Abstract
Background
Diarrhoea accounts for 1.8 million deaths in children in low‐ and middle‐income countries (LMICs). One of the identified strategies to prevent diarrhoea is hand washing.
Objectives
To assess the effects of hand washing promotion interventions on diarrhoeal episodes in children and adults.
Search methods
We searched the Cochrane Infectious Diseases Group Specialized Register (27 May 2015); CENTRAL (published in the Cochrane Library 2015, Issue 5); MEDLINE (1966 to 27 May 2015); EMBASE (1974 to 27 May 2015); LILACS (1982 to 27 May 2015); PsycINFO (1967 to 27 May 2015); Science Citation Index and Social Science Citation Index (1981 to 27 May 2015); ERIC (1966 to 27 May 2015); SPECTR (2000 to 27 May 2015); Bibliomap (1990 to 27 May 2015); RoRe, The Grey Literature (2002 to 27 May 2015); World Health Organization (WHO) International Clinical Trial Registry Platform (ICTRP), metaRegister of Controlled Trials (mRCT), and reference lists of articles up to 27 May 2015. We also contacted researchers and organizations in the field.
Selection criteria
Individually randomized controlled trials (RCTs) and cluster‐RCTs that compared the effects of hand washing interventions on diarrhoea episodes in children and adults with no intervention.
Data collection and analysis
Three review authors independently assessed trial eligibility, extracted data, and assessed risk of bias. We stratified the analyses for child day‐care centres or schools, community, and hospital‐based settings. Where appropriate, incidence rate ratios (IRR) were pooled using the generic inverse variance method and random‐effects model with 95% confidence intervals (CIs). We used the GRADE approach to assess the quality of evidence.
Main results
We included 22 RCTs: 12 trials from child day‐care centres or schools in mainly high‐income countries (54,006 participants), nine community‐based trials in LMICs (15,303 participants), and one hospital‐based trial among people with acquired immune deficiency syndrome (AIDS) (148 participants).
Hand washing promotion (education activities, sometimes with provision of soap) at child day‐care facilities or schools prevents around one‐third of diarrhoea episodes in high income countries (rate ratio 0.70; 95% CI 0.58 to 0.85; nine trials, 4664 participants, high quality evidence), and may prevent a similar proportion in LMICs but only two trials from urban Egypt and Kenya have evaluated this (rate ratio 0.66, 95% CI 0.43 to 0.99; two trials, 45,380 participants, low quality evidence). Only three trials reported measures of behaviour change and the methods of data collection were susceptible to bias. In one trial from the USA hand washing behaviour was reported to improve; and in the trial from Kenya that provided free soap, hand washing did not increase, but soap use did (data not pooled; three trials, 1845 participants, low quality evidence).
Hand washing promotion among communities in LMICs probably prevents around one‐quarter of diarrhoea episodes (rate ratio 0.72, 95% CI 0.62 to 0.83; eight trials, 14,726 participants, moderate quality evidence). However, six of these eight trials were from Asian settings, with only single trials from South America and sub‐Saharan Africa. In six trials, soap was provided free alongside hand washing education, and the overall average effect size was larger than in the two trials which did not provide soap (soap provided: rate ratio 0.66, 95% CI 0.56 to 0.78; six trials, 11,422 participants; education only: rate ratio: 0.84, 95% CI 0.67 to 1.05; two trials, 3304 participants). There was increased hand washing at major prompts (before eating/cooking, after visiting the toilet or cleaning the baby's bottom), and increased compliance to hand hygiene procedure (behavioural outcome) in the intervention groups than the control in community trials (data not pooled: three trials, 3490 participants, high quality evidence).
Hand washing promotion for the one trial conducted in a hospital among high‐risk population showed significant reduction in mean episodes of diarrhoea (1.68 fewer) in the intervention group (Mean difference 1.68, 95% CI 1.93 to 1.43; one trial, 148 participants, moderate quality evidence). There was increase in hand washing frequency, seven times per day in the intervention group versus three times in the control in this hospital trial (one trial, 148 participants, moderate quality evidence).
We found no trials evaluating or reporting the effects of hand washing promotions on diarrhoea‐related deaths, all‐cause‐under five mortality, or costs.
Authors' conclusions
Hand washing promotion probably reduces diarrhoea episodes in both child day‐care centres in high‐income countries and among communities living in LMICs by about 30%. However, less is known about how to help people maintain hand washing habits in the longer term.
22 March 2019
Update pending
Authors currently updating
The update is due to be published in 2019.
Plain language summary
Hand washing promotion for preventing diarrhoea
Review question
This Cochrane Review summarises trials evaluating the effects of promoting hand washing on the incidence of diarrhoea among children and adults in day‐care centres, schools, communities, or hospitals. After searching for relevant trials up to 27 May 2015, we included 22 randomized controlled trials conducted in both high‐income countries (HICs) and low‐ and middle‐income countries (LMICs). These trials enrolled 69,309 children and 148 adults.
How does hand washing prevent diarrhoea and how might hand washing be promoted
Diarrhoea causes many deaths in children below five years of age, mostly in LMICs. The organisms causing diarrhoea are transmitted from person to person through food and water contaminated with faeces, or through person‐to‐person contact. Hand washing after defecation, or after cleaning a baby's bottom, and before preparing and eating food, can therefore reduce the risk of diarrhoea. Hand washing can be promoted through group or individual training on hygiene education, germ‐health awareness, use of posters, leaflets, comic books, songs, and drama.
What this review says
Hand washing promotion at child day‐care facilities or schools in HICs probably prevents around 30% of diarrhoea episodes (high quality evidence), and may prevent a similar proportion in schools in LMICs (low quality evidence). Among communities in LMICs hand washing promotion prevents around 28% of diarrhoea episodes (moderate quality evidence). In the only hospital‐based trial included in this review, hand washing promotion also had important reduction in the mean episodes of diarrhoea (moderate quality evidence). This is based on only a single trial with few participants and thus there is need for more trials to confirm this. Effects of hand washing promotion on related hand hygiene behaviour changes improved more in the intervention groups than in the control in all the settings (low to high quality evidence). None of the included trials assessed the effect of handwashing promotion on diarrhoeal‐related deaths, all‐cause under‐five mortality, or the cost‐effectiveness of hand washing promotions.
Conclusion
Hand washing promotion in HICs and LMICs settings may reduce incidence of diarrhoea by about 30%. However, less is known about how to help people maintain hand washing habits in the longer term.
Summary of findings
Background
Description of the condition
Diarrhoea is a serious global public health problem, accounting for 1.8 million deaths annually especially among children under five years of age (Walker 2013). The yearly global diarrhoeal disease burden is estimated at 72.8 million disability adjusted life years (DALYs) lost through incapacitation and premature deaths, mainly in low‐ and middle‐income countries (LMICs) (Murray 2012).
Diarrhoea contributes significantly to malnutrition in children through a combination of forced low‐nutrient intake, reduced absorption, and increased nutrient excretion (WHO 2003). The malnutrition‐infection complex is clearly reinforced during diarrhoea episodes, as poor nutritional status predisposes children to more severe and persistent diarrhoea, impaired growth and development, and higher case fatality rates (UNICEF/WHO 2009; Lee 2012).
Diarrhoeal disease pathogens are usually transmitted through the faecal‐oral route (Curtis 2000). The pathways include ingestion of food and water contaminated by faecal matter, person‐to‐person contact, or direct contact with infected faeces (Eisenberg 2012). Some trials estimate that over 75% of all diarrhoea cases can be attributed to contaminated food and water (Curtis 2000; Maxwell 2012). Poor hygiene behaviours and improper handling practices of caregivers are associated with high levels of bacterial contamination of food and water (Iroegbu 2000; Mannan 2010; Pickering 2011).
Behaviours that encourage human contact with faecal matter include: improper disposal of faeces; children defecating on the floor; rags being used to cleanse the child after defecation; and lack of hand washing after defecation, handling faeces (including children's faeces) or cleansing the child's perineum and before handling food by caregivers and children (Pickering 2011). In particular, hand contact with ready‐to‐eat food (that is, food consumed without further washing, cooking, or processing/preparation by the consumer) represents a potentially important mechanism by which diarrhoea‐causing pathogens contaminate food and water (UNICEF/WHO 2009). In addition, flies may serve as vectors of diarrhoea‐causing pathogens to humans. Thus, consumption of food exposed to flies is associated with high risk of diarrhoea (Marino 2007).
Household economic status is significantly associated with diarrhoea prevalence (Woldemicael 2001), especially in low‐income countries. Households may lack basic infrastructure for proper hygiene practices, such as facilities for proper disposal of excreta. In addition, even where available, these may not be adapted for children's use (Tumwine 2002; UNICEF/WHO 2009). This often leads to indiscriminate defecation in and around the premises, and to increased risk of excreta handling by mothers, caregivers, and children (Nielsen 2001). A trial in Eritrea found that the availability of a toilet facility in households was associated with a 27% reduction in the risk of diarrhoea (Woldemicael 2001). The same trial also found associations between the number of children living in the house and diarrhoea morbidity. In some cultures children's faeces are regarded as innocuous. For this reason adults may not wash their hands after handling children's faeces and may cleanse a child with their bare hands (Traore 1994; Curtis 2000). However, evidence suggests that children's faeces are equally as hazardous as adult faeces and may contain even higher concentrations of pathogens than those of adults due to the children's increased interactions with contaminated materials in their surroundings (Oketcho 2012).
Description of the intervention
Hygiene promotion interventions constitute one of a number of strategies identified by World Health Organization (WHO) for control of diarrhoea (UNICEF/WHO 2009). These constitute a range of activities aimed at encouraging individuals and communities to adopt safer practices within domestic and community settings to prevent hygiene‐related diseases that lead to diarrhoea (WELL 1999; Ehiri 2001); hand washing is one such intervention. The practice of hand washing and the factors that influence hand washing behaviour among individuals in communities are complex (Whitby 2007); for example, washing hands with water only or with soap may be influenced by both knowledge of best practice and availability of water and soap (Curtis 2011). Also, hand washing may require infrastructural, cultural, and behavioural changes, which take time to develop, as well as substantial resources (for example, trained personnel, community organization, provision of water supply and soap) (Luby 2001a; UNICEF/WHO 2009). Consideration of the wide applicability and sustainability of hygiene interventions have recently come under critical review (Luby 2006 PAK; Ejemot‐Nwadiaro 2008; Gould 2010; Curtis 2011; Huis 2012; Madhu 2012). For example, maintenance of the new hand washing behaviours that result from hand washing promotional interventions is vital in maximizing the associated potential health benefits. Apart from the challenges of sustaining new behaviour (hand washing) among the target communities, cost has been identified as a major factor that limits the sustainability of hand hygiene behaviour (Langford 2007 NPL; Hartinger 2010 PER). For example, to sustain the health benefits of newly acquired hand washing behaviours, it is also important that individuals and communities have access to resources that support hand washing, including water and soap. Thus, lack of access to hand washing resources may limit the potential impact of hand washing on health particularly for low‐income households and communities.
How the intervention might work
Hand washing aims to decontaminate the hands and prevent cross transmission of diarrhoeal‐causing pathogens (Ehiri 2001; Gurjeet 2013). Hand washing promotion employs direct approaches such as training and educating individuals or group of individuals about hygiene, diarrhoea transmission, the relationship between germs and health, demonstrating this relationship through leaflets, posters, drama, and songs (Whitby 2007; Curtis 2011). Washing hands with soap and water removes pathogens mechanically and may also chemically kill contaminating and colonizing flora, making hand washing more effective (Hugonnet 2000). Also washing hands with soap under running water or large quantities of water with vigorous rubbing was found to be more effective than several members of a household dipping their hands into the same bowl of water (often without soap) (Luby 2005), which is a common practice in many low‐income countries, especially before household meals (Ehiri 2001). This may contribute to, rather than prevent, food contamination as pathogens present on contaminated hands of household members can be transferred to those who subsequently dip their hands in the same bowl of water (Prüss 2002).
Why it is important to do this review
Hand washing is a viable intervention in the control of diarrhoeal diseases. It is listed in the UNICEF/WHO 2009 seven‐point plan for comprehensive control of diarrhoea. Hand washing requires infrastructural, cultural, and behavioural changes that take time and substantial resources to develop (Cave 1999; Yeager 1999; Luby 2001b). Given that resources spent on interventions to promote hand washing could be invested on other equally important public health programmes, it is important to ascertain that hand washing promotion is an efficient use of scarce health resources. In 2008, we published a review that assessed the broader question of the effectiveness of hand washing with soap in preventing diarrhoea as against other interventions such as provision of water, improvement of water quality (treatment of water), amongst randomized controlled trials (RCTs) (Ejemot‐Nwadiaro 2008). A review by Curtis 2003, which examined the effectiveness of hand washing with soap in community‐based trials, estimated that hand washing could reduce diarrhoea risk by up to 47%. Similarly, Fewtrell 2005 examined a range of water, sanitation, and hygiene interventions in LMICs, and estimated that hygiene interventions reduced diarrhoea incidence by 44%. However, both reviews included non‐randomized trials. Curtis 2003 included cross‐sectional trials which have inherent limitations with regard to establishment of causal relationships. Fewtrell 2005 presented evidence of publication bias in included trials. In this Cochrane Review, we assessed whether the estimate of effect observed only in RCTs is of similar magnitude to those seen in previous reviews and the applicability of hand washing interventions in reducing diarrhoeal diseases across wide population groups. We also included both institution‐based and community‐based trials in countries of any income level.
Objectives
To assess the effects of hand washing promotion interventions on diarrhoeal episodes in children and adults.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs), including cluster‐RCTs.
Types of participants
Individuals (adults and children) in day‐care centres or schools, patients in hospitals, communities, or households.
Types of interventions
Intervention
Activities that promoted hand washing after defecation or after disposal of children's faeces and before eating, preparing or handling foods; for example, small group discussions and larger meetings on hygiene education, germs‐health awareness interventions, multimedia communication campaigns with posters, radio/TV campaigns, leaflets, comic books, songs, slide shows, use of T‐shirts and badges, pictorial stories, dramas, and games. We included trials that focused exclusively on hand washing and those that had hand washing as part of a broader package of hygiene interventions if they undertook analyses of effects of hand washing on diarrhoea.
Control
No hand washing promotion.
Types of outcome measures
Primary outcomes
Episodes of diarrhoea (self‐reports collected through home visits; hospital/health centre/clinic records including admissions for diarrhoea‐related dehydration).
We defined diarrhoea as:
Acute/primary diarrhoea: passage of three or more loose or watery stools in a 24‐hour period, a loose stool being one that would take the shape of a container; or definitions used by trial authors consistent with this standard definition.
Persistent diarrhoea: diarrhoea lasting 14 or more days.
Dysentery: stool with blood.
Secondary outcomes
Diarrhoea‐related death among children or adults.
Behavioural changes, such as changes in the proportion of people who reported or are observed washing their hands after defecation, disposal of children's faeces, or before preparing or handling foods.
Changes in knowledge, attitudes, and beliefs about hand washing.
All‐cause‐under five mortality.
Cost‐effectiveness.
Search methods for identification of studies
We attempted to identify all relevant trials regardless of language or publication status (published, unpublished, in press, and in progress).
Electronic searches
We searched the following databases using the search terms and strategy described in Table 4: Cochrane Infectious Diseases Group Specialized Register (27 May 2015); Cochrane Central Register of Controlled Trials (CENTRAL), published in the Cochrane Library (2015, Issue 5); MEDLINE (1966 to 27 May 2015); EMBASE (1974 to 27 May 2015); and LILACS (1982 to 27 May 2015).
1. Detailed search strategies.
| Search set | CIDG SRa | CENTRAL | MEDLINEb | EMBASEb | LILACSb |
| 1 | handwashing | Handwashing ti, ab | hand wash* ti, ab | hand wash$ ti, ab | handwashing |
| 2 | diarrhea | hand washing ti, ab | hand disinfec* ti, ab | hand disinfec* ti, ab | diarrhea |
| 3 | diarrhoeal diseases | hand cleansing ti, ab | hand clean* ti, ab | hand clean$ ti, ab | 1 and 2 |
| 4 | — | hand hygiene ti, ab | hand hygiene ti, ab | hand hygiene ti, ab | — |
| 5 | — | 1 or 2 or 3 or 4 | hand sterility ti, ab | hand sterility ti, ab | — |
| 6 | — | Diarrh* ti, ab | "Hand Disinfection"[Mesh] | “Hand washing” [Emtree] | — |
| 7 | — | 5 and 6 | 1 or 2 or 3 or 4 or 5 or 6 | 1 or 2 or 3 or 4 or 5 or 6 | — |
| 8 | — | — | Diarrhea ti, ab | Diarrhea ti, ab | — |
| 9 | — | — | Diarrhoea ti, ab | Diarrhoea ti, ab | — |
| 10 | — | — | 8 or 9 | 8 or 9 | — |
| 11 | — | — | 7 and 10 | 7 and 10 | — |
aCochrane Infectious Diseases Group Specialized Register. bSearch terms used in combination with the search strategy for retrieving trials developed by Cochrane (Lefebvre 2011); upper case: MeSH or EMTREE heading; lower case: free text term.
We also searched the following databases using diarrhoea, diarrhoea, and handwashing as search terms: PsycINFO (1967 to 27 May 2015); Science Citation Index and Social Sciences Citation Index (1981 to 27 May 2015); ERIC (Educational Resources Information Center; 1966 to 27 May 2015); SPECTR (The Campbell Collaboration's Social, Psychological, Educational, and Criminological Trials Register; 2000 to 27 May 2015); Bibliomap and TRoPHI (The Trials Register of Promoting Health Interventions) maintained by the Evidence for Policy and Practice Information and Co‐ordinating Centre (www.eppi.ioe.ac.uk) (1990 to 27 May 2015); and The Grey Literature (www.nyam.org/library/grey.shtml; 2002 to 27 May 2015). We also searched the World Health Organization (WHO) International Clinical Trial Registry Platform (ICTRP) and the metaRegister of Controlled Trials (mRCT) for ongoing trials on 27 May 2015 using diarrhoea, diarrhoea, and handwashing as search terms. The PRISMA flow diagram is shown in Figure 1 below.
1.
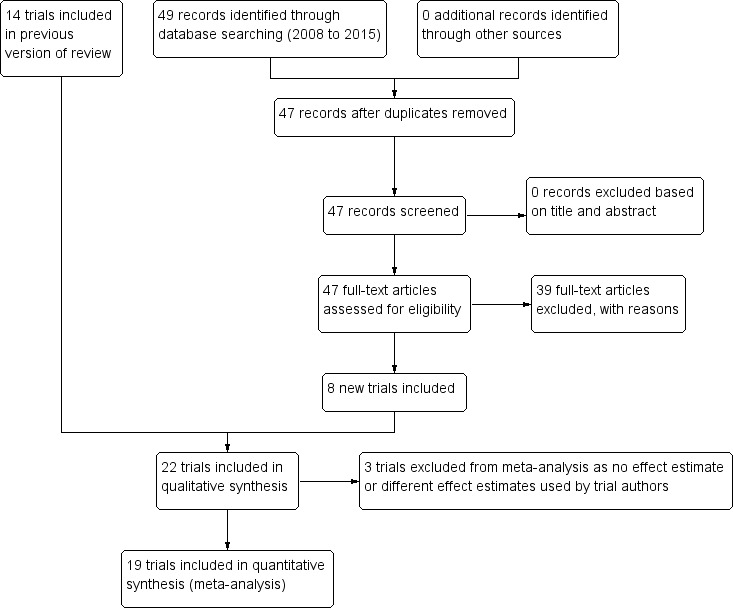
PRISMA flow diagram.
Searching other resources
Researchers and organizations
To obtain information on published, unpublished and ongoing trials, we contacted researchers in the field for unpublished and ongoing trials (October 2013).
Reference lists
We also examined reference lists of articles for relevant trials.
Data collection and analysis
Selection of studies
Three review authors (RIE, JC, and DA) independently screened titles and abstracts of relevant articles to assess their eligibility for inclusion in the review. We retrieved full‐texts of articles that were deemed potentially relevant to the review for further assessment. Decision on inclusion was reached by consensus among all review authors. We scrutinized each trial report to ensure that we included multiple publications from the same trial only once. We listed the excluded trials and the reasons for their exclusion.
Data extraction and management
Three review authors (RIE, DA, and JC) independently extracted data on methods, types of participants, interventions, and outcomes from the selected trials using a standardized data extraction form. We resolved any disagreements by discussion and consensus among review authors. We requested unpublished data and additional information from published trials from relevant individuals, groups, and organizations.
We extracted the year of completion of the trial rather than the year of publication for identification of included trials. When such data were not reported we used the year of publication. In addition, we used a three‐letter international code of the country were the trial was conducted. This was to give a clear time frame for the Cochrane Review (1977 to 2013). We extracted data on each trial site, including any measures of availability of water, soap, and literacy level of the communities. Where data were available, we extracted the socioeconomic status of trial participants since resources for effective hand washing (for example, running water and soap) may be more accessible to higher income households. We carefully summarized details of the intervention including: type of promotional activity, whether soap and water provision was part of the intervention, method of hand washing promoted (washing in a bowl or under running water), and procedure for hand washing.
We had intended to analyse episodes of diarrhoea as a dichotomous outcome, but the data reported by the trials did not permit this type of analysis. We analysed the outcome as count data, when either the incidence rate ratio and 95% confidence intervals (CIs), or the number of episodes of diarrhoea and the person‐time at risk was reported; or as continuous data when the mean number of diarrhoea episodes and standard deviation (SD) were presented.
For individually RCTs, when continuous outcomes data were summarized as arithmetic means, we extracted the arithmetic means, SDs, and numbers of participants for the treatment and control groups. For count (rate) outcome data we extracted the number of episodes, the number of person‐years at risk, and the number of participants for each intervention group, or we extracted a rate ratio and measure of variation (for example, CI) directly from the publication.
Cluster‐RCTs require the use of different data extraction methods and analysis methods because trials with a cluster design require more complex analysis than trials that randomized individuals. Observations on participants in the same cluster tend to be correlated; therefore the intra‐cluster variation must be accounted for during the analysis of the trial. If this correlation is ignored in the analysis and the same techniques are employed as for individually RCTs the resulting measure of effect remains a valid estimate, but the associated variance of the estimate will be underestimated leading to unduly narrow CIs. For meta‐analysis this means that trials analysed without allowing for this design effect will receive too much weight.
For the cluster‐RCTs, we extracted information on the number of clusters, average size of clusters, unit of randomization, whether the trials adjusted for clustering, and the statistical method used to analyse cluster trials. When a trial's analysis had adjusted for clustering, we extracted the point estimate and 95% CI. For count data we extracted the incidence rate ratio. If a trial had not adjusted for clustering, we extracted the same data as for the individually RCTs.
Assessment of risk of bias in included studies
Two review authors (RIE and DA) independently assessed the risk of bias in included trials using the Cochrane 'Risk of bias' assessment tool (Higgins 2011). We assessed the risk of bias across the following domains: randomization sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other biases. We classified our judgements as 'high', 'unclear' or 'low' risk of bias using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
In the blinding domain we acknowledged that double blinding is not possible in trials of hand washing interventions since there is no obvious placebo. However, outcome assessors could be blinded, and we assessed whether or not this had occurred. It is also difficult to assess losses to follow‐up (incomplete outcome data) in open cluster‐RCTs. Some adults and children may leave the trial, but others are born or enter the trial during the follow‐up period; hence participant numbers are in constant flux. Inclusion of all randomized participants in the analysis is thus most clearly represented as the person‐time at risk accrued as a percentage of maximum possible person‐time at risk in each trial arm. Therefore, we reported on this measure and also on any loss to follow‐up of both clusters and participants, and assessed this as low risk if at least 90%. We also assessed whether baseline characteristics were comparable across the intervention groups and assessed whether data was collected at similar time points for the intervention and control sites with a view to identifying selective reporting and other possible biases. The details are shown in Figure 2 and Figure 3.
2.
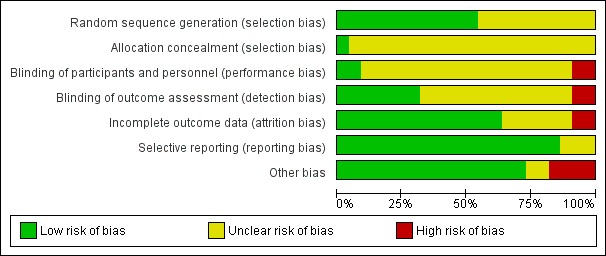
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
3.
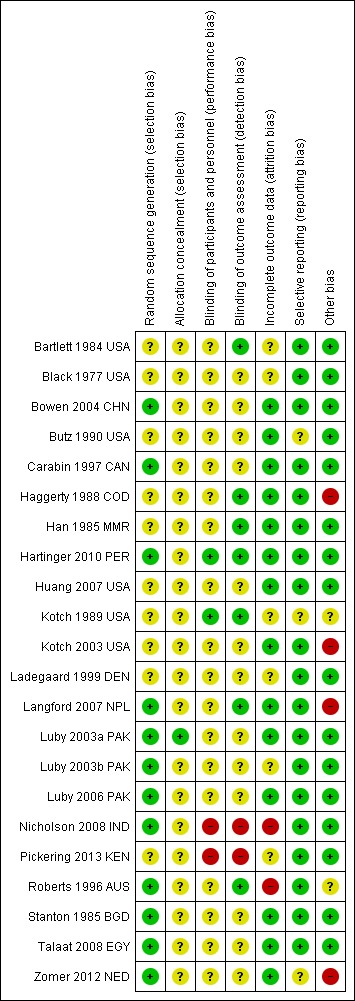
Assessment of quality of evidence
We used the GRADE approach to assess the quality of evidence and interpret our findings. We imported data from Review Manager (RevMan) to GRADEpro 2014 to create a 'Summary of findings' table containing relevant information on the outcomes of interest. We then proceeded to downgrade the quality of evidence (if necessary) for each outcome across the following domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias for each trial that contributed to the outcome. We downgraded the evidence for each outcome by one level (for serious limitations), two levels (for very serious limitations), or left it at 'no limitations' when we found no reason to downgrade.
We included the pre‐specified outcomes for the three independent settings in Table 1, Table 2, and Table 3.
Summary of findings for the main comparison. Summary of findings table 1.
| Hand washing at child day‐care centres and schools compared to no intervention | |||||
| Patient or population: Children Settings: Child day‐care centres or schools Intervention: Hand washing promotion (± provision of hand washing materials) Comparison: No intervention | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| No intervention | Hand washing promotion | ||||
| Episodes of diarrhoea | High income countries | Rate ratio 0.70 (0.58 to 0.85) | 4664 (9 trials) | ⊕⊕⊕⊕ high1,2,3,4,5 | |
| 4 episodes per 100 children per year | 2 episodes per 100 children per year (2 to 3) | ||||
| Low‐ or middle‐income countries | Rate ratio 0.66 (0.43 to 0.99) | 45,380 (2 trials) | ⊕⊕⊖⊖ low6,7,8 | ||
| 22 episodes per 100 children per year | 15 episodes per 100 children per year (9 to 22) | ||||
| Hand washing behaviour | — | — | Not pooled | 1845 (3 trials) | ⊕⊕⊖⊖ low9,10,11 |
| The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1The median incidence of diarrhoea in the control groups was four episodes per 100 children per year. 2No serious risk of bias: Most trials are at high or unclear risk of detection or reporting bias due to no description of blinding of outcome assessors. Restriction of the analysis to just the blinded trials finds a slightly smaller effect size but the result remains statistically significant. Not downgraded. 3No serious inconsistency: Although statistical heterogeneity was high, this heterogeneity was related to the size of the effect not the direction of effect. The individual effect sizes in trials ranged from an 10% relative reduction in diarrhoea to a 50% reduction. 4No serious indirectness: These nine trials were conducted in day‐care centres/schools in high income countries (USA, Denmark, Australia, Netherlands and Canada). 5No serious imprecision: The result is statistically significant and the meta‐analysis adequately powered to detect this result. 6The incidence of diarrhoea in the control group in the trial from Egypt was 22 per 100 children per year. The incidence in the control group in the Kenya trial was not stated. 7No serious inconsistency: While both trials found reductions in diarrhoea incidence the reduction was only statistically significant in the trials from Egypt. However, we did not downgrade. 8Downgraded by 2 for serious indirectness: Only one trial was conducted in a low‐income country (Pickering 2013 KEN). This trial from an urban slum in Nairobi did not find a statistically significant benefit on diarrhoea incidence. 9Downgraded by 1 for serious risk of bias: In the three trials, the observers themselves could not have been blinded and may have influenced the outcome simply by being present. 10Downgraded by 1 for serious indirectness: These three trials are from day care‐centres in the Netherlands and USA and schools in an urban slum in Nairobi, Kenya. Further trials from different settings are needed to confirm this result can be generalized. 11The trials from Netherlands and USA found large and statistically significant improvements in staff hand washing behaviour or hand hygiene compliance. The trial from Kenya found no improvement in hand washing, but large and statistically significant improvements in the use of soap.
Summary of findings 2. Summary of findings table 2.
| Hand washing among communities compared to no intervention for preventing diarrhoea | |||||
| Patient or population: Children Settings: Communities Intervention: Hand washing promotion through community structures (± provision of hand washing materials) Comparison: No intervention | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| No intervention | Hand washing promotion | ||||
| Episodes of diarrhoea | Low‐ or middle‐income countries | Rate ratio 0.72 (0.62 to 0.83) | 14,726 (8 trials) | ⊕⊕⊕⊖ moderate2,3,4,5 | |
| 3 episodes per 100 children per year1 |
2 episodes per 100 children per year1 (2 to 2) |
||||
| Hand washing behavioural changes/changes in knowledge, attitude and practice Follow‐up: mean 7 months | — | — | Not pooled | 3490 (3 trials) | ⊕⊕⊕⊕ high6,7,8,9 |
| *The basis for the assumed risk (for example, the median control group risk across trials) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1The median incidence of diarrhoea in the control groups was 3 episodes per 100 children per year. 2No serious risk of bias: Most trials are at high or unclear risk of detection or reporting bias due to no description of blinding of outcome assessors. Restriction of the analysis to just the blinded trials finds a slightly smaller effect size but the result remains statistically significant. Not downgraded. 3No serious inconsistency: Although statistical heterogeneity was high, this heterogeneity was related to the size of the effect not the direction of effect. The individual effect sizes in trials ranged from an 6% relative reduction in diarrhoea to a 30% reduction. 4Downgraded by 1 for serious indirectness: These eight trials were conducted in LMICs (the Democratic Republic of Congo, Pakistan, Bangladesh, Myanmar, Peru, India and Nepal). 5No serious imprecision: The result is statistically significant and the meta‐analysis adequately powered to detect this result. 6No serious risk of bias: Most trials are at high or unclear risk of detection or reporting bias due to no description of blinding of outcome assessors. Restriction of the analysis to just the blinded trials finds a slightly smaller effect size but the result remains statistically significant. Not downgraded. However this is limited to three trials in low‐income countries. Further trials from other income settings are needed to confirm if this result can be generalized. 7No serious inconsistency: All the included trials found reductions in diarrhoea incidence. 8No serious indirectness: The three trials were conducted in low‐income communities/countries (Nepal, low‐income urban communities in Mumbai, India and Bangladesh). The trials found statistically significant benefit on diarrhoea incidence. 9No serious imprecision: The result is statistically significant and adequately powered to detect this result.
Summary of findings 3. Summary of findings table 3.
| Hand washing compared to no intervention for preventing diarrhoea | |||||
| Patient or population: Patients at risk of diarrhoea Settings: Hospital Intervention: Hand washing promotion Comparison: No intervention | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| No intervention | Hand washing promotion | ||||
| Episodes Self‐reports collected through home visits; hospital/health centre/clinic records including admission for diarrhoea‐related dehydration Follow‐up: 1 year | 2.92 episodes | 1.24 episodes | Mean difference 1.68 episodes (1.93 to 1.43) | 148 (1 trial) | ⊕⊕⊕⊖ moderate1,2,3,4 |
| Hand washing behavioural changes/changes in knowledge, attitude and practice Frequency of hand washing per day Follow‐up: 1 year | 4 times daily | 7 times daily | — | 148 (1 trial) |
⊕⊕⊕⊖ moderate3,4,5 |
| *The basis for the assumed risk (for example, the median control group risk across trials) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; MD: mean difference. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1Outcomes assessed in adults in high risk group (people with AIDS). 2The mean episodes in the control groups was 2.92 while that of the intervention group was 1.24 episodes over the 1 year trial period. 3Downgraded by 1 for serious risk of bias: the trial is at an unclear risk of selection bias due to failure to describe a process of allocation concealment. This trial is also at high detection or reporting bias due to no description of blinding of outcome assessors. Blinding of participants would not have been possible. 4Evidence from this setting was most limited since it is from only one trial (Huang 2007 USA). 5Hand washing rates: intervention ‐ seven times daily from three times at baseline; control ‐ four times daily from three times.
Measures of treatment effect
We qualitatively compared included trials to ascertain the feasibility of pooling them together in a meta‐analysis. Thus we identified three distinct settings which included: child day‐care centres, community‐based interventions, and hospital based trials; since the factors that affect hand washing practice may vary in these settings. We stratified the trials based on these settings for the meta‐analysis and calculated risk ratios (RR) for dichotomous outcomes, mean difference (MD) for continuous outcomes measure on the same scale, and standardized mean difference (SMD) for continuous outcomes measured using different scales.
Unit of analysis issues
For all trials that did not adjust for clustering, we made approximate adjustments for clustering using estimates of the intra‐cluster correlation coefficient (ICC) from other trials that did adjust for clustering and reported this statistic. We did this by multiplying the standard error for each trial by the square root of the design effect. We estimated the design effect as 1+(m‐1)*ICC, where 'm' is the average cluster size and 'ICC' is the intra‐cluster correlation coefficient (Higgins 2011).
Dealing with missing data
We contacted authors of eligible trials for missing data or for additional information when the trials were less than 15 years old.
Assessment of heterogeneity
We checked for heterogeneity by visually inspecting the forest plots, applying the Chi² test with a P value of 0.10 indicating statistical significance, and also implementing the I² test statistic with a value of 50% used to denote moderate levels of heterogeneity. We used the random‐effects model to pool data if we detected heterogeneity and it was still considered clinically meaningful to combine the trials. Due to the limited number of trials in each setting we were unable to explore potential sources of heterogeneity in depth. We explored and attempted to explain heterogeneity where possible using a pre‐defined trial characteristic (provision of hand washing material (soap) as part of intervention, and type of promotional activity employed) and quality characteristics (whether outcome assessors were blind and whether trials had adjusted for clustering).
Assessment of reporting biases
We assessed the possibility of publication bias by plotting a funnel plot if at least ten trials contributed to the treatment comparison. However, we did not undertake this due to an insufficient number of included trials.
Data synthesis
We analysed the data using Review Manager (RevMan) and presented all results with 95% CIs. We stratified the analysis into three categories of settings – child day‐care centres and school‐based interventions (day‐care centres or primary schools), community‐based interventions, and intervention in people at high risk of diarrhoea (people with acquired immune deficiency syndrome (AIDS)). Also we stratified the analyses by the income status of the countries where the trials were conducted. Since the outcomes and methods of measuring behaviour changes were too variable to make meta‐analysis meaningful, we tabulated the results.
Individually RCTs
We summarized continuous outcome data from individually RCTs using the MD value. Meta‐analysis of individually RCTs was not undertaken due to the limited number of individually RCTs.
Cluster‐RCTs that adjusted for clustering
For count outcomes, we pooled incidence rate ratios (IRR) in Review Manager (RevMan) using the generic inverse variance method with the random‐effects model. We used standard techniques for calculating standard errors from 95% CIs (Higgins 2008). When the outcomes and methods of measuring outcomes were too variable to make meta‐analysis meaningful (for changes in hand washing behaviour) we tabulated the results. One trial performed child and site‐level analyses (Haggerty 1988 COD); the 95% CIs were not provided for the site‐level analysis. We therefore estimated the denominator from the number of children by trial arm by assuming that all those who had remained in the trial for at least nine weeks had a total of 12 weeks of follow‐up. The numerator (average number of episodes per child) was provided at the cluster level. We classified this trial as cluster adjusted. One trial, Luby 2006 PAK, presented mean longitudinal prevalence of diarrhoea without presenting data on incidence of diarrhoea and hence we could not include it in the meta‐analyses.
Cluster‐RCTs that did not adjust for clustering
For trials that did not report on or were unclear on the method used to adjust for clustering, we either extracted information on the rate ratio and unadjusted 95% CI or, wherever possible, estimated the unadjusted rate ratios and 95% CIs from the total number of diarrhoea episodes and person‐time at risk in each trial arm. Where data on person‐time at risk were not directly provided by the trial authors, we estimated this as accurately as possible from the follow‐up duration multiplied by the total number of children as the denominator for both intervention and control groups respectively. The measures of effect and CIs are presented in tables. One trial adjusted for clustering by comparing the mean incidence rate of intervention and non‐intervention classrooms (Kotch 1989 USA), but only a cluster‐adjusted 95% CIs for a different outcome (excess mean episodes) and not a rate ratio was presented. We took the cluster‐adjusted estimate of the numerator (the mean incidence rate across the clusters) from the published data and estimated the person‐time at risk crudely by multiplying the number of contacts every two weeks by the number of children and assuming this was equally distributed between the intervention and control groups. We classified this trial as not having adjusted for clustering
For all trials that did not adjust for clustering, we attempted to make an approximate adjustment using estimates of the ICC from one of the trials that did adjust for clustering and reported this statistic. Only two trials reported this statistic: one community‐based trial, Luby 2003b PAK, and one trial in a child day‐care centre, Roberts 1996 AUS. We assumed that these ICC estimates could be generalized to other community‐based and child day‐care centre or school‐based trials respectively. We extracted the number of children and number of clusters from each unadjusted trial to estimate the average cluster size. We then followed standard methods (Higgins 2011) to estimate the design effect for each trial and multiplied the standard error for each trial by the square root of this design effect. This approximate adjustment increases the standard error (and hence width of CIs for the unadjusted trials) and appropriately reduces the weight given to such trial in the meta‐analysis. We performed meta‐analyses by pooling the estimates of the cluster adjusted and approximately adjusted trials together.
Subgroup analysis and investigation of heterogeneity
We planned to explore the possible causes of heterogeneity if we detected any using subgroup analysis. The subgroups used were: trial setting, provision of hand washing material (soap) as part of intervention, type of promotional activity employed), and quality characteristics (whether outcome assessors were blinded).
Sensitivity analysis
We undertook a sensitivity analysis to explore the robustness of our findings, including the trial size, duration of follow‐up, differences in method of assessing the primary outcome, and differences in methodological quality (blinding of outcome assessors) of the included trials.
Results
Description of studies
Results of the search
Our search yielded 47 additional potentially relevant trials, making a total of 84 when combined with the 37 search results of the original review (Ejemot‐Nwadiaro 2008). In total, 22 trials met the inclusion criteria: 14 trials were included in the previous version of the review, Ejemot‐Nwadiaro 2008, and we included eight new trials based on the updated search. We have described them in the 'Characteristics of included studies' section. One trial was in Danish (Ladegaard 1999 DEN), and the rest were written in English. Twelve trials were child day‐care centres or school‐based, nine trials were community‐based, and one trial (Huang 2007 USA) was in a high‐risk group. We have listed reasons for excluding 62 trials in the 'Characteristics of excluded studies' table.
Included studies
Child day‐care centres or schools
All 12 trials in this group were randomized by cluster using primary schools (Bowen 2004 CHN; Talaat 2008 EGY; Pickering 2013 KEN), day‐care centres (Black 1977 USA; Bartlett 1984 USA; Butz 1990 USA; Roberts 1996 AUS; Carabin 1997 CAN; Ladegaard 1999 DEN; Kotch 2003 USA; Zomer 2012 NED ), or classrooms in day‐care centres (Kotch 1989 USA) as the unit of randomization. These trials were all conducted in high‐income countries except for three trials conducted in LMICs Bowen 2004 CHN, (which was undertaken in Fujian province in China) Talaat 2008 EGY (which was conducted in Cairo, Egypt), and Pickering 2013 KEN (conducted in Nairobi, Kenya). The others trials were performed in Australia (Roberts 1996 AUS), Europe (Ladegaard 1999 DEN; Zomer 2012 NED), and North America (Black 1977 USA; Bartlett 1984 USA; Kotch 1989 USA; Butz 1990 USA; Carabin 1997 CAN; Kotch 2003 USA), where resources and materials for hand washing were relatively available and accessible.
Interventions
All trials used multiple hygiene interventions, except Black 1977 USA, Bowen 2004 CHN, and Pickering 2013 KEN which used only a hand washing intervention. Though Pickering 2013 KEN was a three‐arm trial that investigated hand sanitizer and hand washing with soap, we only considered the arm of hand washing with soap in this Cochrane Review, as such it is categorized as a hand washing only intervention. Kotch 2003 USA assessed the impact of provision of hand washing and diapering equipment on incidence and duration of infectious illness (including diarrhoea) in both children and staff. We have described the interventions in more detail in Table 5.
2. Description of hand washing interventions at child day‐care centres and schools.
| Trial | Promotional activity | Classificationa | Message content | Hand washing method | Hand washing styleb | Material provision | Water availability |
| Bartlett 1984 USA |
|
|
Staff and child hand washing, diapering, food handling, and environmental cleaning | Unclear | Not specified | Not specified | Adequate |
| Black 1977 USA | Large group education | Hygiene education | Staff and child hand washing before handling food and after defecation | Water with bar soap and paper towels | Unclear | By the day‐care centres' management | Adequate |
| Bowen 2004 CHN |
|
|
Hand washing before eating and after toileting | Water with soap | Under running water | Supplies of soap to schools in "Expanded Intervention"; 1 bar of soap to homes in both expanded and standard intervention | Adequate (criteria for taking part in trial) |
| Butz 1990 USA | Large group training (in‐home instruction to day‐care providers) |
|
|
Water with soap | Not specified | All supplies provided by researchers | Adequate |
| Carabin 1997 CAN |
|
Hygiene education |
|
Unclear | Not specified | Unclear | Adequate |
| Kotch 1989 USA |
|
Hygiene education |
|
Water with soap plus disposable towel | Under running water | Unclear | Adequate |
| Kotch 2003 USA |
|
|
Training to improve and standardize the hand‐washing, sanitation, diapering and food preparation procedures in both intervention and control enters by addressing knowledge, attitudes and behaviours of child‐care providers and promoting use of the equipment | Not described | Not described | Diapering, hand‐washing and food preparation equipment was provided by the researchers | Adequate |
| Ladegaard 1999 DEN | Small group practical demonstration |
|
|
Water with soap | Under running water | Unclear | Adequate |
| Pickering 2013 KEN |
|
|
|
Water with soap | Not described | Researchers provided liquid soap and water tank | Adequate |
| Roberts 1996 AUS |
|
|
|
Water with soap | Under running water | Unclear | Adequate |
| Talaat 2008 EGY |
|
Hygiene education |
|
Water with soap | Under running water |
|
Adequate (Cairo governate was chosen because of the continuous availability of water in school settings) |
| Zomer 2012 NED |
|
|
|
Water with soap | Not described | Trial investigators provided hand hygiene products free of charge (dispenser for paper towels, soap, alcohol‐based hand sanitizer and hand cream, with refills for 6 months). | Adequate |
aMessage classification. bWhether done under running water; in a bowl by an individual or by several people. cParticipatory learning involves a process that helps engage learners in an active role of inquiry in which they share experiences and reflect critically on practice in a context that many group members find stimulating and relatively safe (Martin 1997).
All but one of the included trials in child day‐care centres or schools institution‐based trials had intervention and control arms (monitoring only). Bowen 2004 CHN had three arms for the standard intervention, expanded intervention (which included the standard intervention and peer‐monitoring of hand‐washing), and control. It is important to note that the control group in most cases received quite frequent monitoring (estimating diarrhoea illness episodes on typically two‐weekly basis). This monitoring may itself have influenced hand washing behaviour. The Carabin 1997 CAN trial attempted to tease out the effects of the intervention alone from 'monitoring'. The 'monitoring' effect in this trial was estimated as the difference in diarrhoea incidence rates within each arm over one year of the trial (September 1996 to November 1997). The crude effectiveness of intervention was estimated as the difference between the monitoring effect in the intervention group.
Participants
Twelve trials including 54,006 children met the inclusion criteria. Seven trials included children aged less than three years, one trial was in children under six years (Ladegaard 1999 DEN), and one trial was with children aged less than seven years (Butz 1990 USA). Bowen 2004 CHN involved children in the first grade at school in China; Talaat 2008 EGY included children in government elementary schools in Cairo, Egypt; and Pickering 2013 KEN involved children aged between five to 10 years in primary schools in Nairobi, Kenya. Hand washing behavioural changes and changes in knowledge, attitude, and belief on hygiene were assessed in the day‐care providers (number not strictly reported) and children, while the primary outcome measures were assessed in the children.
The number of clusters ranged from four (Black 1977 USA) to 87 (Bowen 2004 CHN). Primary outcome measures were assessed across 278 day‐care centres and 151 schools. Participants were exposed to mainly small and large group training sessions on hygiene education and germs‐health theory, that employed multiple promotional techniques (for example, audio and video tapes, pamphlets, practical demonstrations, drama, posters, songs, games, or peer monitoring). Kotch 2003 USA employed the 'Keep‐it‐clean' module in training caregivers to standardise the interventions across the trial arms. The aim was to provide education about personal hygiene, diarrhoea transmission, treatment, and prevention, and the importance of techniques for hand washing. Intervention and control groups were generally comparable regarding important characteristics at baseline (Table 5).
Outcome measures
All included trials measured the primary outcome, episodes of diarrhoea. Three trials reported proportion of people washing their hands and or changes in knowledge, attitude, and beliefs about hand washing (Kotch 1989 USA; Roberts 1996 AUS; Pickering 2013 KEN). No trials reported diarrhoea‐related deaths, all‐cause‐under five mortality or cost‐effectiveness data. However, Kotch 2003 USA reported that the cost of purchasing and installing one unit of the hand washing and diapering equipment was quite exorbitant at USD10,385 (USD7500 for the equipment and the rest for installation per classroom). Follow‐up periods ranged from two to 12 months.
Adjustment for clustering
Five trials did not appear to have accounted for clustering in the analysis for any outcome measure (Black 1977 USA; Bartlett 1984 USA; Butz 1990 USA; Ladegaard 1999 DEN; Talaat 2008 EGY). Kotch 1989 USA adjusted for clustering by comparing the mean incidence rate of intervention and non‐intervention classrooms, but only a cluster adjusted 95% CI for a difference outcome (excess mean episodes) and not a rate ratio was presented. Kotch 2003 USA reported controlling for clustering by estimating a random effect for the centres, but this does not seem to have been reflected in the results. In the other five cluster‐adjusted trials, Bowen 2004 CHN presented only the school level analysis (mean illness and absence rates by school); Carabin 1997 CAN adjusted for clustering using a Bayesian hierarchical model, while Roberts 1996 AUS, Zomer 2012 NED and Pickering 2013 KEN estimated robust standard errors in a Poisson regression model.
Community‐based trials
We included nine cluster‐RCTs that used entire communities (generally villages, squatter settlements, or neighbourhoods, except Han 1985 MMR, which used households) as units of randomization. These trials were conducted in LMICs in Africa (Haggerty 1988 COD), Asia (Han 1985 MMR; Stanton 1985 BGD; Luby 2003a PAK; Luby 2003b PAK; Luby 2006 PAK; Langford 2007 NPL; Nicholson 2008 IND), and South America (Hartinger 2010 PER).
Interventions
Five trials evaluated hand washing only interventions (Han 1985 MMR; Luby 2003a PAK; Luby 2003b PAK; Langford 2007 NPL; Nicholson 2008 IND). Luby 2003a PAK had two hand washing arms, one with plain soap and one with antibacterial soap. These two arms had similar results and are combined in this Cochrane Review. Han 1985 MMR used plain soap. Luby 2003b PAK was a five‐arm trial that investigated water quality interventions, hand washing, and a combination of the two; only the arm with antibacterial soap and hand washing education is considered in this review. Luby 2006 PAK conducted a follow‐up trial to the Luby 2003b PAK trial, maintaining the initial randomization process to assess if learnt hygiene behaviours could be sustained over time without additional hygiene promotion intervention. Three other trials used multiple hygiene interventions that included hand washing with soap (the type of soap used is not described) (Stanton 1985 BGD; Haggerty 1988 COD; Hartinger 2010 PER). We have provided more detailed descriptions of the interventions in Table 6.
3. Description of hand washing intervention in communities.
| Trial | Promotional activity | Classificationa | Message content | Hand washing method | Hand washing styleb | Material provision | Water availability |
| Haggerty 1988 COD | Large group training | Hygiene education |
|
Unclear | Not specified | Unclear | Unknown |
| Han 1985 MMR | Small group education (households) |
|
Hand washing:
|
Water with bar soap | Not specified | Plain bar soap provided by researcher | Unknown |
| Hartinger 2010 PER |
|
|
Hand washing:
|
Water with soap | Not specified | IHIP provided by researchers | Unknown |
| Langford 2007 NPL |
|
|
Hand washing:
|
Water with soap | not specified | Soap provided by researcher (community motivators distributed a new bar of soap to each mother at these meetings) | Adequate (water for hygienic purposes, however was always available from these tubes and deep wells) |
| Luby 2003a PAK |
|
Hygiene education | Hand washing:
|
Water with plain or antibacterial soap | Water from a pitcher (though not clearly stated) | Soap provided by researchers | Unknown |
| Luby 2003b PAK |
|
|
Hand washing:
|
Water with antibacterial soap | Not specified | Soap provided by researchers | Unknown |
| Luby 2006 PAK | Follow‐up trial of Luby 2003b PAK | No intervention was conducted | Follow‐up trial of Luby 2003b PAK above | No intervention | No intervention | No intervention | Follow‐up trial |
| Nicholson 2008 IND |
|
|
|
Water with soap | Not specified | Soap provided by researchers | Unknown |
| Stanton 1985 BGD |
|
Hygiene education |
|
Unclear | Not specified | Unclear | Inadequate |
aMessage classification. bWhether done under running water; in a bowl by an individual or by several people.
Participants
We included nine trials with 15,303 children. In the community‐based trials, three trials were with very young children (< three years) (Haggerty 1988 COD; Langford 2007 NPL; Hartinger 2010 PER) ; two other trials were with children aged less than five years (Han 1985 MMR) or less than six years (Stanton 1985 BGD); and three involved older children up to 15 years of age (Luby 2003a PAK; Luby 2003b PAK; Luby 2006 PAK). Nicholson 2008 IND had four categories of participants: targeted children five years old, children less than five years old, children six to 15 years old, and adults in the families. The primary outcome measure (incidence of diarrhoea) was assessed in each of these categories with their corresponding control groups except for the adults reported as the 'whole family'. In this Cochrane Review we considered results from only the target group as the first three categories had similar effect size. Hand washing behavioural changes and changes in knowledge, attitude, and belief on hygiene were assessed in the mothers (number not strictly reported), while the primary outcome measures were assessed in the children.
The number of clusters varied from 18 (Haggerty 1988 COD) to 1923 (Stanton 1985 BGD). The participants were provided with hand washing materials and were involved in large‐group hygiene education training, except for Luby 2006 PAK which was a follow‐up trial. The intervention and control groups were socioeconomically comparable at baseline.
Outcome measures
All included trials measured diarrhoea episodes except for Luby 2006 PAK, which measured mean longitudinal prevalence of diarrhoea; some trials also assessed different types of diarrhoea. Han 1985 MMR measured dysentery rates, and Luby 2003a PAK and Luby 2003b PAK also assessed the rate of persistent diarrhoea. None of the included trials reported diarrhoea‐related deaths, all‐cause‐under five mortality, nor cost‐effectiveness data. Langford 2007 NPL reported changes in hand washing from baseline to endline at hand washing junctures, Stanton 1985 BGD reported on changes in hand washing behaviour, while Nicholson 2008 IND reported it using soap wrapper collected as a measure of soap consumption as an indirect measure. Length of follow‐up ranged from four to 12 months.
Adjustment for clustering
All trials adjusted for clustering in some way, except for Han 1985 MMR, Langford 2007 NPL, Nicholson 2008 IND, and Hartinger 2010 PER. Stanton 1985 BGD and Luby 2003a PAK adjusted for clustering by estimating rates at the group level; Luby 2003b PAK adjusted for clustering by calculating an ICC based on an analysis of variance level and design effect. Luby 2006 PAK though measured mean longitudinal prevalence of diarrhoea accounted for clustering using generalized estimating equations. Haggerty 1988 COD performed child and site level analyses; the 95% CIs were not provided for the site‐level analysis. The numerator (average number of episodes per child) was provided at the cluster level.
Hospital‐based trial (High‐risk group)
We identified only one trial in a high‐risk group (Huang 2007 USA). It individually randomized 148 adults with AIDS from one human immunodeficiency virus (HIV) clinic in the USA to receive intensive hand washing promotion delivered by specialist nurses (Huang 2007 USA). The intervention included hygiene education, hand washing demonstrations by nurses and participants, and weekly telephone calls to reinforce hand washing messages Table 7. The major outcomes reported were mean episodes of diarrhoea in each group and number of hand washing episodes per day. They reported the mean hand washing frequency per day at baseline and at the end of the intervention (Table 8).
4. Description of hand washing intervention among high‐risk group (AIDS patients).
| Trial | Promotional activity | Classificationa | Message content | Hand washing method | Hand washing styleb | Material provision | Water availability |
| Huang 2007 USA | Demonstration by nurses and patients | Hygiene education |
|
Water with soap | Under running water | Unclear (probably not relevant in this population) | Adequate |
aMessage classification. bWhether done under running water; in a bowl by an individual or by several people.
5. Hand washing in high‐risk group (AIDS patients): behavioural change outcomes and KAB.
| Trial | Cluster adjusted? | KAPa changes | Outcome | Intervention | Control | Effect size/P value |
| Huang 2007 USA | Individual randomization | Frequency of hand washing per day | Mean hand washing frequency per day at baseline | 3.3 | 3.4 | P value not significant |
| Mean hand washing frequency per day at endline | 7 | 4 | P value not provideda |
Abbreviations; KAB = knowledge, attitude, and beliefs. aPercentage change in the mean frequency of hand washing in the intervention arm is 109% versus 18% in the control arm.
Excluded studies
We have listed the excluded trials and the reasons for exclusion in the 'Characteristics of excluded studies' section.
Risk of bias in included studies
See Figure 2 and Figure 3 for a summary of the 'Risk of bias' assessment for all included trials.
Child day‐care centres or school based trials
Five of the 12 trials used an adequate method to generate the allocation sequence (Roberts 1996 AUS; Carabin 1997 CAN; Bowen 2004 CHN; Talaat 2008 EGY; Zomer 2012 NED); the method was unclear in the others. The method used to conceal allocation was unclear in all trials. In cluster‐RCTs, lack of concealment of allocation is not considered a major risk of bias since all clusters are usually randomized at the same time (Higgins 2011, Section 16.3.2).
Three trials reported blinding of the outcome assessors (Bartlett 1984 USA; Kotch 1989 USA; Roberts 1996 AUS); the rest were open trials. It was difficult to assess the number of randomized participants included in the analysis as this was reported at different levels (cluster, child, person time‐at‐risk). However, all trials were able to account for the number of randomized clusters included in the analysis.
Seven trials reported adequate comparability between the intervention and control groups with respect to diarrhoea incidence and sociodemographic characteristics (including mean total enrolment, percentage of drop outs, sex, age, and race composition of children enrolled, diapering, and toilet facilities) at baseline (Black 1977 USA; Bartlett 1984 USA; Butz 1990 USA; Ladegaard 1999 DEN; Bowen 2004 CHN; Talaat 2008 EGY; Pickering 2013 KEN). Investigators in Bowen 2004 CHN were forced to over‐ or under‐sample certain regions to obtain more 'control' schools after the original control schools were sent intervention packs by mistake and thus excluded. This trial reported small differences in household sanitation and piped water at baseline, but no differences between schools in number of students, class size, or hygiene infrastructure. Comparability at baseline was unclear in the two other trials (Kotch 1989 USA; Roberts 1996 AUS), while it was considered inadequate in two trials; Kotch 2003 USA reported baseline differences in total number of children and boys in favour of the intervention which they believed may have influenced the outcome measure and Zomer 2012 NED acknowledged baseline imbalance in crude incidence diarrhoeal episodes per child‐year of 3.0 for intervention versus 5.1 for the control but they applied statistical adjustments for this baseline characteristic. All trials reported collecting data at the same point in time for both the intervention and control groups.
Community‐based trials
Seven included trials reported adequate methods for generating allocation sequence (Stanton 1985 BGD; Luby 2003a PAK; Luby 2003b PAK; Luby 2006 PAK; Langford 2007 NPL; Nicholson 2008 IND; Hartinger 2010 PER). Only Luby 2003a PAK reported adequate allocation concealment; it was unclear in the other trials. Han 1985 MMR, Haggerty 1988 COD, Langford 2007 NPL and Hartinger 2010 PER reported blinding of outcome assessors, and the rest were open trials. Inclusion of all randomized participants in the analysis was unclear as it was reported at different levels of analysis (cluster, household, child) except for Nicholson 2008 IND, which reported 18% average attrition bias for all the subgroups in both arms.
Eight trials reported baseline similarity of diarrhoea morbidity and socioeconomic characteristics (including population/household size, socioeconomic status, hand washing and sanitary facilities, and sources of water supply) between the intervention and control groups (Han 1985 MMR; Stanton 1985 BGD; Luby 2003a PAK; Luby 2003b PAK; Luby 2006 PAK; Langford 2007 NPL; Nicholson 2008 IND; Hartinger 2010 PER). There were some differences at baseline in Haggerty 1988 COD (controls had diarrhoea episodes of longer duration than the intervention group). All the trials reported collecting data at the same period for intervention and control groups.
Hospital‐based trial (High‐risk group)
Huang 2007 USA did not clearly report the method of randomization or allocation concealment and did not use blinding. All 148 randomized participants were followed for the trial's one‐year duration. Participants were similar at the start of the trial in terms of age, sex, ethnicity, hand washing episodes per day, CD4 count, HIV load, and prophylaxis for opportunistic infections. The results were presented as a continuous outcome only (mean and SD of number of diarrhoea episodes in each arm over the year). This should be viewed with caution as it is likely that the distribution of diarrhoea episodes may be highly skewed (the mean of 1.24 and SD of 0.9 episodes in the intervention arm imply a non‐normal distribution of diarrhoea episodes). If so, the mean may not be the most appropriate measure of the 'average number' of episodes per participant. The trial reported collecting data at the same period for intervention and control groups.
Effects of interventions
See: Table 1; Table 2; Table 3
We have presented the results as reported by each trial in Table 8 (behavioural change), Table 9, Table 10, Table 11 (incidence of diarrhoea), Table 12, and Table 13. For trials with cluster‐adjusted results or where trials have been individually randomized, the data are summarized in forest plots. For trials where this was not possible, we have summarized the data in tables in the 'Data and analyses' section.
6. Incidence of diarrhoea in child day‐care centres and schools.
| Trial | Cluster adjusted? | Outcome and result | Method of assessment | Sample size |
| Bartlett 1984 USA | No | Diarrhoea rate per child‐year of observation Intervention: 0.71 (95% CI 0.65 to 0.77) Control: 0.81 (95% CI 0.75 to 0.87) |
|
26 day‐care centres with 374 children (196 intervention, 178 control) aged 0 to 3 years |
| Black 1977 USA | No | Diarrhoea incidence/100/child‐weeks of observation Intervention: 4.2/100/child‐week Control: 8.1/100/child‐week |
Daily record of attendance plus diarrhoea occurrence for each child by day‐care personnel | 4 day‐care centres (2 intervention, 2 control) with 116 children < 3 years |
| Bowen 2004 CHN | Yes | Median episodes of diarrhoea per 100 student weeks Expanded intervention: 0 per 100 student‐weeks Standard intervention: 0 per 100 student‐weeks Control: 0 per 100 student‐weeks |
Teachers trained using standardized case definitions to identify 10 symptoms or signs of illness and record these among students in class, 1 day per week; if parent's reported infection as cause of absence, teachers recorded name of syndrome and asked parent if child suffered any of 10 individual symptoms; verified verbally that reports of diarrhoea met case definition | 3962 children within 87 primary schools |
| Butz 1990 USA | No | Proportion of diarrhoea days per month Diarrhoea episodes/child‐days Intervention: 93/10,159 Control: 133/10,424 |
Daily symptom record for each child by care providers | 24 family day‐care homes with 108 children (58 intervention, 50 control) aged 1 month to 7 years |
| Carabin 1997 CAN | Yes | Diarrhoea incidence: episodes/100 child‐days at risk Incidence rate ratio (95% Bayesian credible interval) 1.10 (0.81 to 1.50), adjusted for age and gender Intervention alone: 0.77 (0.51 to 1.18) Monitoring alone: 0.73 (0.54 to 0.97) |
Daily record of diarrhoea episodes on calendar by educators | 52 day‐care centres with 1729 children aged 18 months to 3 years |
| Kotch 1989 USA | Yes | Diarrhoea rates: incidence density (episodes/child‐year) Intervention (< 2 years): 4.54 Intervention (> 2 years): 2.85 Control (< 2 years): 5.12 Control (> 2 years): 2.79 All: RR 1.19, 95% CI ‐0.48 to 1.96 |
|
24 day‐care centres with 389 children < 3 years |
| Kotch 2003 USA | No | Intervention group experienced significantly lower episodes of diarrhoea Incidence density score: Intervention: 0.90 diarrhoea illness per 100 child days. P < 0.001 Control: 1.58 diarrhoea illness per 100 child days. P < 0.001 Children in the intervention group sick with diarrhoea a lower proportion of days than children in the control group: Days ill with diarrhoea: Intervention: 4.0% Control: 5.0% P < 0.001 |
|
46 child‐care centres (23 child‐care centres in the intervention arm and 23 child‐care centres in the control arm) with 388 children (infants and toddlers < 36 months) |
| Ladegaard 1999 DEN | No | Diarrhoea episodes/child‐month Intervention: 33/848 Control: 61/1052 (34% reduction from 3.25 days per child in favour of children 3 years or more) |
Information on absenteeism recorded on a form by child‐care provider | 8 day‐care centres with 475 children (212 intervention, 263 control) aged 6 years and below |
| Pickering 2013 KEN | Yes | Hierarchical (Poisson) model result soap versus control; Diarrhea (defined as three or more loose/watery stool in 24 hours): RR 0.84, 95% CI 0.58 to 1.22; P = 0.36 Any loose/watery stool in 24 hours: RR 1.09 (95% CI 0.92 to 1.30). P = 0.33 Loose/watery stool identified on Bristol stool Chart: RR 1.04 (95% CI (0.85 to 1.29); P = 0.69 |
|
6 primary schools (2 each for Hand washing with soap (HWWS), Hand sanitizer and control) with a total of 1364 children participants. However, the intervention of interest (HWWS = 460; control = 469) therefore total = 929). aged between 5 to 10 years. |
| Roberts 1996 AUS | Yes | Diarrhoeal rates: episodes/child‐year Intervention: 1.9 episodes/child‐year Control: 2.7 episodes/child‐year All: RR 0.50, 95% CI 0.36 to 0.68 < 2 years: RR 0.90, 95% CI, 0.67 to 1.19 > 2 years: RR 0.48, 95% CI 0.29 to 0.78 (Adjusted for clustering by centre, confounding variables (age, sex, weight at birth, breastfeeding status, child care history, and home factors), and interactions between age and intervention status, and between having a sibling who attends child care and intervention status) |
|
23 day‐care centres (11 intervention, 12 control) with 558 children under 3 years |
| Talaat 2008 EGY | No | Diarrhoea episodes Intervention: 639 episodes Median IQR: 0.2 (0.0 to 0.5) Control: 1316 episodes Median IQR: 0.3 (0.1 to 0.6) 33% reduction P < 0.0001 Incidence of absenteeism caused by diarrhoea was 33% lower in school children in the intervention schools. |
|
60 elementary schools (30 intervention, 30 control) with 44,451 children (20,882 intervention; 23,569 control) Median age: 8 years |
| Zomer 2012 NED | Yes | Diarrhoeal rates: episodes/child‐year (7 symptom‐free days between episodes) Intervention: 3.0 episodes/child‐year Control: 3.4 episodes/child‐year IRR 0.90, 95% CI 0.73 to 1.11 P value: 0.32 |
|
71 day‐care centres (DCC) (36 intervention; 35 control 35) with 545 children (278 from 34 intervention DCC and 267 from 35 control DCC) |
Abbreviations: CI: confidence interval; IQR: interquartile range.
7. Incidence of diarrhoea in communities.
| Trial | Cluster adjusted? | Outcome and result | Method of assessment | Sample size |
| Haggerty 1988 COD | Yes | Diarrhoea rates (mean episodes of diarrhoea ) Intervention site: 0.071 Control site: 0.075 (RR 0.94, 95% CI 0.85 to 1.05; P = 0.3) |
|
18 sites (9 intervention, 9 control) with 1954 children aged 3 months to 35 months |
| Han 1985 MMR | No | Incidence rate per 1000 child days of observation Intervention: 3.5 Control: 4.9 Incidence density ratio 1. Diarrhoea < 2 years: 0.69 (95% CI 0.48 to 1.10) > 2 years: 0.67 (95% CI 0.45 to 0.98) All: 0.70 (95% CI 0.54 to 0.92) 2. Dysentery < 2 years: 0.59 (95% CI 0.22 to 1.55) > 2 years: 1.21 (95% CI 0.52 to 2.80) All: 0.93 (95% CI 0.39 to 2.23) |
Daily surveillance (24 hour recall) for diarrhoea and dysentery | 350 households (162 intervention, 188 control) with 494 children (236 intervention; 258 control) under 5 years |
| Hartinger 2010 PER | Unclear | Diarrhea episodes: Intervention: 287 diarrhoea episodes or a mean of 1.7 episodes per child year at risk Control: 365 diarrhoea episodes or a mean of 2.3 episodes per child year at risk |
Records and observations through monthly home visits | 534 children (267 intervention, 267 control) |
| Langford 2007 NPL | No | Diarrhoea episodes: children from intervention areas experienced on average 31% fewer episodes of diarrhoea than control counterparts Intervention: 3.0 episodes Control: 4.33 episodes P = 0.049 Intervention children also experienced 41% fewer days of diarrhoea than children in control areas, Diarrhoea incidence: Intervention: 9.67 person days Control: 16.33 person days P = 0.023 |
|
88 children (45 intervention, 43 control) aged 3 to 12 months old had complete data sets |
| Luby 2003a PAK | Yes | Incidence density of diarrhoea (number of new episodes of diarrhoea divided by the at‐risk person‐weeks of observation) Mean incidence 1. Primary diarrhoea Intervention: Antibacterial soap: 2.02 Plain soap: 1.91 Control: 4.06 2. Persistent diarrhoea Intervention: Antibacterial soap: 0.14 Plain soap: 0.12 Control: 0.17 |
Weekly observational visits to households | 36 neighbourhoods (25 intervention, 11 control) with 4691 children (3163 intervention, 1528 control) aged < 15 years |
| Luby 2003b PAK | Yes | Diarrhoea episodes/100 child‐weeks: for diarrhoea and persistent diarrhoea Intervention: 3.71 Control: 6.56 RR 0.57, 95% CI 0.35 to 0.86 Diarrhoea, mean incidence: 3.71 Persistent diarrhoea, mean incidence: 0.09 ‐52% (‐100% to 100%) |
Weekly observational visits to households | 18 clusters (544 households; 262 intervention; 282 control) with children < 15 years |
| Luby 2006 PAK | Yes | Crude diarrhoea longitudinal prevalence (%) 1.58 Modeled risk difference (%) vs. control ‐0.16 (95% CI 0.92 to 0.60) |
Weekly observational visits to household/ self reports | 577 households including the hand washing promotion (195 households), hand washing promotion plus water treatment (186 households) and control arm (195 households). |
| Nicholson 2008 IND | No | Per protocol analyses for diarrhoea incidence; episodes per 100 person weeks
|
|
35 matched pairs communities (70 in total for intervention and control); 30 households from each of the communities. Target children (5 year olds) = 2052 (intervention: 1026; control: 1026); under 5 years of age = 2469 (intervention: 1190; Control: 1279); 6 to 15 years = 3519 (intervention: 1784; control: 1735); adults = 3685 (intervention: 1892; control: 1793) All subjects = 11,725 (intervention: 5892; control: 5833) Age: 5 year old children (Target); under‐5 years of age, children 6 to15 years and adults (non‐targets) |
| Stanton 1985 BGD | Yes | Rate of diarrhoea per 100 person‐weeks of observation Intervention: 4.29 Control: 5.78 Incidence density ratio 0.75 (95% CI 0.66 to 0.84; P < 0.0001) < 2 years: 0.54 (95% CI 0.43 to 0.66) > 2 years: 0.68 (95% CI 0.54 to 0.85) |
|
1923 families (937 intervention, 986 control) with children aged < 6 years |
Abbreviations: CI: confidence interval.
8. Incidence of diarrhoea in high risk group (AIDS patients).
| Trial | Cluster adjusted? | Outcome and result | Method of assessment | Sample size |
| Huang 2007 USA | Not applicable | Mean episodes of diarrhoea over trial period (1 year) Intervention group: 1.24 (± 0.9) Control group: 2.92 (± 0.6) |
Daily hand washing diary to record number of hand washing episodes per day and diarrhoea diary to record stool frequency and characteristics; weekly telephone calls from trial nurse to ascertain episodes of these outcomes | 75 in hand washing group, 73 controls |
Abbreviations: CI: confidence interval.
9. Hand washing in child day care centres and schools: behavioural change outcomes and KAB.
| Trial | Cluster adjusted? | Measured by | Outcome | Intervention | Control | Effect size or P value |
| Kotch 1989 USA | Yes | Recorded observations at 5 week intervals | Mean hand washing behaviour score after changing a diaper (0 = none, 0.5 = partial, 1 = correct) | 0.75 | 0.37 | P < 0.01 |
| Mean hand washing behaviour score after contact with child's mucus, saliva, vomit, etc (0 = none, 0.5 = partial, 1 = correct) | 0.66 | 0.21 | P < 0.01 | |||
| Pickering 2013 KEN | Yes | Hand washing events observed 2 to 4 days per week per school | Proportion of people washing hands after toilet use | 38% | 37% | P > 0.05 |
| Proportion of people washing hands with soap after toilet use | 37% | 2% | P < 0.05 | |||
| Proportion of people washing hands before lunch | 82% | 69% | P > 0.05 | |||
| Proportion of students washing hands with soap before lunch | 70% | 1% | P < 0.05 | |||
| Roberts 1996 AUS | Yes | Observation for compliance of recommended practices every 6 weeks | Compliance of children washing their hands | 53% to > 80% | Not reported | Not reported |
| Zomer 2012 NED | Yes | Observation for hand hygiene compliance at 6 months follow‐up | Compliance of caregivers with hand hygiene guidelines | 59% | 44% | OR 4.13, 95% CI 2.33 to 7.32 |
Abbreviations: KAB = knowledge, attitude, and beliefs; OR = odds ratio.
10. Hand washing in communities: behavioural change outcomes and KAB.
| Trial | Cluster adjusted? | Measured by | Outcome | Intervention | Control | Effect size/P value |
| Langford 2007 NPL | Approximately adjusted | Trial staff completed questionnaires with mothers self‐reporting their hand washing behaviour | Proportion washing hands after visiting the toilet | 100% | 90.7% | 0.500 |
| Proportion washing hands after cleaning baby's bottom | 100% | 83.7% | 0.031 | |||
| Proportion washing hands before cooking | 71.1% | 2.3% | < 0.001 | |||
| Proportion washing hands before feeding the baby | 62.2% | 18.6% | 0.004 | |||
| Proportion washing hands before eating | 60% | 0% | 0.003 | |||
| Nicholson 2008 IND | Approximately adjusted | Hand washing behaviour indirectly assessed using soap consumption (soap wrapper collection) | Median soap consumption per household per week | 235 g | 45 g | |
| Stanton 1985 BGD | Yes | Comparison of hygienic practices after intervention | Proportion of mothers who wash their hands before preparing food | 39/79 (49%) | 25/75 (33%) | RR 1.48, 95% CI 1.01 to 2.21; P = 0.056 |
Abbreviations; KAB = knowledge, attitude, and beliefs.
1. Child day‐care centres or schools
1.1. Incidence of diarrhoea
Overall, hand washing promotion reduced diarrhoea episodes by about a third (IRR 0.69, 95% CI 0.59 to 0.81; 11 trials, 50,044 children (Bowen 2004 CHN not included in analysis); Analysis 1.1). Most data were from high income countries (IRR 0.70, 95% CI 0.58 to 0.85; nine trials, 4664 participants; high quality evidence; Analysis 1.1), with only two trials from LMICs (IRR 0.66, 95% CI 0.43 to 0.99; two trials, 45,380 participants; low quality evidence; Analysis 1.1).
1.1. Analysis.
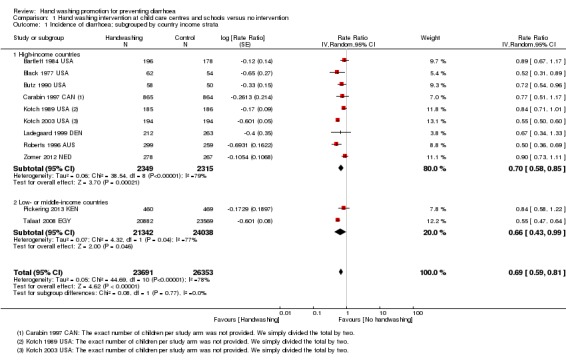
Comparison 1 Hand washing intervention at child care centres and schools versus no intervention, Outcome 1 Incidence of diarrhoea; subgrouped by country income strata.
All trials showed a benefit from the intervention, except for Bowen 2004 CHN which showed no difference between each arm and for which it was not possible to calculate a rate ratio (the median episodes of diarrhoea were 0 per 100 student‐weeks in the control group, standard intervention group, and expanded intervention) (Table 9). Roberts 1996 AUS showed greater risk reduction than other trials (IRR 0.50, 95% CI 0.36 to 0.69; one trial, 558 participants), possibly due to a more specific technique of hand washing used (an approximate "count to 10" to wash and "count to 10" to rinse).
All participants were monitored at least every two weeks to collect data on diarrhoea episodes. This monitoring itself may have helped to improve compliance with hand washing. Only Carabin 1997 CAN attempted to investigate this effect by assessing rates in both groups compared to the pre‐intervention period. They found that monitoring alone appeared to reduce the incidence of diarrhoea (IRR 0.73, 95% CI 0.54 to 0.97; Table 9), and that the intervention effect did not appear to have any benefits over and above this monitoring effect when adjusted for age and gender (IRR 0.77, 95% CI 0.51 to 1.18; Table 9) or when adjusted for age, gender, season, and baseline incidence rate in each cluster (IRR 1.10, 95% CI 0.81 to 1.50; Table 9). However, monitoring was particularly frequent (daily) in this trial. In the Bowen 2004 CHN trial among first grade students in schools in China, monitoring may have been less intensive as in‐class monitoring was carried out one day a week by teachers; reasons for absenteeism were noted when recorded. As the trial was school‐based, no illness information was collected during weekends or school holidays. This design reduced the burden of data collection of teachers, but it may also have reduced the ability of the trial to detect differences in the incidence of diarrhoea between each trial arm.
Two trials, Black 1977 USA and Pickering 2013 KEN, focused only on hand washing intervention and there was no significant difference the effect estimate (IRR 0.69; 95% CI 0.43 to 1.09; two trials, 1045 participants). Nine trials (Bartlett 1984 USA; Kotch 1989 USA; Butz 1990 USA; Roberts 1996 AUS; Carabin 1997 CAN; Ladegaard 1999 DEN; Kotch 2003 USA; Talaat 2008 EGY; Zomer 2012 NED) involved multiple hygiene interventions (IRR 0.69; 95% CI 0.57 to 0.84; nine trials, 48,999 participants; Analysis 1.2). The implication of this aspect of hand hygiene interventions should be further investigated as we had few trials in each category to make a statement.
1.2. Analysis.
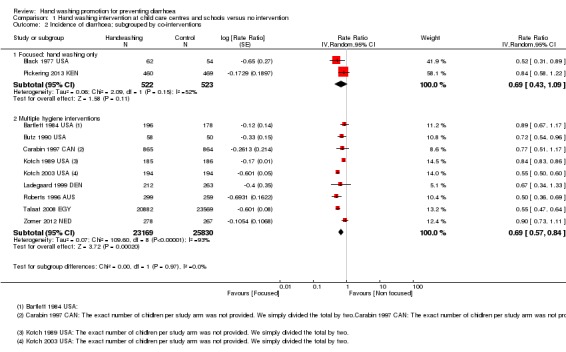
Comparison 1 Hand washing intervention at child care centres and schools versus no intervention, Outcome 2 Incidence of diarrhoea; subgrouped by co‐interventions.
Three trials (Bartlett 1984 USA; Kotch 1989 USA; Roberts 1996 AUS) attempted blinding (of outcome assessors) and the benefit of hand washing seemed to be less, 26% reduction (IRR 0.74, 95% CI 0.56 to 0.98; three trials, 1303 participants), than in the other trials that did not blind outcome assessors (Black 1977 USA; Butz 1990 USA; Carabin 1997 CAN; Ladegaard 1999 DEN; Kotch 2003 USA; Talaat 2008 EGY; Zomer 2012 NED; Pickering 2013 KEN), 33% reduction (IRR 0.67, 95% CI 0.56 to 0.80; eight trials, 48,741 participants; Analysis 1.3).
1.3. Analysis.
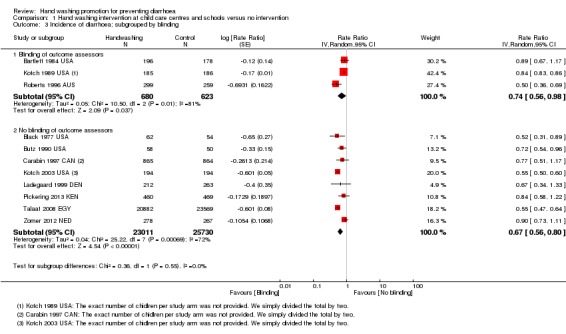
Comparison 1 Hand washing intervention at child care centres and schools versus no intervention, Outcome 3 Incidence of diarrhoea; subgrouped by blinding.
1.2. Behavioural changes
Four trials reported measures of behavioural change (Kotch 1989 USA; Roberts 1996 AUS; Zomer 2012 NED; Pickering 2013 KEN). As described in Table 12, Kotch 1989 USA reported that hand washing behaviour based on 'event sampling scores' improved in the intervention classrooms compared with control classrooms. Roberts 1996 AUS reported that the intervention improved compliance with infection control procedures from 53% at baseline to > 80% at endline. This was associated with a lower illness incidence in children aged ≥ two years (RR 0.34, 95% CI 0.17 to 0.65), reflecting a two‐third reduction in diarrhoeal episodes. Zomer 2012 NED reported significant increase in hand hygiene compliance for caregivers in intervention DCCs than in control but this did not seem to have effect on incidence of episodes of diarrhoea. Pickering 2013 KEN reported a statistically significant rate of hand washing with soap at intervention schools: 37% against 2% for the control for all toilet events (prevalence ratio 17.2; 95% CI 4.4 to 67.5), while the mean proportion (intervention: 0.70; control: 0.01) of students hand washing with soap before lunch events was equally significantly different between schools (prevalence ratio 143.0, 95% CI 38.9 to 525.6) (data not pooled; three trials, 1845 participants, low quality evidence; Table 12).
2. Community‐based trials
2.1. Incidence of diarrhoea
Overall, community based hand washing promotion reduced the incidence of diarrhoea by around a quarter (IRR 0.72, 95% CI 0.62 to 0.83; eight trials; 14,762 participants; high quality evidence; Analysis 2.1). Luby 2006 PAK reported mean longitudinal prevalence of diarrhoea for all children under observation with no apparent benefit of the intervention (Analysis 2.2). All the trials were conducted in LMICs; with six from Asia, one from South America, and one from Africa.
2.1. Analysis.
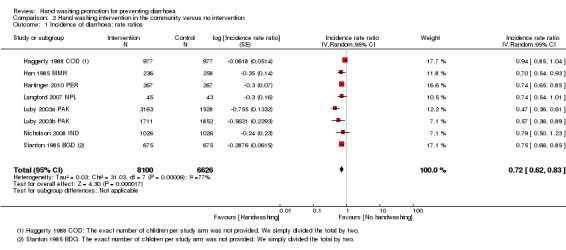
Comparison 2 Hand washing intervention in the community versus no intervention, Outcome 1 Incidence of diarrhoea: rate ratios.
2.2. Analysis.
Comparison 2 Hand washing intervention in the community versus no intervention, Outcome 2 Mean longitudinal prevalence.
| Mean longitudinal prevalence | |||||
|---|---|---|---|---|---|
| Study | Mean longitudinal prevalence of diarrhoea for all children under observation | SD | Co‐efficient of variation between clusters | Handwashing only | Handwashing with water promotion |
| Luby 2006 PAK | 1.68% | 0.00735 | 0.44 | Modeled risk difference (%) vs control (95% CI) ‐0.16 (‐0.92, 0.60) |
Modeled risk difference (%) vs control (95% CI)‐0.15 (0.92, 0.61) |
Three trials assessed the effect of intervention on the incidence rate of different categories of diarrhoea (Han 1985 MMR; Luby 2003a PAK; Luby 2003b PAK). Han 1985 MMR reported on dysentery, and Luby 2003a PAK and Luby 2003b PAK reported on persistent diarrhoea. None of the results were statistically significant (Table 9). Some trials reported the results by participant age (Han 1985 MMR; Stanton 1985 BGD; Luby 2003a PAK; Luby 2003b PAK; Nicholson 2008 IND), with no discernible trend of which age group intervention had greater diarrhoeal reductions (Table 9). Han 1985 MMR and Stanton 1985 BGD reported greater diarrhoeal reduction for children aged less than two years, while Luby 2003a PAK and Luby 2003b PAK reported greater reductions for older children. For Nicholson 2008 IND, the effect for the different age groups (five years old, less than five years, and six to 15 years) were similar.
Five trials (Han 1985 MMR; Luby 2003a PAK; Luby 2003b PAK; Langford 2007 NPL; Nicholson 2008 IND) promoted hand washing only while three trials promoted multiple hygiene interventions (Stanton 1985 BGD; Haggerty 1988 COD; Hartinger 2010 PER). The reduction in the risk of diarrhoea was greater in the trials that promoted hand washing only (IRR 0.63, 95% CI 0.52 to 0.78; 10,888 participants ) than in the trials that promoted multiple hygiene interventions (IRR 0.81, 95% CI 0.69 to 0.95; three trials, 3838 participants; Analysis 2.3). This aspect of hand hygiene interventions should be interpreted with caution as we had few trials in each category to make strong statement.
2.3. Analysis.
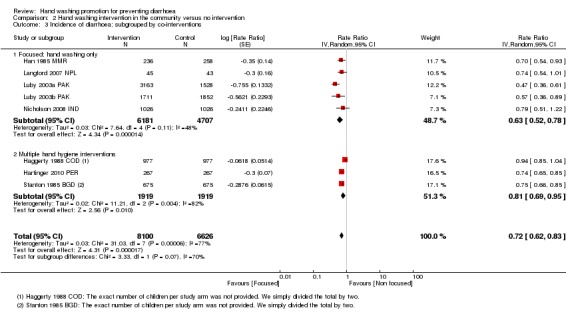
Comparison 2 Hand washing intervention in the community versus no intervention, Outcome 3 Incidence of diarrhoea; subgrouped by co‐interventions.
Four trials attempted blinding of outcome assessors and the benefit of hand washing appeared to be lower than in trials which did not blind outcome assessors (IRR 0.80, 95% CI 0.67 to 0.94; four trials, 3070 participants; versus IRR 0.63, 95% CI 0.48 to 0.83; four trials, 11,656 participants; Analysis 2.4).
2.4. Analysis.
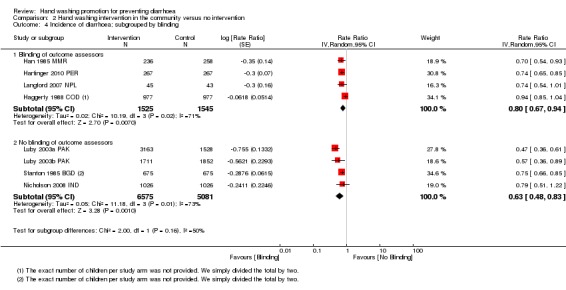
Comparison 2 Hand washing intervention in the community versus no intervention, Outcome 4 Incidence of diarrhoea; subgrouped by blinding.
Six trials provided soap free alongside hand hygiene promotional activities and the effect seemed to be larger in these trials than in those which did not provide soap (IRR 0.66, 95% CI 0.56 to 0.78; six trials, 11,422 participants; versus IRR 0.84, 95% CI 0.67 to 1.05; two trials, 3304 participants; Analysis 2.5).
2.5. Analysis.
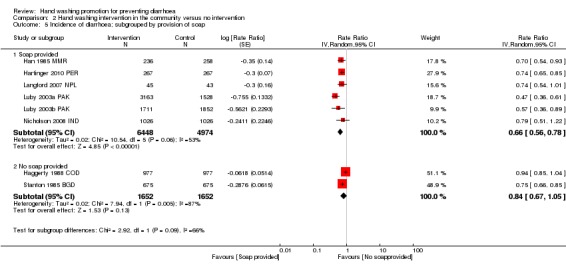
Comparison 2 Hand washing intervention in the community versus no intervention, Outcome 5 Incidence of diarrhoea; subgrouped by provision of soap.
With only a small number of trials, these differences may be due to chance or, even if real, it is difficult to discern which components (providing soap or focusing on hand washing only) may be most effective.
2.2. Behavioural changes
Stanton 1985 BGD adjusted for clustering and reported that the intervention group exhibited a greater increase in hygiene practices (IRR 1.48, 95% CI 1.01 to 2.21), though this increase is of borderline statistical significance (P = 0.056; Table 13). Langford 2007 NPL reports that at the end of the intervention, reported hand washing after cleaning the baby's bottom or before cooking, eating, or feeding the baby had increased in mothers from the intervention areas (McNemar's test, P < 0.01 for all four junctures), while hand washing practices remained unchanged in the control areas. Nicholson 2008 IND measured hand washing behaviour between trial groups indirectly by assessing soap consumption (soap wrapper collection) and reported median soap consumption per household per week of 235g for intervention households as against 45g for the controls (data not pooled; three trials, 3490 participants, high quality evidence; Table 13).
3. Hospital‐based trial (High‐risk group)
3.1. Episodes of diarrhoea
In Huang 2007 USA, the intensive hand washing intervention reduced the mean number of episodes of diarrhoea over the one‐year period of trial (2.92 in control group; 1.24 in intervention group; a reduction of 1.68 episodes, 95% CI ‐1.93 to ‐1.43; 148 participants, moderate quality evidenceAnalysis 3.1).
3.1. Analysis.
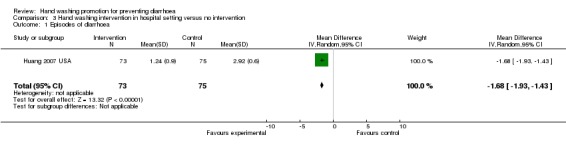
Comparison 3 Hand washing intervention in hospital setting versus no intervention, Outcome 1 Episodes of diarrhoea.
3.2. Behavioural changes
At the beginning of the trial there was no difference in daily hand washing frequency between intervention and control groups (3.4 ± 1.1 in control group; 3.3 ± 0.98 in intervention group; Table 8), but at the end of the trial the intervention group reported hand washing seven times a day compared with four times daily in the control group (P < 0.05) (moderate quality evidence).
Discussion
In the original review, Ejemot‐Nwadiaro 2008, 14 trials met the inclusion criteria. We have included eight additional trials in this Cochrane Review update, giving a total of 22 included trials. One of the eight additional trials, Luby 2006 PAK, was a follow‐up trial to Luby 2003b PAK. This trial involved no primary interventions. It assessed the sustainability of the Luby 2003b PAK hand hygiene interventions in preventing diarrhoea. The other trials had primary interventions.
Summary of main results
Hand washing promotion at child day‐care facilities or schools prevents around one‐third of diarrhoea episodes in high income countries (high quality evidence). It may prevent a similar proportion in LMICs but only two trials from urban Egypt and Kenya have evaluated this (low quality evidence).
Hand washing promotion among communities in LMICs probably prevents around one‐quarter of diarrhoea episodes (moderate quality evidence). However, six of these eight trials were from Asian settings, with only single trials from South America and sub‐Saharan Africa. In six trials soap was provided free alongside education and behavioural change interventions. The overall effect size was larger than in the two trials that did not provide soap. The influence of this on the intervention effect estimate is not well understood.
The effect of hand washing promotion in a hospital‐based setting among high‐risk population had significant reduction in mean episodes of diarrhoea that favoured intervention group (moderate quality evidence). This is only from one trial.
The effect of the intervention on hand hygiene related behavioural outcome in all settings showed increase in proportion of hand washing or hand hygiene compliance at essential junctures (before eating/cooking and after visiting the toilet or cleaning the baby's bottom) favouring the intervention groups (unpooled data; reflecting a range of low to high quality evidence).
We found no trials evaluating or reporting the effects of hand washing interventions on diarrhoea‐related deaths, all‐cause‐under five mortality, or costs.
Overall completeness and applicability of evidence
We believe we identified all RCTs that met our inclusion criteria. We further categorised the included trials into three distinct settings in this Cochrane Review: child day‐care centres or schools, community, and hospital. Although there were only a few trials included in each category, evidence favours hand washing intervention in preventing diarrhoea in all the settings. This suggests that the intervention exhibits population‐wide health gains. However, most included trials in the institution subcategory were from childcare settings in high‐income countries. Thus, we are not confident that this finding can be applied to schools in LMIC settings or alternative institutions. Also, only one hospital‐based trial met the inclusion criteria, so evidence from this setting was limited.
We are unsure of the effect of this intervention in populations with participants above five years of age and adults, as 95% of the participants in which the primary outcome was measured were below five years of age. One trial, Talaat 2008 EGY, measured the primary outcome in participants with a mean age of eight years but did not stratify the results by age. Nicholson 2008 IND measured the primary outcome in participants of various ages (target children aged five years, children below five years of age, children aged between six to 15 years and adults) and stratified results by these independent subgroups and reported effect sizes, with no significant trend observed. Therefore the effect of the intervention may not be generalizable to all age groups.
All included trials were relatively small‐sized and of short follow‐up duration including intensive monitoring and they demonstrated significant reduction in the risk of diarrhoea after hand hygiene intervention. However, in one relatively large trial, Bowen 2004 CHN, and one with longer follow‐up, Luby 2006 PAK, there were no apparent benefits as no significant differences between the incidence or longitudinal prevalence of diarrhoea was found. Therefore, we are unclear if the reductions in incidence of diarrhoea would be maintained if these trials had been larger and conducted over a longer time period.
The effect size was lower in child day‐care centres or school‐based trials that attempted blinding outcome assessors than in trials that did not (26% versus 33% reduction in the incidence of diarrhoea respectively). The same trend was observed for community‐based trials, with 18% reduction for trials that attempted blinding of outcome assessors and 35% reduction for trials that did not attempt blinding. This suggests a possible introduction of bias in trials that did not attempt blinding. However, there were too few trials in each category to make strong conclusions.
Quality of the evidence
We assessed the quality of evidence using the GRADE approach (GRADEpro 2014). In general, the evidence that hand washing reduces the incidence of diarrhoea in both child day‐care centres in high‐income countries and community settings in LMICs is considered high quality (Table 1; Table 2). Most trials were at high or unclear risk of detection or reporting bias due to no description of blinding of outcome assessors. However, this made negligible differences in our findings as restriction of the analysis to just the blinded trials found a slightly smaller but statistically significant effect size. In addition, the trials' results showed a lot of statistical heterogeneity. However, these inconsistencies did not affect the quality of evidence in these settings since all trials favoured the intervention though with varying effect size. We are therefore confident in the estimate of effect and further research is very unlikely to change our confidence in the estimate.
For the trials conducted in schools in LMICs, we considered the quality of evidence to be low due to indirectness as this limits our confidence in the effect estimate. The two trials, Talaat 2008 EGY and Pickering 2013 KEN, were conducted under experimentally controlled situations. Though they showed benefits in favour of the intervention groups, we are unsure if these benefits would be maintained if trials are replicated in a less controlled situations and in other settings.
Quality of evidence from unpooled data for the behavioural outcomes ranged from low to high in all the settings. These should be interpreted with caution as there were too few trials in each setting and method of assessment were too varied to make strong statements. The benefit of adopting an explicit behavioral change model is still unclear; this may influence the maintenance and sustainability of hand hygiene behaviour, as Whitby 2007 has opined that the strongest determinant of hand washing behaviour may be its habituation.The quality of evidence regarding the other outcomes (diarrhoea related deaths, all‐cause‐under five mortality, and cost‐effectiveness) were not determined due to paucity of included trials providing data on which to make such judgements. Thus, further research is necessary to provide a basis for assessment of evidence to these factors critical to hand washing intervention in preventing diarrhoea.
Potential biases in the review process
We did not identify any potential biases in the review process.
Agreements and disagreements with other studies or reviews
The magnitude of intervention effect (≃ 30%) in both child day‐care centres or schools and community settings we observed in this Cochrane Review did not differ significantly from that of the original review (Ejemot‐Nwadiaro 2008). The effect size however remains lower in magnitude than previous reviews of hand washing interventions; 47% (Curtis 2003); and about 44% in Fewtrell 2004 and Fewtrell 2005 reviews. These differences may be attributed to choice of effect measure, mixed trial designs, and single setting. Curtis 2003 used odds ratios, known to inflate effects sizes for conditions such as diarrhoea with common event rates in the analyses. In this Cochrane Review we reported only rate ratios, which Guevara 2004 opines improves clinical interpretation of pooled effect estimates. Fewtrell 2005 presented evidence of publication bias, while Curtis 2003 included case‐control and cross‐sectional trials as well as prospective interventions. Both reviews considered only hand hygiene interventions conducted in LMICs. In this Cochrane Review we included only RCTs and mixed settings (child day‐care centres or schools, community, and hospital based trials conducted in both developing and developed countries). However, they are all in agreement that hand hygiene interventions are effective in reducing diarrhoeal diseases.
Authors' conclusions
Implications for practice.
Hand washing promotion leads to reduction in diarrhoea episodes in both child day‐care centres in high‐income countries and among communities living in LMICs by about 30%. The challenge is to find ways of encouraging people to maintain hand washing habits in the longer term.
Implications for research.
The findings of this Cochrane Review show that further research to determine the efficacy of hand washing intervention in preventing diarrhoea will be unnecessary in child day‐care centres in high‐income countries and in communities in LMICs, although only one trial was conducted in Africa.
More trials conducted in child day‐care centres or schools in LMICs are needed to enhance our ability to generalize the intervention effects. The need to conduct research that is of longer follow‐up duration and uses a structured method of assessing the primary outcome is pertinent, since it has been observed that arbitrary use of methods may have significant effect on precision of estimates. Outcome assessors should be blinded so as to reduce the bias in estimates of effect size.
Evidence of hand washing on diarrhoea incidence in hospital based settings is still limited as we only found one trial that met the inclusion criteria. Therefore, further research in this area would be warranted.
Feedback
Search strategy, 7 December 2011
Summary
I have read the interesting Cochrane Review "Hand washing for preventing diarrhoea" conducted by you and your colleagues, published in The Cochrane Library 2009, issue 3. I would like to take the liberty to comment on the search strategies shown in Table 1:
Search set 8 and 9 are identical for MEDLINE and EMBASE – I assume one of them should be upper case to indicate MeSH/EMTREE, or? (The correct MeSH/EMTREE is DIARRHEA, not DIARRHOEA – but either maps to the correct term, and thus gives the same result)
I suggest you include handwashing$, diarrhoea$ and diarrhea$ as free text terms.
From the attached search sets it appears that you may have missed 98 and 61 potentially relevant records in MEDLINE and EMBASE respectively. Of course, this does not mean that you have not identified all relevant and available trials but it still poses a risk which I suggest you address in your next update of the review. How I searched MEDLINE and EMBASE, via Ovid (other databases were not searched):
Set 1‐11: Identical to the search shown in Table 1 (I assumed set 9 should be in upper case)
Set 12‐16: I added handwashing$ as free text term and show how many records are missed (set 16: records published before 2008)
Set 17‐22: Same as above, but added diarrhoea$ and diarrhea$ to the search (set 22: records published before 2008)
Also, it would be helpful to know how many records your retrieved in your initial searches, how many were excluded due to lack of relevance, methodological flaws etc., i.e. presented in a flowchart.
Best regards,
Ole Nørgaard
Reply
We agree with the contributor that there was an error in Table 1. We have corrected this. We do not believe that we have missed any relevant records, but as this review is due to be updated, we will investigate this further during the updating process. With regard to presenting the results in a flowchart, PRISMA diagrams were not expected in Cochrane Reviews at the time this review was initially produced. This will again be dealt with during the updating process.
Contributors
Ole Frandsen Nørgaard of the Department of Computer Science, Faculty of Health Sciences, University of Copenhagen, Denmark identified slight anomalies in the search strategy used in preparing the original review (Ejemot‐Nwadiaro 2008). We have incorporated his suggestions appropriately into this review update.
What's new
| Date | Event | Description |
|---|---|---|
| 26 August 2015 | New citation required but conclusions have not changed | Review updated and eight new trials included. |
| 26 August 2015 | New search has been performed | We updated the literature search and eight new trials met the inclusion criteria. We used GRADEpro 2014 to assess the quality of the evidence and have included 'Summary of findings' tables in this review update. Also, we have introduced the term 'promotion' into the review title. |
History
Protocol first published: Issue 2, 2003 Review first published: Issue 1, 2008
| Date | Event | Description |
|---|---|---|
| 17 January 2012 | Feedback has been incorporated | We are grateful to an observant reader who identified an error in the search strategy. We have now corrected this. |
| 8 August 2008 | Amended | We converted to new review format with minor editing. |
| 2 July 2008 | Amended | We removed trials that did not adjust for clustering from the meta‐analysis and presented the data in tables. Trials that did not adjust for clustering are clearly labelled in the Results, tables, and 'Characteristics of included studies' sections. We amended the Methods and Results to reflect these changes. |
Acknowledgements
We thank all trial authors that assisted us with information and clarifications regarding their trials. We are particularly grateful to Dr. S Luby of the Centers for Disease Control and Prevention (CDC) and Jonathan Kotch of University of North Carolina at Chapel Hill, USA. We thank Karin Schiöler and Jeppe Schroll for assisting with translation of the Danish trial. The first version of this review (Ejemot‐Nwadiaro 2008) was technically completed during the Cochrane Review Finishing School attended by Regina Ejemot‐Nwadiaro at Liverpool School of Tropical Medicine (LSTM) and organised by the Cochrane Infectious Diseases Group in June 2005.
This document is an output from a project funded by the UK Department for International Development (DFID) for the benefit of LMICs. The views expressed are not necessarily those of DFID.
Data and analyses
Comparison 1. Hand washing intervention at child care centres and schools versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of diarrhoea; subgrouped by country income strata | 11 | 50044 | Rate Ratio (Random, 95% CI) | 0.69 [0.59, 0.81] |
| 1.1 High‐income countries | 9 | 4664 | Rate Ratio (Random, 95% CI) | 0.70 [0.58, 0.85] |
| 1.2 Low‐ or middle‐income countries | 2 | 45380 | Rate Ratio (Random, 95% CI) | 0.66 [0.43, 0.99] |
| 2 Incidence of diarrhoea; subgrouped by co‐interventions | 11 | Rate Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Focused: hand washing only | 2 | 1045 | Rate Ratio (Random, 95% CI) | 0.69 [0.43, 1.09] |
| 2.2 Multiple hygiene interventions | 9 | 48999 | Rate Ratio (Random, 95% CI) | 0.69 [0.57, 0.84] |
| 3 Incidence of diarrhoea; subgrouped by blinding | 11 | Rate Ratio (Random, 95% CI) | Subtotals only | |
| 3.1 Blinding of outcome assessors | 3 | 1303 | Rate Ratio (Random, 95% CI) | 0.74 [0.56, 0.98] |
| 3.2 No blinding of outcome assessors | 8 | 48741 | Rate Ratio (Random, 95% CI) | 0.67 [0.56, 0.80] |
Comparison 2. Hand washing intervention in the community versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of diarrhoea: rate ratios | 8 | 14726 | Incidence rate ratio (Random, 95% CI) | 0.72 [0.62, 0.83] |
| 2 Mean longitudinal prevalence | Other data | No numeric data | ||
| 3 Incidence of diarrhoea; subgrouped by co‐interventions | 8 | 14726 | Rate Ratio (Random, 95% CI) | 0.72 [0.62, 0.83] |
| 3.1 Focused: hand washing only | 5 | 10888 | Rate Ratio (Random, 95% CI) | 0.63 [0.52, 0.78] |
| 3.2 Multiple hand hygiene interventions | 3 | 3838 | Rate Ratio (Random, 95% CI) | 0.81 [0.69, 0.95] |
| 4 Incidence of diarrhoea; subgrouped by blinding | 8 | Rate Ratio (Random, 95% CI) | Subtotals only | |
| 4.1 Blinding of outcome assessors | 4 | 3070 | Rate Ratio (Random, 95% CI) | 0.80 [0.67, 0.94] |
| 4.2 No blinding of outcome assessors | 4 | 11656 | Rate Ratio (Random, 95% CI) | 0.63 [0.48, 0.83] |
| 5 Incidence of diarrhoea; subgrouped by provision of soap | 8 | Rate Ratio (Random, 95% CI) | Subtotals only | |
| 5.1 Soap provided | 6 | 11422 | Rate Ratio (Random, 95% CI) | 0.66 [0.56, 0.78] |
| 5.2 No soap provided | 2 | 3304 | Rate Ratio (Random, 95% CI) | 0.84 [0.67, 1.05] |
Comparison 3. Hand washing intervention in hospital setting versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Episodes of diarrhoea | 1 | 148 | Mean Difference (IV, Random, 95% CI) | ‐1.68 [‐1.93, ‐1.43] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bartlett 1984 USA.
| Methods | Cluster‐RCT Method of allocation sequence: unclear Allocation concealment: unclear Blinding: assessor Inclusion of participants in the analysis: unclear Length of follow‐up: 12 months Cluster‐adjustment method: not adjusted |
|
| Participants | Number: 26 day‐care centres, with 374 children (196 intervention and 178 control) Inclusion criteria: not stated Exclusion criteria: not stated Age: < 3 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Diarrhoea rates | |
| Notes | Location: Maricopa County, Arizona, USA Duration: October 1981 to September 1984 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "22 day care centres were randomly selected from the 108 day care centers in Maricopa county licensed to care for infants and toddlers. The 22 trial day care centers were divided into three strata, based on surveillance rates of infant‐toddler diarrhea in the preceding 12 months. Half of the centers in each stratum were then randomly assigned to intervention groups." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Student nurses were blinded in regard to intervention or control status of the day care centres. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Black 1977 USA.
| Methods | Cluster‐RCT Method of allocation sequence: unclear Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 6 months Cluster‐adjustment method: not adjusted |
|
| Participants | Number: 4 day‐care centres, with 116 children Inclusion criteria: not stated Exclusion criteria: not stated Age: < 3 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: suburban Atlanta, Georgia, USA Duration: June 1976 to April 1977 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Bowen 2004 CHN.
| Methods | Cluster‐RCT Method of allocation sequence: random‐number table Allocation concealment: unclear Blinding: none Inclusion of all participants in the analysis: 93% (3962/4256) agreed to participate Length of follow‐up: 2003 to 2004 school year Cluster‐adjustment method: adjusted |
|
| Participants | Number: 87 schools (57 intervention; 30 control); with 3962 children (2670 intervention; 1292 control) Inclusion criteria: public primary schools; at least 20 students in first grade year in 2003 to 2004; no overnight boarders; at least 1 running water tap for every 30 first grade students Exclusion criteria: no compulsory hand washing or provision of hand‐cleaning products before school lunch; no commercial hand washing promotion programmes at school during previous 5 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: 3 counties in Fujian province, South‐East China | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3962 (93%) first‐grade students from the 4,256 first ‐graders attending the enrolled schools agreed to participate and were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Butz 1990 USA.
| Methods | Cluster‐RCT Method of allocation sequence: unclear Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 12 months Cluster‐adjustment method: not adjusted |
|
| Participants | Number: 24 family day‐care centres, with 108 children (58 intervention, 50 control) Inclusion criteria: not stated Exclusion criteria: unclear Age: 1 month to 7 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Incidence of infectious disease symptoms (diarrhoea) | |
| Notes | Location: Baltimore, Maryland, USA Duration: 12 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 28 children (114 children were enrolled from the FDCHs but actual number of children used in the analysis is 86). |
| Selective reporting (reporting bias) | Unclear risk | Did not measure the relative contribution of each component of intervention, however "to reduce reporting bias, all day care providers were aware that the intervention program was being tested in certain homes". |
| Other bias | Low risk | None observed. |
Carabin 1997 CAN.
| Methods | Cluster‐RCT Allocation sequence: day‐care centres were stratified by incidence of respiratory infections and block randomized by geographical areas Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 6 months Cluster‐adjustment method: adjusted |
|
| Participants | Number: 52 day‐care centres, with 1729 children Inclusion criteria: presence of at least 1 sandbox and 1 play area; at least 12 available toddler places Exclusion criteria: not stated Age: 18 months to 3 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Diarrhoea rates | |
| Notes | Location: Quebec, Canada Duration: September 1996 to November 1997 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated‐ block randomized. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 43 children lost to follow‐up (5 day care centres excluded from the analysis). |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Haggerty 1988 COD.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: unclear Blinding: assessor Inclusion of participants in the analysis: unclear Length of follow‐up: 6 months Cluster‐adjustment method: adjusted and unadjusted results given |
|
| Participants | Number: 18 sites (9 intervention, 9 control), with 1954 children (977 intervention, 977 control) Inclusion criteria: not stated Exclusion criteria: not stated Age: 3 months to 35 months |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Diarrhoeal rates | |
| Notes | Location: Kikwit, Bandundu Province, Zaire (Democratic Republic of Congo) Duration: October 1987 to December 1988 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Observers blind to the diarrhoea histories of families. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 190 children enrolled in the follow‐up were excluded form the analysis. |
| Selective reporting (reporting bias) | Low risk | 1954 children were enrolled in the follow‐up trial but 1764 were retained for analysis. 190 were lost to follow‐up. |
| Other bias | High risk | Reported some baseline differences (Control group had diarrhoea episodes of longer duration than the intervention group). |
Han 1985 MMR.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: unclear Blinding: assessor blinded Inclusion of participants in the analysis: unclear Length of follow‐up: 4 months Cluster‐adjustment method: not adjusted |
|
| Participants | Number: 350 households (162 intervention and 188 control) with 494 children (236 intervention, 258 control) Inclusion criteria: households with 1 or more children between 6 and 59 months; those in which regular follow‐up was possible; not allergic to soap; gave informed consent Exclusion criteria: not stated Age: < 5 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
|
|
| Notes | Location: Nga‐Kha ward of Thin‐Gun‐Kyun township, Rangoon, Burma (now Myanmar) Duration: June to November 1985 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "to avoid bias staff were blind to which households were intervention or otherwise". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12 children (7 from intervention, 5 from control households) out of the 494 enrolled. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Hartinger 2010 PER.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: unclear Blinding: participants and assessors Inclusion of participants in the analysis: unclear Length of follow‐up: 12 months Cluster‐adjustment method: unclear |
|
| Participants | Number: 534 households (267 intervention, 267 control) with 534 children (267 intervention, 267 control) Inclusion criteria:
Exclusion criteria:
Age: 6 to 35 months |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: San Marcos province, Cajamarca region, Peru Duration of trial: March 2008 to January 2010 (23 months) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized "...using covariate‐based constrained randomization as proposed by Moulton (2004)". Researchers went to extra lengths to ensure integrity of the randomizations. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "As a strategy to reduce non‐blinding bias, a child psychomotor development intervention was implemented in the control arm as an equivalent to the IHIP in the intervention arm". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "...and data collection was done by an independent team of field workers, which was not part of the initial education and re‐enforcement of the interventions during the follow‐up period". We consider this an attempt to blinding outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Researchers presented a detailed account of the randomization and follow‐up in a PRISMA flow diagram. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Huang 2007 USA.
| Methods | Individually RCT Allocation sequence: unclear Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: 100% Length of follow‐up: 1 year |
|
| Participants | Number: 73 intervention, 75 control Inclusion criteria: patients with AIDS at local HIV clinic; HIV‐1 infection verified by both ELISA and Western blot; AIDS by CD4 counts and plasma HIV RNA; been on highly active anti‐retroviral therapy (HAART) for at least 6 weeks and without diarrhoea for at least 3 months |
|
| Interventions | Both groups: 3 dedicated trial nurses educated participants on health problem associated with contaminated hands and provided specific hand washing instructions at enrolment; hand washing technique demonstrated by nurses, including wetting hands, lathering completely with soap, running together for at least 15 seconds, and drying hands with towels; all 148 participants then demonstrated adequate hand washing technique Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: USA (location unclear) Duration: 1 year (exact dates unclear) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Kotch 1989 USA.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment unclear Blinding: participants and assessors blinded Inclusion of participants in the analysis: unclear Length of follow‐up: 7 months Cluster‐adjustment method: adjusted |
|
| Participants | Number: 24 day‐care centres, with 389 classrooms Inclusion criteria: children < 3 years; present in the day care at least 20 hour per week; absence of chronic illness or medication that would predispose to infection; youngest of potentially eligible children in the same family; consenting English‐speaking parents with access a telephone; intending to remain in day‐care centre throughout trial Exclusion criteria: not stated Age: < 3 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Diarrhoeal rates | |
| Notes | Location: Cumberland County, North Carolina, USA Duration: October 1988 to May 1989 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | " specifically, parental illness reports were blind to the intervention status of their children's DCCs, potential confounders were controlled for and effect modifiers were examined". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 18 children dropped, 1 day care centre withdrew from the trial. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. |
| Other bias | Unclear risk | Unclear |
Kotch 2003 USA.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: not stated Blinding: open Inclusion of participants in the analysis: unclear Length of follow‐up: 7 months (November 2002 to May 2003) Cluster‐adjustment method: unclear |
|
| Participants | Number: 46 child‐care centres (23 intervention, 23 control) with 388 infants and toddlers Inclusion criteria:
Exclusion criteria: not stated Age: Infants and toddlers < 36 months |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: North Carolina, America Duration: September 2002 to May 2003 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Applied different statistical tests for different nature of variables: "No control variables are included in these descriptive comparisons". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Attrition form the intervention and control groups during the course of the trial was comparable". |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | High risk | "Two significant differences between the 2 trial groups were noted. The total number of children and the number of boys were larger in the intervention classrooms. These differences may have reduced the overall effect of the intervention, because number of children per classroom is a risk factor, and boys tend to stay in diapers longer. In addition, control centres were working hard to get their perceived reward (the free equipment that they were promised at the end of the trial). These 3 factors should have reduced the difference in outcomes between the intervention and control groups, suggesting that the significant differences in illnesses and absences that were found favouring the intervention group are all the more impressive". |
Ladegaard 1999 DEN.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 4 months Cluster‐adjustment method: not adjusted |
|
| Participants | Number: 8 day‐care centres, with 475 children (212 intervention, 263 control) Inclusion criteria: not stated Exclusion criteria: not stated Age: < 6 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Diarrhoeal rates | |
| Notes | Location: Odense, Denmark Duration: 6 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Kind of unclear whether they were divided in two groups manually and then randomized or randomized stratified. " The 8 institutions were allocated based on likeliness and randomised to intervention or control with 4 institutions in each". |
| Allocation concealment (selection bias) | Unclear risk | Randomization not described in detail. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | One institution had not written down attendance for the children 0‐2years. There were 212 children in the intervention group and 263 in the control group but no account over what happened to the children over time. |
| Selective reporting (reporting bias) | Low risk | No evidence of outcomes not presented. |
| Other bias | Low risk | None observed. |
Langford 2007 NPL.
| Methods | Cluster‐RCT Allocation sequence: flipping a coin Allocation concealment: unclear Blinding: assessor Inclusion of participants in the analysis: adequate (11 out of 99) Length of follow‐up: 6 months Cluster‐adjustment method: unclear |
|
| Participants | Number: 88 children (45 intervention, 43 control) Inclusion criteria: not stated Exclusion criteria: not stated Age: 3 to 12 months old |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: Kathmandu, Nepal Duration: May to November 2007 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Groups were randomly allocated by flipping a coin to intervention or control groups. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "To prevent bias in data collection, these field workers were never involved in any aspect of the program to promote handwashing". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 11 children from 99 originally recruited were not included in the analysis. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | High risk | "It was not possible to randomly allocate each separate settlement to control/intervention conditions as many sites were situated very close to one another (e.g. separated just by road or stream) such that the intervention message could easily have crossed over into control settlements." Comments: cross contamination possible. |
Luby 2003a PAK.
| Methods | Cluster‐RCT Allocation sequence: computer‐generated Allocation concealment: serially numbered Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 12 months Cluster‐adjustment method: adjusted |
|
| Participants | Number: 36 neighbourhoods (25 intervention, 11 control), with 4691 children (3163 intervention, 1528 control) Inclusion criteria: household located in the trial area; have at least 2 children < 5 years; intention to reside in the house for the duration of trial Exclusion criteria: not stated Age: < 15 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes | Diarrhoeal rates | |
| Notes | Location: low‐income squatter settlements, Karachi, Pakistan Duration: April 2002 to April 2003 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 139 children from the intervention arm and 85 from the control arm out of the 4691 children originally enrolled were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Luby 2003b PAK.
| Methods | Cluster‐RCT Allocation sequence: computer generated Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 9 months Cluster‐adjustment method: adjusted |
|
| Participants | Number: 18 clusters, with 544 households (262 intervention, 282 control) Inclusion criteria: households with at least 1 child < 5 years; provided informed consent Exclusion criteria: not stated Age range: < 15 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
|
|
| Notes | Location: multi‐ethnic squatter settlements in Central Karachi, Pakistan Duration: April 2003 to December 2003 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The five trial group were assigned a random number generated by a computer spread sheet. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described (open trial). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described (open trial). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clearly stated. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Luby 2006 PAK.
| Methods | Cluster‐RCT Allocation sequence: computer generated Allocation concealment: not described Blinding: open Length of follow‐up: 14 months (63 weeks) Cluster‐adjustment method: adjusted |
|
| Participants | Number: 577 households: hand washing promotion (195 households), hand washing promotion plus water treatment (187 households) and control arm (195 households). Inclusion criteria: same used in Luby 2003b PAK Exclusion criteria: same used in Luby 2003b PAK Age: children under 5 years |
|
| Interventions | Intervention (see Table 5 for detailed description): Follow‐up of earlier trial done in 2003 See Luby 2003b PAK |
|
| Outcomes |
|
|
| Notes | Location: Karachi, Pakistan Duration: 63 weeks |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | None. Trial is a follow‐up on Luby 2003a PAK |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One household was not accounted for in the analysis. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Nicholson 2008 IND.
| Methods | Cluster‐RCT Allocation sequence: coin tossing Allocation concealment: not described Blinding: open Length of follow‐up: 41 weeks Cluster‐adjustment method: not adjusted |
|
| Participants | 35 matched pairs communities (70 in total for intervention and control); 30 households from each of the communities. Target children = 2052 (intervention: 1026; control: 1026); under‐5 years of age = 2469 (intervention: 1190; control: 1279); 6 to 15 years = 3519 (Intervention: 1784; control: 1735); adults = 3685 (intervention: 1892; control: 1793) All subjects = 11,725 (intervention: 5892; control: 5833) Inclusion criteria: informed consent Exclusion criteria: not stated Age: 5 year old children (Target); under‐fives, children 6 to 15 years and adults (non‐targets) |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: West and South Mumbai, India. Duration: 22 October, 2007 to 02 August 2008 (41 Weeks) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Repeated coin‐tossing. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "It was impossible to 'blind' either the participants or those responsible for data collection." None (open trial). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "It was impossible to 'blind' either the participants or those responsible for data collection." None (open trial). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up in both arms and for all the sub‐groups were more than 10% (average attrition in all groups 18%). |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Pickering 2013 KEN.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: not described Blinding: open Length of follow‐up: 2 months (8 weeks) Cluster‐adjustment method: adjusted |
|
| Participants | Number: 6 schools (2 hand sanitizer; 2 hand washing with soap; 2 control). Student numbers: hand washing with soap (n = 460); hand sanitizer (n = 435); control (n = 469) Inclusion criteria: schools with > 100 student population; written consent from parents/teachers Exclusion criteria: schools that shared latrines with community members Age: 5 to 10 year old school children |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: Kibera, Nairobi, Kenya Duration: 2 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "schools randomly assigned to receive". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open trial. "Treatment assignment was not blinded". |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open trial. "Treatment assignment was not blinded". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clearly stated as they only reported total observations. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Roberts 1996 AUS.
| Methods | Cluster‐RCT Allocation sequence: computer generated Allocation concealment: unclear Blinding: assessors Inclusion of participants in the analysis: unclear Length of follow‐up: 9 months Cluster‐adjustment method: adjusted |
|
| Participants | Number: 23 day‐care centres, with 558 children Inclusion criteria: day‐care centres licensed in the Australian Capital Territory; children < 3 years as at January 1996; attendance for at least 3 days per week; have no underlying chronic illness that predisposes to infection Exclusion criteria: not stated Age: < 3 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
|
|
| Notes | Location: Australian Capital Territory, Australia Duration: March to November 1996 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a random number table generated using EpiInfo. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | None described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The observer was not informed of the content of the training sessions or the intervention status of the centers". "The staff members in the centers were aware the observer was watching hygiene practices but not which specific practices were being recorded". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 22% (123 children) from 558 children enrolled were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Unclear risk | Baseline comparable data not given. |
Stanton 1985 BGD.
| Methods | Cluster‐RCT Allocation sequence: table of random numbers Allocation concealment: unclear Blinding: none Inclusion of participants in the analysis: unclear Length of follow‐up: 6 months Cluster‐adjustment method: adjusted |
|
| Participants | Number: 1923 families (937 intervention, 986 control) with 1350 children (675 intervention, 675 control) Inclusion criteria: not stated Exclusion criteria: not stated Age: < 6 years |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
|
|
| Notes | Location: Urban Dhaka, Bangladesh Duration: October 1984 to May 1985 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomized allocation. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Equal number of emigrant and immigrant included in effectiveness analyses but not in behavioral assessment. |
| Selective reporting (reporting bias) | Low risk | None observed. |
| Other bias | Low risk | None observed. |
Talaat 2008 EGY.
| Methods | Cluster‐RCT Allocation sequence: computer generated random number table Allocation concealment: not stated Blinding: open Inclusion of participants in the analysis: adequate Length of follow‐up: 12 weeks (February to May 2008) Cluster‐adjustment method: adjusted |
|
| Participants | Number: 60 government elementary schools (30 intervention, 30 control), with 44,451 children (20,882 intervention, 23,569 control) Inclusion criteria: not stated Exclusion criteria: not stated Age: children in elementary schools (median age 8 years) |
|
| Interventions | Intervention (see Table 5 for detailed description):
School's contribution: Selecting a weekly hand hygiene champion, launching of school contest for drawing, songs and dramas that promote hygiene. Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: Cairo, Eygpt Duration: February to May 2008 (12 weeks) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 60 elementary schools were randomly selected by using a computer‐generated random number table. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Accounted for number enrolled for the trial in the analysis. |
| Selective reporting (reporting bias) | Low risk | Not observed. |
| Other bias | Low risk | "No significant differences were found for the 2 groups in median (8years), sex distribution (51% male) or the median number of students per school (635 [interquartile range 394‐978])". |
Zomer 2012 NED.
| Methods | Cluster‐RCT Allocation sequence: unclear Allocation concealment: not described Blinding: open Inclusion of participants in the analysis: adequate Length of follow‐up: November 2011 to March 2012 Cluster‐adjustment method: adjusted |
|
| Participants | Number: 71 day‐care centres (DCC) (intervention 36; control 35) with 545 children (278 from 34 intervention DCC and 267 from 35 control DCC) Inclusion criteria: children attended the DCC at least two days a week, aged between 6 months and 3 to 5 years, intended to attend the DCC throughout the trial period, if their parents consented, were Dutch speaking and had access to e‐mail or regular post. Exclusion criteria: if the child had chronic illness, if the child was on medication that predisposed him/her to infection and if was sibling is taking part in the trial (one per child per family participant) Age: children between 6 months to 60 months |
|
| Interventions | Intervention (see Table 5 for detailed description):
Control:
|
|
| Outcomes |
Not used in this review:
|
|
| Notes | Location: Rotterdam‐Rijnmond, Gouda and Leiden regions of Netherlands Duration: September 2011 to April 2012 (7 months) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomized allocation. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 553 children included in the trial; 545 included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Not observed. |
| Other bias | High risk | There were some differences in baseline characteristics between intervention and control group. "...the crude incidence of diarrhoeal episodes differed between intervention and control DCCs at baseline..." |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 1993 | Observational trial examining risk factors for diarrhoeal infections. |
| Aiello 2008 | Combined both randomized and quasi‐experimental trials in the analysis. Outcome measure was on general gastro‐intestinal tract (GIT) illnesses including diarrhoea. |
| Alam 1989 | Main intervention was provision of water supply through hand pumps. |
| Arnold 2009 | Cross‐sectional cohort intervention trial (non‐randomized study). |
| Arnold 2013 | Description of planned intervention trail design and rationale. |
| Azor‐Martinez 2014 | Acute gastroenteritis (AGE) outcome assessed, not specific to diarrhoea. |
| Barros 1999 | Observational trial examining risk factors for diarrhoeal infections. |
| Bieri 2013 | Hand washing not an intervention and diarrhoea not an outcome. |
| Biran 2009 | Hand washing an outcome not an intervention. |
| Biran 2014 | Diarrhoea not an outcome, assessed emotional drivers of behaviour for improving hand washing behaviours. |
| Boubacar Maïnassara 2014 | Mixed hygiene interventions not specific to hand washing. |
| Bowen 2012 | Diarrhoea not an outcome, assessed child growth and development. |
| Bowen 2013 | Did not assess diarrhoeal outcomes but assessed hand washing behaviours – one of our secondary outcome measures. |
| Burton 2011 | Measures effect on hand contamination not diarrhoeal rates. |
| Caruso 2014 | Diarrhoea not an outcome, assessed the effect of latrine cleaning and hand washing with soap intervention on school absenteeism. |
| Clasen 2014a | Hand washing promotion not an intervention. |
| Clasen 2014b | Hand washing promotion not specific intervention but latrine use/coverage. |
| Clemens 1987 | Observational trial examining risk factors for diarrhoeal infections. |
| Contzen 2015 | Non‐randomized trial. Diarrhoea incidence not assessed. |
| Correa 2012 | Trial did not promote handwashing but alcohol‐based hand rubs as complement to handwashing and control continued existing handwashing practices. |
| Curtis 2001 | No concurrent control. |
| Doebbeling 1992 | Outcome measure (incidence of nosocomial infection) not specific to diarrhoea episodes but to incidence of gastrointestinal infections in general. |
| Dreibelbis 2014 | Mixed hygiene intervention, not specific to hand washing. |
| Dyer 2000 | Intervention was instant hand sanitizer. |
| Fan 2011 | Non‐randomized study. |
| Freeman 2014 | Mixed water, sanitation and hygiene intervention, not specific to hand washing. |
| Greene 2012 | Measured exposure to fecal pathogen (risk of Escherichia coli). Hand contamination of E. coli. |
| Guinan 2002 | Observational study. |
| Hammond 2000 | Intervention did not involve hand washing. |
| Hartinger 2012 | Already included in the review update (Hartinger 2010 PER). |
| Huda 2012 | Assessed observed handwashing hygiene behaviours. |
| Hübner 2010 | Hand washing not an intervention (but measured the effectiveness of hand disinfection with alcoholic rubs). |
| Jinadu 2007 | Diarrhoea episodes not assessed rather hygiene behavioural change. |
| Johansen 2015 | Outcome measure not directly on diarrhoea but on infectious illness and school absenteeism. Paper describes the design of the RCT. |
| Khan 1982 | Case‐control study. |
| Larson 2003 | No relevant outcome measures. Assesed colony‐forming units of bacteria. |
| Larson 2004 | Outcome measure not specific to incidence of diarrhoea. |
| Lee 1991 | Controlled before‐and‐after study. |
| Luby 2001b | Observational trial. |
| Luby 2004 | Non‐randomized trial. |
| Luby 2007 | Diarrhoea episodes not assessed. Measured hand contamination. |
| Luby 2008 | Hand washing not an intervention but use of flocculant‐disinfectant for treating drinking water. |
| Luby 2010 | Diarrhoea episodes not assessed. Measured hand contamination. |
| Master 1997 | Outcome measure not specific on diarrhoeal episodes. |
| Morton 2004 | Outcome measure not specific on diarrhoeal episodes. |
| Oughton 2009 | Diarrhoea episodes not assessed but removal of Clostridium difficile. |
| Patel 2012 | Non‐randomized trial. |
| Peterson 1998 | Observational trial examining risk factors for diarrhoeal infections. |
| Pinfold 1996 | No comparable baseline information on diarrhoeal episodes provided. |
| Priest 2014 | Diarrhoea episodes not the outcome but illness absence including general GIT infection. |
| Rosen 2009 | Diarrhoea episodes not assessed. Tested effect of hand washing intervention on psychosocial measures. |
| Saboori 2013 | Diarrhoea episodes not assessed. Assessed hand washing episodes and E. coli hand contamination. |
| Savolainen‐Kopra 2012 | Outcome measure not specific to diarrhoeal morbidity but to incidence of GIT infection. |
| Shafique 2013 | Hand sanitizer not hand washing the intervention. Mean duration of diarrhoea and not diarrhoea episodes the main outcome measure. |
| Shahid 1996 | No comparable baseline information provided. |
| Sircar 1987 | No comparable baseline information on diarrhoea episodes provided. |
| Slayton 2013 | Hand towels the main intervention not hand washing. |
| Vindigni 2011 | Combined both randomized and quasi‐experimental trials in the analysis. Measured hand washing adherence. |
| White 2003 | Outcome measure not specific to diarrhoeal morbidity. |
| Wilson 1991 | Controlled before‐and‐after study. |
| Zhang 2013 | Diarrhoea not the direct outcome; Proxy data of 'stomach pain' was reported. |
| Zomer 2013 | Did not report data on diarrhoea outcome, paper describes the design of the RCT. |
Differences between protocol and review
We have introduced the term 'promotion' into the title of this Cochrane Review update. We added methods for assessing blinding and changed our primary outcome measure in the protocol from the relative risk of at least one diarrhoea episode to the incidence rate ratio for diarrhoea episodes. We pooled rate ratios in our analyses rather than relative risks since all trials presented diarrhoea as episodes, and removed "or standard hygiene promotion" as a control because it is included in the "no hand washing promotion" control group. We added all‐cause‐under five mortality and cost‐effectiveness as secondary outcome measures for this review update. We used GRADEpro 2014 to assess the quality of the evidence. In addition, we have included 'Summary of findings' tables in this update. Henry Ejere, a co‐author on the protocol, did not participate in preparation of the original review nor this review update. Dachi Arikpo joined as a co‐author in this review update.
Contributions of authors
Regina Ejemot‐Nwadiaro and Dachi Arikpo extracted and analysed data, and drafted the review. John Ehiri developed the protocol, drafted, and commented on the review. Julia Critchley extracted and analysed data, and edited the review. Martin Meremikwu helped finalize the data extraction form, drafted and commented on the review.
Sources of support
Internal sources
University of Calabar, Nigeria.
Institute of Tropical Diseases Research and Prevention (ITDR&P), Calabar, Nigeria.
Division of Health Promotion Sciences, University of Arizona, Mel & Enid Zuckerman College of Public Health, Tucson, Arizona, USA.
Liverpool School of Tropical Medicine (LSTM), UK.
Higher Education Funding Council for England, UK.
Cochrane Nigeria, Nigeria.
External sources
Department for International Development (DFID), UK.
Declarations of interest
Regina Ejemot‐Nwadiaro, John Ehiri, Dachi Arikpo, Martin Meremikwu and Julia Critchley declare that they have no conflicts of interest.
Unchanged
References
References to studies included in this review
Bartlett 1984 USA {published data only}
- Bartlett AV, Jarvis BA, Ross V, Katz TM, Dalia MA, Englender SJ, et al. Diarrheal illness among infants and toddlers in day care centers: effects of active surveillance and staff training without subsequent monitoring. American Journal of Epidemiology 1988;127(4):808‐17. [DOI] [PubMed] [Google Scholar]
Black 1977 USA {published data only}
- Black RE, Dykes AC, Anderson KE, Wells JG, Sinclair SP, Gary GW Jr, et al. Handwashing to prevent diarrhea in day‐care centers. American Journal of Epidemiology 1981;113(4):445‐51. [DOI] [PubMed] [Google Scholar]
Bowen 2004 CHN {published data only}
- Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E, et al. A cluster‐randomized controlled trial evaluating the effect of a handwashing‐promotion program in Chinese primary schools. American Journal of Tropical Medicine and Hygiene 2007;76(6):1166‐73. [PubMed] [Google Scholar]
Butz 1990 USA {published data only}
- Butz AM, Larson E, Fosarelli P, Yolken R. Occurrence of infectious symptoms in children in day care homes. American Journal of Infection Control 1990;18(6):347‐53. [DOI] [PubMed] [Google Scholar]
Carabin 1997 CAN {published data only}
- Carabin H, Gyorkos TW, Soto JC, Joseph L, Payment P, Collect JP. Effectiveness of a training program in reducing infections in toddlers attending day care centers. Epidemiology 1999;10(3):219‐27. [PubMed] [Google Scholar]
Haggerty 1988 COD {published data only}
- Haggerty PA, Muladi K, Kirkwood BR, Ashworth A, Manunebo M. Community‐based hygiene education to reduce diarrhoeal disease in rural Zaire: impact of the intervention on diarrhoeal morbidity. International Journal of Epidemiology 1994;23(5):1050‐9. [DOI] [PubMed] [Google Scholar]
Han 1985 MMR {published data only}
- Han AM, Hlaing T. Prevention of diarrhoea and dysentery by hand washing. Transactions of the Royal Society of Tropical Medicine and Hygiene 1989;83(1):128‐31. [DOI] [PubMed] [Google Scholar]
Hartinger 2010 PER {published data only}
- Hartinger S, Hattendorf J, Lanata C, Gil A, Verastegui H, Mausezahl D. Integrating home‐based environmental interventions (IHIP): A community‐randomised trial to improve indoor air pollution, drinking water quality and child nutrition in rural Peru. Tropical Medicine & International Health 2011;Supplement 16:354‐5. [Google Scholar]
- Hartinger SM, Lanata CF, Hattendorf J, Gil AI, Verastegui H, Ochoa T, et al. A community randomized controlled trial evaluating a home‐based environmental intervention package of improved stoves, solar water disinfection and kitchen sinks in rural Peru: rationale, trial design and baseline findings. Contemporary Clinical Trials 2011;32(6):864‐73. [DOI] [PubMed] [Google Scholar]
Huang 2007 USA {published data only}
- Huang DB, Zhou J. Effect of intensive handwashing in the prevention of diarrhoeal illness among patients with AIDS: a randomized controlled study. Journal of Medical Microbiology 2007;56(Pt 5):659‐63. [DOI] [PubMed] [Google Scholar]
Kotch 1989 USA {published data only}
- Kotch JB, Weigle KA, Weber DJ, Clifford RM, Harms TO, Loda FA, et al. Evaluation of an hygienic intervention in child day‐care centers. Pediatrics 1994;94(6 Pt 2):991‐4. [PubMed] [Google Scholar]
Kotch 2003 USA {published data only}
- Kotch JB, Isbell P, Weber DJ, Nguyen V, Savage E, Gunn E, et al. Hand‐washing and diapering equipment reduces disease among children in out‐of‐home child care centers. Pediatrics 2007;120(1):e29‐36. [DOI] [PubMed] [Google Scholar]
Ladegaard 1999 DEN {published data only}
- Ladegaard MB, Stage V. Hand‐hygiene and sickness among small children attending day care centres. An intervention study [Handhygiejne og smabornssygelighed i daginstitutioner: En interventionsundersogelse]. Ugeskrift for Laeger 1999;161(31):4396‐400. [PubMed] [Google Scholar]
Langford 2007 NPL {published data only}
- Langford R, Lunn P, Panter‐Brick C. Hand‐washing, subclinical infections, and growth: a longitudinal evaluation of an intervention in Nepali slums. America Journal of Human Biology 2011;23(5):621‐9. [DOI] [PubMed] [Google Scholar]
Luby 2003a PAK {published data only}
- Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, et al. Effect of handwashing in child health: a randomised controlled trial. Lancet 2005;366(9481):225‐33. [DOI] [PubMed] [Google Scholar]
- Luby SP, Agboatwalla M, Painter J, Altaf A, Billhimer WL, Hoekstra RM. Effect of intensive handwashing promotion on childhood diarrhea in high‐risk communities in Pakistan: a randomized controlled trial. JAMA 2004;291(21):2547‐54. [DOI] [PubMed] [Google Scholar]
Luby 2003b PAK {published and unpublished data}
- Luby SP, Agboatwalla M, Painter J, Altaf A, Billhimer W, Keswick B, et al. Combining drinking water treatment and hand washing for diarrhea prevention, a cluster randomised control trial. Tropical Medicine & International Health 2006;11(4):479‐89. [DOI] [PubMed] [Google Scholar]
Luby 2006 PAK {published data only}
- Luby SP, Agboatwalla M, Bowen A, Kenah E, Sharker Y, Hoekstra RM. Difficulties in maintaining improved handwashing behavior, Karachi, Pakistan. American Journal of Tropical Medicine and Hygiene 2009;81(1):140‐5. [PubMed] [Google Scholar]
Nicholson 2008 IND {published data only}
- Nicholson JA, Naeeni M, Hoptroff M, Matheson JR, Roberts AJ, Taylor D, et al. An investigation of the effects of a hand washing intervention on health outcomes and school absence using a randomised trial in Indian urban communities. Tropical Medicine & International Health 2014;19(3):284‐92. [DOI] [PubMed] [Google Scholar]
Pickering 2013 KEN {published data only}
- Pickering AJ, Davis J, Blum AG, Scalmanini J, Oyier B, Okoth G, et al. Access to waterless hand sanitizer improves student hand hygiene behavior in primary schools in Nairobi, Kenya. American Journal of Tropical Medicine and Hygiene 2013;89(3):411‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberts 1996 AUS {published data only}
- Roberts L, Jorm L, Patel M, Smith W, Douglas RM, McGilchrist C. Effect of infection control measures on the frequency of diarrheal episodes in child care: a randomized, controlled trial. Pediatrics 2000;105(4 Pt 1):743‐6. [DOI] [PubMed] [Google Scholar]
Stanton 1985 BGD {published data only}
- Stanton BF, Clemens JD. An educational intervention for altering water‐sanitation behaviors to reduce childhood diarrhea in urban Bangladesh. II. A randomized trial to assess the impact of the intervention on hygienic behaviors and rates of diarrhea. American Journal of Epidemiology 1987;125(2):292‐301. [DOI] [PubMed] [Google Scholar]
Talaat 2008 EGY {published data only}
- Talaat M, Afifi S, Dueger E, El‐Ashry N, Marfin A, Kandeel A, et al. Effects of hand hygiene campaigns on incidence of laboratory‐confirmed influenza and absenteeism in school children, Cairo, Egypt. Emerging Infectious Diseases 2011;17(4):619‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zomer 2012 NED {published data only}
- Zomer TP, Erasmus V, Looman CW, Tjon‐a‐Tsien A, Beeck EF, Graaf JM, et al. A hand hygiene intervention to reduce infections in child daycare: a randomized controlled trial. Epidemiology and Infection 2015 Jan 8 [Epub ahead of print]:1‐9. [DOI] [PMC free article] [PubMed]
References to studies excluded from this review
Ahmed 1993 {published data only}
- Ahmed NU, Zeitlin MF, Beiser AS, Super CM, Gershoff SN. A longitudinal study of the impact of behavioural change intervention on cleanliness, diarrhoeal morbidity and growth of children in rural Bangladesh. Social Science & Medicine 1993;37(2):159‐71. [DOI] [PubMed] [Google Scholar]
Aiello 2008 {published data only}
- Aiello AE, Coulborn RM, Perez V, Larson EL. Effect of hand hygiene on infectious disease risk in the community setting: a meta‐analysis. American Journal of Public Health 2008;98(8):1372‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alam 1989 {published data only}
- Alam N, Wojtyniak B, Henry FJ, Rahaman MM. Mothers' personal and domestic hygiene and diarrhoea incidence in young children in rural Bangladesh. International Journal of Epidemiology 1989;18(1):242‐7. [DOI] [PubMed] [Google Scholar]
Arnold 2009 {published data only}
- Arnold B, Arana B, Mäusezahl D, Hubbard A, Colford JM Jr. Evaluation of a pre‐existing, 3‐year household water treatment and handwashing intervention in rural Guatemala. International Journal of Epidemiology 2009;38(6):1651‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arnold 2013 {published data only}
- Arnold BF, Null C, Luby SP, Unicomb L, Stewart CP, Dewey KG, et al. Cluster‐randomised controlled trials of individual and combined water, sanitation, hygiene and nutritional interventions in rural Bangladesh and Kenya: the WASH Benefits study design and rationale. BMJ Open 2013;3(8):e003476. [DOI] [PMC free article] [PubMed] [Google Scholar]
Azor‐Martinez 2014 {published data only}
- Azor‐Martinez E, Cobos‐Carrascosa E, Gimenez‐Sanchez F, Martinez‐Lopez JM, Garrido‐Fernandez P, Santisteban‐Martinez J, Seijas‐Vazquez ML, Campos‐Fernandez MA, Bonillo‐Perales A. Effectiveness of a multifactorial handwashing program to reduce school absenteeism due to acute gastroenteritis. Pediatric Infectious Disease Journal 2014;33(2):e34‐9. [DOI] [PubMed] [Google Scholar]
Barros 1999 {published data only}
- Barros AJ, Ross DA, Fonseca WV, Williams LA, Moreira‐Filho DC. Preventing acute respiratory infections and diarrhoea in child care centres. Acta Paediatrica 1999;88(10):1113‐8. [DOI] [PubMed] [Google Scholar]
Bieri 2013 {published data only}
- Bieri FA, Gray DJ, Williams GM, Raso G, Li YS, Yuan L, et al. Health‐education package to prevent worm infections in Chinese schoolchildren. New England Journal of Medicine 2013;368(17):1603‐12. [DOI] [PubMed] [Google Scholar]
Biran 2009 {published data only}
- Biran A, Schmidt WP, Wright R, Jones T, Seshadri M, Isaac P, et al. The effect of a soap promotion and hygiene education campaign on handwashing behaviour in rural India: a cluster randomised trial. Tropical Medicine & International Health 2009;14(10):1303‐14. [DOI] [PubMed] [Google Scholar]
Biran 2014 {published data only}
- Biran A, Schmidt WP, Varadharajan KS, Rajaraman D, Kumar R, Greenland K, et al. Effect of a behaviour‐change intervention on handwashing with soap in India (SuperAmma): a cluster‐randomised trial. Lancet Global Health 2014;2(3):e145‐54. [DOI] [PubMed] [Google Scholar]
Boubacar Maïnassara 2014 {published data only}
- Boubacar Maïnassara H, Tohon Z. Assessing the health impact of the following measures in schools in Maradi (Niger): Construction of latrines, clean water supply, establishment of hand washing stations, and health education. Journal of Parasitology Research 2014;2014:190451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bowen 2012 {published data only}
- Bowen A, Agboatwalla M, Luby S, Tobery T, Ayers T, Hoekstra R. Association between intensive handwashing promotion and child development in Karachi, Pakistan: a cluster randomized controlled trial. Archives of Pediatrics & Adolescent Medicine 2012;166(11):1037‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bowen 2013 {published data only}
- Bowen A, Agboatwalla M, Ayers T, Tobery T, Tariq M, Luby S. Sustained improvements in handwashing indicators more than 5 years after a cluster‐randomised, community‐based trial of handwashing promotion in Karachi, Pakistan. Tropical Medicine & International Health 2013;18(3):259‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burton 2011 {published data only}
- Burton M, Cobb E, Donachie P, Judah G, Curtis V, Schmidt WP. The effect of handwashing with water or soap on bacterial contamination of hands. International Journal of Environmental Research and Public Health 2011;8(1):97‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Caruso 2014 {published data only}
- Caruso BA, Freeman MC, Garn JV, Dreibelbis R, Saboori S, Muga R, Rheingans R. Assessing the impact of a school‐based latrine cleaning and handwashing program on pupil absence in Nyanza Province, Kenya: a cluster‐randomized trial. Tropical Medicine and International Health 2014;19(10):1185‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clasen 2014a {published data only}
- Clasen T, Boisson S, Routray P, Torondel B, Bell M, Cumming O, Ensink J, Freeman M, Jenkins M, Odagiri M, Ray S, Sinha A, Suar M, Schmidt WP. Effectiveness of a rural sanitation programme on diarrhoea, soil‐transmitted helminth infection, and child malnutrition in Odisha, India: A cluster‐randomised trial. Lancet Global Health 2014;2:e645‐53. [DOI] [PubMed] [Google Scholar]
Clasen 2014b {published data only}
- Clasen T, Boisson S, Routray P, Torondel B, Jenkins M, Freeman M. The effectiveness of a rural sanitation intervention on health and ORISSA, India: A cluster randomized, controlled trial. 63rd Annual Meeting of the American Society of Tropical Medicine and Hygiene (ASTMH); 20141102‐06; New Orleans, In: American Journal of Tropical Medicine and Hygiene 2014;91(5 SUPPL):215. [Google Scholar]
Clemens 1987 {published data only}
- Clemens JD, Stanton BF. An educational intervention for altering water‐sanitation behaviors to reduce childhood diarrhea in urban Bangladesh. 1. Application of the case‐control method for development of an intervention. American Journal of Epidemiology 1987;125(2):284‐91. [DOI] [PubMed] [Google Scholar]
Contzen 2015 {published data only}
- Contzen N, Meili IH, Mosler HJ. Changing handwashing behaviour in southern Ethiopia: a longitudinal study on infrastructural and commitment interventions. Social Science and Medicine 2015;124:103‐114. [DOI] [PubMed] [Google Scholar]
Correa 2012 {published data only}
- Correa JC, Pinto D, Salas LA, Camacho JC, Rondón M, Quintero J. A cluster‐randomized controlled trial of handrubs for prevention of infectious diseases among children in Colombia. Revista Panamericana de Salud Pública 2012;31(6):476‐484. [DOI] [PubMed] [Google Scholar]
Curtis 2001 {published data only}
- Curtis V, Kanki B, Cousen S, Diallo I, Kpozehouen A, Sangaré M, et al. Evidence of behaviour change following a hygiene promotion programme in Burkina Faso. Bulletin of the World Health Organization 2001;79(6):518‐27. [PMC free article] [PubMed] [Google Scholar]
Doebbeling 1992 {published data only}
- Doebbeling BN, Stanley GL, Sheetz CT, Pfaller MA, Houston AK, Annis L, et al. Comparative efficacy of alternative hand‐washing agents in reducing nosocomial infections in intensive care units. New England Journal of Medicine 1992;327(2):88‐93. [DOI] [PubMed] [Google Scholar]
Dreibelbis 2014 {published data only}
- Dreibelbis R, Freeman MC, Greene LE, Saboori S, Rheingans R. The impact of school water, sanitation, and hygiene interventions on the health of younger siblings of pupils: a cluster‐randomized trial in Kenya. American Journal of Public Health 2014;104(1):e91‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dyer 2000 {published data only}
- Dyer DL, Shinder A, Shinder F. Alcohol‐free instant hand sanitizer reduces elementary school illness absenteeism. Family Medicine 2000;32(9):633‐8. [PubMed] [Google Scholar]
Fan 2011 {published data only}
- Fan VYM, Mahal A. What prevents child diarrhoea? The impacts of water supply, toilets, and hand‐washing in rural India. Journal of Development Effectiveness 2011;3(3):340‐70. [Google Scholar]
Freeman 2014 {published data only}
- Freeman MC, Clasen T, Dreibelbis R, Saboori S, Greene LE, Brumback B, et al. The impact of a school‐based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster‐randomized trial. Epidemiology and Infection 2014;142(2):340‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greene 2012 {published data only}
- Greene LE, Freeman MC, Akoko D, Saboori S, Moe C, Rheingans R. Impact of a school‐based hygiene promotion and sanitation intervention on pupil hand contamination in Western Kenya: a cluster randomized trial. American Journal of Tropical Medicine and Hygiene 2012;87(3):385‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guinan 2002 {published data only}
- Guinan M, McGuckin M, Ali Y. The effect of a comprehensive handwashing program on absenteeism in elementary schools. American Journal of Infection Control 2002;30(4):217‐20. [DOI] [PubMed] [Google Scholar]
Hammond 2000 {published data only}
- Hammond B, Ali Y, Fendler E, Dolan M, Donovan S. Effect of hand sanitizer use on elementary school absenteeism. American Journal of Infection Control 2000;28(5):340‐6. [DOI] [PubMed] [Google Scholar]
Hartinger 2012 {published data only}
- Hartinger SM, Lanata CF, Hattendorf J, Gil AI, Verastegui H, Mäusezahl D. A community randomized controlled trial of an integrated home‐based intervention improving household‐air pollution, drinking water quality and hygiene in rural Peru. 61st Annual Meeting of the American Society of Tropical Medicine and Hygiene (ASTMH); 2012 Nov 11‐15; Atlanta. American Journal of Tropical Medicine and Hygiene. 2012; Vol. 87, issue (5 Suppl 1):285.
Hübner 2010 {published data only}
- Hübner NO, Hübner C, Wodny M, Kampf G, Kramer A. Effectiveness of alcohol‐based hand disinfectants in a public administration: impact on health and work performance related to acute respiratory symptoms and diarrhoea. BMC Infectious Diseases 2010;10:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huda 2012 {published data only}
- Huda TM, Unicomb L, Johnston RB, Halder AK, Yushuf Sharker MA, Luby SP. Interim evaluation of a large scale sanitation, hygiene and water improvement programme on childhood diarrhea and respiratory disease in rural Bangladesh. Social Science and Medicine 2012;75(4):604‐11. [DOI] [PubMed] [Google Scholar]
Jinadu 2007 {published data only}
- Jinadu MK, Adegbenro CA, Esmai AO, Ojo AA, Oyeleye BA. Health promotion intervention for hygienic disposal of children's faeces in a rural area of Nigeria. Health Education Journal 2007;66(3):222‐8. [Google Scholar]
Johansen 2015 {published data only}
- Johansen A, Denbaek AM, Bonnesen CT, Due P. The Hi Five study: design of a school‐based randomized trial to reduce infections and improve hygiene and well‐being among 6‐15 year olds in Denmark. BMC Public Health 2015;15:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 1982 {published data only}
- Khan MU. Interruption of shigellosis by hand washing. Transactions of the Royal Society of Tropical Medicine and Hygiene 1982;76(2):164‐8. [DOI] [PubMed] [Google Scholar]
Larson 2003 {published data only}
- Larson E, Aiello A, Lee LV, Della‐Latta P, Gomez‐Duarte C, Lin S. Short‐ and long‐term effects of handwashing with antimicrobial or plain soap in the community. Journal of Community Health 2003;28(2):139‐50. [DOI] [PubMed] [Google Scholar]
Larson 2004 {published data only}
- Larson EL, Lin SX, Gomez‐Pichardo C, Della‐Latta P. Effect of antibacterial home cleaning and handwashing products on infectious disease symptoms: a randomized, double‐blind trial. Annals of Internal Medicine 2004;140(5):321‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 1991 {published data only}
- Lee W, Stoeckel J, Jintaganont P, Romanarak T, Kullavanijaya S. The impact of a community based health education program on the incidence of diarrheal disease in Southern Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 1991;22(4):548‐56. [PubMed] [Google Scholar]
Luby 2001b {published data only}
- Luby SP, Agboatwalla M, Raza A, Sobel J, Mintz ED, Baier K, et al. Microbiologic effectiveness of hand washing with soap in an urban squatter settlement, Karachi, Pakistan. Epidemiology and Infection 2001;127(2):237‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luby 2004 {published data only}
- Luby SP, Agboatwalla M, Hoekstra RM, Rahbar MH, Billhimer W, Keswick BH. Delayed effectiveness of home‐based intervention in reducing childhood diarrhea, Karachi, Pakistan. American Journal of Medicine and Hygiene 2004;71(4):420‐7. [PubMed] [Google Scholar]
Luby 2007 {published data only}
- Luby SP, Agboatwalla M, Billhimer W, Hoekstra RM. Field trial of a low cost method to evaluate hand cleanliness. Tropical Medicine & International Health 2007;12(6):765‐71. [DOI] [PubMed] [Google Scholar]
Luby 2008 {published data only}
- Luby SP, Mendoza C, Keswick BH, Chiller TM, Hoekstra RM. Difficulties in bringing point‐of‐use water treatment to scale in rural Guatemala. American Journal of Tropical Medicine and Hygiene 2008;78(3):382‐7. [PubMed] [Google Scholar]
Luby 2010 {published data only}
- Luby SP, Kadir MA, Yushuf Sharker MA, Yeasmin F, Unicomb L, Sirajul Islam M. A community‐randomised controlled trial promoting waterless hand sanitizer and handwashing with soap, Dhaka, Bangladesh. Tropical Medicine & International Health 2010;15(12):1508‐16. [DOI] [PubMed] [Google Scholar]
Master 1997 {published data only}
- Master D, Hess Longe SH, Dickson H. Scheduled hand washing in an elementary school population. Family Medicine 1997;29(5):336‐9. [PubMed] [Google Scholar]
Morton 2004 {published data only}
- Morton JL, Schultz AA. Healthy Hands: Use of alcohol gel as an adjunct to handwashing in elementary school children. Journal of School Nursing 2004;20(3):161‐7. [DOI] [PubMed] [Google Scholar]
Oughton 2009 {published data only}
- Oughton MT, Loo VG, Dendukuri N, Fenn S, Libman MD. Hand hygiene with soap and water Is superior to alcohol rub and antiseptic wipes for removal of Clostridium difficile. Infection Control and Hospital Epidemiology 2009;30(10):939‐44. [DOI] [PubMed] [Google Scholar]
Patel 2012 {published data only}
- Patel MK, Harris JR, Juliao P, Nygren B, Were V, Kola S, et al. Impact of a hygiene curriculum and the installation of simple handwashing and drinking water stations in rural Kenyan primary schools on student health and hygiene practices. American Journal Tropical Medicine and Hygiene 2012;87(4):594‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peterson 1998 {published data only}
- Peterson EA, Roberts L, Toole MJ, Peterson DE. Effect of soap distribution on diarrhoea: Nyamithuthu Refugee Camp. International Journal of Epidemiology 1998;27(3):520‐4. [DOI] [PubMed] [Google Scholar]
Pinfold 1996 {published data only}
- Pinfold JV, Horan NJ. Measuring the effect of a hygiene behaviour intervention by indicators of behaviour and diarrhoeal disease. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1996;90(4):366‐71. [DOI] [PubMed] [Google Scholar]
Priest 2014 {published data only}
- Priest P, McKenzie JE, Audas R, Poore M, Brunton C, Reeves L. Hand sanitizer provision for reducing illness absences in primary school children: a cluster randomised trial. PLoS Medicine 2014;11(8):e1001700. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosen 2009 {published data only}
- Rosen L, Zucker D, Brody D, Engelhard D, Manor O. The effect of a handwashing intervention on preschool educator beliefs, attitudes, knowledge and self‐efficacy. Health Education Resources 2009;24(4):686‐98. [DOI] [PubMed] [Google Scholar]
Saboori 2013 {published data only}
- Saboori S, Greene LE, Moe CL, Freeman MC, Caruso BA, Akoko D, et al. Impact of regular soap provision to primary schools on hand washing and E. coli hand contamination among pupils in Nyanza Province, Kenya: a cluster‐randomized trial. American Journal of Tropical Medicine and Hygiene 2013;89(4):698‐708. [DOI] [PMC free article] [PubMed] [Google Scholar]
Savolainen‐Kopra 2012 {published data only}
- Savolainen‐Kopra C, Haapakoski J, Peltola PA, Ziegler T, Korpela T, Anttila P, et al. Hand washing with soap and water together with behavioural recommendations prevents infections in common work environment: an open cluster‐randomized trial. Trials 2012;13:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shafique 2013 {published data only}
- Shafique S, Jalal CSB, Jolly SP, Shikder H, Sellen DW, Zlotkin S. Effects of water‐based hand sanitizers and micronutrient powders along with nutrition and hygiene education to prevent infections and linear growth faltering among low birth weight infants in Bangladesh. FASEB Journal Conference 2013;27(Meeting Abstract Supplement):243.1. [Google Scholar]
Shahid 1996 {published data only}
- Shahid NS, Greenough WB 3rd, Samadi AR, Huq MI, Rahaman N. Handwashing with soap reduces diarrhoea and spread of bacterial pathogens in a Bangladesh village. Journal of Diarrhoeal Diseases Research 1996;14(2):85‐9. [PubMed] [Google Scholar]
Sircar 1987 {published data only}
- Sircar BK, Sengupta PG, Mondal SK, Gupta DN, Saha NC, Ghosh S, et al. Effect of handwashing on the incidence of diarrhoea in a Calcutta slum. Journal of Diarrhoeal Diseases Research 1987;5(2):112‐4. [PubMed] [Google Scholar]
Slayton 2013 {published data only}
- Slayton RB, Murphy JL, Faith SH, Oremo J, Odhiambo A, Ayers T, et al. A cluster randomized controlled evaluation of the health impact of a novel antimicrobial hand towel on the health of children under two years old in rural communities in Nyanza province, Kenya. American Journal of Tropical Medicine and Hygiene (Conference Publication) 2013;85(Suppl 1):314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vindigni 2011 {published data only}
- Vindigni SM, Riley PL, Jhung M. Systematic review: handwashing behaviour in low‐ to middle‐income countries: outcome measures and behaviour maintenance. Tropical Medicine & International Health 2011;16(4):466‐77. [DOI] [PubMed] [Google Scholar]
White 2003 {published data only}
- White C, Kolble R, Carlson R, Lipson N, Dolan M, Ali Y, et al. The effect of hand hygiene on illness rate among students in university residence halls. American Journal of Infection Control 2003;31(6):364‐70. [DOI] [PubMed] [Google Scholar]
Wilson 1991 {published data only}
- Wilson JM, Chandler GN. Sustained improvements in hygiene behaviour amongst village women in Lombok, Indonesia. Transactions of the Royal Society of Tropical Medicine and Hygiene 1993;87(6):615‐6. [DOI] [PubMed] [Google Scholar]
- Wilson JM, Chandler GN, Muslihatun, Jamiluddin. Hand‐washing reduces diarrhoea episodes: a study in Lombok, Indonesia. Transactions of the Royal Society of Tropical Medicine and Hygiene 1991;85(6):819‐21. [DOI] [PubMed] [Google Scholar]
Zhang 2013 {published data only}
- Zhang C, Mosa AJ, Hayward AS, Matthews SA. Promoting clean hands among children in Uganda: a school‐based intervention using 'tippy‐taps'. Public Health 2013;127(6):586‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zomer 2013 {published data only}
- Zomer TP, Erasmus V, Vlaar N, Beeck EF, Tjon‐A‐Tsien A, Richardus JH, et al. A hand hygiene intervention to decrease infections among children attending day care centers: design of a cluster randomized controlled trial. BMC Infectious Diseases 2013;13:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Cave 1999
- Cave B, Curtis V. Effectiveness of promotional techniques in environmental health. WELL Study. Task No.165. March 1999. www.lboro.ac.uk/well/resources/well‐studies/full‐reports‐pdf/task0165.pdf (accessed 1 September 2007).
Claessen 2008
- Claessen J‐P, Bates S, Sherlock K, Seeparsand F, Wright R. Designing interventions to improve tooth brushing. International Dental Journal 2008;58:307‐20. [Google Scholar]
Curtis 2000
- Curtis V, Cairncross S, Yonli R. Domestic hygiene and diarrhoea ‐ pinpointing the problem. Tropical Medicine & International Health 2000;5(1):22‐32. [DOI] [PubMed] [Google Scholar]
Curtis 2003
- Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infectious Diseases 2003;3(5):275‐81. [DOI] [PubMed] [Google Scholar]
Curtis 2011
- Curtis V, Schmidt W, Luby S, Florez R, Touré O, Biran A. Hygiene: new hopes, new horizons. Lancet Infectious Diseases 2011;11(4):312‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ehiri 2001
- Ehiri JE, Azubuike MC, Ubbaonu CN, Anyanwu EC, Ibe KM, Ogbonna MO. Critical control points of complementary food preparation and handling in eastern Nigeria. Bulletin of World Health Organization 2001;79(5):423‐33. [PMC free article] [PubMed] [Google Scholar]
Eisenberg 2012
- Eisenberg JN, Trostle J, Sorensen RJ, Shields KF. Toward a systems approach to enteric pathogen transmission: from individual independence to community interdependence. Annual Review of Public Health 2012;33:239‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fewtrell 2004
- Fewtrell L, Colford JM. Water, Sanitation and Hygiene: Interventions and Diarrhoea: A Systematic Review and Meta‐analysis [Report No 34960]. Washington DC: The International Bank for Reconstruction and Development/The World Bank, 2004. [Google Scholar]
Fewtrell 2005
- Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM Jr. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta‐analysis. Lancet Infectious Diseases 2005;5(1):42‐52. [DOI] [PubMed] [Google Scholar]
Gould 2010
- Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD005186.pub3] [DOI] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- McMaster University. GRADEpro. McMaster University, 2014.
Guevara 2004
- Guevara JP, Berlin JA, Wolf FM. Meta‐analytic methods for pooling rates when follow‐up duration varies: a case study. BMC Medical Research Methodology 2004;4:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gurjeet 2013
- Gurjeet S, Urhekar AD. Effects of hand wash agents: prevent the laboratory associated infections. International Journal of Medical Research & Health Sciences 2013;2(3):564‐8. [Google Scholar]
Higgins 2008
- Higgins JPT, Deeks JJ. Selecting studies and collecting data. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hugonnet 2000
- Hugonnet S, Pittet D. Hand hygiene ‐ beliefs or science. Clinical Microbiology and Infection 2000;6(7):350‐6. [DOI] [PubMed] [Google Scholar]
Huis 2012
- Huis A, Achterberg T, Bruin M, Grol R, Schoonhoven L, Hulscher M. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implementation Science 2012;7:92. [DOI: 10.1186/1748-5908-7-92] [DOI] [PMC free article] [PubMed] [Google Scholar]
Iroegbu 2000
- Iroegbu CU, Ene‐Obong HN, Uwaegute AC, Amazigo UV. Bacteriological quality of weaning food and drinking water given to children of market women in Nigeria: implications for control of diarrhea. Journal of Health, Population, and Nutrition 2000;18(3):157‐62. [PubMed] [Google Scholar]
Lee 2012
- Lee G, Yori P, Olortegui MP, Pan W, Caulfield L, Gilman RH, et al. Comparative effects of vivax malaria, fever and diarrhoea on child growth. International Journal of Epidemiology 2012;41(2):531‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. :.
Luby 2001a
- Luby S. The role of hand washing in improving hygiene and health in low‐income countries. American Journal of Infection Control 2001;29(4):239‐40. [DOI] [PubMed] [Google Scholar]
Luby 2005
- Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, et al. Effect of handwashing on child health: a randomised controlled trial. Lancet 2005;366(9481):225‐33. [DOI] [PubMed] [Google Scholar]
Madhu 2012
- Madhu R, Beinum A. A systematic review of community hand washing interventions leading to changes in hygiene behavior in the developing world. Global Journal on Medicine and Public Health 2012;1(4):49‐55. [Google Scholar]
Mannan 2010
- Mannan SR, Rahman MA. Exploring the link between food‐hygiene practices and diarrhoea among the children of garments worker mothers in Dhaka. Anwer Khan Modern Medical College Journal 2010;1(2):4‐11. [Google Scholar]
Marino 2007
- Marino DD. Water and food safety in the developing world: global implications for health and nutrition of infants and young children. Journal of the American Dietetic Association 2007;107(11):1930‐4. [DOI] [PubMed] [Google Scholar]
Martin 1997
- Martin M. Critical education for participatory research. http://www.socresonline.org.uk/2/2/8.html (accessed 28 September 2007); Vol. 2, issue 2.
Maxwell 2012
- Maxwell O, Oklo A, Bernard A. Profile of water related diseases in Benue State, Nigeria. American Journal of Human Ecology 2012;1(3):87‐94. [Google Scholar]
Murray 2012
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman A, Michaud C, et al. Disability‐adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2197–223. [DOI] [PubMed] [Google Scholar]
Nielsen 2001
- Nielsen M, Hoogvorst A, Konradsen F, Mudasser M, Hoek W. Childhood diarrhea and hygiene: Mothers' perceptions and practices in the Punjab, Pakistan. Working Paper 25. Colombo, Sri Lanka: International Water Management Institute. http://www.iwmi.cgiar.org/Publications/Working_Papers/working/WOR25.pdf (accessed 01 September 2014):1‐21.
Oketcho 2012
- Oketcho R, Nyaruhucha CNM, Taybali S, Karimuribo ED. Influence of enteric bacteria and parasite infection and nutritional status on diarrhoea occurrence in six to 60 month old children admitted at Morogoro Regional Hospital of Tanzania. Tanzania Journal of Health Research 2012;14(2):1‐14. [DOI] [PubMed] [Google Scholar]
Pickering 2011
- Pickering AJ, Julian TR, Mamuya S, Boehm AB, Davis J. Bacterial hand contamination among Tanzanian mothers varies temporally and following household activities. Tropical Medicine & International Health 2011;16(2):233‐9. [DOI] [PubMed] [Google Scholar]
Prüss 2002
- Prüss A, Kay D, Fewtrell L, Bartram J. Estimating the burden of disease from water, sanitation, and hygiene at a global level. Environmental Health Perspectives 2002;110(5):537‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager (RevMan) [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Traore 1994
- Traoré E, Cousens S, Curtis V, Mertens T, Tall F, Traoré A, et al. Childhood defecation behaviour, stool disposal practices, and childhood diarrhoea in Burkina Faso: results from a case‐control study. Journal of Epidemiology and Community Health 1994;48(3):270‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tumwine 2002
- Tumwine JK, Thompson J, Katua‐Katua M, Mujwajuzi M, Johnstone N, Porras I. Diarrhoea and effects of different water sources, sanitation and hygiene behaviour in East Africa. Tropical Medicine & International Health 2002;7(9):750‐6. [DOI] [PubMed] [Google Scholar]
UNICEF/WHO 2009
- United Nations Children's Fund (UNICEF), World Health Organization (WHO). Diarrhoea: why children are still dying and what can be done. Maternal, newborn, child and adolescent health. 2009. http://whqlibdoc.who.int/publications/2009/9789241598415_eng.pdf?ua=1. New York/Geneva, (accessed 18 July 2013):1‐68.
Walker 2013
- Walker C, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet 2013;381(9875):1405‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
WELL 1999
- Water and Environmental Health at London and Loughborough (WELL). DFID guidance manual on water supply and sanitation programmes. 1998. http://www.eenet.org.uk/resources/docs/prelims.pdf (accessed 14 June 2014).
Whitby 2007
- Whitby M, Pessoa‐Silva CL, McLaws ML, Allegranzi B, Sax H, Larson E, et al. Behavioural considerations for hand hygiene practices: the basic building blocks. Journal of Hospital Infection 2007;65(1):1‐8. [DOI] [PubMed] [Google Scholar]
WHO 2003
- World Health Organization. The Treatment of Diarrhoea: a Manual for Physicians and Other Senior Health Workers [WHO/FCH/CAH/03.7]. Geneva: World Health Organization, 2003. [Google Scholar]
Woldemicael 2001
- Woldemicael G. Diarrhoeal morbidity among young children in Eritrea: environmental and socioeconomic determinants. Journal of Health, Population, and Nutrition 2001;19(2):83‐90. [PubMed] [Google Scholar]
Yeager 1999
- Yeager BA, Huttly SR, Bartolini R, Rojas M, Lanata CF. Defecation practices of young children in a Peruvian shanty town. Social Science and Medicine 1999;49(4):531‐41. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Ejemot‐Nwadiaro 2008
- Ejemot‐Nwadiaro RI, Ehiri JE, Meremikwu MM, Critchley JA. Hand washing for preventing diarrhoea. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD004265.pub2] [DOI] [PubMed] [Google Scholar]


