Abstract
Augmentation rhinoplasty can be carried out using a wide range of materials including autologous bone and/or cartilage as well as alloplasts. Use of biologic bone and cartilage grafts results in lower infection rates, but they are associated with long-term resorption and donor-site morbidity. Alloplastic materials, in particular silicone, have been associated in literature with extrusion, necrosis of the tip, mobility and deviation or displacement of the implant, immobile nasal tip and infection. However, they have the advantages of being readily available and easy to reshape with no requirement for harvesting autografts.
Aim:
To overcome these problems associated with silicone implants for which the authors have devised a novel technique, the “rideon technique”.
Materials and Methods:
The present study was carried out on 11 patients over a period of 4 years. The authors have devised a simple technique to fix the silicone implant and retain it in place. Restricting the implant to only dorsum avoided common complications related to the silicone implant.
Results:
The authors have used this technique in 11 patients with encouraging results. Follow-up ranged from 12 months to 36 months during which patients were assessed for implant mobility, implant extrusion and tip necrosis. There was no incidence of above mentioned complications in these patients.
Conclusion:
The “rideon technique” provides excellent stability to silicone implants and restricting the implant only to dorsum not only eliminates chances of tip necrosis and thus implant extrusion but also maintains natural shape, feel and mobility of the tip.
KEY WORDS: Alloplasts, autografts, rhinoplasty, silicone implants
INTRODUCTION
Rhinoplasty is a commonly sought aesthetic surgery. The surgical goal of a rhinoplasty is to provide a stable nasal skeleton with optimal function and a pleasing shape which is in harmony with the rest of the face.[1] To get good results in rhinoplasty, artistic restructuring of individual components is needed which often includes relocation and augmentation.[2] Augmentation can be achieved by a variety of biologic materials which include cartilage,[3] bone,[4,5,6] or fascia.[7] Biologic materials are more resistant to infection but they have the disadvantages of resorption, donor-site morbidity and difficulty in carving.[6] Alloplastic materials include silicone,[8,9,10] supramid,[11] proplast,[12] vicryl,[13] mersilene,[14] medpore,[15] polytetrafluoroethylene[16,17] and ivory.[18] They have the advantage of being readily available, easy to carve and shape with no donor-site morbidity; however, they are associated with a higher rate of infection. Silicone is further criticised for associated translucency, extrusion, displacement, immobility and necrosis of the nasal tip.[11] Despite this it continues to be the most widely used augmentation material in Asia.[19,20,21,22,23,24] In order to overcome these problems associated with silicone implants the authors have proposed a simple and logical ‘ride-on technique’ and restricting its use to the dorsum.
MATERIALS AND METHODS
Our study is based on the use of silicone implant in 11 patients over a period of 4 years. The authors have devised a simple technique to fix the silicone implant and retain it in place.
Surgical technique
Implant should be used to augment only the nasal dorsum and should not extend beyond. It should be cut short of the tip to keep the nasal tip free of the implant. The vertical limb of the L-shaped implant can be cut or folded upon the undersurface to increase the height if required [Figure 1]. We emphasise that tip plasty should be done using a suturing technique or if needed by adding septal/conchal cartilage. This technique maintains natural mobility of the tip in contrast with stiff tip reconstructed with an implant. It also reduces the chances of implant extrusion.
Figure 1.

Vertical limb of silicone implant folded and sutured with knots lying on the undersurface
We have used autograft such as a piece of cartilage [Figure 2] or the perichondrium [Figure 3] which is sutured onto the under surface of the implant with non-absorbable sutures. The authors have described this method as ‘ride-on technique’ as the silicone implant rides on the autograft. Autografts used are septal cartilage or conchal cartilage along with perichondrium. Alternatively fascia or dermis fat graft can also be used. If costal cartilage is being harvested for structural support its perichondrium can be used. While suturing the autografts, knots should be kept down to maintain smooth contour of dorsum [Figure 1]. Nasal dorsum must be roughened with the help of nasal rasp or file for better adhesions. After suturing the autograft with implant, it is then positioned as desired. Fixation sutures with cartilaginous dorsum are required only in open rhinoplasty to stabilise it. Rest of the rhinoplasty is performed as planned. The autograft acts as a biological scaffold and helps to form adhesions with the underlying tissue which stabilizes the implant.
Figure 2.

Pieces of cartilage sutured to the undersurface of silicone implant
Figure 3.

Perichondrium sutured to the undersurface of implant
Nasal plaster of paris splint is applied at the end of the procedure and kept in place for 2 weeks. After 2 weeks, splint is removed, and the patient is asked not to massage or use spectacles at least 6 weeks post-operatively.
RESULTS
The authors have used this technique in 11 patients with encouraging results. Some of our results are shown in Figures 4–19. The stability of the fixation was assessed by measuring the deviation from the midline. Midline of the nose was marked and implant was moved by applying pressure with thumb and index finger. Deviation from midline was thus measured both superiorly and inferiorly. There was no incidence of implant extrusion or tip necrosis. Also, natural mobility of the tip was maintained. Follow-up ranges from 12 months to 36 months. This is a simple and easily reproducible technique to fix the silicone implant. Larger studies and multi-centre experience is needed to establish this as a method for fixation of implants in rhinoplasty but the initial results are encouraging.
Figure 4.

Case 1 — Pre-operative frontal view
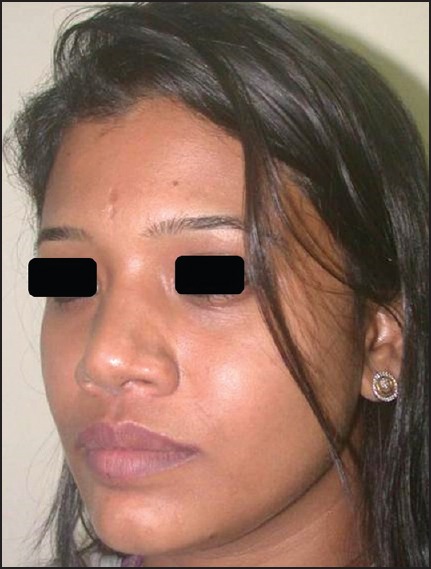
Figure 19.

Case 4 — Post-operative oblique view
Figure 5.

Case 1 — Post-operative frontal view
Figure 6.
Case 1 — Pre-operative oblique view
Figure 7.

Case 1 — Post-operative oblique view
Figure 8.

Case 2 — Pre-operative frontal view
Figure 9.

Case 2 — Post-operative frontal view
Figure 10.

Case 2 — Pre-operative oblique view
Figure 11.

Case 2 — Post-operative oblique view
Figure 12.

Case 3 — Pre-operative frontal view
Figure 13.

Case 3 — Post-operative frontal view
Figure 14.

Case 3 — Pre-operative lateral view
Figure 15.

Case 3 — Post-operative lateral view
Figure 16.

Case 4 — Pre-operative frontal view
Figure 17.

Case 4 — Post-operative frontal view
Figure 18.

Case 4 — Pre-operative oblique view
DISCUSSION
A variety of alloplastic materials have been described for use in rhinoplasty. Although we prefer costo-chondral grafts for augmentation rhionoplasty, we often come across patients who refuse use of costo-chondral grafts. In those patients, silicone implant is used for dorsal augmentation. Normally in rhinoplasty, silicone implants are inserted into the subcutaneous tissue on the dorsum of the nose. This has resulted in certain complications such as persistent mobility of the implant, implant extrusion and stiffness of nasal tip.
We have tried to modify the technique of augmentation rhinoplasty with silicone implants to counter these complications each of which is discussed separately.
Mobility of implant
When the silicone implant is pinched over the nasal bridge, it moves right or left. If the implant moves greatly, then the corrected nose is pleomorphic.[25] This is because silicone implants continue to be slightly mobile in the space between the capsule and the implant. This mobility tends to persist over years and is primarily because of the fact that no natural adhesions are formed between the implant and the underlying native tissue owing to the presence of the capsule. Various methods like sutures, screw fixation and rasping of the dorsum have been described to fix the alloplastic material in the dorsum. Fascial grafts especially from the temporal region have been used alone or in combination with cartilage graft.[3] These biomaterials have significantly lower rate of complications and are stable in their position. Sutures or screws are used to fix the implants in their position and yet some mobility of the implant is almost always seen due to soft nature of implant and it may become palpable. Slight modification using “ride-on technique” greatly reduces implant mobility due presence of biological scaffold causing better adhesions to dorsum.
Silicone implant extrusion
it is one of the most serious complications of augmentation rhinoplasty. Extrusion occurs either through the skin or mucosa. It results either due to tension and necrosis of skin/mucosa. Tip and nasal mucosal necrosis is the rule rather than exception over a period of time when L-shaped implant is used. In our technique of using autograft over implant, we have not encountered implant extrusion in any of our cases.
Stiffness of nasal tip
Nasal tip loses its natural mobility if the implant extends till the tip.
Tip is most vulnerable to trauma and commonly handled and moved sideways during wiping, sneezing, etc. This makes complete implant mobile if it is present under tip and collumella.
These problems are addressed by keeping the nasal tip free of alloplastic material and reconstructing the tip by suturing technique or if needed with cartilage grafts.
CONCLUSION
The authors are of the opinion that implants are not meant to be kept under the nasal tip. We must mould the tip to the desired shape by suturing technique or if needed with the help of cartilage grafts. The “ride-on technique” provides excellent stability to silicone implants and restricting the implant only to dorsum not only eliminates chances of tip necrosis and thus implant extrusion but also maintains natural shape, feel and mobility of the tip. Elimination of all these complications may provide us a near ideal implant.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vuyk HD, Adamson PA. Biomaterials in rhinoplasty. Clin Otolaryngol Allied Sci. 1998;23:209–17. doi: 10.1046/j.1365-2273.1998.00133.x. [DOI] [PubMed] [Google Scholar]
- 2.Tardy ME, Schwartz MS. The evolution of rhinoplasty outcome: Long term results. In: Daniel RK, editor. Rhinoplasty. Boston: Eittle, Brown & Co; 1993. pp. 778–814. [Google Scholar]
- 3.Gunter JP, Rohrich RJ. Augmentation rhinoplasty: Dorsal onlay grafting using shaped autogenous septal cartilage. Plast Reconstr Surg. 1990;86:39–45. [PubMed] [Google Scholar]
- 4.Krause CJ. Augmentation rhinoplasty. Otolaryngol Clin North Am. 1975;8:743–52. [PubMed] [Google Scholar]
- 5.Wheeler ES, Kawamoto HK, Zarem HA. Bone grafts for nasal reconstruction. Plast Reconstr Surg. 1982;69:9–18. [PubMed] [Google Scholar]
- 6.Romo T, rd, Jablonski RD. Nasal reconstruction using split calvarial grafts. Otolaryngol Head Neck Surg. 1992;107:622–30. doi: 10.1177/019459989210700503. [DOI] [PubMed] [Google Scholar]
- 7.Leaf N. SMAS autografts for the nasal dorsum. Plast Reconstr Surg. 1996;97:1249–52. doi: 10.1097/00006534-199605000-00025. [DOI] [PubMed] [Google Scholar]
- 8.Regnault P. Nasal augmentation in the problem nose. Aesthetic Plast Surg. 1987;11:1–5. doi: 10.1007/BF01575475. [DOI] [PubMed] [Google Scholar]
- 9.Khoo BC. Augmentation rhinoplasty in the orientals. Plast Reconstr Surg. 1964;34:81–8. [PubMed] [Google Scholar]
- 10.Beekhuis GJ. Silastic alar-columellar prosthesis in conjunction with rhinoplasty. Arch Otolaryngol. 1982;108:429–32. doi: 10.1001/archotol.1982.00790550033008. [DOI] [PubMed] [Google Scholar]
- 11.Adams JS. Grafts and implants in nasal and chin augmentation. A rational approach to material selection. Otolaryngol Clin North Am. 1987;20:913–30. [PubMed] [Google Scholar]
- 12.Gilmore J. Use of Vicryl mesh in prevention of postrhinoplasty dorsal irregularities. Ann Plast Surg. 1989;22:105–7. doi: 10.1097/00000637-198902000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Juraha LZ. Experience with alternative material for nasal augmentation. Aesthetic Plast Surg. 1992;16:133–40. doi: 10.1007/BF00450605. [DOI] [PubMed] [Google Scholar]
- 14.Fanous N. Mersilene tip implants in rhinoplasty: A review of 98 cases. Plast Reconstr Surg. 1991;87:662–71. [PubMed] [Google Scholar]
- 15.Wellisz T. Clinical experience with the Medpor porous polyethylene implant. Aesthetic Plast Surg. 1993;17:339–44. doi: 10.1007/BF00437109. [DOI] [PubMed] [Google Scholar]
- 16.Godin MS, Waldman SR, Johnson CM., Jr The use of expanded polytetrafluoroethylene (Gore-Tex) in rhinoplasty. A 6-year experience. Arch Otolaryngol Head Neck Surg. 1995;121:1131–6. doi: 10.1001/archotol.1995.01890100043007. [DOI] [PubMed] [Google Scholar]
- 17.Queen TA, Palmer FR., 3rd Gore-Tex for nasal augmentation: a recent series and a review of the literature. Ann Otol Rhinol Laryngol. 1995;104:850–2. doi: 10.1177/000348949510401104. [DOI] [PubMed] [Google Scholar]
- 18.Vilar-Sancho B. An old story: An ivory nasal implant. Aesthetic Plast Surg. 1987;11:157–61. doi: 10.1007/BF01575503. [DOI] [PubMed] [Google Scholar]
- 19.Hiraga Y. Complications of augmentation rhinoplasty in the Japanese. Ann Plast Surg. 1980;4:495–9. doi: 10.1097/00000637-198006000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Wang JW. A new pattern of silastic prosthesis for augmentation rhinoplasty. Zhonghua Zheng Xing Shao Shang Wai Ke Za Zhi. 1987;3:284–5. 320. [PubMed] [Google Scholar]
- 21.Deva AK, Merten S, Chang L. Silicone in nasal augmentation rhinoplasty: A decade of clinical experience. Plast Reconstr Surg. 1998;102:1230–7. doi: 10.1097/00006534-199809040-00052. [DOI] [PubMed] [Google Scholar]
- 22.Shirakabe Y, Suzuki Y, Lam SM. A systematic approach to rhinoplasty of the Japanese nose: A thirty-year experience. Aesthetic Plast Surg. 2003;27:221–31. doi: 10.1007/s00266-003-0098-6. [DOI] [PubMed] [Google Scholar]
- 23.Tham C, Lai YL, Weng CJ, Chen YR. Silicone augmentation rhinoplasty in an Oriental population. Ann Plast Surg. 2005;54:1–5. doi: 10.1097/01.sap.0000141947.00927.49. [DOI] [PubMed] [Google Scholar]
- 24.Liao WC, Ma H, Lin CH. Balanced rhinoplasty in an Oriental population. Aesthetic Plast Surg. 2007;31:636–42. doi: 10.1007/s00266-006-0137-1. [DOI] [PubMed] [Google Scholar]
- 25.Zeng Y, Wu W, Yu H, Yang J, Chen G. Silicone implant in augmentation rhinoplasty. Ann Plast Surg. 2002;49:495–9. doi: 10.1097/00000637-200211000-00009. [DOI] [PubMed] [Google Scholar]


