Sir,
Sleep plays a vital role in maintaining the equilibrium of human psychosocial behavior. Sleep-wake cycle is one of the biological rhythms which are determined by a circadian timing system, predisposed by some factors like physiological function, work schedules, etc. Sleep deprivation results in psychosocial stress, psychiatric disorders, decreased work effectiveness, and learning disability. Nursing is a demanding profession with occupational stress which involves academics, shift duties, and sleep deprivation.[1,2,3,4] The purpose of the present study was to identify the sleep pattern, quality of sleep, sleep disturbances, day time sleepiness and its influence on academics, and routine activities of daily life in nursing students.
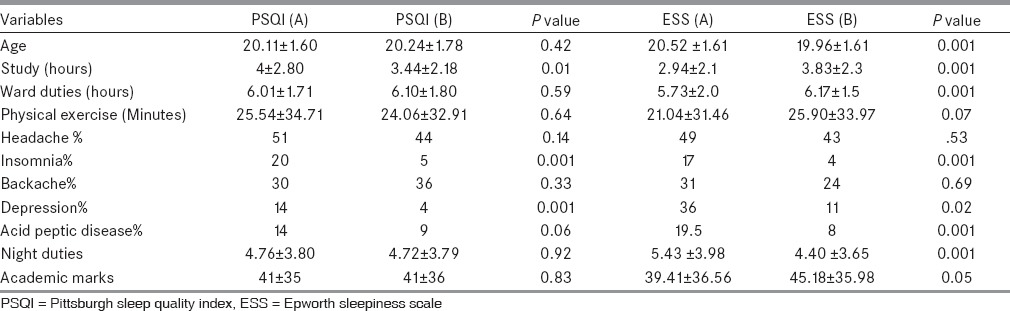
We did a cross-sectional study in two nursing colleges from September 2012 to September 2013. Seven hundred and fifty students were included. A self-administered questionnaire of demographic characteristics, academic performance, night duties, and health complaints was taken. Along with this, Epworth sleepiness scale (ESS)[5] which scores the daytime sleepiness and Pittsburgh sleep quality index (PSQI),[6] which scores sleep quality was also done. The students were divided into two groups according to the PSQI and ESS scores. Students with PSQI more than or equal to 5 as PSQI (A) poor sleepers and less than 5 as PSQI (B) as good sleepers. ESS scores of more than 10 as ESS (A) as excessive day time sleepiness and ESS (B) as normal sleepers. The data was analyzed with the statistical package for social sciences (SPSS) for Windows, version 20 and paired t-test was done between PSQI (A) and PSQI (B) and ESS (A) and ESS (B).
Seven hundred and thirteen students completed the questionnaire. Three hundred and twenty-four (45%) students reported headache, 281 (39%) students tiredness, 193 (27%) back pain, 72 (10%) symptoms of acid peptic disease, 61 (9%) insomnia, 47 (7%) depression. Five hundred and forty-eight (77%) had night duties at least 1 week in a month. Comparison between PSQI (A) and PSQI (B); ESS (A) and ESS (B) are shown in Table 1. Students with better sleep quality had less insomnia and depression and able to study for more hours. Students with excessive daytime sleepiness were older, had more insomnia, depression, acid peptic disease, and were doing more night duties and less ward duties. Our study found that students with poor sleep quality were able to dedicate fewer hours to study and eventually had poor marks and were more depressed than their peers. Earlier studies have also shown similar results.[7] Sleep disruptions probably acts on the cognitive control leading to depressive symptoms.[8] Studies have shown that adolescents with poor sleep quality had poor academic grades because of depression.[7] In this study, result show that PSQI (A) positively correlates to ESS (A). Students with ESS (A) had more night duties and poor academic marks. Poor sleep quality causes excessive daytime sleepiness and thus sleep-debt. Poor sleep is one of the most prevalent complaints of patients with chronic pain conditions results in headache and fatigue. A recent large population-based study concluded that insomnia leads to several mental and physical problems which included depression, headache, rheumatologic ailments to more graver cardiac and neurological disorders.[9] Shift work also affects the work performance and safety.[10] Sleep deprivation adversely effects on the performance of hospital staff nurses. Several studies have shown that failure to obtain adequate sleep is an important contributor to medical error.[10,11] A study showed that residents averaging 5 or fewer hours of sleep per night were more likely to report having made significant medical errors.[10] Our study however did not address the consequence of sleep deprivation on the medical error.
Table 1.
Comparison between PSQI (A) and PSQI (B); ESS (A) and ESS (B)
The study concludes that a significant proportion of nursing students suffer from sleep abnormalities. Advice should be included in both undergraduate programs and continuing education to help nurses to recognize and improve their own sleep quality and life quality managers should create a supportive environment to encourage shift-working nurses to engage in healthy behaviors. They could be advised to get extra sleep before working the first night shift, take a 2-hour afternoon sleep before coming on duty, increasing weekend sleep which will help to keep the sleep debt to a minimum. Scheduled napping for shift workers may be useful in relieving excessive sleepiness during work shifts. It also highlights the need to have cognitive behavioral training for sleep-related complaints in nursing students and to probably assign shift duties to students after survey of their sleep chronotype.
References
- 1.McGrath A, Reid N, Boore J. Occupational stress in nursing. Int J Nurs Stud. 2003;40:555–65. doi: 10.1016/s0020-7489(03)00058-0. [DOI] [PubMed] [Google Scholar]
- 2.Hughes RG, Rogers AE. Are you tired? Am J Nurs. 2004;104:36–8. doi: 10.1097/00000446-200403000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Johnson CJ, Croghan E, Crawford J. The problem and management of sickness absence in the NHS: Considerations for nurse managers. J Nurs Manag. 2003;11:336–42. doi: 10.1046/j.1365-2834.2003.00404.x. [DOI] [PubMed] [Google Scholar]
- 4.McVicar A. Workplace stress in nursing: A literature review. J Adv Nurs. 2003;44:633–42. doi: 10.1046/j.0309-2402.2003.02853.x. [DOI] [PubMed] [Google Scholar]
- 5.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 6.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 7.Short MA, Gradisar M, Lack LC, Wright HR. The impact of sleep on adolescent depressed mood, alertness and academic performance. J Adolesc. 2013;36:1025–33. doi: 10.1016/j.adolescence.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Vanderlind WM, Beevers CG, Sherman SM, Trujillo LT, McGeary JE, Matthews MD, et al. Sleep and sadness: Exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Med. 2014;15:144–9. doi: 10.1016/j.sleep.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sivertsen B, Lallukka T, Salo P, Pallesen S, Hysing M, Krokstad S, et al. Insomnia as a risk factor for ill health: Results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014;23:124–32. doi: 10.1111/jsr.12102. [DOI] [PubMed] [Google Scholar]
- 10.Baldwin DC, Jr, Daugherty SR. Sleep deprivation and fatigue in residency training: Results of a national survey of first- and second-year residents. Sleep. 2004;27:217–23. doi: 10.1093/sleep/27.2.217. [DOI] [PubMed] [Google Scholar]
- 11.Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]


