Abstract
Background
Postoperative readmissions increase costs and affect patient quality of life. Ulcerative colitis (UC) patients are at a high risk for hospital readmission following restorative proctocolectomy (RP).
Objective
To characterize UC patients undergoing RP and identify causes and risk factors for readmission.
Design
A retrospective review of a prospectively maintained institutional database was performed. Postoperative readmission rates and reasons for readmission were examined following RP. Univariate and multivariate analyses were performed to evaluate for risk factors associated with readmission.
Results
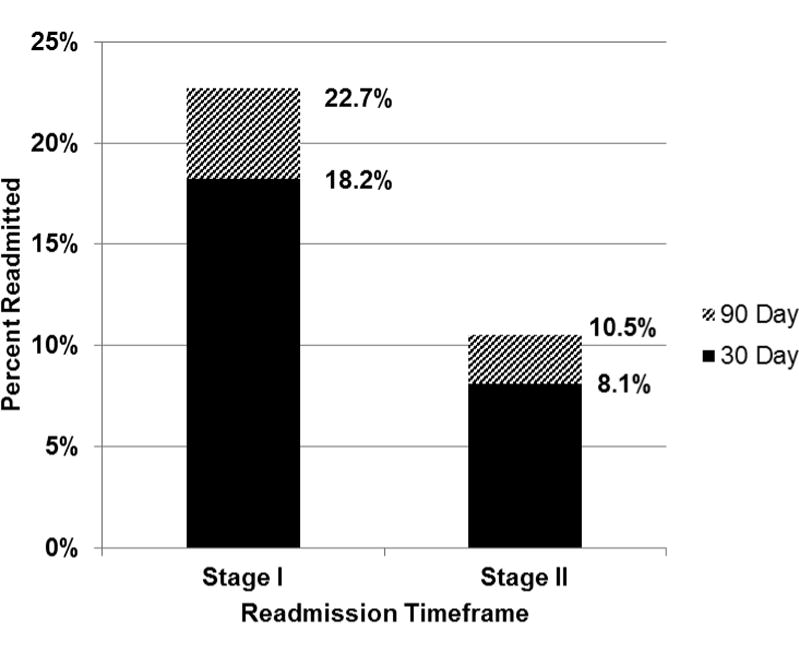
Of 533 patients who met our inclusion criteria, 18.2% (n=97) were readmitted within 30 days while 22.7% (n=121) were readmitted within 90 days of stage I of RP. Younger patient age (OR 1.825, 95% CI 1.139-2.957), laparoscopic approach (OR 1.943, 95 % CI 1.217-3.104) and increased length of initial stay (OR 1.155, 95% CI 1.090-1.225) were all associated with 30-day readmission. The most common reason for readmission was dehydration/ileus/partial bowel obstruction, with 10% of patients readmitted for this reason within 30 days.
Conclusions
Patients undergoing restorative proctocolectomy are at high risk for readmission, particularly following the first stage of the operation. Novel treatment pathways to prevent ileus and dehydration as an outpatient may decrease the rates of readmission following RP.
Keywords: Post-operative readmission, restorative proctocolectomy
Introduction
In addition to negatively impacting patient quality of life, hospital readmissions dramatically increase cost. An estimated $17 billion is spent annually on unplanned readmissions for Medicare patients alone [1]. At the same time, 30 day readmission rates are now being utilized as indicators of quality of care [2-4], and are directly linked to Medicare reimbursement [5]. Despite this, predicting which patients will be readmitted and preventing readmissions continues to be a challenge [6, 7].
A number of studies have examined readmission in general surgery patients. Some studies have found male sex and older age to be associated with increased risk of readmission, while others have implicated obesity, hospital length of stay, surgical site infections and steroid use as the most important predictors of readmission [4, 8-12]. In contrast, other studies have concluded that readmission cannot be predicted at all [13, 14].
While much has been written about hospital readmission in general, there is a paucity of data on readmission rates for patients with ulcerative colitis (UC) undergoing restorative proctocolectomy (RP). The aim of this study was to characterize patients with UC who underwent RP at our institution and evaluate and further define the following: 1) the timeframe of readmission, 2) the reason for readmission and 3) risk factors associated with readmissions. Due to the complexity of the procedure, we hypothesized that patients would be readmitted primarily following the first stage of RP and that the majority of readmissions would be due to gastrointestinal motility complications. Based on previous data from our institution [15], we also hypothesized that younger patients would be at greater risk for readmission.
Methods
Data Source
We performed a retrospective review of a prospectively-maintained institutional colorectal database. The database contains patients who underwent surgical treatment for UC at a single academic institution from 1/1998 to 5/2013. All investigations were approved by the University of Wisconsin-Madison Health Sciences Institutional Review Board and the Human Subjects Committee.
Patient Population
UC is an idiopathic inflammatory bowel disease for which definitive treatment often requires RP. RP at our institution is routinely performed as a 2-stage operation. During the first stage patients undergo proctocolectomy with double stapled ileal pouch creation and a diverting loop ileostomy, while takedown of the loop ileostomy is performed during the second stage.
Patients were included in the study if they underwent RP at our institution during the study time period, were at least 18 years old at the time of the procedure, and had sufficient follow-up to establish 30 and 90 day readmission statuses. Patients were not included if they had a diagnosis other than UC, had incomplete charts or were lost to follow-up, underwent colectomy without ileal pouch creation, underwent reoperation for an existing pouch, or had another procedure not involving initial pouch creation. The creation of the ileal pouch was considered stage I for all analyzed patients. We identified 14 patients who underwent a 3 stage procedure, as well as 2 patients that underwent a single stage procedure in our database. We included patients who underwent single, two stage and three stage procedures together in our statistical analysis.
Perioperative Variables
Explanatory variables included age, sex, American Society of Anesthesiology (ASA) classification, diabetes, hypertension, laparoscopic approach, BMI, initial length of stay (LOS), operative time, and steroid use at the time of discharge. Patient age was stratified by quartiles in the following groups: <28.4 years, 28.4-39 years, 39-50 years, and 50+ years. BMI, LOS, and operative time were evaluated as continuous variables.
Outcomes
The primary outcome was postoperative readmission at 30 and 90 days. Incidents of at least one unplanned readmission were examined following both stage I and stage II of RP. In addition, the reason for readmission was examined. The following categories were included as possible reasons for readmissions: dehydration/ileus/partial small bowel obstruction (pSBO), complete small bowel obstruction (SBO, diagnosed intra-operatively or via imaging), infection (wound or organ space infection), anastomotic complication (bleeding, fistula or anastomotic leak), non-GI complication (cardiovascular, thrombotic, renal and oncologic) and other GI complication (pouchitis, cuffitis). All readmission diagnoses were determined by the admitting surgeon. Patients were included in the dehydration/ileus/partial/pSBO category if they were admitted for ileus/pSBO or for dehydration secondary to ileus/pSBO, high/low output ileostomy, nausea/vomiting, constipation, adrenal insufficiency, or combination of these diagnoses. The diagnosis of anastomotic leak was determined by the admitting provider in conjunction with radiologic evidence or return to the operating room.
Statistical Analysis
To evaluate for risk factors associated with readmission, Chi-squared analysis was performed for categorical variables while continuous variables were evaluated with independent student's t tests. A correlation matrix was used to assure that no collinearity existed amongst explanatory variables. Variables with p value <0.10 on univariate analysis were included in the multivariate model. Variables with less than 10 readmitted patients were excluded from multivariate analysis. Logistic regression analysis was used to determine independent predictors of 30 day readmission, as well as reason for readmission following stage I of RP. Significance for multivariate analyses was defined as p <0.05. All statistical analyses were performed using SPSS Gradpack v. 20.
Results
We identified 838 patients with UC who underwent RP between 1/1998 and 5/2013. After exclusion criteria were applied, our study population consisted of 533 patients (Figure 1). Figure 2 demonstrates 30 and 90 day readmission rates following RP. The majority of readmissions occurred after stage I of RP, and occurred within 30 days of surgery. Therefore, we focused the remainder of our study on this group of patients.
Figure 1. Summary of Study Population.
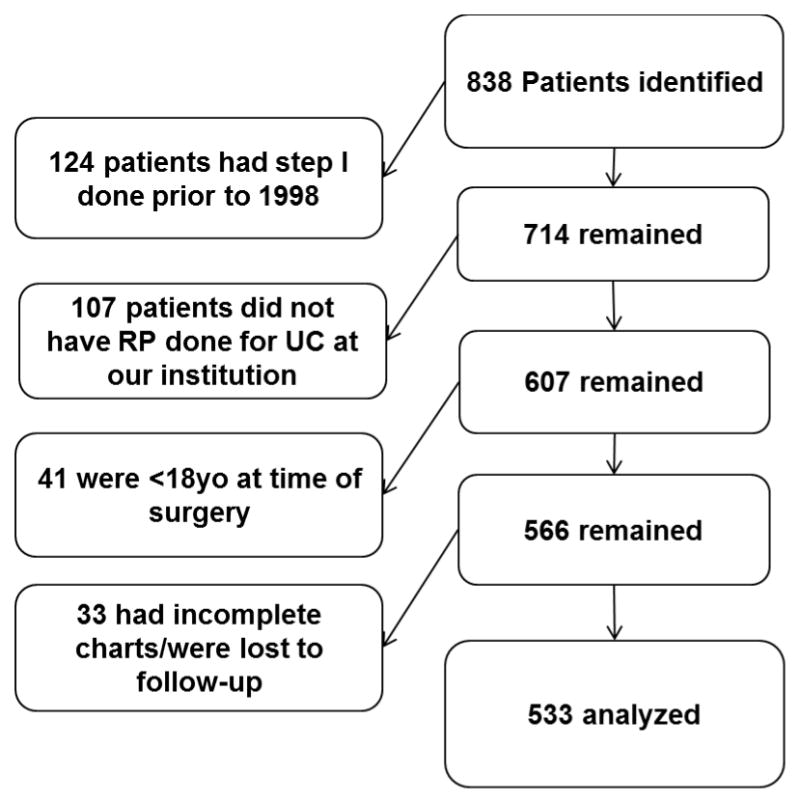
Figure 2. Readmission rates within 30 and 90 days of Stage I and Stage II RP.
Characteristics of patients who were or were not readmitted within 30 days of stage I are demonstrated in Table 1. Patient demographics significantly associated with 30 day readmission included female sex and younger age. Additionally, we found that laparoscopic operative approach and longer LOS were also associated with readmission. Patients who underwent laparoscopic surgery (n = 210) had a mean LOS of 6.7 ± 4.1 days, while patients who underwent open surgery (n = 323) had a mean LOS of 7.4 ± 3.6 days (p = 0.042).
Table 1.
Patient characteristics and risk factors for readmission within 30 days of stage I.
| Characteristic | Readmitted within 30 days | Not readmitted within 30 days | P value | |
|---|---|---|---|---|
| Sex | Male | 46 (15%) | 257 (85%) | 0.025 |
| Female | 51 (22%) | 179 (78%) | ||
|
| ||||
| Age (quartile) | 1st | 34 (26%) | 99 (74%) | 0.017 |
| 2nd | 25 (19%) | 108 (81%) | ||
| 3rd | 14 (11%) | 119 (89%) | ||
| 4th | 24 (18%) | 110 (82%) | ||
|
| ||||
| ASA | 1 | 3 (10%) | 26 (90%) | 0.059 |
| 2 | 85 (19%) | 358 (81%) | ||
| 3 | 4 (9%) | 40 (91%) | ||
| Unknown | 16 (89%) | 2 (11%) | ||
|
| ||||
| Diabetes | Yes | 5 (17%) | 24 (83%) | 0.63 |
| No | 92 (18%) | 408 (82%) | ||
| Unknown | 0 | 4 (100%) | ||
|
| ||||
| Hypertension | Yes | 13 (20%) | 53 (80%) | 0.938 |
| No | 83 (18%) | 379 (82%) | ||
| Unknown | 1 (20%) | 4 (80%) | ||
|
| ||||
| Operative Approach | Laparoscopic | 50 (24%) | 160 (76%) | 0.005 |
| Open | 47 (15%) | 276 (85%) | ||
|
| ||||
| Discharge Steroids | Yes | 65 (27%) | 172 (73%) | 0.139 |
| No | 263 (89%) | 33 (11%) | ||
|
| ||||
| BMI | Median 25.3 | Mean 25.4 | Mean 26.2 | 0.184 |
|
| ||||
| Length of Stay(days) | Median 6 days | Mean 9.1 days | Mean 6.7 days | <0.001 |
|
| ||||
| OR Time(minutes) | Median 380 mins | Mean 401 mins | Mean 391 mins | 0.345 |
The multivariable analysis evaluating risk factors for stage I readmission is demonstrated in Table 2. Younger patient age, longer LOS, and laparoscopic approach were all found to independently predict readmission in patients admitted within 30 days of stage I. Notably, there was no correlation between patient age and initial length of stay (r=0.028, p=0.519).
Table 2.
Multivariable analysis of risk factors for stage I readmission within 30 days.
| Risk Factor | Adjusted OR | 95% CI | P-value |
|---|---|---|---|
| Sex (f) | 1.461 | 0.982-2.412 | 0.131 |
| Age <39 yrs. | 1.825 | 1.139-2.957 | 0.013 |
| Length of stay | 1.155 | 1.090-1.225 | <0.001 |
| Laparoscopic approach | 1.943 | 1.217-3.104 | 0.005 |
A similar analysis was performed to identify predictors of readmission patients following stage II RP. The only variable found to be significantly associated with readmission after stage II RP was ASA classification with a 8% readmission rate in patients with ASA class I, 7.6% in ASA class 2, and 18.6% in ASA class 3 (p=0.043). No variables were found to be independent predictors of readmission following stage II on multivariable analysis.
Reasons for 30 day stage I and stage II readmission are listed in Table 3. The most common reason for stage I readmission (10%) was dehydration/ileus/pSBO. Two thirds of patients with these diagnoses were discharged within 72 hours. The most common reason for stage II readmission was likewise dehydration/ileus/pSBO (4%), with approximately one third of these patients being discharged within 72 hours.
Table 3.
Reasons for 30 day readmission following stage I and II of RP.
| Stage I | Stage II | |
|---|---|---|
|
| ||
| Readmission Diagnosis | N = 97* n (%) | N=43* n (%) |
| Dehydration/Ileus/pSBO | 53 (55) | 22 (51) |
| <72 Hours† | 34 (35) | 8 (18) |
| >72 Hours† | 19 (20) | 14 (33) |
| Complete SBO | 14 (14) | 2 (5) |
| Non-GI Issue | 12 (12) | 7 (16) |
| Infection | 11 (11) | 6 (14) |
| Other GI Issue | 6 (6) | 4 (9) |
| Anastomotic Issue | 5 (5) | 3 (7) |
A small number of patients were readmitted more than once, there were 101 readmissions in 97 patients following stage I RP, and 44 readmission in 43 patients following stage II RP.
Length of stay upon readmission
Note -13 pts in stage II group were lost to follow up
As demonstrated in Table 4, we then performed a multivariate analysis to evaluate risk factors associated with stage I readmission for gastrointestinal motility issues, defined as ileus, partial or complete bowel obstruction. We found that laparoscopic approach, age <39 and longer LOS were the strongest predictors of 30 day readmission in this group.
Table 4.
Multivariable analysis of risk factors associated with 30 day readmission for GI motility issues following stage I of RP.
| Risk Factor | Adjusted OR | 95% CI | P-value |
|---|---|---|---|
| Sex (f) | 1.303 | 0.759-2.236 | 0.338 |
| Age (<39) | 1.696 | 0.959-3.001 | 0.07 |
| Length of Stay | 1.104 | 1.041-1171 | 0.001 |
| Laparoscopic approach | 1.833 | 1.061-3.165 | 0.03 |
| BMI | 0.924 | 0.871-0.980 | 0.009 |
| Steroids | 1.452 | 0.807-2.611 | 0.214 |
Discussion
The aim of this study was to evaluate hospital readmission rates in patients with UC who underwent RP, identify risk factors for readmission, and further characterize reasons for readmission in UC patients. We found that the majority of UC patients readmitted following RP were readmitted within 30 days following the first stage of the procedure. Independent predictors of readmission following stage II RP were younger age, longer LOS, and laparoscopic approach. We evaluated the causes of readmission, and found that gastrointestinal complications comprised nearly all readmissions. The strongest predictors of readmission for gastrointestinal complications were again younger age and laparoscopic approach.
Thirty day readmission following RP for UC was common (18.2%). As we hypothesized, bowel motility issues (ileus or bowel obstructions) or dehydration secondary to these issues accounted for the majority of readmissions, a finding consistent other studies. Previously, Ozturk et al. found that in patients undergoing ileal pouch–anal anastomosis readmissions were primarily due to ileus/obstruction or serum electrolyte abnormalities (54% of all readmissions), although their overall readmission rate was slightly less than our institution at 12% [16]. Similarly, Datta et al. reported that small bowel obstruction alone accounted for 33% of readmissions following RP, with dehydration accounting for an additional 10% and a total readmission rate of 30% [17]. Interestingly, complete bowel obstructions were uncommon in our group, with most patients being readmitted for dehydration due to ileus or a partial obstruction and the majority of patients were discharged home within 72 hours. To our knowledge the timeframe to resolution of symptoms from bowel obstruction following RP has not previously been examined in UC patients.
Complications related to the anastomosis were the least common reason for readmission following both stage I and stage II RP. This may be due to the fact that almost all procedures were performed as a two stage operation. Conversely, this could indicate that anastomotic complications are uncommon in this patient population and RP may safely be performed as a single stage operation. There is recent controversy in the literature on this subject. Some authors have found an increased risk of life threatening complications and reoperation in patients who undergo single stage RP [18]. Patients on steroids have been found to be at particularly high risk for post-operative complications [19]. Others have found decreased complication rates following single stage RP along with the benefit of shorter length of hospital stay [20-23]. Published series on single stage RP have consisted of small numbers of patients with a focus on complications rather than post-operative readmissions, further studies are needed to determine if single stage RP is a safe alternative to a two stage procedure and to delineate reasons for readmission in patients following single stage RP.
With respect to risk factors, we found that younger age, increased LOS and a laparoscopic approach were associated with 30 day readmission following stage I RP. LOS and a laparoscopic approach were also risk factors for readmissions specifically due to gastrointestinal complications. To the authors, the finding that laparoscopic approach increased the risk of readmission was the most surprising. Laparoscopic RP has been shown not only to be as safe and effective as a traditional open approach, but also offers significant benefit, such as reduced length of stay and shorter recovery time [24]. At the same time, there have been reports of laparoscopic approach correlating with increased readmission rates in patients with a diverting ileostomy [25], as well as in patients undergoing RP with IPAA [16]. In fact, Ozturk et al. found laparoscopic approach to be predictive of readmission with an adjusted odds ratio nearly identical to our study [16]. To our knowledge, this is the only other study to show this association between laparoscopic approach and readmission following RP.
The tendency of readmitted patients, especially those readmitted with GI motility issues, to have relatively short hospital stays (<72 hours) raises the question of whether these readmissions may be preventable. Although ileus or a partial SBO may be the admitting diagnosis, dehydration appeared to be the most common presentation to emergency department and often resolved quickly with conservative treatment. As dehydration is often implicated as a primary cause for readmission in patients with an ileostomy [25], as well as UC patients undergoing RP with IPPA,[16] we speculate that early detection and treatment of dehydration in the outpatient setting, could prevent readmissions in UC patients. To this extent we would suggest that protocolized perioperative teaching, such as the “Ileostomy pathway” which has been shown to reduce readmission rates in patients with new ostomies, would also likely be effective in our patient population.[26]
This study was limited by the use of patient data from a single tertiary referral center. While patients who underwent RP at our institution were not likely to be readmitted elsewhere without follow up due to the complexity of the initial procedure, a fraction of patients were lost to follow-up or had incomplete charts. The retrospective nature of this study made it difficult to assess the reason for readmission in patients with gastrointestinal motility issues. Admission notes frequently identified multiple reasons for readmission including dehydration, gastrointestinal motility issues, and adrenal insufficiency. A prospective study with strict diagnosis definitions may be better able to separate these diagnoses, however in reality patients are likely suffering from multiple issues related to gastrointestinal motility complications and therefore grouping these diagnoses is clinically appropriate. While preoperative steroid use was not found to be associated with readmission in this study, the database did not contain information on the use of biologics in these patients, which is a limitation to this study. In addition, patients under the age of 18 were excluded from this study. We estimate that pediatric patients comprise approximately 7% of the UC population at our institution. It would be difficult to extrapolate these results to pediatric patients.
Conclusion
In conclusion, patients undergoing RP are at high risk for readmission, particularly for GI related issues following the first stage of the operation. Novel treatment pathways to prevent ileus and dehydration as an outpatient may decrease the rates of readmission following RP. Given the high rate of readmission, as well as potentially preventable reasons for readmission, we believe this patient population would an ideal group for targeted perioperative teaching and clinics aimed at identifying made post-operative complications early in an effort to decrease readmission rates. While fast track or enhanced recovery protocols have been developed in other colorectal patient populations, patients undergoing RP are not typically included in these programs. This patient population would likely benefit greatly from the standardized preoperative expectation setting, teaching regarding postoperative recovery, and standardized care that have these programs so successful in other patient populations.
Acknowledgments
This study was possible due to the generous support of the UW School of Medicine and Public Health Shapiro program as well as the NIH T32 training grant (CA090217). We would like to thank Chee Paul Lin for his valuable statistical expertise and advice.
Support for this study was generously provided by the University of Wisconsin School of Medicine and Public Health Shapiro Program and by the NIH T32 training grant (CA090217).
This work was presented at the 2014 American Society of Colon and Rectum Surgeons (Hollywood, Florida 5/17/2014-5/21/2014).
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Francois P, Bertrand D, Beden C, et al. Early readmission as an indicator of hospital quality of care. Rev Epidemiol Sante Publique. 2001;49:183–192. [PubMed] [Google Scholar]
- 3.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160:1074–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 4.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54:1475–1479. doi: 10.1097/DCR.0b013e31822ff8f0. [DOI] [PubMed] [Google Scholar]
- 5.Jencks SF. Rehospitalizations among patients in the Medicare fee-forservice program. doi: 10.1056/NEJMsa0803563. In. [DOI] [PubMed] [Google Scholar]
- 6.Vest JR, Gamm LD, Oxford BA, et al. Determinants of preventable readmissions in the United States: a systematic review. Implement Sci. 2010;5:88. doi: 10.1186/1748-5908-5-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manilich E, Vogel JD, Kiran RP, et al. Key factors associated with postoperative complications in patients undergoing colorectal surgery. Dis Colon Rectum. 2013;56:64–71. doi: 10.1097/DCR.0b013e31827175f6. [DOI] [PubMed] [Google Scholar]
- 9.Kariv Y, Wang W, Senagore AJ, et al. Multivariable analysis of factors associated with hospital readmission after intestinal surgery. Am J Surg. 2006;191:364–371. doi: 10.1016/j.amjsurg.2005.10.038. [DOI] [PubMed] [Google Scholar]
- 10.Hendren S, Morris AM, Zhang W, Dimick J. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011;54:1362–1367. doi: 10.1097/DCR.0b013e31822b72d3. [DOI] [PubMed] [Google Scholar]
- 11.Kelly M, Sharp L, Dwane F, et al. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv Res. 2012;12:77. doi: 10.1186/1472-6963-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lucas DJ, Haider A, Haut E, et al. Assessing Readmission After General, Vascular, and Thoracic Surgery Using ACS-NSQIP. Ann Surg. 2013;258:430–439. doi: 10.1097/SLA.0b013e3182a18fcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gu J, Stocchi L, Remzi F, Kiran RP. Factors associated with postoperative morbidity, reoperation and readmission rates after laparoscopic total abdominal colectomy for ulcerative colitis. Colorectal Dis. 2013;15(9):1123–9. doi: 10.1111/codi.12267. [DOI] [PubMed] [Google Scholar]
- 14.Azimuddin K, Rosen L, Reed JF, 3rd, et al. Readmissions after colorectal surgery cannot be predicted. Dis Colon Rectum. 2001;44:942–946. doi: 10.1007/BF02235480. [DOI] [PubMed] [Google Scholar]
- 15.Kohlnhofer BM, Tevis SE, Weber SM, Kennedy GD. Multiple complications and short length of stay are associated with postoperative readmissions. Am J Surg. 2014;207(4):449–56. doi: 10.1016/j.amjsurg.2013.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ozturk E, Kiran RP, Remzi F, Fazio VW. Early readmission after ileoanal pouch surgery. Dis Colon Rectum. 2009;52:1848–1853. doi: 10.1007/DCR.0b013e3181b15610. [DOI] [PubMed] [Google Scholar]
- 17.Datta I, Buie WD, Maclean AR, Heine JA. Hospital readmission rates after ileal pouch-anal anastomosis. Dis Colon Rectum. 2009;52:55–58. doi: 10.1007/DCR.0b013e31819724a3. [DOI] [PubMed] [Google Scholar]
- 18.Williamson ME, Lewis WG, Sagar PM, et al. One-stage restorative proctocolectomy without temporary ileostomy for ulcerative colitis: a note of caution. Dis Colon Rectum. 1997;40:1019–1022. doi: 10.1007/BF02050922. [DOI] [PubMed] [Google Scholar]
- 19.Tjandra JJ, Fazio VW, Milsom JW, et al. Omission of temporary diversion in restorative proctocolectomy--is it safe? Dis Colon Rectum. 1993;36:1007–1014. doi: 10.1007/BF02047291. [DOI] [PubMed] [Google Scholar]
- 20.Sagar PM, Lewis W, Holdsworth PJ, Johnston D. One-stage restorative proctocolectomy without temporary defunctioning ileostomy. Dis Colon Rectum. 1992;35:582–588. doi: 10.1007/BF02050540. [DOI] [PubMed] [Google Scholar]
- 21.Ky AJ, Sonoda T, Milsom JW. One-stage laparoscopic restorative proctocolectomy: an alternative to the conventional approach? Dis Colon Rectum. 2002;45:207–210. doi: 10.1007/s10350-004-6149-5. discussion 210–201. [DOI] [PubMed] [Google Scholar]
- 22.Heuschen UA, Hinz U, Allemeyer EH, et al. One- or two-stage procedure for restorative proctocolectomy: rationale for a surgical strategy in ulcerative colitis. Ann Surg. 2001;234:788–794. doi: 10.1097/00000658-200112000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ikeuchi H, Nakano H, Uchino M, et al. Safety of one-stage restorative proctocolectomy for ulcerative colitis. Dis Colon Rectum. 2005;48:1550–1555. doi: 10.1007/s10350-005-0083-z. [DOI] [PubMed] [Google Scholar]
- 24.Singh P, Bhangu A, Nicholls RJ, Tekkis P. A systematic review and meta-analysis of laparoscopic vs open restorative proctocolectomy. Colorectal Dis. 2013;15:e340–351. doi: 10.1111/codi.12231. [DOI] [PubMed] [Google Scholar]
- 25.Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012;55:175–180. doi: 10.1097/DCR.0b013e31823d0ec5. [DOI] [PubMed] [Google Scholar]
- 26.Nagle D, Pare T, Keenan E, et al. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis Colon Rectum. 2012;55:1266–1272. doi: 10.1097/DCR.0b013e31827080c1. [DOI] [PubMed] [Google Scholar]


