Abstract
Purpose:
We studied the sleep macroarchitecture with polysomnography (PSG) in drug naïve patients with Parkinson's disease (PD) and reassessed them following treatment with levodopa.
Materials and Methods:
This prospective hospital-based study included 15 patients with PD (age: 59 ± 11.2 years, duration of PD: 11.8 ± 12.3 months; and male: female (M:F) = 11:4). They were assessed for demography, phenotype, modified Hoehn and Yahr staging (H & Y); Schwab and England and Activities of Daily Living (S and E ADL) Scale; and Unified PDRating Scale (UPDRS). Sleep was assessed using Epworth Sleepiness Scale (ESS), Pittsburgh Sleep Quality Index (PSQI), and National Institute of Mental Health and Neurosciences (NIMHANS) comprehensive sleep disorder questionnaire. They underwent overnight PSG at baseline and after13.3 ± 5.7 months of levodopa (440 mg/day).
Results:
Patients with PD had responded to levodopa as indicated by the significant improvement in UPDRS motor score in ON state compared to OFF state. Nocturnal sleep quality indices did not vary significantly, but the excessive daytime somnolence improved (P = 0.04) with levodopa. Sleep efficiency (P = 0.65), latency to sleep onset (P = 0.19), latency to stage 1 (P = 0.12), and duration of stage 1 (P = 0.55) had increased. Duration of ‘awake in bed’ (P = 0.24), slow wave sleep (P = 0.29), and rapid eye movement (REM) sleep (P = 0.24) decreased with treatment. Periodic leg movements (PLMs) had reduced (P = 0.68) and mean oxygen saturation during sleep improved (P = 0.002). Surprisingly, snore index (P < 0.03) during sleep had increased with levodopa.
Conclusions:
Sleep alterations in PD occur even in early stages due to the disease process. There was improvement in most of the parameters of sleep macroarchitecture with levodopa.
Keywords: Levodopa, Parkinson's disease, polysomnography, sleep
Introduction
Parkinson's disease (PD) is a neurodegenerative disease associated with loss of dopaminergic nigrostriatal neurons in the brainstem. It is associated with motor and nonmotor manifestations. The nonmotor symptoms of PD including sleep disorders have recently become the subject of intense study.[1,2] Sleep disorders in PD include insomnia, hypersomnia and parasomnia.[3] Sleep disturbances in PD have been variably attributed to the disease process itself and to the dopaminergic medications. However, the contribution of each is not defined. These studies have invariably been in advanced PD patients on medications. A systematic study of sleep objectively in the early stages of the disease, in drug naïve state[4] and studying its course as the disease progresses and the patients are started on medicationis lacking due to the nature and the demands of such a study. Follow-up studies after starting on levodopa are far and few, and hence the need for this study.
We evaluated the sleep macroarchitecture in patients of levodopa naïve PD with overnight polysomnography (PSG) and reassessed them with PSG following treatment with levodopa.
Materials and Methods
This prospective, hospital-based study was carried out in the Department of Neurology at the National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore from January 2008 to December 2010. The study was approved by the institutional ethics committee. Written informed consent was obtained from the study subjects. Fifteen patients with newly diagnosed Parkinson's disease, who had never previously received levodopa, who fulfilled the UK Parkinson's Disease Society Brain Bank Clinical Diagnostic Criteria,[5] and were drug naïve; were recruited. In a study by Hughes et al., involving brains of 143 patients with Parkinsonism, the sensitivity of the final PD clinical diagnosis was 91%, a specificity of 98%, and a positive predictive value of 99%.[6] Patients with features of vascular, drug-induced, post-encephalitic, posttraumatic Parkinsonism, similar familial illness, and other Parkinson's plus syndromes were excluded. Response to levodopa was noted in all after the initial evaluation for the study. They were not on any dopaminergic drugs. All recruited patients who reported during follow-up regularly; maintained on stable dose of the medication, for a minimum of 6 months; and reassessed after 13.3 ± 5.7 months with a repeat clinical questionnaire and overnight PSG were included in the study.
The PD severity was assessed by modified Hoehn and Yahr staging (HandY); Schwab and England Activities of Daily living (S and E ADL) Scale; and Unified PDRating Scale (UPDRS).[5] Sleep was assessed using Epworth Sleepiness Scale (ESS),[7] Pittsburgh Sleep Quality Index (PSQI),[8] and NIMHANS comprehensive sleep disorder questionnaire (NCSDQ).[9]
Overnight PSG recording was performed in patients consenting for the study at baseline and after levodopa. They were subjected to overnight sleep study during which various parameters like electroencephalogram (EEG), electrooculography (EOG), electromyogram (EMG), electrocardiogram (ECG), oxygen saturations, respiratory effort, airflow, and body position were monitored. The participants underwent a full overnight PSG from 10 pm to 6 am. PSG included an electroencephalogram with channels, four channels were used to score sleep; an electromyogram on the chin and right anterior tibialis; an electrooculogram to record eye movements; an electrocardiogram; a nasal airflow sensor; chest and abdomen belts; a pulse oximeter; a snore microphone; and body sensors. Total sleep time (TST), sleep efficiency, sleep latency, sleep stages, arousals, snore indexes, and respiratory events were scored. The scoring of sleep was done according to the rules and technical specification set forward by American Academy of Sleep Medicine (AASM) Manual for the scoring of sleep and associated events.[10] Scoring of sleep stages was in 30 s sequential epochs commencing at the start of the study.[11]
Statistics: Statistical analysis was done using the Statistical Package for Social Sciences v. 16.0. The data were examined for frequencies, characteristics, and distribution. Normally distributed parametric data was expressed as mean ± standard deviation (SD). Correlations between variables in the drug naive and post treatment group were examined using the paired t-test and P-value £ 0.05 was considered significant.
Results
Fifteen patients with PD (male:female (M:F) = 11:4 and mean age: 59 ± 11.2 years) were evaluated. The mean duration of PD was11.8 ± 12.27 months (minimum: 3 months and maximum: 6 months). Details of demographic data, clinical phenotype, sleep assessment with sleep questionnaires, and PSG were analyzed. Their UPDRS motor score at baseline was 27.6 ± 11.5.
Comparison of phenotypic characteristics before and after treatment (n = 15) [Table 1].
Table 1.
Phenotypic characteristics of the cohort (n = 15)
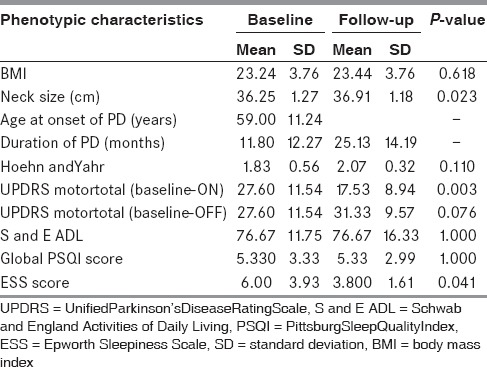
The drug naive patients recruited for the study responded to levodopa as indicated by the significant improvement in UPDRS motor scores in the ON compared to OFF state. The patients were not significantly fatigued at baseline or on follow-up (Fatigue Severity Scale (FSS) score of 1.59 before and 2.00 after treatment, P = 0.047). Nocturnal sleep quality as assessed by PSQI did not show a significant change. The mean ESS prior to start of medication was 6.00, which improved to 3.8 after treatment with levodopa (P-value = 0.04).
Comparison of PSG parameters characteristics before and after treatment (n = 15) [Table 2]: The sleep efficiency (P = 0.65); latency to onset of sleep (P = 0.19), especially latency to stage 1 (P = 0.12), time spent in stage 1 sleep (P = 0.55) had improved and time spent awake in bed (P = 0.24), slow wave sleep (P = 0.29), and rapid eye movement (REM; P = 0.24) had reduced after being on treatment.
Table 2.
Polysomnographic characteristics of the cohort (n = 15)
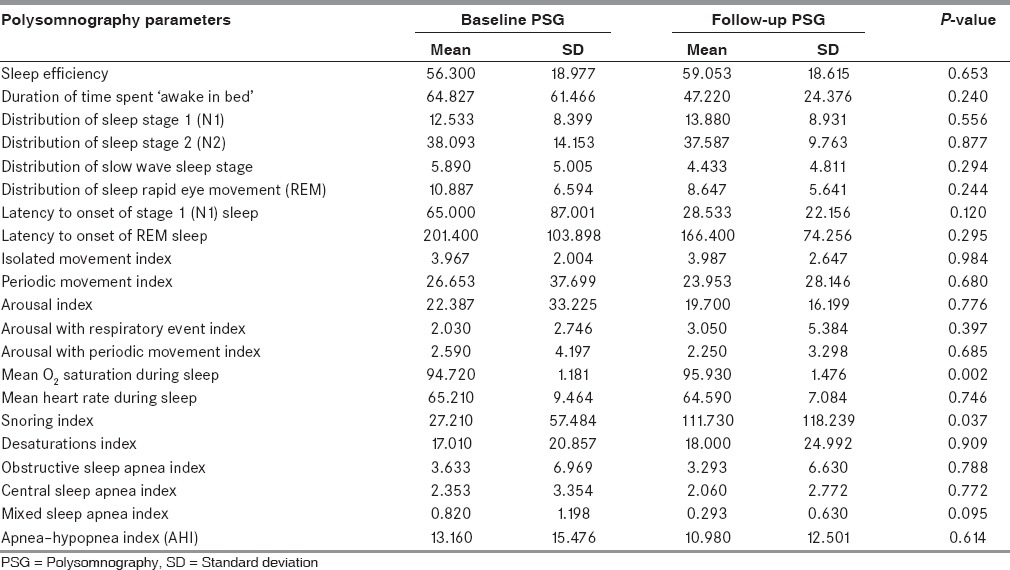
There was no statistically significant change in involuntary movements during sleep including isolated (P = 0.98) and periodic leg movement (PLM) indices (P = 0.68), arousal index (P = 0.77), arousal indices associated with periodic movement (P = 0.68), and respiratory events (P = 0.39).
The mean oxygen saturation during the entire sleep had improved with levodopa (P = 0.002). The snoring index in the drug naive patients (27.2 ± 57.5 snoring events/hour) worsened while on stable levodopa medication (111.7 ± 118.2 events/h; P = 0.037). These snore events had increased both during REM (P = 0.32) and nonrapid REM (NREM) sleep (P = 0.24). The desaturation index worsened marginally (P = 0.90). The apnea–hypopnea index (AHI) did not show significant variation with treatment, although absolute values showed marginal improvement.
Discussion
Patients with PD have disturbance of nocturnal sleep and daytime somnolence.[2,12,13,14] Sleep disturbances in PD were studied mostly in advanced PD patients and in them the cause was variably attributed to the severe disease and to dopaminergic treatment.[15,16,17] Initial studies attempting to study the individual contribution of either concluded that both disease and dopaminergic treatment was responsible without a clear distinction.[18] Hence, studies focused on sleep characteristics in early PD patients.[19] To understand the role of the disease independently in sleep disorders, patients without exposure to dopaminergic drugs or those with an adequate washout period were recruited in previous studies.[20,21] Sleep disorders were observed in patients with PD who had never received dopaminergic drugs and hence it was concluded that sleep disorder was due to the disease per se.[22] The question remained as to how dopaminergic therapy would affect sleep in these early PD patients, would the combined contribution of disease and therapy result in worsening of sleep. There was no change in the activities of daily living as indicated by lack of any change in the S and E ADL scores with treatment. Long-term follow-up might help to ascertain this.
Sleep questionnaires comparing the nocturnal sleep as assessed by PSQI and daytime somnolence as assessed by ESS in patients before and after medication observed that the subjective quality of sleep did not differ significantly, while the subjective evaluation of daytime somnolence improved with dopaminergic medications.[23,24] The reason for this might be due to the small sample size or short follow-up. The ESS scores in patients with advanced PD worsen with levodopa and dopamine agonists and the same has often been implicated as a cause for excessive daytime somnolence in PD.[25,26,27,28,29] Patients with restless leg syndrome on dopaminergic therapy have a lower risk of sudden onset of sleep during the day compared to those not treated.[30]
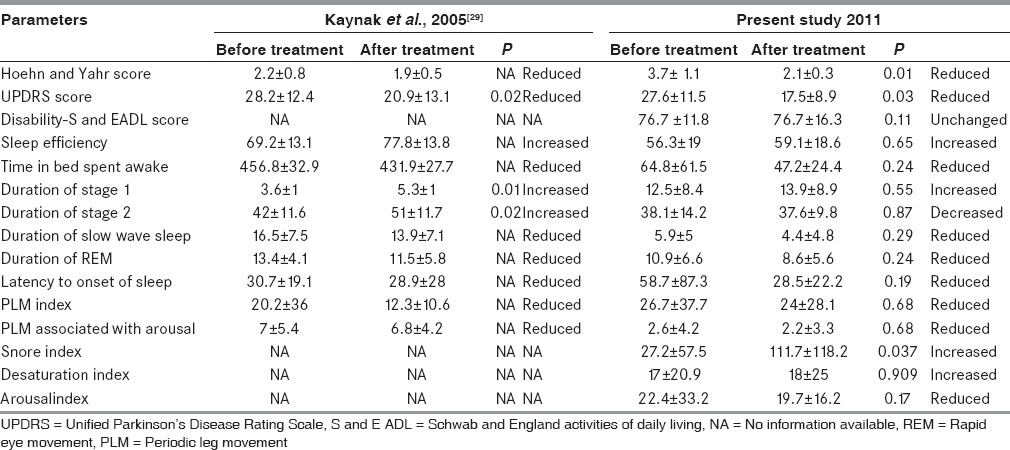
Sleep efficiency (P = 0.65); latency to onset of sleep (P = 0.19), especially latency to stage 1 (P = 0.12); and time spent in stage 1 sleep (P = 0.55) had improved and time spent awake in bed (P = 0.24); slow wave sleep (P = 0.29); and REM (P = 0.24) had reduced after being on treatment. The PSG parameters related to sleep macroarchitecture remained unchanged with treatment. This might be due to small sample size, relatively early PD, and short follow up. However, as observed in the only previous similar study, the improvement was not statistically significant.[31] Table 3 depicts the salient comparative features between the present study and the one reported by Kaynak et al., (2005).
Table 3.
Comparison of change in sleep parameters with dopaminergic drugs with the previous study
The PLM index showed a reduction after starting on medication (P= 0.68). PLM associated with arousal also reduced (P = 0.68).[32] The total arousal events expressed as index had shown a tendency to reduce (P = 0.17). The total arousal associated with periodic movements had also decreased against a marginal increase during REM sleep (P = 0.57).[33] Dopaminergic treatment also improves restless leg syndrome in patients without PD.[34,35] In this study with early drug naïve PD, REM sleep behavior disorder (RBD) was not a prominent observation and a short follow-up with levodopa might preclude this important feature.
Despite the significant improvement in mean oxygen saturation during the entire sleep (P = 0.002), snoring during sleep (snore index, P < 0.03) had increased significantly resulting in the number of desaturation events increasing marginally (P = 0.90).[36,37] The reason for this is difficult to explain.
Small sample size is a limitation and one needs to exercise caution before drawing any conclusions. Nevertheless, this longitudinal study is one of the few studies which had recruited levodopa naïve patients with a cohort that is very difficult to obtain and again carried out serial PSG study while on stable levodopa dosage. Detailed analysis of data was restricted to only those patients who exhibited sustained therapeutic response to levodopa, thereby excluding cases with atypical PD/“plus” syndromes. Follow-up observations on these patients also provided unique opportunity to evaluate effect of levodopa and disease progression on the sleep parameters as well.
Sleep in PD patients showed improvement in majority of the sleep parameters with levodopa, like many of the nonmotor symptoms. It may be emphasized that even in early stages of PD, sleep is affected. Similar studies involving larger cohort might support it, and there by assist in focused treatment and unravel questions regarding sleep and PD.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
References
- 1.Menza M, Dobkin RD, Marin H, Bienfait K. Sleep disturbances in Parkinson's disease. Mov Disord. 2010;1:S117–22. doi: 10.1002/mds.22788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Claassen DO, Kutscher SJ. Sleep disturbances in Parkinson's disease patients and management options. Nat Sci Sleep. 2011;3:125–33. doi: 10.2147/NSS.S18897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diederich NJ, Vaillant M, Leischen M, Mancuso G, Golinval S, Nati R, et al. Sleep apnea syndrome in Parkinson's disease. A case-control study in 49 patients. Mov Disord. 2005;20:1413–8. doi: 10.1002/mds.20624. [DOI] [PubMed] [Google Scholar]
- 4.Joy SP, Sinha S, Pal PK, Panda S, Philip M, Taly AB. Alterations in Polysomnographic (PSG) profile in drug-naïve Parkinson's disease. Ann Indian Acad Neurol. 2014;17:287–91. doi: 10.4103/0972-2327.138501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Litvan I, Bhatia KP, Burn DJ, Goetz CG, Lang AE, Mckeith I, et al. Movement Disorders Society Scientific Issues Committee Movement Disorders Society Scientific Issues Committee report. SIC Task Force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Mov Disord. 2003;18:467–86. doi: 10.1002/mds.10459. [DOI] [PubMed] [Google Scholar]
- 6.Hughes AJ, Daniel SE, Ben Shlomo Y, Lees AJ. The accuracy of diagnosis of Parkinsonian syndromes in a specialist movement disorder service. Brain. 2002;125:4–70. doi: 10.1093/brain/awf080. [DOI] [PubMed] [Google Scholar]
- 7.Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 8.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 9.Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraj D. Prevalence of sleep related disorders among healthy population in South India. Neurol India. 2012;60:68–74. doi: 10.4103/0028-3886.93601. [DOI] [PubMed] [Google Scholar]
- 10.Iber C, Ancoli-Israel S, Chesson A, editors. 1st ed. Westchester: American Academy of Sleep Medicine; 2007. Quan SF editors The AASM manual for the scoring of sleep and associated events: Rules, terminology, and technical specification. [Google Scholar]
- 11.Avidan AY. Recognition of Sleep Stages and Adult Scoring Technique. In: Bhatt M, Thomas RJ, editors. Chapter. Sudhansu Chokroverty. 1st edition. Atlas of Sleep Medicine; Elsevier Pub; 2007. pp. 95–121. [Google Scholar]
- 12.Tandberg E, Larsen JP, Karlsen K. A community-based study of sleep disorders in patients with Parkinson's disease. Mov Disord. 1998;13:895–9. doi: 10.1002/mds.870130606. [DOI] [PubMed] [Google Scholar]
- 13.Happe S, Klosch G, Lorenzo J, Kunz D, Penzel T, Roschke J, et al. Perception of sleep: Subjective versus objective sleep parameters in patients with Parkinson's disease in comparison with healthy elderly controls. Sleep perception in Parkinson's disease and controls. J Neurol. 2005;252:936–43. doi: 10.1007/s00415-005-0785-0. [DOI] [PubMed] [Google Scholar]
- 14.Zoccolella S, Savarese M, Lamberti P, Manni R, Pacchetti C, Logroscino G. Sleep disorders and the natural history of Parkinson's disease: The contribution of epidemiological studies. Sleep Med Rev. 2011;15:41–50. doi: 10.1016/j.smrv.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Factor SA, Mcalarney T, Sanchez-Ramos JR, Weiner WJ. Sleep disorders and sleep effect in Parkinson's disease. Mov Disord. 1990;5:280–5. doi: 10.1002/mds.870050404. [DOI] [PubMed] [Google Scholar]
- 16.Stocchi F, Barbato L, Nordera G, Berardelli A, Ruggieri S. Sleep disorders in Parkinson's disease. J Neurol. 1998;245:S15–8. doi: 10.1007/pl00007731. [DOI] [PubMed] [Google Scholar]
- 17.Kumar S, Bhatia M, Behari M. Sleep disorders in Parkinson's disease. Mov Disord. 2002;17:775–81. doi: 10.1002/mds.10167. [DOI] [PubMed] [Google Scholar]
- 18.Rye DB, Jankovic J. Emerging views of dopamine in modulating sleep/wake state from an unlikely source: PD. Neurology. 2002;58:341–6. doi: 10.1212/wnl.58.3.341. [DOI] [PubMed] [Google Scholar]
- 19.Young A, Home M, Churchward T, Freezer N, Holmes P, Ho M. Comparison of sleep disturbance in mild versus severe Parkinson's disease. Sleep. 2002;25:573–7. [PubMed] [Google Scholar]
- 20.Bergonzi P, Chiurulla C, Gambi D, Mennuni G, Pinto F. L-dopa plus dopa-decarboxylase inhibitor. Sleep organization in Parkinson's syndrome before and after treatment. Acta Neurol Belg. 1975;75:5–10. [PubMed] [Google Scholar]
- 21.Dhawan V, Dhoat S, Williams AJ, Dimarco A, Pal S, Forbes A, et al. The range and nature of sleep dysfunction in untreated Parkinson's disease (PD). A comparative controlled clinical study using the Parkinson's disease sleep scale and selective polysomnography. J Neurol Sci. 2006;248:158–62. doi: 10.1016/j.jns.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 22.Wetter TC, Collado-Seidel V, Pollmacher T, Yassouridis A, Trenkwalder C. Sleep and periodic leg movement patterns in drug-free patients with Parkinson's disease and multiple system atrophy. Sleep. 2000;23:361–7. [PubMed] [Google Scholar]
- 23.Fabbrini G, Barbanti P, Aurilia C, Vanacore N, Pauletti C, Meco G. Excessive daytime sleepiness in de novo and treated Parkinson's disease. Mov Disord. 2002;17:1026–30. doi: 10.1002/mds.10193. [DOI] [PubMed] [Google Scholar]
- 24.Pal PK, Thennarasu K, Fleming J, Schulzer M, Brown T, Calne SM. Nocturnal sleep disturbances and daytime dysfunction in patients with Parkinson's disease and in their caregivers. Parkinsonism Relat Disord. 2004;10:157–68. doi: 10.1016/j.parkreldis.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Kumar S, Bhatia M, Behari M. Excessive daytime sleepiness in Parkinson's disease as assessed by Epworth Sleepiness Scale (ESS) Sleep Med. 2003;4:339–42. doi: 10.1016/s1389-9457(03)00105-9. [DOI] [PubMed] [Google Scholar]
- 26.Hobson DE, Lang AE, Martin WR, Razmy A, Rivest J, Fleming J. Excessive daytime sleepiness and sudden-onset sleep in Parkinson disease: A survey by the Canadian Movement Disorders Group. JAMA. 2002;287:455–63. doi: 10.1001/jama.287.4.455. [DOI] [PubMed] [Google Scholar]
- 27.Paus S, Brecht HM, Koster J, Seeger G, Klockgether T, Wüllner U. Sleep attacks, daytime sleepiness, and dopamine agonists in Parkinson's disease. Mov Disord. 2003;18:659–67. doi: 10.1002/mds.10417. [DOI] [PubMed] [Google Scholar]
- 28.Roth T, Rye DB, Borchert LD, Bartlett C, Bliwise DL, Cantor C, et al. Assessment of sleepiness and unintended sleep in Parkinson's disease patients taking dopamine agonists. Sleep Med. 2003;4:275–80. doi: 10.1016/s1389-9457(03)00058-3. [DOI] [PubMed] [Google Scholar]
- 29.Verbaan D, van Rooden SM, Visser M, Marinus J, van Hilten JJ. Nighttime sleep problems and daytime sleepiness in Parkinson's disease. Mov Disord. 2008;23:35–41. doi: 10.1002/mds.21727. [DOI] [PubMed] [Google Scholar]
- 30.Möller JC, Körner Y, Cassel W, Meindorfner C, Krüger HP, Oertel WH, et al. Sudden onset of sleep and dopaminergic therapy in patients with restless legs syndrome. Sleep Med. 2006;7:333–9. doi: 10.1016/j.sleep.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Kaynak D, Kiziltan G, Kaynak H, Benbir G, Uysal O. Sleep and sleepiness in patients with Parkinson's disease before and after dopaminergic treatment. Eur J Neurol. 2005;12:199–207. doi: 10.1111/j.1468-1331.2004.00971.x. [DOI] [PubMed] [Google Scholar]
- 32.Lavault S, Bloch F, Houeto JL, Konofal E, Welter ML, Agid Y, et al. Periodic leg movements and REM sleep without atonia in Parkinson's disease with camptocormia. Mov Disord. 2009;24:2419–23. doi: 10.1002/mds.22854. [DOI] [PubMed] [Google Scholar]
- 33.Wetter TC, Brunner H, Hogl B, Yassouridis A, Trenkwalder C, Friess E. Increased alpha activity in REM sleep in de novo patients with Parkinson's disease. Mov Disord. 2001;16:928–33. doi: 10.1002/mds.1163. [DOI] [PubMed] [Google Scholar]
- 34.Ondo WG, Vuong KD, Jankovic J. Exploring the relationship between Parkinson disease and restless legs syndrome. Arch Neurol. 2002;59:421–4. doi: 10.1001/archneur.59.3.421. [DOI] [PubMed] [Google Scholar]
- 35.Nomura T, Inoue Y, Nakashima K. Clinical characteristics of Restless legs syndrome in patients with Parkinson's disease. J Neurol Sci. 2006;250:39–44. doi: 10.1016/j.jns.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 36.Maria B, Sophia S, Michalis M, Charalampos L, Andreas P, John ME, et al. Sleep breathing disorders in patients with idiopathic Parkinson's disease. Respir Med. 2003;97:1151–7. doi: 10.1016/s0954-6111(03)00188-4. [DOI] [PubMed] [Google Scholar]
- 37.Noradina AT, Karim NA, Hamidon BB, Norlinah I, Raymond AA. Sleep-disordered breathing in patients with Parkinson's disease. Singapore Med J. 2010;51:60–4. [PubMed] [Google Scholar]


