Abstract
Despite an unprecedented urgency to control health care costs while simultaneously improving quality, there are many barriers to investing in quality improvement. Traditional fee-for-service reimbursement models fail to reward providers whose improved processes lead to decreases in billable clinical activity. In addition, providers may lack the necessary skills for improvement, or the organizational infrastructure to conduct these activities. Insurance firms lack incentives to invest in health care delivery system improvements that lead to benefits for all patients, even those covered by competitors. In this paper, we describe a novel program in its sixth year of existence that funds ambulatory care improvements through a collaborative partnership between a local academic healthcare delivery system and an insurance firm. The program is designed as a competitive grant program and the payer and the health care organization jointly benefit from completed improvements projects. Factors contributing to the ongoing success of the program and lessons learned are discussed in order to inform the potential development of similar programs in other markets.
Keywords: quality improvement, academic medical center, ambulatory care
Introduction
Despite an unprecedented urgency to control health care costs while simultaneously improving quality, barriers to investing in improvement continue to stymie progress. Physicians and insurers struggle alike to find sustainable models to align priorities and fund health care innovations. Practices are challenged by the misalignments between achieving improvements in care and reimbursement, lack of time for and costs of improvement work, inadequate performance data available for performance measurement, and lack of process improvement knowledge and skills (Audet, Doty, Shamasdin, & Schoenbaum, 2005; Holmboe et al., 2005; Wolfson et al., 2009). Even efforts made by insurers to optimize health care value through benefit design, communicating and sharing data with providers, and financial incentives (such as pay for performance programs) have had variable impacts, as physicians working with multiple insurers are frequently overwhelmed by insurer's differing priorities that affect only a subset of the provider's actual panel (Goldberg, Mick, Kuzel, Feng, & Love, 2012; Rosenthal, Fernandopulle, Song, & Landon, 2004).
In response to demands to rapidly improve health care value, new multi-stakeholder partnerships have developed. These alliances recognize the inter-dependencies between the community, payers, delivery system, and regulators, and leverage the complimentary knowledge and capabilities of each entity (Lasker, Weiss, & Miller, 2001). While some improvement collaboratives have had remarkable success (Clampitt & DeKoch, 2011), there are many challenges. Recent research raises questions about the effectiveness and sustainability of these approaches (Hearld, Alexander, & Mittler, 2012; Landon et al., 2004; McHugh et al., 2012; Mittman, 2004; Ovretveit et al., 2002; Young, 2012). There is a growing literature examining large regional or national healthcare-focused collaboratives, but little attention has been directed to success factors for small partnerships between local health care systems and insurers created to support innovations in care. Local partnerships may be advantageous for working on problems that are specific to a particular market or delivery system (“bottom up” solutions) and may be easier to manage given the smaller number of collaborating agents, geographic proximity resulting in easier relationship-building, and the congruence of improvement goals.
In this article, we describe a sustained six-year partnership, between an academic physician practice and a local health insurance plan, designed to support improvements in ambulatory health care. Our program is structured as a competitive grant program, providing frontline care teams with one year of financial support and improvement resources to innovate care processes. Since 2006, this program has provided funding for 78 improvement projects, with over $1.1M total funding awarded. We describe lessons learned from this collaboration in the hopes that this successful program can be a model for others seeking sustainable funding for delivery system improvements through collaboration with a local insurer.
Methods
Description of the Health Care Setting
This program is a collaboration between University of Wisconsin Medical Foundation (UWMF), an academic faculty practice, and Physicians Plus Insurance Corporation (PPIC), a commercial insurer; both are located in Madison, Wisconsin. UW Health represents the academic health care entities of the University of Wisconsin-Madison: UWMF, UW Hospital and Clinics, UW School of Medicine and Public Health, American Family Children's Hospital and UW Carbone Comprehensive Cancer Center. When the program started, approximately 14% of UW Health's patient charges were received from the commercial insurer's population. The commercial insurer is a locally owned health maintenance organization with approximately 95,000 members at the time the co-funded improvement program was created. PPIC's population received primary care from multiple different physician group practices, and UWMF physicians provided 77% of total services to the insurer's population at the time the program was created in 2006.
Description of the Current Ambulatory Care Innovation Grant Program
The Ambulatory Care Innovation Grant (ACIG) program was designed to stimulate innovations in ambulatory care, including improved health outcomes, patient experience, and efficiency. All members of the health system are encouraged to apply, including physicians, residents, clinical, and non-clinical staff. UWMF and PPIC contribute to a fund that supports the innovations that are selected through this competitive grant program. The total program funding is determined by each contributing partner's budget. Grants are awarded annually. On average, between eight and nine ACIG projects have been funded each year. The number of annual funded projects has ranged from four to 14 in the 10 rounds since the start of the program.
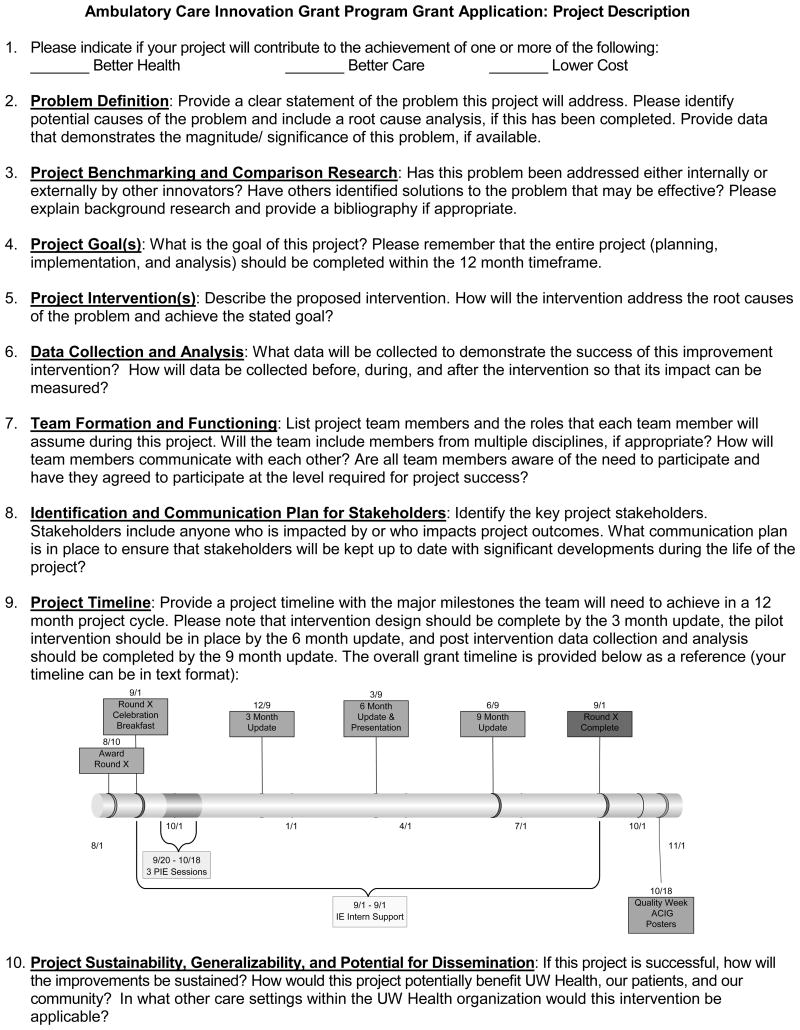
Applicants complete an application identifying a lead contact and the team that will be engaged in the improvement work. They also outline the focus of the proposed improvement, project goals, data collection plan, timeline, and budget. A portion of this application has been included as Figure 1.
Figure 1. Ambulatory Care Innovation Grant Application.
The maximum amount that can be requested for each project is $25,000. Each proposed budget is reviewed in detail, and for projects that are selected, the funding amount that is awarded is dependent on appropriateness of the requested items. Applicants are expected to review the relevant literature prior to the application, as well as previous work done on this problem at the local setting. The ACIG program does not require use of previously described interventions as the intent is to support innovation. In addition, applicants must provide appropriate letters of support from site leadership and other stakeholders. Criteria for selection are described for the applicants.
The ACIG Selection Committee individually scores grant applications according to a standardized scoring template (Table 1). The selection committee is comprised of a multidisciplinary group of physicians and administrators from the health system and the insurance corporation who meet to discuss each application individually and determine awards.
Table 1.
ACIG Scoring Template.
| Applicants score each item (except 0) from 1-5 (where 5 is the highest). |
|---|
| 0. Should this application be considered for an award? Yes/No |
| If this answer is no, you are not required to provide scores for any of the following questions, but please indicate why in the “Notes” section |
| 1. Alignment with Triple Aim |
| Project is aligned with one or more of the following: |
| 1. Improve the health of the population |
| 2. Enhance the patient experience and quality of care |
| 3. Optimize the value of care |
| 2. Problem Definition |
| Application includes a clear statement of the problem |
| Potential causes of the problem or improvement opportunity have been identified |
| Magnitude/significance of the project is established |
| 3. Project Benchmarking and Comparison Research |
| Research conducted on existence and/or effectiveness of intervention in other systems |
| Bibliography of literature reviewed is provided |
| 4. Project Goals |
| Goal of the project is clearly defined, reasonable, and feasible in the 12 month timeline |
| 5. Project Intervention(s) |
| Application includes a clear definition of the intervention(s) |
| Intervention appears appropriately designed to achieve goal |
| Intervention addresses identified root causes (if applicable) |
| 6. Data Collection and Analysis |
| High level data collection plan detailing what measures will be collected and used |
| Measures are appropriate, objective, and obtainable |
| Team plans to collect baseline and post intervention data to measure its impact |
| 7. Team Formation and Functioning |
| Proper team is assembled to complete and meet project objectives |
| Team has multidisciplinary representation from project stakeholders |
| Roles for the team members are clearly defined |
| Basic communication plan has been developed |
| 8. Identification and Communication Plan for Stakeholders |
| Project stakeholders have been identified |
| Describes the impact of the intervention on the stakeholders and/or customers |
| Communication plan is identified to ensure stakeholders are informed |
| 9. Project Timeline |
| Application includes a timeline with major milestones and tasks |
| Project timeline is realistic, feasible, and allows timely completion of the project |
| 10. Project Sustainability, Generalizability, and Potential for Dissemination |
| Project team has plan to maintain changes after ACIG period |
| Project outcome is generalizable to other locations |
| Intervention has potential to produce desirable outcomes at the pilot site or beyond |
| 11. Resources and Funding |
| Requested budget is appropriate for proposed intervention and implementation |
| 12. Grant Total Score |
| 13. Additional Notes/Missing Items |
After selection, ACIG recipients are honored at an award breakfast and oriented to the ACIG program. Recipients are required to participate in three process improvement education sessions (provided by the quality staff at UW Health) within the first two months of receiving their award. During the 12-month grant period, ACIG recipients are required to submit status updates to the program manager at three-month intervals. Project funds are disbursed throughout the course of the grant period by completing a Request for Funds Disbursement Form. These funds are provided to support the intervention, and are not dependent on achieving specific milestones or goals.
Each team is assigned an improvement coach to work with them for five hours per week through the year grant cycle. An additional expense of $4,500 per project is allocated for this coach support. These coaches are advanced industrial engineering graduate students from the University of Wisconsin who work as part-time members of the Quality, Safety, and Innovation (QSI) department at UWMF. Industrial engineers provide expertise to teams in the form of project management, human factors analysis, process edesign, data analysis, facilitation, and teaching improvement skills (including on-site process improvement training) throughout the course of the grant. Each coach works directly with the project team to ensure deadlines are completed successfully. A senior health systems engineer (a QSI staff member) supervises the coaches and meets with them weekly to review the status of each grant, discuss barriers, and troubleshoot ongoing issues as needed.
This program has enhanced our partnership with UW Health and the UW School of Engineering by providing students with real-life experiences in health care and supporting teams with the unique skills and knowledge that industrial engineers provide. Improvement teams gather on multiple occasions through the year to share lessons learned and identify opportunities to collaborate on projects. The teams share final results through poster and oral presentations during UW Health's annual Quality Week event.
ACIG projects are limited to one year in length. By design, the ACIG program does not provide continued funding for projects not completed in one year. As part of the application process, team leaders are asked to discuss plans for sustaining improvements if their project is successful. However, project leads may apply for grants in future funding cycles that move the original projects in new directions. This allows project teams to build on their previous results.
Direct program oversight is provided by an ACIG executive committee that consists of physicians, administrators, and quality improvement specialists. This team includes both the medical directors of operations and quality from the academic faculty group practice and the medical director and quality director of the insurance company. These executives oversee the management and operations of the program, and make collaborative decisions. UW Health provides the entire infrastructure for the program. A program manager who is a highly skilled member of the health system's quality improvement department provides oversight to ACIG teams and coaches, and manages administrative responsibilities (budget, personnel, operational). The program manager also keeps the executive committee up-to-date with program questions or concerns. Program decisions ranging from grant selection to operational issues are made by consensus and all information about the program is fully transparent. Interested parties in both organizations are kept up-to-date through email, phone communication, and participation in structured learning sessions held throughout the grant cycle during which improvement teams present results they achieved.
Changes to the Program over Time
Over the years, the ACIG program evolved from a “simple” distribution of funds to a comprehensive program of improvement. The selection process has evolved from an informal discussion about the merits of each application to a standardized scoring process, including both quantitative and qualitative evaluations. The structured application process requires the applicants to identify roles and responsibilities of team members, clarify the current problem, and ensure organizational support for the proposed improvement work.
Mandatory team training in basic improvement principles and tools and year-long support with an improvement coach was instituted in the third year of the program after reviewing the variable quality of early improvement projects. Formal project updates were instituted every three months to keep teams on schedule, along with a final report upon project completion. These interventions were very impactful; subsequent grants now routinely finish on time and within budget. Critical to ACIG's success is the overall management of the program, in particular the oversight and communication responsibilities of the program manager, as this degree of transparency between the partners results in high levels of trust.
In addition, over time, several operational improvements and processes (improved budget request forms, revised intranet site for communications, Institutional Review Board FAQ related to quality improvement) were implemented. We also recognize the importance of dissemination and made poster and oral presentations a requirement for each project team.
Program Evaluation
To assess if improvement interventions from ACIG grants are sustained over time, an e-mail survey was distributed in 2012 to ACIG project leaders from 2006-2010. Surveys were distributed to 37 of the 55 project leaders as 18 of the original project leaders had changed employment and were unable to provide feedback. Two multiple-choice questions were asked: “Have you sustained the improvements made as part of your ACIG project?” (answer choices included: completely sustained, somewhat sustained, and not sustained) and “Do you continuously monitor data regarding your ACIG improvement?” (answer choices included continuously monitor data, sometimes monitor data, and never monitor data). The third question was open-ended and asked, “What changes have you made to your new ACIG process or intervention since the end of the ACIG period?” A final yes/no question was asked about dissemination, “Have you spread your intervention or improved process to a different department or unit at UW Health?” Each e-mail was personalized and provided a link to the online survey. Participants had two weeks for survey completion. The response rate was 65%. Results were downloaded and analyzed through basic graphical displays of percentages.
Results
The 78 projects that have been completed are categorized in Table 2. These projects have occurred across a wide spectrum of activities, from patient and provider education to care processes and operational workflows. Examples of these projects include: urgent care patient flow redesign to improve utilization, centralized triage process for three dermatology clinics, centralized referral process for chronic pain appointments, and developing sinus infection phone protocols to improve access with physicians. Depending on the intervention, many teams involve patients as advisors to inform their interventions.
Table 2.
Summary of ACIG Projects by Category.
| Category | Description | Number of Projects |
|---|---|---|
| Chronic Care Management | Chronic disease models and condition specific interventions for asthma, diabetes, hypertension, and obesity | 13 |
| Clinical Intervention | Testing new therapy methods such as healing touch and experiential therapy | 4 |
| Efficiency | Improving access, patient flow, and operational processes (e.g., phone triage) | 5 |
| Operational Interventions | Implementing data collection plans, patient panel management systems, and incentive programs | 8 |
| Patient Education | Videos, brochures, websites and other patient educational materials for specific conditions | 13 |
| Provider Education | Educational resources for providers such as decision support tools, scorecards, videos, and training sessions | 9 |
| Shared Medical Appointments | Testing shared medical appointment and peer support models for various conditions and patient types | 12 |
| Tools & Technology | Innovative cell phone applications, interactive websites, patient screening tools and improvements within the Electronic Health Record | 14 |
| 78 |
Improvement teams work on problems that are experienced at their local area of care, but a number of grants have led to interventions that have been disseminated beyond a single care unit. Table 3 shows the results of the 2012 survey sent to past ACIG project leaders. Most (88%) of the projects have been completely or somewhat sustained; and 50% of projects spread their intervention to a different department or unit within the academic health care system.
Table 3.
ACIG Sustainability Survey.
| Survey Question | Number of Responses | Percentage of Response |
|---|---|---|
| Have you sustained the improvements made as part of your ACIG project? | ||
| Completely sustained | 12 | 50% |
| Somewhat sustained | 9 | 38% |
| Not sustained | 3 | 13% |
| Have you spread your intervention or improved process to a different department or unit at UW Health? | ||
| Yes | 12 | 50% |
| No | 12 | 50% |
| Do you continuously monitor data regarding your ACIG improvement? | ||
| Continuously monitor | 6 | 25% |
| Sometimes monitor | 7 | 29% |
| Never monitor | 11 | 46% |
Operational directors, who directly observe ambulatory processes, have confirmed these sustained improvements.
Two case studies are provided as examples of successful projects. Case 1 highlights a funded intervention that resulted in improvements in patient satisfaction and clinical metrics, along with staff knowledge.
The second case demonstrates the role of the improvement coach supporting the project team.
Not all projects have developed sustained improvements. The inability to sustain improvements has been related to a variety of causes, including: turnover of staff or faculty who served as the improvement champion, failure to embed an improved process into standard management practice with continuous monitoring of pertinent data, and changing local or organizational priorities over time resulting in redeployment of resources. For example, one of the grants focused on bringing families together at a primary care clinic to discuss improving fitness and healthy lifestyles. When the physician champion left the clinic, other staff resources were not available to sustain the peer support group. Over the years, the selection committee has addressed these challenges by selecting grants that: (1) have identified operational resources that can be committed to sustaining improvements as part of the initial application, and (2) have improvement goals that are aligned with broad organizational priorities.
Discussion
We describe a six-year partnership between an academic physician practice and a local insurance plan that has funded 78 ambulatory care improvement projects. This co-funded program provides frontline teams with training in improvement skills and financial and coaching support for improvement work throughout the grant period. Limitations to the success of this program include the inability to sustain all successful interventions and engage patients in each improvement effort. Despite these limitations, the program has been co-funded for six years with both partners finding value in the successful innovations discovered by grant-funded improvement teams. In addition to measurable improvements developed by project teams, the program has had a number of positive impacts that are not easily quantifiable. Program funders have continued to support this program over the years, which may be considered an indirect measure of the value this program provides. There is an increased interest in improvement work as confirmed by increases in the number of applications over the years (123%). The improvement training that teams receive can be applied to future improvement work, thereby building the organization's organizational capacity for continuous improvement by frontline teams. Grant recipients have used their ACIG work to serve as pilot data for larger competitive grant submissions. Physicians, clinical, and non-clinical staff have published their work (Schrager & Gaard, 2009; A. Sheehy et al., 2011; A. M. Sheehy et al., 2010), presented projects at professional meetings, used their work to inform state health policy plans (Wisconsin Asthma Coalition, 2009), and created freely available highly-accessed online teaching modules and handouts (UW Integrative Medicine Program, 2008).
This ongoing program has increased our organizational capacity for performance improvement. Our experience managing a portfolio of high quality improvement projects has provided us with the expertise to support faculty working on recertification; UW Health has recently been accepted as a Maintenance of Certification Portfolio Sponsor. Also, the ACIG improvement education programs were the prototype for our enterprise-wide system of process improvement education.
Our improvement program addresses many of the improvement barriers identified in the literature for practices and insurers. Physician practices face multiple challenges to improvement work, including lack of time, costs related to the improvement work, lack of improvement skills and knowledge, and little reward for this work (Audet, et al., 2005; Goldberg, et al., 2012; Holmboe, et al., 2005; Rosenthal, et al., 2004; Wolfson, et al., 2009). Our program successfully removed these barriers by providing financial support, improvement education and mentoring, and public recognition for project teams. Successful improvement relies on engaged teams working toward clear goals. The application process allows for the selection of highly motivated teams who have articulated the focus of their improvement work and established goals (Cohen, Ptaskiewicz, & Mipos, 2010; Grumbach & Bodenheimer, 2004; Nelson et al., 2002). ACIG applications require letters of support from senior leaders, ensuring organizational support for this improvement work. Our survey results confirm that, unlike many “top-down” improvement interventions imposed on frontline care teams, the ACIG team improvements tend to sustain. We postulate that this is due to the selection of highly invested teams who are solving relevant problems. A number of these local improvements have been disseminated between care sites within our delivery system, which supports the benefit of this program as an “incubator” for innovation. Similarly, the insurer can disseminate successful practices to physicians and facilities not affiliated with the academic system or directly implemented by the insurance corporation.
Improvement collaboratives have gained traction as a strategy to align improvement resources to solve healthcare problems, but there is little evidence on effectiveness and the growing recognition of the large amount of resources required to maintain these groups (Hearld, et al., 2012; Landon, et al., 2004; Leatherman et al., 2003; McHugh, et al., 2012; Mittman, 2004). We believe that local partnerships may be more successful and easier to maintain in the long term as partners focus on highly congruent improvement goals and geographic proximity facilitates close working relationships. Partnerships have a greater chance of being successful if each partner achieves benefits from the collaboration that are greater than could be achieved if each acted alone (Lasker, et al., 2001). In our program, both funding partners benefit from the improvements demonstrated by the ACIG teams and each acknowledges the fact that these “bottom up” improvements might not otherwise be possible given the current environment that is fraught with budget constraints and increasing mandatory “top down” improvement priorities generated by external organizations. Our grant selection process ensures that both funding partners have the opportunity to award only those teams that are working on problems of interest to both parties. Frequent communications and meetings have contributed to the success of this six-year program. This small, local partnership minimizes the costs of maintaining a larger multi-stakeholder alliance while still addressing problems that span both the provider and payer communities.
Our experience with the ACIG program has led to important lessons for implementing and developing similar innovation programs. Defined improvement project criteria (Table 1) and standardized improvement training increased the number of teams that successfully achieved project aims by the end of the grant period. Ongoing support from a skilled improvement coach was critically important to maintain project momentum, especially for busy clinical teams who struggle to find time for long-term projects. Projects that were tightly aligned to organizational priorities were more successful, potentially due to the increased interest and support of senior leaders. Our experience with this program has led to an increased number of training sessions in improvement knowledge and skills, now available to all members of the health system. As reimbursement is increasingly tied to performance, health systems have an increased incentive to invest in programs that can effectively develop high performing teams. Our findings and subsequent discussion are subject to limitations and risk. Our results are drawn from the experience of a large group practice and might not apply to other settings without the resources available to support such an endeavor. In addition, the ability to use resources from our affiliated academic departments (e.g., industrial engineering students) is not replicable in all settings. Neither ACIG partner can fully articulate the return on investment in this program which threatens ongoing financial commitment. Internal politics and changes in the external environment challenge the trust and cohesiveness that are crucial to the partnership. Increasing demands resulting from federal and state health care reform decrease the time and resources that either PPIC or UW Health can devote to this program. Our finding that only 54% of teams continued to monitor data reflects the difficulty of embedding site-specific quality improvement activities into standard operations. Additionally, we are limited in our knowledge of project sustainability to what was reported on the survey. While verified by operational leaders, the program did not have the data resources to provide ongoing monitoring of each project. However, in some cases (such as the example in Case Study 2), program-assisted implementation was a first step to longer projects beyond the end of the grant cycle. Project team goals are not mandated beyond alignment with the IHI Triple Aim (Institute for Healthcare Improvement, 2013). As a result, not all projects engaged patients or were designed to change patient behavior. This may be viewed as a limitation by some. Finally, we have increasingly recognized the value of patient participation in improvement project design. The importance of involving patients has been incorporated into our quality improvement training, however it is not a mandatory part of project proposals.
Despite these limitations, we have created and shared the elements of our successful partnership between an academic physician practice and a local payer to co-fund grants for improvement work in ambulatory care. This model has led to care improvements that are beneficial to both partners. We hope that others can use this information as anticipatory guidance for forming similar partnerships with local health insurers and physician practices in order to promote improvement work that is locally relevant and mutually beneficial.
Figure 2. UWHealth A1c Control Rates and Clinic Ranking.
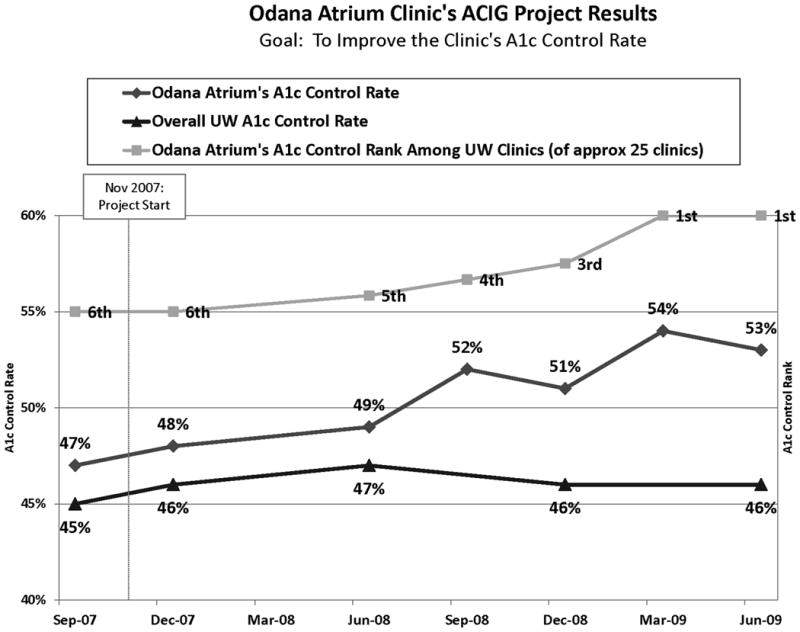
Case Study 1. ACIG Diabetes Education and Medication Titration Project.
Background
An example of a successful ACIG project is Accelerated Access to Basic Diabetes Education and Medication Titration for Patients in their Medical Home, led by a nurse practitioner at a Family Medicine clinic from 2007-2009. The goal of the project was to improve glucose control in type 2 diabetes patients (as measured by A1c levels) by developing educational programs for patients and staff and providing ongoing medication titration by care managers through evidence-based algorithms. This project was awarded $23,000 in grant funding in support of audio-visual equipment, information technology support, educational materials, certified diabetes educator hours, and float staff time.
Methods
A series of educational classes were offered to all clinic staff to learn about diabetes management and the new model of care. Care managers, registered nurses overseen by the nurse practitioner project lead, titrated diabetes medications using protocols. An educational program was developed for patients at their clinic, instead of referring patients to outside diabetes educators. To measure the impact of these interventions on A1c, the project leader referred to UW Health metrics reported to the Wisconsin Collaborative for Healthcare Quality. Metrics on A1c are fly reported quarterly and externally reported annually. Staff and providers were knowledge tested before and after participating in the education sessions to understand the effectiveness of the sessions (n=71). To test retention of knowledge, the test was administered again to staff and providers eight months after the sessions (n=59). Patients were surveyed during the educational intervention to obtain feedback about their satisfaction with the educational program and confidence in staff's knowledge (n=50). The survey consisted of eight questions, with response choices on a scale from 0 (low) to 5 (high).
Results
The interventions resulted in improved A1c control in patients from 47% in control at the start of the project to 53% at the end of the project. The clinic's rank for glucose control among other UW Health primary care clinics increased from sixth to first (Figure 2). Staff and provider test scores increased by 24 percentage points (n=64) after participating in the education sessions. In the follow-up test, scores increased further by an additional 15 percentage points. The results of the patient satisfaction survey showed 96% of patients were confident in the staff's knowledge, 90% were confident in the staff's ability to manage patients with diabetes, 92% were satisfied with medication teaching, and 92% felt they had adequate time with staff. The results of this project led to an organization-wide spread of the process across all primary care clinic sites.
Case Study 2. Highlighting the Coach Role: ACIG Prevention of Excess Gestational Weight Gain Project.
Background
The Prevention of Excess Gestational Weight Gain was led by an obstetrician in 2011-2012. Its goal was to increase the percentage of prenatal patients who receive antenatal gestational weight gain counseling consistent with Institute of Medicine (IOM) guidelines.
Methods
A best practice alert was implemented in the electronic health record (EHR), triggered by new pregnancy. This alert continued at each visit until weight gain counseling was provided and documented. Additionally, education was provided to nurses and prenatal providers in the form of presentations at meetings and a formal Grand Rounds presentation. The project lead also conducted site visits at each participating clinic to champion this work.
The Role of the Industrial Engineering Coach
The coach provided project management so that deliverables were met. They performed human factors analysis for creating the electronic alert. They then performed chart abstraction and data analysis of baseline and post-intervention values.
Results
The intervention was successful. Fifty-one percent of women received gestational weight gain counseling consistent with IOM guidelines as compared to 3% who received this pre-intervention (p=.005). Eighty-nine percent of pre-gravid BMI were documented in the EHR as compared to 80% pre-intervention (p=.000). The project lead is in the process of publishing these results and plans to apply for an external grant to analyze post-delivery data on the women in this study. The team also is seeking opportunities to further disseminate their results through state-wide research networks.
Acknowledgments
The authors want to acknowledge Ron Parton, MD MPH, as the co-originator of the program in 2006 when he was the Vice President and Chief Medical Officer for Physicians Plus Insurance. They appreciate the contributions of Pat Udelhofen, NP, and Marilyn Chohaney, MD, who were the ACIG grant team leaders for the Odana case study described in this article. The authors also thank Zaher Karp for his editorial assistance. This paper was supported by the Primary care Academics Transforming Healthcare (PATH) Writing Collaborative and the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. In addition, Nancy Pandhi is supported by a National Institute on Aging Mentored Clinical Scientist Research Career Development Award, grant number l K08 AG029527. Additional support was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program.
Biography
Dr. Sally Kraft is the Medical Director for the University of Wisconsin Health Quality, Safety and Innovation department in Madison, Wisconsin. She is a Clinical Associate Professor of Medicine at the University of Wisconsin School of Medicine and Public Health. She has completed fellowships in critical care medicine, pulmonary medicine, and in quality improvement and health services.
Elizabeth Strutz is a Senior Health Systems Engineer with the University of Wisconsin Health Quality, Safety and Innovation department. She holds a bachelor's and master's degree in Industrial and Systems Engineering, with a concentration on human factors in healthcare, from the University of Wisconsin-Madison. Ms. Strutz has been the Program Manager of the Ambulatory Care Innovation Grant program for the past three years.
Dr. Kay is Vice President and Chief Medical Officer of the Physicians Plus Insurance Corporation in Madison, Wisconsin. He is responsible for strategic direction and operational oversight for medical and pharmacy management, provider contracting and network management, and clinical quality for a regional commercial managed care insurance plan.
Dr. Welnick provides strategic leadership for all UW Medical Foundation clinical operations, including physician work force planning, implementation and ongoing clinic management as Medical Director of Ambulatory Clinic Operations at the University of Wisconsin Medical Foundation. He directs the clinic administration of both UW Medical Foundation and UW Hospital and Clinics, working closely with the clinical department chairs and UW Health leadership. He is also an Associate Clinical Professor in the Department of Medicine.
Dr. Pandhi is an Assistant Professor in the Department of Family Medicine. She is a health services researcher and practicing family physician. Her research program is directed towards effective ambulatory primary care transformation.
Footnotes
No financial disclosures were reported by the authors of this paper.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
Sally Kraft, Quality, Safety, and Innovation, UW Health; Department of Medicine, University of Wisconsin School of Medicine and Public Health; Primary care Academics Transforming Healthcare (PATH) Writing Collaborative, University of Wisconsin School of Medicine and Public Health.
Elizabeth Strutz, University of Wisconsin Medical Foundation.
Lawrence Kay, Physicians Plus Insurance Corporation.
Richard Welnick, Ambulatory Clinic Operations, University of Wisconsin Medical Foundation; Department of Medicine, University of Wisconsin School of Medicine and Public Health.
Nancy Pandhi, Department of Family Medicine, University of Wisconsin School of Medicine and Public Health; Health Innovation Program, University of Wisconsin School of Medicine and Public Health; Primary care Academics Transforming Healthcare (PATH) Writing Collaborative, University of Wisconsin School of Medicine and Public Health.
References
- Audet AM, Doty MM, Shamasdin J, Schoenbaum SC. Measure, learn, and improve: physicians' involvement in quality improvement. Health Affairs (Millwood) 2005;24(3):843–853. doi: 10.1377/hlthaff.24.3.843. [DOI] [PubMed] [Google Scholar]
- Clampitt PG, DeKoch RJ. Transforming Leaders Into Progress Makers: Leadership for the 21st Century. Thousand Oaks, CA: SAGE Publications; 2011. [Google Scholar]
- Cohen PM, Ptaskiewicz M, Mipos D. The Case for Unit-Based Teams: A Model for Front-line Engagement and Performance Improvement. The Permanente Journal. 2010;14(2):70–75. doi: 10.7812/tpp/09-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DG, Mick SS, Kuzel AJ, Feng LB, Love LE. Why Do Some Primary Care Practices Engage in Practice Improvement Efforts Whereas Others Do Not. Health Services Research. 2012 doi: 10.1111/1475-6773.12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? The Journal of the American Medical Association. 2004;291(10):1246–1251. doi: 10.1001/jama.291.10.1246. [DOI] [PubMed] [Google Scholar]
- Hearld LR, Alexander JA, Mittler JN. Fostering change within organizational participants of multisectoral health care alliances. Health Care Management Review. 2012;37(3):267–279. doi: 10.1097/HMR.0b013e31822aa443. [DOI] [PubMed] [Google Scholar]
- Holmboe E, Kim N, Cohen S, Curry M, Elwell A, Petrillo MK, Meehan TP. Primary care physicians, office-based practice, and the meaning of quality improvement. The American Journal of Medicine. 2005;118(8):917–922. doi: 10.1016/j.amjmed.2005.05.015. [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. Triple aim: the best care for the whole population at the lowest cost. 2013 from http://www.ihi.org/offerings/Initiatives/TripleAim.
- Landon BE, Wilson IB, McInnes K, Landrum MB, Hirschhorn L, Marsden PV, Cleary PD. Effects of a quality improvement collaborative on the outcome of care of patients with HIV infection: the EQHIV study. Annals of Internal Medicine. 2004;140(11):887–896. doi: 10.7326/0003-4819-140-11-200406010-00010. [DOI] [PubMed] [Google Scholar]
- Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Quarterly. 2001;79(2):179–205. III–IV. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leatherman S, Berwick D, Iles D, Lewin LS, Davidoff F, Nolan T, Bisognano M. The business case for quality: case studies and an analysis. Health Affairs (Millwood) 2003;22(2):17–30. doi: 10.1377/hlthaff.22.2.17. [DOI] [PubMed] [Google Scholar]
- McHugh MC, Harvey JB, Aseyev D, Alexander JA, Beich J, Scanlon DP. Approaches to improving healthcare delivery by multi-stakeholder alliances. American Journal of Managed Care. 2012;18(6 Suppl):s156–162. [PubMed] [Google Scholar]
- Mittman BS. Creating the evidence base for quality improvement collaboratives. Annals of Internal Medicine. 2004;140(11):897–901. doi: 10.7326/0003-4819-140-11-200406010-00011. [DOI] [PubMed] [Google Scholar]
- Nelson EC, Batalden PB, Huber TP, Mohr JJ, Godfrey MM, Headrick LA, Wasson JH. Microsystems in health care: Part 1. Learning from high-performing front-line clinical units. The Joint Commission Journal on Quality Improvement. 2002;28(9):472–493. doi: 10.1016/s1070-3241(02)28051-7. [DOI] [PubMed] [Google Scholar]
- Ovretveit J, Bate P, Cleary P, Cretin S, Gustafson D, McInnes K, Wilson T. Quality collaboratives: lessons from research. Quality and Safety in Health Care. 2002;11(4):345–351. doi: 10.1136/qhc.11.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal MB, Fernandopulle R, Song HR, Landon B. Paying for quality: providers' incentives for quality improvement. Health Affairs (Millwood) 2004;23(2):127–141. doi: 10.1377/hlthaff.23.2.127. [DOI] [PubMed] [Google Scholar]
- Schrager S, Gaard S. What should you do when your patient brings a list? Fam Pract Manag. 2009;16(3):23–27. [PubMed] [Google Scholar]
- Sheehy A, Pandhi N, Coursin DB, Flood GE, Kraft SA, Johnson HM, Smith MA. Minority status and diabetes screening in an ambulatory population. Diabetes Care. 2011;34(6):1289–1294. doi: 10.2337/dc10-1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehy AM, Flood GE, Tuan WJ, Liou JI, Coursin DB, Smith MA. Analysis of guidelines for screening diabetes mellitus in an ambulatory population. Mayo Clin Proc. 2010;85(1):27–35. doi: 10.4065/mcp.2009.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson D, Bernabeo E, Leas B, Sofaer S, Pawlson G, Pillittere D. Quality improvement in small office settings: an examination of successful practices. BMC Family Practice. 2009;10:14. doi: 10.1186/1471-2296-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young GJ. Multistakeholder regional collaboratives have been key drivers of public reporting, but now face challenges. Health Affairs (Millwood) 2012;31(3):578–584. doi: 10.1377/hlthaff.2011.1201. [DOI] [PubMed] [Google Scholar]
- UW Integrative Medicine Program. Teaching modules & patient handouts. 2008 http://www.fammed.wisc.edu/integrative/modules.
- Wisconsin Asthma Coalition. Wisconsin asthma plan: 2009-2014. Madison, WI: Wisconsin Department of Health Services; 2009. [Google Scholar]