Abstract
We report on a patient with Amanita pantherina poisoning who showed a burst suppression pattern on electroencephalography during a comatose state. The patient recovered without sequelae a week after ingestion. Burst suppression pattern is defined as alternating bursts and periods of electrical silence, and it is associated with comatose states of various causes. The major toxins contained in A. pantherina are ibotenic acid, an excitatory amino acid at the glutamate receptors, and muscimol, an agonist of the gamma-aminobutyric acid receptors. Alteration of the synaptic transmission in the central nervous system by these toxins may lead to a burst suppression pattern.
Keywords: Burst suppression, Muscimol, Ibotenic acid, Amanita pantherina, GABA receptor
1. Introduction
Burst suppression pattern is a peculiar EEG sign which is observed in some special conditions: deep general anesthesia [1], cerebral hypoxia [2], hypothermia [3], early infantile encephalopathy [4], baclofen overdose [5], and dengue encephalopathy [6]. The brain condition associated with this EEG pattern is serious and irreversible in many causes, but it may be reversible in cases resulting from anesthesia or drug intoxication. Amanita pantherina is a mushroom which is widespread in Asia, on the North American continent, in Europe, and in some areas of the southern hemisphere [7]. It contains ibotenic acid and muscimol [8,9]. We report on a patient with A. pantherina poisoning who developed a comatose state associated with a burst suppression pattern on EEG and recovered to a normal state after treatment.
2. Case report
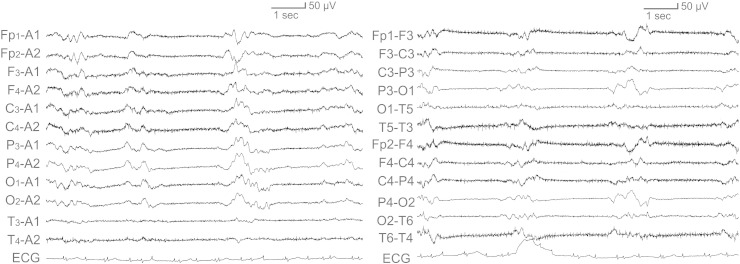
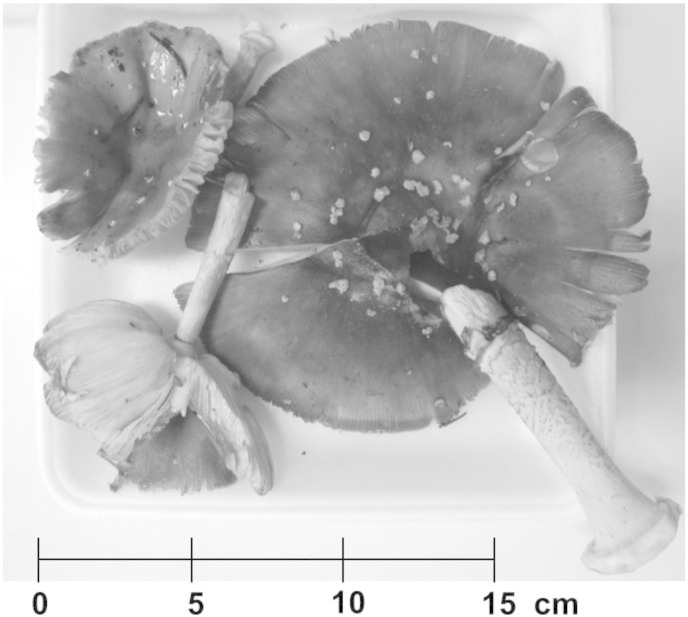
A 68-year-old woman was transferred to our emergency room because of an acute comatose state (Glasgow Coma Scale, E1V1M2) and vomiting. The blood pressure, pulse rate, body temperature, and oxygen saturation were 120/66 mm Hg, 45 beats/min, 35.6 °C, and 100% with an oxygen supply of 6 L/min through a face mask. She showed Cheyne–Stokes respiration. Her pupils were normal in size and reactive to light. Spontaneous repetitive downward gaze was observed, and doll's eye phenomenon was absent. Decorticate posture appeared intermittently. Tendon reflexes were increased, associated with extensor plantar responses. Routine laboratory tests, including blood glucose, electrolytes, and ammonia, as well as cerebrospinal fluid were unremarkable. Brain CT showed no abnormality. Electroencephalogram (EEG) recorded 4 h after admission showed a burst suppression pattern (Fig. 1). There were no jerks associated with the bursts. It was disclosed that the patient had eaten some pieces of wild mushrooms grown in her yard 3 h before admission mistaken for edible ones, and the species was identified from the remaining mushrooms as A. pantherina (Fig. 2). We diagnosed her as having A. pantherina poisoning and gave her a supportive treatment with a relatively rapid supplement of fluid infusion. The patient gradually recovered from coma 18 h after mushroom ingestion. She became alert on Day 2 after ingestion, but showed depression for the following few days; the follow-up EEG recorded 29 h after ingestion returned to normal activity. No hepatic or renal dysfunction appeared. The patient was discharged without any residual deficit a week after ingestion.
Fig. 1.
Burst suppression EEG recorded during a comatose state 7 h after mushroom digestion.
Fig. 2.
The remaining mushroom, Amanita pantherina, which the patient ate before admission.
3. Discussion
As the patient developed coma 3 h after ingestion of A. pantherina without any other cause, she was diagnosed as having A. pantherina poisoning, though a chromatographic assay of the poison was not performed. Clinical symptoms of A. pantherina poisoning consist of a dysfunction of the peripheral autonomic nerves, gastrointestinal tract, and central nervous system and appear from 30 min to 2 h after ingestion [7–9]. Amanita pantherina poisoning is less lethal compared with poisoning by some other species of the Amanita genus, and patients suffering from the poisoning usually recover without consequences. The course of illness in our patient fits well with that of A. pantherina poisoning, but the severity of symptoms may vary depending on the amount ingested and individual susceptibility to the toxins [7–9].
This is the first report on burst suppression pattern on EEG caused by mushroom poisoning. Burst suppression pattern is a peculiar EEG sign which is defined as alternating bursts and periods of electrical silence [10]. With regard to changes in the neuronal membrane underlying this pattern, bursts are associated with phasic depolarization, and suppression episodes are associated with an electrical silence in anesthetized cats [10]. The synaptic mechanism of burst suppression EEG includes glutamate and gamma-aminobutyric acid (GABA) transmission in the neocortex [11]. Amanita pantherina contains several kinds of toxins, but the major active toxins have been found to be ibotenic acid and muscimol, possibly together with their metabolites [12]. Ibotenic acid acts as an excitatory amino acid at the glutamate receptors, and muscimol acts as an agonist of the GABA receptors. It was observed that muscimol produced burst suppression activity in a rat neocortical slice EEG preparation [13]. Both toxins cross the blood–brain barrier via an active transport system [14]. Therefore, general administration of these two toxins may be hypothesized to potentiate glutamate and GABA transmission in the central nervous system, leading to burst suppression pattern on EEG.
Conflict of interest statement
The authors declare that they have no conflict of interest.
References
- 1.Brown E.N., Lydic B.R., Schiff N.D. General anesthesia, sleep, and coma. N Engl J Med. 2010;363:2638–2650. doi: 10.1056/NEJMra0808281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young G.B. The EEG in coma. J Clin Neurophysiol. 2000;17:473–485. doi: 10.1097/00004691-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Marion D.W., Penrod L.E., Kelsey S.F., Obrist W.D., Kochanek P.M., Palmer A.M., Wisniewski S.R., DeKosky S.T. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997;336:540–546. doi: 10.1056/NEJM199702203360803. [DOI] [PubMed] [Google Scholar]
- 4.Ohtahara S., Yamatogi Y. Epileptic encephalopathies in early infancy with suppression-burst. J Clin Neurophysiol. 2003;20:398–407. doi: 10.1097/00004691-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Caron E., Morgan R., Wheless J.W. An unusual cause of flaccid paralysis and coma: baclofen overdose. J Clin Neurol. 2014;29:555–559. doi: 10.1177/0883073813479668. [DOI] [PubMed] [Google Scholar]
- 6.Liou L.M., Lan S.H., Lai C.L. Electroencephalography burst suppression in a patient with dengue encephalopathy: a case report. Clin Neurophysiol. 2008;119:2205–2208. doi: 10.1016/j.clinph.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Bosman C.K., Berman L., Isaacson M., Wolfowitz B., Parkes J. Mushroom poisoning caused by Amanita pantherina. S Afr Med J. 1965;39:983–986. [PubMed] [Google Scholar]
- 8.Satora L., Pach D., Ciszowski K., Winnik L. Panther cap Amanita pantherina poisoning case report and review. Toxicon. 2006;47:605–607. doi: 10.1016/j.toxicon.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Vendramin A., Brvar M. Amanita muscaria and Amanita pantherina poisoning: two syndromes. Toxicon. 2014;90:269–272. doi: 10.1016/j.toxicon.2014.08.067. [DOI] [PubMed] [Google Scholar]
- 10.Steriade M., Amzica F., Contreras D. Cortical and thalamic cellular correlates of electroencephalographic burst-suppression. Clin Neurophysiol. 1994;90:1–16. doi: 10.1016/0013-4694(94)90108-2. [DOI] [PubMed] [Google Scholar]
- 11.Lukatch H.S., Kiddoo C.E., MacIver M.B. Anesthetic-induced burst suppression EEG activity requires glutamate-mediated excitatory synaptic transmission. Cereb Cortex. 2005;15:1322–1331. doi: 10.1093/cercor/bhi015. [DOI] [PubMed] [Google Scholar]
- 12.Michelot D., Melendez-Howell L.M. Amanita muscaria: chemistry, biology, toxicology, and ethnomycology. Mycol Res. 2003;107:131–146. doi: 10.1017/s0953756203007305. [DOI] [PubMed] [Google Scholar]
- 13.Lukatch H.S., Maclver M.B. Synaptic mechanisms of thiopental-induced alterations in synchronized cortical activity. Anesthesiology. 1996;84:1425–1434. doi: 10.1097/00000542-199606000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Olpe H.R., Koella W.P. The action of muscimol on neurons of the substantia nigra of the rat. Experientia. 1978;34 doi: 10.1007/BF01944700. :235. [DOI] [PubMed] [Google Scholar]