Abstract
The present study aimed to evaluate the efficacy of photodynamic therapy with topical applied 5-aminolevulinic acid (ALA-PDT) for the treatment of cervical condylomata accuminate (CA). 161 Patients with cervical CA were randomly divided into ALA-PDT group and CO2 laser (control) group. Patients (n=89) in the ALA-PDT group were treated with topical 5% ALA under occlusive dressing for 3 h followed by irradiation with semiconductor laser at a dose of 1000 J/cm-2 and a power of 100 mW. Patients were treated 2 weeks later if necessary. Patients (n=72) in the control group were treated with CO2 laser. The treatment was repeated at 1-week interval when necessary. No response rate, complete response rate (CR) and recurrence rate of wart lesions as well as rate of eradication of HPVs were analyzed. The CR rate was 90.2% in the ALA-PDT group and 96.2% in the control group. The eradication rate was 90.2% in the ALA-PDT group and 65.8% in the control group after 3 months of follow-up. Both the eradication rate and recurrence rate in the ALA-PDT group were significantly lower than those in the control group (P<0.001). The adverse event in patients receiving ALA-PDT was mainly mild bleeding. ALA-PDT is a more effective and well-tolerated treatment for cervical CA compared with conventional CO2 laser therapy.
Keywords: 5-aminolaevulinic acid, cervical condylomata acuminate, photodynamic therapy
Introduction
Cervical condylomata acuminate (CA) are the most common sexually transmitted disease, which is caused by human papilloma virus (HPV) infection. Clinical evidence suggests that most sexually active adults will contract an HPV infection at least once in their life time [1]. Approximately 40 types of HPVs infect the anogenital region and those with oncogenic potential are classified as high-risk HPVs [1]. Some of them lead to not only genital warts but also low-grade squamous intraepithelial lesions (SILs), high-grades SILs and cervical cancer.
The ideal endpoint of treatment for cervical CA is to make lesions clear and never recur. However, conventional therapy could not eradicate HPV infection. For instance, the clearance rate of surgical excision is 72%, whereas the recurrence rate is 19~29%. Electric cauterization carries an excellent clearance of 94%, but with a recurrence of 22%. Although widely used, CO2 laser therapy is reported to have a clearance rate of 23~52% and a recurrence rate of 60~77% [2]. There are also kinds of side effects caused by the above therapies such as cervical incompetence and cervical canal stenosis. Thus attending physicians will consider all pros and cons associated with each therapeutic modality, including cost, convenience and compliance.
Fortunately, 5-aminolaevulinic acid (ALA)-mediated photodynamic therapy (PDT), a new and exciting therapeutic strategy has occurred and become widely used during the last decade. ALA is a precursor of the tissue photosensitizer protoporphyrin IX (PPIX) in the heme biosynthesis pathway [6]. The presence of an excess of exogenous ALA could bypass the feedback control and lead to increased accumulation of PPIX in mitochondria. Interestingly this occurred only in certain types of cells [4-6]. Animal experiments showed that the epidermal cells, pilosebaceous units, urothelium and endometrium of a mouse developed marked accumulation of PPIX and became photosensitive with systemic administration of ALA, whereas the dermis, blood vessels, cartilage of the ear and myometrium did not [5]. Clinical trials revealed that hyper-proliferative cells such as skin cancer lesions and infected cells with specific virus became photosensitized following local application of a solution of ALA, but normal tissue did not [5,6]. Such tissue specificity made it get over the prolonged skin photosensitivity defect of standard forms of photodynamic therapy and became widely used.
ALA-PDT has been considered as an effective means for the treatment of CA due to lower recurrence rate and less complications [7-10]. In the past 5 years, many patients with cervical CA have been treated with ALA-PDT and shown very good results especially those with multiple lesions and latent infection [11-13]. However, there is a lack of controlled clinical studies to evaluate efficacy and tolerability of this therapy. In this study, we compared the topical application of ALA-PDT with CO2 laser therapy to evaluate the efficacy of ALA-PDT.
Methods and materials
Study design
This was a randomized controlled trial that was performed during February 2008 to March 2014 at the Department of Dermatology in Huashan Hospital. Patients with a pathologic diagnosis of cervical CA were eligible for inclusion. All patients provided informed consents. This study was approved by the Ethical committee of Huashan Hospital and was conducted in accordance with Declaration of Helsinki.
Patients
Totally 161 patients recruited from the outpatient Department of Dermatology in Huashan Hospital with newly diagnosed cervical CA were enrolled in this study. The diagnosis was confirmed by colposcopy, histological examination and polymerase chain reaction. All patients had no systematic or topical treatment before this study.
Patients with the following conditions were excluded from the study: cutaneous sensitization, porphyria, immune deficiency or other severe systematic disease, congenital or acquired coagulation disorders, pregnancy or lactation. After treatment, patients were asked to abstain from tub bathing and sexual intercourse.
ALA-PDT therapy
All patients were randomly allocated into the ALA-PDT group and the control group. Patients in the ALA-PDT group (n=89) were asked to lie still in the lithotomy position. The vagina and cervix were cleaned with an aqueous 0.4% chlorhexidine solution. ALA powder (Zhangjiang Bio-Pharm Co. Ltd, Shanghai, China) was dissolved in sterile saline to make a 5% ALA-solution (w/v) immediately before use. A thin cotton swab was soaked in the ALA-solution and applied to the cervical mucosa to be in contact with and cover the warts and the adjacent normal skin (5-mm border). Then cling film was used to cover the cervix, and thick gauze was packed in the canal for light protection. After 3 hours of incubation, ALA was completely removed with sterile saline, and the lesions and adjacent normal skin (5-mm border) was exposed to a cylindrical laser fiber emitting a 635 nm semiconductor laser (KDL-300, Beijing Kedian Microwave Electronic Co. Ltd, Beijing, China) at a fluency of 1000 J/cm2 at 100 mw. Patients were treated two times at two-week intervals if necessary. Colposcopy was performed after treatment once a month and biopsy and HPV test were given 2 and 6 months after PDT.
CO2 laser therapy
For patients in the control group, lidocaine ointment was applied to the lesions after routine sterilization for topical anesthesia. After the lidocaine was removed with sterile saline, CO2 laser was given to vaporize the lesions and their adjacent normal skin (5 mm border). A repeat treatment was given at one-week interval where the lesions were not completely removed, but no more than three times totally was given. The follow-up was performed for the above groups.
Assessment of clinical efficacy
The indicators of efficacy were the clearance rate of wart lesions including complete remission rate (CR), partial remission rate (PR) and no response rate (NR), in addition to the clearance rate of HPV (HPV CR) which defined as no HPV infection was found until the endpoint of follow-up after treatment, as well as the recurrence rate (RR) and the incidence of adverse event. Treatment outcomes were classified as: CR: cervical lesions were completely cleared and the mucosa returned to normal looking; PR: lesion size reduced by 50% or more; NR: less than 50% reduction in lesion size [12].
Biopsy examination and genotyping analysis were performed for all patients at two month and six month after treatment respectively. An appearance of wart lesion after complete remission was defined as recurrence and was fixed by monthly colposcopy examination. Adverse events were asked to report at each follow-up during the study.
Statistical analysis
Analysis of all data was performed by SPSS 19.0 software. Comparison of mean was used to analysis the baseline characteristics between the two groups. Rank-sum test was used to evaluate the general efficacy of two treatments. The CR, NR, HPV CR and RR were analyzed with chi-square test. P<0.05 was considered to be significant in all statistical analyses.
Results
Demographical data of the patients
The age range of patients enrolled in this study was 18 to 64 years with an average of 30.2±9.0. The number of wart lesions ranged from 1 to 4 with an average of 1.72. All 161 participants were randomized divided into two groups. 89 patients were allocated into the ALA-PDT group and 72 patients into the CO2 laser (control) group. 146 of them completed the whole treatment and 6 months of follow-up, and 7 patients who did not finish 3 times of treatments were considered as “no response” to corresponding treatment. For the other 8 patients dropped out of the follow-up, data from their last visit were included in the analysis. Baseline characteristics including age, number of lesions, size of lesions and disease duration made no difference between groups.
Comparison of distribution of efficacy to lesions
Mann-Whitney U test was used to analyze the general distribution of efficacy to lesions between groups. The test statistic Z=-1.6, P=0.13, indicated no significant difference between groups (α=0.05).
Comparison of efficacy to wart lesions
We attempted to treat cervical CA with lower concentration of ALA and achieved satisfactory results (Figure 1).
Figure 1.
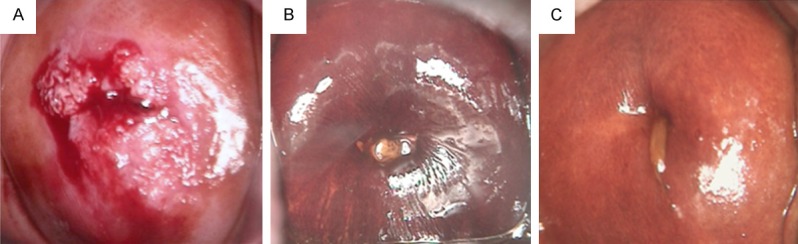
Cervical condylomata acuminate detected by colposcopy (lodine staining). Clinical appearance (A) before, (B) 2 months after and (C) 6 months after photodynamic therapy using 5-aminolaevulinic acid.
For CR, there was no statistical difference between ALA-PDT and control group (P=0.13), whereas NR rate showed statistical difference (P=0.42) (Table 1). The x2 was 4.1 and 2.2 for NR and CR, respectively.
Table 1.
Comparison of efficacy in the two treatments
| Group | NR (95% CI) | CR (95% CI) | HPV CR (95% CI) | RR (95% CI) |
|---|---|---|---|---|
| ALA-PDT | 7.3% (1.70%-12.93%) | 90.20% (83.76%-96.64%) | 90.20% (83.76%-96.64%) | 4.90% (0.23%-9.57%) |
| Control | 0 | 96.2% (91.98%-100.0%) | 65.80% (55.34%-76.26%) | 19.00% (10.35%-27.65%) |
NR: no response rate; CR: complete response rate; HPV CR: eradication rate of HPV infection; RR: recurrence rate.
Comparison of HPV eradication
The eradication of HPVs infection was defined as the negative result of biopsy examination and HPV DNA test at the end of the treatments and at 6 months during follow-up. The analysis of HPV CR rate of both groups showed marked statistical difference (x2=14.1, P<0.001) (Table 1). In addition, the RR also showed significant statistical different (x2=7.7, P=0.006).
Adverse events
In all patients with ALA-PDT treatment, only 2 underwent mild bleeding, no infection or cervical scaring occurred. But in the control group, 20 patients had bleeding during treatment. 5 patients got infection and 24 had cervical scaring (Table 2).
Table 2.
Adverse events in the two therapies
| Group | Bleeding | Infection | Cervical scaring |
|---|---|---|---|
| ALA-PDT | 2 (2.44%) | 0 | 0 |
| Control | 20 (25.32%) | 5 (6.33%) | 24 (30.38%) |
Discussion
In the present study, we found that after ALA-PDT therapy, both the CR rate and the HIV eradication rate were 90.2% in the ALA-PDT group. In addition, the eradication rate and recurrence rate in the ALA-PDT group were significantly lower than those in the control group. Although our study showed that ALA-PDT achieved CR rate to CO2 laser vaporization, the latter causing a higher frequency of side effects.
The action mechanism of ALA-PDT was to excite the accumulated PPIX which was increased by local ALA using specific light. The singlet oxygen and other free radicals from this course lead to necrosis and apoptosis of cells [4]. The maximum absorption band of porphyrins is in the blue light spectrum (405-415 nm). The weaker absorption bands are located in the green (506-540 nm), yellow (572-582 nm), and red spectra (628-635 nm) [16]. The 635 nm red light is clinically used due to both absorption rate and penetration depth.
There is a need for optimization of ALA concentrations and incubation time. The most widely used modality is 20% of ALA solution and 3 hours incubation [11-13], which is basically derived from the past reports and treatment of skin diseases [14]. However, cervical tissue is different with skin, which is lower in keratinization and stronger in penetration. In addition, previous research indicated that 5% to 10% ALA made optimal condition for the photodynamic therapy of urethral CA [15]. Since ALA was expensive to most people, we attempted to treat cervical CA with lower concentration of ALA and achieved satisfactory results.
CO2 laser treatment was considered to be the best method to remove lesions. However, in our study, we found that the clearance rate in ALA-PDT group and NR rate were not different from CO2 laser group. This result indicated that low concentration ALA-PDT can effectively eliminate CA.
In CA treatment, another important problem is recurrence rate. Based on our results, the recurrence rate in ALA-PDT group is much less than that in control group. There are only 2 patients in ALA-PDT group had slight bleeding. Moreover, there is no report on infection, cervical scar and menstrual disorder during the follow-up.
In general, ALA PDT therapy has significant advantages in HPV elimination and almost has no side effects. We concluded that, topical ALA-PDT, which is associated with a pretty lower RR and less adverse events versus CO2 laser therapy, is an effective, minimally invasive, and well-tolerated treatment for cervical CA, especially for patients with multiple lesions.
Disclosure of conflict of interest
None.
References
- 1.Bhatia N, Lynde C, Vender R, Bourcier M. Understanding genital warts: epidemiology, pathogenesis, and burden of disease of human papillomavirus. J Cutan Med Surg. 2013;17(Suppl 2):S47–54. [PubMed] [Google Scholar]
- 2.Lynde C, Vender R, Bourcier M, Bhatia N. Clinical features of external genital warts. J Cutan Med Surg. 2013;17(Suppl 2):S55–60. [PubMed] [Google Scholar]
- 3.Dougherty TJ, Kaufman JE, Goldfarb A, Weishaupt KR, Boyle D, Mittleman A. Photoradiation therapy for the treatment of malignant tumors. Cancer Res. 1978;38:2628–2635. [PubMed] [Google Scholar]
- 4.Iinuma S, Farshi SS, Ortel B, Hasan T. A mechanistic study of cellular photodestruction with 5-aminolaevulinic acid-induced porphyrin. Br J Cancer. 1994;70:21–28. doi: 10.1038/bjc.1994.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kennedy JC, Pottier RH, Pross DC. Photodynamic therapy with endogenous protoporphyrin IX: basic principles and present clinical experience. J Photochem Photobiol B. 1990;6:143–148. doi: 10.1016/1011-1344(90)85083-9. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy JC, Pottier RH. Endogenous protoporphyrin IX, a clinically useful photosensitizer for photodynamic therapy. J Photochem Photobiol B. 1992;14:275–292. doi: 10.1016/1011-1344(92)85108-7. [DOI] [PubMed] [Google Scholar]
- 7.SeFehr MK, Chapman CF, Krasieva T, Tromberg BJ, McCullough JL, Berns MW, Tadir Y. lective photosensitizer distribution in vulvar condyloma acuminatum after topical application of 5-aminolevulinic acid. Am J Obstet Gynecol. 1996;174:951–957. doi: 10.1016/s0002-9378(96)70332-0. [DOI] [PubMed] [Google Scholar]
- 8.Stefanaki IM, Georgiou S, Themelis GC, Vazgiouraki EM, Tosca AD. In vivo fluorescence kinetics and photodynamic therapy in condylomata acuminata. Br J Dermatol. 2003;149:972–976. doi: 10.1111/j.1365-2133.2003.05553.x. [DOI] [PubMed] [Google Scholar]
- 9.Kacerovska D, Pizinger K, Kumpova M, Cetkovska P. Genital warts treated by photodynamic therapy. Skinmed. 2007;6:295–297. doi: 10.1111/j.1540-9740.2007.06352.x. [DOI] [PubMed] [Google Scholar]
- 10.Nucci V, Torchia D, Cappugi P. Treatment of anogenital condylomata acuminata with topical photodynamic therapy: report of 14 cases and review. Int J Infect Dis. 2010;14(Suppl 3):e280–282. doi: 10.1016/j.ijid.2009.11.031. [DOI] [PubMed] [Google Scholar]
- 11.Liu YX, Zheng HY, Liu XR. 5-aminolaevulinic acid-photodynamic therapy for the treatment of cervical condylomata acuminata. Chin Med Sci J. 2009;24:151–155. doi: 10.1016/s1001-9294(09)60080-8. [DOI] [PubMed] [Google Scholar]
- 12.Wang HW, Zhang LL, Miao F, Lv T, Wang XL, Huang Z. Treatment of HPV infection-associated cervical condylomata acuminata with 5-aminolevulinic acid-mediated photodynamic therapy. Photochem Photobiol. 2012;88:565–569. doi: 10.1111/j.1751-1097.2011.01060.x. [DOI] [PubMed] [Google Scholar]
- 13.Chen MK, Luo DQ, Zhou H, Huang ZW, Zhang QF, Han JD. 5-aminolevulinic acid-mediated photodynamic therapy on cervical condylomata acuminata. Photomed Laser Surg. 2011;29:339–43. doi: 10.1089/pho.2010.2864. [DOI] [PubMed] [Google Scholar]
- 14.Szeimies RM, Karrer S, Sauerwald A, Landthaler M. Photodynamic therapy with topical application of 5-aminolevulinic acid in the treatment of actinic keratoses: an initial clinical study. Dermatology. 1996;192:246–251. doi: 10.1159/000246376. [DOI] [PubMed] [Google Scholar]
- 15.Wang XL, Wang HW, Huang Z, Stepp H, Baumgartner R, Dannecker C, Hillemanns P. Study of protoporphyrin IX (PpIX) pharmacokinetics after topical application of 5-aminolevulinic acid in urethral condylomata acuminata. Photochem Photobiol. 2007;83:1069–1073. doi: 10.1111/j.1751-1097.2007.00178.x. [DOI] [PubMed] [Google Scholar]
- 16.Mei X, Shi W, Piao Y. Effectiveness of photodynamic therapy with topical 5-aminolevulinic acid and intense pulsed light in Chinese acne vulgaris patients. Photodermatol Photoimmunol Photomed. 2013;29:90–96. doi: 10.1111/phpp.12031. [DOI] [PubMed] [Google Scholar]


