Abstract
Objectives
The relationship between job strain and weight gain has been unclear, especially for women. Using data from over 52 000 working women, we compare the association between change in job strain and change in BMI across different levels of baseline BMI.
Subjects/Methods
We used data from participants in the Nurses’ Health Study II (n=52 656, mean age = 38.4), an ongoing prospective cohort study. Using linear regression, we modeled the change in BMI over 4 years as a function of the change in job strain, baseline BMI, and the interaction between the two. Change in job strain was characterized in four categories combining baseline and follow-up levels: consistently low strain [low at both points], decreased strain [high strain at baseline only], increased strain [high strain at follow-up only], and consistently high strain [high at both points]. Age, race/ethnicity, pregnancy history, job types, and health behaviors at baseline were controlled for in the model.
Results
In adjusted models, women who reported high job strain at least once during the four-year period had a greater increase in BMI (ΔBMI=0.06–0.12, p<0.05) than those who never reported high job strain. The association between the change in job strain exposure and the change in BMI depended on the baseline BMI level (p=0.015 for the interaction): the greater the baseline BMI, the greater the BMI gain associated with consistently high job strain. The BMI gain associated with increased or decreased job strain was uniform across the range of baseline BMI.
Conclusions
Women with higher BMI may be more vulnerable to BMI gain when exposed to constant work stress. Future research focusing on mediating mechanisms between job strain and BMI change should explore the possibility of differential responses to job strain by initial BMI.
INTRODUCTION
Obesity is a risk factor for five of the top ten causes of death in the United States (cardiovascular disease, cancer, stroke, diabetes, and kidney disease)1 and associated conditions such as hypertension, dyslipidemia, and sleep apnea. Although weight gain is often discussed as a matter of individuals’ behavioral choices (i.e., diet, physical activity), the importance of environmental factors, including working conditions, is increasingly recognized.2–5 Some studies have examined weight gain as a consequence of job strain,6 but results have been inconclusive especially for women.2–5, 7 Two cross-sectional studies reported that high job strain was associated with greater body mass index (BMI) for women 4, 8, but the few large-scale longitudinal studies have not provided consistent evidence for the link between job strain and subsequent weight gain or obesity incidence.2, 3, 9
These inconsistent findings may be partly explained by the possibility that associations of job strain with weight gain are not uniform across the range of baseline BMI: in particular, a tendency of initially overweight people to gain weight under stress, countered by a tendency of people who were initially on the lower spectrum of BMI to lose weight under stress.10, 11 Using the Whitehall II data, Kivimäki et al. 10 demonstrated that during a 5-year follow-up period, among those who reported high job strain at baseline, men with low baseline BMI (<22 kg/m2) were more likely to lose weight while those with high baseline BMI (>27 kg/m2) were more likely to gain weight. This relationship was statistically significant only among men. In a smaller study, Block et al.11 found similar evidence of effect modification by baseline BMI for both job demands and job control for men; but for women, the association was significant only for job demands. In both studies, job strain and its components (i.e., job control, job demands) were measured only once at baseline, and therefore they could not account for potential change in the exposure during the follow-up period. In the Japan Work Stress and Health Cohort Study, Ishizaki et al.9 measured job strain twice and examined the association between the chance in job strain and change in BMI over 6 years among 1371 women and 2200 men. Overall they found no significant associations, and the pattern of BMI gain and job strain exposure was quite similar across different levels of baseline BMI. This study further examines the association between job strain and BMI change by including the possibility of effect modification by baseline BMI as well as changes in job strain exposure over time. More specifically, we expect that the greater the baseline BMI is, the greater the effect of job strain on BMI gain. We used data from over 52 000 working women participating in the Nurses’ Health Study II to evaluate the relation between change in job strain and change in BMI over a 4-year period.
METHODS
Study Participants
This is a prospective analysis of data from the Nurses’ Health Study II (NHSII), an ongoing cohort study started in 1989 with 116 430 female registered nurses, age 25–42 at the time of enrollment. Every two years since 1989, these women have been providing a wide range of information on health, lifestyle, health behavior, and work characteristics through self-administered questionnaires. Job strain was measured twice, in 1993 and 1997; this analysis uses the 1993 data as baseline and 1997 data as follow-up.
At baseline, 87 021 women participated; of those, 71 694 (82.4%) women provided data also at follow-up. Those who did not provide follow-up data were more likely to be obese (19% vs. 15%), African American (3% vs. 1%), a current smoker (14% vs. 10%), and reported high job strain in 1993 (22% vs. 20%). We excluded 2568 who developed cancer before 2001 because cancer may have affected their weight before diagnosis. Those who were not working (n=12 593) or who were pregnant (n=2358) at either baseline or follow-up were excluded. In addition, those with missing data on job strain (n=500) or body weight (n=3273) were excluded; so were women with a BMI value less than 15 or greater than 50 (n=314). After exclusions, 52 656 women (73.4% of those who were present at baseline and follow-up) were included in the current analysis. Those who were included and those who were excluded had nearly identical distributions of all study variables, including the baseline BMI and job strain exposure.
Main Study Variables
Body Mass Index
Body mass index (BMI, weight (kg)/height (m)2) was calculated using the data on height reported at the enrollment in 1989 and the current body weight reported in 1993 and 1997. In the analysis, we subtracted the 1993 BMI from the 1997 BMI and used the change as a continuous outcome. A previous validation study confirmed that the self-reported measures of anthropometry were highly correlated with technician-measured data (r = 0.98) in a validation subsample.12
Job strain
Job strain is defined as high job demands combined with low job control.13 Psychological job demands and job control, the components of job strain, were assessed using Karasek’s Job Content Questionnaire.13 Psychological job demands are measured with five items, and job control with nine items. We calculated the mean score for each scale after applying reverse coding to make higher scores indicate stronger endorsement for experiencing job demands and job control. Cronbach’s alpha in this sample was .73 for job demands, and .80 for job control. Scores were dichotomized at the median in order to define “high job strain” as a combination of high job demands (i.e., above median) and low job control (i.e., below median).14 Women were categorized according to their baseline job strain and changes in job strain during follow-up in accordance with previous studies.3, 9
Behavioral Covariates at Baseline
Information on age, race/ethnicity, smoking and pregnancy history was obtained at baseline in 1989. Pregnancy history and smoking were updated in each follow-up questionnaire. Average sleep duration over a 24-hour period (<5 hours, 5 hours, 6 hours, 7 hours, 8 hours, 9 hours, 10+ hours) was recalled retrospectively in 2009 for each decade of the woman’s life since age 25. Diet was assessed in 1991 and updated every 4 years using a previously validated semi-quantitative food frequency questionnaire (FFQ).15 Responses to this questionnaire were used to calculate the alternative Healthy Eating Index (aHEI),16 a summary score of dietary factors previously related to chronic disease risk and BMI.16,17 Physical activity and sedentary activities were assessed in 1991 and updated in 1997 using a previously validated questionnaire.18 Time spent in moderate to vigorous activities (≥ 4 metabolic equivalents; METs)19 was multiplied by the MET value of each activity and their sum was expressed as MET-hours-per-week.
The type of employment was asked both at baseline and follow-up with the following response options: inpatient/emergency room, outpatient/community nurse, operating room, nursing education, nursing administration, other nursing occupation, or non-nursing employment.
Statistical Analysis
The 56 262 women who met inclusion criteria for this analysis had no missing data on job strain, BMI or age at either baseline or follow-up. All other study variables had less than 4% of missing data, except for the alternative healthy eating index (6.3%) and average hours of sleep (18.7%). All missing values were coded as missing indicators so that all observations were retained in the regression analysis. We first present the sample characteristics adjusted for age and stratified by change in job strain exposure over time. Then we show descriptive statistics of the bivariate relationship between the change in BMI and the baseline BMI category. Informed by Nyberg et al.’s findings from the pooled analysis of 13 cohort studies,6 we examine the association between change in job strain and change in BMI. We model the change in BMI over 4 years as a function of the change in job strain exposure, adjusted for baseline BMI, baseline BMI squared, and demographic covariates (i.e., age, race/ethnicity, pregnancy history before baseline, and the number of pregnancies between baseline and follow-up). The square term of baseline BMI was added to the model because the descriptive statistics showed a strong quadratic curve. To test the hypothesis that the association of job strain change with BMI change would depend on baseline BMI, we included the interaction term between job strain change and baseline BMI (Model 1). For clearer interpretations of the interaction, baseline BMI was grand-mean centered, and the square term was calculated using the centered baseline BMI value. This makes the main effect of job strain to be applicable to the women whose baseline BMI was the average value (=25.2 kg/m2), and the interaction effect to be applicable to all others. In Model 2, we added baseline behavioral covariates (i.e., physical activity, TV watching hours, sleep, and smoking) and the type of the job. Changes in these behavioral covariates were not included in our analysis because they could reflect coping behaviors under job stress.20 All analyses were performed on SAS version 9.3.
RESULTS
Table 1 presents demographic characteristics of the study participants. At the baseline of this analysis, the age of the participants ranged from 29 to 46 years old, with an average age of 38.5 years (SD = 4.6). A vast majority (94%) was Caucasian. The average BMI at baseline was 25.2 kg/m2 (SD = 5.4). While a large majority (71%) reported no job strain at either time, 7% reported high strain at both times. Inpatient, emergency room, and operating room nurses were more likely to report high job strain at both baseline and follow-up. At baseline, mean BMI was slightly lower for the job strain remained low group compared with other groups.
Table 1.
Age-standardized characteristics among 52 656 NHSII participants by job strain change from baseline (1993) to follow-up (1997).
| Job strain exposure at baseline and follow-up
|
Total (n=52656, 100%) | ||||
|---|---|---|---|---|---|
| No-no (n=37247, 70.7%) | Yes-no (n=6726, 12.8%) | No-yes (n=5011, 9.5%) | Yes-yes (n=3672, 7.0%) | ||
| Age in 1993*, mean (SD) | 38.6(4.6) | 38.0(4.6) | 38.2(4.6) | 38.0(4.6) | 38.5(4.6) |
| BMI in 1993, mean (SD) | 25.1(5.4) | 25.4(5.5) | 25.4(5.5) | 25.5(5.7) | 25.2(5.4) |
| Race/Ethnicity | |||||
| African-American, % | 1 | 2 | 1 | 1 | 1 |
| Latina, % | 1 | 1 | 1 | 1 | 1 |
| Asian, % | 1 | 2 | 1 | 2 | 1 |
| Caucasian, % | 95 | 93 | 94 | 94 | 94 |
| Other, % | 2 | 2 | 2 | 2 | 2 |
| Employment type in 1993 | |||||
| Inpatient/ER nurse, % | 31 | 46 | 43 | 55 | 36 |
| Outpatient/community nurse, % | 18 | 14 | 16 | 11 | 17 |
| OR nurse, % | 4 | 9 | 6 | 10 | 6 |
| Nursing education, % | 7 | 3 | 3 | 1 | 6 |
| Nursing student, % | 1 | 1 | 1 | 0 | 1 |
| Nursing administration, % | 12 | 6 | 9 | 4 | 11 |
| Other nursing job, % | 21 | 19 | 19 | 17 | 20 |
| Non-nursing job, % | 5 | 2 | 2 | 2 | 4 |
| Smoking status in 1993 | |||||
| Never smoked, % | 66 | 65 | 65 | 65 | 65 |
| Former smoker, % | 24 | 24 | 23 | 23 | 24 |
| Current smoker, % | 11 | 12 | 12 | 12 | 11 |
| #cigarettes/day, mean (SD) | 15.3(9.8) | 15.9(10.3) | 16.6(10.3) | 16.3(9.5) | 15.5(9.9) |
| METs/week, mean (SD) | 19.5(21.2) | 19.0(21.3) | 18.5(21.4) | 18.4(20.8) | 19.3(21.1) |
| #hours/week watching TV, mean (SD) | 8.6(7.9) | 9.2(8.8) | 9.3(8.6) | 9.6(8.9) | 8.8(8.2) |
| Alternative Healthy Eating Index (range: 2.5 – 87.5), mean (SD) | 37.2(10.7) | 36.8(10.7) | 36.3(10.4) | 36.3(10.4) | 37.0(10.6) |
| Average hours of sleep, mean (SD) | 7.0(0.9) | 6.9(1.0) | 6.9(1.0) | 6.8(1.0) | 7.0(0.9) |
Notes. Values are standardized to the age distribution of the study population.
Value is not age adjusted. Values of polytomous variables may not sum to 100% due to rounding.
The number of cigarettes per day was calculated for current and former smokers. METs = metabolic equivalent of tasks.
Missing data in each variable were less than 4% except for the alternative healthy eating index (6.3%) and average hours of sleep (18.7%). All missing data were coded as missing and kept in the regression analyses
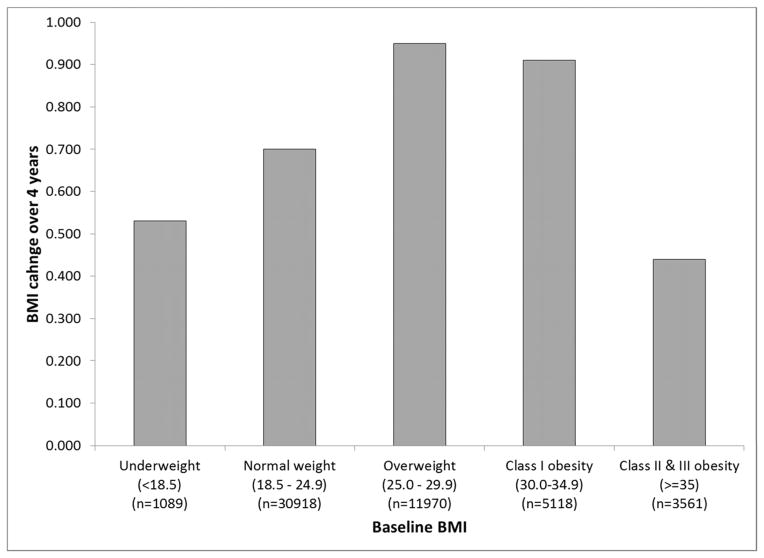
Over the course of four years, 50.8% of the women gained >5 lbs (2.27 kg), 15.4% lost >5 lbs, and 33.8% maintained the weight within ±5 lbs. The average change in BMI was 0.87 kg/m2, which translates as 5.25 lbs (2.38 kg) increase for the woman of the average height in this sample (5 feet 5 inches (1.65 m)). Figure 1 shows the median change in BMI by baseline BMI category (underweight: BMI<18.5; normal: 18.5–24.9; overweight: 25–29.9; class I obesity: 30.0–34.9; class II and III obesity: ≥35.0). Those who were lower and higher ends of the baseline BMI distribution tended to have a smaller average increase than those who were in the middle of the distribution.
Figure 1.
Median change in BMI over four years by baseline BMI category
Table 2 summarizes the regression analysis results by showing the mean difference in BMI change associated with baseline BMI, baseline BMI squared, job strain change categories, and the interaction between baseline BMI and job strain change. Model 1 was adjusted for age, race, and parity. Model 2 had additional adjustments for job types at both baseline and follow-up as well as behavioral covariates at baseline; however, as shown in Table 2, including these additional covariates did not materially change the results. Baseline BMI and baseline BMI squared were both significantly associated with BMI change. The main effect of job strain change was statistically significant: on average, those who experienced job strain change in either direction (decreased or increased) had a greater BMI gain (b=0.063 – 0.077, p=0.01 – 0.03) than those with no job strain exposure at either time point. Women who experienced job strain at both times also gained BMI compared to women who experienced job strain at neither time, and the BMI gain for them was greater than for women who reported high job strain at only one of the two time periods.
Table 2.
Mean BMI change from baseline (1993) to follow-up (1997) associated with baseline BMI, baseline BMI squared, and job strain exposure patterns.
| Independent variable | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| ΔBMI | (95% CI) | p-value | ΔBMI | (95% CI) | p-value | |
| Baseline BMI (mean-centered) | 0.032 | (0.027, 0.038) | <0.0001 | 0.031 | (0.025, 0.036) | <.0001 |
| Baseline BMI (mean-centered) squared | −0.007 | (−0.007, −0.006) | <0.0001 | −0.007 | (−0.007, −0.006) | <.0001 |
| Job strain exposure at baseline and follow-upa | <0.001b | 0.002b | ||||
| Remained low (ref.) | 0.000 | -- | 0.000 | -- | ||
| Decreased | 0.073 | (0.017, 0.129) | 0.011 | 0.063 | (0.006, 0.120) | 0.030 |
| Increased | 0.077 | (0.013, 0.141) | 0.019 | 0.074 | (0.009, 0.138) | 0.025 |
| Remained high | 0.125 | (0.052, 0.199) | <0.001 | 0.118 | (0.044, 0.193) | 0.002 |
| Baseline BMI*job strain exposure | 0.016b | 0.015b | ||||
| Baseline BMI*Remained low (ref.) | 0.000 | -- | 0.000 | -- | ||
| Baseline BMI*Decreased | 0.001 | (−0.009, 0.012) | 0.820 | 0.001 | (−0.009, 0.011) | 0.843 |
| Baseline BMI*Increased | −0.000 | (−0.012, 0.011) | 0.977 | 0.000 | (−0.011, 0.012) | 0.975 |
| Baseline BMI*Remained high | 0.021 | (0.008, 0.034) | 0.001 | 0.022 | (0.008, 0.035) | 0.001 |
Notes. Baseline BMI was mean-centered, and the square term was calculated with the centered value. Model 1is adjusted for baseline age, race/ethnicity, the number of pregnancies up to baseline, and the number of pregnancies between baseline and follow-up. Model 2 includes the following baseline covariates in addition to what is in Model 1: type of job at baseline and follow-up, average sleep duration, smoking status, the number of cigarettes per day, diet, physical activity, and average time spent on watching TV.
Because the interaction term is included in the models, the main effect results should be interpreted only when baseline BMI (mean-centered)=0; that is, the main effects of job strain exposure are for women whose baseline BMI was the average value (=25.2). For all others, the effect of job strain exposure depends on the baseline BMI.
p-value for the likelihood ratio test with df=3
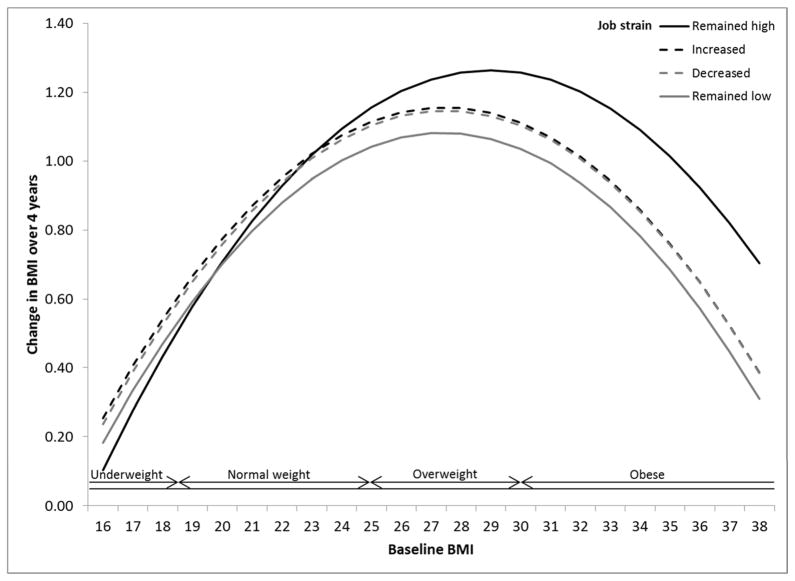
The interaction between baseline BMI and job strain change was statistically significant (p=0.015), which indicates that the relationship between job strain change and BMI change depends on each woman’s baseline BMI. The positive and significant regression coefficient for the interaction between baseline BMI and job strain that remained high (b=0.022, p=0.001) indicates that the greater the baseline BMI, the greater the BMI gain associated with job strain that remained high. The nature of this interaction is illustrated in Figure 2 as marginal means of BMI change by job strain change and baseline BMI. The differences in BMI change among the four job strain change groups are not prominent in the under- and normal weight range. However, among women whose baseline BMI was in the overweight or obese range, the difference between job strain that remained low (gray solid line) and job strain that remained high (black solid line) is greater; that is, those who experienced job strain at both times gained more BMI than those whose job strain remained low, and the greater the baseline BMI, the greater the BMI gain associated with job strain that remained high. Those who experienced high job strain only once, either at baseline (job strain decreased, gray dotted line) or at follow-up (job strain increased, black dotted lines) had a greater BMI gain, as described in the previous paragraph. The magnitude of BMI gain associated with increased or decreased job strain is uniform across the full range of baseline BMI (i.e., interaction was not significant).
Figure 2.
BMI change by job strain change categories based on Model 2 presented in Table 2
As a sensitivity analysis, we conducted the same regression analysis with those who did not change job types (e.g., emergency room nursing, operating room nursing, nursing management) between baseline and follow-up because taking a different type of job could be a stressful event that impacts BMI change regardless of change in job strain that may or may not accompanied the job change. The results were similar to the full sample results, both the main effect and interaction, which suggest that change in job types did not impact the association between job strain and BMI change.
DISCUSSION
This study examined the association between the change in job strain exposure and the change in BMI over 4 years among more than 52 000 working women. Our specific focus was to test whether the effect of job strain on BMI gain would be greater for women whose baseline BMI was at the higher end of the spectrum. The analysis indicated that experience of job strain at baseline, follow-up, or both times were associated with a greater BMI gain. Moreover, the higher the baseline BMI, the greater the BMI gain associated with job strain that remained high. This study clarifies previous inconsistent findings for women2, 3, 9–11 by using a large sample size and multiple measurements of both job strain and BMI as well as by accounting for a quadratic relationship between baseline BMI and BMI change over time.
Our data showed that the BMI gain associated with constantly high job strain is greater for women who had a higher BMI at baseline. Three previous studies took similar approaches to examining the association between BMI change and job strain change, yet reported different findings. Block et al. 11 followed 722 women over 9 years to examine the interaction between baseline BMI and a baseline measure of job demands. Their results were similar to ours: the interaction was significant in that the BMI increase associated with job strain was greater for initially obese women than for normal and overweight women. A limitation of the Block study is that because they measured job demands only once at baseline, the BMI change after 9 years was averaged across groups who may have experienced job demand changes during the 9 year follow-up period. Ishizaki et al.’s study of Japanese workers had two measurements of job strain 6 years apart and categorized the change in job strain the same way we did in this study. Among the 1370 women, however, Ishizaki et al. did not find support for baseline BMI moderating the association between job strain change and BMI change. This could be due to the smaller sample size, the smaller proportion of overweight and obese women (14% in this Japanese sample), and also a further loss of statistical power by categorizing the baseline BMI distribution. Eek and Östergren3 accounted for the baseline BMI in quartiles while they examined the associations between job strain change and BMI change over 5 years with nearly 5500 women in the Scania Public Health Cohort Study. Although they did not include the interaction term, their findings for middle-aged women are similar to the main effect of job strain change in our analysis. While cross-sectional studies4, 7, 8 and some prospective studies with job strain measured only at the baseline10, 11 reported inconsistent findings, the current study together with Eek and Östergren3 provides stronger evidence for the link between job strain and women’s weight gain over time.
Both physiological and behavioral paths from job strain exposure to weight gain have been suggested. Exposure to chronic stress, including job strain, results in neuroendocrine dysregulation,21, 22 such as increased cortisol production and disruption of diurnal cortisol curve, which is associated with greater BMI and waist circumference as well as higher intra-abdominal fat.23, 24 This association is especially prominent among women,22 and there has been a report suggesting that obese women may be more vulnerable to stress-induced disturbance of cortisol production,25 which offers potential explanation for our findings.
In addition to these physiological changes, exposure to job strain may also lead to unhealthy behaviors, but so far research findings are inconsistent.26, 27 Our results suggest that one explanation for previous inconsistent findings may be those with higher BMI being more prone to developing unhealthy behavioral habits under stress. Although its methodological shortcomings have been pointed out,28, 29 a recent pooled longitudinal analysis of 4 European studies30 showed that among those who did not have a healthy lifestyle at the baseline, high job strain exposure was associated with a lower likelihood of adopting healthy behaviors. Important future research questions include whether job strain leads to unhealthy behaviors and whether the link is stronger for overweight and obese individuals.
In our sample, women who reported high job strain only at baseline or follow-up had on average greater BMI increase than those who reported no job strain at either time. Eek and Östergren3 found a similar result. If the women had been exposed to high job strain for a long time before the baseline, the effect may linger even if the exposure diminished during the study period.21, 31 Another possibility to consider is job change. In our data, those who reported high job strain only at baseline were more likely to have changed the types of jobs during the study period than those who reported no strain at both times (46.3% vs. 37.3%). Potentially as a result of the job change, their job strain declined, but other job characteristics may have changed as well. For example, it is common for nurses who are new to the workplace to take less desirable shifts, which might result in weight gain.32 Moreover, changing jobs in and of itself could be stressful, especially if the job change was not voluntary. However, our sensitivity analysis showed that job change was not a likely factor to alter the association between job strain and BMI change in this sample.
This study has a number of strengths such as a large sample size, well-established measure of job strain, and prospective design. Nevertheless, the interpretation of the results should take into account the following data limitations. Obesity is strongly patterned by socioeconomic status (SES), often measured by income, education, and occupation. For this analysis, household income was not available, although the participants were all registered nurses with roughly similar educational backgrounds. Examining weight change in a socioeconomically somewhat homogeneous sample (i.e., a single-occupation sample) limits generalizability of our findings; however, single-occupation samples have its advantages as well because the homogeneous sample helps to separate the effect of job strain from that of SES.33 We did control for the type of the nursing job, which could be a rough proxy to SES (e.g., nurse administration, nursing education, ER nurse). In our sample, both the job control and demands scales had a full-range, normal distribution. Moreover, the mean job demands and control scores differ significantly across different types of nursing jobs: the mean job control score was the highest for nursing educators and administrators and the lowest for ER and OR nurses, whereas the mean job demands score was the highest for ER and OR nurses as well as nurse administrators. This mitigates the concern that a single occupation sample may limit the variability of the job demands and job control scores. Although the job type had a significant association with BMI change (data not shown), including the variable did not change the regression coefficients for the job strain main effect or interaction. The same was true for the sleep variable. Because sleep was recalled retrospectively in 2009, the validity of the data is questionable; however, the presence or absence of this variable did not change the main results. All study variables, including height and weight, were collected via self-report, which is subject to various biases. In a validation subsample, the self-reported measures of anthropometry were highly correlated with technician-measured data (r = 0.98).12 In addition, because this analysis used the change in BMI as the dependent variable, the potential downward bias is unlikely to have affected our results.34 Finally, we followed the standard formulation of job strain,14 which involves dichotomizing the job control and demands scores at the sample median score. This could lead to misclassification of exposure to those who scored on the median score and biases the results toward the null. We acknowledge this limitation, but in order to make comparisons with other studies easier, we followed this widely accepted procedure. Finally, this study addressed only one type of job stress. Future research should also examine other types of job stress such as effort-reward imbalance.35
Conclusion
This analysis of over 52 000 working women’s weight change over 4 years showed that the association between job strain and weight gain is stronger for those with higher baseline BMI. This finding is directly applicable to over 3 million registered nurses in the United States. We contribute to job stress research by providing methodologically sound analysis of women’s data in a sample large enough to detect interactions between variables. Our findings identify that women with higher BMI are more vulnerable to weight gain if they were exposed to high job strain. Future research focusing on mediating mechanisms between job strain and weight gain should explore the possibility of differential responses to job strain by initial weight. Finally, our findings underscore the importance of an integrated approach toward obesity prevention in the workplace between health promotion (traditionally focuses on individual health behaviors) and occupational safety (addresses changes in work characteristics, including job stressors, to reduce adverse health impacts) as the National Institute for Occupational Safety and Health (NIOSH) advocates in its Total Worker Health Program (http://www.cdc.gov/niosh/twh/). Occupational safety and health practitioners and health promoters should be aware of the different vulnerability to work stress by BMI levels, and intervention resources should be allocated more toward those who are already overweight and exposed to work stress.
Acknowledgments
The collection of the Nurses’ Health Study II data was supported by the National Institutes of Health (UM1 CA176726). The analysis for this paper was supported by NIH grant P30 DK046200 and the National Institute for Occupational Safety and Health intramural grant (NORA-FY13-927ZKWG).
Footnotes
Conflict of interests: None.
Disclaimers: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Poirier P, Giles TD, Bray GA, Hong YL, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss - An update of the 1997 American Heart Association Scientific Statement on obesity and heart disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113(6):898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 2.Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. American Journal of Epidemiology. 2007;165:828–837. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- 3.Eek F, Östergren P-O. Factors associated with BMI change over five years in a Swedish adult population: Results from the Scania Public Health Study. Scandinavian Journal of Public health. 2009;37:532–544. doi: 10.1177/1403494809104359. [DOI] [PubMed] [Google Scholar]
- 4.Kouvonen A, Kivimäki M, Cox SJ, Cox T, Vahtera J. Relationship between work stress and body mass index among 45810 female and male employees. Psychosomatic Medicine. 2005;67:577–583. doi: 10.1097/01.psy.0000170330.08704.62. [DOI] [PubMed] [Google Scholar]
- 5.Overgaard D, Gamborg M, Gyntelberg F, Heitmann BL. Psychological workload is associated with weight gain between 1993 and 1999: Analyses based on the Danish Nurse Cohort Study. International Journal of Obesity. 2004;28:1072–1081. doi: 10.1038/sj.ijo.0802720. [DOI] [PubMed] [Google Scholar]
- 6.Nyberg ST, Heikkilä K, Fransson EI, Alfredsson L, DeBacquer D, Bjorner JB, et al. Job strain in relation to body mass index: Pooled analysis of 160,000 adults from 13 cohort studies. J Intern Med. 2011;272:65–73. doi: 10.1111/j.1365-2796.2011.02482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wardle J, Chida Y, Gibson EL, Whitaker KL, Steptoe A. Stress and adiposity: A meta-analysis of longitudinal studies. Obesity. 2011;19:771–778. doi: 10.1038/oby.2010.241. [DOI] [PubMed] [Google Scholar]
- 8.Hellerstedt WL, Jeffery RW. The association of job strain and health behaviors in men and women. International Journal of Epidemiology. 1997;26:575–583. doi: 10.1093/ije/26.3.575. [DOI] [PubMed] [Google Scholar]
- 9.Ishizaki M, Nakagawa H, Morikawa Y, Honda R, Yamada Y, Kawakami N, et al. Influence of job strain on changes in body mass index and waist circumference: 6-year longitudinal study. Scand J Work Environ Health. 2008;43:288–296. [PubMed] [Google Scholar]
- 10.Kivimäki M, Head J, Ferrie JE, Shipley MJ, Brunner E, Vahtera J, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. International Journal of Obesity. 2006;30:982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 11.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. American Journal of Epidemiology. 2009;170:181–192. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LG, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Karasek RA, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. Journal of Occupational Health Psychology. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 14.Landsbergis PA, Schnall PL, Schwartz JE, Pickering TG, Warren K. The association of ambulatory blood pressure with alternative forms of job strain. Scandinavian Journal of Work, Environment, and Health. 1994;20:349–63. doi: 10.5271/sjweh.1386. [DOI] [PubMed] [Google Scholar]
- 15.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. American Journal of Epidemiology. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 16.McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. American Journal of Clinical Nutrition. 2002;76(6):1261–1271. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 17.Mujahid MS, Diez Roux A, Shen M, Gowda D, Sanchez B, Shea S, et al. Relation between neighborhood environment and obesity in the Multi-Ethnic Study of Atherosclerosis. American Journal of Epidemiology. 2008;167:1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 18.Wolf A, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano K. Reproducibility and validity of a self-administered physical activity questionnaire. International Journal of Epidemiology. 1994;23:991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 19.Ainsworth BE, Haskell WL, Leon AS, Jacobs DRJ, Montoye HJ, Sallis JF. Compendium of physical activities: classification of energy costs of human physical activities. Medicine and Science in Sports and Exercise. 1993:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Pinto BM, Borrelli B, King TK, Bock BC, Clark MM, Roberts M, et al. Weight control smoking among sedantary women. Addictive Behaviors. 1999;24:75–86. doi: 10.1016/s0306-4603(98)00034-3. [DOI] [PubMed] [Google Scholar]
- 21.McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 22.Pasquali R, Vicennati V, Gambineri A, Pagotto U. Sex-dependent role of glucocorticoids and androgens in the pathophysiology of human obesity. International Journal of Obesity. 2008;32:1764–1779. doi: 10.1038/ijo.2008.129. [DOI] [PubMed] [Google Scholar]
- 23.Champaneri S, Xu X, Carnethon MR, Bertoni AG, Seeman T, DeSantis AS, et al. Diurnal salivary cortisol is associated with body mass index and waist circumference: The Multiethnic Study of Atherosclerosis. Obesity. 2013;21(1):E56–E63. doi: 10.1002/oby.20047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Purnell JQ, Kahn SE, Samuels MH, Brandon D, Loriauz DL, Brunzell JD. Enhanced cortisol production rates, free cortisol, and 11β-HSD-1 expression correlate with visceral fat and insulin resistance in men: Effect of weight loss. American Journal of Physiology Endocrinology and Metabolism. 2009;296:E351–E357. doi: 10.1152/ajpendo.90769.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Epel ES, McEwen BS, Seeman T, Matthews K, Castellazzo G, Brownell KD, et al. Stress and body shape: Stress-induced cortisol secretion is consistently greater among women with gentral fat. Psychosomatic Medicine. 2000;62(Suppl 1):623–632. doi: 10.1097/00006842-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Kouvonen A, Kivimäki M, Väänänen A, Elovainio M, Ala-Mursula L, Virtanen M, et al. Job strain and adverse health behaviors: The Finnish Public Sector Study. Journal of Occupational and Environmental Medicine. 2007;49:68–74. doi: 10.1097/JOM.0b013e31802db54a. [DOI] [PubMed] [Google Scholar]
- 27.Lallukka T, Lahelma E, Rahkonen O, Roos E, Laaksonen E, Martikainen P, et al. Associations of job strain and working overtime with adverse health behaviors and obesity: Evidence from the Whitehall II Study, Helsinki Health Study, and the Japanese Civil Servants Study. Social Science & Medicine. 2008;66(8):1681–1698. doi: 10.1016/j.socscimed.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 28.Choi B, Ko S, Landsbergis PA, Dobson M, Schnall PL. Job strain and health-related lifestyle. American Journal of Public Health. 2014;104:e3. doi: 10.2105/AJPH.2013.301757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith P. Potentially misleading conclusions: Job strain and health behaviors. American Journal of Public Health. 2014;104:e4. doi: 10.2105/AJPH.2013.301758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heikkila K, Fransson EI, Nyberg ST, Zins M, Westerlund H, Westerholm P, et al. Job Strain and Health-Related Lifestyle: Findings From an Individual-Participant Meta-Analysis of 118 000 Working Adults. American Journal of Public Health. 2013;103(11):2090–2097. doi: 10.2105/AJPH.2012.301090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lupien SJ, McEwen BS, Cunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behavior, and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- 32.Zhao I, Bogossian F, Turner C. Does maintaining or changing shift types affect BMI?: A longitudinal study. Journal of Occupational and Environmental Medicine. 2012;54:525–531. doi: 10.1097/JOM.0b013e31824e1073. [DOI] [PubMed] [Google Scholar]
- 33.Leclere A. Shift-work and cardiovascular disease. European Journal of Epidemiology. 2010;25:286–286. doi: 10.1007/s10654-010-9456-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hattori A, Sturm R. The obesity epidemic and changes in self-report biases in BMI. Obesity. 2013;21:856–860. doi: 10.1002/oby.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siegrist J. Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]