Abstract
Atrial fibrillation (AF) is a common complication of acute myocardial infarction (AMI) and this arrhythmia is associated with increased morbidity and mortality in patients with AMI. Limited information is available, however, about changing, and contemporary, trends in the incidence and death rates associated with AF complicating AMI. We examined the magnitude and impact of AF, and the risk of stroke and hospital and long-term death rates, in a population-based study of patients hospitalized with AMI. The study population consisted of 7,513 residents of the Worcester, MA, metropolitan area hospitalized with AMI at all greater Worcester medical centers during 9 biennial years between 1990 and 2005. The overall incidence of AF complicating AMI was 13.3% and the rates of AF increased during the most recent years under study. Patients who developed AF were at greater risk for acute stroke (adjusted OR = 2.25; 95% CI 1.36, 3.71) and dying during hospitalization (adjusted OR = 1.79; 95% CI 1.46, 2.19) in comparison to patients who did not develop AF during hospitalization for AMI. Post-discharge survival was significantly poorer in patients who developed AF. The odds of dying after AF did not change appreciably over the years under study. In conclusion, the results of this study in residents of a large New England metropolitan area suggest that AF remains a frequent complication of AMI and is associated with a poor prognosis. Increased surveillance and targeted therapeutic approaches appear warranted for these high-risk patients.
Keywords: Atrial fibrillation, acute myocardial infarction, population-based study
Introduction
Using data from the Worcester Heart Attack Study, a community-wide investigation of patients hospitalized with acute myocardial infarction (AMI) in a large New England community,1,2 we examined 15-year trends in the incidence rates of atrial fibrillation (AF), patient characteristics associated with the occurrence of AF, and the association between AF and the development of acute stroke as well as hospital and long-term mortality. The study population consisted of 7,513 residents of the Worcester, Massachusetts, metropolitan area without a history of AF hospitalized with AMI at all greater Worcester medical centers in 9 annual periods between 1990 and 2005.
Methods
The Worcester Heart Attack Study is an ongoing population-based investigation that is examining long-term trends in the incidence, hospital, and post-discharge case-fatality rates of AMI among residents of the Worcester metropolitan area hospitalized at all greater Worcester medical centers.1,2
The details of this study have been described previously.1,2 In brief, the medical records of residents of the Worcester metropolitan area hospitalized for possible AMI at all greater Worcester medical centers were individually reviewed and a diagnosis of AMI was validated according to predefined criteria.2 The presence of AF was determined based on information available from the medical record and review of electrocardiographic findings obtained during hospitalization for AMI. All electrocardiographic findings were reviewed by the physician project coordinator and were independently interpreted at each greater Worcester hospital by staff physicians and overread by the hospital computer. The criteria for AF included documentation of AF in the attending physicians’ notes or occurrence of typical electrocardiographic changes consistent with a diagnosis of AF.2,3 We did not collect information about the timing of AF relative to hospital admission or whether the AF was paroxysmal or sustained.
Patients with a history of AF were excluded from the present analyses (n=979) since we wanted to examine the magnitude of, and long-term trends in, the incidence rates of new onset AF and its natural history. The sample was further restricted to patients who did not undergo coronary artery bypass surgery during hospitalization for AMI (n=409). Post-operative AF is relatively common in patients undergoing coronary bypass surgery and may be caused by different factors than AF that develops in patients who do not undergo this procedure.
Demographic and clinical data were abstracted from the hospital medical records of geographically eligible patients with confirmed AMI by trained study physicians and nurses. Information was collected about patient's age, sex, prior comorbidities, AMI order (initial vs. prior), type (Q wave vs. non–Q wave) and location (anterior vs. inferior/posterior), hospital treatments, length of hospital stay, and hospital discharge status. Information was also collected about the occurrence of clinically significant in-hospital complications including AF,3 stroke,4 heart failure,5 and cardiogenic shock6 by our trained reviewers. Survival status after hospital discharge was ascertained through the review of medical records for additional hospitalizations and a statewide and national search of death certificates for residents of the Worcester metropolitan area.
We examined differences in the characteristics, treatment practices, and hospital outcomes according to the hospital development of AF through the use of chi-square and t-tests for discrete and continuous variables, respectively. Short-term prognosis in each of the periods under study was examined by calculating in-hospital case-fatality rates (CFRs). Logistic regression analysis was used to examine changes over time in the occurrence of AF, and in-hospital CFRs according to the occurrence of AF, controlling for factors associated with the risk of AF and short-term death rates. Multivariate logistic regression analysis was also used to examine the association between the occurrence of AF and inhospital stroke, 30-day post admission mortality, and 1-year post-discharge all-cause mortality. We did not control for the receipt of cardiac medications or coronary reperfusion strategies in these analyses due to the potential for confounding by treatment indication and lack of data regarding the timing of administration of these therapies. A proportional hazards regression analysis was used to examine the association between AF and long-term survival after hospital discharge, controlling for a number of potentially confounding demographic and clinical factors and duration of post-discharge follow-up.
Results
Of the 7,513 residents of the Worcester metropolitan area (mean age = 69 years; 43% female) hospitalized between 1990 and 2005 with confirmed AMI, and without a prior history of AF, at all greater Worcester medical centers, a total of 999 patients (13.3%) developed AF during hospitalization for AMI.
Patients who developed AF were significantly older, more likely to be female, and were more likely to have a history of hypertension, stroke, or heart failure than patients who did not develop AF. Patients with new onset AF were less likely to have a history of AMI and were more likely to have their hospital stay complicated by heart failure, cardiogenic shock, and stroke compared to patients who did not develop AF (Table 1). Patients who developed AF had lower admission blood pressures and a higher heart rate. Patients who developed AF were significantly less likely to undergo cardiac catheterization or a percutaneous coronary intervention. Patients with AF were more likely to be treated with angiotensin converting enzyme inhibitors, anticoagulants, calcium channel blockers, digoxin, and diuretics but were less likely to be treated with aspirin, beta blockers, or thrombolytic therapy during hospitalization than patients who did not develop AF (Table 1).
Table 1.
Characteristics of patients with acute myocardial infarction according to presence of atrial fibrillation: Worcester Heart Attack Study
| Atrial Fibrillaion | |||
|---|---|---|---|
| Characteristic | Present (n=999) | Absent (n=6,514) | p-value |
| Age (mean, SD, years) | 75.8 (11.3) | 68.2 (14.0) | <.001 |
| Age (years) | |||
| <65 | 16.5% | 38.0% | <0.001 |
| ≥ 85 | 23.2% | 12.2% | |
| Male | 51.1% | 57.9% | <0.001 |
| White race | 93.1% | 90.5% | <0.01 |
| Length of hospital stay (mean,days) | 8.6 | 6.4 | <0.001 |
| Medical history | |||
| Angina pectoris | 20.3% | 23.0% | 0.06 |
| Diabetes mellitus | 29.6% | 29.6% | 0.96 |
| Hypertension | 65.5% | 61.1% | 0.008 |
| Stroke | 12.6% | 9.4% | 0.005 |
| Heart failure | 24.0% | 17.6% | <0.001 |
| AMI characteristics | |||
| Initial | 69.2% | 65.6% | 0.05 |
| Q Wave | 35.4% | 33.7% | 0.28 |
| Anterior | 24.5% | 24.7% | 0.89 |
| ST segment elevation AMI | 24.0% | 23.9% | 0.95 |
| Admission findings (means, SD) | |||
| Systolic blood pressure (mmHg) | 134.8 (35.6) | 144.0 (33.6) | <0.001 |
| Diastolic blood pressure (mmHg) | 74.7 (22.0) | 78.3 (20.7) | <0.001 |
| Initial heart rate (beats/minute) | 94.2 (30.1) | 85.6 (22.3) | <0.001 |
| Hospital complications | |||
| Heart failure | 55.6% | 32.9% | <0.001 |
| Cardiogenic shock | 14.0% | 4.9% | <0.001 |
| Stroke | 3.2% | 1.2% | <0.001 |
| Procedures | |||
| Cardiac catheterization | 33.6% | 42.6% | <0.001 |
| Percutaneous coronary intervention | 21.9% | 24.9% | <0.05 |
| Medications prescribed during hospitalization | |||
| Angiotensin converting enzyme inhibitors | 51.4% | 44.4% | <0.001 |
| Anticoagulants | 76.4% | 73.3% | <0.05 |
| Aspirin | 83.0% | 89.2% | <0.001 |
| Beta blockers | 70.6% | 80.1% | <0.001 |
| Calcium channel blockers | 39.9% | 29.5% | <0.001 |
| Digoxin | 53.2% | 14.5% | <0.001 |
| Diuretics | 71.2% | 48.7% | <0.001 |
| Thrombolytics | 11.9% | 18.6% | <0.001 |
Note. SD = standard deviation
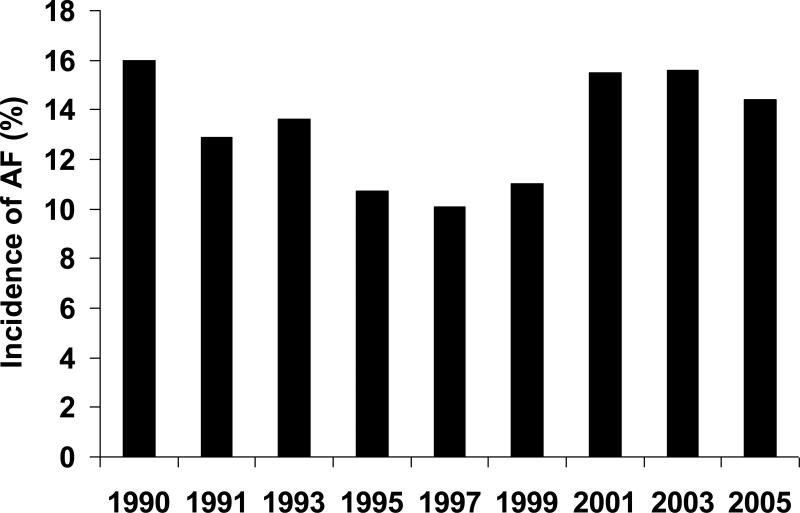
The proportion of patients who developed AF declined between 1990 (16.0%) and 1999 (11.3%) (Figure 1). Following this steady decline, the proportion of patients who developed a first episode of AF increased to 15.5% in 2001 and remained at 14.4% in our most recent study year of 2005. After controlling for several demographic factors, comorbid conditions, AMI characteristics, and in-hospital complications, the odds of developing AF were significantly lower in 1995 and 1997, but were not significantly different from our index study year of 1990, during the other years under study (Table 2).
Figure 1.
Trends in the incidence rates of atrial fibrillation in patients hospitalized with acute myocardial infarction: The Worcester Heart Attack Study
Table 2.
Crude and multivariable adjusted odds of developing atrial fibrillation during hospitalization for acute myocardial infarction (AMI): Worcester Heart Attack Study
| Period | N | Crude OR | 95% CI | Adjusted OR† | 95% CI |
|---|---|---|---|---|---|
| 1990° | 701 | 1.0 | - | 1.0 | --,-- |
| 1991 | 776 | 0.78 | 0.58,1.04 | 0.76 | 0.56,1.04 |
| 1993 | 873 | 0.83 | 0.62,1.10 | 0.91 | 0.67,1.23 |
| 1995 | 876 | 0.63 | 0.47,0.85 | 0.69 | 0.50,0.95 |
| 1997 | 952 | 0.59 | 0.44,0.79 | 0.67 | 0.48,0.92 |
| 1999 | 908 | 0.65 | 0.48,0.87 | 0.75 | 0.55,1.03 |
| 2001 | 1065 | 0.96 | 0.74,1.26 | 1.08 | 0.80,1.45 |
| 2003 | 987 | 0.97 | 0.74,1.27 | 1.17 | 0.87,1.58 |
| 2005 | 781 | 0.88 | 0.66,1.18 | 1.07 | 0.78,1.48 |
referent study year
Adjusted for age, sex, history of angina, hypertension, diabetes, stroke, heart failure, AMI associated characteristics, development of heart failure, cardiogenic shock, and stroke during hospitalization, and length of hospital stay.
CI – confidence intervals
OR – odds ratio
A total of one hundred and thirteen patients (1.5%) developed an acute stroke during hospitalization for AMI. The crude odds of experiencing a stroke were 2.63 (95%CI 1.74, 3.98) times greater in patients who had AF diagnosed during their acute hospitalization. After adjusting for a number of demographic factors, comorbid conditions, and AMI associated characteristics, the association between AF and occurrence of stroke remained significant (adjusted OR = 2.25; 95% CI 1.36, 3.71). The in-hospital death rate was 43.8% for patients with AF who developed a stroke compared to 22.1% in patients with AF but who did not develop a stroke during their acute hospitalization.
Patients with new onset AF who experienced a stroke were significantly older (with stroke: 24% ≥85 years, without stroke: 14% ≥85 years) and more likely to have presented with a non-Q Wave AMI (92% vs 70%) in comparison to those who did not develop a stroke (p <0.05). There were no significant differences in the management of patients who did, as compared to those who did not, develop a stroke. The odds of developing a stroke increased over time (1.4% in 1990, 3.3% in the late 1990's, and 3.2% during 2003 and 2005).
Patients who developed AF were more than twice as likely to die during hospitalization for AMI compared to those who did not develop AF (22.8% vs 10.1%, p<.001). After adjusting for previously described demographic and clinical factors, patients with AF remained at significantly increased risk for dying during hospitalization for AMI compared to those who did not develop this arrhythmia (adjusted OR = 1.79; 95% CI 1.46,2.19).
Patients with AMI complicated by AF experienced significantly higher inhospital death rates compared to patients who did not develop AF during each of the years under study (Figure 2). We observed a steady decline over time in mortality among patients hospitalized for AMI without AF (12.8% in 1990, 5.9% in 2005). A slight decrease in hospital death rates was observed in patients who developed AF complicating AMI over time (24.6% in 1990, 21.3% in 2005). After controlling for potential confounders and mediating factors, the risk of dying during hospitalization for AMI did not change significantly in those who developed AF over the 15 year period under study (data not shown).
Figure 2.
Hospital case fatality rates (CFR) according to presence of atrial fibrillation (AF) in patients hospitalized with acute myocardial infarction: Worcester Heart Attack Study
Compared to patients with AMI who did not develop AF, those who developed AF during hospitalization for AMI had a significantly higher 30-day death rate after hospital admission (26.5% vs. 12.9%, p<.001). After controlling for previously described potentially confounding factors, patients with AF remained at significantly increased risk for dying at 30-days after hospital admission compared to patients who did not develop AF (adjusted OR = 1.76; 95% CI 1.46, 2.13). The multivariable adjusted odds of dying at 30 days after hospital admission did not change significantly between 1990 and 2005.
Incident AF during hospitalization for AMI was also associated with significantly higher crude 1-year post-discharge mortality rates (28.2% vs. 16.1%, p<.001). The odds of dying during the first year after hospital discharge for AMI was significantly greater in patients who developed AF as a complication of AMI after adjustment for demographic factors, comorbid conditions, AMI characteristics, length of hospital stay, and hospital complications (adjusted OR = 1.27; 95% CI 1.05,1.55). There were no significant changes over time in the multivariable adjusted odds of dying during the first year after hospital discharge for AF during the years under study (Table 3).
Table 3.
Crude and multivariable adjusted odds of 1-year mortality among those who developed atrial fibrillation during hospitalization for acute myocardial infarction (AMI): Worcester Heart Attack Study
| Period | N | Crude OR | 95% CI | Adjusted OR† | 95% CI |
|---|---|---|---|---|---|
| 1990° | 120 | 1.0 | - | 1.0 | - |
| 1991 | 104 | 1.17 | 0.57,2.43 | 1.23 | 0.56,2.70 |
| 1993 | 126 | 1.32 | 0.77,3.00 | 1.47 | 0.70,3.07 |
| 1995 | 112 | 1.23 | 0.59,2.59 | 1.42 | 0.63,3.22 |
| 1997 | 108 | 1.22 | 0.59,2.54 | 1.33 | 0.59,3.00 |
| 1999 | 106 | 1.48 | 0.74,2.98 | 1.73 | 0.80,3.76 |
| 2001 | 184 | 1.84 | 0.98,3.45 | 1.89 | 0.92,3.87 |
| 2003 | 161 | 0.94 | 0.49,1.81 | 0.84 | 0.40,1.77 |
| 2005 | 121 | 0.85 | 0.41,1.75 | 0.77 | 0.34,1.76 |
referent study year
Adjusted for age, sex, history of angina, hypertension, diabetes, stroke, heart failure, AMI associated characteristics, development of heart failure, cardiogenic shock, and stroke during hospitalization, and length of hospital stay.
CI – confidence intervals
OR – odds ratio
More extended long-term survival after hospital discharge was lower in patients with AF compared to those without AF (Figure 3). A proportional hazards regression analysis was carried out to control for previously described prognostic factors in examining the association of the hospital development of AF with long-term survival. Post-discharge survival was significantly poorer in patients who did, as compared to those who did not, develop AF during hospitalization for AMI (adjusted hazards ratio = 1.26; 95% CI 1.15,1.38).
Figure 3.
Long-term survival according to presence of atrial fibrillation (AF) during hospitalization for acute myocardial infarction: Worcester Heart Attack Study
Discussion
The results of this community-wide study suggest that the incidence rates of AF declined during the 1990s but increased thereafter such that approximately 1 in every 7 patients hospitalized with AMI between 2003 and 2005 developed new onset AF. The development of AF during hospitalization for AMI was associated with an increase in both in-hospital and post-discharge mortality as well as with an increased risk of stroke during hospitalization.
The overall incidence rate of AF (13%) observed in the present investigation is within the range of published studies (5-23%), but is slightly higher than has been observed in the most recently published studies (5-10%).7-11. These differences may be due to the varying definitions of AF, the size and characteristics of the patient samples studied, or differences in the use of therapies that may reduce the risk of AF. The systematic exclusion of patients at high risk for AF (i.e., those with prior stroke) in clinical trials may also have contributed to the lower incidence of AF noted in some studies, including the Global Utilization of Streptokinase and Tissue plasminogen activator for Occluded coronary arteries (GUSTO) I and GUSTO-III studies.7,8
Limited data are available describing long-term trends in the incidence rates of AF in patients hospitalized with AMI. The incidence rate of paroxysmal AF in patients with AMI declined from 10.2% to 7.6% during the 1990s in the SPRINT study.10 This decrease was paralleled by similar declines in the incidence rates of AF observed in our study population during the same period.3 Our more recent data suggest that the incidence of AF has increased in the greater Worcester population since 2000. This change may be explained by an increasingly older hospitalized population with a greater prevalence of comorbidities.
Similar to previously published studies7,9,10-13, we found a greater than 2-fold increase in the risk of acute stroke in patients with AMI who developed AF. While the frequency of AF was highest during the most recent study years, the odds of developing an acute stroke during hospitalization for AMI in patients with AF relative to those without AF was elevated throughout the 15-year period under study. Older age and the development of a non-Q Wave AMI were associated with an increased risk for stroke in patients who developed AF. The association between type of AMI, stroke, and occurrence of acute AF warrants further examination in future studies, particularly since an increasing frequency of older patients are being hospitalized with a non-Q wave MI.14
We found that patients with new onset AF were approximately twice as likely to die during hospitalization for AMI compared to patients who did not develop AF. Our data are consistent with those of the Global Registry of Acute Coronary Events study where patients with new onset AF had a >3-fold increased risk for dying during hospitalization for an acute coronary syndrome compared to those who did not develop AF.9 While hospital death rates decreased over the 15-year period under study for patients with AMI who did not develop AF, hospital mortality rates remained considerably higher in patients who developed AF. This could be due to the fact that patients who developed AF during more recent years were older and had more comorbidities.
Thirty-day and 1 year mortality rates were also higher among greater Worcester residents who developed AF during hospitalization for AMI. The multivariable-adjusted odds of dying at 30 days and at 1 year observed among patients with incident AF are of a similar magnitude to those observed in previously published studies. 7,10,15
Our data build on prior work by demonstrating that the development of AF during hospitalization for AMI remains common. Recent increases in the incidence rates of AF complicating AMI contrast with prior trends of decreases in the rates of AF seen in our cohort and with the findings reported from other studies in this area. Prior trends showing a reduction in AF complicating AMI have been attributed to the increased use of effective cardiac medications and early coronary revascularization. This trend may now be countered by the fact that an increasing number of older patients with a greater burden of cardiovascular disease are being hospitalized for AMI.
The strengths of the present study include our population-based design that included all patients hospitalized with AMI in a well-characterized urban New England community. We were able to control for a number of potentially confounding factors in examining changing trends in the magnitude and death rates associated with AF in patients hospitalized with AMI. Our findings are limited, however, by a lack of information on the timing of AF, timing and use of selected therapies in relation to the development of, or prognosis after, AF, and our inability to examine whether time of occurrence of AF is associated with the development of important complications of AMI, including stroke. There were too few cases of acute stroke to determine whether AF is associated with ischemic or hemorrhagic strokes. Our findings were carried out in a single metropolitan area and may not be generalizable to other communities.
Acknowledgments
Funding support provided by the National Institutes of Health (RO1 HL35434).
References
- 1.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–9. [PubMed] [Google Scholar]
- 2.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Yarzebski J, Lessard D, Wu J, Gore JM. Recent trends in the incidence rates of and death rates from atrial fibrillation complicating initial acute myocardial infarction: A community-wide perspective. Am Heart J. 2002;143:519–527. doi: 10.1067/mhj.2002.120410. [DOI] [PubMed] [Google Scholar]
- 4.Saczynski JS, Spencer FA, Gore JM, Gurwitz JH, Yarzebski J, Lessard D, Goldberg RJ. Twenty-year trends in the incidence of stroke complicating acute myocardial infarction: Worcester Heart Attack Study. Arch Intern Med. 2008;168:2104–2110. doi: 10.1001/archinte.168.19.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spencer FA, Meyer TE, Goldberg RJ, Yarzebski J, Hatton M, Lessard D, Gore JM. Twenty year trends (1975-1995) in the incidence, in-hospital and long-term death rates associated with heart failure complicating acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;34:1378–1387. doi: 10.1016/s0735-1097(99)00390-3. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM. Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med. 1999;340:1162–1168. doi: 10.1056/NEJM199904153401504. [DOI] [PubMed] [Google Scholar]
- 7.Crenshaw BS, Ward SR, Granger CB, Stebbins AL, Topol EJ, Califf RM. Atrial fibrillation in the setting of acute myocardial infarction: The GUSTO-I Experience. J Am Coll Cardiol. 1997;30:406–413. doi: 10.1016/s0735-1097(97)00194-0. [DOI] [PubMed] [Google Scholar]
- 8.Wong CK, White HD, Wilcox RG, Criger DA, Califf RM, Topol EJ, Ohman EM. Significance of atrial fibrillation during acute myocardial infarction, and its current management: insights from the GUSTO-3 trial. Card Electrophysiol Rev. 2003;7:201–207. doi: 10.1023/B:CEPR.0000012382.81986.47. [DOI] [PubMed] [Google Scholar]
- 9.Mehta RH, Dabbous OH, Granger CB, Kuznetsova P, Kline-Rogers EM, Anderson FA, Jr, Fox KA, Gore JM, Goldberg RJ, Eagle KA. GRACE Investigators. Comparison of outcomes of patients with acute coronary syndromes with and without atrial fibrillation. Am J Cardiol. 2003;92:1031–1036. doi: 10.1016/j.amjcard.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Eldar M, Canetti M, Rotstein Z, Boyko V, Gottlieb S, Kaplinsky E, Behar S. Significance of paroxysmal atrial fibrillation complicating acute myocardial infarction in the thrombolytic era. Circulation. 1998;97:965–970. doi: 10.1161/01.cir.97.10.965. [DOI] [PubMed] [Google Scholar]
- 11.Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2008:ehn579. doi: 10.1093/eurheartj/ehn579. [DOI] [PubMed] [Google Scholar]
- 12.Lopes RD, Pieper KS, Horton JR, Al-Khatib SM, Newby LK, Mehta RH, Van de Werf F, Armstrong PW, Mahaffey KW, Harrington RA, Ohman EM, White HD, Wallentin L, Granger CB. Short- and long-term outcomes following atrial fibrillation in patients with acute coronary syndromes with or without ST-segment elevation. Heart. 2008;94:867–873. doi: 10.1136/hrt.2007.134486. [DOI] [PubMed] [Google Scholar]
- 13.Ezekowitz MD, Levine JA. Preventing stroke in patients with atrial fibrillation. JAMA. 1999;281:1830–1835. doi: 10.1001/jama.281.19.1830. [DOI] [PubMed] [Google Scholar]
- 14.Furman MI, Dauerman HL, Goldberg RJ, Yarzbeski J, Lessard D, Gore JM. Twenty-two year (1975 to 1997) trends in the incidence, in-hospital and long-term case fatality rates from initial Q-wave and non-Q-wave myocardial infarction: a multi-hospital, community-wide perspective. J Am Coll Cardiol. 2001;37:1571–1580. doi: 10.1016/s0735-1097(01)01203-7. [DOI] [PubMed] [Google Scholar]
- 15.Wong C-K, White HD, Wilcox RG, Criger DA, Califf RM, Topol EJ, Ohman EM. New atrial fibrillation after acute myocardial infarction independently predicts death: The GUSTO-III experience. Am Heart J. 2000;140:878–885. doi: 10.1067/mhj.2000.111108. [DOI] [PubMed] [Google Scholar]