Abstract
Thyroid diseases have an anesthetic implication that includes difficult airway management, uncontrolled hyperthyroidism, hypothyroidism and postthyroidectomy complications. Securing airway: Intubation and extubation both require skillful management and timely decision to reduce morbidity and mortality in the case of large goiter with retrosternal extension that leads to tracheal compression and deviation. We present the anesthetic management in a patient with a large goiter with retrosternal extension leading to tracheal compression and deviation. We managed the case with an awake fiberoptic intubation and guided extubation.
Keywords: Difficult airway, fiberoptic intubation, goiter, retrosternal extension
INTRODUCTION
Diseases of the thyroid like goiters still exist in many endemic parts of the world.[1] Enlargement of the thyroid gland is due to iodine deficiency in 90% of cases and 10% due to selenium deficiency in the African countries like Sudan, Tanzania, South Africa, Zaire, etc.[2] A large goiter did compress and deviate the trachea causing breathing difficulty, swallowing difficulty in our patient that made intubation and extubation both difficult. In addition to endocrine and metabolic effects, the mass extends sub-sternally which makes more challenges for the anesthesiologist to manage the airway. Up to 45% of goiter patients may have a sub-sternal component.[3]
Several techniques are available to select the level of obstruction however it depends on the anesthesiologist's expertise and familiarity. We describe here the presentation, diagnosis, peri-operative management and outcome of the patient who was managed with an awake fiberoptic intubation and guided extubation.
CASE REPORT
A 52-year-old patient was admitted to our hospital with very large swelling in the midline and both sides of the neck since >8 years. It was extending from chin to the sternum with retrosternal extension. His symptoms started 15 years ago with palpitations, tremors, and increase in appetite and weight loss. He had a history of proximal myalgia that increased progressively over the years. His swelling was small initially and increased in size progressively with change in voice and subsequent hoarseness. When the swelling became large, he was experiencing symptoms of compression that is, shortness of breath and dysphagia. Gradually, he had increased shortness of breath when he was lying supine, so he adopted the lateral position while he sleeps. He had type II diabetes mellitus and factor VIII deficiency. The factor VIII deficiency was hereditary as per his family history. There was no history of bleeding or history of blood or factor VIII transfusion. He was treated for thyrotoxicosis in his native country.
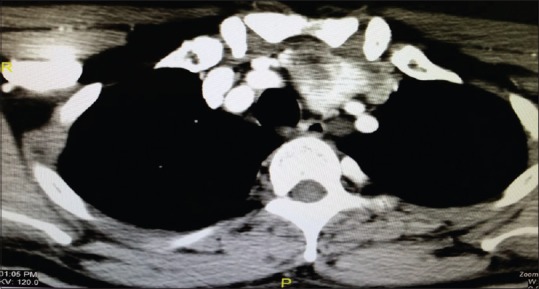
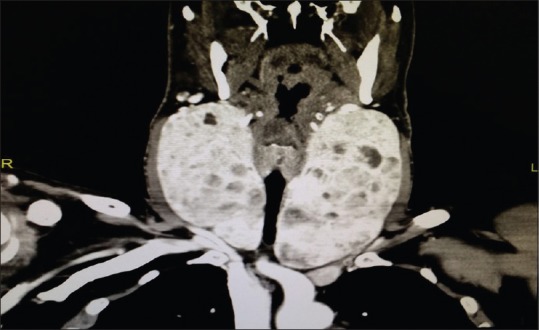
On examination, he was stable. There was a huge swelling anterior and at both sides of the neck which was lobulated and cystic on palpation [Figure 1]. Swelling was extending retrosternally. There was no obvious resting tremor, no exophthalmos, no lid lag and no palpable lymph nodes. Thyroid function test was suggestive of hyperthyroidism. On ultrasound and computed tomography (CT) scan examination it was shown that the right and left lobe size of the thyroid gland was 8.3 cm × 7.8 cm × 13 cm and 7.3 cm × 7.4 cm × 13.9 cm respectively. There were compression and deviation of the trachea [Figure 2] and marked extension of the left lobe retrosternally into the superior mediastinum with displacement of the great vessels [Figures 3-5]. He was on carbimazole 20 mg, propranolol 80 mg both 2 times a day and sitagliptin 50 mg + metformin 500 mg twice daily. Diagnosis was a huge multinodular toxic goiter. ENT consultation via fiberoptic examination was done which showed normal bilateral vocal cord movement. He was preoperatively started on Lugol's iodine. Hematology and endocrine consultation were done. Diabetes was well controlled, and factor VIII was reserved if in need.
Figure 1.

Neck swelling-thyroid
Figure 2.
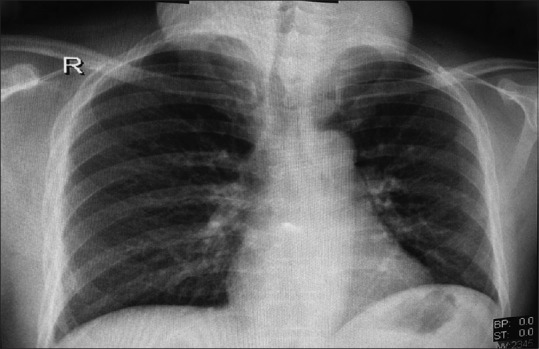
Chest X-ray showing deviation and compression of the trachea
Figure 3.
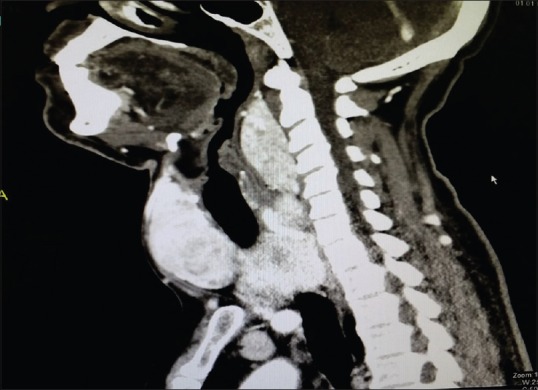
Computed tomography scan (lateral view) showing retrosternal extension
Figure 5.
Computed tomography scan showing retrosternal extension
Figure 4.
Computed tomography scan (Anterior view) showing retrosternal extension
Awake fiberoptic intubation was the preferred choice of airway management in this patient. Detailed procedure of an awake intubation was explained to the patient and written informed consent for procedure and publication was taken. Preparation of patient was started with 2% lignocaine gargles in the ward as 4% viscous lignocaine solution was not available. Patient was taken to the theatre, and all the routine monitoring was applied. The difficult intubation cart was kept ready. A flexometallic endotracheal (ET) tube number: 7 mm internal diameter was loaded on to the well-lubricated Karl Storz® fiberscope. The fiberscope was advanced through the oral route with the help of the Ovassapian airway. When the larynx was visualized, topical anesthesia of the larynx and trachea was applied via “spray as-you-go” technique through the drug channel of the bronchoscope using 3 ml of lidocaine 2% in increments. The fiberscope was advanced into the larynx and trachea gradually till the level of the carina. The flexometallic tube was “railroaded” on the fiberscope into the larynx and at the same time induction of anesthesia was done with fentanyl and propofol. ET tube position was confirmed through fiberscope, and clinically by chest auscultation and capnography [Figure 6]. Total lignocaine dose was kept <4.5 mg/kg. Patient was maintained on cisatracurium, remifentanil infusion and sevoflurane/oxygen-air mixture. Total thyroidectomy was done [Figure 7]. An awake gradual extubation was done after leak test and patient was reversed with neostigmine and glycopyrrolate. Postextubation, bilateral vocal cord movement was checked with glidescope that was normal. Patient was kept in surgical Intensive Care Unit for observation in the postoperative period. Pain management was given via multimodal analgesia.
Figure 6.

After intubation
Figure 7.

Postthyroidectomy specimen
DISCUSSION
In some parts of the world, thyroid diseases are common due to deficiency of iodine with an incidence of 10–15% in adult populations.[1] Anesthetic management of a patient with goiter depends on the size of the goiter, vascularity, compression on the surrounding organs and sub-sternal extension. This requires careful preanesthetic assessment of the patient with symptoms and control of the disease, airway assessment, blood investigations and imaging studies. WHO has classified goiter according to the size, according to which Class 0-palpable mass within neck structure and Class I-visible, palpable and undermines the curves and the neck line. Class II is a very large goiter with retrosternal extension that makes the tracheal deviation, compression of trachea and esophagus.[2]
Our patient was having a very large goiter [Figures 1 and 3-5] Class II type as per WHO classification. He was from a part of Sudan, which is endemic for iodine deficiency. He presented with symptoms of palpitation, increased appetite, weight loss and change of voice initially. He also had difficulty in breathing in the supine position and dysphagia to solids over a period of 5 years, as the size of the mass increased. Up to 45% of goiter patients may have a sub-sternal component.[3] The large goiter compresses on the tracheal diameter of >70% of patients, which leads to dyspnea at rest, and then symptoms of dysphagia.[4,5] And, above all, the symptoms also suggest that there was a retrosternal extension’ present in our patient.
There are multiple modalities to manage the difficult airway in the patient with thyroid enlargement however it depends on the anesthesiologist's expertise and familiarity. If the enlargement is small, and there is no deviation or compression, and if the airway examination is normal, then we would proceed for a normal airway management. Bouaggad et al. found in his study that there was an easy tracheal intubation in 36.9% patients and mild tracheal difficult intubation in 57.8% patients. However, 5.3% patients have moderate to major difficult airway.[2,6]
Preoperative imaging studies [Figure 2] gives us details of the tracheal deviation (tracheal shift of 1 cm from midline), degree of tracheal compression (<30% narrowing of tracheal diameter) and tracheal cartilage erosion suggestive of tracheomalacia.[2] Keeping the clinical symptoms in mind and imaging studies, our patient was in need of an awake fiberoptic intubation. This can prevent conditions like “can’t ventilate and can’t intubate” scenarios occurring after induction of anesthesia due to a complete tracheal collapse. In this condition, lifting of the thyroid mass or rigid bronchoscopy can only help keep the airway patent.[7] Direct laryngoscopy has no role in this situation.
An awake fiberoptic intubation avoids tracheostomy and its complications in these patients. Tracheostomy was not planned in our case, because of the anatomical restrictions. The goiter was very large and extended retrosternally. Blind nasal endotracheal intubation needs inhalational induction, which may lead to total airway obstruction. Multiple attempts and trauma to the airway that leads to infrequent success in blind intubation was mentioned by Ovassapian et al. in their study.[8]
Keeping in mind of the advantages and drawbacks of all procedures for management of the difficult airway, we managed the case with an awake fiberoptic intubation. Saxena et al. mentioned that awake fiberoptic intubation prevents much bleeding and edema that leads to higher success of airway management.[9] Sendasgupta et al. and Tan and Esa stated in their studies that awake fiberoptic intubation offers more hemodynamic stability, better patient tolerance and patency of the airway.[10,11] Ghai et al. suggested that early fiberoptic intubation should be planned when there is suspicion of significant airway obstruction.[7,12] Eldawlatly et al. stated that the success of awake fiberoptic is based on preoperative airway assessment that predict difficult airway, proper planning, and it is well-tolerated if explanation is given to the patient about procedure, risk and comorbidities.[13] Eldawlatly et al. had also stated that the airway access under local anesthesia constitutes better alternative to failed fiberoptic intubation.[14]
An awake extubation is as important as awake intubation in the case of a large goiter with chronicity. Chronic, huge goiters cause tracheal cartilage erosion and tracheomalacia postextubation. Preoperative CT scan studies will enable us to assess the degree of tracheal cartilage erosion. Though there were no signs on imaging study in our case, we decided to go for a gradual awake extubation after the leak test.[15,16]
CONCLUSION
A single universal technique of intubation may not be favorable in all circumstances. Careful selection of technique has been done as per risk versus benefit of various available techniques based on available evidence-based studies. Proper preoperative airway assessment, preparation and timely decision and skillful management reduce the morbidity and mortality in difficult airway cases involving thyroid enlargement.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Farling PA. Thyroid disease. Br J Anaesth. 2000;85:15–28. doi: 10.1093/bja/85.1.15. [DOI] [PubMed] [Google Scholar]
- 2.Bartolek D, Frick A. Huge multinodular goiter with mid trachea obstruction: Indication for fiberoptic intubation. Acta Clin Croat. 2012;51:493–8. [PubMed] [Google Scholar]
- 3.Hegedüs L, Bonnema SJ. Approach to management of the patient with primary or secondary intrathoracic goiter. J Clin Endocrinol Metab. 2010;95:5155–62. doi: 10.1210/jc.2010-1638. [DOI] [PubMed] [Google Scholar]
- 4.Dy B, Wise K, Farley D, McGlinch B. Extreme tracheal compression due to substernal goiter: Surgical and Anesthetic management. World J Endocr Surg. 2012;4:71–3. [Google Scholar]
- 5.Netterville JL, Coleman SC, Smith JC, Smith MM, Day TA, Burkey BB. Management of substernal goiter. Laryngoscope. 1998;108:1611–7. doi: 10.1097/00005537-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Bouaggad A, Nejmi SE, Bouderka MA, Abbassi O. Prediction of difficult tracheal intubation in thyroid surgery. Anesth Analg. 2004;99:603–6. doi: 10.1213/01.ANE.0000122634.69923.67. [DOI] [PubMed] [Google Scholar]
- 7.Ambareesha M, Upadhya M, Ranjan RK, Kamath S. Pre-operative fibreoptic endoscopy for management of airway in huge thyroid. Indian J Anaesth. 2003;47:489–90. [Google Scholar]
- 8.Ovassapian A, Tuncbilek M, Weitzel EK, Joshi CW. Airway management in adult patients with deep neck infections: A case series and review of the literature. Anesth Analg. 2005;100:585–9. doi: 10.1213/01.ANE.0000141526.32741.CF. [DOI] [PubMed] [Google Scholar]
- 9.Saxena KN, Kumar S, Taneja B, Gaba P. Awake fibreoptic intubation in the sitting position in a patient with a huge goitre. Case Rep Anesthesiol 2011. 2011 doi: 10.1155/2011/352672. 352672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sendasgupta C, Sengupta G, Ghosh K, Munshi A, Goswami A. Femoro-femoral cardiopulmonary bypass for the resection of an anterior mediastinal mass. Indian J Anaesth. 2010;54:565–8. doi: 10.4103/0019-5049.72649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan PC, Esa N. Anesthesia for massive retrosternal goiter with severe intrathoracic tracheal narrowing: The challenges imposed - A case report. Korean J Anesthesiol. 2012;62:474–8. doi: 10.4097/kjae.2012.62.5.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghai A, Hooda S, Wadherra R, Garg N. Gross tracheal deviation: Airway challenges and concerns – Two case reports. Acta Anaesthesiol Belg. 2011;62:203–6. [PubMed] [Google Scholar]
- 13.Eldawlatly A, Alsaif A, AlKattan K, Turkistani A, Hajjar W, Bokhari A, et al. Difficult airway in a morbidly obese patient with huge goiter: A case report and review of literature. [Last accessed on 2015 Feb 08];Internet J Anesthesiol. 2006 13:1. Available from: https://www.ispub.com/IJA/13/1/8490 . [Google Scholar]
- 14.Eldawlatly A, Takrouri M, Elbakry A, Ashour M, Kattan K, Hajjar W, et al. Perioperative management of huge goiter with compromized airway. [Last accessed on 2015 Feb 08];Internet J Anesthesiol. 2002 7:2. Available from: https://www.ispub.com/IJA/7/2/3451 . [Google Scholar]
- 15.Fisher MM, Raper RF. The ‘cuff-leak’ test for extubation. Anaesthesia. 1992;47:10–2. doi: 10.1111/j.1365-2044.1992.tb01943.x. [DOI] [PubMed] [Google Scholar]
- 16.Srivastava D, Dhiraaj S. Airway management of a difficult airway due to prolonged enlarged goiter using loco-sedative technique. Saudi J Anaesth. 2013;7:86–9. doi: 10.4103/1658-354X.109829. [DOI] [PMC free article] [PubMed] [Google Scholar]


