Abstract
This prospective clinical study aimed at assessing three pulmonary scintigraphic algorithms to detect acute pulmonary embolism (PE): Lung ventilation/perfusion (V/Q) scintigraphy along with modified prospective investigation of pulmonary embolism diagnosis (PIOPED) criteria; lung perfusion scintigraphy along with prospective investigative study of acute pulmonary embolism diagnosis (PISAPED) criteria; and lung perfusion scan in combination with ventilation scan, along with modified PISAPED criteria, which were newly developed. Patients with suspicion of PE were eligible for this study if they had no abnormal chest x-ray. Their diagnostic workup included a clinical assessment, a pulmonary V/Q scintigraphy, and CT pulmonary angiography (CTPA), as well as a clinical outcome assessment over a period of 24 weeks. Referred to the final clinical diagnosis of patients, the sensitivity and specificity of each algorithm were evaluated. The diagnostic performance of each algorithm by the area under the maximum likelihood fitted receiver operating characteristic (ROC) curve was determined. With respect to the PISAPED criteria, the sensitivity was 60.8% and specificity was 87.3%. No patient was classified into nondiagnostic category. The PIOPED criteria showed that the sensitivity was 95.0% and specificity was 88.2%, while 57.4% of the patients were in nondiagnostic category. The areas under the ROC curve constructed from the PISAPED criteria results and the modified PIOPED criteria results were 0.734 and 0.859 (P < 0.01), respectively. The modified PISAPED criteria demonstrated that the sensitivity was 83.8% and specificity was 89.1%. No patient was classified into nondiagnostic category. The area under the ROC curve constructed from modified PISAPED criteria was 0.864 (P < 0.01). Perfusion scans used with ventilation scans and modified PISAPED criteria may increase the diagnostic accuracy of pulmonary scintigraphy for acute PE, compared with the two major algorithms.
Keywords: Acute pulmonary embolism, modified prospective investigation of pulmonary embolism diagnosis criteria, modified prospective investigative study of acute pulmonary embolism diagnosis criteria, PISAPED criteria, pulmonary scintigraphy
Introduction
Efficacy and continued technical improvements in CT pulmonary angiography (CTPA) have produced a significant rise in its use for the diagnosis of acute pulmonary embolism (PE).[1] The growth of CTPA has produced a corresponding reduction in the utilization of pulmonary scintigraphy to the extent that some publications have suggested that lung scanning has become a second-line test.[2,3,4] The several distinct advantages of multiple detector CT (MDCT) including high specificity, availability, and the superior ability to supply alternative diagnoses have come at the expense of an increased radiation burden.[4] The effect of a low clinical threshold for utilization that promotes indiscriminate and repeated use, particularly in younger patients, is yet to be felt.[4] Although the statistical data may be difficult to gather, it is intuitive that the lower radiation dose and higher sensitivity of scintigraphy in younger patients can only be beneficial.[4] As with CT, scintigraphy offers specific advantages in a number of scenarios, particularly those in which high negative predictive value and low radiation dose are of parallel importance, such as in a young pregnant patient.[4] The routine use of scinitigraphy in patients who are young, have no preexisting lung pathology, and have a normal chest radiograph should not be demeaned.[4] Scinitigraphy remains one of the best tests yet established for the follow-up of PE after diagnosis and shows significant advantage in the investigation of the etiology of pulmonary hypertension.[4]
Lung ventilation/perfusion (V/Q) scintigraphy along with modified prospective investigation of pulmonary embolism diagnosis (PIOPED) interpretation criteria has been utilized to diagnose acute PE.[5,6,7] More recently, a simplified algorithm comprising pulmonary perfusion scan along with prospective investigative study of pulmonary embolism diagnosis (PISAPED) interpretation criteria[8] has shown a reduction of intermediate probability as one of the lung scan readings generated by the modified PIOPED criteria and has improved the sensitivity and specificity of the lung scintigraphy along with the modified PIOPED criteria to detect acute PE.[9] However, it has been reported that results obtained with the perfusion scan along with the PISAPED criteria are less satisfactory than those results obtained in the context in which the test was developed.[10]
Therefore, a prospective clinical study conducted by the International Atomic Energy Agency (IAEA) through the Coordinated Research Project (CRP) E1.30.20 was undertaken to assess two pulmonary scintigraphic algorithms, one employing lung V/Q scan along with modified PIOPED criteria[5,6,7] and the other employing only a pulmonary perfusion scan along with PISAPED criteria.[8] In addition, a new algorithm and lung perfusion scintigraphy in combination with ventilation scan along with modified PISAPED criteria, which were developed by us in an effort to improve the sensitivity and specificity to detect acute PE, were similarly evaluated.
Materials and Methods
Study protocol
A standard procedure of the IAEA CRP E1.30.20, entitled “Evaluation of a single utilization of pulmonary perfusion scintigraphy in patients with suspected pulmonary embolism” is described as follows:
-
All patients suspected of having PE will be given a clinical score of pretest likelihood based on clinical and biochemical data, results of a chest x-ray (CXR), an electrocardiogram (ECG), arterial blood gases, and a digital ultrasound (DUS)
- Patients with low likelihood and a negative D-dimer (DD) will not proceed to any further imaging but will be followed up for 24 weeks
- Patients with positive DD, or an intermediate or high likelihood, will have a V/Q scan and CTPA
- All patients will be assessed clinically by a physician every 12 weeks for 24 weeks. The physician will be aware of the results of all the above tests so as to formulate an overall judgment on patients’ outcome
- DUS should be repeated at the final follow-up examination.
If echocardiography was used in the initial scoring, it should also be used in the final follow-up examination.
Inclusion criteria are
Patients presenting with suspicion of acute PE within 24 h
Informed written consent, approved by the local ethical committee, should be obtained.
Exclusion criteria are
Pregnant females and children under 18 years
Patients with established major right-left shunt
Patients with a life expectancy of less than 24 weeks
Patients who have been on thrombolytic therapy for >3 days before the event
Patients who can be difficult to follow up for 24 weeks
Patients who are known to be allergic to iodine
Patients who suffer renal failure
Patients who are known to have pulmonary hypertension.
The study procedure is summarized in Figure 1.
Figure 1.
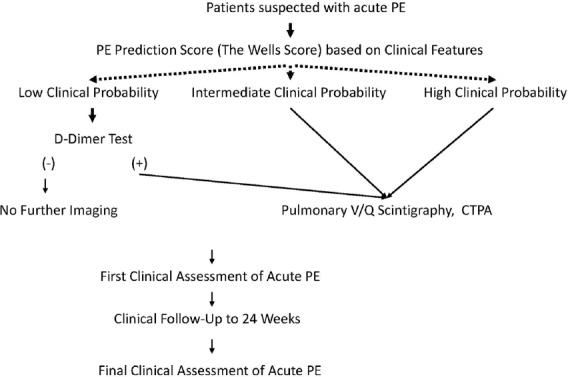
Main scheme of a study of IAEA CRP E1.30.29
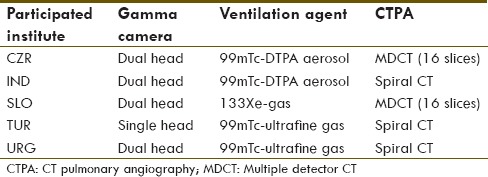
The type of gamma camera, ventilation agent, and CTPA in each institute is summarized in Table 1. The methodology for pulmonary scintigraphy followed the procedure guidelines for lung scintigraphy as published by the Society of Nuclear Medicine.[11] The CTPA procedure was conducted following local protocols in each institute. All patients had given informed consent for the present study, and no patient was personally identified in this study.
Table 1.
Type of gamma camera, ventilation agent, and CTPA in each institute
Patients
Patients were enrolled from five nuclear medicine departments in Slovenia, Turkey, the Czech Republic, Uruguay, and India between October 2004 and September 2008. Two hundred and one patients with suspected acute PE were registered in the study. Out of the total number of patients, 129 were eligible for this current study since they showed no abnormalities in CXR. The group comprised 66 females (mean age 60 years, range 19–95 years) and 63 males (mean age 58 years, range 22–85 years).
Scintigraphic criteria for PE interpretation
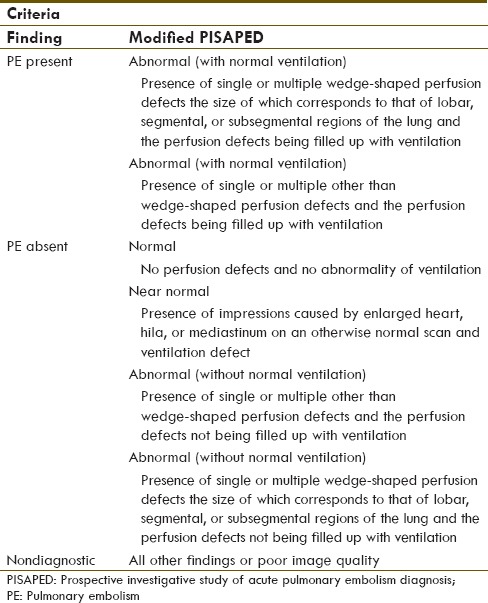
Two experienced nuclear medicine physicians who had no clinical information on patients independently assessed the V/Q scans according to modified PIOPED criteria as PE present, PE absent, or nondiagnostic [Table 2]. Then, they independently evaluated perfusion scans according to the conventional PISAPED criteria as PE present, PE absent, or nondiagnostic [Table 2]. Finally, the nuclear medicine physicians interpreted the perfusion scans in combination with ventilation scans according to modified PISAPED criteria as PE present, PE absent, or nondiagnostic [Table 3].
Table 2.
Modified PIOPED criteria and PISAPED scintigraphic criteria
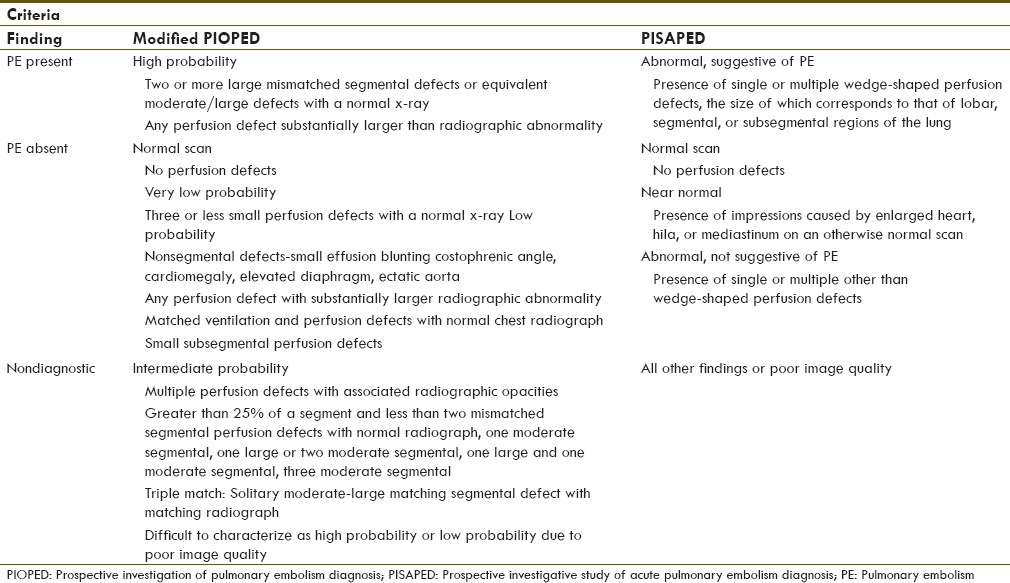
Table 3.
Modified PISAPED scintigraphic criteria
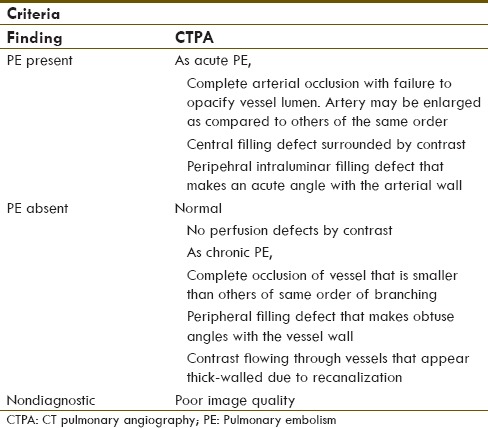
CTPA criteria for PE interpretation
Two experienced radiologists who had no clinical information on patients independently assessed CTPAs according to the CTPA criteria as PE present, PE absent, or nondiagnostic [Table 4].[12,13,14]
Table 4.
CTPA criteria
Evaluation of final clinical assessment
A clinician with extensive experience in acute PE who was blind to interpretations on any medical imaging, except for CXR, assessed the clinical follow-up within a period of 24 weeks (the efficacy of subsequent anticoagulation treatment and the clinical outcome of the patients at 24 weeks from the acute episode brought by the local physicians). This assessment was a reference standard for the final clinical diagnosis of acute PE in this study.
Data analysis
The primary analysis compared the CTPA criteria results, the modified PIOPED criteria results, the PISAPED criteria results, and the modified PISAPED criteria results using the clinical outcome at 24 weeks as reference standard for the final clinical diagnosis of acute PE. The sensitivity and specificity of each algorithm were obtained. Nondiagnostic scintigram readings were then excluded from the calculation of sensitivity and specificity.
The second analysis determined the diagnostic performance of each algorithm by the area under maximum likelihood fitted receiver operating characteristic (ROC) curve.
P values smaller than 0.01 were assumed to be statistically significant.
Results
Of the 129 patients, 74 were evaluated as acute PE and 55 as nonacute PE according to the final clinical assessment, based on the clinical follow-up at 24 weeks. The two cases of CTPA fell in the nondiagnostic category on account of poor image quality. There was no discordance in clinical diagnosis of acute PE between the expert physicians and local physicians in the institutes for this study. Further, there was no discordance in interpretation of medical images except for CTPA between the expert readers for this study and local readers in the institutes.
The CTPA criteria resulted in 68 (53.5%) patients being classified as PE present and 59 (46.5%) as PE absent. Two (1.6%) were in the nondiagnostic category because of poor image quality. The sensitivity of CTPA to detect acute PE was 91.7% and specificity was 96.4%.
The modified PIOPED criteria resulted in 40 (31.0%) patients being classified as PE present and 17 (13.2%) as PE absent. A further 74 (57.4%) were in the nondiagnostic category (intermediate probability). The sensitivity of the V/Q scan along with the modified PIOPED criteria to detect acute PE was 95.0% and specificity was 88.2%.
The PISAPED criteria resulted in 52 (40.3%) patients being classified as PE present and 77 (59.7%) as PE absent. No patient was classified into the nondiagnostic category. The sensitivity of perfusion scan along with the PISAPED criteria was 60.8% and specificity was 87.3%.
The modified PISAPED criteria resulted in 68 (52.7%) patients being classified as PE present and 61 (47.3%) as PE absent. No patient was classified into the nondiagnostic category. The sensitivity of the perfusion scan in combination with ventilation scan, along with the modified PISAPED criteria was 83.8% and specificity was 89.1%.
The diagnostic performance of the V/Q lung scan along with the modified PIOPED criteria, as determined by the area under a maximum likelihood fitted ROC curve, measured 0.858 (95% CI, 0.804–0.913) [Figure 2]. The value was significantly higher (P = 0.002) when compared with that of the perfusion lung scan along with the PISAPED criteria, which measured 0.734 (95% CI, 0.660–0.807) [Figure 2].
Figure 2.
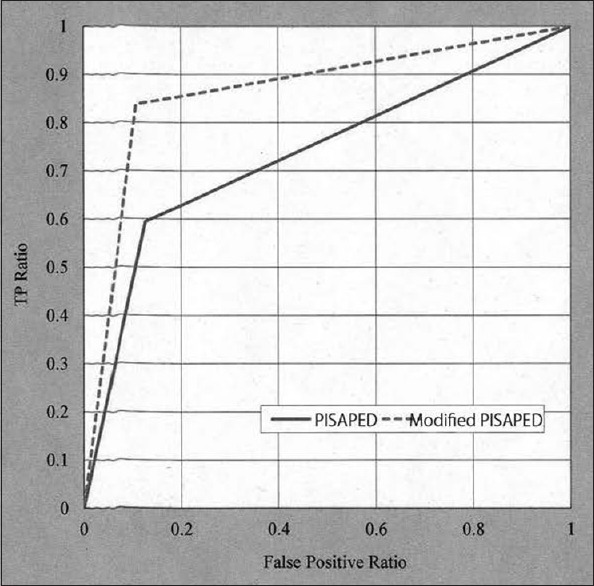
ROC curves demonstrated no superior diagnostic performance of the pulmonary perfusion scan along with the PISAPED criteria (solid line) compared with the lung V/Q scan along with the modified PIOPED criteria (dotted line)
The diagnostic performance of the perfusion scan in combination with ventilation scan, along with the modified PISAPED criteria measured 0.864 (95% CI, 0.807–0.922) as determined by the area under a maximum likelihood fitted ROC curve [Figure 3]. This value was significantly higher (P = 0.001) in comparison to that of the perfusion lung scan along with the PISAPED criteria [Figure 3].
Figure 3.
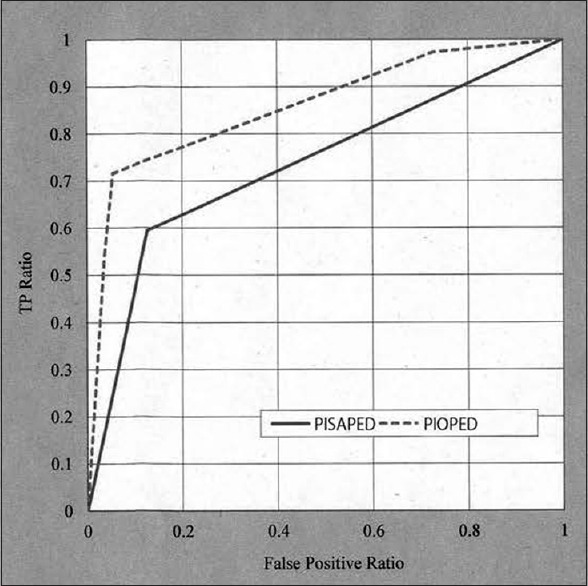
ROC curves showed the superior diagnostic performance of the pulmonary perfusion scan in combination with lung ventilation scan along with the modified PISAPED criteria (dotted line) compared with the pulmonary perfusion scan along with the PISAPED criteria (solid line)
Discussion
The aim of this study was to evaluate three pulmonary scintigraphic algorithms for the detection of acute PE. In our study, the pulmonary perfusion scan along with the PISAPED criteria showed no improved accuracy in predicting acute PE compared with the V/Q scan along with the modified PIOPED criteria, except for reduction in the number of nondiagnostic cases. The simplified algorithm performed poorly in this regard as was previously reported.[10] On the other hand, the new algorithm, the pulmonary perfusion scan in combination with ventilation scan along with the modified PISAPED criteria, which were developed by us demonstrated significantly improved accuracy in predicting acute PE in comparison to the simplified algorithm.
It was observed that 58.6% of the false-negative cases recognized by the PISAPED criteria were reclassified into the true positive category by making reference to the corresponding ventilation findings. Non-single, non-wedge-shaped defects with normal ventilation (50% of the false-negative cases) may be the result of acute PE. Pulmonary thromboembolism could dissolve into smaller parts with time.[15] Therefore, wedge-shaped defects of pulmonary scintigraphic findings of perfusion may be transformed into non-wedge-shaped ones.[15] Such a scene might be delineated in the first scintigraphy of the study. Serial-combined pulmonary ventilation-perfusion imaging is very useful to maximize diagnostic specificity for PE.[15] On the other hand, wedge-shaped defects with abnormal ventilation (50% of the false-negative cases) may originate from non-PE. The decrease in pulmonary perfusion can emerge by means of the physiological mechanism of hypoxic vasoconstriction caused by ventilation abnormalities such as emyphysema, pneumonia.[16] These abnormalities are not so easy to detect on CXR images. Regional pulmonary ventilation abnormalities seem to become distinct in acute PE patients suffered from polypnea.
Our study may highlight that the finding of pulmonary ventilation scan is indispensable to the scintigraphic interpretation of acute PE.
Conclusion
The perfusion scan in combination with ventilation scan along with the modified PISAPED criteria may bring about reduction in the number of nondiagnostic cases and increase the diagnostic accuracy of pulmonary scintigraphy for acute PE in comparison to the two major algorithms.
Acknowledgment
A part of the study was presented at the Radiological Society of North America's 97th Scientific Assembly and Annual Meeting in Chicago, IL (RSNA2011).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Schoepf UJ. Diagnosing pulmonary embolism: Time to rewrite the textbooks. Int J Caridiovasc Imaging. 2005;21:155–63. doi: 10.1007/s10554-004-5345-7. [DOI] [PubMed] [Google Scholar]
- 2.Hayashino Y, Goto M, Noguchi Y, Fukui T. Ventilation-perfusion scanning and helical CT in suspected pulmonary embolism: Meta-analysis of diagnostic performance. Radiology. 2005;234:740–8. doi: 10.1148/radiol.2343031009. [DOI] [PubMed] [Google Scholar]
- 3.O’Neil JM, Wright L, Murchison JT. Helical CTPA in the investigation of pulmonary embolism: A 6-year review. Clin Radiol. 2004;59:819–25. doi: 10.1016/j.crad.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Reid JH, Coche EE, Inoue T, Kim EE, Dondi M, Watanabe N, et al. International Atomic Energy Agency Consultants’ Group. Is the lung scan alive and well? Facts and controversies in defining the role of lung scintigraphy for the diagnosis of pulmonary embolism in the era of MDCT. Eur J Nucl Med Mol Imaging. 2009;36:505–21. doi: 10.1007/s00259-008-1014-8. [DOI] [PubMed] [Google Scholar]
- 5.Freitas FE, Sarosi MG, Nagle CC, Yeomans ME, Freitas AE, Juni JE. Modified PIOPED criteria used in clinical practice. J Nucl Med. 1995;36:1573–8. [PubMed] [Google Scholar]
- 6.Sostman HD, Coleman RE, DeLong DM, Newman GE, Paine S. Evaluation of revised criteria for ventilation-perfusion scintigraphy in patients with suspected pulmonary embolism. Radiology. 1994;193:103–7. doi: 10.1148/radiology.193.1.8090877. [DOI] [PubMed] [Google Scholar]
- 7.Worsely DF, Alavi A. Comprehensive analysis of the results of the PIOPED study. Prospective Investigation of Pulmonary Embolism Diagnosis Study. J Nucl Med. 1995;36:2380–7. [PubMed] [Google Scholar]
- 8.Miniati M, Pistolesi M, Mariani C, Di Ricco G, Formichi B, Prediletto R, et al. Value of perfusion lung scan in the diagnosis of pulmonary embolism: Results of the prospective investigative study of acute pulmonary embolism diagnosis (Pisa-PED) Am J Respir Cri Care Med. 1996;154:1387–93. doi: 10.1164/ajrccm.154.5.8912753. [DOI] [PubMed] [Google Scholar]
- 9.Miniati M, Sostman HD, Gottschalk A, Monti S, Pistolesi M. Perfusion lung scintigraphy for the diagnosis of pulmonary embolism: A reappraisal and review of the prospective investigative study of acute pulmonary emblosim diagnosis methods. Semin Nucl Med. 2008;38:450–61. doi: 10.1053/j.semnuclmed.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 10.McLean RG, Carolan M, Bui C, Arvela O, Ford JC, Chew M, et al. Comparison of new clinical and scintigraphic algorithms for the diagnosis of pulmonary embolism. Br J Radiol. 2004;77:372–6. doi: 10.1259/bjr/83624598. [DOI] [PubMed] [Google Scholar]
- 11.Parker JA, Coleman RE, Hilson AJ, Royal HD, Siegel BA, Sostman HD. Society of Nuclear Medicine Procedure Guideline for Lung Scintigraphy. The Society of Nuclear Medicine. Version 3.0. Approved February 7, 2004. [PubMed] [Google Scholar]
- 12.Qanadli SD, Hajjam M, Mesurolle B, Barré O, Bruckert F, Joseph T, et al. Pulmonary embolism detection: Prospective evaluation of dual-section helical CT versus selective pulmonary arteriography in 157 patients. Radiology. 2000;217:447–55. doi: 10.1148/radiology.217.2.r00nv01447. [DOI] [PubMed] [Google Scholar]
- 13.Schoepf UJ, Holzknecht N, Helmberger TK, Crispin A, Becker CR, et al. Subsegmental pulmonary emboli: Improved detection with thin-collimation multi-detector row spiral CT. Radiology. 2002;222:483–90. doi: 10.1148/radiol.2222001802. [DOI] [PubMed] [Google Scholar]
- 14.Wittram C, Maher MM, Yoo AJ, Kalra MK, Shepard JA, McLoud TC. CT angiography of pulmonary embolism: Diagnostic criteria and causes of misdiagnosis. Radiographics. 2004;24:1219–38. doi: 10.1148/rg.245045008. [DOI] [PubMed] [Google Scholar]
- 15.Watanabe N, Oriuchi N, Suzuki H, Yukihiro M, Fukushima Y, Higuchi T, et al. A “changing stripe sign” in serial pulmonary perfusion imaging. Clin Nucl Med. 1996;21:111–4. doi: 10.1097/00003072-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe N, Hirano T, Inoue T, Matsumoto M, Oriuchi N, Tateno M, et al. Transient unilateral reverse ventilation/perfusion mismatch in a patient with lung cancer. Clin Nucl Med. 1992;17:705–8. doi: 10.1097/00003072-199209000-00003. [DOI] [PubMed] [Google Scholar]


