Abstract
Background:
A diagnostic tool designed as part of a telepsychiatry application for diagnosis and management of child and adolescent psychiatric disorders in India was developed considering the paucity of trained child psychiatrists and mental health professionals in India.
Materials and Methods:
The diagnostic tool consisted of screening and 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) criteria-based diagnostic algorithms for 18 psychiatric disorders seen in childhood and adolescence. Accuracy of diagnoses and feasibility of use of the tool was examined by comparing it with detailed semi-structured clinical evaluations by a qualified psychiatrist with 50 psychiatric patients (children and adolescents).
Statistical Analysis:
Descriptive analyses and paired t-tests were conducted to compare the mean number of diagnosis generated by the two interviews. Sensitivity, specificity, positive and negative predictive values were computed for the screening and the diagnostic sub-modules of the tool, compared to the clinical diagnoses. Kappa coefficients were computed to assess agreement between the diagnoses generated by the diagnostic sub-module and the clinical diagnoses.
Results:
The screening sub-module had high sensitivity, high specificity and negative predictive values for all disorders. For the diagnostic sub-module, there was moderate (kappa-0.4–0.6) to substantial agreement (kappa > 0.6) for all the disorders, (except psychosis) and high sensitivity (barring a few disorders) and specificity for almost all the disorders. Positive predictive values were found to be acceptable to high for most disorders, with consistently high negative predictive values.
Conclusion:
The new tool was found to be comprehensive, reasonably short and feasible. Results showed acceptable level of accuracy in diagnosis generated by the tool.
Keywords: Adolescent, child, diagnosis, psychiatric disorders, telepsychiatry
INTRODUCTION
Child and adolescent mental health problems are common, persistent, distressing and disabling all over the world.[1] The World Health Report suggests a worldwide prevalence of mental disorders in children and adolescents as about 20%.[2] In India too, this rate is estimated between 7-20%.[3]
About 41% (approximately 490 million) of the population in India consists of children and adolescents.[4] Considering a conservative prevalence rate of 10%, over 50 million children suffer from mental health problems. In addition to these huge numbers, mental illnesses in children and adolescents differ in many ways from those of adults, in terms of psychopathological patterns, methods of assessments, co-morbidities and response to treatment. Thus, specific training in diagnosing and managing these disorders is essential.[1] However, there are only a handful of trained child psychiatrists in India and there were no child psychiatry training centres till about a couple of years ago. Main burden of care for children's mental disorders in India lies on general adult psychiatrists or paediatricians who have practically no training in child psychiatry in India. There is a huge deficiency in the number of trained professionals needed to meet the mental health needs of children and adolescents in low- and middle-income countries.[5] Moreover, most of these professionals are settled in urban areas or work in private hospitals, further widening the gap between demand for child psychiatric care and the supply of mental health services for children and adolescents.
One of the strategies to overcome this mental health gap is integration of child mental health services with primary and general healthcare.[6] Even though efforts have been underway in India to reduce the mental health gap under the aegis of the National Mental Health Programme by strengthening existing resources, developing new ones and enhancing manpower,[6,7] but these have not succeeded to give the desired results on account of several practical difficulties in implementation of these conventional measures which have long gestation period and require huge amount of resources. There is need for alternative and innovative programmes that can support both training as well as service needs. One strategy could be the utilization of advancements in information and communication technology to further mental healthcare in India, by developing telepsychiatry services. Telepsychiatry programmes are being increasingly used in developed nations, but the focus of such programmes is usually on direct patient management by psychiatrists through the medium of video-conferencing.[8] However, in developing countries like India, such an approach would burden the existing and already deficient specialized workforce and, thus, would not be suitable. Instead, it would be more fruitful to develop systems that empower the general psychiatrist or the paediatrician or the general physician to diagnose and treat child psychiatric disorders effectively and comprehensively, with the expert child psychiatrists providing consultation, supervision and education to mental health professionals caring for children and adolescents.[1,9,10,11] It is suggested that developing software packages with codified medical knowledge and logical decision support systems to aid assessment, diagnosis and management of psychiatric disorders in children and adolescents can serve this need. With the target to reach out to remotely set geographical areas, such a programme in India can function as a medium to address the vast ‘mental health gap’ and allow effective as well as timely management of childhood psychiatric disorders. The extension of services provided by non-specialists (medically trained physicians, psychologists, social workers) supported by child psychiatrists through this method holds the potential to provide a high-quality and effective intervention to masses even in remote areas.
This study represents an effort to develop such a net-based telepsychiatry application for diagnosis and management of common psychiatric disorders in children and adolescents, with the broader aims of codifying medical knowledge, and providing a net-based decision support system for diagnosis and treatment to be used by non-mental health practitioners. The application is designed to empower non-specialists, who shall also be provided support, supervision and consultation by child psychiatrists through synchronous and asynchronous modes of communication. The model being employed, thus, goes beyond the usual practice of direct patient management by telepsychiatric services. The Department of Psychiatry at the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh is engaged in developing a model of telepsychiatry services for the distant and remote areas in northern hill states of India where the department of psychiatry at PGIMER, Chandigarh is the nodal centre and Tata Consultancy Services (TCS) is the IT partner, while the three peripheral sites are located in the hill states of north-India constitute the distant locations to provide services. A structured diagnostic and management system for adult psychiatric patients has been developed separately and has already been reported.[12] This paper describes the development of the diagnostic tool intended for use on children and adolescents with psychiatric disorders. It also presents preliminary results on the accuracy of diagnoses generated by the tool and data on its feasibility of use by non-mental health professionals on children and adolescents with psychiatric disorders. The project was approved by the institutional ethics committee.
MATERIAL AND METHODS
Development of the diagnostic tool
Several existing and well-validated diagnostic interview schedules were reviewed for their suitability for the purpose. Many of the existing standardized structured and semi-structured diagnostic interviews specifically designed for children and adolescents such as the Schedule for Affective Disorders and Schizophrenia for School-aged Children,[13] the Child and Adolescent Psychiatric Assessment[14] and the Diagnostic Interview for Children and Adolescents[15] were found to be lengthy and required up to 2 to 3 hours to administer, as reviewed by Sheehan et al.[16] Moreover, many of these interviews had a complicated cross-checking, scoring and navigation system. Most required considerable training.
Another instrument reviewed was the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID).[16] This measure was found to be more suitable and less time-consuming than some of the other measures considered. However, it did not cover certain common childhood disorders such as specific learning disorders, mental retardation and enuresis. Early identification of the symptoms and effective diagnosis of such disorders is imperative due to the long lasting effects that might ensue in case of misdiagnosis or diagnosis after some time lapse. Due to the above cited reasons, as well as for reasons of copyright protections, it was evident that none of the existing tools could be used for our purpose. It was necessary to develop an entirely new diagnostic tool for identifying mental disorders in children and adolescents in Indian setting.
The new net-based diagnostic tool was designed to consist of a comprehensive psychiatric clinical interview, albeit with a more focused and systematic approach. A balance between an objective criteria-based diagnostic exercise as well as the freedom to conduct the interview in one's own preferred style was considered crucial. The aim was to replicate ordinary clinical encounter (as opposed to research settings) between a doctor and a patient where there is a greater need to establish a therapeutic relationship with the patient and their care givers at the very beginning of an assessment The primary purpose of this study was to develop such a comprehensive semi-structured diagnostic system, in a format, which is amenable to computerization, along with checking the feasibility of use and accuracy of diagnoses generated by the tool.
In the presently discussed version, the tool was mainly meant to be used by non-specialists (not trained in child psychiatry) namely, general psychiatrists, general physicians, paediatricians and mental health para-professionals. In keeping with these objectives, a structured format was considered appropriate. Simple and colloquial language easily understood by patients/caregivers and interviewers was used. Since clinical interview depends upon the developmental level, intellectual ability and psychological sophistication of the children/adolescents, input from their parents, school teachers and other significant people in the child's social environment contribute significantly to the diagnostic process. Considering these population-specific characteristics, commonly seen symptomatic presentations were covered in this tool using several culturally relevant examples. The interview was directed at both the child/adolescent and their caregivers, with additional questions referring to reports or complaints from other sources.
In addition, observation of the child's behaviour during the interview was also included. Diagnoses were based primarily on 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) criteria, both from the Clinical Diagnostic Guidelines[17] and the Diagnostic Criteria for Research.[18] In certain parts (e. g., the diagnosis of psychosis) Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV)[19] criteria were also incorporated. Another key feature included in the diagnostic tool was that of referrals to different specialists. Acknowledging the nuances of diagnosing childhood disorder, the diagnostic tool was designed to provide an analysis of the signs and symptoms reported and reach a provisional diagnosis accordingly. Thus, a referral to see a specialist could also be made by the tool in case of the requirement of additional and more in depth assessment. In the case of certain disorders, for example mental retardation, specific learning disorders, etc., additional and more specialized assessment is imperative for an effective diagnosis. The new diagnostic tool, therefore, allowed it's administrator to become aware of the possible diagnosis of the child and refer to a specialist in the matter for more specialized testing.
Though the original version was prepared in English, the need for a local language (Hindi) version was considered to be vital. Thus, a parallel version in Hindi was made and applied. To meet the dual objectives of a comprehensive as well as a focused evaluation, a two-stage procedure was adopted. The first stage included an initial screening of the patient for all the disorders. During this stage, the questions put forward were arranged in a way so as to cover key aspects of all the disorders included in the tool. This was followed by detailed assessment for specific disorders based on the results of the screening phase. Time taken for diagnosis was considered vital for clinical purposes and therefore, the tool was designed in a way so that the entire diagnostic interview should not exceed more than half an hour.
Flow and structure of the diagnostic tool
The diagnostic tool assesses for 19 broad categories of disorders in children and adolescents, namely, mental retardation, specific learning disability, attention deficit hyperactivity disorder, oppositional defiant disorder and conduct disorder, autism, depression, mania, psychosis, obsessive-compulsive disorder, generalized anxiety disorder, specific phobias, social anxiety disorder, separation anxiety disorder, somatoform disorder, dissociative disorder, alcohol dependence, substance use disorders and enuresis. To avoid multiple diagnoses, it includes a diagnostic hierarchy based on the exclusion criteria in the ICD-10 manual.
The diagnostic exercise follows a step-wise process in order to reach the final descriptive clinical diagnosis [Figure 1]. The interview begins, with the identification details, socio-demographic profile, presenting complaints and precipitating events being elicited and recorded. This is followed by the ‘core’ diagnostic assessment. The ‘core’ diagnostic assessment includes initial screening for all disorders and subsequent diagnostic sub-modules. The screening questionnaire contains a total of 21 items pertaining to various disorders. It acts as the first gateway to the entire diagnostic exercise and in many cases is sufficient to generate a psychiatric diagnosis. Depending upon the responses during screening, the detailed diagnostic modules open up. These modules cover detailed criteria-based questions for the specific disorders included in the tool. A key feature of the diagnostic modules is that they open in an order based on an inbuilt hierarchy. Thus, a disorder considered to be major or more severe will open first.
Figure 1.
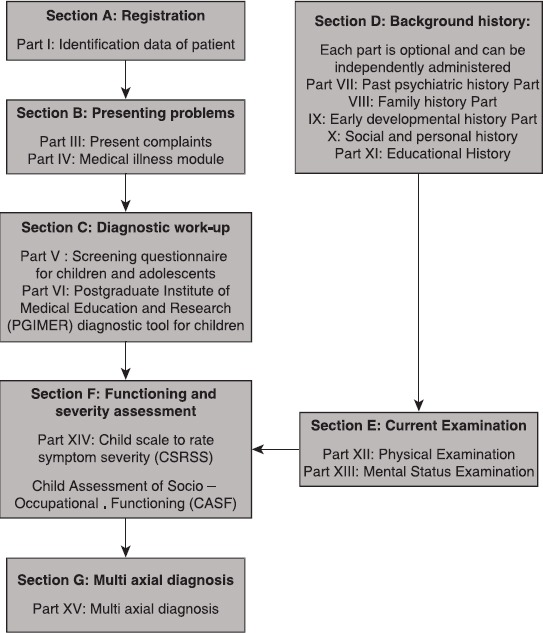
Showing the flow of the child and adolescent diagnostic tool
In each diagnostic module, there are second-level gateway questions. These questions basically enquire about the primary symptoms of the disorder. The interview proceeds with items pertaining to another criteria only if the specified threshold for the preceding one is met. It is also equipped to ‘skip’ the remaining part of the module and moves to the next module if necessary.
The ‘core’ diagnostic assessment is supplemented by ‘additional’ sections. These sections aim to include past, family, personal, developmental, medical and treatment history and physical and mental status examinations. Since such information has bearing on management, there record is included diligently. These additional sections can be used to elicit and record other significant history and the details of different specialized examination findings.
At the conclusion of the diagnostic interview with the application, the interviewer is directed to a separate segment involving the assessment of the overall functioning of the patient (social, occupational and symptom related) based on the current assessment of his/her clinical picture. To allow the assessment to be circumspect and cohesive, two separate scales were developed and included for assessment, namely, Scale to Rate Symptom Severity (SRSS) and Assessment of Socio-Occupational Functioning (ASOF). The purpose of SRSS is to allow the inclusion of a rating focusing on the level of severity associated with the symptoms the patient presents with during the assessment. The interviewer can report ratings following a 5-point scale; mild, mild-moderate, moderate, moderate-severe and severe. On the other hand, the ASOF takes into account different areas-self-care, interpersonal relations and occupational functioning. A visual analogous scale is then used to consider the pointers given against each score. For example, for ‘optimal to near optimal functioning’, the range is 8-10, as far as overall functioning is considered. During the assessment, the child and accompanying family members (parents, teachers, relatives, etc.) can be seated together for the screening as well as during the diagnostic module assessment. Questions are put forward to all the individuals involved during the interview collectively.
However, it is left to the discretion of the professional involved to interview the child alone as well. Such a scenario is especially necessary if the interviewer would like to form a more formal rapport with the child. Based on such considerations and professional discretions, information on the different levels of the assessment is collected. Due consideration is also given to factors associated with the developmental level of the child such as the psychological sophistication, intellectual ability, current mental state, etc.
The flow of the diagnosis for the screening and diagnostic sub-modules consists of three main components, namely, the question item with its serial number, the ‘rater's rule’ and the ‘decision rule’ [Figure 2]. Each question item is based on the official classificatory systems, but is more descriptive, uses culturally relevant idioms and examples and is simple to comprehend. For every question item of the screening and diagnostic sub-modules, a rater's rule has been framed which is answered in a ‘yes/no’ format. The rater's rule guides the interviewer in judging the response elicited when the specific question is asked. This rule further clarifies the intent of the question, emphasizes on the duration and persistence of symptoms and the distress or dysfunction caused by the symptoms. For example, in the sub-module for generalized anxiety disorder of childhood, the response to the question ‘has this anxiety been present for a long time….’ is considered positive only if the anxiety ‘been present for more than 1 month’, as mentioned in the ‘rater's rule’.
Figure 2.
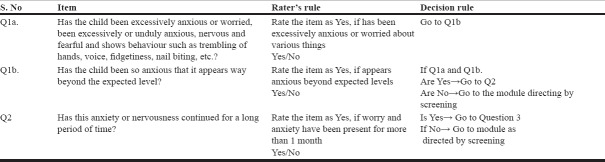
Components of the diagnostic algorithm: Section A: Diagnostic module for generalized anxiety disorders
There is also a provision for recording information, which is considered significant by the interviewer, but is not captured in the categorical ‘yes/no’ format. The third component, the ‘decision rule,’ is the rule for eventual automation that would govern the flow of the diagnostic algorithm as it defines the next step after eliciting response to each question item. The decision rules have been built based on the diagnostic thresholds set by standardized classification systems as well as socio-cultural norms, duration of symptoms, possibility of self-limiting symptoms and dysfunction caused by symptoms. The decision rules also incorporate hierarchical rules for skipping certain modules if a specific diagnosis is made even though those modules are indicated by the screening (for example, if a diagnosis of psychosis is made, the module for anxiety would not open even if indicated by screening). For example, is the diagnostic module for generalized anxiety disorder, for which the Figure 2 gives the rater's rule and dcision rule.
Examining diagnostic accuracy and feasibility of use of the tool
Prior to computerization of the diagnostic decision support system, the paper-pencil forms in English and Hindi language were prepared and tested for its diagnostic accuracy and feasibility. This study was conducted at the department of psychiatry of PGIMER, the nodal centre. For this purpose, consecutive outpatients aged less than 18 years, who gave assents and their parents, who gave written informed consent, were assessed using the new diagnostic tool. This was done in addition to the routine detailed semi-structured clinical assessment undertaken in the department by a team of a trainee psychiatrist and a consultant psychiatrist, which generates ICD-10 diagnoses. Patients were randomly allocated to undertake the tool-based assessment followed by routine clinical evaluation, or vice versa. The interviewers using the new diagnostic toolwere blind to the clinical diagnoses. Demographic data, ratings on screening and diagnostic modules, diagnoses generated by the tool and the clinical diagnoses were all recorded. Additionally, details regarding the completion rate, the total time taken and feedback on comprehensibility of language, style of questioning and interviewer satisfaction were also obtained.
Data analysis
Statistical analysis was carried out using the Statistical Package for Social Sciences-version 15.[20] Apart from descriptive analyses, paired t-tests were conducted to compare the mean number of diagnosis generated by the two interviews. The diagnosis obtained following detailed clinical evaluation was used as the standard to compare both the diagnoses obtained by the screening and diagnostic assessments of the new tool. Sensitivity, specificity, positive and negative predictive values were computed for the screening and the diagnostic sub-modules of the tool, compared to the clinical diagnoses. Additionally, kappa coefficients were computed to assess agreement between the diagnoses generated by the diagnostic sub-module and the clinical diagnoses.
RESULTS
Over a period of 6 months, a total of 50 children and adolescents were included in the study. About half of these patients were assessed on the telepsychiatry diagnostic tool first, while the remaining patientsunderwent clinical evaluation by a psychiatrist prior to assessment with the telepsychiatry diagnostic tool. Interviews with the diagnostic tool were, for the most part, conducted by psychologists after a brief training session of familiarization with the telepsychiatry diagnostic system.
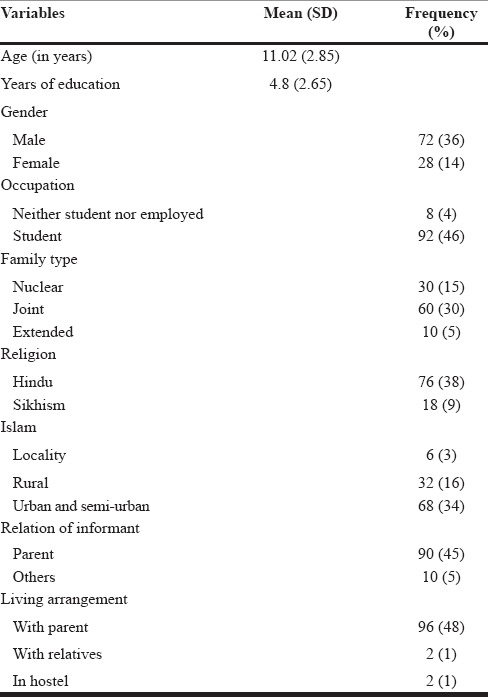
Demographic profile of participants
Table 1 indicates the demographic profile of the 50 patients included in the study. Patients had an average age of 11.06 years, with more boys than girls constituting the study sample. Most of them were students and mainly came from urban or semi-urban areas. This corresponded to the usual profile of child and adolescent attendees at this centre.
Table 1.
Demographic details of participants (n = 50)
Diagnostic profile of participants
The mean number of total diagnoses made by the new diagnostic tool per patient was 1.48 (S. D-1.03) and those made with detailed clinical interview was 1.40 (S. D-0.75); this difference was, however, found to be not significant. Mental retardation was diagnosed in 30%, specific developmental disorder of scholastic skills in 12%, attention deficit hyperactivity disorder (ADHD) in 20%, conduct disorder in 14%, oppositional defiant disorder in 6%, emotional disorders with onset specific to childhood in 10%, depressive disorder in 6%, dissociative disorders in 16%, enuresis in 14%, obsessive compulsive disorder in 8%, mania in 2% and psychoses in 6% of the patients when assessed by the telepsychiatry diagnostic tool.
None of the patients received diagnosis related to the spectrum of substance use/abuse either by the telepsychiatry diagnostic tool or by clinical assessment. No definitive diagnosis could be reached by the telepsychiatry tool for a total seven patients. The clinical diagnoses for these seven patients after detailed clinical assessment by a psychiatrist, however, were emotional disorders with onset specific to childhood (n = 4), ADHD (n = 1) and no psychiatric illness diagnosed (n = 2).
Agreement between the diagnostic tool and clinical diagnosis
Screening sub-module of the diagnostic tool versus clinical diagnoses
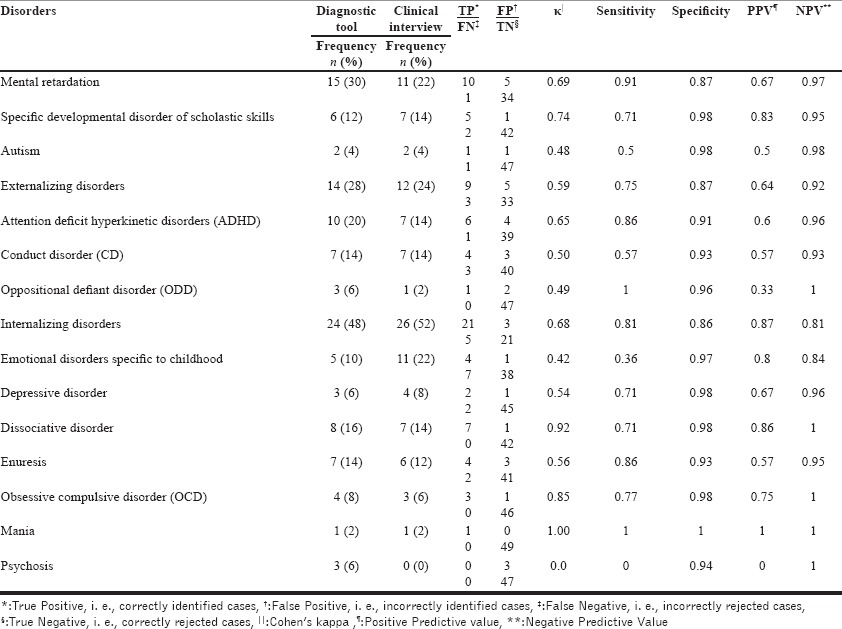
Table 2 depicts the sensitivity, specificity, positive predictive value and negative predictive values of the screening sub-module of the diagnostic tool, compared to the diagnoses obtained following the clinical evaluation.
Table 2.
Sensitivity, specificity, positive and negative predictive values of screening sub-module of the diagnostic tool, as compared to that of the clinical interview
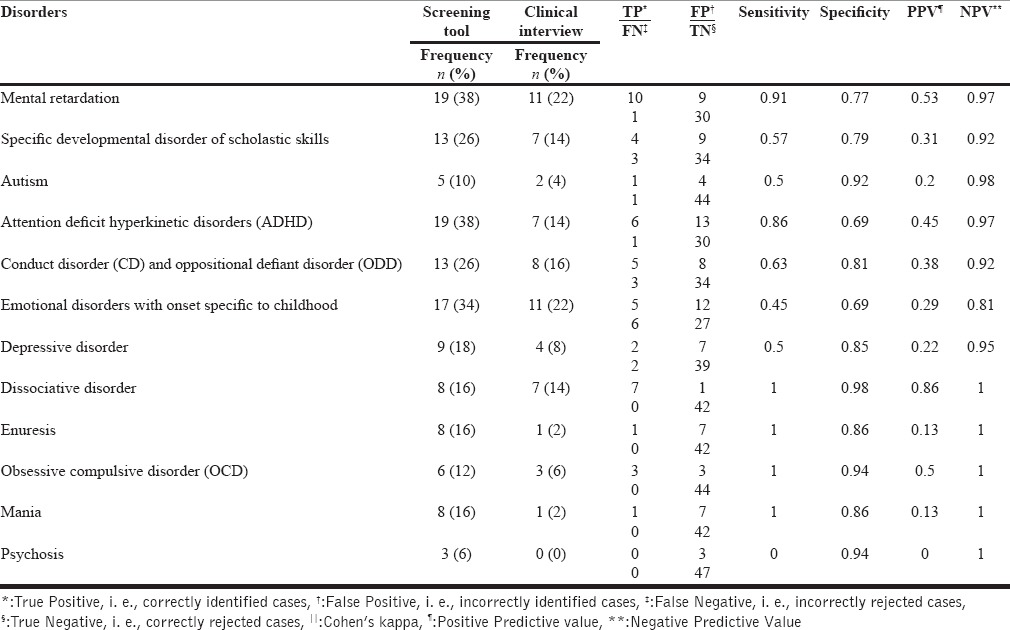
The results show that the sensitivity of screening part of the tool was high for most disorders except emotional disorders specific to childhood, depressive disorders and autism. In the categories of depressive disorders and autism, this seems to be because of the small number of patients, i. e., two and four, respectively. Sensitivity for psychotic disorders could not be calculated as no patient was diagnosed with psychosis on clinical assessment. The specificity of screening was high for all disorders. Positive predictive values were low for almost all disorders, except for dissociative disorders. This was a reflection of the high rates of false positive diagnoses in all categories, except dissociative disorder. On the other hand, negative predictive values were consistently high because of the high rates of true negative cases in most categories.
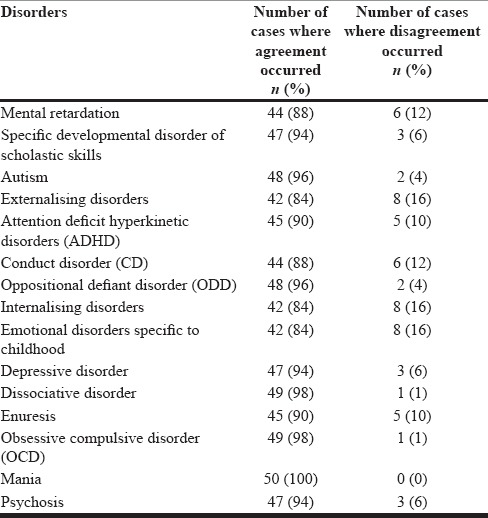
Diagnostic sub-module of the tool versus clinical diagnoses
Table 3 depicts the Cohen's kappa, sensitivity, specificity and positive and negative predictive values of the diagnostic sub-modules of the tool, compared to that of the clinical diagnosis. Cohen’ kappa values revealed substantial to near perfect agreement (> 0.6) for mental retardation, specific developmental disorder of scholastic skills, ADHD, dissociative disorder, obsessive compulsive disorder (OCD) and mania and moderate agreement (0.4–0.6) for autism, conduct disorder, oppositional defiant disorder, emotional disorders specific to childhood, depressive disorder and enuresis. Diagnosis of psychosis was not made in any patienton clinical evaluation.
Table 3.
Cohen's kappa (κ), sensitivity, specificity and positive and negative predictive values of the diagnostic sub-modules of the tool, compared to that of the clinical interview
Sensitivity of diagnoses was high apart from emotional disorders with onset specific to childhood (36%) and autism (50%). Low sensitivities were primarily due to the high rates of false negative cases in the former category and due to small number of patients in the latter. Specificity was high for all the disorders.
Unlike the screening sub-module, positive predictive values were acceptable to high for most disorders, except oppositional defiant disorder (0.33) and autism (0.5). Thus, the numbers of false positive diagnoses were reduced after applying the diagnostic sub-modules. Similar to the screening sub-module, negative predictive values were consistently high because of the high rates of true negative cases.
Discordance analysis
The number of discordant cases in each diagnostic categoryis is shown in Table 4. For most of the cases with discordance in a particular diagnostic category, there were additional diagnoses that were agreeing between the two methods of assessment. For example, in the diagnostic category of psychosis, discordance between the diagnoses made by the two methods occurred in a total of three cases. In one out of these three cases diagnosed with psychoses by the diagnostic tool, the clinical diagnosis made was dissociative disorder. However, in the remaining two cases, agreement between the two methods of assessment was seen as a diagnosis of OCD was made by clinical evaluation as well as by the tool (in addition to psychosis).
Table 4.
Frequency of concordant and discordant cases in each diagnostic category
Length of the assessment using the new diagnostic tool
Details regarding the length of the assessment are shown in Table 5. The average amount of time taken for assessment by the ‘core’ diagnostic tool was 30.32 minutes (SD-11.63) and that for screening alone was 4.18 minutes (SD-1.03).
Table 5.
Results of the feasibility analysis of the diagnostic tool
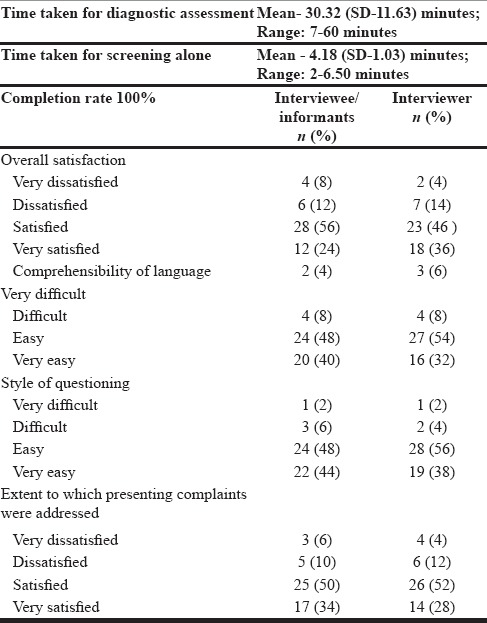
Feasibility of use of the new diagnostic tool
Feasibility results are depicted in Table 5. All the participants completed the entire interview. A majority of the patients and their relatives, and the persons conducting the assessment were satisfied with the interview, especially with the language used and the style of questioning, as well the extent to which the presenting complaints were addressed by the interview.
DISCUSSION
Diagnostic assessment of psychiatric disorders in children and adolescents is complex and there is no such diagnostic system available in and applicable to Indian population. Need for a suitable tool for accurate detection of mental disorders in general health care settings has also been repeatedly expressed.[21] The net-based tool for diagnosing psychiatric disorders among children and adolescents developed as part of this project has the potential to fulfil many of these needs. The advantages of the tool are that though it is based on standardized classificatory systems such as the ICD-10 and the DSM-IV, it has been developed from scratch keeping in mind the requirements of Indian users, both patients and their relatives, as well as the interviewers who have had minimal experience of diagnosing psychiatric disorders. The style of the interview, and the flexibility incorporated by having ‘core’ and ‘additional’ sections make it ideally suited for this purpose.
At the same time, the interview is highly structured, fully automated, with an in-built logical support system and facilities for real-time and post-interview monitoring and support, whenever required. The nature of the language used is based on a non-technical and colloquial platform. This was done from a three pronged scenario which includes firstly, the interviewer (which can be a non-specialist), secondly, the interviewee and finally, closely associated individuals of the patient present at the time of the interview. The use of such an approach allows the interviewee to understand questions directed to him in a more effective way and in turn allows the administrator of the tool to record genuine, well-described information. These features not only enhance the performance of the tool, but also empower the interviewer to carry out the process of diagnosis accurately.
Screening instruments for psychiatric disorders should include commonly encountered disorders and have high sensitivity for detection of these disorders.[22] The screening sub-module of the diagnostic tool fulfilled both these criteria, as it included a broad range of commonly prevalent disorders and, with certain exceptions, had a high sensitivity for detecting these disorders. Sensitivity was low for emotional disorders with onset specific to childhood and autism, but the small number of patients in the latter case limits the interpretation of the results. In the six children diagnosed with emotional disorders by clinical assessment, but not detected so by screening, the patients were evaluated for one of more of the following disorders by the diagnostic tool based on the clinical symptoms reported during the diagnostic interview; conduct disorder, ADHD, enuresis, OCD, mental retardation, specific learning disability and autism. Another reason can be based on the possibility that parents/other significant individuals around the child fail to report/notice certain nuances in the child's symptoms in such cases. Brandbo[23] suggested that parent often fail to report emotional difficulties as problematic in a structured (yes/no) format, resulting in low sensitivity for emotional disorders.
The specificity of screening was high for all the disorders, thoughpositive predictive values were low for most disorders, which indicatesa high rate of true negative diagnoses coexisting with a high rate of false positive diagnoses. This is a problem that has been noted for psychiatric screening tools.[24,25] However, a substantial number of patients with false positive results meet diagnostic criteria for other mental disorders and the burden of follow-up assessments for patients with positive screens is usually not too high. Hence, it has been suggested that erring on the side of sensitivity is preferable for instruments screening for psychiatric disorders.[26]
There was no significant difference between the number of diagnoses made by the tool and that made by clinical evaluation. This finding was unlike that seen with other diagnostic interviews, for example MINI-KID identified a mean of 3.6 (SD-2.8) disorders per patient.[16] While this may be useful in research interviews, it might present problems for routine clinical setting. In this regard, the inbuilt hierarchies and exclusion rules of the diagnostic tool reduced the chances of multiple diagnoses, thereby simplifying the entire process for the interviewer. In other aspects, the diagnostic module performed well compared to the detailed clinical evaluation. The kappa values indicated moderate to high agreement between the two assessments for all disordersexcept for psychosis.[27]
In one patient diagnosed with dissociative disorder by clinical assessment, the presence of auditory and visual hallucinations lead to misdiagnosis of psychosis by the diagnostic tool. Misdiagnosis due to such dissociative symptoms has been well-noted in literature.[28] Compared to other disorders, low concordance was seen for emotional disorders with onset specific to childhood (kappa-0.42). This finding was similar to that seen with the MINI-KID,[16] where the agreement for generalized anxiety, social anxiety, separation anxiety and specific phobias varied from 0.18 to 0.35. Low diagnostic agreement for these disorders has been noted with other instruments as well.[29,30] As seen with screening, the sensitivity of diagnoses with clinical assessment was high for most disorders apart from that for emotional disorders with onset specific to childhood and autism. Specificity was high for all the disorders and positive predictive values were also acceptable to high for most disorders. Negative predictive values continued to remain high for all disorders.
On all the parameters, the new diagnostic tool was found to be broadly comparable to several other diagnostic instruments such as the MINI-KID, Diagnostic Interview Schedule for Children (DISC), the Child and Adolescent Psychiatric Assessment (CAPA) and the Development and Well-Being Assessment (DAWBA).[16,30,31,32,33] Features such as low time consumptions and results indicating high sensitivity (for most disorders) and specificity (for all disorders) bolster the future potential of the diagnostic tool developed.
Finally, the feasibility analysis demonstrated that the instrument was easy to administer and was rated highly both by the interviewers and the interviewees (patient and her relatives). In the new tool, a lot of emphasis has been placed on flexibility of interviewing and establishing a therapeutic relationship with the patient, without compromising on the objectivity of assessment. The feasibility analysis suggested that these features of the tool helped it recreate the clinical situation to a large extent. All this was achieved in a time of about 30 minutes, which was comparable to that of MINI-KID,[16] and much less than other instruments. However, MINI-KID does not cover several disorders including mental retardation unlike the diagnostic tool. Moreover, the time taken for using the screening sub-module was about 5 minutes. It has been suggested that screening time for use in primary care settings should not be more than about 5 minutes if an instrument is to be widely adopted.[34] Further, the newly developed diagnostic tool included the choices for including inputs directly from the child/adolescent so as to strengthen rapport with child and providing an essential element of the clinical setting. Thus, a one-on-one session with the child could be held with the parent and significant others such as peers or teachers serving as imperative additional sources of eliciting in-depth information about the child. Thus, one of the strengths of the interview is that it relies upon multiple sources of information as well as observation; such an approach is considered crucial to the assessment of child and adolescent psychiatric disorders.[35]
Though the results of this study were encouraging in terms of the accuracy of diagnoses generated by the tool and the feasibility of its use among adults with psychiatric disorders, they must be viewed with caution, because of certain methodological limitations. Firstly, the size of the total sample was small and the numbers involved for most diagnostic categories, except the broad categories of mood and neurotic disorders, were also small. Diagnoses obtained following detailed clinical evaluation was used as the gold standard against which the diagnostic tool was tested. However, there are variations in clinical diagnosis across clinicians. Using another structured interview schedule would be a useful comparison in addition to specialist opinion.
The sample was drawn from persons attending a tertiary-care psychiatric facility; so, the results cannot be immediately generalised to primary and secondary care settings. Finally, the tool does not cover a few other childhood psychiatric disorders such as tic disorder and eating disorders. However, since these are expected to be uncommon even in specialist settings, this is not expected to affect the utility of tool to a great extent. Methodological problems notwithstanding, the findings of the present study provided the impetus for further evaluation of the new diagnostic tool. Our diagnostic tool has been fully computerized and gives an automated diagnosis. Efforts are underway to further enhance the accuracy of the diagnostic tool, test its validity at the primary care level with non-mental health workers, and compare its validity with other structured diagnostic tools. It is hoped that following further refinements, the tool would be more suitable for use in the peripheral sites, where its utility is likely to be the greatest.
ACKNOWLEDGMENT
The authors gratefully acknowledge the financial support received from Department of Science & Technology, Government of India, New Delhi, India.
Footnotes
Source of Support: Department of Science & Technology, Ministry of Science and Technology, Government of India, New Delhi, India
Conflict of Interest: None declared.
REFERENCES
- 1.Sharan P, Malhotra S. Telepsychiatry: The bridge across the access gap in child and adolescent mental health. J Indian Assoc Child Adolesc Ment Health. 2007;3:18–20. [Google Scholar]
- 2.Geneva: World Health Organization; 2001. The world health report 2001: Mental health: New understanding, new hope; p. 169. [Google Scholar]
- 3.Geneva: WHO; 2005. World Health Organization. Child and adolescent mental health policies and plans: Mental health policy and service guidance package. [Google Scholar]
- 4.Census of India. (2011). Population Enumeration Data: Age Data. [Last accessed on 2014 May 25]. Available from: http://www.censusindia.gov.in/2011census/population_enumeration.aspx .
- 5.Geneva: WHO; 2005. World Health Organization. Atlas: Child and Adolescent Mental Health Resources-Global concerns: Implications for the Future. [Google Scholar]
- 6.Thirunavukarasu M. Closing the treatment gap. Indian J Psychiatry. 2011;53:199–201. doi: 10.4103/0019-5545.86803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murthy P, Sekar K. A decade after the NHRC quality assurance initiative: Current status of government psychiatric hospitals in India. Mental health care and human rights. In: Nagaraja D, Murthy P, editors. 1st ed. New Delhi: National Human Rights Commission; 2008. pp. 101–42. [Google Scholar]
- 8.Melaka A, Edirippulige S. Psych-technology: A systematic review of the telepsychiatry literature. Telepsychiatry appendices. 2009. [Last accessed 2014 Sep 15]. Available from: http://www.priory.com/psychiatry/telepsychiatry.htm .
- 9.Malhotra S. Telepsychiatry. A feasible option for primary care. Indian J Soc Psychiatry. 2011;27:89–95. [Google Scholar]
- 10.Malhotra S, Chakrabarti S. Telepsychiatry: A new paradigm for mental health care delivery. J Postgrad Med Educ Res. 2012:46. [Google Scholar]
- 11.Malhotra S, Chakrabarti S, Shah R. Telepsychiatry: Promise, potential and challenges. Indian J Psychiatry. 2013;55:3–11. doi: 10.4103/0019-5545.105499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malhotra S, Chakrabarti S, Shah R, Gupta A, Mehta A, Nithya B, et al. Development of a novel diagnostic system for a telepsychiatric application: A pilot validation study. BMC Res Notes. 2014. [Last accessed 2014 Aug 14]. pp. 7–508. Available from: http://www.biomedcentral.com/1756-0500/7/508 . [DOI] [PMC free article] [PubMed]
- 13.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) J Am Acad Child Adolesc Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Reich W. Diagnostic interview for children and adolescents (DICA) J Am Acad Child Adolesc Psychiatry. 2000;39:59–66. doi: 10.1097/00004583-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) J Clin Psychiatry. 2010;71:313–26. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 17.New Delhi: Oxford University Press; 1992. World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- 18.Geneva: World Health Organization; 1993. World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research. [Google Scholar]
- 19.Text revision. 4th ed. Washington, DC: American Psychiatric Association; 1994. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [DSM-IV] [Google Scholar]
- 20.Chicago, IL, USA: SPSS Inc; Statistical Package for Social Sciences, version fifteen (SPSS-15) [Google Scholar]
- 21.Murthy RS, Wig NN. Psychiatric diagnosis and classification in developing countries. In: Maj M, Gaebel W, Lopez-Ibor JJ, Sartorius N, editors. Psychiatric Diagnosis and Classification. UK: John, Wiley and Sons Ltd; 2002. pp. 249–79. [Google Scholar]
- 22.Broadhead WE, Leon AC, Weissman MM, Barrett JE, Blacklow RS, Gilbert TT, et al. Development and validation of the SDSS-PC screen for multiple mental disorders in primary care. Arch Fam Med. 1995;4:211–9. doi: 10.1001/archfami.4.3.211. [DOI] [PubMed] [Google Scholar]
- 23.Brøndbo PH, Mathiassen B, Martinussen M, Heiervang E, Eriksen M, Moe TF, et al. The strengths and difficulties questionnaire as a screening instrument for Norwegian child and adolescent mental health services, application of UK scoring algorithms. Child Adolesc Psychiatry Ment Health. 2011;5:32. doi: 10.1186/1753-2000-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leon AC, Portera L, Olfson M, Weissman MM, Kathol RG, Farber L, et al. False positive results: A challenge for psychiatric screening in primary care. Am J Psychiatry. 1997;154:1462–4. doi: 10.1176/ajp.154.10.1462. [DOI] [PubMed] [Google Scholar]
- 25.Nease DE, Jr, Malouin JM. Depression screening: A practical strategy. J Fam Pract. 2003;52:118–24. [PubMed] [Google Scholar]
- 26.Leon AC, Portera L, Olfson M, Kathol R, Farber L, Lowell KN, et al. Diagnostic errors of primary care screens for depression and panic disorder. Int J Psychiatry Med. 1999;29:1–11. doi: 10.2190/7AMF-D1JL-8VHA-APGJ. [DOI] [PubMed] [Google Scholar]
- 27.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 28.Putnam FW. Dissociative disorders in children: Behavioral profiles and problems. Child Abuse Negl. 1993;17:39–45. doi: 10.1016/0145-2134(93)90006-q. [DOI] [PubMed] [Google Scholar]
- 29.Kim YS, Cheon KA, Kim BN, Chang SA, Yoo HJ, Kim JW, et al. The reliability and validity of Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version- Korean version (K-SADS-PL-K) Yonsei Med J. 2004;45:81–9. doi: 10.3349/ymj.2004.45.1.81. [DOI] [PubMed] [Google Scholar]
- 30.Lewczyk CM, Garland AF, Hurlburt MS, Gearity J, Hough RL. Comparing DISC-IV and clinician diagnoses among youths receiving public mental health services. J Am Acad Child Adolesc Psychiatry. 2003;42:349–56. doi: 10.1097/00004583-200303000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The development and well-being assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41:645–55. [PubMed] [Google Scholar]
- 32.Piacentini J, Shaffer D, Fisher P, Schwab-Stone M, Davies M, Gioia P. The Diagnostic Interview Schedule for Children-Revised Version (DISC-R): III. Concurrent criterion validity. J Am Acad Child Adolesc Psychiatry. 1993;32:658–65. doi: 10.1097/00004583-199305000-00025. [DOI] [PubMed] [Google Scholar]
- 33.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic p sychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 35.Mc Conaughy SH. 2nd ed. New York: Guilford Press; 2013. Clinical interviews for children and adolescents: Assessment to intervention; p. 267. [Google Scholar]


