Sir,
Dengue, a flavivirus disease, has varied presentations, right from an asymptomatic state to a hemorrhagic disorder with multiorgan failure. Dengue virus has not been classically thought to be neurotropic; however, there is increasing evidence that it may be so.[1] An unusual case of dengue infection that presented with encephalitis is described here. The remarkable imaging feature in this case was bilaterally symmetrical involvement of parietooccipital lobes on magnetic resonance imaging (MRI).
A 27-year-old male presented with severe occipital headache, blurring of vision, and one episode of vomiting since 1 day. There was no history of antecedent fever, seizure, rash, or bleeding episodes. There was no history of drug abuse or alcoholism. On examination, the patient was febrile with a temperature of 101°F, pulse rate of 80 per min, and blood pressure of 110/80 mmHg. He was conscious and oriented. There was noneck stiffness. Plantar extensor response was elicited. Visual acuity was reduced to finger counting at 1 m in both eyes. The MRI of brain revealed symmetrical gyral hyperintensity in bilateral parietooccipital regions on T2-weighted (T2W) and fluid-attenuated inversion recovery (FLAIR) sequences [Figure 1a–c]. No evidence of restriction was seen on diffusion-weighted images [Figure 1d]. No evidence of abnormal enhancement was seen on intravenous gadolinium-enhanced MRI. Hemogram revealed a low white blood cell count of 2,500/mm3 and a platelet count of 150,000/mm3. Serological marker for Japanese B encephalitis was not detected. The dengue virus antigen NS1 was positively detected on serology. Subsequently, rising titers of IgM antibody against dengue virus were seen in two samples by immunoglobulin (Ig) M-antibody capture enzyme-linked immunosorbent assay (MAC-ELISA). Cerebrospinal fluid (CSF) examination revealed normal opening pressure, lymphocytic pleocytosis (85% lymphocytes), glucose of 73 mg/dL, and total protein of 102 mg/dL. IgM antibody against dengue virus was also detected in CSF by MAC-ELISA. Culture of blood and CSF samples was negative for bacterial and fungal growth. Rest of the laboratory parameters were within normal limits. A diagnosis of dengue encephalitis was made. The patient was treated with intravenous fluids and paracetamol was used as antipyretic. Platelet count was regularly monitored as it dropped to its lowest value of 46,000/mm3 on day 5 of admission, and then subsequently recovered. He was afebrile after the 4th day and was discharged on day 8, at which time he had completely recovered. Follow-up after a month did not reveal any abnormality.
Figure 1.
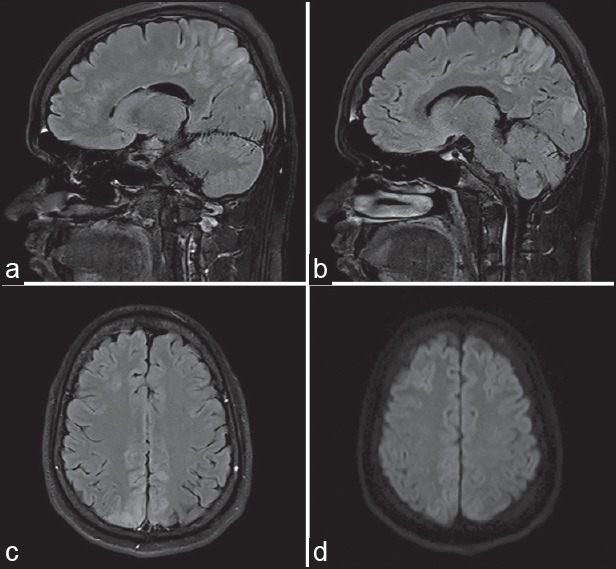
MRI reveals symmetrical hyperintensity in bilateral parietooccipital regions on (a and b) sagittal and (c) axial fluid-attenuated inversion recovery (FLAIR) sequence. MRI = Magnetic resonance imaging, FLAIR = fluid attenuated inversion recovery (d) No evidence of restriction is seen on diffusion-weighted MRI
Dengue infection presenting first as encephalitis is rare. Research suggests that direct invasion of the nervous system by dengue virus is possible.[1] The other possible mechanism is infiltration of virus-infected macrophages into the brain.[1,2] The clinical symptomatology which includes altered level of consciousness, seizures, headache, meningeal signs, and pyramidal tract signs are nonspecific. Laboratory diagnosis of dengue encephalitis is based upon detection of either the virus itself or viral antigen NS1, or the dengue-specific IgM antibody, in the CSF. Viral cultures are generally difficult, and hence, serology is commonly used for laboratory diagnosis. MRI reveals the focal involvement of brain parenchyma, thus suggesting encephalitis rather than encephalopathy as the underlying etiology. In addition, MRI can be useful in differentiating between viral infections of central nervous system, as some viral encephalitides display a tropism for certain brain structures resulting in characteristic imaging features.[3] There are no characteristic MRI features of dengue encephalitis. Some studies describe involvement of globus pallidus, temporal lobes, thalamus, hippocampus, pons, and spinal cord on MRI.[4,5,6] The symmetrical hyperintense signal in bilateral parietooccipital regions on FLAIR and T2W sequences as seen in our patient has not been described earlier. Bilateral symmetrical parietooccipital involvement on MRI is typically seen in posterior reversible encephalopathy syndrome (PRES), which is a clinicoradiologic entity occurring as a result of failure of the posterior circulation to autoregulate in response to acute changes in blood pressure. The clinical manifestations of PRES overlap with that of encephalitis. However, its usual association with acute hypertension, and the frequent involvement of cortical as well as subcortical regionon MRI are the differentiating features of PRES. The complete clinical recovery in our patient is consistent with good prognosis for most cases of dengue encephalitis as described in literature.[2]
References
- 1.Domingues RB, Kuster GW, Onkuni-Castro FL, Souza VA, Levi JE, Pannuti CS. Involvement of the central nervous system in patients with dengue virus infection. J Neurol Sci. 2008;267:36–40. doi: 10.1016/j.jns.2007.09.040. [DOI] [PubMed] [Google Scholar]
- 2.Varatharaj A. Encephalitis in the clinical spectrum of dengue infection. Neurol India. 2010;58:585–91. doi: 10.4103/0028-3886.68655. [DOI] [PubMed] [Google Scholar]
- 3.Kumar S, Misra UK, Kalita J, Salwani V, Gupta RK, Gujral R. MRI in Japanese encephalitis. Neuroradiology. 1997;39:180–4. doi: 10.1007/s002340050388. [DOI] [PubMed] [Google Scholar]
- 4.Wasay M, Channa R, Jumani M, Shabbir G, Azeemuddin M, Zafar A. Encephalitis and myelitis associated with dengue viral infection clinical and neuroimaging features. Clin Neurol Neurosurg. 2008;110:635–40. doi: 10.1016/j.clineuro.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Kamble R, Peruvamba JN, Kovoor J, Ravishankar S, Kolar BS. Bilateral thalamic involvement in dengue infection. Neurol India. 2007;55:418–9. doi: 10.4103/0028-3886.37103. [DOI] [PubMed] [Google Scholar]
- 6.Yeo PS, Pinheiro L, Tong P, Lim PL, Sitoh YY. Hippocampal involvement in dengue fever. Singapore Med J. 2005;46:647–50. [PubMed] [Google Scholar]


