Abstract
We present the case report of a patient 83 year old female who developed progressive shortness of breath and subsequently underwent scintigraphic evaluation of her symptoms with a ventilation/perfusion scintigraphic exam. A matched perfusion defect was seen involving the basal segments of the left lower lobe. Following this, the patient was examined with a contrast enhanced CT of the chest to further investigate the defect, which revealed compression of the bronchi and vasculature of the left lower lobe basal segments by the hernia larger than the actual hernia. To our knowledge there has not been a case report of a large hiatal hernia as a cause of matched lower lobe defect.
Keywords: Hiatal hernia, lung scintigraphy, matched defect, ventilation/perfusion scan
Introduction
Ventilation/perfusion (V/Q) matched defects with associated with radiographic abnormality (i.e. triple matched defects) in the lower lung zone have traditionally been interpreted as representing an intermediate probability of pulmonary embolism,[1] especially if perfusion is absent.[2] While a diaphragmatic hernia may cause a V/Q matched defect in the lower lobes,[3,4] it is easily differentiated on radiography or computed tomography (CT) from other causes of matched defect and, therefore, does not generally cause incorrect scan reading. On the other hand, if the extent and size of the matched defect could not be explained by the mass of the hernia alone, other causes should be looked for. We present a case of external compression of the left basal segment vessels and airway by a large hiatal hernia with associated matched ventilation and perfusion defects in the basal segments of the left lower lobe not entirely accounted for by the mass of the hiatal hernia.
Case Report
The patient is an 83-year-old female with biopsy-proven lung adenocarcinoma that developed shortness of breath and clinical concern for pulmonary embolism. V/Q lung scintigraphy was performed for further evaluation of possible pulmonary thromboembolic disease as a source of the patient's new onset shortness of breath. Dynamic ventilation scintigraphic imaging of the lungs was obtained using Xenon-133 gas in the anterior and posterior projections (only posterior images shown). This was followed by the injection of 4 mCi technetium-99m macroaggregated albumin through the left antecubital vein, and subsequent scintigraphic imaging in multiple projections.
Large matched defects involving virtually the entire basal segments of the left lower lobe were seen as well as a perfusion defect corresponding to the known left upper lobe malignancy [Figure 1]. Follow-up CT angiogram was then performed in the further evaluation of pulmonary embolism, which demonstrated no evidence of pulmonary thromboembolic disease, but rather a large hiatal hernia compressing the lower lobe pulmonary vasculature and airways [Figure 2]. Relatively decreased pulmonary vasculature and associated air trapping seen in the CT images demonstrated by the differences when compared to the contralateral right lower lobe, corresponding to the scintigraphic findings.
Figure 1.
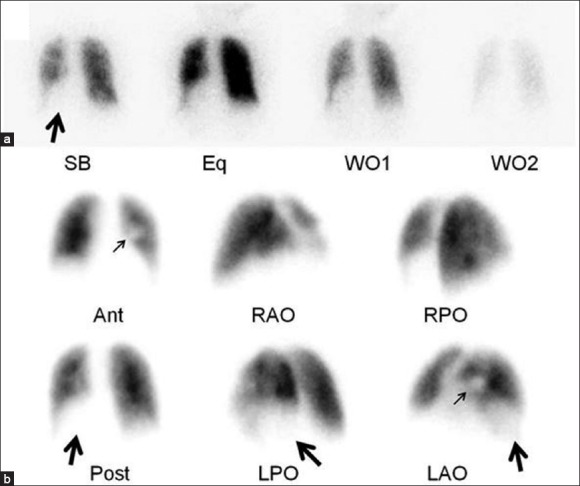
Scintigraphic images from a ventilation/perfusion (V/Q) scan. (a) Dynamic ventilation portion of the exam performed with Xenon-133, which demonstrates the ventilation defect in the left lower lobe (large arrow). (b) Corresponding perfusion portion of the exam which shows the matched defects involving virtually all of the basal segments of the left lower lobe (large arrows) as well as the moderate perfusion defect in the medial portion of the left middle lung zone (small arrows) that was secondary to the known tumor
Figure 2.
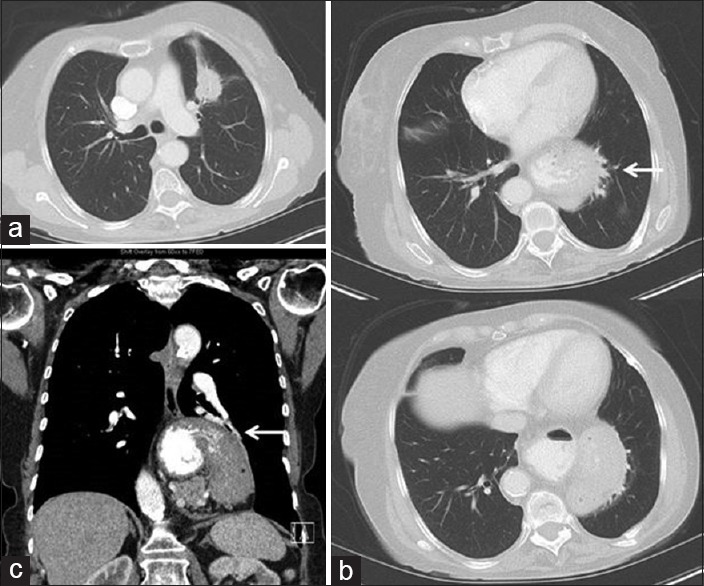
Contrast-enhanced computed tomography (CT) images from the same patient. (a) Transaxial CT image in a lung window near the level of the carina shows the known left upper lobe tumor. (b) A set of transaxial CT images in a lung window at the level of the left lower lobe which demonstrates the hiatal hernia narrowing the adjacent airway and vessels (white arrow). (c) A coronal reformatted CT image in soft tissue window that also shows the compression of the left lower lobe basal segment airway and vasculature (white arrow)
Discussion
Triple matched defects on V/Q scintigraphy and associated chest radiograph involving the lower lung zone are classically interpreted as intermediate probability of pulmonary embolism.[1] Anatomic correlates causing the defects, like a hiatal hernia in this case, are easily differentiable from other causes and can, therefore, be appropriately categorized. While the defect on scintigraphy caused by hiatal hernia typically reflects the herniated portion itself, we noticed that the extent and size of the matched defect could not be explained by the hernia alone. This was supported by the follow-up CT angiogram which demonstrated no evidence of pulmonary thromboembolic disease, but rather compression of the adjacent lower lobe pulmonary vasculature and airways by the hiatal hernia. There was also associated, relatively decreased pulmonary vasculature and associated air trapping, corresponding to the scintigraphic findings. To our knowledge, this is the first case report of such findings. We suggest that when ventilation and/or perfusion defect in the lower lung zone is larger than the hernia itself, interpreting physicians look for other etiology (external compression of the bronchovascular tree in this case) that may also explain the patient's symptoms.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Worsley DF, Kim CK, Alavi A, Palevski HI. Detailed analysis of patients with matched ventilation-perfusion defects and chest radiographic opacities. J Nucl Med. 1993;34:1851–3. [PubMed] [Google Scholar]
- 2.Kim CK, Worsley DF, Alavi A. Ventilation/perfusion/chest radiography match is less likely to represent pulmonary embolism if perfusion is decreased rather than absent. Clin Nucl Med. 2000;25:665–9. doi: 10.1097/00003072-200009000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Pober BR, Russell MK, Ackerman KG. In: Congenital Diaphragmatic Hernia Overview. Pagon RA, Adam MP, Bird TD, editors. Seattle (WA): University of Washington, Seattle; 1993-2013. 2006 Feb 1. [PubMed] [Google Scholar]
- 4.Sherigar RM, Bader DA. Scintigraphic intervention in a lung scan confirming a large hiatal hernia. Clin Nucl Med. 1999;24:127–8. doi: 10.1097/00003072-199902000-00014. [DOI] [PubMed] [Google Scholar]


