Abstract
Background
The presence of autoantibodies has been proposed as evidence for a role of autoimmunity in autism. This report investigates the prevalence of autoantibodies in children with autism using the luciferase immunoprecipitation systems (LIPS) immunoassay technology. A panel of autoantibody targets against several known and candidate neurological autoantigens, autoimmune-associated autoantigens and viruses was employed.
Methods
Serological analysis was performed on typically developing children (n = 55), developmentally delayed children without autism (n = 24) and children diagnosed with autism (n = 104). Autoantibodies were measured against glutamic acid decarboxylase-65 (GAD65), a CNS autoantigen proposed to be associated with autism and against Ro52, glial fibrillary acidic protein, tyrosine hydroxylase, aquaporin-4, and gamma-enolase, the mouse mammary tumor virus and the xenotropic murine leukemia virus. Antibody levels and seropositivity prevalence were analyzed for statistically significant differences between the three groups.
Results
The majority of the children (98%) were seronegative for all targets in the antigen panel. No GAD65 seropositive children were detected in the cohort. Several low level seropositive sera against several of the protein targets were identified in isolated children in each of the three groups, but there was no difference in prevalence.
Conclusion
Using this panel of antigens and a sensitive, robust assay, no evidence of unusual immunoreactivity was detected in children with autism, providing evidence against a role of autoimmunity against several previously implicated proteins in autism spectrum disorder pathogenesis.
General significance
The idea that autoantibodies represent an underlying cause or are biomarkers for autism pathophysiology is not supported by this report.
Keywords: Autism spectrum disorders, Autoantibodies, Glutamic acid decarboxylase, Virus
1. Introduction
Autism spectrum disorder (ASD) is a behaviorally defined neurodevelopmental disorder [1]. The deficits in social-communication and the presence of restricted interests and repetitive behaviors result in lifelong impairments and disability. ASD has been reported to affect as many as 1 of 88 children in the US [2]. A variety of genetic and environmental triggers have been proposed to be involved in causing autism [3], [4].
One focus of ASD pathophysiology involves a dysfunctional immune response, which is based in part on the controversial findings of autoantibodies in early fetal brain development or during the first few years of a child's life [5]. Likely contributing to often contradictory and conflicting autoantibody results has been the use of immunoassay methodologies measuring autoantibodies against undefined antigens such as by immunohistochemistry of brain tissue and Western blot of brain extracts using human serum [6], [7], [8], [9], [10]. Along these lines, a study by Singer et al. found that more children with ASD demonstrated increased staining intensity on Western blots corresponding to a 100 kDa band in the caudate, putamen and prefrontal cortex and for a 73 kDa band in the cerebellum and cingulate gyrus compared to controls [6]. Another group found immunoreactivity against a 52 kDa cerebellar protein as the major autoantigen species in ASD [7]. However, other studies examining autoantibodies in ASD and controls found no difference in immunoreactivity using Western blot analysis [9] and immunohistochemistry of simian brain slices [10]. Thus, the relevance, if any, of autoantibodies in ASD based on these methodologies remains unclear. Additionally, specific antigen immunoassays have been used to measure autoantibodies in ASD including autoantibodies against target proteins such as glial fibrillary acidic protein (GFAP), myelin basic protein (MBP) and glutamic acid decarboxylase-65 (GAD65) [11], [12], [13], [14], [15]. Singh et al. reported that subjects with ASD had a higher prevalence of autoantibodies against GFAP compared to controls [14], yet another group found no association of autoantibodies against GFAP with ASD [11]. Similar inconsistent reports have been reported for MBP [12], [15]. Although autoantibodies against GAD65, an enzyme responsible for producing the inhibitory transmitter gamma-aminobutyric acid, have also been reported in subjects with ASD [13], these findings have yet to be reproduced by others. Together the inconsistencies of the findings highlight the need for employing more powerful immunoassay methodologies to clarify the frequency of autoantibodies in ASD.
Unlike ELISAs, fluid-phase immunoassays are generally regarded as the most sensitive and specific immunoassay format for identifying autoantibody responses and for the diagnosis of autoimmune diseases [16]. The luciferase immunoprecipitation systems (LIPS) is a fluid-phase immunoassay employing defined recombinant proteins expressed as an in-frame fusion with the low molecular weight light-emitting luciferase protein obtained from Renilla reniformis. LIPS permits robust detection of antibodies against a variety of infectious and autoimmune targets or panels of antigens from such diseases [17]. LIPS has shown high diagnostic performance for the diagnosis of autoimmune diseases that includes type I diabetes [18], [19], Sjögren's syndrome [20], [21], systemic lupus erythematosus [22], myositis [23], anti-cytokine associated diseases [24], [25] and several autoimmune neurological diseases such as stiff person syndrome [26], [27], [28], [29]. In the current study, LIPS was used to investigate whether ASD children had previously reported autoantibodies against GAD65. In addition, antibodies were evaluated against several other autoimmune-associated autoantigens, candidate neurological autoantigens, and viral proteins. For most antigens in this study, detection of autoimmune reactivity has been previously verified in earlier reports using appropriate patient groups in which (a) the target antigen or autoantigens are known and (b) the cohort contains patients positive for the clinical diagnosis and positive for the target antibodies in their serum.
2. Methods
The cohort of children with ASD and controls were evaluated at the National Institute of Mental Health, National Institutes of Health, Bethesda, MD under institutional review board approved protocol NCT00298246: Clinical and Immunological Investigations of Subtypes of Autism. The children with ASD (n = 104; mean age = 4.3 yr; SD = 1.3; range = 2.2–7.4 yrs), were diagnosed by Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM IV) [30] after administration of the Autism Diagnostic Observation Schedule [31] and the Autism Diagnostic Interview (ADI-R), a semi-structured parent interview concerning all domains of impairment in autism [32]. Typically developing children (n = 55) were used as a control group, (mean age = 3.3 yr; SD = 1.4; range = 1.3–7.6 yrs). A control group of developmentally delayed children without autism (n = 24) was also employed and was approximately matched on a developmental level to the autistic group (mean age = 4.3 yr; SD = 1.2; range = 2.7–7.6 yrs). Lastly, following antibody evaluation of the cohort, one sample was excluded from the analysis. This sample, from a subject with ASD, had unusual immunoreactivity against five of the six proteins. It appeared that the polyreactive serum recognized the Renilla luciferase which is the reporter enzyme in LIPS antibody test and so, the sample was excluded from consideration, leaving 103 samples in the ASD group.
Previously described LIPS tests were employed to detect autoantibodies against GAD65, Ro52, GFAP, aquaporin-4 (AQP-4), and tyrosine hydroxylase (TH) [18], [19], [22]. Three additional new antigen constructs for gamma-enolase (γ-enolase, neuron specific enolase), the gag protein from xenotropic murine leukemia virus (XMRV) and p24 from mouse mammary tumor virus (MMTV) were generated in the pREN2 vector [26] as C-terminal Renilla luciferase antigen fusions. γ-Enolase was chosen as a potential target based on its high expression in neurons and reports of it being an autoantigen target in post-streptococcal autoimmune CNS disease [33]. MMTV is a potential zoonotic infection in humans [34] and XMRV infection was reported to cause chronic fatigue [35]. Both the γ-enolase and MMTV p24 were amplified by PCR using commercial cDNA plasmids. The XMRV gag protein was generated by synthetic gene synthesis (Blue Heron, Bothell, WA) using optimized human codons. The three new expression constructs were verified by sequencing and details of their construction are available upon request.
LIPS testing was performed as previously described [18], [19]. Light units were measured in a Berthold LB 960 Centro luminometer (Berthold Technologies, Germany) using coelenterazine substrate mix (Promega, Madison, WI). In some cases, control sera samples from type I diabetes patients and systemic lupus erythematosus were used as known positive controls. Seropositivity status for GAD65, Ro52, GFAP, AQP-4 and TH was based on known cut-offs. For the three new autoantigens (γ-enolase, gag XMRV and p24 MMTV), cut-off values were assigned based on the mean plus three standard deviations of the typically developing children controls. Researchers were blinded to patient diagnosis during analysis.
The non-parametric Mann–Whitney U statistical test was used for comparison of antibody levels in the three different groups. For comparing the seroprevalence of antibody responses in the different groups, contingency tables were generated and analyzed using the Fisher exact test for statistical significance.
3. Results
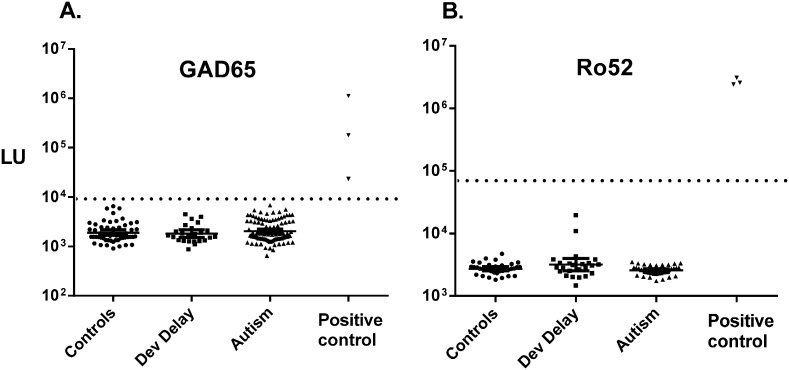
Based on the report that children with ASD have GAD65 autoantibodies [13], LIPS was used to measure autoantibodies against this target in a cohort with ASD. As described in the Methods section, three sera from subjects with Type I diabetes, an autoimmune disease known to generate anti-GAD65 autoantibodies, were employed as positive controls (17–19). As expected, the three type I diabetes sera showed highly elevated levels of GAD65 autoantibodies all above the established cut-off (Fig. 1A). However, testing of serum from the typically developed children (n = 55), developmentally delayed children (n = 24) and children with ASD (n = 103) demonstrated no seropositive autoantibodies to GAD65: all measured LU values were below the cut-off (Fig. 1A). To determine if the ASD children might have a lupus-like autoimmune phenotype, the LIPS Ro52 autoantibody test was employed (20–23). In contrast to three positive control samples from subjects with systemic lupus erythematosus, none of the children in the ASD cohort showed seropositivity with Ro52. All values were below the known cut-off (Fig. 1B). It should be noted that LIPS tests for both GAD65 and Ro52 detected antibody levels in the positive control samples that were often 10–1000-fold higher than the control and ASD samples. Therefore, any subtle low positivity, if present in the cohort, should have been detected (Fig. 1). These findings rule out the possibility that GAD65 and Ro52 autoantibodies are biomarkers of ASD.
Fig. 1.
Lack of autoantibodies against GAD65 and Ro52 in the ASD cohort. Autoantibody levels were evaluated for (A) GAD65 and (B) Ro52 in the cohort. Additional positive control serum samples from type I diabetes and systemic lupus erythematosus subjects were included for the detection of GAD65 and Ro52 autoantibodies, respectively. The light units (LU) plotted on the y-axis using a log10 scale measure the autoantibody levels for each sample. The dotted lines represent the cut-off values for determining seropositivity for each autoantigen.
Autoantibodies against several other known or potential autoantigen targets, including GFAP, TH, γ-enolase and AQP-4 (the autoantigen in neuromyelitis optica), were also measured by LIPS in the three groups. In certain individuals, occasional sporadic, low-level seropositive autoantibodies against the four proteins were detected. For example, two of the 55 typically developing, two of the 25 developmental delayed and four of the 103 ASD children were seropositive, exhibiting low levels of autoantibodies to GFAP (Table 1). However, statistical analysis of the GFAP seropositivity by Fisher's exact testing with contingency tables revealed no significant differences in seroprevalence between the three groups. Similar analyses for autoantibodies against AQP-4, TH, and γ-enolase also revealed occasional weak seropositivity in the children, but no significant increase in seropositivity was detected in ASD (Table 1).
Table 1.
Prevalence of antibodies in the autism cohort.
| Antigen | Typically developing (N = 55) seropositivity | Developmental delay (N = 25) seropositivity | ASD (N = 103) seropositivitya |
|---|---|---|---|
| GAD-65 | 0/55 | 0/25 | 0/103 |
| Ro52 | 0/55 | 0/25 | 0/103 |
| GFAP | 2/55 | 2/25 | 4/103 |
| AQP-4 | 3/55 | 0/25 | 5/103 |
| TH | 1/55 | 0/25 | 1/103 |
| γ-Enolase | 1/55 | 0/25 | 2/103 |
| XMRV gag | 1/55 | 0/25 | 0/103 |
| MMTV p24 | 1/55 | 0/25 | 0/103 |
Fisher exact tests revealed no statistical difference in prevalence of antibodies against the eight targets in ASD compared to typically developing and developmental delay children.
Based on the known ability of LIPS to detect robust antibodies to the capsid proteins from HIV [36] and HTL-I retroviruses [37], we explored the possibility of detecting antibodies against two capsid proteins derived from MMTV and gag of XMRV in the cohort. Based on a cut-off derived from the healthy control children, no significant immunoreactivities were detected in any of the ASD or other children (Table 1).
4. Discussion
Primarily, we attempted to reproduce previous reports showing a high prevalence of GAD-65 autoantibodies in children with ASD. For our investigation, a validated GAD-65 LIPS test that performs with the same high sensitivity and specificity as the gold-standard radiolabel binding immunoassay was employed [18]. Using this LIPS assay, positive control clinical serum samples were used to confirm the capacity of LIPS to detect autoantibodies against GAD65. However, no seropositive GAD65 autoantibodies were detected in any of the children from the autism cohort, which was unlike the earlier study that detected 15% seropositivity in an ASD cohort [13]. One likely explanation for this discrepancy in GAD65 prevalence in ASD is that the previous study used a solid-phase ELISA. This test format, in which target antigen proteins are bound to the ELISA plate, is known to be susceptible to non-specific reactivities [16]. Thus, it is possible that the reactivity to GAD65 in earlier ELISA-based studies was a result of such non-specific signals.
Antibodies against several other autoantigens also show no association with ASD. The lack of autoantibodies against Ro52, a commonly detectable target of autoantibodies in lupus [22], rules out a lupus-like neurological phenotype in ASD. This finding also eliminates the possibility that Ro52 is the 52 kDa target antigen seen in ASD sera by Western blotting [7]. Additionally, no evidence was found supporting a role of increased prevalence of GFAP autoantibodies in ASD, which is in agreement with a previous study [11]. Specifically, 1% and 2%, of the ASD and control groups, respectively, showed GFAP seropositivity, but the absolute levels were low. Thus, both a neuronal and a glial autoantibody either were not present or their prevalence was not elevated in ASD subjects. No differences between the three groups were found for the prevalence of autoantibodies against AQP-4, tyrosine hydroxylase or neuron-specific γ-enolase. The lack of autoantibodies against AQP-4, an astrocytic protein involved with maintenance of the blood brain barrier and a pathognomonic autoantibody in neuromyelitis optica rules out this target as a potential source of autoimmune blood brain barrier disruption in ASD. Moreover, seropositivity to the neuron-specific γ-enolase was found in 1% and 2%, of the ASD and control groups, respectively, but again the absolute levels were low. Also, no difference was seen between the three groups for TH autoantibodies. Thus, two more neuronal autoantibody targets either were not present or their prevalence was not elevated in ASD subjects. TH is particularly relevant since it is the first enzyme in the biosynthetic pathway for the catecholamines dopamine and norepinephrine, which are major neurotransmitters in circuits subserving affect and attention. Similar to our GFAP observations there are occasional sporadic low level signals to several of these targets that likely reflect uncharacterized immune responses.
Two possible viral targets, MMTV and XMRV, also showed no significant immunoreactivity in the cohort. The fact that we did not detect antibodies against XMRV in autism using LIPS is also in agreement with two other reports [38], [39], which used mainly polymerase chain reaction molecular methods for detection. Thus, three independent reports using different methodologies do not support detection of the XMRV artifact in ASD. Despite no evidence for a role of XMRV or MMTV, additional studies are needed to determine if other infectious agents, or the body's response to such infections agents, might play a role.
From the results presented here, we conclude that autoantibodies against GAD65 and the other targets that we tested are unlikely to be significant contributors to autism spectrum disorder. However, given the limited number of antigens examined, it is possible there are other neurological antigens and target proteins which might targets of humoral responses in ASD. It would be worthwhile to explore the immunoreactivity reported in ASD by several groups that employed Western blot [7] and immunohistochemical techniques [7], [40] by using high sensitivity LIPS assays. These investigations would first require that the antigens be identified, in order that defined recombinant proteins might be used to construct quantitative immunoassays for analysis of a large number of controls and ASD subjects. The presence of an autoimmune component in ASD is an important question to resolve in a definitive fashion. The data presented in this report suggest that newer more specific and defined methodologies can make a substantial contribution to realizing this goal.
5. Conclusions
This study employed a fluid-phase immunoassay, LIPS, which shows high diagnostic performance for autoantibodies present in multiple autoimmune disorders and for infectious agents. Using this assay, we found no evidence of autoantibodies against GAD65 and several other autoantigens in children with autism spectrum disorder. No antibodies were detected against two retroviruses, MMTV or XMRV. These results suggest that autoimmunity against the tested neuronal, astrocytic, and other proteins is not likely a causative factor or diagnostic biomarker in autism.
Conflict of interest
The authors declare no conflict of interest.
Transparency Document
Transparency document
Acknowledgments
This work was supported by the intramural research programs of the Clinical Center, National Institutes of Health, National Institute of Dental and Craniofacial Research, and the National Institute of Mental Health protocol 06-M-0102; NCT00298246. We thank current and former members of the Pediatrics and Developmental Neuroscience Branch, and extend sincere gratitude to the children and families who participated in this research.
Footnotes
The Transparency document associated with this article can be found, in the online version.
References
- 1.Association A. P. 5th edn. American Psychiatric Association; Washington, D.C.: 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. [Google Scholar]
- 2.Investigators A. a. D. D. M. N. S. Y. P., Prevention C. f. D. C. a Prevalence of autism spectrum disorders — autism and developmental disabilities monitoring network, 14 sites, United States, 2008. MMWR Surveill. Summ. 2012;61:1–19. [PubMed] [Google Scholar]
- 3.Devlin B., Scherer S.W. Genetic architecture in autism spectrum disorder. Curr. Opin. Genet. Dev. 2012;22:229–237. doi: 10.1016/j.gde.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Lai M.C., Lombardo M.V., Baron-Cohen S. Autism. Lancet. 2014;383:896–910. doi: 10.1016/S0140-6736(13)61539-1. [DOI] [PubMed] [Google Scholar]
- 5.Gesundheit B., Rosenzweig J.P., Naor D., Lerer B., Zachor D.A., Prochazka V., Melamed M., Kristt D.A., Steinberg A., Shulman C. Immunological and autoimmune considerations of autism spectrum disorders. J. Autoimmun. 2013;44:1–7. doi: 10.1016/j.jaut.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Singer H.S., Morris C.M., Williams P.N., Yoon D.Y., Hong J.J., Zimmerman A.W. Antibrain antibodies in children with autism and their unaffected siblings. J. Neuroimmunol. 2006;178:149–155. doi: 10.1016/j.jneuroim.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 7.Wills S., Cabanlit M., Bennett J., Ashwood P., Amaral D.G., Van de Water J. Detection of autoantibodies to neural cells of the cerebellum in the plasma of subjects with autism spectrum disorders. Brain Behav. Immun. 2009;23:64–74. doi: 10.1016/j.bbi.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazur-Kolecka B., Cohen I.L., Gonzalez M., Jenkins E.C., Kaczmarski W., Brown W.T., Flory M., Frackowiak J. Autoantibodies against neuronal progenitors in sera from children with autism. Brain Dev. 2014;36:322–329. doi: 10.1016/j.braindev.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Morris C.M., Zimmerman A.W., Singer H.S. Childhood serum anti-fetal brain antibodies do not predict autism. Pediatr. Neurol. 2009;41:288–290. doi: 10.1016/j.pediatrneurol.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 10.Rossi C.C., Van de Water J., Rogers S.J., Amaral D.G. Detection of plasma autoantibodies to brain tissue in young children with and without autism spectrum disorders. Brain Behav. Immun. 2011;25:1123–1135. doi: 10.1016/j.bbi.2011.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirkman N.J., Libbey J.E., Sweeten T.L., Coon H.H., Miller J.N., Stevenson E.K., Lainhart J.E., McMahon W.M., Fujinami R.S. How relevant are GFAP autoantibodies in autism and tourette syndrome? J. Autism Dev. Disord. 2008;38:333–341. doi: 10.1007/s10803-007-0398-9. [DOI] [PubMed] [Google Scholar]
- 12.Libbey J.E., Coon H.H., Kirkman N.J., Sweeten T.L., Miller J.N., Stevenson E.K., Lainhart J.E., McMahon W.M., Fujinami R.S. Are there enhanced MBP autoantibodies in autism? J. Autism Dev. Disord. 2008;38:324–332. doi: 10.1007/s10803-007-0400-6. [DOI] [PubMed] [Google Scholar]
- 13.Rout U.K., Mungan N.K., Dhossche D.M. Presence of GAD65 autoantibodies in the serum of children with autism or ADHD. Eur. Child Adolesc. Psychiatry. 2012;21:141–147. doi: 10.1007/s00787-012-0245-1. [DOI] [PubMed] [Google Scholar]
- 14.Singh V.K., Warren R., Averett R., Ghaziuddin M. Circulating autoantibodies to neuronal and glial filament proteins in autism. Pediatr. Neurol. 1997;17:88–90. doi: 10.1016/s0887-8994(97)00045-3. [DOI] [PubMed] [Google Scholar]
- 15.Singh V.K., Warren R.P., Odell J.D., Warren W.L., Cole P. Antibodies to myelin basic protein in children with autistic behavior. Brain Behav. Immun. 1993;7:97–103. doi: 10.1006/brbi.1993.1010. [DOI] [PubMed] [Google Scholar]
- 16.Liu E., Eisenbarth G.S. Accepting clocks that tell time poorly: fluid-phase versus standard ELISA autoantibody assays. Clin. Immunol. 2007;125:120–126. doi: 10.1016/j.clim.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burbelo P.D., Lebovitz E.E., Notkins A.L. Luciferase immunoprecipitation systems for measuring antibodies in autoimmune and infectious diseases. Transl. Res. 2015;165:325–335. doi: 10.1016/j.trsl.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burbelo P.D., Hirai H., Issa A.T., Kingman A., Lernmark A., Ivarsson S.A., Notkins A.L., Iadarola M.J. Comparison of radioimmunoprecipitation with luciferase immunoprecipitation for autoantibodies to GAD65 and IA-2beta. Diabetes Care. 2010;33:754–756. doi: 10.2337/dc09-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burbelo P.D., Lebovitz E.E., Bren K.E., Bayat A., Paviol S., Wenzlau J.M., Barriga K.J., Rewers M., Harlan D.M., Iadarola M.J. Extrapancreatic autoantibody profiles in type I diabetes. PLoS One. 2012;7:e45216. doi: 10.1371/journal.pone.0045216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ching K.H., Burbelo P.D., Gonzalez-Begne M., Roberts M.E., Coca A., Sanz I., Iadarola M.J. Salivary anti-Ro60 and anti-Ro52 antibody profiles to diagnose Sjogren's syndrome. J. Dent. Res. 2011;90:445–449. doi: 10.1177/0022034510390811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burbelo P.D., Leahy H.P., Issa A.T., Groot S., Baraniuk J.N., Nikolov N.P., Illei G.G., Iadarola M.J. Sensitive and robust luminescent profiling of anti-La and other autoantibodies in Sjogren's syndrome. Autoimmunity. 2009;42:515–524. doi: 10.1080/08916930902911738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ching K.H., Burbelo P.D., Tipton C., Wei C., Petri M., Sanz I., Iadarola M.J. Two major autoantibody clusters in systemic lupus erythematosus. PLoS One. 2012;7:e32001. doi: 10.1371/journal.pone.0032001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gan L., O'Hanlon T.P., Gordon A.S., Rider L.G., Miller F.W., Burbelo P.D. Twins discordant for myositis and systemic lupus erythematosus show markedly enriched autoantibodies in the affected twin supporting environmental influences in pathogenesis. BMC Musculoskelet. Disord. 2014;15:67. doi: 10.1186/1471-2474-15-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Browne S.K., Burbelo P.D., Chetchotisakd P., Suputtamongkol Y., Kiertiburanakul S., Shaw P.A., Kirk J.L., Jutivorakool K., Zaman R., Ding L. Adult-onset immunodeficiency in Thailand and Taiwan. N. Engl. J. Med. 2012;367:725–734. doi: 10.1056/NEJMoa1111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burbelo P.D., Browne S.K., Sampaio E.P., Giaccone G., Zaman R., Kristosturyan E., Rajan A., Ding L., Ching K.H., Berman A. Anti-cytokine autoantibodies are associated with opportunistic infection in patients with thymic neoplasia. Blood. 2010;116:4848–4858. doi: 10.1182/blood-2010-05-286161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burbelo P.D., Groot S., Dalakas M.C., Iadarola M.J. High definition profiling of autoantibodies to glutamic acid decarboxylases GAD65/GAD67 in stiff-person syndrome. Biochem. Biophys. Res. Commun. 2008;366:1–7. doi: 10.1016/j.bbrc.2007.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ching K.H., Burbelo P.D., Kimball R.M., Clawson L.L., Corse A.M., Iadarola M.J. Recombinant expression of the AChR-alpha1 subunit for the detection of conformation-dependent epitopes in myasthenia gravis. Neuromuscul. Disord. 2011;21:204–213. doi: 10.1016/j.nmd.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakane S., Higuchi O., Koga M., Kanda T., Murata K., Suzuki T., Kurono H., Kunimoto M., Kaida K., Mukaino A. Clinical features of autoimmune autonomic ganglionopathy and the detection of subunit-specific autoantibodies to the ganglionic acetylcholine receptor in Japanese patients. PLoS One. 2015;10:e0118312. doi: 10.1371/journal.pone.0118312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higuchi O., Hamuro J., Motomura M., Yamanashi Y. Autoantibodies to low-density lipoprotein receptor-related protein 4 in myasthenia gravis. Ann. Neurol. 2011;69:418–422. doi: 10.1002/ana.22312. [DOI] [PubMed] [Google Scholar]
- 30.Association A.P. 4th edn. American Psychiatric Association; Washington, DC: 1994. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. [Google Scholar]
- 31.Lord C., Rutter M., DiLavore P.C., Risi S. Western Psychological Services; Los Angeles, California: 1999. Autism Diagnostic Observation Schedule (ADOS) [Google Scholar]
- 32.Lord C., Rutter M., Le Couteur A. Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J. Autism Dev. Disord. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 33.Dale R.C., Candler P.M., Church A.J., Wait R., Pocock J.M., Giovannoni G. Neuronal surface glycolytic enzymes are autoantigen targets in post-streptococcal autoimmune CNS disease. J. Neuroimmunol. 2006;172:187–197. doi: 10.1016/j.jneuroim.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 34.Voisset C., Weiss R.A., Griffiths D.J. Human RNA "rumor" viruses: the search for novel human retroviruses in chronic disease. Microbiol. Mol. Biol. Rev. 2008;72:157–196. doi: 10.1128/MMBR.00033-07. (table of contents) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lombardi V.C., Ruscetti F.W., Das G.J., Pfost M.A., Hagen K.S., Peterson D.L., Ruscetti S.K., Bagni R.K., Petrow-Sadowski C., Gold B. Detection of an infectious retrovirus, XMRV, in blood cells of patients with chronic fatigue syndrome. Science. 2009;326:585–589. doi: 10.1126/science.1179052. [DOI] [PubMed] [Google Scholar]
- 36.Burbelo P.D., Bayat A., Rhodes C.S., Hoh R., Martin J.N., Fromentin R., Chomont N., Hutter G., Kovacs J.A., Deeks S.G. HIV antibody characterization as a method to quantify reservoir size during curative interventions. J. Infect. Dis. 2014;209:1613–1617. doi: 10.1093/infdis/jit667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burbelo P.D., Meoli E., Leahy H.P., Graham J., Yao K., Oh U., Janik J.E., Mahieux R., Kashanchi F., Iadarola M.J. Anti-HTLV antibody profiling reveals an antibody signature for HTLV-I-associated myelopathy/tropical spastic paraparesis (HAM/TSP) Retrovirology. 2008;5:96. doi: 10.1186/1742-4690-5-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Satterfield B.C., Garcia R.A., Gurrieri F., Schwartz C.E. PCR and serology find no association between xenotropic murine leukemia virus-related virus (XMRV) and autism. Mol. Autism. 2010;1:14. doi: 10.1186/2040-2392-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lintas C., Guidi F., Manzi B., Mancini A., Curatolo P., Persico A.M. Lack of infection with XMRV or other MLV-related viruses in blood, post-mortem brains and paternal gametes of autistic individuals. PLoS One. 2011;6:e16609. doi: 10.1371/journal.pone.0016609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wills S., Rossi C.C., Bennett J., Martinez Cerdeno V., Ashwood P., Amaral D.G., Van de Water J. Further characterization of autoantibodies to GABAergic neurons in the central nervous system produced by a subset of children with autism. Mol. Autism. 2011;2:5. doi: 10.1186/2040-2392-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document