 participants who participated in the Seven Realms Assessment (www.biomedicalmetrics.com/cgi-bin/home.cgi). The data are presented in Table 4. This analysis revealed that only 10.5% had reported they had no pain conditions. In addition, 26.3% of participants reported having neck and back pain and 21.5% reported head, face, ear, and jaw pain. The participants with pain reported their worst pain had a mean severity of 8.2 (0=no pain to 10= highest severity), the mean number of days per month with pain was 14 days, and the mean interference score was 7.1 of 10 (0=no interference with 10=extreme interference). The mean frequency of worst pain was 23 of 30 days with a duration ranging from several hours per day to all day. The most common previous care involved outpatient visits to health professionals with a mean of 9.2 visits in the past year. The top onset events for the pain included “Nothing; it just came on” (42.7%), sports injury (12.1%), and a stressful situation (8.4%).
Table 4.
Personal Assessment of Participants in the Massive Open Online Course (N=2435)
| Gender | Female (57%), male (43%) |
|---|---|
| Pain areas (in order of frequency) | Neck and back (26.3%) Head, jaw, ear, and face (21.5%) Leg, knee, and feet (14.8%) Arm, elbow, and hand (10.5%) Shoulder, chest, abdomen (9.9%) Pelvic area and hip (6.6%) No pain at all (10.5%) |
| Severity of worst pain | Mean pain severity of 8.2 of 10 (SD:2.3) Mean interference score was 7.1 of 10 (SD:2.9) Mean frequency of pain was 14 days of 30 days (SD:11.3) Duration was in hours (category scale of Minutes (1), Hours (2), Days (3), Constant (4) mean of 2.8 with SD of 1.1) |
| Previous care for pain condition | Visits to health professionals in the past year (mean 9.2; SD:15.9) Visits to emergency rooms in the past year (mean 0.4; SD:1.5) Days in the hospital in the past year due to pain (mean 0.4;SD:2.0) Surgeries have you had for the pain (mean 0.4; SD:1.5) |
| Onset event for pain | Nothing, pain just came on (42.7%) Sports injury (12.1%) Stressful situation (8.4%) Home injury (4.7%) Illness (4.4%) Work injury (4.4%) Motor vehicle accident (3.6%) After treatment/surgery (1.8%) After dental care (0.9%) After medication (0.3%), Other (16.4%) |
| Self-care strategies used to reduce pain(in order of frequency) | Stretching exercise, eg, yoga (47.0%) Lying down (45.0%) Hot or cold applications (44.7%) Staying positive in the present moment (44.6%) Maintaining balanced relaxed posture (44.0%) Taking breaks during day (43.3%) Distracting self from the pain (43.0%) Going to sleep (37.8%) Deep breathing (37.3%) Massaging trigger points/muscle knots (37.3%) Conditioning exercise, eg, running or swimming (33%) General massage (30.7%) Long walks (29.1%) Warm baths (28.9%) Strengthening exercise, eg, weights (27.3%) Meditation (28.6%) Practicing calming technique (26.8%) Being alone (26.6%) Socializing or spending time with others (26.2%) Relaxation or self-hypnosis (21%) Being creative (18.4%) Prayer (18.3%) Taking herbs (15.0%) Aromatherapy (9.5%) |
Self-care Strategies
The participants (N=2435) used a variety of self-care strategies for their pain as listed in Table 4. The most common self-care strategies to prevent chronic pain included stretching exercise (eg, yoga [47%]), lying down (45%), hot or cold applications (44.7%), staying positive in the present moment (44.6%), maintaining balanced relaxed posture (44%), activities that distract from the pain (43%), and taking breaks during day (43%).
Course Evaluation
A course evaluation was also completed by 771 participants (3% of total) with 93% of these respondents completing the entire course. Overall, the experiences of the course were satisfying (91% agreed); the course met the objectives (92% agreed) and was relevant and applicable to daily life (91% agreed). Of the participants with pain, 93% believed the course changed their lives (n=516) and 85% health-provider participants believed that it changed the care of their patients (n=300). The quality of each course element was rated very good to excellent, including the video lectures (95%), speakers (91%), experiential training exercise (82%), quizzes (82%), self-assessments (75%), handouts (68%), music video introductions (66%), and discussion forums (56%).
Self-care Strategies
Comments about the MOOC included the following.
“The learning experience has been tremendous!! Everyone should have this knowledge, especially those in the health profession.”
“Absolutely fascinating and enlightening. This information should be part of every healthcare educational program! ”
“This course has really helped me to understand myself better and why I think, act and see the world as I do.”
“I am eternally grateful for taking the time and energy to provide this beacon of knowledge to the world.”
“I think this course is a wonderful gift, because pain is an avoidable part of our life. I have learned so many things.”
There were also some constructive criticisms.
“Way too technical. I understand it can be a complicated topic, but it was way over my head. I think a lot of the students felt similar.”
“The course tried to be too many things to too many people. It needs division into clinical provider and consumer segments. Also, the high number of instructors made the quality of the information provided vary too much.”
“Need more input from other medical professionals such as orthopedic surgeons.”
DISCUSSION
This is the first offering of a MOOC on preventing chronic pain and the first that included patients as participants, attesting to the great interest in the topic. It is clear from the 2011 Institute of Medicine report on chronic pain in America that more effort is needed on prevention and early intervention of chronic pain.1 To this end, there were several key concepts that made the course compelling to both health professionals and people with pain. They included the following concerns.
Since chronic pain is the top reason for patients to seek care and the top cause of increased disability, addiction, and healthcare costs, we need more effort in preventing chronic pain to transform the health-care system from primarily doctor-centered passive care to more patient-centered transformative care.
Preventing chronic pain includes preventing the onset of chronic pain, the progression of acute to chronic pain, and the progression from chronic to intractable pain. Each is important in the big picture of chronic pain.
Understanding the whole person with chronic pain and all of their risk and protective factors is critical to successful prevention and care. Unaddressed risk factors often lead to delayed recovery or treatment failure. Thus using a broader conceptual basis with a human systems approach can shift the focus to more patient-centered transformative care paradigms.
Improving the safety of treatments will minimize chronic pain as an adverse event. This is particularly true of treatments such as surgery, injections, chronic opioid use, and multiple conflicting medications.
Recognizing that fear of pain flares and avoidance of physical and social activities may lead to delayed recovery and more chronic pain needs to be addressed.
Implementing a transformative care model that integrates robust self-management training with evidence-based pain treatments through a team approach will improve quality of care and patient outcomes while reducing dependency on the healthcare system and healthcare costs. Teams of healthcare professionals that include a patient-centered health coach will play a growing role in most health reform efforts by supporting patients in self-management.
To teach these innovative healthcare concepts in preventing chronic pain, the MOOC was successful in providing a new format for training large numbers of both patients and healthcare providers about the challenges of chronic pain. Furthermore, the course had a broad impact on participants with 93% believing it changed their lives and 85% of healthcare providers believing it changed their care of patients. This is significant considering the extensive reach of a course with 11 579 participants learning from at least 1 module. To put this into perspective for a teaching faculty, the MOOC included more students than are typically taught in an entire 30-year teaching career.
There were many other advantages to the MOOC platform. The no-cost feature and self-paced nature of the modules attract participants who normally have limited funds or time to participate. The ability to take the course in any setting with an online computer extended the reach to an international community of participants. The ability to provide both didactic and experiential online lessons allowed a more engaging strategy for learning than a lecture-only format.
There were also disadvantages to the MOOC. A frequent criticism of all MOOCs is the low completion rate for the course.49,50 Since there is no cost, the challenge of integrating a university-level course into a busy daily life is sometimes too much for participants, who frequently drop out. In this course, of the 23 650 participants who joined the course, only 49% or 11 579 participated in more than 1 module and only 2112 completed all modules. Most MOOC attrition happens after students first register for a course, with more than 50% of people leaving within 2 weeks of course initiation. After that window, attrition rates decrease substantially. This also lead to a lower percentage of participants who filled out the course evaluation (n=771) because it was offered at the end of the course. However, this still reflects a high number compared to other university courses but may have biased the sample to be more positive about the course.
Another weakness is the difficulty in tailoring the learning to the level of each participant's knowledge, training, and cultural background. Since this was a course in English, those who are not fluent in English had difficulty. A global translator community is part of Coursera and works to make the educational content such as this course accessible across geographic and linguistic boundaries.
As some participants noted, some of the modules were too technical for them to understand and others were less relevant to their interest. As noted, about half of the students were people with chronic pain and the other half were health professionals with a wide diversity of knowledge levels. This can happen within in-person or professional online courses also. However, both the patients and health professionals who completed the course and the evaluations (3%) felt they gained from taking the MOOC, with 92% of participants who completed believed the MOOC met its objectives. Thus we believe the goal of expanding knowledge on preventing chronic pain was accomplished. This was reinforced by the fact that 14 942 participants registered for a second course held later during the year with 10 173 (69%) completing at least 1 module, compared to 49% in the first course. We conclude that there is strong growing interest in this course and in preventing chronic pain.
Despite the low retention rate in the course, the number of participants is still large and can have a potentially large impact. Demographic information about registrants can be misleading without context. Although the most typical MOOC course registrant is male with a bachelor's degree 26 years or older, this course drew in a different group of participants: more women, all age groups, and all educational backgrounds. Most participants were international, with a full quarter from emerging or developing countries where higher education may not be available.49,50 Thus these MOOCs are reaching many nontraditional and underserved communities, very different from typical students on campuses at traditional universities. The potential for a great international impact is high.
Although there were both advantages and disadvantages to the MOOC format for this course, the general rise of MOOCs has encouraged pedagogical research, extended the reach of educators, and disseminated information to the general population who may not otherwise have access to this knowledge.50,51 These new teaching strategies may provide faculty with more flexibility and offer novel opportunities to gather data as in this paper. Likewise, online learning platforms put students in the driver's seat, allowing an individual to engage in a manner that best suits his or her personal needs. To some extent, this kind of course represents the democratization of learning where knowledge is open to anyone and learners are in control. It is hoped that this will also lead to a better understanding of how people learn, how universities may educate them better, and how to make education scalable. It is also hoped that this research will serve as a benchmark for future studies on MOOCs, support studies in the science of learning (particularly in healthcare), and assist the expansion of consumer education on health issues.
Future Directions
There was sufficient interest in this initial offering of the course to repeat it in the same year and in future years. Based on the results of the evaluation, a number of revisions were made as part of a second offering of the course in 2015. Data from the additional 14 942 participants who took the course will be analyzed and compared to the data from the first offering. Since the course was originally designed for health professionals, we are also developing patient-centered online training programs that are based on the concepts and results of this MOOC.
In addition, we are initiating more effort on preventing chronic pain through The People's Campaign for Preventing Chronic Pain at www.preventingchronicpain.org.49 The goal of this campaign is three-fold.
Research on preventing chronic pain with the development of the Chronic Pain Research Network as well as developing strategies and tools that health professionals can use to improve their prevention and early management of chronic pain conditions.
Education of both patients and health professionals on how to prevent chronic pain using self-management and transformative care.
Advocacy to increase awareness and provide tools to health plans, businesses, government agencies, and communities to improve their efforts in preventing chronic pain.
As part of this effort, online training specific to patients, consumers, and employees is in progress. This will also ensure that the quality, format, and delivery of each module are consistent across the course for these key participants.
CONCLUSION
Chronic pain conditions are the primary reason patients seek healthcare, the most common reason for disability and addiction, and highest driver of healthcare costs. Care of chronic pain patients costs more than cancer, heart disease, and diabetes care combined. This article presents the results of a University of Minnesota MOOC with thousands of participants who joined in an effort to broaden the teaching on the prevention of chronic pain. The results of the MOOC data suggest that the course was successful in accomplishing its goals of improving education on the concepts of chronic pain prevention for both patients and health professionals. By accomplishing these goals, we will address the Institute for Healthcare Improvement's triple aim to improve the patient's experience of care, enhance the health of the patient, and reduce the cost of healthcare.47
Acknowledgments
The authors would like provide a special thanks to Annette McNamara, David Lindeman, Jane O'Brien, Kristi Jensen, Robert Rubinyi, PhD, and the rest of the development staff at the University of Minnesota Office of Information Technology and Center for Educational Innovation who made the development of this course possible.
Disclosures The authors completed the ICMJE Form for Potential Conflicts of Interest and had no conflicts to disclose.
Contributor Information
James Fricton, University of Minnesota, Minneapolis, HealthPartners Institute for Education and Research, Minnesota Head and Neck Pain Clinic, St Paul, International Myopain Society, Nine Mile Falls, Washington, United States (Dr Fricton).
Kathleen Anderson, University of Minnesota, Minneapolis, United States (Dr Anderson).
Alfred Clavel, HealthPartners Institute for Education and Research, Minnesota Head and Neck Pain Clinic, St Paul, United States (Dr Clavel).
Regina Fricton, Statistical Analysis, Edina, Minnesota, United States (Ms Fricton).
Kate Hathaway, University of Minnesota, Minneapolis, Minnesota School of Professional Psychology, Minneapolis, St Catherine University, Minneapolis, United States (Dr Hathaway).
Wenjun Kang, Bioinformatics, Education Management, University of Chicago, Illinois, United States (Mr Kang).
Bernadette Jaeger, University of California, Los Angeles, United States (Dr Jaeger).
William Maixner, University of North Carolina, Chapel Hill, United States (Dr Maixner).
Daniel Pesut, University of Minnesota, Minneapolis, United States (Pesut).
Jon Russell, Department of Medicine, Division of Clinical Immunology, University of Texas Health Science Center, Houston, Texas, United States (Dr Russell).
Mark B. Weisberg, Minnesota Head and Neck Pain Clinic, St Paul, United States (Dr Weisberg); Center for Spirituality and Healing, University of Minnesota, United States (Dr Weisberg).
Robin Whitebird, HealthPartners Institute for Education and Research, United States (Dr Whitebird).
REFERENCES
- 1.Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press: 2011. [PubMed] [Google Scholar]
- 2.The Mayday Fund. A call to revolutionize chronic pain care in America: an opportunity in health care reform. New York: Mayday Fund; 2009. [Google Scholar]
- 3.PAINS. Fostering innovative state & community-based initiatives. http://www.painsproject.org/our-work/fostering-innovative-community-based-initiatives/. Accessed July 27, 2015.
- 4.St Sauver J L, Warner DO, Yawn BP. et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined American population. Mayo Clin Proc. 2013. January;88(1):56–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. The Surgeon General's call to action to improve the health and wellness of persons with disabilities. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2005. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009. May 1;58(16):421–6. [PubMed] [Google Scholar]
- 7.US Centers for Disease Control and Prevention. Injury prevention and control: prescription drug overdose. http://www.cdc.gov/drugoverdose/. Accessed July 27, 2015.
- 8.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013 Feb 20;309(7):657–9 [DOI] [PubMed] [Google Scholar]
- 9.Berland D, Rodgers P. Rational use of opioids for management of chronic nonterminal pain. Am Fam Physician. 2012. August 1;86(3):252–8. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC). Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011. November 4;60(43):1487–92. [PubMed] [Google Scholar]
- 11.Dunn KM, Saunders KW, Rutter CM. et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010. January 19;152(2):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bohnert AS, Valenstein M, Bair MJ. et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011. April 6;305(13):1315–21. [DOI] [PubMed] [Google Scholar]
- 13.US Centers for Disease Control and Prevention. Injury prevention & control: data and statistics (WISQARSTM). http://www.cdc.gov/injury/wisqars/fatal.html. Accessed July 27, 2015.
- 14.Preventing chronic pain: a human systems approach. http://www.coursera.org/course/chronicpain. Accessed July 27, 2015. [DOI] [PMC free article] [PubMed]
- 15.Deyo RA, Mirza SK, Turner JA, Martin BI. Over-treating chronic back pain: time to back off? J Am Board Fam Med. 2009;22(1):62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hestbaek L, Leboeuf-Yde C, Manniche C. Low-back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003. April;12(2):149–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. 2000 Fall;14(4):310–9. [PubMed] [Google Scholar]
- 18.Bigos SJ, Battie MC, Spengler DM, Fisher LD, Fordyce WE, Hansson T, Nachemson AL, Zeh J. A longitudinal, prospective study of industrial back injury reporting. Clin Orthop Relat Res. 1992. June;(279):21–34. [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin D, Conrad D, Volinn E. Cost, controversy, crisis: low back pain and the health of the public. Annu Rev Public Health. 1991;12: 141–56. [DOI] [PubMed] [Google Scholar]
- 20. Bigos SJ, Holland J, Holland C, Webster JS, Battie M, Malmgren JA. High-quality controlled trials on preventing episodes of back problems: systematic literature review in working-age adults. Spine J. 2009. February;9(2):147–68. [DOI] [PubMed] [Google Scholar]
- 21.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002. March 1; 27(E):E109–20. [DOI] [PubMed] [Google Scholar]
- 22.Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol. 2002. June;70(3):678–90. [DOI] [PubMed] [Google Scholar]
- 23.Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007. February;127(3):276–86. [DOI] [PubMed] [Google Scholar]
- 24.Gensichen J, von Korff M, Peitz M. et al. ; PRoMPT (PRimary care Monitoring for depressive Patients Trial). Case management for depression by health care assistants in small primary care practices. Ann Intern Med. 2009. September 15; 151(6):369–78. [DOI] [PubMed] [Google Scholar]
- 25.Fricton J. The need for preventing chronic pain: the “big elephant in the room” of healthcare. Global Adv Health Med. 2015. January;4(1):6–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Childs JD, Fritz JM, Flynn TW. et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004. December 21; 141(12):920–28. [DOI] [PubMed] [Google Scholar]
- 27.Coleman E, Parry C, Chalmers S, Min S. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006. September 25; 166(17):1822–8. [DOI] [PubMed] [Google Scholar]
- 28.Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev. 2007. October 17;(4):CD005108. [DOI] [PubMed] [Google Scholar]
- 29.Bair MJ, Matthias MS, Nyland KA. et al. Barriers and facilitators to chronic pain self-management: a qualitative study of primary care patients with comorbid musculoskeletal pain and depression. Pain Med. 2009. October;10(7):1280–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Macea DD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010. October;11(10):917–29. [DOI] [PubMed] [Google Scholar]
- 31.Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004. November 10; 6(4):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paul CL, Carey ML, Sanson-Fisher RW, Houlcroft LE, Turon HE. The impact of web-based approaches on psychosocial health in chronic physical and mental health conditions. Health Educ Res. 2013. June;28(3):450–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011. July 13; 13(3):e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005. May 3; 142(9):776–85. [DOI] [PubMed] [Google Scholar]
- 35.Eaton LH, Doorenbos AZ, Schmitz KL, Carpenter KM, McGregor BA. Establishing treatment fidelity in a web-based behavioral intervention study. Nurs Res. 2011. Nov-Dec;60(6):430–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chou R, Huffman LH; American Pain Society; American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007. October 2; 147(7):492–504. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Krebs EE, Bair MJ. Pharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviews. Gen Hosp Psychiatry. 2009. May-Jun;31(3):206–19. [DOI] [PubMed] [Google Scholar]
- 38.Devineni T, Blanchard EB. A randomized controlled trial of an internet-based treatment for chronic headache. Behav Res Ther. 2005. March;43(3):277–92. [DOI] [PubMed] [Google Scholar]
- 39.Lorig KR, Sobel DS, Stewart AL. et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999. January;37(1):5–14. [DOI] [PubMed] [Google Scholar]
- 40.Flor H1, Braun C, Elbert T, Birbaumer N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci Lett. 1997. March 7; 224(1):5–8. [DOI] [PubMed] [Google Scholar]
- 41.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977. April 8; 196(4286):129–36. [DOI] [PubMed] [Google Scholar]
- 42.Mansour M. Systems theory and human science. Annu Rev Control. 2002;26(1):1–13 [Google Scholar]
- 43.Bailey KD. Living systems theory and social entropy theory. Syst Res Behav Sci. 2006;22(3):291–300. [Google Scholar]
- 44.Bateson G. Mind and nature: a necessary unity: advances in systems theory, complexity, and the human sciences. New York: Hampton Press; 1979. [Google Scholar]
- 45.Rolland JS. Chronic illness and the life cycle: a conceptual framework. Fam Process. 1987. June;26(2):203–21. [DOI] [PubMed] [Google Scholar]
- 46.Dym D. The cybernetics of physical illness. Fam Process. 1987. March;26(1):35–48. [DOI] [PubMed] [Google Scholar]
- 47.Institute for Healthcare Improvement. Initiatives: IHI triple aim. http://www.ihi.org/offerings/Initiatives/TripleAim. Accessed July 27, 2015.
- 48.Dworkin RH, Turk DC, Farrar JT. et al. ; IMMPACT. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005 Jan;113(1-2):9–19.. [DOI] [PubMed] [Google Scholar]
- 49.Preventing Chronic Pain. The problem. https://www.preventingchronicpain.org/drupal/pcpnet/problem. Accessed July 27, 2015.
- 50.Ho AD, Chuang I, Reich J. et al. HarvardX and MITx: 2 years of open online courses, Fall 2012-Summer 2014. http://dspace.mit.edu/bitstream/handle/1721.1/96825/SSRN-id2586847.pdf?sequence=1. Accessed July 27, 2015.
- 51.Liyanagunawardena TR, Adams AA, Williams SA. MOOCs: a systematic study of the published literature 2008-2012. Int Rev Res Open Distrib Learn. 2013;14(3).http://www.irrodl.org/index.php/irrodl/article/view/1455/2531\ [Google Scholar]