Abstract
Objective
Telehealth has proven effective with a wide range of disorders, but there is a paucity of data on the use of telehealth using cognitive-behavior therapy (CBT) with late-life insomnia and depression. This pilot study was designed to examine the feasibility and effectiveness of using telehealth to treat older adults with comorbid insomnia and depression living in rural Alabama.
Method
Five patients received 10 sessions of CBT for insomnia and depression. Patients were engaged in treatment via Skype from their primary care physician’s office. Assessments were conducted at baseline, posttreatment, and 2-month follow-up.
Results
Patients exhibited clinically significant improvement in both insomnia (sleep diaries and Insomnia Severity Index) and depression (Hamilton Rating Scale for Depression) at posttreatment, and these gains were well maintained at 2-month follow-up.
Conclusions
These preliminary data suggest that telehealth may be an effective means of providing treatment to older adults, including underserved populations.
Keywords: telehealth, cognitive behavior therapy, insomnia, depression
Clinically significant insomnia is found in 10% of the population and prevalence accelerates with advancing age (Ohayon, 2002). The prevalence of depression ranges from 3%-13%, with rates of dysthymia likely being higher still (Bruce et al., 2002). As occurs with insomnia, the prevalence of depression also increases in late-life (Solhaug, Romuld, Romild, & Stordal, 2012). Importantly, insomnia and depression frequently co-occur (Riemann, 2007).
Insomnia and depression share several intersection points: (a) insomnia is a high risk factor for subsequent depression (Perlis et al., 2006); (b) treating either one prompts partial improvement in the other (Lichstein, Wilson, & Johnson, 2000; Manber et al., 2008); (c) disturbed sleep moderates depression treatment (Dew et al., 1997); and (d) residual subjective poor sleep beckons depression relapse (Buysse et al., 1996). These disorders are intimately connected and are risk factors for adverse outcomes including mental/physical health comorbidities, decreased health-related quality of life, and impairment in cognitive functioning (Riemann, 2007; Schubert et al., 2002; Taylor, Lichstein, & Durrence, 2003). As such, there is increased need to find efficacious treatments for coexisting insomnia and depression.
Cognitive-behavior therapy (CBT) is the most thoroughly investigated psychological treatment for both insomnia and depressive symptoms experienced by older adults (Morin et al., 2006; Scogin, Welsh, Hanson, Stump, & Coates, 2005). Combinations of pharmacotherapy and CBT for co-occurring insomnia/depression have proven more effective than unitary treatments for either (Fava et al., 2006; Manber et al., 2008). This is the first study to provide joint CBT for both insomnia and depression.
Telehealth refers to the delivery of health services by use of telecommunication and information technology (Rees & Haythornthwaite, 2004). Telehealth (i.e., telephone therapy) has been found to be effective in treating adults with insomnia (Espie et al., 2007) and depression (Mohr, Hart, & Marmar, 2006) with similar outcomes to face-to-face therapy (Ruskin et al., 2004). Videoconferencing represents one type of telehealth intervention that involves real time interactions supported by cameras and video monitors between provider and patient who are separated by distance and has been used to deliver health services to patients with a wide range of health problems (Hilty, Marks, Urness, Yellowlees, & Nesbitt, 2004). The use of telehealth may be particularly useful in rural settings, where healthcare access is limited (Griffiths, Blignault, & Yellowlees, 2006; Hilty et al., 2004).
There are many studies on CBT for insomnia and CBT for depression. However, nearly all of these are efficacy trials, leaving unanswered questions of how well these treatments work in primary care settings, especially those in rural, medically underserved locales. The current study hopes to address these unanswered questions by using telehealth in rural primary care settings to target co-occurring insomnia and depression in older adults.
Methods
This paper presents findings from the first stage of a two-part study. Stage 1 was a small, uncontrolled series of case studies aimed to refine the treatment manual and explore critical experimental/process variables such as patient referral flow, obstacles to adherence, and treatment acceptability to patients. Stage 2, currently in progress, is a randomized clinical trial.
Patients
Patients were recruited from three different primary care clinics located in rural counties in middle, west Alabama. Patient eligibility criteria are as follows: (a) 50 years of age or older (initial age criterion was 60, but we adjusted it downward to remedy slow recruiting); (b) resident of the Black Belt or adjacent counties (financially disadvantaged, rural Alabama) and receiving services from one of the primary care collaborators; (c) absence of significant cognitive impairment as indicated by a score of 20 or higher on The Saint Louis University Mental Status Examination (SLUMS; Tariq, Tumosa, Chibnall, Perry, & Morley, 2006); (d) absence of other sleep disorders as determined by interview; (e) not currently receiving psychological treatment; (f) absence of suicidality; (g) absence of a psychotic disorder or substance dependence or abuse; (h) concurrence from patient’s primary care physician indicating presence of both insomnia and depression symptoms of sufficient significance to warrant initiation or continuance of primary care treatment (formal diagnosis of either depression or insomnia was not required). Many of the patients we screened were already receiving pharmacotherapy for depression and/or insomnia with partial success.
Settings and Equipment
The study was based in the Department of Psychology, University of Alabama, from which graduate students in clinical psychology delivered therapy, and five rural, primary care physician offices located in or adjacent to Black Belt counties stretching across middle Alabama (although the patients reported herein came from three of these sites). The Black Belt was originally named for its dark, fertile soil, but is now distinguished by extensive poverty and health disparities (Winemiller, 2011). We installed laptop computers in private rooms in these offices to enable therapy transmission.
Patients were administered individual therapy using real-time audio and visual computer-based communication. The study employed Skype, a voice over Internet Protocol (VoIP) application used to make voice calls over the Internet. Skype was configured for secure voice and videoconferencing therapy sessions. Windows registry changes were made so that Skype was configured as “not” to be a supernode, and within the Skype program, the default incoming port settings were deselected. Although a port above 1024 is chosen at random as the port for incoming connections when Skype was installed, a different port for incoming connections was assigned manually. The software application Pretty May Call Recorder for Skype was used to record both patient and therapist audio during the therapy sessions. The audio was saved as an .mp3 file and was reviewed at a later date as part of treatment implementation assessment.
Therapists
Treatment was delivered by advanced graduate students in clinical psychology. Therapists were trained in a workshop format, therapeutic procedures were guided by a treatment manual, and coprincipal investigators experienced in these interventions provided weekly clinical supervision (KL for insomnia and FS for depression).
Materials
Measures were selected to assess the domains of sleep, depression, diagnosis, and psychotherapy process (see Table 1). Because some of our patients had low literacy and sensory impairments, questionnaires were read to all patients to standardize the assessment procedure.
Table 1. Screening, Process, and Outcome Measures by Period of Use.
| Measures | Baseline | During treatment | Post | 2-Month follow-up |
|---|---|---|---|---|
| Sociodemographic Questionnaire | x | |||
| SLUMS | x | |||
| CSD | x | x | x | |
| ISI | x | x | x | |
| HRSD | x | x | x | |
| SCID | x | |||
| WAI-O | x | |||
| Treatment feasibility | x | |||
| Treatment implementation | x |
Note. The following measures are reported: Saint Louis University Mental Status Examination (SLUMS), Consensus Sleep Diary (CSD), Insomnia Severity Index (ISI), Hamilton Rating Scale for Depression (HRSD), the Structured Clinical Interview for DSM-IV (SCID), and the Working Alliance Inventory-Observer Rating Form (WAI-O).
Sociodemographic information
Sociodemographic information was obtained using a researcher-developed questionnaire that included variables such as age, sex, height, weight, race, marital status, educational attainment, perceived income adequacy, and occupational history. This questionnaire also inquired about symptoms of sleep apnea, periodic limb movements, restless legs, and narcolepsy. Information on past and current use of sleep and antidepressant medication, including herbal and folk remedies, was also obtained through review of medical records and interview.
Saint Louis University Mental Status Examination (SLUMS)
The SLUMS (Tariq et al., 2006) is an 11-item measure that assesses four areas of cognitive function: orientation, memory, attention, and executive function. Scores on the SLUMS range from 0–30, with lower scores indicating increasing severity of cognitive impairment. Scores lower than 20, or 19 for individuals with less than high school education, were disqualified due to presumed significant cognitive impairment.
Consensus Sleep Diary (CSD)
The CSD (Carney et al., 2012) was used to gather self-report sleep data. The diary provides a record of the time the patient entered bed and the final morning exit (TIB, time in bed), sleep onset latency (SOL), number of awakenings (NWAK), wake time after sleep onset (WASO), terminal wake time before the final morning arising (TWAK), and sleep quality rating (SQR) on a scale ranging from 1 (very poor) to 5 (very good). The core CSD was slightly modified to include naptime (NAP). A comment section permits collecting additional information such as illness or substances taken at bedtime that are sleep active (e.g., medications and alcohol). Total sleep time (TST: TIB minus SOL, WASO, and TWAK) and sleep efficiency percent (SE = TST ÷ TIB × 100) are derived from the above variables. These variables and their definitions conform to the recommendations of the Pittsburgh Consensus Conference on evaluating insomnia (Buysse, Ancoli-Israel, Edinger, Lichstein, & Morin, 2006).
Insomnia Severity Index (ISI)
The ISI (Morin, 1993) comprises 7 self-report insomnia items that are each rated on a 0 to 4 scale of severity. Sum scores of 7 or less indicate no clinically significant insomnia, 8–14 subclinical, 15–21 moderate, and 22–28 severe insomnia. Strong reliability and validity have been well established (Bastien, Vallieres, & Morin, 2001; Savard, Savard, Simard, & Ivers, 2005).
Hamilton Rating Scale for Depression (HRSD)
The HRSD (Hamilton, 1960) is a 21-item structured interview that measures depression severity. Total scores on the measure range from 0 to 50, with higher scores indicating greater levels of depression. A more structured 17-item version of the HRSD was used in the current data analyses (Whisman et al., 1989). The HRSD possesses adequate overall, if not item-level, convergent, discriminant, and predictive validity (Bagby, Ryder, Schuller, & Marshall, 2004).
Working Alliance Inventory-Observer Rating Form (WAI-O)
Therapeutic alliance addresses degree of collaboration between patient and therapist, and is conceptualized as a prerequisite to change. We assessed therapeutic alliance with the WAI-O (Tichenor & Hill, 1989). The WAI-O is a 36-item measure that is scored on a 7-point Likert scale ranging from 1 (never) to 7 (always). Therefore, scores range from 36 to 252, with higher scores indicating a stronger alliance. The WAI-O can also be broken down into three 12-item subscales that assess bond, task, and goals. Scores on these subscales range from 12 to 84. An audio-recorded session from early in treatment (Sessions 2–5) and from late in treatment (Sessions 6–9) were randomly chosen and rated by a trained independent rater. The WAI-O has been found to have good internal consistency, with an alpha of .98 (Tichenor & Hill, 1989).
Treatment feasibility
We created a questionnaire to assess the feasibility of the intervention. This questionnaire included rating scales to evaluate the clarity of the session, ranging from 1 (very unclear) to 5 (very clear), and the patient’s comfort with the computer and telehealth, in general, ranging from 1 (not at all) to 5 (very much). For example, one question asked, “Did you feel at ease using the computer?” Additionally, open-ended questions were included to evaluate process variables and refine the treatment protocol. For example, patients were asked, “What did you like about the computer?”
Treatment implementation
We monitored delivery, receipt, and enactment treatment components to ensure treatment was conducted as intended (Lichstein, Riedel, & Grieve, 1994). Delivery refers to the proper presentation of the treatment protocol; receipt refers to mastery of the treatment rationale and procedures by the patient; and enactment refers to the patient’s adherence with home assignments. Treatment sessions were audiotaped to allow delivery assessment, receipt was assessed by a brief true/false quiz, and enactment was assessed by evaluating homework adherence.
Treatment
There were 10, 50-minute, weekly manualized treatment sessions. The first five sessions were equally divided between insomnia and depression treatment. The last five sessions were more heavily focused on depression. Insomnia treatment components introduced sequentially were sleep hygiene, sleep compression, stimulus control, and passive relaxation. Depression treatment components were the cognitive-behavior mediational model, behavioral activation, and identification and disputation of unhelpful thoughts. The distribution of therapy components was tailored to patient needs. In addition to CBT, patients continued in usual care with their primary care physician (e.g., hypnotics/antidepressants).
Procedures
Patients were recruited by three means: (a) physician and nurse referral at the collaborating primary care sites, (b) recruitment by research assistants at the primary care sites, and (c) recruitment cards placed at the primary care sites. The prospective patient had the option to contact the project personnel themselves, leave their name and phone number to have project staff contact them, or have their primary care provider initiate the referral.
Patients were first given a thorough description of the study via telephone and basic eligibility was confirmed. Those who were both eligible and interested were scheduled for a baseline assessment that took place in-person at the participating physician’s office. This was our only in-person contact with the patient. In addition to a consent form, the following questionnaires were administered during this interview: sociodemographic questionnaire, SLUMS, ISI, HRSD, and SCID. The patient was sent home to complete 2 weeks of the CSD. A subset of these questionnaires were administered by telephone along with 2 weeks of home sleep diaries at posttreatment and 2 month-follow-up (see Table 1).
Shortly after the baseline assessment interview, a telephone interview was conducted to determine if the patient satisfied the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV; American Psychiatric Association, 2000) depression and insomnia criteria. Additionally, questions were also included from the International Classification of Sleep Disorders, II (American Academy of Sleep Medicine, 2005) for insomnia diagnostic criteria. Formal diagnosis was not a requirement of participation.
Weekly Skype therapy sessions were scheduled after completion of the baseline assessment. For these appointments, the therapist was situated in an office in the Department of Psychology, University of Alabama, and the patient was in an exam room or a staff office at their customary primary care physician’s office in rural Alabama. Nursing and secretarial staff provided minimal assistance when needed to set up the Skype session.
Results
Description of Sample
A total of 18 patients from three different primary care sites were initially enrolled and 13 patients did not complete the study. Reasons for noncompletion were as follows: four were lost to contact, four cited lack of interest or too busy, one was uncomfortable with Skype, one had mounting medical problems, one had transportation difficulty, one did not state a reason, and one was disqualified due to obstructive sleep apnea.
Demographic data for the five patients who completed the study are presented in Table 2. All patients had a high school diploma, one had 2 years of college, and two had a bachelor’s degree. All patients complained of insomnia and depression. Four patients met DSM-IV criteria for major depression and insomnia. One patient did not satisfy diagnostic criteria for either. None of our patients was currently employed: three were retired and two were receiving disability benefits. Three individuals owned computers and were experienced in their use. Two did not own computers and had minimal computer experience.
Table 2. Demographic Characteristics of Completers (n = 5).
| Age (years) | 65.8 (SD = 10.4), range 57–82 |
| Sex | |
| Male (%) | 20 |
| Female (%) | 80 |
| Race | |
| Caucasian (%) | 100 |
| Mean (SD) education (years) | 14.0 (2.0) |
| Mean (SD) BMI | 29.5 (2.9) |
| Mean (SD) SLUMS | 24.4 (1.5) |
Note. SD = standard deviation; BMI = body mass index; SLUMS = Saint Louis University Mental Status Examination.
The medical status of one of the patients changed between posttreatment and follow-up, adversely affecting our outcome measures. She was advised that her long time battle with cancer had taken a bad turn, and she was terminal.
At baseline, four patients were taking sedative/hypnotics and three of these individuals were also taking antidepressants. For all four of these patients, there were no psychotropic medication changes during this study. The fifth patient was started on an antidepressant between posttreatment and follow-up.
Sleep
Patients exhibited clinically meaningful improvement on all sleep diary measures at posttreatment: SOL, NWAK, WASO, and SQR (see Table 3). These gains were maintained or enhanced at follow-up.
Table 3. Sleep and Mood Scores at Baseline, Posttreatment, and Follow-up.
| Baseline |
Posttreatment |
Follow-up |
Post-ES | ||||
|---|---|---|---|---|---|---|---|
| Sleep and mood | M | SD | M | SD | M | SD | d a |
| SOL | 39.9 | 28.56 | 20.3 | 14.26 | 21.5 | 11.35 | −1.10 |
| NWAK | 2.1 | 2.26 | 0.8 | 0.89 | 0.4 | 0.50 | −0.94 |
| WASO | 30.6 | 13.30 | 7.1 | 5.35 | 6.8 | 5.81 | −2.03 |
| SQR | 2.4 | 0.31 | 2.8 | 0.53 | 2.9 | 0.27 | +0.63 |
| ISI | 15.0 | 4.06 | 5.4 | 2.97 | 3.75 | 1.26 | −1.64 |
| HRSD with sleep | 17.0 | 9.97 | 7.2 | 4.32 | 10.0 | 9.77 | −1.14 |
| HRSD without sleep | 14.0 | 8.86 | 6.8 | 3.83 | 9.4 | 8.99 | −1.02 |
Note. M = mean; SD = standard deviation; SOL = sleep onset latency; NWAK = number of awakenings; WASO = wake after sleep onset; SQR = sleep quality rating; ISI = Insomnia Severity Index; HRSD = Hamilton Rating Scale for Depression; ES = effect size.
ES were calculated so that a negative ES indicates reduction from baseline.
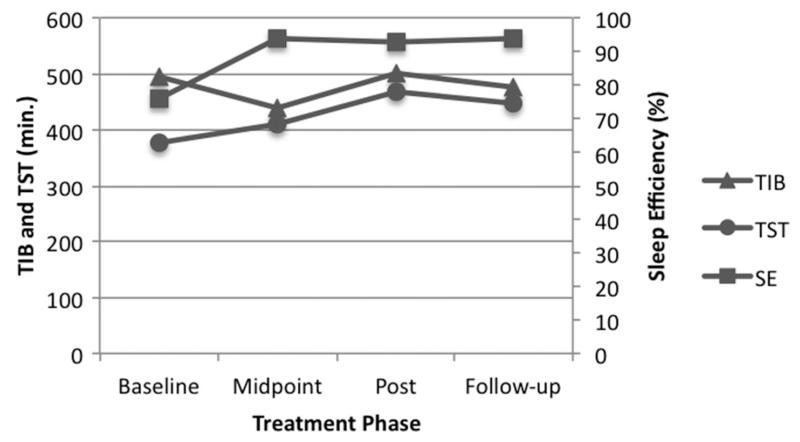
Sleep compression gradually decreases TIB to closely match TST to improve SE and decrease time spent awake in bed. Figure 1 displays the reduction in TIB from baseline to the mid-point in treatment with concurrent improvement in TST, resulting in SE ascending to the normal range. At this point, as prescribed, TIB was expanded and TST continued to accrue, resulting in sustained SE growth through follow-up. Concordant with sleep pattern improvement, insomnia severity, as monitored by the ISI, dropped from the clinical range at baseline to the normal range at posttreatment and follow-up (Table 3).
Figure 1.
Time in bed (TIB) and total sleep time (TST) are referenced to the left ordinate, and sleep efficiency percent (SE) is referenced to the right ordinate.
Note. Sleep compression resulted in decreased TIB and increased SE at treatment mid-point. TIB was gradually increased once improvement in sleep was achieved at treatment mid-point. Improvement in TST and SE maintained at posttreatment and follow-up.
Repeated measures effect size changes for the sleep measures from baseline to posttreatment are reported in Table 3. According to convention, all but one exceeded Cohen’s d large effect criterion of 0.8 (Cohen, 1987). SQR change was a medium effect size.
Depression
Patients’ HRSD scores decreased from 17.0 (moderate depression) at baseline to 7.2 (normal range) at posttreatment, followed by a small increase to 10.0 (mild depression) at follow-up (Table 3). To focus on nonsleep depressive symptoms, sleep items were removed from the HRSD. Trimmed HRSD scores decreased from 14.0 at baseline to 6.8 at posttreatment and 9.4 at follow-up. Large repeated measures effect size changes occurred for the two depression measures from baseline to posttreatment (Table 3).
Therapeutic Alliance
Overall and subscale WAI-O scores were comparable to those typically obtained in other clinical trials (LoTempio et al., 2013). The total score for early session alliance was mean (M) = 182.0 (standard deviation [SD] = 10.7) and late session alliance was M = 175.8 (SD = 28.4). For the early session, the mean task, bond, and goal subscale scores were 60.3 (SD = 3.7), 63.6 (SD = 3.3), and 58.1 (SD = 4.5), respectively, and for the late session, scores were 57.4 (SD = 10.9), 61.6 (SD = 8.8), and 56.8 (SD = 9.0), respectively.
Treatment Feasibility and Implementation
Feasibility ratings were introduced after the study began. Two of the five patients provided treatment feasibility data. These patients consistently reported that the treatment procedures were “clear” or “very clear.” One patient reported that cognitive therapy was “most helpful” and indicated that there were no aspects of treatment that were “least helpful.” The other patient reported that behavioral activation, sleep compression, and relaxation techniques were “most helpful.” This patient also reported that learning to monitor mood and stimulus control techniques were “least helpful.”
Patients liked the computer “much” to “very much,” felt “somewhat” to “very comfortable” with the therapist via computer, and felt “very at ease” with the computer. In general, patients consistently reported comfort with using a computer, including the two patients who were not computer savvy. Importantly, the patient who initially reported being “somewhat comfortable” with the therapist via computer later reported being “very comfortable.” These patients preferred using Skype over telephone, largely due to being able to see the therapist, but would still prefer in-person treatment. Complaints regarding conducting therapy over the computer focused on technical issues (e.g., computer and/or Skype malfunction) and interpersonal discomfort (e.g., difficulty reading body language). Patients reported that the audio and video were occasionally offset, which they found to be distracting.
Treatment delivery was problematic to assess because therapists were granted authority to tailor treatment to maximize therapeutic effect, while still being scored on adherence to a manual. Treatment delivery scores were generally good. Treatment delivery scores for therapist #1 ranged from 77.5% to 100% with an average score of 96%, and for therapist #2 ranged from 77.5% to 90% with an average score of 82.5%.
All five patients provided treatment receipt data and obtained perfect scores on each treatment receipt quiz. This confirms that patients understood the protocol information.
In general, patients were engaged in therapy and were adherent to treatment enactment, including homework assignments. All five patients attended 10 treatment sessions. Three patients completed 100% of the homework assignments, one patient completed 66.7% of the homework assignments, and one patient did not complete any homework assignments. Patients were less adherent to treatment that they perceived to be either challenging or unhelpful. For example, one patient reported that sleep compression was both difficult and not helpful, and they were not fully adherent to this treatment modality. Another patient found relaxation techniques uncomfortable and was not adherent to this treatment modality.
Discussion
Preliminary data indicate telehealth to treat insomnia and depression in older adults is both feasible and effective. Clinically significant gains in both insomnia and depressive symptoms were observed at posttreatment and maintained at 2-month follow-up.
Subjective measures of sleep quantity and quality showed improvement at posttreatment assessment. Importantly, these gains were maintained at follow-up. Patients also demonstrated clinically significant change in their depressive symptoms. Even after removing sleep-related items from the HRSD, patients’ HRSD scores decreased at posttreatment and were maintained at follow-up. For three of our patients, it does not appear that their health status or medications impinged on this study. One patient experienced adverse health prior to follow-up, exerting a negative effect on our outcome measures, and one patient began antidepressant therapy prior to follow-up. Though we did experience a high attrition rate, it appeared that only one patient quit in reaction to treatment. These data encourage further efforts to disseminate insomnia and depression treatments by telehealth to older adults in rural settings.
An important question addressed by this study concerns the feasibility and tolerability of providing CBT for depressive and insomnia symptoms via telehealth in a rural primary care setting. Patients consistently reported comfort with receiving treatment via telehealth. Additionally, one patient who reported being “somewhat comfortable” with engaging a therapist via telehealth reported being “very comfortable” in later sessions, suggesting that tolerance for using a computer for therapy may accrue over time.
This study also assessed treatment implementation through treatment delivery, receipt, and enactment. Treatment delivery by both therapists was good and reflected both adherence to a manualized format while simultaneously tailoring the treatment to the patient’s presenting complaints. A primary example of such tailoring was adjusting the presentation of the manualized material for a patient who had cognitive deficits. Additionally, modifications were made to allow for one patient to utilize prayer in the place of relaxation techniques. For another patient, the depression portion was expanded and the insomnia part contracted to match the unequal strength of their complaint. Treatment receipt for all patients was strong and suggests that the material was well understood. Last, treatment enactment assessment showed that patients were generally actively engaged in therapy. It should be noted that one patient did not complete homework assignments, largely due to significant memory impairment. Therefore, homework assignments for this patient were completed in session.
This study is limited by its small sample size and absence of a control group accounting for time, placebo effects, and social influence. Only five patients completed all phases of this study and these results may not generalize to the larger population. It is possible that individuals who did not perceive therapeutic benefit or who were not comfortable with these setting conditions did not complete treatment. Another limitation of this sample is that it comprises mostly Caucasian females. The primary care offices from which we were recruiting estimated that their patient population was 50%–60% African American. Indeed, these sites were selected because we were interested in testing our intervention with a substantially minority sample. Our success in recruiting African American participants has been going well in our ongoing studies from these sites, but we cannot explain why our early efforts reported herein did not attract minority participants. Therefore, these results may not replicate in more diverse populations. Last, despite the use of a treatment manual, therapy was tailored to the patient’s presenting complaints. Although this results in some variation in treatment, it is felt that this tailoring best reflects what would be done in healthcare settings and is therefore appropriate for an effectiveness trial.
Research has demonstrated the effectiveness of CBT for depression and insomnia. The present, albeit preliminary, data extend this conclusion to the telehealth environment with older adults experiencing co-occurring insomnia and depression, and these results expand the range of influence of CBT.
It is worth emphasizing that a typical treatment course for insomnia comprises six sessions and for depression, 16–20 sessions. In this first trial joining CBT for insomnia and depression, we may have achieved enhanced treatment outcome in 10 sessions. This possible synergistic effect of joint CBT for the common co-occurrence of these two disorders merits further study.
Importantly, this study also suggests that using telehealth may be well tolerated, even by technologically naive patients. Randomized, controlled clinical trials are needed to assess the feasibility, tolerability, and effectiveness of using telehealth to deliver CBT for this comorbidity pair, particularly in underserved populations.
Acknowledgments
This research was supported by National Institute of Mental Health grant MH086643.
References
- American Academy of Sleep Medicine . Diagnostic and coding manual. second edition Author; Westchester, IL: 2005. International classification of sleep disorders. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text rev. [Google Scholar]
- Bagby MR, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: Has the gold standard become a lead weight? American Journal of Psychiatry. 2004;161:2163–2177. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bruce ML, McAvay GJ, Raue PJ, Brown EL, Meyers BS, Keohane DJ, Weber C. Major depression in elderly home health care patients. The American Journal of Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–1173. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Hoch CC, Houck PR, Kupfer DJ, Mazumdar S, Frank E. Longitudinal effects of nortriptyline on EEG sleep and the likelihood of recurrence in elderly depressed patients. Neuropsychopharmacology. 1996;14:243–252. doi: 10.1016/0893-133X(95)00114-S. [DOI] [PubMed] [Google Scholar]
- Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, Morin CM. The Consensus Sleep Diary: Standardizing prospective sleep self-monitoring. Sleep. 2012;35:287–302. doi: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Erlbaum; Hillsdale, NJ: 1987. [Google Scholar]
- Dew MA, Reynolds CF, Houck PR, Hall M, Buysse DJ, Kupfer DJ. Temporal profiles of the course of depression during treatment: Predictors of pathways toward recovery in the elderly. Archives of General Psychiatry. 1997;54:1016–1024. doi: 10.1001/archpsyc.1997.01830230050007. [DOI] [PubMed] [Google Scholar]
- Espie CA, MacMahon KMA, Kelly HL, Broomfield NM, Douglas NJ, Engleman HM, Wilson P. Randomized clinical effectiveness trial of nurse-administered small-group cognitive behavior therapy for persistent insomnia in general practice. Sleep. 2007;30:574–584. doi: 10.1093/sleep/30.5.574. [DOI] [PubMed] [Google Scholar]
- Fava M, McCall WV, Krystal A, Wessel T, Rubens R, Caron J, Amato D, Roth T. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biological Psychiatry. 2006;59:1052–1060. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Griffiths L, Blignault I, Yellowlees P. Telemedicine as a means of delivering cognitive-behavioural therapy to rural and remote mental health clients. Journal of Telemedicine and Telecare. 2006;12:136–140. doi: 10.1258/135763306776738567. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilty DM, Marks SL, Urness D, Yellowlees PM, Nesbitt TS. Clinical and educational telepsychiatry applications: A review. The Canadian Journal of Psychiatry. 2004;49:12–23. doi: 10.1177/070674370404900103. [DOI] [PubMed] [Google Scholar]
- Lichstein KL, Riedel BW, Grieve R. Fair tests of clinical trials: A treatment implementation model. Advances in Behaviour Research and Therapy. 1994;16:1–29. [Google Scholar]
- Lichstein KL, Wilson NM, Johnson CT. Psychological treatment of secondary insomnia. Psychology and Aging. 2000;15:232–240. doi: 10.1037//0882-7974.15.2.232. [DOI] [PubMed] [Google Scholar]
- LoTempio E, Forsberg S, Bryson SW, Fitzpatrick KK, Le Grange D, Lock J. Patients’ characteristics and the quality of the therapeutic alliance in family-based treatment and individual therapy for adolescents with anorexia nervosa. Journal of Family Therapy. 2013;35:29–52. [Google Scholar]
- Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Marmar C. Telephone administered cognitive-behavioral therapy for the treatment of depression in a rural primary care clinic. Cognitive Therapy and Research. 2006;30:29–37. [Google Scholar]
- Morin CM. Insomnia: Psychological assessment and management. Guilford; New York: 1993. [Google Scholar]
- Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: Update of the recent evidence (1998–2004) Sleep. 2006;29:1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Medicine Reviews. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Smith LJ, Lyness JM, Matteson SR, Pigeon WR, Jungquist CR, Tu X. Insomnia as a risk factor for onset of depression in the elderly. Behavioral Sleep Medicine. 2006;4:104–113. doi: 10.1207/s15402010bsm0402_3. [DOI] [PubMed] [Google Scholar]
- Rees CS, Haythornthwaite S. Telepsychology and videoconferencing: Issues, opportunities and guidelines for psychologists. Australian Psychologist. 2004;39:212–219. [Google Scholar]
- Riemann D. Insomnia and comorbid psychiatric disorders. Sleep Medicine. 2007;8:S15–S20. doi: 10.1016/S1389-9457(08)70004-2. [DOI] [PubMed] [Google Scholar]
- Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Bradham DD, Hebel JR, Hauser P. Treatment outcomes in depression: Comparison of remote treatment through telepsychiatry to in-person treatment. The American Journal of Psychiatry. 2004;161:1471–1476. doi: 10.1176/appi.ajp.161.8.1471. [DOI] [PubMed] [Google Scholar]
- Savard MH, Savard J, Simard S, Ivers H. Empirical validation of the Insomnia Severity Index in cancer patients. Psycho-Oncology. 2005;14:429–441. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- Schubert CR, Cruickshanks KJ, Dalton DS, Klein BEK, Klein R, Nondahl DM. Prevalence of sleep problems and quality of life in an older population. Sleep. 2002;25:889–893. [PubMed] [Google Scholar]
- Scogin F, Welsh D, Hanson A, Stump J, Coates A. Evidence–based psychotherapies for depression in older adults. Clinical Psychology: Science and Practice. 2005;12:222–237. [Google Scholar]
- Solhaug HI, Romuld EB, Romild U, Stordal E. Increased prevalence of depression in cohorts of the elderly: an 11-year follow-up in the general population- the HUNT study. International Psychogeriatrics. 2012;24:151–158. doi: 10.1017/S1041610211001141. [DOI] [PubMed] [Google Scholar]
- Tariq SH, Tumosa N, Chibnall JT, Perry MH, III, Morley JE. Comparison of the Saint Louis University Mental Status Examination and the Mini-Mental State Examination for detecting dementia and mild neurocognitive disorder–A pilot study. American Journal of Geriatric Psychiatry. 2006;14:900–910. doi: 10.1097/01.JGP.0000221510.33817.86. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behavioral Sleep Medicine. 2003;1:227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- Tichenor V, Hill CE. A comparison of six measures of working alliance. Psychotherapy. 1989;26:195–199. [Google Scholar]
- Whisman MA, Strosahl K, Fruzzetti AE, Schmaling KB, Jacobson NS, Miller DM. A structured interview version of the Hamilton Rating Scale for Depression: Reliability and validity. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:238–241. [Google Scholar]
- Winemiller TL. Black Belt region in Alabama. In Encyclopedia of Alabama. 2011 Retrieved from http://www.encyclopediaofalabama.org/face/Article.jsp?id=h-2458.