Abstract
Elderly patients are at high risk of mortality when they present with ST-elevation myocardial infarction (STEMI). However, the clinical outcomes of this sub-group undergoing primary percutaneous coronary intervention (PPCI) have not been well established, despite recent advances in both devices and techniques. In the present retrospective cohort study from a Chinese single center, we assessed the clinical outcomes and predictors of mortality in elderly patients (≥60 years) underwent with PPCI. The primary endpoints were immediate angiographic success and in-hospital procedural success. The secondary endpoints were all-cause death in hospital. Between January 2011 and December 2013, a total of 184 consecutive patients with acute STEMI underwent PPCI were enrolled. 116 (63.04%) patients were in the elderly group. Despite the difference in lesion complexity between groups, the immediate angiographic success rate was similar (93.97% in the elderly group, and 94.12% in the non-elderly group, P=0.966). The procedural success rate were not significantly different between the two groups (90.52% in the elderly group, and 94.12% in the non-elderly group, P=0.389). However, in-hospital mortality was statistically higher in elderly group than in the non-elderly group (8.62% Vs 1.47%, P=0.048). The major causes of death were cardiac shock and malignant arrhythmias (ventricular tachycardia and fibrillation). Our results indicate that PPCI in the elderly is feasible and has a high likelihood of immediate angiographic and procedural success.
Keywords: Coronary artery disease, ST-elevation myocardial infarction, elderly, primary percutaneous coronary intervention
Introduction
The population is progressively aging and cardiovascular prevention is improving in China. Thus, the age of patients suffered from ST-elevation myocardial infarction (STEMI) is expected to rise in the next decades. In elderly patients, the outcome after STEMI is worse than in younger people, but they are less likely to receive reperfusion therapies [1-3]. Compared to younger patients, the elderly patients with acute STEMI have a heavier burden of comorbid conditions [4-7], making the treatment more difficult. As fibrinolytic therapy could be associated with increased bleeding risk, especially in the elderly [8-10], the advantages of primary percutaneous coronary intervention (PPCI) in elderly patients with acute STEMI are apparent. In recent years, interventional techniques [11,12] and antithrombotic therapies [13-15] made a lot of progress. PPCI is recommended as the treatment of choice in patients with STEMI when feasible, regardless of age [16]. However, there is paucity of evidence-based data about safety and efficacy of PPCI in the elderly STEMI patients due to their exclusion and under-representation in clinical trials [17]. The Chinese data regarding clinical characteristics and outcomes of elderly patients undergoing PPCI have scarcely been well established.
The present study is a retrospective cohort report from a Chinese single center, presenting the differences in baseline characteristics and in-hospital outcomes after PPCI between elderly and non-elderly acute STEMI patients in the contemporary era. The aim of this study is to assess the outcomes and predictors of mortality in this subgroup in the real world.
Subjects and methods
Study subject
Between January 2011 and December 2013, a total of 184 consecutive patients with acute STEMI underwent PPCI admitted to our hospital were enrolled. Diagnosis ofacute STEMI should meet 2 below criteria or more [16]: (1) within 12 hours from the onset of chest pain, or ≥12 h from symptom onset presenting evidence of ongoing ischemia, or cardiac shock; (2) new ST segment elevation at the J point in at least 2 contiguous leads of 0.2 mV in men or 0.15 mV in women in leads V2-V3 and/or of 0.1 mV in other contiguous chest leads or the limb leads, or New or presumably new left bundle-branch block (LBBB); (3) release of biomarkers of myocardial necrosis (such as Troponin I, creatine kinase, myoglobin). These patients were divided into the elderly group (age ≥60 years, n=116) and the non-elderly group (age <60 years, n=68). Current smoking, hypertension, and diabetes mellitus (DM) were defined according to past literature reports [18-21]. Measurement of leukocyte, platelet (PLT), creatinine (Cr), total cholesterol (TC), high density lipoprotein-cholesterol (HDL-C), low density lipoprotein-cholesterol (LDL-C), and triglycerides (TG) was performed as described previously [18-24]. Written informed consent about interventional operation was obtained from all patients.
Interventional procedure
Before PPCI, Aspirin (300 mg) and a P2Y12 receptor inhibitor (clopidogrel 300-600 mg, or ticagrelor 180 mg) were orally administrated. After the sheath was placed into radial or femoral artery access, a bolus of unfractionated heparin (70-100 IU/kg) was given. Standard Judkin’s technique was used to perform coronary angiography. Combining the selective coronary angiography results with preoperative ECG findings, the target lesion sites were determined. PPCI only on the infarct-related artery was recommended, except the situation of cardiac shock. After completion of PPCI, all patients were treated with clopidogrel (75 mg daily) or ticagrelor (90 mg twice per day) at least 1 year, in addition to lifelong oral aspirin (100-150 mg daily).
Study endpoints and definitions
The primary endpoints were immediate angiographic success and in-hospital procedural success. The secondary endpoints were all-cause death in hospital. Immediate angiographic success was defined as achievement of culprit arterial lumen diameter reduction to less than 20% with grade 3 Thrombolysis In Myocardial Infarction (TIMI) flow [25]. Procedural success was defined as achievement of immediate angiographic success without any complications during hospitalization [25]. Complications included all-cause death, recurrence of MI, stroke, major bleeding complications, worsened renal function, coronary artery perforation, cardiac rupture. Coronary artery disease (CAD) was defined as serious stenosis (≥70% reduction of lumen diameter) in major coronary artery on coronary angiography. Multivessel disease was defined as the presence of serious stenosis (≥70% reduction of lumen diameter) in ≥2 major coronary arteries. Left main trunk (LMT) disease was defined as the presence of ≥50% reduction of lumen diameter, which was equalized to two vessels disease [19,25].
Statistical analysis
All continuous variables are expressed as the mean and standard deviation (SD), while categorical data are presented as numbers by direct count. Differences between the two groups were compared, using student’s t-test for continuous variables and chi-squared test for categorical data. All significant tests were two-tailed and were considered statistically significant at P<0.05. SPSS for Windows version 16.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
Baseline characteristics
Table 1 summarizes the baseline characteristics of all patients enrolled in the study. Of the total 184 cases, 116 patients were ≥60 years, accounting for 63.04%. No significant differences were seen between the two groups with regard to prevalence of DM, leukocyte count, PLT count, random plasma glucose, Cr, HDL-C, and TG. Pre-hospital delay despite a longer trend in the elderly group did not differ substantially in the two groups. However, compared with the non-elderly group, the elderly patients had significantly older ages, more cardiac dysfunction, longer mean in-hospital duration, higher percentage of female and presence of hypertension, but lower smoking status, TC, and TC levels.
Table 1.
Baseline characteristics between two groups
| Baseline characteristics | Non-elderly (n=68) | Elderly (n=116) | P value |
|---|---|---|---|
| Age (years) | 49.21±7.56 | 70.97±7.23 | 0.000 |
| Female (n, %) | 2 (2.94%) | 29 (25%) | 0.000 |
| Hypertension (n, %) | 30 (44.12%) | 81 (69.83%) | 0.000 |
| Diabetes mellitus (n, %) | 10 (14.71%) | 20 (17.24%) | 0.653 |
| Smoking (n, %) | 46 (67.65%) | 50 (43.10%) | 0.001 |
| Pre-hospital delay (hours) | 5.97±3.17 | 6.47±4.09 | 0.384 |
| Killip level 2-4 (n, %) | 7 (10.29%) | 38 (32.76%) | 0.001 |
| Leukocyte count (109/L) | 11.06±3.66 | 10.45±3.15 | 0.233 |
| Platelet count (109/L) | 201.13±53.65 | 190.19±51.49 | 0.172 |
| Random glucose (mmol/L) | 7.53±2.47 | 8.51±4.40 | 0.055 |
| TC (mmol/L) | 5.30±1.22 | 4.87±1.00 | 0.009 |
| LDL-C (mmol/L) | 3.35±1.07 | 2.91±0.77 | 0.001 |
| HDL-C (mmol/L) | 1.14±0.28 | 1.16±0.32 | 0.613 |
| TG (mmol/L) | 1.53±1.02 | 1.33±0.77 | 0.145 |
| Creatinine (umol/L) | 71.63±15.79 | 75.14±18.83 | 0.178 |
| Mean in-hospital duration (days) | 10.76±3.79 | 12.46±6.63 | 0.029 |
TC, total cholesterol; LDL-C, lower density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; TG, triglyceride.
Angiographic characteristics
Angiographic characteristics between two groups are shown in Table 2. The majority of patients underwent catheterization through a transradial approach (92.24% in the elderly group, and 95.59% in the non-elderly group). The culprit lesion was most often found in the left anterior descending artery (LAD) in both the elderly group (49.14%) and the non-elderly group (52.94%).There were no statistically differences in the constitution of culprit arteries, preoperative flow level, and bifurcation lesions between the two groups. However, more number of vessels affected and calcified lesions were found in the elderly group than in the non-elderly group.
Table 2.
Angiographic characteristics between two groups
| Angiographic characteristics | Non-elderly (n=68) | Elderly (n=116) | P value |
|---|---|---|---|
| Procedure access (n, %) | |||
| Transradial approach | 65 (95.59%) | 107(92.24%) | |
| Transfemoral approach | 3 (4.41%) | 9 (7.76%) | 0.375 |
| Culprit artery (n, %) | |||
| LMT | 0 | 3 (2.59%) | |
| LAD | 36 (52.94%) | 57 (49.14%) | |
| LCX | 9 (13.24%) | 10 (8.62%) | |
| RCA | 23 (33.82%) | 46 (39.65%) | 0.368 |
| Number of vessels affected (n, %) | |||
| Single-vessel | 33 (48.53%) | 36 (31.03%) | |
| Multi-vessel | 35 (51.47%) | 80 (68.97%) | 0.018 |
| Preoperative flow level (n, %) | |||
| TIMI flow 0/1 | 52 (76.47%) | 95 (81.90%) | |
| TIMI flow 2/3 | 16 (23.53%) | 21 (18.10%) | 0.375 |
| Bifurcation lesion (n, %) | 20 (29.41%) | 31 (26.72%) | 0.694 |
| Calcified lesion (n, %) | 9 (13.24%) | 32 (27.59%) | 0.024 |
LMT, Left main trunk; LAD, left anterior descending artery; LCX, left circumflex coronary artery; RCA, right coronary artery; TIMI, thrombolysis in myocardial infarction.
Immediate angiographic success and in-hospital procedural success
As shown in Table 3, procedure time was longer in the elderly group than in the non-elderly group. However, no significant differences were found in such aspects between the two groups, including bare metal stent (BMS) proportion, drug-eluting stent (DES) proportion, intra-aortic balloon pump (IABP) utilization, temporary pacemaker utilization, average stent diameter and length, incidence of ventricular tachycardia (VT) and ventricular fibrillation (VF) during PPCI procedure. There were 4 patients failed during the PPCI procedure in the non-elderly group (coronary perforation in 1 case, slow reflow and final TIMI flow ≤2 in 1 case, wires failed to run through occluded lesions in 2 cases); while 7 cases in the elderly group (death in 2 cases, dissection in 1 case, slow reflow and final TIMI flow ≤2 in 1 case, wires failed to run through occluded lesions in 1 cases, choosing coronary artery bypass grafting (CABG) in 1 case, given up by family members in 1 case). Despite the difference in lesion complexity between groups, the immediate angiographic success rate was similar (93.97% in the elderly group, and 94.12% in the non-elderly group, P=0.966).
Table 3.
Procedural characteristics between two groups
| Procedural characteristics | Non-elderly (n=68) | Elderly (n=116) | P value |
|---|---|---|---|
| Number of stents (n, %) | |||
| BMS | 12 (15.38%) | 23 (14.20%) | |
| DES | 66 (84.62%) | 139 (85.80%) | 0.807 |
| Average stent diameter (mm) | 3.19±0.40 | 3.09±0.42 | 0.080 |
| Average stent length (mm) | 24.23±7.11 | 24.85±6.72 | 0.511 |
| VT/VF during PCI (n, %) | 4 (5.88%) | 15 (12.93%) | 0.129 |
| Use of IABP (n, %) | 1 (1.47%) | 2 (1.72%) | 0.896 |
| Aspiration thrombectomy (n, %) | 5 (7.35%) | 9 (7.76%) | 0.920 |
| Temporary pacemaker | 6 (8.82%) | 14 (12.07%) | 0.495 |
| Immediate angiographic success (n, %) | 64 (94.12%) | 109 (93.97%) | 0.966 |
| In-hospital procedural success (n, %) | 64 (94.12%) | 105 (90.52%) | 0.389 |
| Procedure time (minutes) | 55.85±16.08 | 62.84±22.57 | 0.016 |
BMS, bare metal stent; DES, drug-eluting stent; VT, ventricular tachycardia; VF, ventricular fibrillation; PCI, percutaneous coronary intervention; IABP, intra-aortic balloon pump.
In the patients with angiographic success, 4 cases died in the elderly group during hospitalization, while none in the non-elderly group. Nevertheless, the procedural success rate were not significantly different between the two groups (90.52% in the elderly group, and 94.12% in the non-elderly group, P=0.389). Seen in Figure 1.
Figure 1.
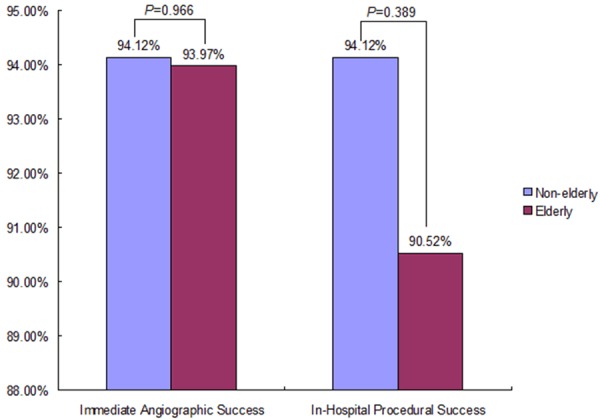
Immediate angiographic success and in-hospital procedural success rates between two groups.
In-hospital mortality
The total in-hospital mortality was 5.98% in 184 STEMI patients, which was statistically higher in elderly group than in the non-elderly group (8.62% Vs 1.47%, P=0.048).
Discussion
The present retrospective study from a single center was conducted in a cohort of 116 patients’ age ≥60 years undergoing PPCI and outlines a real-world experience for invasive treatment of STEMI in the elderly. Our results confirm that these patients account for a significant proportion of patients with acute MI [16,26].
Population aging process in China is gradually accelerating. Aging is an independent predictor of atherosclerosis and cardiovascular events. Compared with non-elderly patients, elderly patients with STEMI have more complications and severe coronary lesions. It is of note that the prevalence of smoking status and hyperlipidemia was significantly higher in the non-elderly, suggesting that patients with hyperlipidemia and smoking tend to suffer from STEMI earlier. Thus, healthy lifestyles and control of traditional risk factors are important to these patients, in order to control the occurrence and development of CAD.
Our center’s data show that more number of vessels affected and calcified lesions were found in the elderly group than in the non-elderly group, presenting heavier plaque burden in the elderly. These angiographic lesion characteristics limit the application of fibrinolytic therapy and reduce the treatment effect in the elderly. Thus, PPCI technique benefits the elderly patients with acute STEM apparently, but put forward stricter requirements.
The present study demonstrates that PPCI in the elderly is feasible and has a high likelihood of immediate angiographic and procedural success, which is consistent with previous studies of elderly patients [5,26,27]. However, the elderly group had a longer duration of hospitalization, and a higher rate of in-hospital mortality than the non-elderly group. Considering the serious non-criminal vascular stenosis still leads to myocardial ischemia, change of PPCI strategy in multivessel diseased patients, who are frequent in aged group, may be reasonable. The PRAMI [28] research enrolled 465 patients with acute STEMI, who were randomly divided into preventive PCI (234 patients) or non-preventive PCI (231 patients, only treating the artery responsible for the infarct during PPCI). During an average follow-up of 23 months, the primary outcome (death from cardiac causes, nonfatal myocardial infarction, refractory angina) occurred in 21 (9%) patients assigned to preventive PCI and in 53 (23%) patients assigned to non-preventive PCI, hazard ratio in the preventive-PCI group was 0.35 (95% confidence interval [CI], 0.21 to 0.58; P<0.001). The PRAMI study suggest that, compared with PPCI limited to the infarct-related artery in STEMI patients with multivessel disease, preventive PCI in non-criminal coronary arteries with major stenosis significantly reduced the risk of adverse cardiovascular events. However, in PRAMI study, subsequent PCI for angina was recommended only for refractory angina with objective evidence of ischemia. In our center, PPCI only on the infarct-related artery was recommended, except the situation of cardiac shock [16]. But subsequent PCI in non-criminal coronary arteries with major stenosis were operated conventionally, also obtaining satisfying clinical effect.
Time for acute STEMI patients means myocardium and survival. Nowadays guidelines emphasize shortening Door-to-Balloon time. The GRACE [29] study showed marked geographic differences in extent of pre-hospital delay in patients with acute STEMI. The shortest duration of pre-hospital delay was observed from Australia/New Zealand (median 2.2 hours), whereas patients from Argentina and Brazil delayed the longest (median 4.0 hours). However, our center’s local data presented even significantly longer duration of pre-hospital delay in both elderly (6.47±4.09 hours) and non-elderly group (5.97±3.17 hours). Pre-hospital delay in acute STEMI patients should be paid enough attention in China. Popularizing knowledge of STEMI and improving emergency medical services (EMS) [30,31], could help to shorten the duration of pre-hospital delay, dramatically improve the prognosis.
Consensus document on the transradial approach in percutaneous cardiovascular interventions was published in 2013 [32]. Our data showed that 90.52% in the elderly group, and 94.12% in the non-elderly group underwent PCI through transradial access. Compared to transfemoral access, transradial approach has more attractive advantages, including fewer vascular complications, more rapid ambulation, and greater post-procedural comfort. The OCTOPLUS study [33] showed that, compared to femoral access, radial access in 80 elderly patients can obviously reduce the incidence of vascular complications (1.6% vs 6.5%, P=0.03). Achenbach at al [34] also observed similar results in elderly patients aged over 75 years. Regarding puncture of radial artery, our experiences include: (1) Choosing puncture site exactly, not too close to the wrist crease, otherwise it would increase the difficulty of inserting sheath. (2) Injection of too much anesthetic drug will affect the judgment of the radial pulse, after successful puncture, we could add dosage of anesthetics. (3) Radial artery is relatively slim, often occurs spasm. Thus, success in first time is very important. (4) Variations in radial anatomy are frequent. Sometimes, putting through wires and inserting the sheath under X-ray may be necessary.
Study limitations
Our study has some potential limitations. Firstly, a retrospective, single center cohort study has its inherent limitation. Secondly, the size of the enrolled participants is relatively small, which may weaken statistical conclusions. Thirdly, our study did not evaluate long-term outcomes, and data regarding post-discharge treatment were also not collected.
Conclusions
In conclusion, elderly patients with acute STEMI tend to have more severe complex lesions (multivessels, calcifications, in particular). However, despite the higher mortality in the elderly group during hospitalization, PPCI in the elderly is feasible and has a high likelihood of immediate angiographic and procedural success. Progress in interventional techniques, shortening the duration of pre-hospital delay and changes related to PPCI strategy may improve the prognosis further.
Acknowledgements
This work was supported by the Clinical Medicine Special Foundation of Nantong City (HS2013069), and “Summit of the Six Top Talents” Program of Jiangsu Province (2009046), P. R. China.
Disclosure of conflict of interest
None.
References
- 1.Gharacholou SM, Alexander KP, Chen AY, Wang TY, Melloni C, Gibler WB, Pollack CV Jr, Ohman EM, Peterson ED, Roe MT. Implications and reasons for the lack of use of reperfusion therapy in patients with ST-segment elevation myocardial infarction: findings from the CRUSADE initiative. Am Heart J. 2010;159:757–763. doi: 10.1016/j.ahj.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Islam S, Yakout SM, Daghri NM, Alhomida AS, Khan HA. Serum levels of thrombotic markers in patients with acute myocardial infarction. Int J Clin Exp Med. 2014;7:1059–1063. [PMC free article] [PubMed] [Google Scholar]
- 3.Xiao J, Shen B, Li J, Lv D, Zhao Y, Wang F, Xu J. Serum microRNA-499 and microRNA-208a as biomarkers of acute myocardial infarction. Int J Clin Exp Med. 2014;7:136–141. [PMC free article] [PubMed] [Google Scholar]
- 4.Kaneko H, Yajima J, Oikawa Y, Tanaka S, Fukamachi D, Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Kano H, Uejima T, Koike A, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita T. Impact of aging on the clinical outcomes of Japanese patients with coronary artery disease after percutaneous coronary intervention. Heart Vessels. 2014;29:156–164. doi: 10.1007/s00380-013-0339-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miura T, Miyashita Y, Motoki H, Shimada K, Kobayashi M, Nakajima H, Kimura H, Akanuma H, Mawatari E, Sato T, Hotta S, Kamiyoshi Y, Maruyama T, Watanabe N, Eisawa T, Aso S, Uchikawa S, Hashizume N, Sekimura N, Morita T, Ebisawa S, Izawa A, Tomita T, Koyama J, Ikeda U. In-hospital clinical outcomes of elderly patients (≥80 years) undergoing percutaneous coronary intervention. Circ J. 2014;78:1097–1103. doi: 10.1253/circj.cj-14-0129. [DOI] [PubMed] [Google Scholar]
- 6.Chen SJ, Gong Z, Duan QL. Evaluation of heart function with impedance cardiography in acute myocardial infarction patients. Int J Clin Exp Med. 2014;7:719–727. [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan S, Kaplan ST, Kiris A, Gedikli O. Impact of initial platelet count on baseline angiographic finding and end-points in ST-elevation myocardial infarction referred for primary percutaneous coronary intervention. Int J Clin Exp Med. 2014;7:1064–1070. [PMC free article] [PubMed] [Google Scholar]
- 8.Angeja BG, Gibson CM, Chin R, Canto JG, Barron HV. Use of reperfusion therapies in elderly patients with acute myocardial infarction. Drugs Aging. 2001;18:587–596. doi: 10.2165/00002512-200118080-00003. [DOI] [PubMed] [Google Scholar]
- 9.Karha J, Topol EJ. Primary percutaneous coronary intervention vs. fibrinolytic therapy for acute ST-elevation myocardial infarction in the elderly. Am J Geriatr Cardiol. 2006;15:19–21. doi: 10.1111/j.1076-7460.2006.05290.x. [DOI] [PubMed] [Google Scholar]
- 10.Khan HA, Alhomida AS, Rammah TY, Sobki SH, Ola MS, Khan AA. Alterations in prothrombin time and activated partial thromboplastin time in patients with acute myocardial infarction. Int J Clin Exp Med. 2013;6:294–297. [PMC free article] [PubMed] [Google Scholar]
- 11.Wijns W, Steg PG, Mauri L, Kurowski V, Parikh K, Gao R, Bode C, Greenwood JP, Lipsic E, Alamgir F, Rademaker-Havinga T, Boersma E, Radke P, van Leeuwen F, Camenzind E. Endeavour zotarolimus-eluting stent reduces stent thrombosis and improves clinical outcomes compared with cypher sirolimus-eluting stent: 4 year results of the PROTECT randomized trial. Eur Heart J. 2014;35:2812–2820. doi: 10.1093/eurheartj/ehu318. [DOI] [PubMed] [Google Scholar]
- 12.Lee JM, Park KW, Han JK, Yang HM, Kang HJ, Koo BK, Bae JW, Woo SI, Park JS, Jin DK, Jeon DW, Oh SK, Park JS, Kim DI, Hyon MS, Jeon HK, Lim DS, Kim MG, Rha SW, Her SH, Hwang JY, Kim S, Choi YJ, Kang JH, Moon KW, Jang Y, Kim HS. Three-Year Patient-Related and Stent-Related Outcomes of Second-Generation Everolimus-Eluting Xience V Stents Versus Zotarolimus-Eluting Resolute Stents in Real-World Practice (from the Multicenter Prospective EXCELLENT and RESOLUTE-Korea Registries) Am J Cardiol. 2014;114:1329–1338. doi: 10.1016/j.amjcard.2014.07.065. [DOI] [PubMed] [Google Scholar]
- 13.Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 14.Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington RA, Freij A, Thorsen M. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 15.Bhatt DL, Stone GW, Mahaffey KW, Gibson CM, Steg PG, Hamm CW, Price MJ, Leonardi S, Gallup D, Bramucci E, Radke PW, Widimsky P, Tousek F, Tauth J, Spriggs D, McLaurin BT, Angiolillo DJ, Genereux P, Liu T, Prats J, Todd M, Skerjanec S, White HD, Harrington RA. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med. 2013;368:1303–1313. doi: 10.1056/NEJMoa1300815. [DOI] [PubMed] [Google Scholar]
- 16.O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Caretta G, Passamonti E, Pedroni PN, Fadin BM, Galeazzi GL, Pirelli S. Outcomes and Predictors of Mortality Among Octogenarians and Older With ST-Segment Elevation Myocardial Infarction Treated With Primary Coronary Angioplasty. Clin Cardiol. 2014;37:523–529. doi: 10.1002/clc.22313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan M, Zhu JH, Liu ZH, Jiang WP, Cui ZC, Yu XH, Li HM, Yang XJ. Angiotensin-converting enzyme gene 2350 G/A polymorphism is associated with left ventricular hypertrophy but not essential hypertension. Hypertens Res. 2007;30:31–37. doi: 10.1291/hypres.30.31. [DOI] [PubMed] [Google Scholar]
- 19.Pan M, Jiang MH, Wei MF, Liu ZH, Jiang WP, Geng HH, Cui ZC, Zhang DL, Zhu JH. Association of angiotensin-converting enzyme gene 2350-G>A polymorphism with myocardial infarction in a Chinese population. Clin Appl Thromb Hemost. 2009;15:435–442. doi: 10.1177/1076029608316013. [DOI] [PubMed] [Google Scholar]
- 20.Chen F, Guo J, Gao SP, Chen C, Guo YF, Gui L, Geng HH, Ge LJ, Zhu JH, Pan M. Interleukin-6 -634C>G polymorphism in hypertensive patients with and without left ventricular hypertrophy. Mol Med Rep. 2011;4:283–289. doi: 10.3892/mmr.2011.411. [DOI] [PubMed] [Google Scholar]
- 21.Li J, Song J, Jiang MH, Zheng JG, Gao SP, Zhu JH, Pan M. Interleukin-6 promoter polymorphisms and susceptibility to atrial fibrillation in elderly han chinese patients with essential hypertension. J Interferon Cytokine Res. 2012;32:542–547. doi: 10.1089/jir.2012.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao SP, Pan M, Chen C, Ge LJ, Jiang MH, Luan H, Zheng JG, Deng XT, Pan HY, Zhu JH. The G to A polymorphism at -597 of the interleukin-6 gene is extremely rare in southern Han Chinese. Cytokine. 2011;55:1–3. doi: 10.1016/j.cyto.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 23.Jiang MH, Su YM, Tang JZ, Shen YB, Deng XT, Yuan DS, Wu J, Pan M, Huang ZW. Angiotensin-converting enzyme gene 2350 G/A polymorphism and susceptibility to atrial fibrillation in Han Chinese patients with essential hypertension. Clinics (Sao Paulo) 2013;68:1428–1432. doi: 10.6061/clinics/2013(11)08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deng XT, Jiang MH, Zhu JH, Ge LJ, Guo J, Gao SP, Zheng JG, Luan H, Shi GL, Wang RX, Shi HF, Pan M. The Association of Interleukin 6-634C/G Polymorphism With Left Atrial Thrombus and Severe Spontaneous Echocontrast in Patients With Atrial Fibrillation. Clin Appl Thromb Hemost. 2013;19:673–678. doi: 10.1177/1076029612457706. [DOI] [PubMed] [Google Scholar]
- 25.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–122. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Caretta G, Passamonti E, Pedroni PN, Fadin BM, Galeazzi GL, Pirelli S. Outcomes and Predictors of Mortality Among Octogenarians and Older With ST-Segment Elevation Myocar- dial Infarction Treated With Primary Coronary Angioplasty. Clin Cardiol. 2014;37:523–529. doi: 10.1002/clc.22313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gharacholou SM, Lopes RD, Alexander KP, Mehta RH, Stebbins AL, Pieper KS, James SK, Armstrong PW, Granger CB. Age and outcomes in ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: findings from the APEX-AMI trial. Arch Intern Med. 2011;171:559–567. doi: 10.1001/archinternmed.2011.36. [DOI] [PubMed] [Google Scholar]
- 28.Wald DS, Morris JK, Wald NJ, Chase AJ, Edwards RJ, Hughes LO, Berry C, Oldroyd KG. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013;369:1115–1123. doi: 10.1056/NEJMoa1305520. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, Dedrick R, Gore JM. Prehospital Delay in Patients With Acute Coronary Syndromes (from the Global Registry of Acute Coronary Events [GRACE] ) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 30.Faxon D, Lenfant C. Timing is everything: motivating patients to call 9-1-1 at onset of acute myocardial infarction. Circulation. 2001;104:1210–1211. [PubMed] [Google Scholar]
- 31.McDermott MM, Mandapat AL, Moates A, Albay M, Chiou E, Celic L, Greenland P. Knowledge and attitudes regarding cardiovascular disease risk and prevention in patients with coronary or peripheral arterial disease. Arch Intern Med. 2003;163:2157–2162. doi: 10.1001/archinte.163.18.2157. [DOI] [PubMed] [Google Scholar]
- 32.Hamon M, Pristipino C, Di MC, Nolan J, Ludwig J, Tubaro M, Sabate M, Mauri-Ferre J, Huber K, Niemela K, Haude M, Wijns W, Dudek D, Fajadet J, Kiemeneij F. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care and Thrombosis of the European Society of Cardiology. EuroIntervention. 2013;8:1242–1251. doi: 10.4244/EIJV8I11A192. [DOI] [PubMed] [Google Scholar]
- 33.Louvard Y, Benamer H, Garot P, Hildick-Smith D, Loubeyre C, Rigattieri S, Monchi M, Lefevre T, Hamon M. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study) Am J Cardiol. 2004;94:1177–1180. doi: 10.1016/j.amjcard.2004.07.089. [DOI] [PubMed] [Google Scholar]
- 34.Achenbach S, Ropers D, Kallert L, Turan N, Krahner R, Wolf T, Garlichs C, Flachskampf F, Daniel WG, Ludwig J. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008;72:629–635. doi: 10.1002/ccd.21696. [DOI] [PubMed] [Google Scholar]


