Abstract
Accessory ossicles are widely prevalent in the ankle and foot. Although they are often asymptomatic, they can present clinically with symptoms at times. When they occur bilaterally in a patient who presents with unilateral complaints, it is clinically difficult to attribute the symptoms to the presence of these common anatomic variants. One needs specific imaging to assess the clinical relevance of the accessory ossicles, in order to tailor the treatment plan. The case presented in this article is one such example, where the patient presented with chronic unilateral ankle pain and initial radiographs revealed bilateral os trigonum and os subtibiale. He underwent a technetium-99m methyl diphosphonate (Tc-99m MDP) bone scan and single photon emission computed tomography/computed tomography (SPECT/CT). The Tc-99m MDP scan showed a focal uptake in the ankle of concern. SPECT/CT complemented the finding by exactly localizing the uptake to the posterior subtalar joint and around the os trigonum, thereby pointing to the diagnosis of os trigonum syndrome.
Keywords: Os trigonum, posterior ankle impingement, single photon emission computed tomography/computed tomography
Introduction
The workup of the foot and ankle problems includes various conventional and advanced imaging modalities. Although magnetic resonance imaging (MRI) has become the preferred investigation for most of the ankle pathologies, nuclear scintigraphy has an important diagnostic role in chronic ankle pain of uncertain etiologies.[1] Limitation of the poor spatial resolution of the bone scan in evaluating a complex anatomical part such as the ankle is effectively overcome by single photon emission computed tomography/computed tomography (SPECT/CT) fusion imaging. By nature, ankle has few common osseous variations, which may be either symptomatic or asymptomatic normal variants. By combining the anatomic and functional data, SPECT/CT helps in recognizing clinically impactful anatomical and radiological variations as exemplified by the presented case.
Case Report
A 38-year-old man presented to our nuclear medicine department with a complaint of left ankle pain for about 5 years duration. His history was unremarkable except for left ankle sprain 7 years ago. His basic blood investigations and rheumatoid screening were negative. Clinically, there was focal tenderness in the posterior aspect of the ankle and subtalar joints, aggravated by extreme passive plantar flexion. Radiograph of the left ankle showed accessory ossicles posterior to the talus (os trigonum) and inferior to the medial malleolus (os subtibiale) [Figure 1].
Figure 1.

Frontal and lateral radiographs of bilateral ankles showed os trigonum (arrow heads) and os subtibiale (arrows) in both sides. (a and b) The left ankle and (c and d) the right
A triple-phase bone scintigraphy was performed after intravenous injection of 18.62 mCi of technetium-99m methyl diphosphonate, with subsequent image acquisition in blood flow, blood pool and 3-h delayed phases. Focal increase in the tracer uptake was appreciated in the posterior aspect of left ankle in all the three phases of imaging [Figure 2]. With SPECT/CT correlation, the abnormal uptake was localized to the os trigonum and adjoining portions of posterior facet of subtalar joint [Figure 3]. Right ankle appeared normal. Accurate anatomical localization by the SPECT/CT helped in the diagnosis of posterior ankle impingement syndrome or os trigonum syndrome. The patient was conservatively managed with oral anti-inflammatory drugs and bracing, and had good response.
Figure 2.
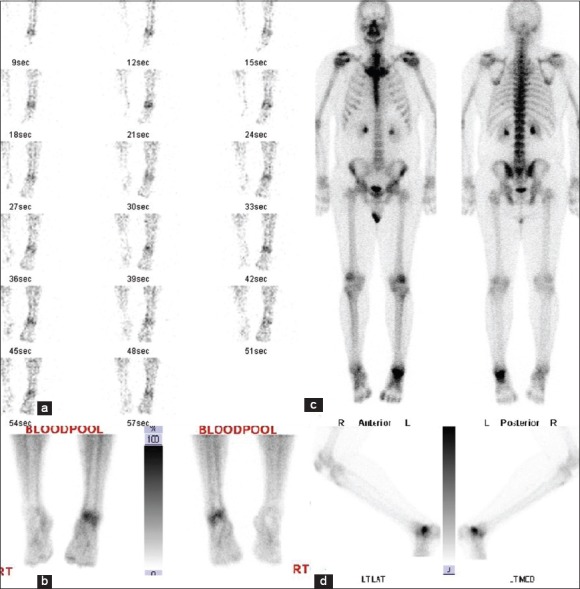
Technetium-99m methyl diphosphonate bone scan images in the blood flow phase (a), blood pool phase (b), delayed whole body (c) and delayed lateral spot view of left ankle (d). Increased tracer distribution and localization are noted in blood flow and blood pool phases respectively. Delayed images demonstrated increased tracer uptake in talocalcaneal region
Figure 3.
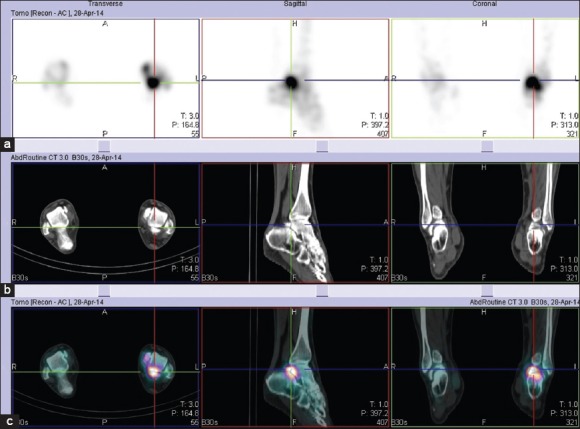
Single photon emission computed tomography (a) computed tomography (b) and combined Single photon emission computed tomography/computed tomography (c) images of the left ankle in three orthogonal planes confirmed that increased tracer uptake clearly corresponds to the posterior aspect of talus, the os trigonum and their synchondrosis
Discussion
Ankle impingements are one of the well-recognized causes of subacute to chronic ankle pain. According to the site, the impingement can be anterior, anteromedial, anterolateral, posterior or posteromedial.[2] Often they occur secondary to the ankle sprain or as a sequel of chronic repetitive, trivial trauma. Posterior ankle impingement is commonly described in the classic ballet dancers, athletes and professional soccer players.[3] Clinically, it presents as pain in the posterior aspect of the ankle exacerbated by either plantar or dorsiflexion. Tenderness is appreciated in the posterior aspect of the ankle with or without a palpable thickening of inflammatory soft tissue, anterior to and separate from the Achilles tendon.
The pathophysiology of posterior ankle impingement involves a nutcracker phenomenon, where the posterior aspect of the talus and nearby soft tissues are compressed by posterior aspect of tibia and calcaneus during forceful or extreme plantar flexion of the foot.[4,5] Osseous abnormalities that are known to be associated with high incidence of posterior ankle impingement include an os trigonum, elongated lateral (stieda) process of the talus, fracture fragments in the posterior aspect of the talus, inferiorly breaking elongated posterior end of the tibia and prominent superior aspect of calcaneus.[2,6]
Magnetic resonance imaging can detect marrow edema of the involved bones and soft tissue abnormalities, in addition to identifying the above-mentioned osseous abnormalities. The soft tissues that are commonly impinged in posterior ankle impingement include the synovium of the ankle and subtalar joints, tendon sheath of the flexor hallucis longus and various ligaments in the posterior aspect of the ankle namely the posterior intermalleolar ligament (a normal variant that is present in some individuals),[7] posterior talo-fibular ligament and posterior tibio-fibular ligament.
Bone scan shows increased tracer uptake in the posterior aspect of the talus and os trigonum in the posterior ankle impingement syndrome.[8] A negative bone scan essentially rules out os trigonum syndrome as a cause of chronic ankle pain.[6] Bone scan is useful in those patients with chronic ankle pain with contraindications for formal MRI examination. SPECT/CT has an additional advantage of cross-sectional anatomic registration of the abnormal tracer uptake. Hence, it can exactly localize and characterize the impingement syndromes and associated soft tissue pathologies.[9] Role of SPECT/CT is considered complementary to MRI in evaluating chronic ankle pain and impingement syndromes.
Conclusion
Our case underlines the efficacy of SPECT/CT as a problem-solving tool in chronic ankle pain of uncertain etiology. Clinicians should be familiar with the potential of SPECT/CT in evaluating such patients and should make the most of this imaging modality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Groshar D, Gorenberg M, Ben-Haim S, Jerusalmi J, Liberson A. Lower extremity scintigraphy: The foot and ankle. Semin Nucl Med. 1998;28:62–77. doi: 10.1016/s0001-2998(98)80019-6. [DOI] [PubMed] [Google Scholar]
- 2.Cerezal L, Abascal F, Canga A, Pereda T, García-Valtuille R, Pérez-Carro L, et al. MR imaging of ankle impingement syndromes. AJR Am J Roentgenol. 2003;181:551–9. doi: 10.2214/ajr.181.2.1810551. [DOI] [PubMed] [Google Scholar]
- 3.Roche AJ, Calder JD, Lloyd Williams R. Posterior ankle impingement in dancers and athletes. Foot Ankle Clin. 2013;18:301–18. doi: 10.1016/j.fcl.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Hedrick MR, McBryde AM. Posterior ankle impingement. Foot Ankle Int. 1994;15:2–8. doi: 10.1177/107110079401500102. [DOI] [PubMed] [Google Scholar]
- 5.Bureau NJ, Cardinal E, Hobden R, Aubin B. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215:497–503. doi: 10.1148/radiology.215.2.r00ma01497. [DOI] [PubMed] [Google Scholar]
- 6.Karasick D, Schweitzer ME. The os trigonum syndrome: Imaging features. AJR Am J Roentgenol. 1996;166:125–9. doi: 10.2214/ajr.166.1.8571860. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg ZS, Cheung YY, Beltran J, Sheskier S, Leong M, Jahss M. Posterior intermalleolar ligament of the ankle: Normal anatomy and MR imaging features. AJR Am J Roentgenol. 1995;165:387–90. doi: 10.2214/ajr.165.2.7618563. [DOI] [PubMed] [Google Scholar]
- 8.Johnson RP, Collier BD, Carrera GF. The os trigonum syndrome: Use of bone scan in the diagnosis. J Trauma. 1984;24:761–4. [PubMed] [Google Scholar]
- 9.Chicklore S, Gnanasegaran G, Vijayanathan S, Fogelman I. Potential role of multislice SPECT/CT in impingement syndrome and soft-tissue pathology of the ankle and foot. Nucl Med Commun. 2013;34:130–9. doi: 10.1097/MNM.0b013e32835c0964. [DOI] [PubMed] [Google Scholar]


