Abstract
Background-Critical limb ischemia (CLI) is one of the most severe peripheral artery diseases. Angioplasty and bypass surgery are two major approaches for the treatment of CLI, however, it remains unclear which treatment has better benefit/risk ratio. In this paper, we performed a meta-analysis on the available clinical trials to compare these two approaches in terms of mortality, amputation-free survival, 5-year leg salvage, and freedom from surgical re-intervention. The results of this article will provide evidence based information for clinical treatment of CLI. Method-Randomized clinical trials comparing results between angioplasty and bypass surgery in CLI were identified by searching Pubmed (2000-2014) and EMBASE (2000-2014) using the search terms “angioplasty” or “bypass”, “CLI” and “clinical trials”. Primary outcome subjected to meta-analysis was amputation (of trial leg) free survival in 5 years. Secondary outcomes were 30-day mortality; mortality, re-interventions and leg salvage in 1, 3 and 5 years. Results-Seven clinical trials were selected for meta-analysis. No significant difference was found in the primary outcome-amputation free survival, between angioplasty and bypass surgery groups. The amputation free survival in 1, 3 and 5 years were 332/498 (66.7%), 169/346 (48.8%) and 21/60 (35%) in angioplasty group, versus 484/749 (64.6%), 250/494 (50.6%) and 46/132 (34.8%), in bypass group, respectively. The 30 days mortality rate was significantly higher in bypass treatment group [79/1304 (6.1%)] than in angioplasty group [30/918 (3.3%) [95% CI 0.55 [0.36, 0.86], P=0.008). However, there was no statistical significance in 1, 3 and 5 years mortality between these two groups. Two clinical trials showed that there was no difference in leg salvage between angioplasty and bypass surgery groups either. In addition, no difference was observed in re-vasculation between the two groups. Conclusion-Angioplasty is non-inferior to bypass surgery in regarding the amputation free survival, re-vasculation, leg amputation and overall mortality. However, angioplasty is safer, simple, and less invasive and less cost procedure. It should be considered as the first choice for feasible CLI patients.
Keywords: Critical limb ischemia, angioplasty, bypass, amputation free survival, meta analysis
Introduction
Critical limb ischemia (CLI) is clinically defined as persistent, recurring ischemic rest pain that persists for at least 2 weeks, ulceration or gangrene of the foot or toes, and is commonly associated with ankle systolic pressure less than 50 mmHg or toe systolic pressures less than 30 mmHg [1]. Patients with CLI who were treated successfully with surgical or endovascular revascularization have better quality of life and longer survival than those treated conservatively or with primary amputation [2,3]. Bypass surgery has traditionally been considered an approach of choice to re-vascularize ischemic limbs with rest pain, non-healing ulcers, or gangrene to avoid major amputation [4].
Transluminal angioplasty, in which the area of occlusion is expanded by a balloon inserted within the artery, is an important treatment for patients with more severe symptoms (short-distance claudication, rest pain, ulcers, and gangrene) [5]. Recently, an increasing number of cases of endovascular revascularizations have reported good leg salvage rates, even in the most challenging target area such as the infrapopliteal segment [6].
However, nowadays it is still unclear which treatment, angioplasty or bypass surgery, has better benefit/risk ratio. In this paper, we used meta-analysis to summarize all previous randomized clinical trials to compare these two approaches in terms of amputation-free survival, leg salvage, and freedom from surgical re-intervention and mortality. The results of this meta-analysis will provide evidence based information for clinical treatment for CLI patients and physicians.
Methods
Database and search strategy
We searched the following database for relevant studies: PubMed (from 2000 to May 2014) and EMBASE (from 2000 to May 2014). The search terms used for PubMed were: (“Angioplasty” or “bypass surgery” and “clinical limb ischemia” and “clinical trials”)
Study selection criteria and quality assessment
Eligible studies were selected based on the following criteria: 1) study design: randomized controlled clinical trials (RCTs); 2) subjects: patients who were diagnosed with CLI; 3) intervention: Angioplasty or Bypass surgery. All authors independently conducted study selection based on these criteria. Any discrepancy was resolved by group discussion of all authors. The quality of included trials was assessed using the Jadad scale score (0 to 5), with a score of 3 or above indicating high quality [7].
Primary and secondary outcomes
Primary outcome subjected to meta-analysis was amputation (of trial leg) free survival in 5 years. Secondary outcomes were all-cause mortality, 30-day mortality, re-interventions, leg salvage in 1, 3 and 5 years.
DATA extraction and statistical analysis
The following information was extracted from selected studies: author, publication year, study design, number of patients analyzed, treatment regimen, primary and secondary outcomes. All statistical analyses were performed using the Review Manager, version 5.1.0 (Cochrane Collaboration, Oxford, UK). Dichotomous outcomes were presented as event with a 95% confidence interval (CI). The presence of heterogeneity across trials was also evaluated. A P value < 0.05 was considered statistically significant. Peto-stastical models were used for the meta-analysis.
Results
Study identification and characteristics
A total of 31 unique records were identified by our search strategy. After initial screening by title and abstract, 7 relevant studies were selected for full text retrieving [8-14] (Figure 1). Among these studies, a total of 918 patients with the treatment with Angioplasty and 1304 patients with the treatment with bypass surgery were included in the final statistical analysis. The study characteristics and quality assessment are summarized in Table 1.
Figure 1.
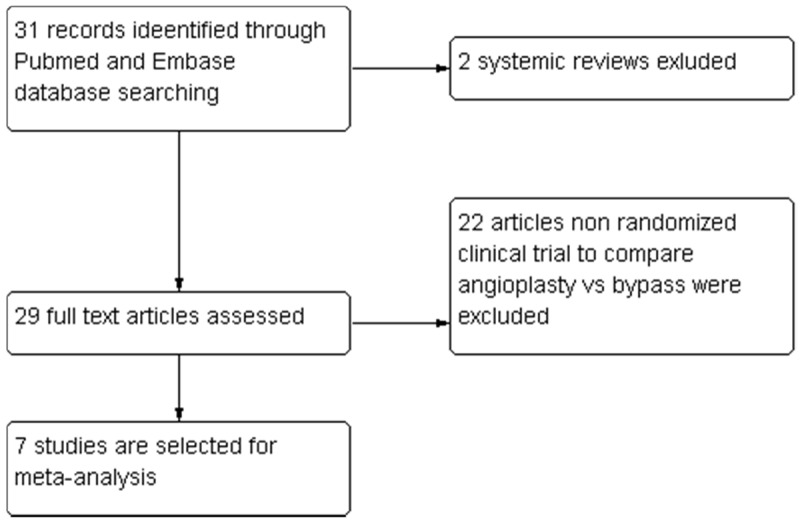
Flow diagram of study selection.
Table 1.
Study characteristics
| Study (year) | Study design | Number of Patients analyzed | Outcomes |
|---|---|---|---|
|
| |||
| Treatment regimen | |||
| Adam DJ (2005) | Randomized, multi-centered | PTA (224) | A bypass-surgery-first and a balloon-angioplasty-first strategy are associated with broadly similar outcomes in terms of amputation-free survival, and in the short-term, surgery is more expensive than angioplasty |
| Bypass (n=228) | |||
| Arvela E (2011) | prospectively | PTA (277) or bypass surgery (307) | A strategy of PTA first appears to achieve better results than infrainguinal bypass surgery in patients aged 80 years and older |
| Hynes N (2004) | retrospective analysis of a prospectively maintained vascular registry | PTA (158) | SIA plays a major role in the initial management of CLI, because it is cost effective, minimally invasive, associated with a high limb salvage rate, and is preferred by patients |
| Bypass (671) | |||
| Laurila J (2000) | retrospective | PTA (86) | PTA is a feasible and cost-effective procedure in chronic critical ischaemia of the lower limb and should be the treatment of choice in the subset of patients where both procedures are possible |
| Bypass (38) | |||
| Linnakoski H (2013) | retrospective, non-randomized | PTA (68) | First-line treatment for patients with SFA atherosclerotic occlusive disease is yet to be determined |
| Bypass (63) | |||
| Söderström MI (2010) | Treatment method (open or endovascular) were discussed among vascular surgeons and interventional radiologists. | PTA (262) | When feasible, infrapopliteal PTA as a first-line strategy is expected to achieve similar long-term results to bypass surgery in CLI when redo surgery is actively utilized |
| Bypass (761) | |||
| A propensity score was used for adjustment in multivariable analysis, for stratification, and for one-to-one matching. | |||
| van der Zaag ES (2004) | Randomized, multi-centered | PTA (31) | with respect to patency, for long superficial femoral artery (SFA) stenoses or occlusions, surgery is better than PTA |
| Bypass (25) |
Primary outcome-amputation survival
Three clinical trials were selected for amputation survival analysis. 498 patients underwent angioplasty treatment, while 749 patients received bypass surgeries. The meta-analysis revealed that in these 2 groups, there were no statistically significances at 1 year, 3 years and 5 years in amputation survival. At 1 year, Angioplasty amputation survival was 332/498 (66.7%) verse bypass group 484/749 (64.6%), 95% CI 1.11 (0.86, 1.42), P=0.42. At 3 years and 5 years, the amputation survival in angioplasty group was 169/346 (48.8%) vs 250/494 (50.6%) in bypass group, 95% CI 0.90 (0.67, 1.21), P=0.49; angioplasty group 21/60 (35%) vs bypass group 46/132 (34.8%), 95% CI 1.17 (0.57, 2.38), P=0.67 separately (Figure 2A-C).
Figure 2.
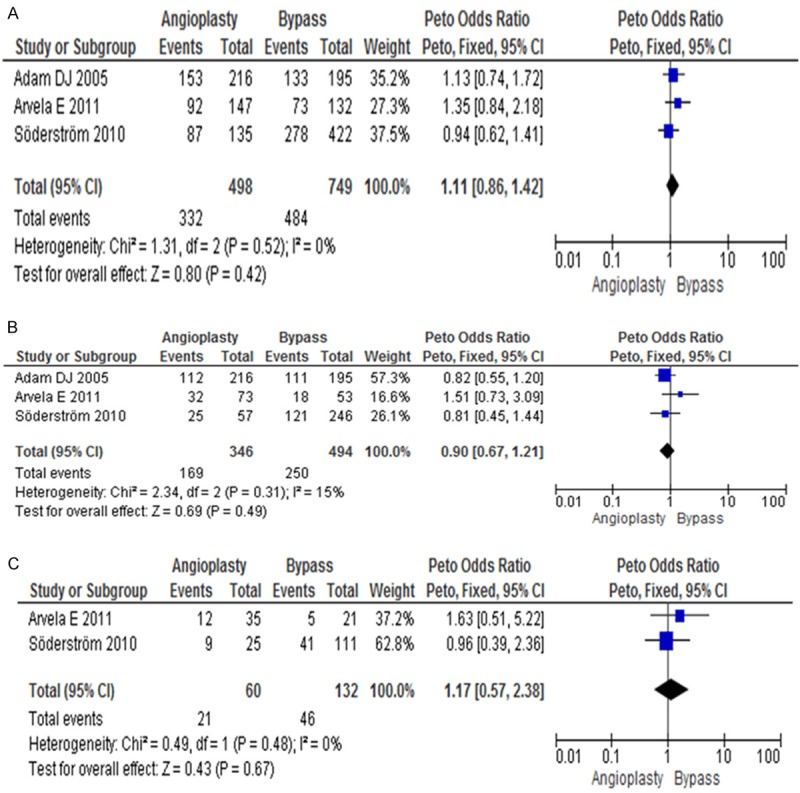
Forest plots comparing amputation-free survival between angioplasty group and bypass group. A. 1 year amputation-free survival; B. 3 year amputation survival; C. 5 year amputation survival.
Secondary outcomes
Mortality
The mortality rate within 30 days is less in angioplasty group [30/918 (3.26%)] when comparing with bypass surgery group [79/1304 (6.06%)]. 95% CI was 0.55 (0.36, 0.86), P=0.008. But no difference was observed in 1, 3 and 5 years long term follow up between these two groups (Figure 3A-D).
Figure 3.
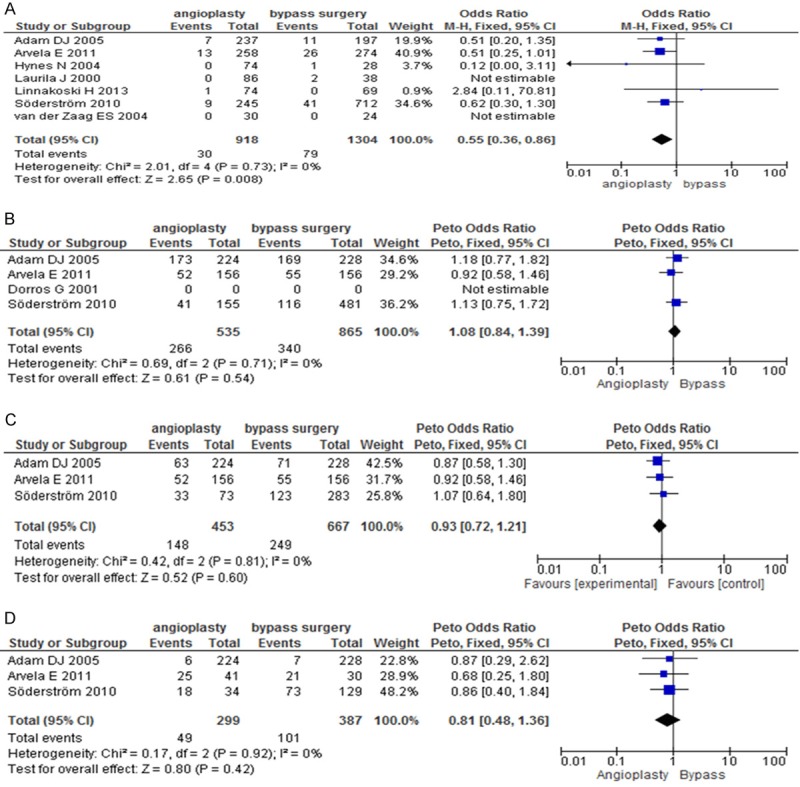
Forest plots comparing mortality rate between angioplasty group and bypass group in (A) 30 days; (B) 1 year; (C) 3 years; and (D) 5 years.
Leg salvage
No statistically difference was observed in leg salvage in 1, 3 and 5 years. Follow up. In angioplasty group were 246/282 (87.2%), 103/129 (79.8%) and 46/60 (76.7%), while in bypass group were 452/554 (81.6%), 235/299 (78.6%) and 99/132 (75%) (Figure 4A-C).
Figure 4.
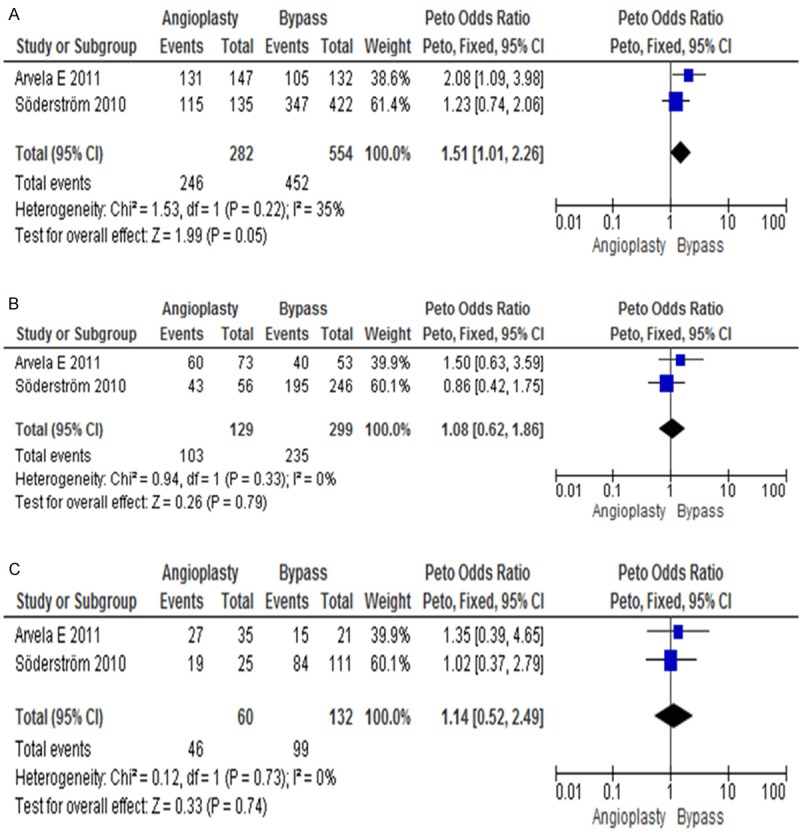
Forest plots comparing the leg salvage rate between angioplasty group and bypass group in (A) 1 year; (B) 3 years; and (C) 5 years.
Hospital stay and cost
We did not analyze the days of hospital stay and cost because there are different policies for different hospital which can affect the inpatient stay duration and costs. However, we know the angioplasty is min-invasive procedure, it should have less inpatient stay, less complications and cost when comparing with bypass surgery treatment.
Publication bias and quality
Begg’s funnel plot was used for the assessment of the publication bias of selected studies used for meta-analysis. No publication bias was detected (Figure 5). The Jadad score of these studies ranged from 3 to 5, indicating that these trials were of satisfactory quality.
Figure 5.
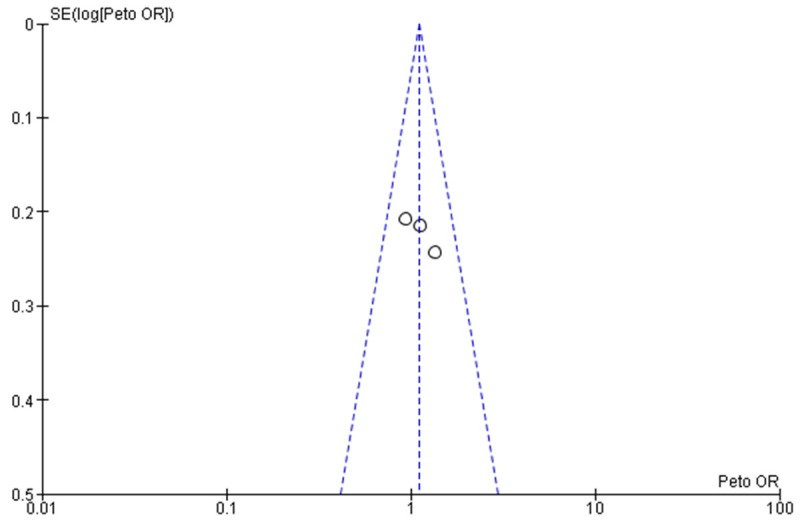
Funnel plot of the studies selected. The plot is for qualitative estimation of publication bias of the studies. No bias was found.
Discussion
Patients with CLI who were treated successfully with surgical or endovascular revascularization had better quality of life and longer survival than those treated conservatively or with primary amputation [15,16]. However, the CLI patients often have cardiovascular, diabetes or other co-morbidities, which are associated with increased perioperative and postoperative mortality [17]. In recent years, endovascular interventions are widely used for CLI patients.
Currently in clinic, it remains unclear which intervention has better outcomes. Some studies showed that short-term survival is better in patients with angioplasty than those with bypass surgery [8,16], which favorably made angioplasty as a tempting first-choice treatment in CLI patients. However, other studies showed that bypass surgery resulted in better leg salvation survival than angioplasty [13]. The aim of this study was to compare the amputation free survival, mortality and leg salvage rate in angioplasty versus surgical bypass in a population of patients with CLI.
Our multiple analysis results showed that there are no differences in leg salvation survival, re-vasculation, and long term mortality between these two groups. However, the mortality rate within 30 days was lower in angioplasty group than in bypass group. Also, angioplasty was non-inferior to bypass surgery in regarding the amputation free survival, re-vasculation, leg amputation and overall mortality. In contrast, angioplasty was a safer, simpler, and less invasive procedure with less cost, compared to bypass surgery. Based on these results, it is suggested that angioplasty should be considered as the first choice for feasible CLI patients.
There are a few limitations in this meta-analysis. Specifically, 1) the studies included lack large sample size, randomized and double blinded clinical trials. A few clinical trial studies had to early termination in a short period due to poor enrollment. 2). Two groups patient population cannot be similar because the treatment option was chosen by the physician based on patient CLI severity.
In the future, it still needs multi-center, large sample size, double blind clinical trials to draw the evidence-based conclusion. From the data we have, we can at least conclude that angioplasty is not inferior to bypass treatment.
Disclosure of conflict of interest
None.
References
- 1.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) J Vasc Surg. 2007;45:S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 2.Klevsgård R, Risberg BO, Thomsen MB, Hallberg IR. A 1-year follow-up quality of life study after hemodynamically successful or unsuccessful surgical revascularization of lower limb ischemia. J Vasc Surg. 2001;33:114–122. doi: 10.1067/mva.2001.109769. [DOI] [PubMed] [Google Scholar]
- 3.Brosi P, Dick F, Do DD, Schmidli J, Baumgartner I, Diehm N. Revascularization for chronic critical lower limb ischemia in octogenarians is worthwhile. J Vasc Surg. 2007;46:1198–1207. doi: 10.1016/j.jvs.2007.07.047. [DOI] [PubMed] [Google Scholar]
- 4.Conte MS. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) and the (hoped for) dawn of evidence-based treatment for advanced limb ischemia. J Vasc Surg. 2010;51:69S–75S. doi: 10.1016/j.jvs.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Fowkes F, Leng GC. Bypass surgery for chronic lower limb ischaemia. Cochrane Database Syst Rev. 2008:CD002000. doi: 10.1002/14651858.CD002000.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Romiti M, Albers M, Brochado-Neto FC, Durazzo AE, Pereira CA, De Luccia N. Metaanalysis of infra-popliteal angioplasty for chronic critical limb ischemia. J Vasc Surg. 2008;47:975–981. doi: 10.1016/j.jvs.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 8.Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, Fowkes FG, Gillepsie I, Ruckley CV, Raab G, Storkey H BASIL trial participants. BASIL trial participants. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366:1925–1934. doi: 10.1016/S0140-6736(05)67704-5. [DOI] [PubMed] [Google Scholar]
- 9.Arvela E, Venermo M, Söderström M, Korhonen M, Halmesmäki K, Albäck A, Lepäntalo M, Biancari F. Infrainguinal percutaneous transluminal angioplasty or bypass surgery in patients aged 80 years and older with critical leg ischaemia. Br J Surg. 2011;98:518–26. doi: 10.1002/bjs.7390. [DOI] [PubMed] [Google Scholar]
- 10.Hynes N, Akhtar Y, Manning B, Aremu M, Oiakhinan K, Courtney D, Sultan S. Subintimal angioplasty as a primary modality in the management of critical limb ischemia: comparison to bypass grafting for aortoiliac and femoropopliteal occlusive disease. J Endovasc Ther. 2004;11:460–71. doi: 10.1583/04-1242.1. [DOI] [PubMed] [Google Scholar]
- 11.Laurila J, Brommels M, Standertskjöld-Nordenstam CG, Leinonen S, Lepäntalo M, Edgren J, Suramo II. Cost-effectiveness of Percutaneous Transluminal Angioplasty (PTA) Versus Vascular Surgery in Limb-threatening Ischaemia. Int J Angiol. 2000;9:214–219. doi: 10.1007/BF01623897. [DOI] [PubMed] [Google Scholar]
- 12.Linnakoski H, Uurto I, Suominen V, Vakhitov D, Salenius J. Comparison of above-the-knee prosthetic femoro-popliteal bypass versus percutaneous transluminal angioplasty and stenting for treatment of occlusive superficial femoral artery disease. Scand J Surg. 2013;102:227–233. doi: 10.1177/1457496913501591. [DOI] [PubMed] [Google Scholar]
- 13.Söderström MI, Arvela EM, Korhonen M, Halmesmäki KH, Albäck AN, Biancari F, Lepäntalo MJ, Venermo MA. Infrapopliteal percutaneous transluminal angioplasty versus bypass surgery as first-line strategies in critical leg ischemia: a propensity score analysis. Ann Surg. 2010;252:765–73. doi: 10.1097/SLA.0b013e3181fc3c73. [DOI] [PubMed] [Google Scholar]
- 14.Van der Zaag ES, Legemate DA, Prins MH, Reekers JA, Jacobs MJ. Angioplasty or bypass for superficial femoral artery disease? A randomised controlled trial. Eur J Vasc Endovasc Surg. 2004;28:132–7. doi: 10.1016/j.ejvs.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Klevsgård R, Risberg BO, Thomsen MB, Hallberg IR. A 1-year follow-up quality of life study after hemodynamically successful or unsuccessful surgical revascularization of lower limb ischemia. J Vasc Surg. 2001;33:114–122. doi: 10.1067/mva.2001.109769. [DOI] [PubMed] [Google Scholar]
- 16.Brosi P, Dick F, Do DD, Schmidli J, Baumgartner I, Diehm N. Revascularization for chronic critical lower limb ischemia in octogenarians is worthwhile. J Vasc Surg. 2007;46:1198–1207. doi: 10.1016/j.jvs.2007.07.047. [DOI] [PubMed] [Google Scholar]
- 17.Plecha FR, Bertin VJ, Plecha EJ, Avellone JC, Farrell CJ, Hertzer NR, Mayda J 2nd, Rhodes RS. The early results of vascular surgery in patients 75 years of age or older: an analysis of 3259 cases. J Vasc Surg. 1985;2:769–774. [PubMed] [Google Scholar]


