Abstract
Background:
Hospital-based outpatient departments traditionally charge higher prices for ambulatory procedures, compared with freestanding surgery centers. Under emerging reference-based benefit designs, insurers establish a contribution limit that they will pay, requiring the patient to pay the difference between that contribution limit and the actual price charged by the facility. The purpose of this study was to evaluate the impact of reference-based benefits on consumer choices, facility prices, employer spending, and surgical outcomes for orthopaedic procedures performed at ambulatory surgery centers.
Methods:
We obtained data on 3962 patients covered by the California Public Employees’ Retirement System (CalPERS) who underwent arthroscopy of the knee or shoulder in the three years prior to the implementation of reference-based benefits in January 2012 and on 2505 patients covered by CalPERS who underwent arthroscopy in the two years after implementation. Control group data were obtained on 57,791 patients who underwent arthroscopy and were not subject to reference-based benefits. The impact of reference-based benefits on consumer choices between hospital-based and freestanding facilities, facility prices, employer spending, and surgical complications was assessed with use of difference-in-differences multivariable regressions to adjust for patient demographic characteristics, comorbidities, and geographic location.
Results:
By the second year of the program, the shift to reference-based benefits was associated with an increase in the utilization of freestanding ambulatory surgery centers by 14.3 percentage points (95% confidence interval, 8.1 to 20.5 percentage points) for knee arthroscopy and by 9.9 percentage points (95% confidence interval, 3.2 to 16.7 percentage points) for shoulder arthroscopy and a corresponding decrease in the use of hospital-based facilities. The mean price paid by CalPERS fell by 17.6% (95% confidence interval, −24.9% to −9.6%) for knee procedures and by 17.0% (95% confidence interval, −29.3% to −2.5%) for shoulder procedures. The shift to reference-based benefits was not associated with a change in the rate of surgical complications. In the first two years after the implementation of reference-based benefits, CalPERS saved $2.3 million (13%) on these two orthopaedic procedures.
Conclusions:
Reference-based benefits increase consumer sensitivity to price differences between freestanding and hospital-based surgical facilities.
Clinical Relevance:
This study shows that the implementation of reference-based benefits does not result in a significant increase in measured complication rates for those subject to reference-based benefits.
The prices charged for similar health-care services vary widely across different clinical settings, partly because of the indifference of well-insured consumers to price differences when selecting providers. In particular, the prices paid for ambulatory surgical procedures by private insurers are often much higher in hospital outpatient departments than in freestanding ambulatory surgery centers1. Medicare also pays substantially higher rates to hospital outpatient departments than to ambulatory surgery centers for similar services2.
Consumers are being expected to take a more active role in their own health-care decision-making, especially for acute treatments such as arthroplasty and arthroscopy. Patient choices increasingly benefit from price transparency3, the inclusion of patient-reported outcomes in quality measurement4, and mechanisms to encourage shared decision-making with physicians5. Patients also are facing greater cost sharing at the time of receiving care, in part as an encouragement to select lower-priced providers. Some employers and insurers are establishing reference-based benefits that require the patient to pay the difference between a defined contribution limit and the price actually charged, if a higher-priced facility is chosen6-8. Reference-based benefits often are referred to as reference pricing9. Previous research has documented strong associations between reference-based benefit designs and consumer choices and spending for inpatient knee and hip arthroplasty10 as well as for drugs11,12, laboratory tests13, and cataract removal1.
Materials and Methods
Data on Patients
Insurance claims data were obtained for patients undergoing shoulder or knee arthroscopy who were enrolled in the self-insured health benefits plan maintained by the California Public Employees’ Retirement System (CalPERS) between January 2009 and December 2013. CalPERS covers 1.3 million individuals, of whom 450,000 are enrolled in its self-insured Preferred Provider Organization (PPO) product. A control group was obtained consisting of all enrollees covered by Anthem Blue Cross insurance who underwent arthroscopy during these five years in California but who were not subject to reference-based benefits.
In January 2012, CalPERS shifted to reference-based benefits for arthroscopy, building on its reference-based benefit program for inpatient knee and hip replacement surgery10,14. All enrollees in the CalPERS PPO insurance faced deductible and coinsurance requirements. Under its reference-based benefit initiative, CalPERS continued to pay the facility’s allowed charge, subject to these deductible and coinsurance provisions, if the patient selected an ambulatory surgery center. However, for patients selecting a hospital outpatient department, CalPERS limited its payment contribution to $6000 and continued to require deductibles and coinsurance.
Patients were exempted from the reference-based benefit initiative if their surgeon presented a clinical case for needing services in a hospital outpatient department, based on patient age and comorbid conditions, or if the patient lived in a rural area more than thirty miles from an ambulatory surgery center. For patients exempted from the reference-based benefit initiative, CalPERS paid the hospital outpatient department’s allowed charge, less the standard patient’s deductible and coinsurance, and did not require the patient to pay the difference between the hospital outpatient department price and the $6000 reference-based benefit contribution limit.
The measured characteristics of the patients included age, sex, and the diagnostic and procedure codes according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)15 from claims incurred for all purposes, not merely arthroscopic procedures. The diagnostic and procedure codes were used to develop a measure of patient health status and comorbidities with use of the Charlson Comorbidity Index16. The study population was limited to adults under the age of sixty-five years. All physician office visit, inpatient, outpatient, emergency department, and ambulatory service claims were included in the analysis.
Our measure of procedure price was the allowed charge negotiated between the payer and the facility and actually paid to the facility. We did not use the facility’s billed charge, which is typically much higher than the allowed charge and is not actually paid.
The rates of surgical complications were calculated for thirty and ninety days after the arthroscopy date. The measurement period for some types of complications was limited to thirty days so as not to attribute to the arthroscopy adverse events due to other causes. Complications measured only for thirty days after the procedure consisted of bleeding (ICD-9-CM codes 39.98, 719.10, 719.16, 719.17, and 998.1), postoperative deep vein thrombosis (ICD-9-CM codes 453.40-453.42, 453.50-453.52, and 453.9), and pulmonary embolism (ICD-9-CM code 415.1). Complications measured for the full ninety days after the procedure consisted of mechanical failure (ICD-9-CM codes 996.4, 996.40, and 996.49), wound infection (ICD-9-CM codes 682.1-682.9, 686.9, 996.66, 996.67, 998.3, 998.5, 998.6, 998.7, and 998.83 and Current Procedural Terminology [CPT] codes 00.70-00.73, 00.80-00.82, 00.84, 80.05, 80.06, 80.09, 81.53, 81.55, 81.59, 86.04, 86.22, and 86.28), and postoperative nerve injury (ICD-9-CM codes 955, 956, 957.8, and 957.9).
Analytic Methods
We analyzed trends in facility choice, prices paid, employer spending, and clinical complications for the three years prior and the two years subsequent to reference-based benefit implementation.
For each year before and after implementation of reference-based benefits, we calculated the percentage of patients selecting an ambulatory surgery center, the percentage of patients selecting a hospital outpatient department, the mean price paid per procedure, and the rate of complications. These calculations were made for CalPERS and Anthem patients separately. We then conducted multivariable difference-in-differences regressions with use of the individual patient as the unit of observation. These regressions analyze the association between the implementation of the reference-based benefit and facility choice, prices, and complications after adjusting for changes in demographic characteristics, comorbidities, and other factors over the five-year period. Covariates in the regression analyses included year, payer (CalPERS compared with Anthem), interaction terms between year and payer, an indicator variable for whether the patient was exempted from the reference-based benefit initiative because of clinical or geographic considerations, the Charlson Comorbidity Index, patient age categories, patient sex, and indicators for each hospital referral region17.
Difference-in-differences analysis, which is commonly used to identify causal effects in observational studies, uses the same analytic logic that is used in clinical trials featuring a treatment and a comparison group. There are two differences that are computed with respect to the outcome variable of interest: the mean change over time in the outcome of the treatment group and the mean change over time in the comparison group; the difference in differences is the difference between the mean change over time in the outcome in the treatment group and the mean change over time in the comparison group. The difference in differences reflects the extent to which the treatment group differs from the comparison group in the post-treatment period, compared with the extent to which the treatment group differs from the comparison group in the pre-treatment period18.
The regression parameters for the probability of selecting an ambulatory surgery center and the probability of complications were estimated with use of both linear probability and logistic regression, as the dependent variables are dichotomous. The two models generated similar results. For easier interpretation, we reported the linear probability model results. All analyses were performed with use of Stata 11.0 (StataCorp, College Station, Texas) and all standard errors were clustered at the provider level and were robust to heteroskedasticity19. The study was approved by the institutional review board at the University of California, Berkeley.
Source of Funding
The authors received support for this research through a research contract from the California Public Employees Retirement System (CalPERS) and a grant (RO1 HS022098) from the Agency for Healthcare Research and Quality (AHRQ).
Results
Trends in Choice, Payments, and Complications
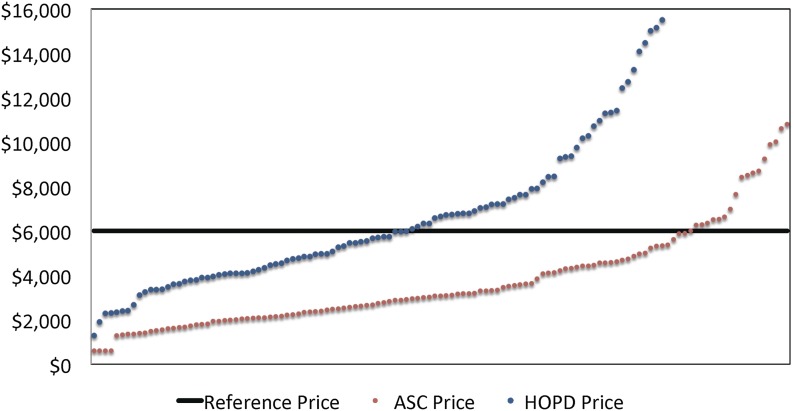
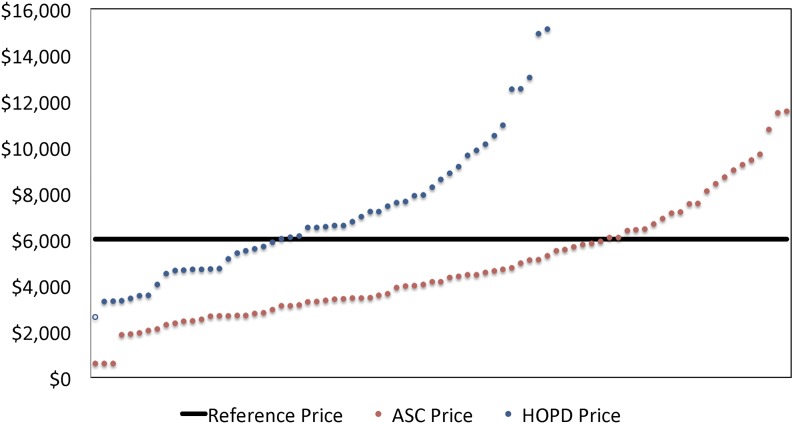
Figures 1 and 2 present the distribution of prices (allowed charges) for arthroscopy across ambulatory surgery centers and hospital outpatient departments in 2011, the year prior to the implementation of reference-based benefits by CalPERS. The wide variability of prices was the main impetus for the shift to reference-based benefits by CalPERS. The median price for knee arthroscopy was $5668 (range, $1280 to $15,503) for the hospital outpatient departments and $3083 (range, $604 to $10,803) for the ambulatory surgery centers. The median price for shoulder arthroscopy was $6522 (range, $2618 to $15,130) for the hospital outpatient departments and $4153 (range, $605 to $11,549) for the ambulatory surgery centers.
Fig. 1.
Distribution of the prices in hospital outpatient departments (HOPD) and freestanding ambulatory surgery centers (ASC) prior to implementation of reference-based benefits: knee arthroscopy.
Fig. 2.
Distribution of the prices in hospital outpatient departments (HOPD) and freestanding ambulatory surgery centers (ASC) prior to implementation of reference-based benefits: shoulder arthroscopy.
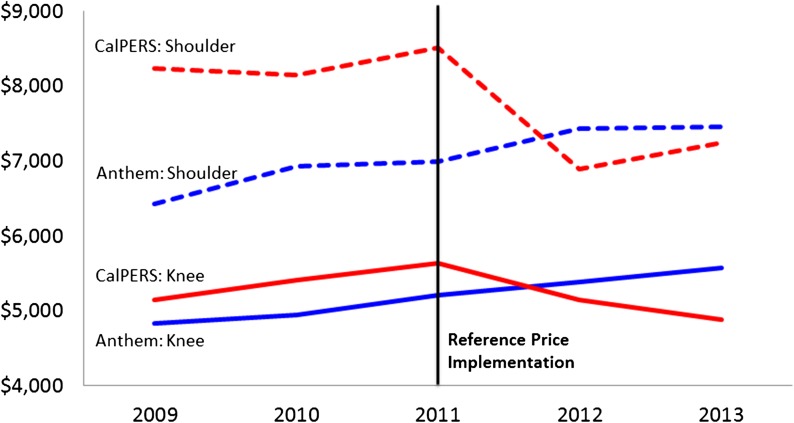
Figure 3 presents the percentage of CalPERS and Anthem enrollees selecting an ambulatory surgery center (as distinct from a hospital outpatient department) for their procedure in each year. From 2009 to 2011, prior to implementation of reference-based benefits, the share of CalPERS members who underwent a knee arthroscopy at an ambulatory surgery center remained unchanged at approximately 60%. After the reference-based benefit implementation, the share of members selecting an ambulatory surgery center increased to 82%. For Anthem enrollees not subject to reference-based benefits, the use of an ambulatory surgery center remained unchanged at approximately 66% during the entire period. The bivariate difference between CalPERS and Anthem enrollees in use of an ambulatory surgery center changed by 22 percentage points, from 5 percentage points lower for CalPERS than Anthem in 2009 to 17 percentage points higher in 2013. Similar differences are evident in Figure 3 for shoulder arthroscopy.
Fig. 3.
Line graph showing the percentage of patients selecting ambulatory surgery centers instead of hospital outpatient departments before and after implementation of reference-based benefits: knee and shoulder arthroscopy.
Figure 4 presents the mean prices (allowed charges) paid per procedure between 2009 and 2013 by CalPERS and Anthem for the two forms of arthroscopy. Prior to reference-based benefit implementation, the mean prices paid by CalPERS were higher than prices paid by Anthem, because of the concentration of public employees in the state capital of Sacramento. Health-care market consolidation in Sacramento has fostered high prices20. In the year after the reference-based benefit implementation, the mean price charged to CalPERS declined by 8.8% for knee arthroscopy and by 19.0% for shoulder arthroscopy, although it continued to rise by 3.3% for knee arthroscopy and by 6.4% for shoulder arthroscopy for Anthem. The mean price charged to CalPERS patients in 2013 was 12.3% below that charged to Anthem enrollees for knee arthroplasty and 2.8% below that charged for shoulder arthroscopy.
Fig. 4.
Line graph showing the total payment before and after implementation of reference-based benefits: knee and shoulder arthroscopy.
Figure 5 presents the 2009 to 2013 rates of complications during the ninety days after the arthroscopy. The rates of complications for CalPERS members declined in the first year after the reference-based benefit implementation and then rose in the second year, but the differences were small. The rates of complications did not change over time for the Anthem members.
Fig. 5.
Line graph showing the ninety-day complication rates before and after implementation of reference-based benefits: knee and shoulder arthroscopy.
Multivariable Statistical Analyses
Tables I and II present descriptive statistics on the patients and procedures included in the study. Tables III and IV present difference-in-differences regression analyses of the association between reference-based benefits and ambulatory surgery center choice, procedure prices, and surgical complications for arthroscopy of the knee and shoulder.
TABLE I.
Knee Arthroscopy Descriptive Characteristics
| 2009 | 2010 | 2011 | 2012 | 2013 | |
| CalPERS | |||||
| No. of procedures | 884 | 856 | 953 | 828 | 808 |
| Performed at ambulatory surgery center | 529 | 532 | 593 | 559 | 598 |
| Performed at hospital outpatient department: not exempt | 355 | 324 | 360 | 186 | 131 |
| Performed at hospital outpatient department: exempt | 0 | 0 | 0 | 83 | 79 |
| Procedure payment* | $5146 | $5412 | $5638 | $5395 | $5402 |
| Hospital outpatient departments* | $6717 | $7016 | $7565 | $6640 | $7534 |
| Ambulatory surgery centers* | $4092 | $4435 | $4469 | $4795 | $4653 |
| Charlson Comorbidity Index score* | 0.3 | 1.2 | 1 | 0.1 | 0.7 |
| Male patients | 47.70% | 47.40% | 46.80% | 46.60% | 49.90% |
| Patient age* (yr) | 50.7 | 50.6 | 50.2 | 50.3 | 50.7 |
| Ninety-day complications | |||||
| Complication rate* | 1.92% | 1.40% | 1.89% | 1.69% | 2.48% |
| No. of complications | 17 | 12 | 18 | 14 | 20 |
| Anthem | |||||
| No. of procedures | 7997 | 7830 | 7667 | 7925 | 8347 |
| Performed at ambulatory surgery center | 2824 | 2658 | 2541 | 2616 | 2913 |
| Performed at hospital outpatient department | 5173 | 5172 | 5126 | 5309 | 5434 |
| Procedure payment* | $4824 | $4946 | $5205 | $5378 | $5568 |
| Hospital outpatient departments* | $6380 | $7056 | $7158 | $7139 | $7409 |
| Ambulatory surgery centers* | $3975 | $3862 | $4236 | $4510 | $4581 |
| Charlson Comorbidity Index score* | 0.8 | 0.6 | 0.6 | 0.7 | 0.6 |
| Male patients | 58.30% | 57.00% | 57.10% | 56.40% | 57.00% |
| Patient age* (yr) | 45.8 | 46.4 | 46.2 | 46.1 | 46.3 |
| Ninety-day complications | |||||
| Complication rate* | 1.90% | 1.86% | 1.71% | 1.83% | 1.76% |
| No. of complications | 152 | 146 | 131 | 145 | 147 |
The values are given as the mean.
TABLE II.
Shoulder Arthroscopy Descriptive Characteristics
| 2009 | 2010 | 2011 | 2012 | 2013 | |
| CalPERS | |||||
| No. of procedures | 432 | 433 | 404 | 456 | 413 |
| Performed at ambulatory surgery center | 266 | 239 | 245 | 291 | 293 |
| Performed at hospital outpatient department: not exempt | 166 | 194 | 159 | 97 | 56 |
| Performed at hospital outpatient department: exempt | 0 | 0 | 0 | 68 | 64 |
| Procedure payment* | $8233 | $8146 | $8504 | $7626 | $8657 |
| Hospital outpatient departments* | $10,955 | $10,059 | $11,837 | $9361 | $11,808 |
| Ambulatory surgery centers* | $6534 | $6594 | $6340 | $6642 | $7367 |
| Charlson Comorbidity Index score* | 2.1 | 0.5 | 0.5 | 0.7 | 0.2 |
| Male patients | 56.50% | 57.50% | 57.20% | 52.60% | 55.00% |
| Patient age* (yr) | 53.1 | 52.1 | 53 | 53.3 | 52.6 |
| Ninety-day complications | |||||
| Complication rate* | 1.39% | 1.39% | 0.99% | 0.44% | 0.73% |
| No. of complications | 6 | 6 | 4 | 2 | 3 |
| Anthem | |||||
| No. of procedures | 3634 | 3588 | 3458 | 3602 | 3743 |
| Performed at ambulatory surgery center | 1425 | 1368 | 1272 | 1318 | 1309 |
| Performed at hospital outpatient department | 2209 | 2220 | 2186 | 2284 | 2434 |
| Procedure payment* | $6420 | $6925 | $6984 | $7430 | $7449 |
| Hospital outpatient departments* | $8158 | $9298 | $9247 | $9483 | $9323 |
| Ambulatory surgery centers* | $5298 | $5463 | $5667 | $6245 | $6440 |
| Charlson Comorbidity Index score* | 1 | 1.1 | 0.5 | 0.6 | 1 |
| Male patients | 61.50% | 62.40% | 60.50% | 60.90% | 61.80% |
| Patient age* (yr) | 48.7 | 48.9 | 49.6 | 49.6 | 49.9 |
| Ninety-day complications | |||||
| Complication rate* | 1.13% | 0.84% | 1.01% | 1.05% | 0.83% |
| No. of complications | 41 | 30 | 35 | 38 | 31 |
The values are given as the mean.
TABLE III.
Knee Arthroscopy Multivariable Regression Results*
| Probability of Selecting Ambulatory Surgery Center | Procedure Price Paid (Percent Difference) | Procedure Price Paid (Dollar Difference) | Probability of Ninety-Day Complication | |
| CalPERS × 2013 | 0.143† ± 0.0317 | −17.61† ± 4.850 | −1009† ± 261.0 | 0.00236 ± 0.00773 |
| CalPERS × 2012 | 0.0568‡ ± 0.0232 | −11.45‡ ± 4.926 | −633.6‡ ± 260.6 | −0.00509 ± 0.00588 |
| CalPERS × 2010 | 0.0219 ± 0.0264 | 3.978 ± 4.916 | 203.2 ± 247.7 | −0.00594 ± 0.00609 |
| CalPERS × 2009 | −0.0110 ± 0.0244 | 3.195 ± 4.159 | 163.8 ± 212.3 | −0.00125 ± 0.00690 |
| CalPERS | −0.0408§ ± 0.0217 | 3.586 ± 3.463 | 183.5 ± 177.1 | 0.00130 ± 0.00427 |
| 2013 | −0.0224 ± 0.0170 | 9.673† ± 2.833 | 481.0† ± 145.9 | 0.000442 ± 0.00210 |
| 2012 | −0.00322 ± 0.0113 | 3.677 ± 2.476 | 188.1 ± 127.9 | 0.00112 ± 0.00227 |
| 2011 | Reference | Reference | Reference | Reference |
| 2010 | −0.00767 ± 0.0118 | −5.486† ± 2.190 | −293.9† ± 111.9 | 0.00131 ± 0.00221 |
| 2009 | −0.0228 ± 0.0170 | −8.017† ± 2.814 | −435.3† ± 146.3 | 0.00173 ± 0.00222 |
| Male patients | 0.00507 ± 0.00587 | −0.0426 ± 0.945 | −2.219 ± 48.97 | 0.00373† ± 0.00143 |
| Charlson Comorbidity Index | −0.241† ± 0.0367 | 10.24‡ ± 4.061 | 507.6‡ ± 212.2 | 0.0202§ ± 0.0112 |
| Age in years | ||||
| 30 to 39 | −0.0164 ± 0.0117 | −14.07† ± 2.739 | −953.7† ± 175.3 | 0.00747‡ ± 0.00306 |
| 40 to 49 | −0.00101 ± 0.0154 | −24.95† ± 2.881 | −1692† ± 184.7 | 0.00421§ ± 0.00221 |
| 50 to 59 | 0.00646 ± 0.0166 | −30.94† ± 2.832 | −2098† ± 192.7 | 0.00275 ± 0.00203 |
| 60 to 64 | −0.00541 ± 0.0179 | −31.14† ± 2.845 | −2111† ± 187.6 | 0.00883† ± 0.00252 |
The values are given as the mean and the standard error based on 44,068 observations in each group.
Significant at p < 0.01.
Significant at p < 0.05.
Not significant at p < 0.1.
TABLE IV.
Shoulder Arthroscopy Multivariable Regression Results*
| Probability of Selecting Ambulatory Surgery Center | Procedure Price Paid (Percent Difference) | Procedure Price Paid (Dollar Difference) | Probability of Ninety-Day Complication | |
| CalPERS × 2013 | 0.0995† ± 0.0343 | −17.02‡ ± 8.549 | −1336‡ ± 605.9 | 0.000999 ± 0.00700 |
| CalPERS × 2012 | 0.0444 ± 0.0320 | −21.87† ± 7.447 | −1768† ± 547.6 | −0.00493 ± 0.00654 |
| CalPERS × 2010 | −0.0219 ± 0.0308 | −0.718 ± 5.346 | −51.64 ± 373.3 | 0.00638 ± 0.00793 |
| CalPERS × 2009 | 0.0382 ± 0.0318 | 3.144 ± 7.493 | 221.8 ± 517.5 | 0.00302 ± 0.00798 |
| CalPERS | −0.0401§ ± 0.0235 | 9.999‡ ± 4.162 | 682.7‡ ± 294.8 | −0.00150 ± 0.00532 |
| 2013 | 0.00810 ± 0.0260 | 9.111‡ ± 4.082 | 624.6‡ ± 281.9 | −0.00198 ± 0.00218 |
| 2012 | −0.00249 ± 0.0180 | 6.554‡ ± 3.059 | 454.8‡ ± 213.8 | 0.000447 ± 0.00242 |
| 2011 | Reference | Reference | Reference | Reference |
| 2010 | −0.0158 ± 0.0151 | −1.547 ± 2.591 | −111.7 ± 183.5 | −0.00187 ± 0.00228 |
| 2009 | −0.0322 ± 0.0212 | −8.424† ± 3.302 | −630.4† ± 242.0 | 0.00144 ± 0.00242 |
| Male patients | −0.00362 ± 0.00771 | 8.332† ± 1.550 | 573.3† ± 119.0 | 0.00138 ± 0.00143 |
| Charlson Comorbidity Index | −0.238† ± 0.0570 | 12.55§ ± 7.239 | 846.8§ ± 500.5 | 0.00128 ± 0.00639 |
| Age in years | ||||
| 30 to 39 | −0.0373§ ± 0.0207 | −0.105 ± 4.086 | −6.807 ± 260.7 | 8.23×10-5 ± 0.00270 |
| 40 to 49 | −0.0230 ± 0.0224 | 6.955§ ± 3.697 | 452.9§ ± 241.5 | 0.00142 ± 0.00224 |
| 50 to 59 | −0.0196 ± 0.0230 | 11.60† ± 3.530 | 755.6† ± 233.3 | 0.00508‡ ± 0.00217 |
| 60 to 64 | −0.0317 ± 0.0235 | 18.53† ± 3.933 | 1206† ± 277.9 | 0.00864† ± 0.00274 |
The values are given as the mean and the standard error based on 20,142 observations in each group.
Significant at p < 0.01.
Significant at p < 0.05.
Not significant at p < 0.1.
Tables III and IV present results from multivariable difference-in-differences regressions. Each table presents regressions with four outcome variables: choice of ambulatory surgery center (compared with hospital outpatient department), price measured in logarithmic units, price measured in dollar units, and surgical complications within ninety days of the original arthroscopy.
The difference-in-differences models were tested for violations of the parallel trends assumption via the 2009 and 2010 interaction terms18,21. The regressions for procedure prices used a generalized linear model with a log-link and a gamma distribution, because the dependent variables are continuous22. Park tests supported using a gamma distribution23.
The multivariable analyses generate an estimate of reference-based benefit impact on selection of an ambulatory surgery center instead of a hospital outpatient department that is similar in magnitude to the bivariate estimates presented in Figure 4. As indicated in the Probability of Selecting Ambulatory Surgery Center column of Table III, the shift by CalPERS to reference-based benefits was associated with an increase in the probability of ambulatory surgery center utilization by 5.7 percentage points (95% confidence interval [95% CI], 1.1 to 10.2 percentage points; p < 0.05) in 2012 and by 14.3 percentage points (95% CI, 8.1 to 20.5 percentage points; p < 0.001) in 2013, compared with the probability of utilization by Anthem enrollees.
The changes in the prices paid for knee arthroscopy are presented in percentage terms in the Procedure Price Paid (Percent Difference) column of Table III. The mean price paid fell in the first year after implementation of reference-based benefits by −11.5% (95% CI, −19.4% to −2.7%; p = 0.01), controlling for other relevant factors. The prices paid in the second year after reference-based benefit implementation were lower than those paid prior to implementation by 17.6% (95% CI, −24.9% to −9.6%; p < 0.001).
Knee arthroscopy prices are analyzed in dollar terms in the Procedure Price Paid (Dollar Difference) column of Table III. The multivariable analyses generate an estimate of the reference-based benefit impact that is similar in magnitude to the bivariate estimates presented in Figure 5. In 2012, procedure payments for CalPERS enrollees were $634 less per procedure (95% CI, −$1144 to −$121; p = 0.01) than for Anthem enrollees, after adjusting for other relevant factors. The prices paid continued to decrease in the second year after implementation and in 2013 were below 2011 levels by $1009 (95% CI, −$1520 to −$597; p < 0.001).
As indicated in the Probability of Ninety-Day Complication column of Table III, the multivariable statistical analyses found no significant association between implementation of reference-based benefits and the probability of a surgical complication. The multivariable results thus are similar to the bivariate results presented in Figure 5.
Table IV presents analogous multivariable regression analyses for shoulder arthroscopy. As indicated in the Probability of Selecting Ambulatory Surgery Center column of Table IV, the shift by CalPERS to reference-based benefits was associated with an increase in the probability of ambulatory surgery center utilization by 4.4 percentage points (95% CI, −1.8 to 10.7 percentage points; p = 0.16) in 2012 and by 9.9 percentage points (95% CI, 3.2 to 16.7 percentage points; p < 0.01) in 2013, after controlling for differences in patient demographic characteristics, comorbidities, and other factors.
In Table IV, the changes in the prices paid for shoulder arthroscopy are presented in percentage terms in the Procedure Price Paid (Percent Difference) column and in dollar terms in the Procedure Price Paid (Dollar Difference) column. In the first year after implementation of reference-based benefits, the mean price paid fell by 21.9% (95% CI, −32.1% to −10.1%; p < 0.001), controlling for other relevant factors. Prices paid remained decreased in the second year after implementation and in 2013 were below 2011 levels by $1336 (95% CI, −$2524 to −$149; p = 0.03), which is equivalent to a 17.0% (95% CI, −29.3% to −2.5%) reduced payment per procedure. As indicated in the Probability of Ninety-Day Complication column of Table IV, the multivariable statistical analyses found no significant association between the implementation of the reference-based benefit and the probability of a surgical complication for shoulder arthroscopy.
Discussion
Employers, insurers, governmental programs, and individuals who pay for health care face wide variation in the prices charged for similar services. As illustrated in Figures 1 and 2, the prices charged to CalPERS for arthroscopy ranged more than tenfold. Negotiated rates for hospital-based outpatient departments exceeded those charged by freestanding centers by a mean of 73% ($2714) for knee arthroplasty and 48% ($2262) for shoulder arthroplasty. Medicare also pays substantially more for ambulatory procedures if they occur in a hospital outpatient department than if they occur in a freestanding ambulatory surgery center2,24.
The findings of this study should be interpreted in light of its limitations. The data reflected the experience of working-age individuals covered by employment-based health insurance and may not have been generalizable to an older, Medicare-eligible population.
We were not able to measure whether implementation of reference-based benefits influenced the propensity of CalPERS members to undergo an arthroscopy, as we did not have data on age-adjusted total CalPERS enrollment. There is no strong reason to assume that the reference-based benefit initiative would affect the probability of undergoing a procedure, as the patient faced no reference-based benefit-related cost sharing at any ambulatory surgery center. The patient also faced no reference-based benefit-related cost sharing at a hospital outpatient department if the treating physician indicated a clinical reason for needing hospital-based care or if the patient resided in a geographic area without convenient access to an ambulatory surgery center.
Our measures of patient outcomes were limited to complications reported on inpatient, outpatient, emergency department, or physician office visit claims within ninety days after the arthroscopy. Our ninety-day window for complications was consistent with the global outcomes measurement period used for most shoulder and knee arthroscopic procedures25. We did not have access to patient-reported outcome measures, which were not collected by CalPERS or Anthem. Future research should include patient-reported outcomes wherever possible.
Reference-based benefit designs represent a strategy by employers and insurers to counter variable health-care pricing that cannot be justified by differences in quality or outcomes. The employer or insurer establishes a limit to what it will contribute toward payment for a procedure, requiring the patient to pay the difference between this limit and what the provider actually charges. The contribution limit is established at a level sufficiently high to ensure access at a sufficient number of facilities in each geographic region. Patients who need to use a high-priced provider for special clinical reasons or who live in a remote rural area are exempted from the reference-based benefit cost sharing.
As documented in this study, patients requiring an arthroscopy of the knee or shoulder respond strongly to the economic incentives embodied in reference-based benefit designs. Use of the lower-priced ambulatory surgery centers by CalPERS members grew substantially after the implementation of reference-based benefits, although Anthem enrollees not subject to reference-based benefits did not change their facility choices. The shift toward freestanding ambulatory surgery centers reduced CalPERS spending in the first two years after reference-based benefit implementation by $2.3 million (13%), compared with what it would have spent on these two procedures in the absence of the new benefit design. These reduced payments were not accompanied by any increased rates of procedural complications.
The consumer is being accorded an ever-greater decision-making role in the U.S. health-care system, especially for acute interventions such as orthopaedic surgery. Patient-reported experience and outcomes increasingly are being included in quality measurements and rewards26. Physicians and patients are being encouraged to engage in shared decision-making with respect to treatment options5. Health plans and independent technology vendors are making available information on price and quality at the level of the individual provider and procedure3,27.
Patients are being asked to pay a substantial portion of the cost of the services that they select. In much of the non-health economy, the value of a product or service is the amount that the consumer is willing to pay for it, given the consumer’s expectations of performance. This definition of value now is being applied to musculoskeletal health care as well.
Footnotes
Investigation performed at the University of California, Berkeley, California
A commentary by Kern Singh, MD, and Junyoung Ahn, BS, is linked to the online version of this article at jbjs.org.
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality (AHRQ). California Public Employees’ Retirement System (CalPERS) and AHRQ played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Robinson JC, Brown T, Whaley C. Reference-based benefit design changes consumers’ choices and employers’ payments for ambulatory surgery. Health Aff (Millwood). 2015. March 1;34(3):415-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassidy A. Site-neutral payments: Medicare uses different payment methods depending on where care is delivered. Recent proposals seek to eliminate this differential. Health Affairs. 2014. July 24 http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=121. Accessed 2014 Nov 26. [Google Scholar]
- 3.Whaley C, Schneider Chafen J, Pinkard S, Kellerman G, Bravata D, Kocher R, Sood N. Association between availability of health service prices and payments for these services. JAMA. 2014. October 22-29;312(16):1670-6. [DOI] [PubMed] [Google Scholar]
- 4.SooHoo NF, Li Z, Chenok KE, Bozic KJ. Responsiveness of patient reported outcome measures in total joint arthroplasty patients. J Arthroplasty. 2015. February;30(2):176-91. Epub 2014 Oct 2. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Belkora J, Chan V, Youm J, Zhou T, Dupaix J, Bye AN, Braddock CH 3rd, Chenok KE, Huddleston JI 3rd. Shared decision making in patients with osteoarthritis of the hip and knee: results of a randomized controlled trial. J Bone Joint Surg Am. 2013. September 18;95(18):1633-9. [DOI] [PubMed] [Google Scholar]
- 6.Robinson JC, MacPherson K. Payers test reference pricing and centers of excellence to steer patients to low-price and high-quality providers. Health Aff (Millwood). 2012. September;31(9):2028-36. [DOI] [PubMed] [Google Scholar]
- 7.Fronstin P, Roebuck C. Reference pricing for health care services: a new twist on the defined contribution concept in employment-based health benefits. Employee Benefit Research Institute Brief. 2014: 398. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=2428270##. Accessed 2015 May 20. [Google Scholar]
- 8.Melton LD, Bradley K, Fu PL, Armata R, Parr JB. Reference-based pricing: an evidence-based solution for lab services shopping. Am J Manag Care. 2014. December;20(12):1033-40. [PubMed] [Google Scholar]
- 9.Shih T, Dimick JB. Is reference pricing the next big thing in payment reform? JAMA Surg. 2014. December;149(12):1219-20. [DOI] [PubMed] [Google Scholar]
- 10.Robinson JC, Brown TT. Increases in consumer cost sharing redirect patient volumes and reduce hospital prices for orthopedic surgery. Health Aff (Millwood). 2013. August;32(8):1392-7. [DOI] [PubMed] [Google Scholar]
- 11.Lee JLY, Fischer MA, Shrank WH, Polinski JM, Choudhry NK. A systematic review of reference pricing: implications for US prescription drug spending. Am J Manag Care. 2012. November;18(11):e429-37. [PubMed] [Google Scholar]
- 12.Galizzi MM, Ghislandi S, Miraldo M. Effects of reference pricing in pharmaceutical markets: a review. Pharmacoeconomics. 2011. January;29(1):17-33. [DOI] [PubMed] [Google Scholar]
- 13.Melton LD, Bradley K, Fu PL, Armata R, Parr JB. Reference-based pricing: an evidence-based solution for lab services shopping. Am J Manag Care. 2014. December;20(12):1033-40. [PubMed] [Google Scholar]
- 14.Lechner A, Gourevitch R, Ginsburg P. The potential of reference pricing to generate health care savings: lessons from a California pioneer. Center for Studying Health System Change. HSC Research Brief. 2013: 30. http://www.hschange.org/CONTENT/1397/. Accessed 2015 May 20. [Google Scholar]
- 15.Centers for Disease Control and Prevention, National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). 2013 Jun 18: 30. http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed 2015 Jun 2. [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. [DOI] [PubMed] [Google Scholar]
- 17.Trustees of Dartmouth College. Data by region. Dartmouth atlas of health care. 2015. http://www.dartmouthatlas.org/data/region/. Accessed 2015 May 22. [Google Scholar]
- 18.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014. December 10;312(22):2401-2. [DOI] [PubMed] [Google Scholar]
- 19.Wooldridge J. Econometric analysis of cross section and panel data. 2nd ed. Cambridge, MA: MIT Press; 2010. [Google Scholar]
- 20.Tu H, Felland L, Ginsburg PB, Liebhaber A, Cohen G, Kemper N. Sacramento: powerful hospital systems dominate a stable market. California Healthcare Almanac. 2009. July http://www.chcf.org/∼/media/MEDIA%20LIBRARY%20Files/PDF/A/PDF%20AlmanacRegMktBriefSacramento09.pdf. Accessed 2015 May 20. [Google Scholar]
- 21.Ryan AM, Burgess JF Jr, Dimick JB. Why we should not be indifferent to specification choices for difference-in-differences. Health Serv Res. 2014. December 11 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manning WG. The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ. 1998. June;17(3):283-95. [DOI] [PubMed] [Google Scholar]
- 23.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001. July;20(4):461-94. [DOI] [PubMed] [Google Scholar]
- 24.Medicare Payment Advisory Commission. Site-neutral payments for select conditions treated in inpatient rehabilitation facilities and skilled nursing facilities. Report to the congress: Medicare and the health care delivery system. Chapter 6. 2014. http://medpac.gov/documents/reports/jun14_entirereport.pdf?sfvrsn=0. Accessed 2015 May 20.
- 25.Wisconsin Physicians Service Insurance Corporation. 90 day global period calculator for major surgeries. 2015. http://www.wpsmedicare.com/j5macpartb/claims/claims-tools/globalperiod_calculators.shtml. Accessed 2015 May 22.
- 26.Bozic KJ, Grosso LM, Lin Z, Parzynski CS, Suter LG, Krumholz HM, Lieberman JR, Berry DJ, Bucholz R, Han L, Rapp MT, Bernheim S, Drye EE. Variation in hospital-level risk-standardized complication rates following elective primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2014. April 16;96(8):640-7. [DOI] [PubMed] [Google Scholar]
- 27.Wu SJ, Sylwestrzak G, Shah C, DeVries A. Price transparency for MRIs increased use of less costly providers and triggered provider competition. Health Aff (Millwood). 2014. August;33(8):1391-8. [DOI] [PubMed] [Google Scholar]