Abstract
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a recently described inflammatory disease of central nervous system with distinct clinical and radiological features. The etiopathogenesis of this rare entity remains to be understood. The histopathological findings closely resemble chronic inflammatory diseases like sarcoidosis and malignancies like lymphoma. With advancements in serology, immunopathology and radiology CLIPPERS is identified as a distinct entity that differs considerably in its clinical presentation, immunopathology, radiological findings and response to steroids. We describe a case that presented to us with progressive quadriparesis and lower cranial nerve deficits whose radiological and pathological findings were consistent with CLIPPERS. The patient had a good outcome with long term immunosuppression.
Keywords: Brainstem mass, CLIPPERS, pontine lesion
Introduction
There is a broad spectrum of pathologies that afflict the brainstem with varied clinical presentations. This along with a difficulty in obtaining tissue diagnosis makes it challenging to diagnose and manage these lesions. With the advancing radiological, histopathological and immunological techniques, newer entities affecting the brainstem are being constantly identified and described. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a recent addition to this spectrum of brainstem predominant lesions. The term was coined by Keegan et al in a case series consisting of 8 patients in which they described them as being characteristically symmetric and curvilinear lesions on a gadolinium-enhanced MRI, which appeared as “peppering of pons”.[1] We describe a case of a pontine lesion in a middle-aged lady suffering from a prolonged cutaneous disease. Her radiological and histopathological findings were consistent with those of CLIPPERS. She showed excellent clinical and radiological response to steroids and long-term immunosuppression.
Case Report
A 50-year-old housewife presented with progressive quadriparesis following a febrile illness. She noticed weakness involving her left upper and lower limb on day three following the febrile episode. The weakness progressed to involve the opposite side the next day. She also developed urinary incontinence, diplopia, facial weakness, slurred speech and difficulty in swallowing over the next few days. On examination, she was found to have bilateral 6th, 7th, 9th and 10th cranial nerve palsies, spastic quadriparesis and exaggerated tendon reflexes with up going plantars.
There was a history of long-standing nodular cutaneous lesions involving lower limbs and back. Biopsy of these lesions done in 2009 showed features of cutaneous T-cell lymphoma (Mycosis fungoides) for which she was treated with vincristine. The patient had no skin lesions at presentation and was not on any immunosuppression.
MRI scan of the brain showed a bulky pons with iso to mildly hypointense lesions on T1-weighted images, which were hyperintense on T2 and flair images. These lesions showed gadolinium contrast enhancement [Figure 1a–c] giving a typical peppering of pons appearance. CSF analysis showed protein 108 mg/dL and glucose 86 mg/dL, RBC-0, WBC-2, no bacteria on Gram stain, and AFB smear and fungal mount were negative. Culture showed no growth and no malignant cells on cytological examination. Work up for CNS vasculitis, which included anti-neutrophil cytoplasmic auto-antibodies (ANCA), anti-SSA/Ro, anti-SSB/La, dsDNA and anti–Sm, were negative. Infectious screening panel for HIV, Hepatitis A/B/C and tuberculosis were negative. Chest X-ray and serum ACE levels were normal.
Figure 1.
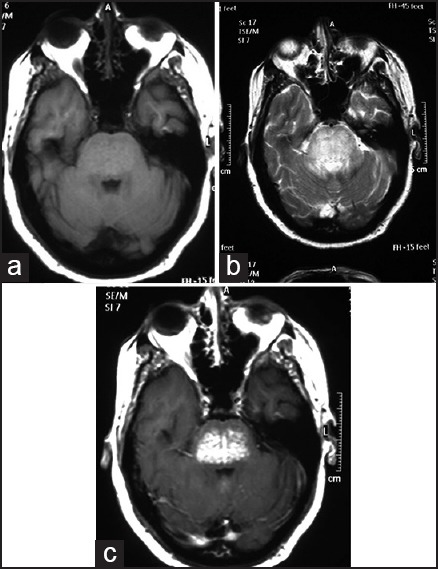
(a): Axial T1-weighted MRI showing a bulky pons with an isointense lesion (b) The lesion was hyperintense on T2-weighted MRI (c) Contrast MRI with gadolinium showed multiple punctuate enhancing lesions giving the classic “peppering of pons” appearance
A CT-guided stereotactic biopsy of the pontine lesion was done, which revealed a marked lymphocytic infiltrate in the white matter with perivascular predominance [Figure 2a]. The lymphocytic infiltrate was composed predominantly of T lymphocytes that were CD3 reactive [Figure 2b] and few CD20-positive B lymphocytes [Figure 2c]. A few CD68-positive histiocytes were also seen [Figure 2d]. Myelin was intact, there were no granulomas, and special stains for fungi and AFB were negative. These findings were consistent with CLIPPERS, and she was treated with methyl prednisolone 1 g once daily for a week followed by tapering dose of oral steroids over 1 month. Methotrexate 10 mg once a week was started and is being continued for the last 2 years. She gradually improved and at 6 months she was ambulant, her cranial nerve symptoms had improved and MRI imaging showed resolution of the brainstem lesion. At 1- and 2-year follow-up, the MRI lesions had completely resolved [Figure 3].
Figure 2.
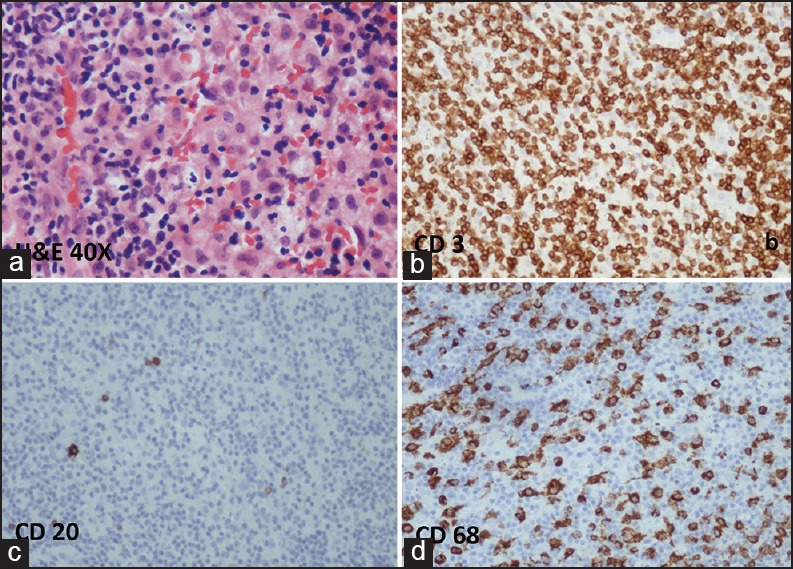
Histopathology (a) showing a marked lymphocytic infiltrate in the white matter with perivascular predominance (hematoxylin and eosin 40×). Immunohistochemistry showing the lymphocytic infiltrate was composed predominantly of T lymphocytes that were CD3 reactive (b) and few CD20-positive B lymphocytes (c). A few CD68-positive histiocytes were also seen (d)
Figure 3.

Follow-up axial contrast MRI at 2 years showing complete resolution of the lesion
Discussion
CLIPPERS is an inflammatory disorder of the brainstem, which is very responsive to steroids with excellent prognosis.[1] There have been an increasing number of case reports in recent medical literature of this newly defined entity helping us to better define the clinical and radiological features, management strategies and prognosis.[2,3,4] The clinical presentation in CLIPPERS is variable but generally is that of insidious onset and progressive brainstem, spinal and cerebellar signs. Ataxia and diplopia are the predominant signs. Additionally the patients may present with spastic quadri or paraparesis, dysarthria, cognitive deficits, psychomotor slowing and altered sensation of face and scalp.[1,3,4] The basic hematological evaluation and cerebrospinal fluid analysis are unremarkable except for elevated protein, which was noticed in almost all of the previously reported cases.[1,2,3,4] Serological inflammatory markers are negative and analysis for malignant cells is negative.
Contrast-enhanced MRI of the brain shows punctuate gadolinium enhancement (“salt-and-pepper-like appearance”) centered on the brachium pontis with extension of the lesions into the white matter of the cerebellar hemispheres variably.[5] There is corresponding non-specific decreased T1 signal and increasedT2 signal in the regions of gadolinium enhancement. These findings are considered characteristic of CLIPPERS and variable extension of this contrast enhancement involving the brainstem, cervical spinal cord, basal ganglia and cerebral deep white matter have also been described.[1] Clinical and radiological differentials that are considered include pontine tumor (lymphoma/glioma), acute demyelination, nocardiosis, neurosarcoidosis, lymphomatoid granulomatosis, CNS vasculitis and Bickerstaff brainstem encephalitis.[1,4] These disorders are excluded based on the absence of associated systemic symptoms and laboratory evidence. The differentiating features of these CNS disorders and CLIPPERS were well-described by Pittock et al.[1] The clinical and radiological features of CLIPPERS are very distinctive and disappearance of the typical lesions on MRI following steroid therapy may be considered diagnostic. However, a glial tumor can occasionally be missed as reported by Jones et al[6] and therefore a biopsy is needed for definitive diagnosis. CNS spread of the cutaneous T-cell lymphoma was also a possibility though isolated CNS spread is extremely rare.[7]
The pathogenesis of CLIPPERS has so far has been an enigma. Is CLIPPERS a disease entity or just an immunological response to a disease elsewhere has to be determined. In most of the previous reported cases, an extensive immunological workup has been done but no consistent abnormality was detected.[4] The presence of prolonged immune-mediated cutaneous disease in our patient might have had a bearing on the pathogenesis of CLIPPERS. The presence of a perivascular and parenchymal inflammatory cell infiltrate, combined with the clinical response to immunosuppressive therapies suggests an immune-mediated pathogenesis. The target auto-antigen is likely to be located in perivascular regions and has yet to be identified.
Though it is well-established that these lesions respond to steroid therapy, the dose and duration of treatment is not standardized. The indications for additional immunosuppressive therapy have also to be identified. In a small series of CLIPPERS, some authors have used steroids with or without additional immunosuppression upfront while others have reserved additional immunosuppresion for relapses.[1,2,8] Wijntjes et al reviewed the treatment of CLIPPERS and suggested that imunosuppressive therapy should be continued for at least 2 to 5 years and tapering should be considered thereafter.[9]
Conclusion
CLIPPERS is an immune-mediated inflammatory disorder of the brainstem, which is increasingly being reported. It has characteristic radiological and histological features with good outcome following long-term immunosuppression like in our patient.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
References
- 1.Pittock SJ, Debruyne J, Krecke KN, Giannini C, van den Ameele J, De Herdt V, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) Brain. 2010;133:2626–34. doi: 10.1093/brain/awq164. [DOI] [PubMed] [Google Scholar]
- 2.Kastrup O, van de Nes J, Gasser T, Keyvani K. Three cases of CLIPPERS: A serial clinical, laboratory and MRI follow-up study. J Neurol. 2011;258:2140–6. doi: 10.1007/s00415-011-6071-4. [DOI] [PubMed] [Google Scholar]
- 3.Taieb G, Wacongne A, Renard D, Figarella-Branger D, Castelnovo G, Labauge P. A new case of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids with initial normal magnetic resonance imaging. Brain. 2011;134:e182. doi: 10.1093/brain/awq390. [DOI] [PubMed] [Google Scholar]
- 4.Jerca O, Manouchehrinia A, Tanasescu R. A new defined entity among the spectrum of central nervous system inflammation: Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) Rom J Neurol. 2011;10:77–81. [Google Scholar]
- 5.Simon NG, Parratt JD, Barnett MH, Buckland ME, Gupta R, Hayes MW, et al. Expanding the clinical, radiological and neuropathological phenotype of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) J Neurol Neurosurg Psychiatry. 2012;83:15–22. doi: 10.1136/jnnp-2011-301054. [DOI] [PubMed] [Google Scholar]
- 6.Jones JL, Dean AF, Antoun N, Scoffing DJ, Burnet NG, Coles AJ. Radiologically compatible CLIPPERS may conceal a number of pathologies. Brain. 2011;134:e187. doi: 10.1093/brain/awr134. [DOI] [PubMed] [Google Scholar]
- 7.del Carpio-O’Donovan R, Freeman C. Brainstem involvement with mycosis fungoides: An unusual central nervous system complication. AJNR Am J Neuroradiol. 2002;23:533–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Taieb G, Duflos C, Renard D, Audoin B, Kaphan E, Pelletier J, et al. Long-term outcomes of CLIPPERS (Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids) in a consecutive series of 12 patients. Arch Neurol. 2012;69:847–55. doi: 10.1001/archneurol.2012.122. [DOI] [PubMed] [Google Scholar]
- 9.Wijntjes J, Wouda EJ, Siegert CE, Karas GB, Vlaar AM. Need for prolonged immunosuppressive therapy in CLIPPERS — a case report. BMC Neurol. 2013;13:49. doi: 10.1186/1471-2377-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]


