Abstract
Background
Rett syndrome is a severe neurodevelopmental disorder mainly affecting females and scoliosis is a common comorbidity. Spinal fusion may be recommended if the scoliosis is progressive. This qualitative study investigated recovery of girls with Rett syndrome during the first 12 postoperative months and explored family perspectives and coping around the time of surgery.
Method
Parents registered with the population-based Australian Rett Syndrome Database were recruited to this study if their daughter had a confirmed pathogenic MECP2 mutation and spinal fusion between 2006 and 2012. Twenty-five interviews were conducted to determine their daughter’s recovery and parental stresses and coping. Themes in the interview data were identified with content analysis and the regaining of gross motor skills over the first 12 postoperative months were described with time-to-event (survival) analysis.
Results
Pain and energy levels, appetite, mood and coinciding health issues influenced their daughter’s postoperative recovery. The majority of girls recovered preoperative sitting (88%), standing (81%) and walking (80%) by 12 months. The decision to proceed with surgery was associated with feelings of fear, obligation, relief and guilt for families. Development of complications, poor support and feelings of isolation increased their emotional burden whilst adequate information and discharge preparation, confidence in self and staff, and balancing personal needs with their daughter’s care relieved this burden.
Interpretation
Our study identified clinical practice issues in relation to families whose daughter with Rett syndrome undergoes spinal fusion, issues that are also relevant to other severe disabilities. Return of wellness and gross motor skills following spinal fusion in girls with Rett syndrome occurred within the first 12 postoperative months in most cases. Parents require information and practical support to alleviate their emotional burden.
Keywords: Rett syndrome, scoliosis, spinal fusion, gross motor skill, family coping, qualitative, population-based
INTRODUCTION
Rett syndrome (RTT) is a rare neurodevelopmental disorder generally associated with a mutation on the X-linked MECP2 gene.(Amir et al. 1999) Whilst early development is largely normal, it is followed by a period of regression with loss of hand and communication skills and the development of hand stereotypies and impaired gait.(Neul et al. 2010, Hagberg 2002) Scoliosis is a common comorbidity in RTT diagnosed in approximately 75% of a population-based sample by 13 years.(Ager et al. 2006)A scoliosis that is progressive may be associated with pain, decline in motor skills and restrictive lung disease,(Berven and Bradford 2002) and spinal surgery may be recommended when the curve is progressive and reaches a magnitude greater than 50°.(Downs et al. 2009) Families then have to weigh up the benefits and risks of spinal surgery, a process accompanied by considerable emotional stress in Rett syndrome(Ager et al. 2009) as for other conditions with severe scoliosis.(Barnard et al. 2013, Salisbury et al. 2007) Spinal fusion is a complex and lengthy procedure, and the likelihood of post-operative complications is high.(Gabos et al. 2012)
There has been some investigation of the recovery of wellbeing and gross motor skills following spinal fusion in the girls with RTT. In a Swedish study (n=23), improved posture and balance as well as fewer daytime naps were observed at 12 months and maintained in 19 of the subjects followed over six years.(Larsson et al. 2009) A UK parent-report survey reported that 42/50 (84%) individuals improved primarily in relation to sitting posture, respiratory infections and digestion of food, and pre-operative ability to walk was maintained post-operatively after at least 12 months.(Kerr et al. 2003) Whilst physical wellbeing appears to improve, information is limited on this recovery.
Parents of teenagers with adolescent idiopathic scoliosis have indicated less seeking of social support following their child’s spinal fusion.(Salisbury et al. 2007) In a qualitative study involving parents with a child with complex needs (mainly severe cerebral palsy) and a spinal fusion, fifteen reported difficulties meeting their physical, emotional and social needs following surgery.(Barnard et al. 2013) Families with a child with Rett syndrome reported additional physical strain when supporting their daughter’s activities of daily living postoperatively.(Ager et al. 2009) There are many challenges for families on the journey of parents as their child recovers from spinal fusion but limited literature on factors that could reduce the profound accompanying stress.
There remains a need for better evidence and advice that supports the decision making of both clinicians and families whilst the option of spinal fusion is being considered. We recently investigated family satisfaction following spinal fusion in RTT,(Downs et al. 2014) an important outcome in the quality of care framework which encompasses treatment effectiveness; patient safety; economic costs; accessibility to treatment; and acceptability of the treatment including satisfaction.(Long et al. 1993) The population-based Australian Rett Syndrome Database (ARSD) was established in 1993 and collects data longitudinally on girls and women with RTT.(Downs et al. 2008) To understand more about treatment effectiveness and acceptability to families, the current study recruited families from the ARSD and explored the course of their daughter’s recovery following discharge from hospital and family perspectives.
METHODS
In May 2013, the ARSD included 394 girls and women born since 1976 with 69 (17.7%) having died since data collection commenced. Over this period, 87 (22.1%) girls and women with RTT in Australia have undergone a spinal fusion. Families whose daughters were registered with the ARSD were included in the current study if their daughter had a pathogenic MECP2 mutation and a spinal fusion between 2006 and 2012, a recent time period chosen to reduce recall error. Twenty-eight individuals with RTT met the study criteria three having died prior to recruitment, and families of 21/25 (84%) females with RTT were recruited. An additional four families whose daughters’ surgery was prior to 2006 were also recruited to enable greater variability and achievement of thematic saturation: two girls walked pre-operatively, one mother had health needs simultaneously with her daughter’s surgery and one girl experienced very frequent seizures and poor feeding at the time of surgery. Twenty-four parents (one father) who were the primary caregiver participated representing 25 females with RTT (one mother had twin daughters). Data in the ARSD was supplemented with data collected from medical records for subject description including mutation type, best pre-operative level of mobility and aspects of the hospital stay (Table 1). The mean (SD) age at interview was 17 years 6 months (4 years 4 months).
Table 1.
Distribution of MECP2 mutation type and description of preoperative characteristics and the hospital stay (n=25)
| Mean (standard deviation) | |
|---|---|
| Pre-operative Cobb angle (degrees) | 71 (19) |
| Age at surgery (years) | 12.5 (2.5) |
| Median (range) | |
| Days ventilated | 0 (0 – 3) |
| Days in the intensive care unit | 2 (0 – 16) |
| Length of hospital stay (days) | 11.5 (5 – 31) |
| n (%) | |
| Pathogenic mutation | |
| Early truncating | 1 (4%) |
| Large deletion | 3 (12%) |
| p.R106W | 3 (12%) |
| p.R133C | 2 (8%) |
| p.R168X | 3 (12%) |
| p.R270X | 3 (12%) |
| p.R294X | 1 (4%) |
| p.T158M | 4 (16%) |
| Other | 5 (20%) |
| Pre-operative mobility level | |
| Independent walking | 4 (16%) |
| Walking with assistance | 6 (24%) |
| Supported standing | 11 (44%) |
| Wheelchair-dependent | 4 (16%) |
| Spinal fusion procedurea | |
| Posterior | 19 (76%) |
| Anterior/posteriorb | 4 (16%) |
| Anterior | 2 (8%) |
| Post-operative complications | |
| Respiratoryc | 8 (32%) |
| Bleedingd | 6 (24%) |
| Over-sedation | 4 (16%) |
| Wound infection | 1 (4%) |
| Spinal cord injury | 1 (4%) |
Fusion extended to the pelvis for eight subjects;
All surgeries that including anterior and posterior fusion were conducted in one stage;
Respiratory complication defined as a named diagnosis in the medical record of either pneumonia, atelectasis, pleural effusion or pneumothorax;
Bleeding complication recorded if a blood transfusion was recorded in the medical record.
A semi-structured stem and leaf interview schedule was designed with questions pertaining to parental concerns and their daughter’s recovery to 12 months postoperatively. The interview schedule was piloted with two mothers and their suggestions were accommodated. The interview included exploration of contextual factors such as family events to identify the timing of recovery of gross motor skills. All interviews were conducted on the telephone, recorded, transcribed and sent to participants for member checking (completed by 19/24 [79.2%]). Questions in the ARSD 2011/2 family questionnaire on family satisfaction or otherwise with the spinal fusion procedure(Downs et al. 2014) were reviewed for triangulation of findings to improve data credibility.(Krefting 1991) Data from both sources were consistent.
This study was approved by the Curtin University Human Research Ethics Committee (HR PT216/2012). Ethics approvals for access to medical records were obtained from the Princess Margaret Hospital for Children, Perth; Royal Perth Hospital, Perth; Women’s and Children’s Hospital, Adelaide; Royal Children’s Hospital, Melbourne; Sydney Children’s Hospitals Network, Sydney; Mater Children’s Hospital, Brisbane; and Royal Children’s Hospital, Brisbane.
Analysis
Content analysis of the interview transcripts was conducted. Initial grouping of data based on the content area of the question was completed using NVivo10 software and then read and re-read to form initial ideas of the data set. Common words and concepts within content areas were grouped to establish the key themes.(Liamputtong 2009) The themes were marked within the data to allow further reflection on each thematic decision and either confirm, refute or modify the original interpretations. A second researcher checked the coding. Coding of data continued until thematic saturation was achieved. Time-to-event (survival) analysis using the Kaplan-Meier method was used to describe regaining of gross motor skills over the first 12 postoperative months.
RESULTS
Post-operative course of the child’s recovery
Inpatient rehabilitation
Inpatient rehabilitation differed for each individual depending on recovery from the anaesthetic and post-operative complications. Almost all girls sat over the edge of the bed or in a wheelchair within the first post-operative week. “Physio started as soon as she was in ICU…she had surgery Friday morning and Saturday they had her sitting in her wheelchair”. Just under half of those with standing skills stood within the first week and a further two stood during the second post-operative week. Six of the ten girls with preoperative walking skills walked within seven days, three independently and three with assistance, and one walked with assistance in the second post-operative week. “The third day after surgery she was taking a few steps… and each day she would just do a little bit more”. The remaining three girls did not attempt to walk at all in hospital: one due to a spinal cord injury during surgery, one refusing to walk in the hospital setting and one with very limited pre-operatively walking abilities whose mother feared the impact walking might have on the spinal fusion. “I never walked her after surgery because I was too nervous that she was going to collapse…I was too nervous with the rods that she would put too much strain on them if she fell”.
Regaining activity levels and wellness
Periods of six weeks, three months or six months were given as the timeframe for recovery and return to pre-operative level of activities, and parents were asked to restrict participation in activities such as swimming and horse riding until medically advised to do so. Nevertheless, daily effort and commitment to rehabilitation were considered important during the early months, particularly in families whose daughter walked preoperatively or had experienced post-operative complications. “Every day, numerous times... it was really quite an intensive routine”. Determination and commitment were considered key factors influencing their daughter’s recovery. “I was very positive and determined she would get back to things. I would try little bits each day… to get her back to normal”. Strategies included formal physiotherapy, hydrotherapy, daily physical activity routines, and involving other carers to assist with day-to-day management.
Appetite returned following discharge. Some mothers reporting improved appetite, attributed to now not needing to support head posture and improved trunk posture. Increased constipation was frequently reported during the hospital and early post-discharge phases. Pain levels improved markedly following discharge and energy levels also improved by around six months postoperatively. Mothers watched carefully their daughter’s mood, some working to encourage their daughter’s smiles during the early post-operative period but mood also appeared back to normal by around six months postoperatively. Table 2 contains sample quotes describing the recovery of wellness at intervals over the first 12 months postoperatively.
Table 2.
Sample quotes describing the course of general wellness from when in hospital until 12 months postoperatively.
| Theme | In hospital | Within 6 weeks of discharge | 6 months following surgery | 12 months following surgery |
|---|---|---|---|---|
|
Energy levels |
“She was just very sleepy and very lethargic.” “She came out of the anaesthetic at the given time. And was remarkably bright, I would have expected her to be more drowsy and groggy, but she was pretty good.” |
“She was doing everything but she was tired, she would have sleeps in the afternoon, she just had a lot taken out of her.” “Her energy levels were low, but her alertness just got better and better each day.” |
“She was a lot more active by that stage, her energy levels were a lot stronger.” “Even pre-operatively she would have days where she would be sleepy all day and another day where she is alert so it is much the same now.” |
“She wouldn’t fatigue as quickly as she did prior to surgery. Her stamina just got better.” “She was back to what she was before surgery in terms of energy levels, her sleeping was an issue but it wasn’t because of pain or surgery.” |
|
Pain and comfort |
“She would wake up and start saying “my back Mum, my back” and she had never said those words at all, so whenever she was in pain she would be screaming at me.” “She was in a lot of pain, so prior to moving her for the first couple of days she was given oxycodone to help with the pain.” “Any activities on the physical side of things, she had her pain relief half an hour prior.” |
“I was giving it to her regularly because I wasn’t sure if she was in pain or not” “I was just giving her paracetamol…if it looked like she was in pain.” “Probably within less than two weeks she was off the pain medication.” |
“She was a lot more comfortable.” |
“It had levelled out by 6 to 12 months, you wouldn’t really have even known she had had surgery.” |
| Eating | “Eating returned to normal after about a week, but they had her on a nasogastric tube because they lose a lot of weight, so that came back after a week.” “Because she had the nasal tube down her throat, it was very tender to swallow…Until they took out the nasal tube, it took another day before we could get her to swallowing. But once she started eating she was on full recovery.” “She wouldn’t eat. She was being fed through a NG tube. I think that was part of the shock of everything. Whenever she gets sick, the first thing she does is not eat.” |
“She didn’t really eat until she came home.” “Her eating improved out of sight, it was amazing. Although she has the PEG and we were using that for fluid and medication, she was eating all her meals, was eating more, and eating so much better.” “I didn’t have to keep her head upright and she was eating and chewing and the food wasn’t falling out, she was enjoying eating again which was really nice to see, so yes definitely her appetite improved.” |
“I think her food intake increased, and she did eat more food because she wasn’t suffering indigestion or heart burn.” |
|
| Mood | “She knew she wasn’t herself… She was very introverted, she just wasn’t terribly interested in anything that was going on.” “We noticed she was much better, she was happy, more relaxed and she was eating well.” |
“She was still tiring very easily, but she was much happier.” “Maybe it was just the fact she was sitting so straight, but she just seemed really pleased with herself and really proud of herself.” “I really had to fight and find ways to get her to look at me, to even smile and she is a smiley child” |
“She was just very happy and happy to be sitting up. And alert and watching what was going on and being involved in things….” “She was much better, pretty much back to her old self. She was smiling and she was happy, and eager for her food again.” |
“She is just her usual self. I think she is a lot happier now that she is able to support herself and her spine.” “She was definitely back to her old self after 12 months.” |
|
Coinciding health related issues |
“Constipation…that was one of the biggest problems coming home because of all the drugs.” “We found if she was constipated and had to push then it really hurt her back. So we had to increase her dose of Movicol.” |
“Her seizures were under control which they hadn’t been before, whether or not that was related to her overall health or not, but certainly we had better seizure control since she had her back done.” “Unfortunately after the surgery in April, in October of that year we had the worst ever pneumonia.” |
“As for chest infections I think they did improve. The severity didn’t lessen, she would still be sick for 2 or 3 weeks at a time, but the frequency of them decreased.” “Overall, her health has improved out of sight, she hasn’t been into hospital since the surgery, she hasn’t had a chest infection, if she gets a cold she seems to clear it.” |
|
Regaining gross motor skills
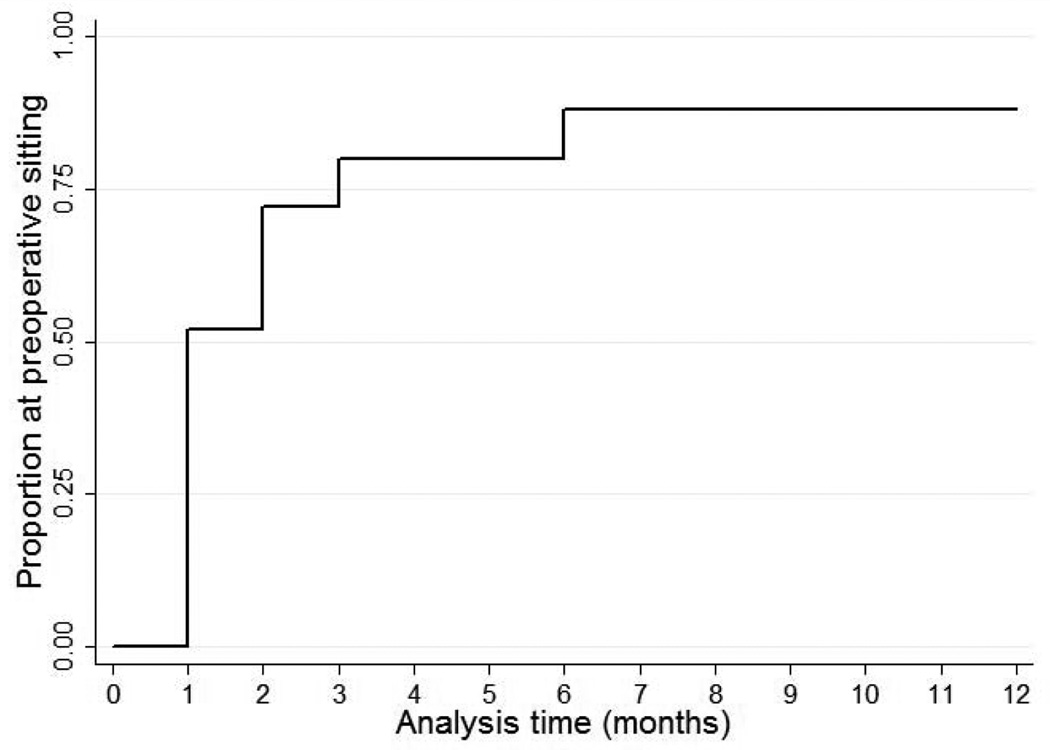
Preoperative sitting ability was regained in thirteen girls (52%) after one month and 22 (88%) by six and 12 months (Figure 1). All parents reported improved sitting posture following surgery with additional improvements reported for duration of sitting (11/25, 44%) and head control (2/25, 4%). The majority of parents perceived improvements in comfort levels when sitting although this was difficult to judge given impaired communicative skills. Three girls did not regain their preoperative level of sitting by 12 months: one suffered a spinal cord injury and took longer to regain motor skills, one had an intervening femoral fracture and one sat independently but for a shorter duration.
Figure 1.
Time to return to preoperative level of sitting ability over the first 12 months postoperatively (n=25)
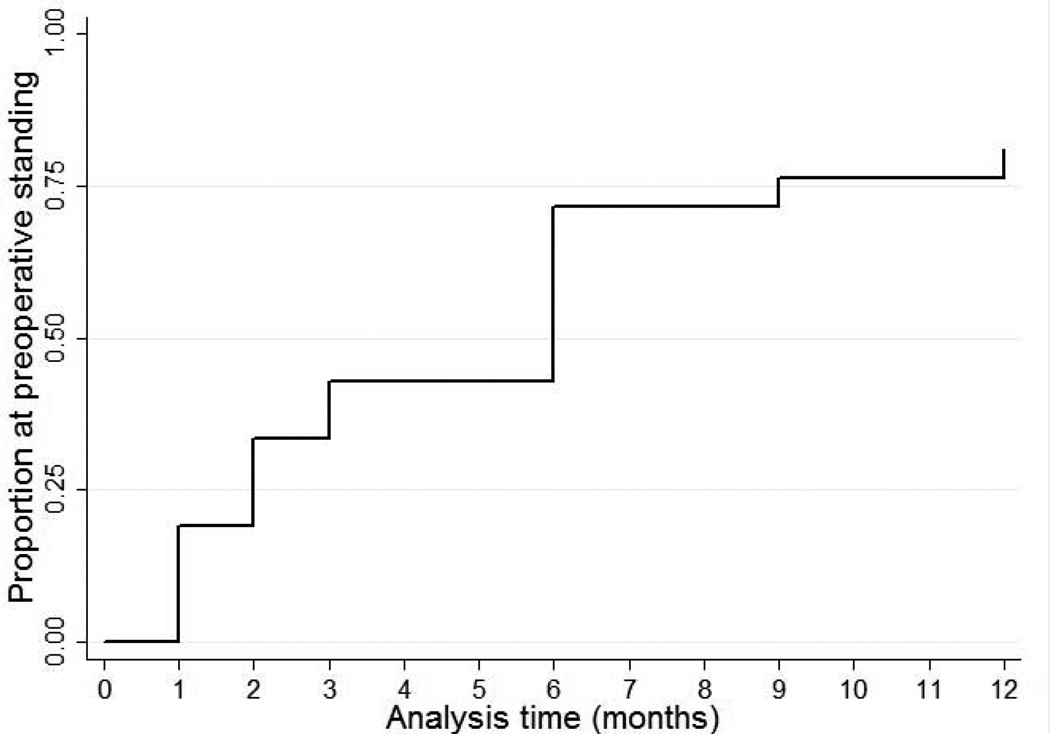
Of the 21 girls with pre-operative standing skills, four (19%) regained preoperative levels by one month, 15 (71%) by six months and 17 (81%) by 12 months post-surgery (Figure 2). In addition to improvements in posture and alignment, three girls improved in duration of standing. Four did not recover their preoperative standing ability within 12 months: two did not attempt standing (one family believed that standing was not allowed), one took longer due to spinal cord injury and one was generally weaker. One girl who did not stand preoperatively recovered supported standing over the first three months.
Figure 2.
Time to return to preoperative level of standing ability over the first 12 months postoperatively (n=21)
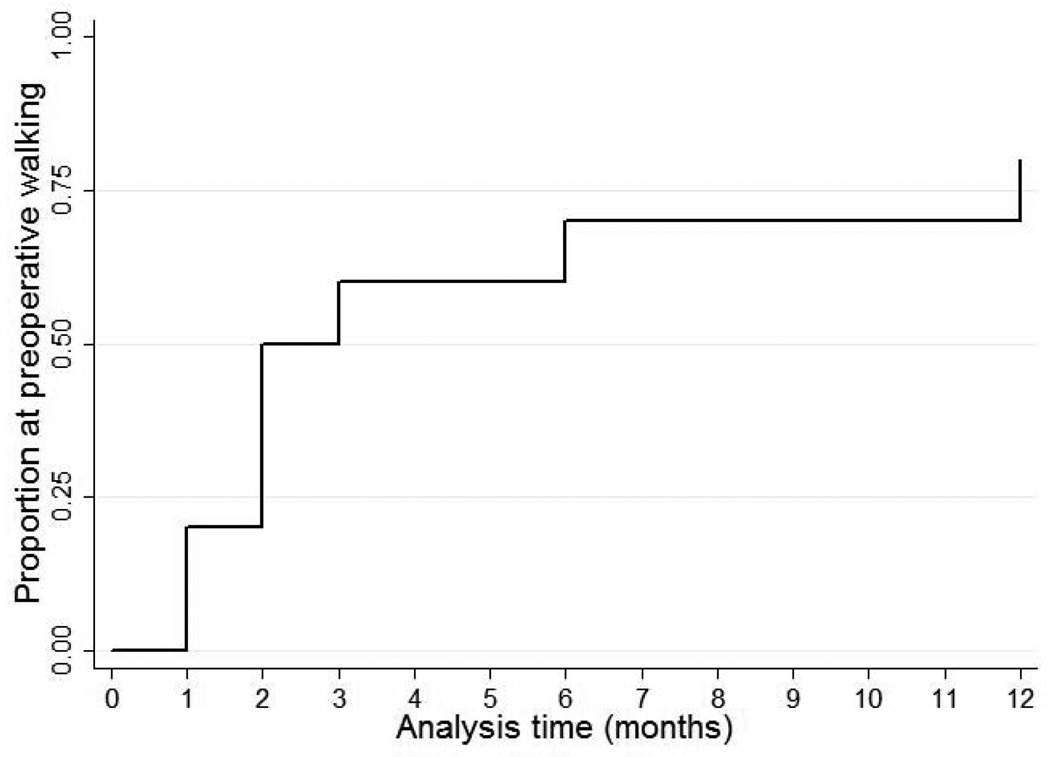
Pre-operative walking skills were regained by two of the 10 girls (20%) by one month, seven (70%) by six months and eight (80%) by 12 months postoperatively (Figure 3). Two girls who walked with assistance did not recover preoperative walking by 12 months: one did not attempt to walk again and the girl with the spinal cord injury took longer to regain preoperative walking levels. All girls who recovered their preoperative skills improved in posture and alignment. Additionally, improved duration of walking was reported in one and improved ease of walking reported for four.
Figure 3.
Time to return to preoperative level of walking ability over the first 12 months postoperatively (n=10)
Family experiences
Emotions when consenting to surgery
Agreeing to proceed with surgery was accompanied by emotions of fear, obligation, guilt and relief. Most parents reported feelings of fear and worry in relation to the potential for complications, pain and also for their daughter’s life. “It was fear of the unknown when you haven’t been through anything like that yourself and then having to put your child through something like that”.
Feelings of having no other choice but surgery were described by approximately two thirds consequent to the progressive nature of the curve and its detrimental effects on the daughter’s function and health. “It was becoming life threatening to leave her as she was, it was one evil or the other and one had more chance of success than leaving her”. A minority of mothers were less clear on the need for surgery but agreed with their doctor’s advice. “It wasn’t something we wanted, the doctor said it was getting bad and that she needed to do it”.
Slightly fewer than half felt relief or happiness once their decision to choose surgery was made. Families were hopeful and confident that surgery would reverse the detrimental effects scoliosis and prevent future complications. “Once we had decided it was kind of a relief. It is the beforehand when you don’t know what you are going to do that is stressful.” Some described feelings of guilt at deciding on surgery on their daughter’s behalf, putting their daughter through a high-risk procedure and inevitably causing her to experience a period of discomfort and suboptimal health. “We were making a decision on her behalf, it wasn’t her decision, she hadn’t been consulted”.
Family challenges during recovery
Families made arrangements to adjust work patterns and maintain family routines during the hospital stay, with a longer hospital stay associated with greater feelings of frustration and exhaustion. “Being in hospital was stressful for everybody. My mum had to come and live with my boys and I was in hospital 24/7”. Post-operative complications (Table 1) were stressful for parents. More severe complications required a prolonged hospital stay that was associated with emotional turmoil for the whole family. “Because we were there for so long, it had a really stressful impact on the family”. For some, a prolonged hospital stay proved beneficial in allowing additional practice with handling and transfer skills in a supervised environment, more time to organise home equipment and support services, and reduced concerns regarding wound management.
The provision of information regarding post-discharge management enabled feelings of preparedness and confidence for management at home. “They gave me everything I needed to know. I remember them saying what I needed to do and how I needed to manage her”. Others did not feel adequately informed on post-discharge management in relation to aspects such as equipment adjustment and installation and practising correct handling techniques, and this was associated with anxiety. “Setting up of the wheelchair and what you have to deal with when you get home I thought would all fall in place, I probably didn’t put enough thought into it and they didn’t explain it enough”.
Some mothers were full-time carers and did not work but for the majority (17/24), one or both parents took time off work during the inpatient stay and up to eight weeks following discharge to provide their daughter with care. Feeling “isolated” particularly in the first two months following discharge was expressed by parents who took time off work, lacked strong family support or time to themselves for relaxation and recuperation. “I did feel very isolated because I was home for six weeks with not much support…I remember getting very down about it all”.
In these early months, networks of family members and friends were helpful in supporting the provision of care. Without these networks, the emotional and physical impacts of care were increased and greater reliance was placed on formal services. For some families, obtaining help from appropriate services was a challenging task in itself. “It became more stressful trying to get the help and manage the situation than what it was to do it myself”.
Strategies to relieve stress
Family-reported ingredients for managing stress including feeling that surgery had been the right choice, preoperative planning of postoperative support structures, developing confidence in themselves to support their daughter, and finding balance between caring for their daughter’s and their own needs for personal time after discharge. Table 3 provides sample quotes of personal experiences and advice to future families in relation to stress.
Table 3.
Themes and sample quotes describing factors that influenced parent’s emotional burden and their advice to other families.
| Theme | Personal experiences | Advice to other families | ||
|---|---|---|---|---|
|
Certainty in their decision |
“She looked so thrilled with herself, sitting up, big smiles and looking really proud of herself…So at that point in time we just knew we had made the right decision.” “Once the pain ceased and she was getting strong again and it had improved her posture quite dramatically, then we had definitely done the right thing.” |
“I would highly recommend it to anyone who was concerned before to go with it, because the benefits far outweighed any of the concerns.” “The earlier you choose to make the decision, the better the recovery for your child and the hope of them getting through it.” |
||
|
Importance of pre- and postoperative preparation |
“Because I was worried about looking after her, I did organise some emergency respite before I went in, which in retrospect was very very handy.” “I may have got the physio involved and talked about wheelchair adjustments and things like that earlier on…ours all ended up being rush rush rush.” |
“They need to prepare by talking about what will happen before, after and during it. Be prepared mentally for any setbacks because there are highs and lows.” “From the time the surgeon says ‘you’ll need this and that’ start getting an OT and physio involved to help prepare with the equipment you’ll need.” |
||
|
Reliance on support structures |
“I had home-care people coming, that helped because when they came I could go out to the shops, grab groceries.” “I would have asked for a lot more help and I would have insisted on a lot more help.” |
“The main thing is to make sure they get the support, because that will help a lot…the support helps you get through it.” “For families who haven’t got great informal support, just to make sure they’ve got good formal support and council support.” |
||
|
Confidence in parental intuition |
“I would have pushed them to repeat the UTI test or at least start some sort of medication…I would have been more proactive in that area if I had known how bad that could go.” “When she had that complication when the wires had broken on the rod…I would have pushed or made more of an effort to get over to Melbourne sooner rather than leave it to the point when it became an issue.” |
“Be confident about it, that you can handle it, because you have to be sure you are doing the right thing.” “Be assertive towards staff, have confidence in the staff looking after her, but if you do have an issue then talk about it because it’s your child that is laying there.” |
||
|
Balancing commitment to daughter’s care and personal time |
“The biggest thing was having more time for myself. Having a break, because it was 24/7, and just needing that bit of time out.” “From my perspective it was that every hour of every day was completely devoted to her… And sometimes you just think ‘ah I want to be like normal people, get in the car, go shopping’ and do something for myself.” |
“It is hard work, but only hard work for the first 2 months and then you will be able to sit back and say it was worth it.” “It is really hard and you do have to prepare yourself for it, but the long term benefits, in our case, far outweigh the inconvenience of hospital and recovery time.” |
||
DISCUSSION
Scoliosis occurs commonly in RTT and for those with a progressive scoliosis, a substantial proportion will undergo spinal fusion. Spinal fusion is extensive surgery and should be conducted within a multidisciplinary paediatric setting following preoperative planning and with specialist paediatric pain management teams.(Gibson 2004, Graham et al. 2009, Playfor et al. 2006) Families in Australia with a daughter with Rett syndrome have reported high satisfaction with hospital processes particularly those in intensive care settings.(Downs et al. 2014)
Spinal fusion is however associated with a high incidence of short-term complications, often respiratory(Gabos et al. 2012) as also found in our sample. A previous cross-sectional survey(Kerr et al. 2003) (n=50) reported delayed oral feeding postoperatively in a small number of girls, possibly influenced by different caregivers and routines in hospital. In our study, the majority experienced poor appetite in hospital that improved after discharge. Constipation occurs commonly in Rett syndrome(Motil et al. 2012) and was often exacerbated following surgery, likely due to use of opioid medications and reduced mobility. Monitoring pain following discharge was challenging for families as the girls were unable to communicate verbally and its presence was often difficult to interpret.(Downs et al. 2010) Families therefore relied on their own intuition and their daughter’s body language when deciding if pain was present. Complete wellness was perceived around six months postoperatively coinciding with bony healing,(Reuter-Rice and Bolick 2011) and possibly associated with reduced discomfort and fatigue and improved alertness and social engagement when sitting upright with improved posture. Our findings are consistent with previous studies(Larsson et al. 2009, Kerr et al. 2003) but our rich qualitative dataset enabled us to track the recovery of these important everyday general health issues. Our data also articulated the breadth of family concerns for their daughter’s recovery beyond the immediate surgical outcomes such as reduction in the severity of the scoliosis.
The majority of girls continued rehabilitation after discharge with family commitment to a proactive lifestyle. In some cases, avoidance of postoperative mobilisation in relation to parental anxiety could have been prevented with education and advice because one aim of the surgery is to maintain functional abilities.(Ager et al. 2009) Almost all girls regained their preoperative sitting, standing and walking levels by 12 months postoperatively. In previous studies, 11 of 13 girls (n=50)(Kerr et al. 2003) who walked preoperatively were walking at 12 months and all 7 (n=19) girls who walked preoperatively continued to walk at four years follow-up (Larsson et al. 2009). In our genetically confirmed sample, we have additionally plotted the recovery of gross motor skills at intervals over 12 months finding rapid recovery of sitting and a more gradual return of standing and walking skills. We also report improved posture in all and improved skills in approximately half of the girls. However, postoperative complications and the general fragility of RTT (eg, high incidence of fracture (Downs et al. 2008)) influenced a small proportion of girls whose recovery took longer.
Families experienced many emotions when choosing spinal fusion for their daughter, their fears and anxiety likely attributable to the complexity of the procedure, the risk of complications and concerns as to how their daughter would recover. Consistent with previous literature, families whose daughter could walk preoperatively appeared to experience greater emotional burden.(Ager et al. 2009) Following the surgery, parents needed to trust their own knowledge about their daughter and have opportunity to voice any concerns regarding medical issues. A survey of 348 parents of children admitted to hospital found that on discharge, parent perceptions that their child was well enough were strongly associated with lower likelihood of readmission during a 30-day period.(Berry et al. 2013) These findings are consistent with our previous observations that strong partnerships between parents and clinicians are highly valued.(Downs et al. 2014) In a recent qualitative study, families with less discharge preparation and postoperative supports reported more negatively regarding their stress.(Barnard et al. 2013) In the current study, parents identified specific needs for information and supports consistent with good clinical practice that could potentially alleviate such stressors for future families facing scoliosis surgery. The child needs the very best surgical care, but families also need a more comprehensive range of supports to help them to manage and support their daughter’s and family’s health following discharge.
The ARSD enabled identification of almost all females with RTT in Australia who have had spinal fusion and despite RTT being a rare disorder, we have investigated detail pertaining to recovery following a complex clinical care episode. To reduce recall error, we restricted the sample to those who had surgery after 2006, however included four additional families who gave greater variability of experiences to the study and enabled the data to reach thematic saturation. Our response fraction for the current study was high giving representativeness to the data and allowing us to report for almost the entire cohort over this time period. Our high member checking response fraction improved data accuracy. We acknowledge that parents were likely to report favourably on their experiences given they had consented to surgery.(Redelmeier and Dickinson 2011) To offset this potential for bias, interviews were conducted by researchers who were not involved in the provision of clinical care and participants were encouraged to discuss their experiences in depth describing positive and negative aspects. We also acknowledge that our data are retrospective. However, we mainly recruited families whose daughter had surgery over the last five years to reduce recall error and asked probing questions pertaining to the contexts and family events that occurred when aspects of recovery were reported so that we could plot the course of recovery more precisely. Finally, our data were reported by the primary caregivers who were mainly mothers. We acknowledge that fathers often serve different roles, have different experiences and that their perspectives would be a valuable topic for research.
We have conducted a qualitative study sourced from a population-based register on postoperative recovery following spinal fusion in RTT. Our findings provide a greater understanding of the course of care beyond the surgery and the early days in hospital, and enable clinicians to provide families with more accurate information regarding the likely postoperative course for recovery of wellbeing and motor skills. We have also reported strategies consistent with good clinical practice that could help families reduce their substantial emotional burden. These support strategies are relevant not only to RTT but also to families of children with other severe disabilities and scoliosis who need surgical correction.
KEY MESSAGES.
Appetite, mood and energy levels improved markedly by six months post-discharge.
Most girls regained preoperative gross motor skill levels and many had improved by 12 months.
Families reported mixed emotions when consenting to spinal fusion for their daughter.
Support and preparation for discharge favourably influenced family coping and reduced the substantial emotional burden.
Acknowledgements
The authors would like to thank those families who participate in the Australian Rett Syndrome Study and gave their time and thoughts for our interviews. We extend our gratitude to the Australian Paediatric Surveillance Unit (APSU) and the Rett Syndrome Association of Australia for their ongoing support in case ascertainment. Lastly, we gratefully acknowledge the advice and support of Associate Professors Diana Hopper and Kylie Hill in the School of Physiotherapy and Exercise Science, Curtin University. The Australian Rett Syndrome Study was previously supported by the National Institute of Health Grant 5R01HD043100-05 and NHMRC project grant #303189 and is currently supported by NHMRC project grant #1004384 and ARC Linkage grant LP098984. Helen Leonard was previously funded by a NHMRC program grant #353514. Her current funding is from an NHMRC Senior Research Fellowship #57256.
Footnotes
Conflict of interest
The authors report no conflicts of interest.
Contributor Information
Caitlin Marr, Email: caitlinmarr@hotmail.com, School of Physiotherapy and Exercise Science, Curtin University, Perth, Australia.
Helen Leonard, Email: helen.leonard@telethonkids.org.au, Telethon Kids Institute, University of Western Australia, Perth, Australia.
Ian Torode, Email: Ian.Torode@rch.org.au, Department of Orthopaedics, Royal Children’s Hospital, Melbourne, Australia.
Jenny Downs, Email: jenny.downs@telethonkids.org.au, School of Physiotherapy and Exercise Science, Curtin University, Perth, Australia and Telethon Kids Institute, University of Western Australia, Perth, Australia.
REFERENCES
- Ager S, Downs J, Fyfe S, Leonard H. Parental experiences of scoliosis management in Rett syndrome. Disability and Rehabilitation. 2009;31:1917–1924. doi: 10.1080/09638280902846392. [DOI] [PubMed] [Google Scholar]
- Ager S, Fyfe S, Christodoulou J, Jacoby P, Schmitt L, Leonard H. Predictors of scoliosis in Rett syndrome. Journal of Child Neurology. 2006;21:809–813. doi: 10.1177/08830738060210091501. [DOI] [PubMed] [Google Scholar]
- Amir RE, Van Den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genetics. 1999;23:185–188. doi: 10.1038/13810. [DOI] [PubMed] [Google Scholar]
- Barnard JG, Albright K, Morrato EH, Nowels CT, Benefield EM, Hadley-Miller NA, Kempe A, Erickson MA. Paediatric spinal fusion surgery and the transition to home-based care: provider expectations and carer experiences. Health Soc Care Community. 2013;21:634–643. doi: 10.1111/hsc.12049. [DOI] [PubMed] [Google Scholar]
- Berry JG, Ziniel SI, Freeman L, Kaplan W, Antonelli R, Gay J, Coleman EA, Porter S, Goldmann D. Hospital readmission and parent perceptions of their child's hospital discharge. Int J Qual Health Care. 2013;25:573–581. doi: 10.1093/intqhc/mzt051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berven S, Bradford DS. Neuromuscular scoliosis: Causes of deformity and principles for evaluation and management. Seminars in Neurology. 2002;22:167–178. doi: 10.1055/s-2002-36540. [DOI] [PubMed] [Google Scholar]
- Downs J, Bebbington A, Woodhead H, Jacoby P, Jian L, Jefferson A, Leonard H. Early determinants of fractures in Rett syndrome. Pediatrics. 2008;121:540–546. doi: 10.1542/peds.2007-1641. [DOI] [PubMed] [Google Scholar]
- Downs J, Bergman A, Carter P, Anderson A, Palmer GM, Roye D, Van Bosse H, Bebbington A, Larsson EL, Smith BG, Baikie G, Fyfe S, Leonard H. Guidelines for management of scoliosis in Rett syndrome patients based on expert consensus and clinical evidence. Spine. 2009;34:E607–E617. doi: 10.1097/BRS.0b013e3181a95ca4. [DOI] [PubMed] [Google Scholar]
- Downs J, Geranton S, Bebbington A, Jacoby P, Bahi Buisson N, Ravine D, Leonard H. Linking MECP2 and pain sensitivity: the example of Rett syndrome. American journal of medical genetics. Part A. 2010;152A:1197–1205. doi: 10.1002/ajmg.a.33314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs J, Torode I, Ellaway C, Jacoby P, Bunting C, Wong K, Christodoulou J, Leonard H. Family satisfaction following spinal fusion in Rett syndrome. Dev Neurorehabil. 2014 doi: 10.3109/17518423.2014.898107. [DOI] [PubMed] [Google Scholar]
- Gabos PG, Inan M, Thacker M, Borkhu B. Spinal Fusion for Scoliosis in Rett Syndrome With an Emphasis on Early Postoperative Complications. Spine. 2012;37:E90–E94. doi: 10.1097/BRS.0b013e3182404698. [DOI] [PubMed] [Google Scholar]
- Gibson PR. Anaesthesia for correction of scoliosis in children. Anaesth Intensive Care. 2004;32:548–559. doi: 10.1177/0310057X0403200413. [DOI] [PubMed] [Google Scholar]
- Graham RJ, Wachendorf MT, Burns JP, Mancuso TJ. Successful and safe delivery of anesthesia and perioperative care for children with complex special health care needs. J Clin Anesth. 2009;21:165–172. doi: 10.1016/j.jclinane.2008.06.033. [DOI] [PubMed] [Google Scholar]
- Hagberg B. Clinical manifestations and stages of Rett syndrome. Ment Retard Dev Disabil Res Rev. 2002;8:61–65. doi: 10.1002/mrdd.10020. [DOI] [PubMed] [Google Scholar]
- Kerr AM, Webb P, Prescott RJ, Milne Y. Results of surgery for scoliosis in Rett Syndrome. Journal of Child Neurology. 2003;18:703–708. doi: 10.1177/08830738030180101201. [DOI] [PubMed] [Google Scholar]
- Krefting L. Rigor in Qualitative Research - The Assessment of Trustworthiness. American Journal of Occupational Therapy. 1991;45:214–222. doi: 10.5014/ajot.45.3.214. [DOI] [PubMed] [Google Scholar]
- Larsson EL, Aaro S, Ahlinder P, Normelli H, Tropp H, Oberg B. Long-term follow-up of functioning after spinal surgery in patients with Rett syndrome. Eur Spine J. 2009;18:506–511. doi: 10.1007/s00586-008-0876-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liamputtong P. Qualitative Research Methods. Melbourne: Oxford University Press; 2009. [Google Scholar]
- Long AF, Dixon P, Hall R, Carr-Hill RA, Sheldon TA. The outcomes agenda: contribution of the UK clearing house on health outcomes. Qual Health Care. 1993;2:49–52. doi: 10.1136/qshc.2.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motil KJ, Caeg E, Barrish JO, Geerts S, Lane JB, Percy AK, Annese F, Mcnair L, Skinner SA, Lee HS, Neul JL, Glaze DG. Gastrointestinal and nutritional problems occur frequently throughout life in girls and women with Rett syndrome. J Pediatr Gastroenterol Nutr. 2012;55:292–298. doi: 10.1097/MPG.0b013e31824b6159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neul JL, Kaufmann WE, Glaze DG, Christodoulou J, Clarke AJ, Bahi-Buisson N, Leonard H, Bailey MES, Schanen NC, Zappella M, Renieri A, Huppke P, Percy AK, Rettsearch C. Rett Syndrome: Revised Diagnostic Criteria and Nomenclature. Annals of Neurology. 2010;68:944–950. doi: 10.1002/ana.22124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Playfor S, Jenkins I, Boyles C, Choonara I, Davies G, Haywood T, Hinson G, Mayer A, Morton N, Ralph T, Wolf A. Consensus guidelines on sedation and analgesia in critically ill children. Intensive Care Med. 2006;32:1125–1136. doi: 10.1007/s00134-006-0190-x. [DOI] [PubMed] [Google Scholar]
- Redelmeier DA, Dickinson VM. Determining Whether a Patient is Feeling Better: Pitfalls from the Science of Human Perception. Journal of General Internal Medicine. 2011;26:900–906. doi: 10.1007/s11606-011-1655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter-Rice K, Bolick B. Pediatric Acute Care: A Guide for Interprofessional Practice. Jones & Bartlett Learning; 2011. [Google Scholar]
- Salisbury MH, Lamontagne LL, Hepworth JT, Cohen F. Parents' self-identified stressors and coping strategies during adolescents' spinal surgery experiences. Clin Nurs Res. 2007;16:212–230. doi: 10.1177/1054773807302732. [DOI] [PubMed] [Google Scholar]