Abstract
Background
Postpartum women are encouraged to participate in ≥150 minutes/week of moderate-intensity aerobic activity, but few women achieve this recommendation. This study sought to identify factors associated with participation in physical activity following pregnancy.
Methods
We examined correlates of any self-reported moderate to vigorous physical activity (MVPA) (≥10 minutes/week across all modes) and any recreational MVPA (≥10 minutes/week) among women enrolled in the Pregnancy, Infection, and Nutrition Postpartum study at 3-months (n=667) and 12-months (n=530) postpartum. Potential correlates were identified according to the socio-ecological framework.
Results
At 3- and 12-months postpartum, lower odds of participation in any MVPA were associated with lower education, breastfeeding, and minimal emotional support. Low exercise self-efficacy, receipt of advice about physical activity, and warmer seasons were associated with higher odds of any MVPA. For recreational MVPA, lower odds of participation were associated with unmarried status, lower education, employment, low income, preeclampsia, and minimal emotional support. Involvement in child/adult care activities, transportation MVPA, and warmer seasons were associated with higher odds of recreational MVPA.
Conclusion
These findings suggest there are several modifiable intrapersonal and interpersonal factors associated with postpartum MVPA that should be considered when developing interventions to help women maintain or increase MVPA after pregnancy.
INTRODUCTION
Physical activity has many health benefits for women in the postpartum period, including improved mood, weight loss, and cardiorespiratory fitness.1, 2 Postpartum physical activity is also associated with decreased anxiety,3, 4 depression,3, 4 and urinary incontinence.4 The American Congress (formerly “College”) of Obstetricians and Gynecologists recommends that pregnant women engage in at least 30 min of moderate-intensity exercise most days of the week in the absence of medical and obstetric complications.5 Postpartum women are encouraged to resume exercise programs gradually and only when it is physically and medically safe to do so.5 The time frame for restarting exercise routines after pregnancy varies among women, with some able to resume activities more quickly than others.5 According to 2008 guidelines developed by the United States (U.S.) Department of Health and Human Services (HHS), weekly participation in at least 150 minutes/week of moderate-intensity aerobic activity is recommended for pregnant and postpartum women who are not already highly active.1
Despite these reported health benefits and recommendations, few women engage in the recommended levels of physical activity during and after pregnancy. Between 1999 and 2006, approximately 23% of U.S. pregnant women reported meeting the U.S. HHS guidelines.6 During the postpartum period, women may return to the levels of physical activity achieved during early pregnancy,7 but they may be less physically active than they were prior to pregnancy.8 Several studies have examined the correlates of physical activity during the postpartum period to inform postnatal interventions.8–13 However, these studies have been limited as sample sizes were relatively small;8, 9 study populations were restricted to women with recent gestational diabetes mellitus (GDM);11, 12 physical activity measures often lacked information on other non-recreational modes, duration or intensity;8, 10–13 and physical activity was only measured at one time point during the postpartum period.8–13
To inform the development of interventions aimed at maintaining or increasing physical activity following pregnancy, it is important to understand what factors are associated with physical activity during the postpartum period. The objective of this study was to identify correlates of self-reported total and recreational moderate to vigorous physical activity (MVPA) at 3- and 12-months postpartum among a cohort of women enrolled in the Pregnancy, Infection, and Nutrition (PIN) Postpartum Study.
METHODS
Study Population
The PIN Postpartum Study prospectively followed women who were initially enrolled in the third phase of the PIN Study (PIN3). PIN3 participants (N=2006) were enrolled before the 20th week of gestation from prenatal care clinics in the University of North Carolina Hospital system. Recruitment occurred from 2001 to 2005, with the last birth occurring in December 2005. Women were eligible for participation in PIN3 if they were English speaking, at least 16 years of age, planning to continue care and deliver at the study site, carrying singleton gestations, and had access to a telephone. Among the 2006 pregnant women enrolled in the PIN3 study, there were 1169 who met the eligibility criteria for the PIN Postpartum Study (i.e., delivered a singleton live birth between October 2002 and December 2005, did not drop out of the study, completed the first PIN3 interview, continued to live in the study area, and were not pregnant at the time of data collection). Of these women, 231 were further excluded because they had medical constraints, were unreachable, or were greater than 5 months postpartum at the time of recruitment, leaving 938 women to be invited for participation. There were 688 women (73% of the 938 invited for participation) who participated in home visits for data collection at 3-months postpartum and 550 (80%) of these 688 women also participated in a second home visit at 12-months postpartum. The women who did not participate at 12-months postpartum (n=138) included those who were lost to follow-up, moved out of the recruitment area, or became pregnant during the two postpartum visits. In-home interviews occurred from 2003 to 2007, with the last interview occurring in January 2007. Information about the reasons for dropout and assessment of selection bias can be found elsewhere.7, 14, 15 We further excluded 21 women with more than one pregnancy in the PIN3 and PIN Postpartum studies to remove correlated observations. Our final sample included 667 women at 3-months postpartum (i.e., 688-21) and 530 at 12-months postpartum (i.e., 550-20; one of the 21 women with two or more pregnancies only participated at 3-months postpartum and was not part of the sample at 12-months postpartum). This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board, and each participant provided informed consent.
Measures
Self-reported physical activity
Physical activity was measured using an interviewer-administered in-home questionnaire that assessed the frequency, duration, and mode (e.g., occupational, recreational, transportation, child and adult care, and both indoor and outdoor household activity) of MVPA in which the woman participated in the week prior to the interview. The participant’s perception of physical activity intensity was assessed using a modified Borg scale.16 The questionnaire was administered during the in-home interviews at 3- and 12-months postpartum and provided an estimate of the total number of minutes in the past week of MVPA. For this study, we considered two outcomes of physical activity: any MVPA (across all modes of activity) and any recreational MVPA. Women were categorized as participating in any MVPA if they reported at least 10 minutes per week of “somewhat hard” or “hard or very hard” physical activity in the past week. Similarly, women were categorized as participating in any recreational MVPA if they reported at least 10 minutes per week of “somewhat hard” or “hard or very hard” recreational activity (e.g., walking for exercise, swimming) in the past week. A cut point of 10 minutes was chosen because the U.S. HHS guidelines recommends that moderate- and vigorous-intensity aerobic activity be sustained in bouts of at least 10 minutes to improve cardiovascular fitness and selected risk factors for type 2 diabetes and heart disease among adults.1
The validity and reliability of the questionnaire were evaluated in a previous study.17 Test-retest reliability was assessed among 109 pregnant women who completed the questionnaire twice over the telephone within a 48-hour time period. The measures displayed substantial agreement with intraclass correlation coefficients ranging from 0.56 to 0.84.17 The criterion validity of the physical activity questionnaire was assessed among 177 pregnant women who kept a structured diary and wore an accelerometer for one week. These women completed the interviewer-administered questionnaire at the end of the week for comparison. Moderate to substantial agreement was observed when comparing the questionnaire and diary (Spearman correlation coefficients ranged from 0.47–0.69); lower agreement was displayed when comparing the questionnaire and accelerometer (coefficients ranged from 0.16–0.34).17
Correlates
Potential correlates were identified according to the socio-ecological framework18 and represented intrapersonal (i.e., individual characteristics) and interpersonal (i.e., social networks and structures) measures that may influence physical activity participation. Intrapersonal measures included: socio-demographics (age, race and Hispanic ethnicity, marital status, education, current employment, income); behavioral characteristics (body mass index or BMI, sleep quality and duration, smoking status, child and adult care MVPA, indoor and outdoor household MVPA, transportation MVPA, work MVPA); reproductive history (number of children aged <18 years in the household, pregnancy-related complications, Cesarean section); infant care (breastfeeding, co-sleeping); psychosocial factors (depressive symptoms, state anxiety, perceived stress), and individual barriers (exercise self-efficacy). Non-recreational modes of MVPA were only assessed as potential correlates of recreational MVPA. Interpersonal measures included receipt of advice about physical activity from a health professional or family member and emotional support from the child’s father. We also identified season of interview administration as an environmental factor that may be associated with participation in MVPA. Depressive symptoms were measured by the Edinburgh Postnatal Depression Scale (EPDS),19, 20 anxiety was measured by the State-Trait Anxiety Inventory (STAI),21 and perceived stress was measured by the 10-item Cohen Perceived Stress Scale (PSS).22 Cut points for psychosocial measures were selected based on the scale’s recommendation and the perinatal literature.
All items were assessed during in-home interviews at 3- and 12- months postpartum, with the exception of recent pregnancy characteristics (i.e., pregnancy-related complications and cesarean section), which were obtained from medical records. Self-reported race, Hispanic ethnicity, and education were measured once during pregnancy at the time of enrollment into the PIN3 Study.
Statistical Analysis
Descriptive analyses were conducted to examine participant characteristics at 3- and 12-months postpartum. Logistic regression models were used to estimate odds ratios (OR) for the association between selected correlates and both dichotomous outcomes: any MVPA and recreational MVPA. We used generalized estimating equations with the logit link function, binomial variance function, and exchangeable correlation structure to account for repeated measurements for each woman.23, 24 Reported p-values are based on the model-based variance estimates. There was no evidence of endogeneity (i.e., correlation between 3-month physical activity outcomes and 12-month correlates, while controlling for 3-month correlates). Stepwise regression with backwards elimination was performed to select an adjusted model. Main effects were retained in the model if p-values were <0.2. Interactions with time (i.e., 3-months vs. 12-months postpartum) were assessed collectively for all predictors in the final model and remained in the model if the p-value was <0.1. We only considered variables in the final model as being statistically significant if p-values were ≤0.05.
RESULTS
Study population
More than half of women in the study population were aged 30 and older, non-Hispanic white, married, college graduates, employed, and had an income greater than 200% of the poverty level at both time points; at least 25% were obese (Table 1). While recreational MVPA was reported by the largest proportion of participants, other modes of MVPA were less frequent, with 25% or less of the participants reporting participation in child and adult care, indoor and outdoor household, transportation, and work MVPA at each time point.
Table 1.
Characteristics of postpartum women in the Pregnancy, Infection, and Nutrition Postpartum Study
| 3-Months Postpartum |
12-Months Postpartum |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Overall | 667 | 530 | ||
| Socio-demographics | ||||
| Age | ||||
| <20 | 18 | 2.7 | 6 | 1.1 |
| 20–29 | 243 | 36.4 | 162 | 30.6 |
| ≥30 | 406 | 60.9 | 362 | 68.3 |
| Race & Hispanic ethnicity | ||||
| Non-Hispanic white | 499 | 75.2 | 408 | 77.4 |
| Non-Hispanic black | 99 | 14.9 | 66 | 12.5 |
| Non-Hispanic other | 34 | 5.1 | 29 | 5.5 |
| Hispanic | 32 | 3.2 | 24 | 4.6 |
| Missing | 3 | 3 | ||
| Marital status | ||||
| Married | 542 | 81.3 | 449 | 84.7 |
| Not married | 125 | 18.7 | 81 | 15.3 |
| Education | ||||
| Less than high school | 36 | 5.4 | 18 | 3.4 |
| High school graduate | 81 | 12.1 | 63 | 11.9 |
| Some college | 115 | 17.2 | 87 | 16.4 |
| College graduate | 435 | 65.2 | 362 | 68.3 |
| Employment status | ||||
| Employed | 353 | 52.9 | 334 | 63.0 |
| Not employed | 314 | 47.1 | 196 | 37.0 |
| Income (% of poverty) | ||||
| <200% | 196 | 29.7 | 119 | 22.7 |
| 200 -< 500% | 344 | 52.0 | 294 | 56.0 |
| ≥500% | 121 | 18.3 | 112 | 21.3 |
| Missing | 6 | 5 | ||
| Behavioral characteristics | ||||
| Body mass index | ||||
| Underweight | 28 | 4.2 | 51 | 9.9 |
| Normal | 332 | 49.9 | 262 | 50.9 |
| Overweight | 106 | 15.9 | 75 | 14.6 |
| Obese | 200 | 30.0 | 127 | 24.7 |
| Missing | 1 | 15 | ||
| Smoking status | ||||
| Yes | 69 | 10.3 | 49 | 9.2 |
| No | 598 | 89.7 | 481 | 90.8 |
| Sleep quality | ||||
| Good or excellent | 387 | 58.0 | 329 | 62.1 |
| Fair or poor | 280 | 42.0 | 201 | 37.9 |
| Sleep duration | ||||
| Short (<7 hours) | 229 | 34.3 | 143 | 27.0 |
| Normal (7–8 hours) | 369 | 55.3 | 333 | 62.8 |
| Long (>=9 hours) | 69 | 10.3 | 54 | 10.2 |
| Child & adult care MVPA | ||||
| None | 502 | 75.3 | 391 | 73.8 |
| Any | 165 | 24.7 | 139 | 26.2 |
| Indoor household MVPA | ||||
| None | 539 | 80.8 | 443 | 83.6 |
| Any | 128 | 19.2 | 87 | 16.4 |
| Outdoor household MVPA | ||||
| None | 623 | 93.4 | 487 | 91.9 |
| Any | 44 | 6.6 | 43 | 8.1 |
| Transportation MVPA | ||||
| None | 634 | 95.0 | 507 | 95.7 |
| Any | 33 | 5.0 | 23 | 4.3 |
| Work MVPA | ||||
| None | 599 | 89.8 | 482 | 90.9 |
| Any | 68 | 10.2 | 48 | 9.1 |
| Reproductive history | ||||
| Number of children aged <18 years in the household | ||||
| 1 | 316 | 47.4 | 254 | 47.9 |
| 2 | 239 | 35.8 | 196 | 37.0 |
| 3+ | 112 | 16.8 | 80 | 15.1 |
| Gestational diabetes (PIN3 study pregnancy) | ||||
| Yes | 30 | 4.5 | 27 | 5.1 |
| No | 635 | 95.5 | 502 | 94.9 |
| Missing | 2 | 1 | ||
| Pregnancy-induced hypertension (PIN3 study pregnancy) | ||||
| Yes | 167 | 25.1 | 139 | 26.3 |
| No | 498 | 74.9 | 390 | 73.7 |
| Missing | 2 | 1 | ||
| Preeclampsia (PIN3 study pregnancy) | ||||
| Yes | 28 | 4.2 | 23 | 4.3 |
| No | 637 | 95.8 | 506 | 95.7 |
| Missing | 2 | 1 | ||
| Cesarean section (PIN3 study pregnancy) | ||||
| Yes | 206 | 31.0 | 165 | 31.2 |
| No | 459 | 69.0 | 364 | 68.8 |
| Missing | 2 | 1 | ||
| Infant care | ||||
| Current breastfeeding | ||||
| Yes | 427 | 64.0 | 135 | 25.5 |
| No | 240 | 36.0 | 395 | 74.5 |
| Co-sleeping with infant | ||||
| Yes | 168 | 25.2 | 104 | 19.6 |
| No | 498 | 74.8 | 426 | 80.4 |
| Missing | 1 | 0 | ||
| Psychosocial factors | ||||
| Perceived stress score | ||||
| <11 | 226 | 33.9 | 181 | 34.2 |
| 11–16 | 250 | 37.5 | 193 | 36.4 |
| ≥17 | 191 | 28.6 | 156 | 29.4 |
| State anxiety score | ||||
| <29 | 351 | 52.6 | 262 | 49.4 |
| 29–39 | 250 | 30.4 | 182 | 34.3 |
| ≥39 | 191 | 16.9 | 86 | 16.2 |
| Depressive symptoms score | ||||
| <10 | 553 | 82.9 | 458 | 86.4 |
| ≥10 | 114 | 17.1 | 72 | 13.6 |
| Barriers/external influences | ||||
| Confidence in ability to exercise more | ||||
| Very | 369 | 55.4 | 273 | 51.7 |
| Somewhat | 251 | 37.7 | 204 | 38.6 |
| Not at all | 46 | 6.9 | 51 | 9.7 |
| Missing | 1 | 2 | ||
| Advised about physical activity or exercise | ||||
| Yes | 242 | 36.3 | 137 | 25.9 |
| No | 425 | 63.7 | 393 | 74.1 |
| Amount of emotional support from the child’s father | ||||
| A lot | 454 | 70.3 | 334 | 65.9 |
| Somewhat | 159 | 24.6 | 138 | 27.2 |
| Not much | 21 | 3.3 | 28 | 5.5 |
| None | 12 | 1.9 | 7 | 1.4 |
| Missing | 21 | 23 | ||
| Season | ||||
| Fall (September-November) | 186 | 27.9 | 139 | 26.2 |
| Winter (December-February) | 145 | 21.7 | 118 | 22.3 |
| Spring (March-May) | 145 | 21.7 | 129 | 24.3 |
| Summer (June-August) | 191 | 28.6 | 144 | 27.2 |
| Physical activity outcomes | ||||
| Total MVPA (all modes of activity) | ||||
| None | 218 | 32.7 | 170 | 32.1 |
| Any | 449 | 67.3 | 360 | 67.9 |
| Recreational MVPA | ||||
| None | 353 | 52.9 | 282 | 53.2 |
| Any | 314 | 47.1 | 248 | 46.8 |
Abbreviations: MVPA, moderate to vigorous physical activity; PIN3, third phase of the Pregnancy, Infection and Nutrition Study
The majority of women (at least 75% at each time point) did not have selected pregnancy complications (Table 1). A high proportion of women were breastfeeding at 3-months postpartum, whereas a low proportion of women were breastfeeding at 12-months postpartum. At both time points, a low proportion of women reported low exercise self-efficacy (i.e., low confidence in ability to exercise more) or received advice about physical activity while a high proportion reported having a lot of emotional support from the child’s father. The postpartum interviews were distributed similarly across all four seasons.
At both 3- and 12-months postpartum, 67% of women participated in any MVPA and 47% participated in recreational MVPA for at least 10 minutes per week (Table 1). At 3-months postpartum, the median (interquartile range or IQR) minutes of MVPA were 0 (0–120) for recreational MVPA and 90 (0–270) for total MVPA. At 12-months postpartum, the median (IQR) minutes of MVPA were 0 (0–120) for recreational MVPA and 94 (0–240) for total MVPA.
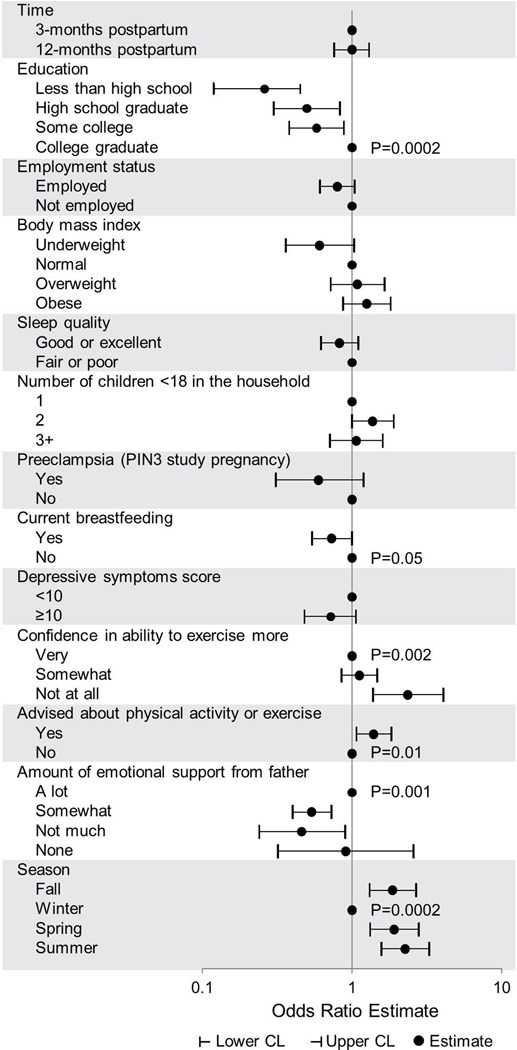
Correlates of any MVPA
In the final model, lower odds of participation in any MVPA at both 3- and 12-months postpartum were associated with lower education levels (less than high school vs. college graduate: OR=0.23, 95% confidence interval, CI, 0.12, 0.45; high school graduate vs. college graduate: OR=0.50, 95% CI 0.30, 0.83; some college vs. college graduate: OR=0.58, 95% CI 0.38, 0.88), current breastfeeding (OR=0.73, 95% CI 0.54, 1.00), and minimal emotional support (some vs. a lot of support: OR=0.54, 95% CI 0.40, 0.73; not much vs. a lot of support: OR=0.46, 95% CI: 0.24, 0.90; none vs. a lot of support: OR=0.91, 95% CI: 0.32, 2.57) (Figure 1). In contrast, higher odds of participation in any MVPA were associated with lower exercise self-efficacy (somewhat vs. very confident; OR=1.12, 95% CI 0.85, 1.47; not at all vs. very confident: OR=2.37, 95% CI 1.38, 4.07), receipt of advice about physical activity (OR=1.40, 95% CI 1.07, 1.83), and warmer seasons (fall vs. winter: OR=1.87, 95% CI 1.31, 2.67; spring vs. winter: OR=1.92, 95% CI 1.32, 2.79; summer vs. winter: OR=2.27, 95% CI 1.57, 3.28). Age, race, marital status, employment, poverty index, BMI, smoking status, sleep quality or duration, number of children aged <18 years in the household, GDM, pregnancy-induced hypertension, cesarean section, co-sleeping with an infant, perceived stress, anxiety, and depressive symptoms were not associated with participation in any MVPA. No significant time interactions were observed for correlates of any MVPA.
Figure 1.
Correlates of any MVPA among postpartum women in the Pregnancy, Infection, and Nutrition Postpartum Study. Correlates were identified from a multivariable analysis and variables were selected into the final model if p-values <0.2, while adjusting for all other variables. P-values were estimated from a group test of all coefficients simultaneously and are presented at the referent level for the variable. Only p-values ≤0.05 are shown.
Abbreviations: MVPA, moderate to vigorous physical activity; PIN3, third phase of the Pregnancy, Infection and Nutrition Study.
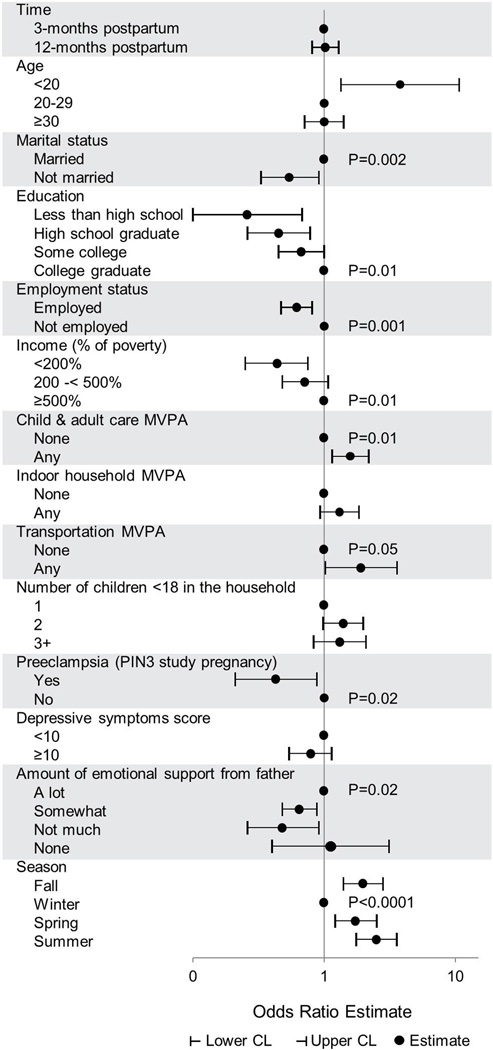
Correlates of any recreational MVPA
In the final model, lower odds of participation in any recreational MVPA at both 3- and 12-months postpartum were associated with unmarried status (OR=0.54, 95% CI 0.33, 0.91), lower education (less than high school vs. college graduate: OR=0.26, 95% CI 0.10, 0.68; high school graduate vs. college graduate: OR=0.45, 95% CI 0.26, 0.78; some college vs. college graduate: OR=0.67, 95% CI 0.45, 1.00), employment (OR=0.62, 95% CI 0.47, 0.81), lower poverty index (<200% vs. ≥500%: OR=0.44, 95% CI 0.25, 0.75; 200-<500% vs. ≥500%: OR=0.71, 95% CI 0.48, 1.07), recent preeclampsia (OR=0.43, 95% CI 0.21, 0.88), and minimal emotional support (some vs. a lot of support: OR=0.65, 95% CI 0.48, 0.88; not much vs. a lot of support: OR=0.48, 95% CI 0.26, 0.91; none vs. a lot of support: OR=1.12, 95% CI 0.40, 3.12) (Figure 2). Higher odds of participation in any recreational MVPA at both 3- and 12-months postpartum were associated with involvement in child/adult care activities (OR=1.58, 95% CI 1.15, 2.18), transportation MVPA (OR=1.91, 95% CI 1.02, 3.59), and warmer seasons (fall vs. winter: OR=1.98, 95% CI 1.40, 2.81; spring vs. winter: OR=1.72, 95% CI 1.21, 2.52; summer vs. winter: OR=2.51, 95% CI 1.75, 3.58). Age, race, BMI, smoking status, sleep quality or duration, indoor and outdoor household MVPA, work MVPA, number of children aged <18 years in the household, GDM, pregnancy-induced hypertension, cesarean section, breastfeeding, co-sleeping with an infant, perceived stress, anxiety, depressive symptoms, exercise self-efficacy, and receipt of advice about physical activity were not associated with participation in recreational MVPA. No significant time interactions were observed for correlates of recreational MVPA.
Figure 2.
Correlates of any recreational MVPA among postpartum women in the Pregnancy, Infection, and Nutrition Postpartum Study. Correlates were identified from a multivariable analysis and variables were selected into the final model if p-values <0.2, while adjusting for all other variables. P-values were estimated from a group test of all coefficients simultaneously and are presented at the referent level for the variable. Only p-values ≤0.05 are shown.
Abbreviations: MVPA, moderate to vigorous physical activity; PIN3, third phase of the Pregnancy, Infection and Nutrition Study.
DISCUSSION
The socio-ecological model provides a framework for understanding the multiple levels of influence (e.g., an individual’s characteristics, personal relationships, community, and societal factors) that can promote or hinder a woman’s participation in physical activity. This comprehensive approach can help to inform the development of interventions that are more likely to be successful at promoting engagement in physical activity following pregnancy. In this prospective study of postpartum women, we identified several intrapersonal and interpersonal level factors that were associated with participation in any and recreational MVPA during the postpartum period. Many of these factors are amenable to intervention. This information is useful for targeting future interventions towards postpartum women with these characteristics.
Similar to findings from a previous study of postpartum women with GDM11 and in contrast to prior studies that found an inverse association13 or no association between education and physical activity in the postpartum period,8, 12 women in the present study were more likely to be physically active (any MVPA and recreational MVPA) if they were highly educated. Higher educational attainment, in general, is known to be associated with healthier behaviors and better health status.25 This may be due to family background, greater resources, and being better informed about health. We also found that postpartum women who were currently breastfeeding were less likely to participate in any MVPA. This may be explained by having less time to exercise or concerns about adverse effects of physical activity on successful breastfeeding.26 To our knowledge, no prior studies have assessed breastfeeding as a correlate of postpartum physical activity. In contrast to previous studies,11, 12 women in the present study were more likely to participate in any or recreational MVPA if they had low exercise self-efficacy. This finding may suggest reverse causality such that very active women do not think they can participate in any more physical activity beyond what they are already doing.
There were several intrapersonal factors associated with participation in recreational MVPA that were not associated with any MVPA. In contrast to one previous study,12 women in the present study were less likely to participate in recreational MVPA if they were unmarried. Two theories have been proposed for explaining the associations between marriage, healthier lifestyles, and better health outcomes in the general population, including marriage protection (i.e., married individuals have more resources and support) and marriage selection (i.e., healthier individuals get married and stay married).27 These theories are helpful for explaining the associations observed in our study, such that married postpartum women may be healthier and have more partner support and economic resources to participate in recreational MVPA than unmarried women. Similar to previous studies10, 13 and in contrast to one study,12 women in the present study were less likely to participate in postpartum recreational MVPA if they were employed. This is likely due to the lack of non-working time available for women to participate in leisure activities while they balance work and family in the postpartum period.
We also found that postpartum women who had a low poverty index were less likely to participate in recreational MVPA. Low-income women may lack the resources and support needed to lead a physically active lifestyle. In addition, the neighborhoods in which low-income families live often lack recreational facilities and parks,28, 29 thus creating environmental barriers to physical activity in these households. Women with preeclampsia during the PIN3 Study pregnancy were also less likely to participate in recreational MVPA during the postpartum period. Physical activity is a known protective factor for preeclampsia.30, 31 Thus, our finding may suggest reverse causality such that women who were less active during pregnancy may be more likely to develop preeclampsia and less likely to participate in recreational MVPA during the postpartum period. In the present study, postpartum women who participated in child/adult care (e.g., playing with children) or transportation (e.g., walking to work) MVPA were more likely to participate in recreational MVPA. Women who maintain a physically active lifestyle in several areas of their life (i.e., at home and on the road) may be more likely to engage in recreational activities. To our knowledge, no prior studies have assessed non-recreational modes of MVPA as correlates of recreational MVPA in the postpartum period.
Few studies have examined interpersonal correlates of physical activity during the postpartum period9, 11, 12 and even fewer have explored environmental or policy level characteristics.26, 32 Similar to our finding that postpartum women were less likely to participate in any or recreational MVPA if they had little or no emotional support from the child’s father, prior studies reported that women were more likely to be physically active if they had support from family or friends11, 12 and a spouse or partner.9 Although these other studies did not assess advice about physical activity, the present study found that women were more likely to participate in any MVPA if they received physical activity advice from a health professional or family member. These findings underscore the importance of social support, either in the home environment or during physician visits, for encouraging postpartum women to participate in physical activity. This factor may be the most amenable to intervention following pregnancy.
Strengths and limitations
The strengths of this study include the prospective cohort design, access to medical records, and detailed information on a number of potential correlates. Also, correlates were identified according to the socio-ecological framework, thus allowing us to address multiple levels of influence on physical activity participation. Due to the prospective design and the collection of information at two time points, we were able to examine time interactions for all correlates in our models.
This study has limitations. Physical activity measures were self-reported and are subject to misclassification from errors in recall. However, the questionnaire has evidence for both validity and reliability.17 These measures may also reflect different recall periods (one week recall for physical activity) as compared to other variables that were included in the study (e.g., one month recall for sleep measures and perceived stress). While we assessed almost thirty potential correlates, there are likely several other variables that could have been considered but were not measured. The socio-ecological framework guided our selection of potential correlates, but they were primarily intrapersonal and interpersonal level factors. Future studies should explore community and policy levels of this framework. Model selection was based on a p-value cut-off, thus introducing the potential for bias as small associations may be less likely to achieve significance while significant associations may be overestimated.33
The generalizability of this study may be limited, as the women were recruited from one clinic in central North Carolina and likely do not represent the general population. Participation in MVPA, reported individual and interpersonal characteristics, and the observed associations between these measures may differ from those in the general population. In addition, the women were not necessarily representative of the original pregnancy cohort due to attrition and being excluded for having a subsequent pregnancy before 12-months postpartum or other factors, thus selection bias may affect our results.
CONCLUSION
This study addresses the potential for improving participation in MVPA after pregnancy by identifying intrapersonal and interpersonal correlates associated with being physically active during the postpartum period. This information should be considered when developing interventions to help postpartum women maintain or increase physical activity. In particular, interventions should focus on increasing postpartum women’s involvement in other non-recreational modes of MVPA (e.g., child/adult care or transportation MVPA), encouraging more health professionals and/or family members to provide advice to women about participating in physical activity or exercise, and improving postpartum women’s emotional support systems. Additional research is needed to better understand which environmental and policy level factors may also influence physical activity behavior of postpartum women.
ACKNOWLEDGMENTS
The authors thank Fang Wen from the University of North Carolina at Chapel Hill for her help with data management and Tom Swasey from the Carolina Population Center for his help with the figures. The Pregnancy, Infection, and Nutrition Study is a joint effort of many investigators and staff members whose work is gratefully acknowledged.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
FUNDING SOURCE
CJV received financial support from grant T32-HL007055 from the National Heart, Lung, and Blood Institute, National Institutes of Health (NIH). Funding for the study was provided by the NIH/National Cancer Institute (#CA109804). Data collected were supported by the NIH/National Institute of Child Health and Human Development (#HD37584), NIH General Clinical Research Center (#RR00046), and NIH/National Institute of Diabetes and Digestive and Kidney Diseases (#DK061981). Support was also received from the Carolina Population Center (#R24 HD050924). AMJ was supported by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences.
REFERENCES
- 1.U.S. Department of Health & Human Services. [Accessed April 2, 2014];2008 Physical Activity Guidelines for Americans. 2008 http://www.health.gov/PAGUidelines/guidelines/default.aspx.
- 2.Larson-Meyer DE. Effect of postpartum exercise on mothers and their offspring: a review of the literature. Obes Res. 2002;10(8):841–853. doi: 10.1038/oby.2002.114. [DOI] [PubMed] [Google Scholar]
- 3.Lewis B, Kennedy B. Effects of exercise on depression during pregnancy and postpartum: a review. Am J Lifestyle Med. 2011;5:370–378. [Google Scholar]
- 4.Pivarnik JM, Chambliss H, Clapp J, III, et al. Impact of physical activity during pregnancy and postpartum on chronic disease risk. Med Sci Sports Exerc. 2006;38(5):989–1006. doi: 10.1249/01.mss.0000218147.51025.8a. [DOI] [PubMed] [Google Scholar]
- 5.Practice ACO. ACOG Committee opinion. Number 267, January 2002: exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002;99(1):171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 6.Evenson KR, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev Med. 2010;50(3):123–128. doi: 10.1016/j.ypmed.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Borodulin K, Evenson K, Herring A. Physical activity patterns during pregnancy through postpartum. BMC Women's Health. 2009;9:32, 1–7. doi: 10.1186/1472-6874-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albright C, Maddock JE, Nigg CR. Physical activity before pregnancy and following childbirth in a multiethnic sample of healthy women in Hawaii. Women & Health. 2005;42(3):95–110. doi: 10.1300/j013v42n03_06. [DOI] [PubMed] [Google Scholar]
- 9.Blum JW, Beaudoin CM, Caton-Lemos L. Physical activity patterns and maternal well-being in postpartum women. Matern Child Health J. 2004;8(3):163–169. doi: 10.1023/b:maci.0000037649.24025.2c. [DOI] [PubMed] [Google Scholar]
- 10.Pereira M, Rifas-Shiman S, Kleinman K, Rich-Edwards J, Peterson K, Gillman M. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med. 2007;32:312–319. doi: 10.1016/j.amepre.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith BJ, Cheung NW, Bauman AE, Zehle K, McLean M. Postpartum physical activity and related psychosocial factors among women with recent gestational diabetes mellitus. Diabetes Care. 2005;28(11):2650–2654. doi: 10.2337/diacare.28.11.2650. [DOI] [PubMed] [Google Scholar]
- 12.Koh D, Miller YD, Marshall AL, Brown WJ, McIntyre D. Health-enhancing physical activity behaviour and related factors in postpartum women with recent gestational diabetes mellitus. J Sci Med Sport. 2010;13(1):42–45. doi: 10.1016/j.jsams.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Durham HA, Morey MC, Lovelady CA, Namenek Brouwer RJ, Krause KM, Ostbye T. Postpartum physical activity in overweight and obese women. J Phys Act Health. 2011;8(7):988–993. doi: 10.1123/jpah.8.7.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borodulin K, Evenson K, Wen F, Herring A, Benson A. Physical activity patterns during pregnancy. Med Sci Sports Exerc. 2008;40(11):1901–1908. doi: 10.1249/MSS.0b013e31817f1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siega-Riz AM, Herring AH, Carrier K, Evenson KR, Dole N, Deierlein A. Sociodemographic, perinatal, behavioral, and psychosocial predictors of weight retention at 3 and 12 months postpartum. Obesity (Silver Spring, Md) 2010;18(10):1996–2003. doi: 10.1038/oby.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borg G, Linderholm H. Perceived exertion and pulse rate during graded exercise in various age groups. Acta Med Scand. 1974;472:194–206. [Google Scholar]
- 17.Evenson KR, Wen F. Measuring physical activity among pregnant women using a structured one-week recall questionnaire: evidence for validity and reliability. Int J Beh Nutr Phys Act. 2010;7:21. doi: 10.1186/1479-5868-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Quart. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 19.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy R, Suttenfield K. Postpartum depression. Medscape Mental Health. 2001;6(4) [Google Scholar]
- 21.Spielberger C. Manual for the state-trait anxiety iventory. Palo Alto, California: 1983. [Google Scholar]
- 22.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 23.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 24.Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986:13–22. [Google Scholar]
- 25.Telfair J, Shelton TL. Educational attainment as a social determinant of health. N Carolina Med J. 2012;73(5):358–365. [PubMed] [Google Scholar]
- 26.Evenson KR, Aytur SA, Borodulin K. Physical activity beliefs, barriers, and enablers among postpartum women. J Women's Health (2002) 2009;18(12):1925–1934. doi: 10.1089/jwh.2008.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schoenborn C. Marital status and health: United States, 1999–2002 Advance data from vital and health statistics; no. 351. Hyattsville, MD: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- 28.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34(1):16–22. doi: 10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: a national study. Am J Public Health. 2006;96(9):1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sorensen T, Williams M, Lee I-M, Dashow E, Thompson M, Luthy D. Recreational physical activity during pregnancy and risk of preeclampsia. Hypertension. 2003;41(6):1273–1280. doi: 10.1161/01.HYP.0000072270.82815.91. [DOI] [PubMed] [Google Scholar]
- 31.Magnus P, Trogstad L, Owe KM, Olsen SF, Nystad W. Recreational physical activity and the risk of preeclampsia: a prospective cohort of Norwegian women. Am J Epidemiol. 2008;168(8):952–957. doi: 10.1093/aje/kwn189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keller C, Todd M, Ainsworth B, et al. Overweight, obesity, and neighborhood characteristics among postpartum Latinas. J Obes. 2013;2013:916468. doi: 10.1155/2013/916468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller AJ. Selection of subsets of regression variables. J R Stat Soc Ser A Stat Soc. 1984;147:389–425. [Google Scholar]