Abstract
Previously, recombinant vesicular stomatitis virus (rVSV) pseudotypes expressing Ebolavirus glycoproteins (GPs) in place of the VSV G protein demonstrated protection of nonhuman primates from lethal homologous Ebolavirus challenge. Those pseudotype vectors contained no additional attenuating mutations in the rVSV genome. Here we describe rVSV vectors containing a full complement of VSV genes and expressing the Ebola virus (EBOV) GP from an additional transcription unit. These rVSV vectors contain the same combination of attenuating mutations used previously in the clinical development pathway of an rVSV/human immunodeficiency virus type 1 vaccine. One of these rVSV vectors (N4CT1-EBOVGP1), which expresses membrane-anchored EBOV GP from the first position in the genome (GP1), elicited a balanced cellular and humoral GP-specific immune response in mice. Guinea pigs immunized with a single dose of this vector were protected from any signs of disease following lethal EBOV challenge, while control animals died in 7–9 days. Subsequently, N4CT1-EBOVGP1 demonstrated complete, single-dose protection of 2 macaques following lethal EBOV challenge. A single sham-vaccinated macaque died from disease due to EBOV infection. These results demonstrate that highly attenuated rVSV vectors expressing EBOV GP may provide safer alternatives to current EBOV vaccines.
Keywords: attenuation, rVSV vector, Ebola vaccine, glycoprotein, challenge, nonhuman primates
The genus Ebolavirus is classified within the Filoviridae family and comprises 5 closely related but antigenically distinct virus species: Bundibugyo ebolavirus, Reston ebolavirus, Sudan ebolavirus, Tai Forest ebolavirus, and Zaire ebolavirus [1, 2]. In nature, all but Reston virus have been isolated only in sub-Saharan Africa, where the likely virus reservoir is thought to be in bats [3, 4]. All but the Tai Forest and Reston viruses have caused sporadic, deadly outbreaks of disease in humans since the discovery of Ebolavirus 38 years ago, with case-fatality rates of 30%–90% [5, 6]. The ongoing 2014 Ebola virus (EBOV) outbreak in West Africa is the largest recorded, with case-fatality rates of around 50%. Hospitalization of patients seemingly improves clinical outcome and public health initiatives may slow the spread of disease, but mass vaccination programs in EBOV-endemic regions will likely be required to extinguish the current outbreak and prevent such occurrences in the future.
The EBOV genome is composed of a single strand of negative-sense RNA, approximately 19 kb in length, encoding 7 major viral polypeptides. One of these proteins is the EBOV glycoprotein (EBOVGP), which mediates virion attachment and fusion to susceptible cells [7]. The EBOVGP also contains the major virus neutralization epitopes [8, 9]; accordingly, the EBOVGP has been the target for a variety of EBOV vaccine designs. For a thorough review of vaccine approaches see Falzarano et al [10]. The vector in one such vaccine is recombinant vesicular stomatitis virus (rVSV), in which the gene encoding VSV G has been replaced with the gene encoding EBOVGP [11, 12]. This rVSV pseudotype replicates efficiently in cell culture and also propagates in vivo.
VSV is a member of the Rhabdoviridae family and, similar to EBOV, has a single-strand, negative-sense RNA genome, approximately 11 kb long, encoding 5 major viral proteins. In nature, VSV cycles between biting insects, which are the likely reservoir, and livestock [13–15]. The virus replicates to high titer in virus-induced vesicles at insect bite sites on the nose, lips, teats, and coronary bands of hooves. Disease in livestock is self-limiting and typically resolves in 10–11 days without significant consequences. VSV can also infect humans who have close contact with infected animals or purified virus [16, 17]. Infection results in mild influenza-like symptoms, which typically resolve in 3–5 days without complications [16, 17]. The very low seroprevalence of VSV in humans favored development of VSV as a vaccine vector and became feasible when Rose et al developed a system for recovery of rVSV from genomic complementary DNA (cDNA) [18]. Since then, rVSV vectors expressing antigens from human pathogens have demonstrated high levels of efficacy in the respective animal disease models [19–22].
VSV exhibits a pronounced 3′ to 5′ gradient of gene expression due to discontinuous messenger RNA (mRNA) transcription across intergenic regions [23, 24], allowing modulation of virus protein or foreign antigen expression as a function of gene distance from the 3′ transcription promoter [25, 26]. A highly attenuated rVSV vector expressing human immunodeficiency virus type 1 (HIV) gag from the first position in the genome was developed and has been demonstrated to be safe in stringent mouse and nonhuman primate (NHP) neurovirulence and biodistribution studies [27–29]. This rVSV vector was attenuated by combining N gene translocation from position 1–4 (N4) in the genome and truncation of the G protein cytoplasmic tail (CT) from 29 amino acids (aa) in native form to 1 aa (CT1) [28, 30]. This N4CT1-HIVgag1 vector was subsequently shown to be safe and immunogenic in phase 1 clinical trials (HVTN 090 and HVTN 087; available at: http://clinicaltrials.gov/), and after vaccination viremia was undetectable by an VSV infectivity assay or a VSV-specific polymerase chain reaction assay in blood, urine, or saliva specimens obtained from trial participants (unpublished data).
Here we describe the generation of attenuated rVSV vectors expressing EBOVGP and their immunogenicity in mice. The vector that elicited the most balanced EBOVGP-specific humoral and cellular immune response in mice was then evaluated for protective efficacy in guinea pig and NHP challenge studies.
MATERIALS AND METHODS
Animal Care and Use
For murine studies, 8–10-week-old female BALB/c mice were used. Mice were maintained according to the Guide for the Care and Use of Laboratory Animals [31]. In addition, procedures for the use and care of the mice were approved by Profectus BioSciences and New York Medical College institutional animal care and use committees (IACUCs). The guinea pig and macaque studies were carried out in strict accordance with the recommendations described in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health, the Office of Animal Welfare, and the US Department of Agriculture. All animal work was approved by the National Institute of Allergy and Infectious Diseases Division of Intramural Research IACUC at the Rocky Mountain Laboratories (RML). The facility is accredited by the American Association for Accreditation of Laboratory Animal Care. All procedures were performed on animals after they were anesthetized by trained personnel under the supervision of veterinary staff. All efforts were made to minimize the pain and suffering of animals, with early end point criteria specified by the RML IACUC–approved score parameters used to determine when animals should be humanely euthanized.
Generation of EBOV Vectors
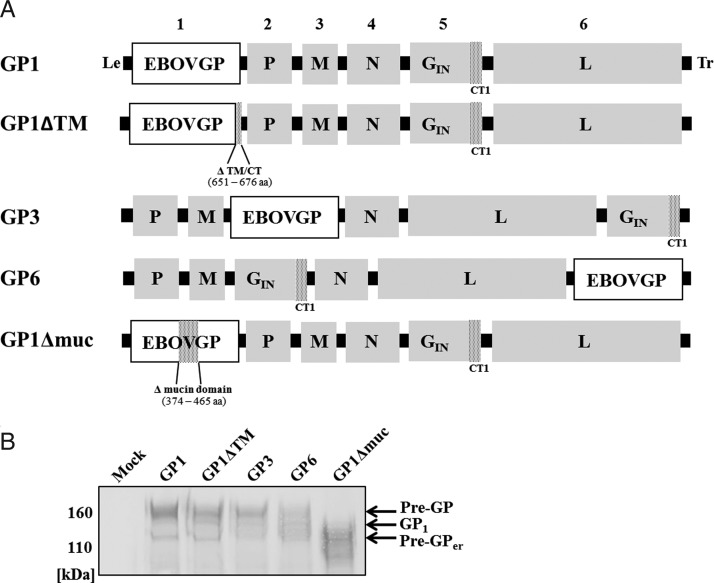
As described previously [28, 30], the N4CT1-HIVgag1 vector was used as template for generating all rVSV/EBOV vectors expressing EBOVGP. The N4CT1-HIVgag1 genomic cDNA was modified by exchanging the gag gene located in position 1 of the genome with the EBOVGP gene (1976, Mayinga isolate), generating N4CT1-EBOVGP1 cDNA (GP1; Figure 1A). A vector expressing a third-position EBOVGP (GP3; Figure 1A) was generated by inserting an expression cassette between the M and N genes. To insert the EBOVGP gene in genome position 6 (GP6; Figure 1A), the N and G genes were swapped and an expression cassette was positioned between VSV L and the trailer sequence. For adventitious agent testing of clinical trial material, large quantities of EBOVGP-specific neutralizing antibody are required to neutralize vaccine virus infectivity. To avoid this requirement, a gene expressing secreted EBOVGP was generated by deleting the sequence encoding the transmembrane region and cytoplasmic tail (aa 651–676). This modified EBOVGP gene was inserted into position 1 of N4CT1 (GP1ΔTM; Figure 1A). The mucin-like domain of EBOVGP spans aa 305–485, and part of this domain (aa 374–465) was deleted (GP1Δmuc; Figure 1A). This modified EBOVGP gene was generated following observations that part of the mucin region was deleted upon multiple serial passage of N4CT1-EBOVGP1 on Vero cell monolayers and was included here to assess the effect of partial removal of the glycan “coat” on EBOVGP immunogenicity. EBOVGP expression was analyzed by Western blotting for all vectors (Figure 1B).
Figure 1.
A, Genetic organization of recombinant vesicular stomatitis virus (rVSV)/Ebola virus (EBOV) vectors. rVSV genomes containing the N gene translocation (N4) and truncated G protein cytoplasmic tail (CT1) were used in all vector designs. Anchored full-length EBOV glycoprotein (EBOVGP) was inserted either in the first, third, or sixth position and designated as GP1, GP3, or GP6, respectively. An EBOVGP inserted in position 1 with the hydrophobic membrane anchor deleted at amino acid positions 651–676 was generated to make a secreted protein (GP1ΔTM). An EBOVGP with part of the mucin-like domain deleted at positions 374–465 (GP1Δmuc) was inserted in position 1. Virus leader (Le), trailer (Tr), and intergenic regions are shown in black, and shaded areas in EBOVGP represent deleted amino acid regions. Numbers above the N4CT1 constructs indicate gene position within the genome. GP1, N4CT1-EBOVGP1; GP1Δmuc, N4CT1-EBOVGP1Δmuc; GP1ΔTM, N4CT1-EBOVGP1ΔTM; GP3, N4CT1-EBOVGP3; GP6, N4CT1-EBOVGP6. B, Western blot analysis of EBOVGP expression. Protein lysates from infected Vero cells were evaluated using 4%–12% polyacrylamide gel electrophoresis and probed with a monoclonal mouse anti-EBOVGP antibody (IBT BioServices; catalog number 0201-020). Bands were detected by an anti-mouse–AP conjugate immunoglobulin G (H + L; Promega) and developed with a chromogenic substrate (Western Blue, Promega). Bands were seen at approximately 160, 140, and 110 kDa with varied expression levels depending on the position of EBOVGP within the genome. GP1Δmuc showed a lower-molecular-weight EBOVGP band as a result of lost glycosylation sites due to deletion of amino acid positions 374–465. Abbreviations: GP1, processed by furin proteolysis into mature EBOVGP; pre-GP, full-length EBOVGP containing mature carbohydrates (O-/N-linked glycosylations); pre-Gper, endoplasmic reticulum–localized form of full-length EBOVGP.
Vectors were rescued from genomic cDNA as previously described [32]. Rescued virus was plaque purified and amplified on Vero cell monolayers (ATCC CCL-81). For animal studies, vectors were purified from infected cell supernatants by centrifugation through a 10% sucrose cushion. Virus pellets were resuspended in phosphate-buffered saline (PBS), pH 7.0, mixed with stabilizer (7 mM K2HPO4, 4 mM KH2PO4, and 218 mM sucrose), snap frozen, and stored at −80°C.
Animal Vaccinations, Inoculations, and Sample Collection
For the mouse immunogenicity study, rVSV/EBOV vectors were administered at 1 × 107 plaque-forming units (PFU) by intramuscular injection of the tibialis anterior muscle (total injection volume, 0.05 mL). Serum was collected at weeks 0, 3, and 5. Ten days after final the inoculation, mice were euthanized by CO2 inhalation, and serum and spleen cells were harvested.
For the mouse neurovirulence study, groups of ten 5-week-old female Swiss Webster mice were anesthetized and inoculated intracranially with 0.02 mL of serial 10-fold dilutions of each vector as previously described [30]. After inoculation, mice were weighed daily and assessed for signs of disease over 3 weeks. Neurovirulence was assessed by measuring morbidity and mortality as an end point. Mice that were showing severe signs of disease or were moribund were promptly euthanized. Cumulative deaths across all doses tested allowed the 50% lethal dose to be calculated for each vector [33].
For guinea pig immunization, 2 × 105 PFU of each vector was administered intraperitoneally. On day 21 after vaccination guinea pigs were challenged with 10 focus-forming units (FFU) of guinea pig–adapted EBOV (GPA-EBOV) [34] by intraperitoneal injection. All animals were weighed daily and monitored for signs of illness.
For macaque challenge, 3 healthy, EBOV-naive, adult (age, 5–10 years; weight, 3–12 kg), male and female Rhesus macaques (Macaca mulatta) were randomly assigned to a vaccination group (n = 2) and a nonvaccination control group (n = 1). At study day −21, macaques were anesthetized with ketamine and inoculated in the caudal thigh muscle with 1 × 107 PFU of rVSV/EBOV vector (total volume, 1 mL). At study day 0, macaques were anesthetized with ketamine and challenged with 1000 FFU of EBOV [11] by intramuscular injection of the caudal thigh muscle (total volume, 1 mL). Macaques were monitored for signs of illness (ie, abnormal temperature, weight loss, clinical examination findings, hematology findings, and blood chemistry findings) following vaccination and the EBOV challenge portions of the study.
Murine Interferon γ (IFN-γ) Enzyme-Linked Immunospot (ELISpot) Assay
For murine studies, vaccine-elicited IFN-γ ELISpot responses were determined using a mouse IFN-γ ELISpot kit (BD Biosciences, San Diego, California) as previously described [35]. Splenocytes were incubated with 2 µg/mL Con-A (Sigma), peptide pools (15-mers overlapping by 11 aa; final peptide concentration, 1 µM [each]) spanning EBOVGP, or medium alone.
Serologic Analyses
A murine enzyme-linked immunosorbent assay (ELISA) previously described [35] was modified by using ELISA plates coated with 100 ng/well of purified recombinant EBOVGP (IBT Bioservices) to determine EBOVGP-specific serum immunoglobulin G (IgG) titers. Murine serum samples were added to ELISA plates at a starting dilution of 1:100 and were further diluted 3-fold across the plates. Antigen-specific antibody titers were defined as the reciprocal of the last serum dilution giving an OD450 of >0.1.
Antigens for the macaque ELISA were produced as previously described [36]. Macaque sera were inactivated by γ-irradiation (5 Mrad) according to a standard operating protocol approved by the institutional biosafety committee at RML. ELISA with EBOVGPΔTM was performed as described previously [36].
RESULTS
Immunogenicity of rVSV/EBOV Vectors in Mice
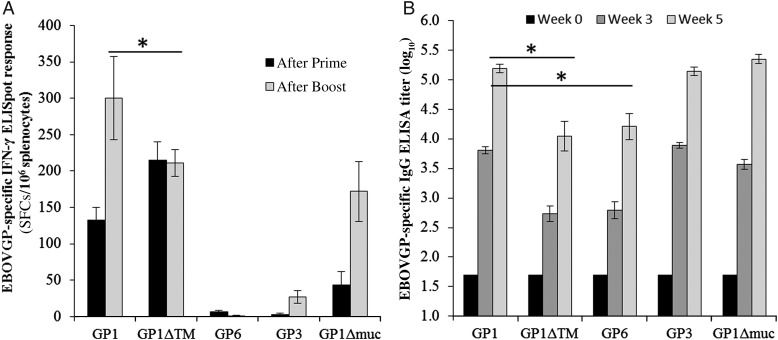
To identify the most-effective rVSV/EBOV vector design for induction of EBOVGP-specific immune responses, the vectors outlined in Figure 1A were compared for their ability to elicit EBOVGP-specific cell-mediated immune and binding antibody responses in mice (Figure 2). Groups of BALB/c mice (n = 10) were immunized intramuscularly at study week 0 (Figure 2A). Ten days after primary immunizations, splenocytes were collected from 5 mice/group and tested for EBOVGP-specific IFN-γ secretion by ELISpot assay. The remaining 5 mice/group were boosted intramuscularly at study week 3 with 107 PFU of each rVSV/EBOV vector. Ten days after boosting, splenocytes were collected and tested as described above.
Figure 2.
Cell-mediated immune and humoral responses elicited by recombinant vesicular stomatitis virus (rVSV)/Ebola virus (EBOV) vectors in mice. At study weeks 0 and 3, BALB/c mice were immunized intramuscularly with 107 plaque-forming units (PFU) of rVSV/EBOV vectors. A, EBOV glycoprotein (EBOVGP)–specific interferon γ (IFN-γ) enzyme-linked immunospot (ELISpot) responses. Data represent the average EBOVGP-specific IFN-γ ELISpot responses (n = 5/group) 10 days after prime and 10 days after boost, with standard errors of the mean. B, EBOVGP-specific serum immunoglobulin G (IgG) enzyme-linked immunosorbent assay (ELISA) titers. Data represent the average log10 EBOVGP-specific IgG ELISA titer (n = 5/group), with standard errors of the mean. *P < .05. Abbreviations: GP1, processed by furin proteolysis into mature EBOVGP; SFC, spot-forming cell.
After 1 immunization, the highest mean EBOVGP-specific IFN-γ ELISpot responses (±standard error of the mean [SEM]) were detected in mice immunized with N4CT1-EBOVGP1ΔTM (215 ± 25 spot-forming cells [SFCs]/106 splenocytes) and N4CT1-EBOVGP1 (133 ± 17 SFC/106 splenocytes). Interestingly, N4CT1-EBOVGP1Δmuc, elicited a significantly reduced response (mean ± SEM, 43 ± 19 SFCs/106 splenocytes) relative to N4CT1-EBOVGP1 and N4CT1-EBOVGP1. Notably, after 1 immunization, GP responses were undetectable in mice immunized with vectors expressing EBOVGP from genome positions 3 or 6.
After boosting, the highest mean EBOVGP-specific IFN-γ ELISpot responses (±SEM) were again detected in mice immunized with N4CT1-EBOVGP1ΔTM (211 ± 18 SFCs/106 splenocytes) and N4CT1-EBOVGP1 (mean ± SEM, 300 ± 57 SFCs/106 splenocytes). Mice immunized with N4CT1-EBOVGP1Δmuc showed an improved response (mean ± SEM, 172 ± 41 SFCs/106 splenocytes), and mice boosted with N4CT1-EBOVGP3 or N4CT1-EBOVGP6 still failed to demonstrate a measurable EBOVGP-specific IFN-γ ELISpot response.
Immunized mice were also monitored for induction of serum antibody responses by ELISA (Figure 2B). Ten days after boosting, mean serum EBOVGP-specific IgG titers (±SEM) were highest in mice immunized with N4CT1-EBOVGP1Δmuc vector (5.35 ± 0.08), N4CT1-EBOVGP1 (5.19 ± 0.07), and N4CT1-EBOVGP3 (5.14 ± 0.07). Interestingly, a statistically significant, approximately 10-fold lower EBOVGP-specific IgG titer was detected in mice immunized with N4CT1-EBOVGP1ΔTM (mean ± SEM, 4.05 ± 0.25) relative to mice immunized with N4CT1-EBOVGP1. A 10-fold lower titer was also detected in mice immunized with N4CT1-EBOVGP6 (4.21 ± 0.22) relative to mice immunized with vectors expressing EBOVGP from genome positions 1 or 3.
On the basis of the data presented in Figure 2, the N4CT1-EBOVGP1 vector expressing an anchored full-length EBOVGP in position 1 of the rVSV genome appeared to be the most immunogenic (with regard to cell-mediated and humoral immunity) in mice, so N4CT1-EBOVGP1 was selected for guinea pig and NHP challenge studies.
Protective Efficacy of rVSVN4CT1-EBOVGP1 in Guinea Pigs
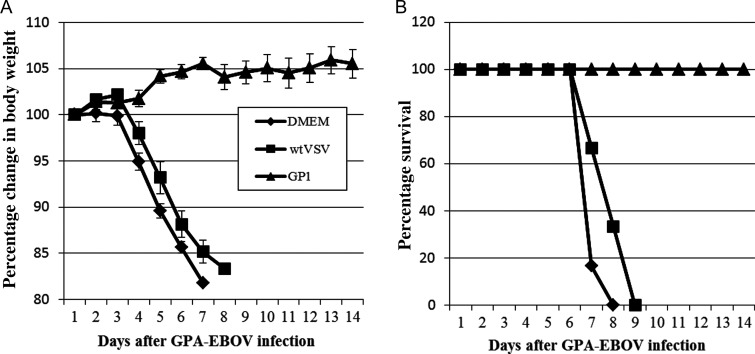
We next tested whether N4CT1-EBOVGP1 could protect guinea pigs from a lethal challenge (Figure 3). In this experiment, guinea pigs were immunized intraperitoneally with 2 × 105 PFU of N4CT1-EBOVGP1. For controls, additional groups of guinea pigs were immunized with 2 × 105 PFU of wtVSV or medium alone. On day 21 after immunization, all guinea pigs were challenged intraperitoneally with 10 FFU of GPA-EBOV. After challenge, guinea pigs were monitored for changes in body weight (Figure 3A), signs of disease, and survival (Figure 3B).
Figure 3.
Percentage change in body weight and percentage survival among guinea pigs immunized with N4CT1–Ebola virus glycoprotein (EBOVGP1) after EBOV challenge. Guinea pigs (n = 6) were immunized intramuscularly with 2 × 105 plaque-forming units (PFU) of N4CT1-EBOVGP1 (GP1), 2 × 105 PFU wtVSV, or Dulbecco's modified Eagle's medium (DMEM) alone. A total of 21 days after vaccination, the immunized guinea pigs were challenged with 10 focus-forming units of GPA-EBOV and monitored for percentage change in body weight (A) and percentage survival (B). Data represent the average percentage change, with standard errors of the mean. Abbreviation: GPA-EBOV, guinea pig–adapted EBOV.
Guinea pigs immunized with medium alone or wtVSV began to lose weight on day 4 after challenge and died from EBOV infection during study days 7 and 9 as observed previously [37]. In contrast, N4CT1-EBOVGP1 immunized guinea pigs gained weight and were completely protected from disease during the course of the study.
Immunogenicity and Protective Efficacy of rVSVN4CT1aGP1 in Macaques
Encouraged by findings from the guinea pig study, we determined whether N4CT1-EBOVGP1 could protect macaques from lethal EBOV challenge (Table 1). Three rhesus macaques were immunized intramuscularly in the caudal thigh muscle as follows: 2 were immunized with 1 × 107 PFU N4CT1-EBOVGP1 in a total volume of 1 mL (EBOV1 and EBOV2), and 1 macaque (CTRL) was mock immunized. At day 14 after immunization, both N4CT1-EBOVGP1–immunized macaques demonstrated measurable EBOVGP-specific serum IgG responses (titer, 1:100), and these responses increased (titer, 1:400) by study day 0. In contrast, the sham-immunized macaque remained seronegative for EBOVGP.
Table 1.
Preliminary Efficacy Study of N4CT1–Ebola Virus Glycoprotein (EBOVGP1) Vaccine in Rhesus Macaques
| Macaque | EBOVGP-Specific Antibody Titer |
||||
|---|---|---|---|---|---|
| Day −7 | Day 0a | Day 6 | Day 10 | Day 14 | |
| EBOV1b | 100 | 400 | 6400 | 25 600 | 25 600 |
| EBOV2b | 100 | 400 | 1600 | 25 600 | 25 600 |
| Control | 0 | 0 | 0 | NDc | NDc |
a Day of challenge with 1000 focus-forming units of EBOV by intramuscular injection.
b Macaques EBOV1 and EBOV2 were vaccinated on day −21 by intramuscular injection with 107 plaque-forming units of N4CT1-EBOVGP1. Both animals were alive on day 21 after challenge.
c No data (ND) were available because the control macaque was euthanized on day 6 after challenge.
At study day 0, all 3 macaques were challenged with 1000 FFU EBOV Mayinga by intramuscular injection in the caudal thigh muscle. As shown in Table 1, the single control animal failed to mount an EBOVGP-specific response on day 6 after challenge and quickly died from EBOV infection. Importantly, a rapid increase in the EBOVGP-specific serum IgG titer was observed on days 6, 10, and 14 after challenge in both vaccinated macaques, and they survived without showing signs of disease.
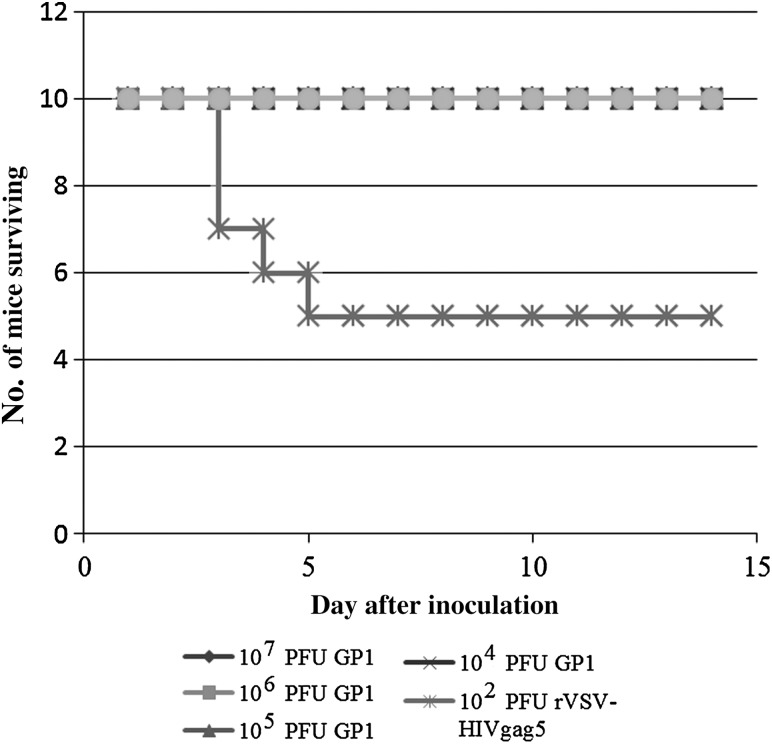
Lack of Neurovirulence of Attenuated rVSVN4CT1 Vectors Expressing EBOVGP
Mice are exquisitely sensitive to intracranial instillation of wtVSV [28, 30], leading to lethal viral encephalitis. Previously, it was shown that intracranial inoculation of 5-week-old Swiss Webster mice with 108 PFU of the highly attenuated N4CT1-HIVgag1 vector caused no significant illness, so a 50% lethal dose could not be achieved for this vector [28]. To test the neurovirulence potential of N4CT1-EBOVGP1, groups of outbred Swiss Webster mice were inoculated intracranially with N4CT1-EBOVGP1 in a dose-ranging study (104–107 PFU; Figure 4). Two control groups were inoculated with 102 PFU of a less attenuated rVSV (rVSV-HIVgag5) or with PBS alone. Following inoculation, mice were assessed for morbidity and mortality over 2 weeks.
Figure 4.
Mouse survival chart following intracranial inoculation with N4CT1–Ebola virus glycoprotein (EBOVGP1). Forty, 5-week-old female Swiss Webster mice (n = 10/group) were inoculated intracranially with 4 dose levels (104–107 plaque-forming units [PFU]) of N4CT1-EBOVGP1, 102 PFU rVSV-HIVgag5, or phosphate-buffered saline. Mice were assessed for morbidity and mortality for 2 weeks following inoculation. Abbreviations: HIV, human immunodeficiency virus; rVSV, recombinant vesicular stomatitis virus.
Consistent with previously published reports [28, 30], mice inoculated intracranially with PBS survived, and approximately half of the mice inoculated with rVSV-HIVgag5 died 3–5 days after inoculation. Importantly, all mice inoculated with N4CT1-EBOVGP1 survived and were disease free.
DISCUSSION
Previous work demonstrated that vaccination with a single dose of replication-competent rVSV pseudotyped with EBOVGPs protected mice, hamsters, guinea pigs, and NHPs from lethal EBOV challenge [12, 38, 39]. The rVSV vector used in those studies retained the natural VSV genome organization, except the VSV G gene was replaced with the EBOVGP gene [39]. Here we demonstrate protection of guinea pigs and NHPs with a highly attenuated, replication competent form of rVSV that retains the VSV G gene [27, 28, 30] and expresses the EBOVGP from an additional transcription unit inserted at position 1 in the rVSV genome.
The mouse immunogenicity study demonstrated that EBOVGP-specific cell-mediated immune responses were more robust when the EBOVGP gene was in the first position in the genome, compared with the third and sixth positions, consistent with greater relative abundance of EBOVGP in infected cells due to the steep 3′ to 5′ transcription gradient present during VSV replication [23, 24, 26]. The cell-mediated immune response was similar for secreted and anchored forms of EBOVGP, indicating that both forms of EBOVGP underwent a similar degree of processing and presentation of T-cell epitopes in antigen-presenting cells. Interestingly, there was a significant reduction in the cell-mediated immune response to EBOVGP when part of the mucin-rich region was deleted, possibly as a result of altered proteosomal processing of EBOVGP or direct deletion of T-cell epitopes. After decay of the primary cell-mediated immune response, a second vaccine dose boosted ELISpot responses to levels seen after primary vaccination; however, there was still no detectable cell-mediated immune response elicited by vectors expressing EBOVGP from position 3 and 6, indicating the requirement for higher EBOVGP levels in infected cells to generate detectable EBOVGP-specific cell-mediated immune responses.
As expected, the EBOVGP-specific IgG response in mice was greatest for N4CT1-EBOVGP1 and N4CT1-EBOVGP1Δmuc vectors expressing the highest levels of EBOVGP from genome position 1. Interestingly, N4CT1-EBOVGP1ΔTM elicited much lower levels of EBOVGP-specific IgG than N4CT1-EBOVGP1. We speculate this may reflect differences in the tertiary and quaternary structure of secreted EBOVGP, compared with the trimeric conformation achieved by anchored EBOVGP. Notably, the secreted EBOVGP described here is different from the naturally occurring secreted form of EBOVGP that is translated from unedited EBOVGP mRNA [40]. The corollary is that anchored trimeric EBOVGP spikes on the surface of infected cells and virus particles present a dense array of structural epitopes that may interact more efficiently with B cells than soluble secreted EBOVGP, as is the case for other particulate antigen compositions [41, 42]. EBOVGP-specific IgG responses were highest for N4CT1-EBOVGP1Δmuc [43], possibly reflecting better exposure of EBOVGP epitopes by removal of part of the carbohydrate cloak [44]. The N4CT1-EBOVGP3 vector also elicited a robust EBOVGP-specific IgG response, which contrasts with the undetectable EBOVGP-specific cell-mediated immune response induced by this vector. The explanation for this anomaly is unclear but could be due to relative differences in EBOVGP-specific cellular and humoral antigenicity. We believe the approximate 30% attenuation of expression across each gene junction could drop the EBOVGP level below a threshold required to elicit cell-mediated immune responses (N4CT1-EBOVGP3), while the EBOVGP level is still adequate to induce a relatively robust humoral response. However, for N4CT1-EBOVGP6, the EBOVGP-specific humoral response does decline markedly, presumably as a result of the calculated 85% reduction in EBOVGP expression when in the sixth position in the genome.
Previous work demonstrated that the N4CT1 vector backbone was highly attenuated in the mouse intracranial NV model [28, 30]. However, Western blot data demonstrated that EBOVGP was present on the surface of virus particles when expressed by an rVSV vector that retained the VSV G gene (unpublished data). Therefore, a mouse NV study was performed to assess any changes in virulence arising from the possible alteration of vector tropism mediated by EBOVGP. Results confirmed the highly attenuated nature of N4CT1-EBOVGP1 in the mouse central nervous system, indicating that the presence of EBOVGP on the virion surface, in addition to VSV G protein, did not enhance virus spread in the brain, presumably because cells in the central nervous system lack the EBOVGP-specific receptor [45–47] and because virus using VSV G receptors remained attenuated as previously described [30].
Because N4CT1-EBOVGP1 elicited a desirable balance of humoral and cellular immune responses to EBOVGP after a single vaccine dose in mice, it was selected for guinea pig and NHP challenge studies. One dose of this vector protected guinea pigs from signs of disease following challenge with a lethal dose of GPA-EBOV. Interestingly, there was a slight delay in onset of the first signs of disease after challenge of wtVSV-vaccinated guinea pigs. One possible explanation is that induction of IFNs and other innate immune responses by rVSV [48, 49] leaves the guinea pig innate immune system on high alert, even 21 days after vaccination, resulting in a generalized antiviral state that may initially slow the GPA-EBOV infection [49, 50].
A single dose of N4CT1-EBOVGP1 vector also protected NHPs from disease following EBOV challenge. An EBOVGP-specific IgG titer was detected in both immunized macaques prior to challenge and was expanded following EBOV challenge, indicating that a preexisting EBOVGP-specific antibody response is important for protection. Unfortunately cell-mediated immune responses in NHPs were not measured and may also contribute significantly to protection. The N4CT1-EBOVGP1 vector used in these challenge studies is similar to the highly attenuated N4CT1-gag1 vector that demonstrated safety and immunogenicity in 2 phase 1 clinical studies. The studies described here are the first to demonstrate protection of guinea pigs and macaques with a single dose of highly attenuated rVSV expressing EBOVGP, and we believe that the N4CT1-EBOVGP1 vector has the essential safety and efficacy characteristics for use in a vaccine to prevent EBOV infection in humans and the great apes. This highly attenuated vector platform will likely also have the potential to serve in a vaccine against other EBOV strains that cause disease in humans and apes. Ultimately, a multivalent EBOV vaccine may be possible by combining ≥2 vaccine vectors in a single vaccine formulation.
Notes
Financial support. This work was supported by Profectus BioSciences and the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Potential conflicts of interest. D. M., T. L., R. X., A. O.-S., S. H., B. N., M. A. E., J. H. E., and D. K. C. are paid employees of Profectus BioSciences. D. K. C. is a coinventor of the attenuated VSV vector (US patent 8 287 878) and does not receive royalties or other payments. T. W. G. has pending US patents (61/014 626, 61/014 669, and 61/070 748) on behalf of Boston University. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Kuhn JH, Becker S, Ebihara H et al. Proposal for a revised taxonomy of the family Filoviridae: classification, names of taxa and viruses, and virus abbreviations. Arch Virol 2010; 155:2083–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macneil A, Reed Z, Rollin PE. Serologic cross-reactivity of human IgM and IgG antibodies to five species of Ebola virus. PLoS Negl Trop Dis 2011; 5:e1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leroy EM, Kumulungui B, Pourrut X et al. Fruit bats as reservoirs of Ebola virus. Nature 2005; 438:575–6. [DOI] [PubMed] [Google Scholar]
- 4.Pourrut X, Delicat A, Rollin PE, Ksiazek TG, Gonzalez JP, Leroy EM. Spatial and temporal patterns of Zaire ebolavirus antibody prevalence in the possible reservoir bat species. J Infect Dis 2007; 196(suppl 2):S176–83. [DOI] [PubMed] [Google Scholar]
- 5.Feldmann H. Ebola—a growing threat? N Engl J Med 2014; 371:1375–8. [DOI] [PubMed] [Google Scholar]
- 6.Kucharski AJ, Edmunds WJ. Case fatality rate for Ebola virus disease in West Africa. Lancet 2014; 384:1260. [DOI] [PubMed] [Google Scholar]
- 7.Lee JE, Fusco ML, Hessell AJ, Oswald WB, Burton DR, Saphire EO. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 2008; 454:177–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marzi A, Yoshida R, Miyamoto H et al. Protective efficacy of neutralizing monoclonal antibodies in a nonhuman primate model of Ebola hemorrhagic fever. PLoS One 2012; 7:e36192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qiu X, Fernando L, Melito PL et al. Ebola GP-specific monoclonal antibodies protect mice and guinea pigs from lethal Ebola virus infection. PLoS Negl Trop Dis 2012; 6:e1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falzarano D, Geisbert TW, Feldmann H. Progress in filovirus vaccine development: evaluating the potential for clinical use. Expert Rev Vaccines 2011; 10:63–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falzarano D, Feldmann F, Grolla A et al. Single immunization with a monovalent vesicular stomatitis virus-based vaccine protects nonhuman primates against heterologous challenge with Bundibugyo ebolavirus. J Infect Dis 2011; 204(suppl 3):S1082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geisbert TW, Feldmann H. Recombinant vesicular stomatitis virus-based vaccines against Ebola and Marburg virus infections. J Infect Dis 2011; 204(suppl 3):S1075–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jonkers AH. The epizootiology of the vesicular stomatitis viruses: a reappraisal. Am J Epidemiol 1967; 86:286–91. [DOI] [PubMed] [Google Scholar]
- 14.Tesh RB, Chaniotis BN, Johnson KM. Vesicular stomatitis virus, Indiana serotype: multiplication in and transmission by experimentally infected phlebotomine sandflies (Lutzomyia trapidoi). Am J Epidemiol 1971; 93:491–5. [DOI] [PubMed] [Google Scholar]
- 15.Tesh RB, Chaniotis BN, Johnson KM. Vesicular stomatitis virus (Indiana serotype): transovarial transmission by phlebotomine sandflies. Science 1972; 175:1477–9. [DOI] [PubMed] [Google Scholar]
- 16.Johnson KM, Vogel JE, Peralta PH. Clinical and serological response to laboratory-acquired human infection by Indiana type vesicular stomatitis virus (VSV). Am J Trop Med Hyg 1966; 15:244–6. [DOI] [PubMed] [Google Scholar]
- 17.Tesh RB, Boshell J, Modi GB et al. Natural infection of humans, animals, and phlebotomine sand flies with the Alagoas serotype of vesicular stomatitis virus in Colombia. Am J Trop Med Hyg 1987; 36:653–61. [DOI] [PubMed] [Google Scholar]
- 18.Lawson ND, Stillman EA, Whitt MA, Rose JK. Recombinant vesicular stomatitis viruses from DNA. Proc Natl Acad Sci U S A 1995; 92:4477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kahn JS, Roberts A, Weibel C, Buonocore L, Rose JK. Replication-competent or attenuated, nonpropagating vesicular stomatitis viruses expressing respiratory syncytial virus (RSV) antigens protect mice against RSV challenge. J Virol 2001; 75:11079–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapadia SU, Rose JK, Lamirande E, Vogel L, Subbarao K, Roberts A. Long-term protection from SARS coronavirus infection conferred by a single immunization with an attenuated VSV-based vaccine. Virology 2005; 340:174–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts A, Buonocore L, Price R, Forman J, Rose JK. Attenuated vesicular stomatitis viruses as vaccine vectors. J Virol 1999; 73:3723–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose NF, Marx PA, Luckay A et al. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 2001; 106:539–49. [DOI] [PubMed] [Google Scholar]
- 23.Abraham G, Banerjee AK. Sequential transcription of the genes of vesicular stomatitis virus. Proc Natl Acad Sci U S A 1976; 73:1504–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ball LA, White CN. Order of transcription of genes of vesicular stomatitis virus. Proc Natl Acad Sci U S A 1976; 73:442–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ball LA, Pringle CR, Flanagan B, Perepelitsa VP, Wertz GW. Phenotypic consequences of rearranging the P, M, and G genes of vesicular stomatitis virus. J Virol 1999; 73:4705–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flanagan EB, Ball LA, Wertz GW. Moving the glycoprotein gene of vesicular stomatitis virus to promoter-proximal positions accelerates and enhances the protective immune response. J Virol 2000; 74:7895–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clarke DK, Nasar F, Chong S et al. Neurovirulence and immunogenicity of attenuated recombinant vesicular stomatitis viruses in nonhuman primates. J Virol 2008; 88:6690–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper D, Wright KJ, Calderon PC et al. Attenuation of recombinant vesicular stomatitis virus HIV-1 vaccine vectors by gene translocations and G gene truncation reduces neurovirulence and enhances immunogenicity in mice. J Virol 2008; 82:207–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson JE, Coleman JW, Kalyan NK et al. In vivo biodistribution of a highly attenuated recombinant vesicular stomatitis virus expressing HIV-1 Gag following intramuscular, intranasal, or intravenous inoculation. Vaccine 2009; 27:2930–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clarke DK, Nasar F, Lee M et al. Synergistic attenuation of vesicular stomatitis virus by combination of specific G gene truncations and N gene translocations. J Virol 2007; 81:2056–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guide for the care and use of laboratory animals. Washington, DC: National Academies Press, 1996. [PubMed] [Google Scholar]
- 32.Witko SE, Kotash CS, Nowak RM et al. An efficient helper-virus-free method for rescue of recombinant paramyxoviruses and rhadoviruses from a cell line suitable for vaccine development. J Virol Methods 2006; 135:91–101. [DOI] [PubMed] [Google Scholar]
- 33.Reed E, Muench H. A simple method of estimating fifty percent endpoints. Am J Hyg 1938; 27:493–7. [Google Scholar]
- 34.Connolly BM, Steele KE, Davis KJ et al. Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis 1999; 179(suppl 1):S203–17. [DOI] [PubMed] [Google Scholar]
- 35.Megati S, Garcia-Hand D, Cappello S et al. Modifying the HIV-1 env gp160 gene to improve pDNA vaccine-elicited cell-mediated immune responses. Vaccine 2008; 26:5083–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nakayama E, Yokoyama A, Miyamoto H et al. Enzyme-linked immunosorbent assay for detection of filovirus species-specific antibodies. Clin Vaccine Immunol 2010; 17:1723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marzi A, Ebihara H, Callison J et al. Vesicular stomatitis virus-based Ebola vaccines with improved cross-protective efficacy. J Infect Dis 2011; 204(suppl 3):S1066–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geisbert TW, Daddario-Dicaprio KM, Geisbert JB et al. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 2008; 26:6894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones SM, Feldmann H, Stroher U et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med 2005; 11:786–90. [DOI] [PubMed] [Google Scholar]
- 40.Falzarano D, Krokhin O, Wahl-Jensen V et al. Structure-function analysis of the soluble glycoprotein, sGP, of Ebola virus. Chembiochem 2006; 7:1605–11. [DOI] [PubMed] [Google Scholar]
- 41.Heinz FX, Allison SL, Stiasny K et al. Recombinant and virion-derived soluble and particulate immunogens for vaccination against tick-borne encephalitis. Vaccine 1995; 13:1636–42. [DOI] [PubMed] [Google Scholar]
- 42.Warfield KL, Bosio CM, Welcher BC et al. Ebola virus-like particles protect from lethal Ebola virus infection. Proc Natl Acad Sci U S A 2003; 100:15889–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinez O, Tantral L, Mulherkar N, Chandran K, Basler CF. Impact of Ebola mucin-like domain on antiglycoprotein antibody responses induced by Ebola virus-like particles. J Infect Dis 2011; 204(suppl 3):S825–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dowling W, Thompson E, Badger C et al. Influences of glycosylation on antigenicity, immunogenicity, and protective efficacy of Ebola virus GP DNA vaccines. J Virol 2007; 81:1821–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carette JE, Raaben M, Wong AC et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 2011; 477:340–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wool-Lewis RJ, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol 1998; 72:3155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang Z, Delgado R, Xu L et al. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science 1998; 279:1034–7. [DOI] [PubMed] [Google Scholar]
- 48.Conzelmann KK. Transcriptional activation of alpha/beta interferon genes: interference by nonsegmented negative-strand RNA viruses. J Virol 2005; 79:5241–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van den Broek MF, Muller U, Huang S, Aguet M, Zinkernagel RM. Antiviral defense in mice lacking both alpha/beta and gamma interferon receptors. J Virol 1995; 69:4792–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Biron CA, Nguyen KB, Pien GC, Cousens LP, Salazar-Mather TP. Natural killer cells in antiviral defense: function and regulation by innate cytokines. Annu Rev Immunol 1999; 17:189–220. [DOI] [PubMed] [Google Scholar]